Abstract
Objectives
To examine race and sex-based variation in the associations between modifiable risk factors and incident heart failure (HF) among Southern Community Cohort Study (SCCS) participants.
Background
Low-income individuals in the southeastern United States have high HF incidence rates, but relative contributions of risk factors to HF are understudied in this population.
Methods
We studied 27,078 black or white SCCS participants (mean age 56 years, 69% black, 63% women) enrolled between 2002 and 2009, without prevalent HF, receiving Centers for Medicare or Medicaid Services (CMS). The presence of hypertension, diabetes mellitus, physical underactivity, high body mass index (BMI), smoking, high cholesterol, and poor diet was assessed at enrollment. Incident HF was ascertained using International Classification of Diseases, 9th revision codes 428.x in CMS data through December 31, 2010. Individual risk and population attributable risk (PAR) for HF for each risk factor was quantified using multivariable Cox models.
Results
During a median (25th, 75th percentile) 5.2 (3.1, 6.7) years, 4,341 (16%) participants developed HF. Hypertension and diabetes were associated with greatest HF risk, while hypertension contributed the greatest PAR, 31.8% (95% CI: 27.3% to 36.0%). In black participants, only hypertension and diabetes associated with HF risk; in white participants, smoking and high BMI also associated with HF risk. Physical underactivity was a risk factor only in white women.
Conclusions
In this high-risk low-income cohort, contributions of risk factors to HF varied, particularly by race. To reduce the population burden of HF, interventions tailored for specific race and sex groups may be warranted.
Keywords: diabetes, hypertension, low-income, physical activity, public health, Southeast
Introduction
Despite substantial advances in the prevention and treatment of cardiovascular disease, heart failure (HF) remains a major public health problem.(1,2) A large proportion of HF risk can be attributed to modifiable cardiovascular risk factors, suggesting HF may be preventable.(1) The American Heart Association identified seven modifiable risk factors, coined “Life’s Simple 7,” that substantially contribute to cardiovascular disease. These seven factors are hypertension, diabetes mellitus, smoking, high cholesterol, high body mass index (BMI), physical underactivity, and poor diet.(3) Though prior studies demonstrate that increasing burden of these seven risk factors is associated with greater risk for HF, the relative contribution of each risk factor to incident HF varies by study population.(4–6)
Quantifying the individual risk and population attributable risk (PAR) for HF for modifiable risk factors in different populations facilitates prioritization of both personalized and public health interventions. Most studies of HF risk factors have been conducted in predominantly middle-income, white cohorts from populations with relatively low rates of HF, such as the Framingham Heart Study (FHS), Olmsted County, MN, and the Atherosclerosis Risk in Communities (ARIC) study.(7)(8)(9) The relative contributions of modifiable risk factors to incident HF in high-risk low-income individuals and whether these vary by race and sex have been understudied. Within the United States, the greatest burden of HF is in the Southeast, known as the “HF belt.”(10) The Southern Community Cohort Study (SCCS) provides a unique opportunity to assess risk factors for HF in a low-income, predominantly black population in this region.(11) Thus, in the SCCS, we examined the risk of incident HF associated with the seven modifiable risk factors at the individual and population levels, overall and stratified by race-sex group.
Methods
Design and study sample
The SCCS is a prospective cohort study designed to investigate disparities in cancer and other chronic diseases in a low-income, underinsured population in the southeast United States, for which detailed methods have been published.(11) SCCS participants provided written informed consent, and protocols were approved by the Institutional Review Boards of Vanderbilt University Medical Center and Meharry Medical College. From 2002 to 2009, the study enrolled 84,797 participants, nearly two-thirds black, aged 40–79, living in 12 southeastern states. Approximately 86% of participants were recruited at community health centers (CHC) that provide care to underserved populations. The remaining 14% enrolled by completing questionnaires mailed to a random sample of the general population. At enrollment, participants provided demographic, lifestyle, and health history information and completed validated questionnaires on food frequency (FFQ) and physical activity.(12,13)
This analysis included 27,078 SCCS participants aged ≥65 years at enrollment (n=7,001) or <65 years at enrollment and (1) reported being covered by Centers for Medicare and Medicaid Services (CMS) on the baseline questionnaire or (2) did not report CMS coverage on the baseline questionnaire but had a CMS claim within 90 days of SCCS enrollment (n=20,077).(14) These inclusion criteria allowed identification of incident HF events through linkage with CMS claims files. Only black and non-Hispanic white participants were included because the small number of individuals in other racial groups did not allow for stable statistical analysis.(14) Participants with prevalent HF (n = 4,530) at enrollment were excluded.
Modifiable risk factors and other covariates
We used data from participants’ enrollment questionnaires to assess seven modifiable cardiovascular risk factors: hypertension, diabetes mellitus, high BMI, high cholesterol, smoking, poor diet, and physical underactivity. The presence of hypertension, diabetes, and high cholesterol was based on a participant’s self-reported history of a physician diagnosis of these conditions. Diet was characterized using FFQ data, which was used to calculate each participant’s Healthy Eating Index (HEI) 2010 score, which measures on a scale of 0 to 100 how well an individual’s diet aligns with the Dietary Guidelines for Americans 2010.(15,16) Poor diet was defined as HEI score in the lowest quintile in the overall analysis and within each race-sex group.(16,17) The remaining risk factors were defined in accordance with the American Heart Association’s definitions of ideal cardiovascular health, as high BMI (≥ 25 kg/m2), smoking (current smoking or quit within the past year), and physical underactivity (<150 minutes/week of moderate exercise or <75 min/wk of vigorous exercise or <150 min/wk of combined moderate or vigorous exercise).(3) Diagnosed hypertension was used instead of systolic blood pressure, as the latter was measured in a sub-sample of participants (n = 6,214 [23%]) at enrollment (Online Table 1). Several independent validation studies in the SCCS using nutrient biomarkers, accelerometers, and medical records have previously shown the reliability of self-reported variables such as diet, physical activity, and diabetes, respectively.(11–13)
Covariates were ascertained from enrollment questionnaire and included self-reported history of physician-diagnosed myocardial infarction (MI) or coronary artery bypass grafting (CABG) and stroke or transient ischemic attack (TIA), demographics (age, sex, race), socioeconomic characteristics (highest education level, annual household income, marital status), and enrollment source (CHC or general population).
Outcome ascertainment
HF events were identified via SCCS linkage with CMS Research Identifiable Files. Incident HF was defined as the first medical claim with an International Classification of Diseases, 9th revision (ICD-9) code of 428.x in the Medicare institutional, Part B carrier, outpatient-based claims files, or the Medicaid Analytic Extract Inpatient and Other Services claims files, from the SCCS enrollment date to December 31, 2010, as previously described.(14) Vital status was ascertained via SCCS linkage with the Social Security Administration vital status service and the National Death Index through December 31, 2010. Censoring occurred at the date of HF event, date of death, or December 31, 2010, whichever occurred first.(14)
Statistical analysis
Participants were categorized into four race-sex groups, as black male, black female, white male, and white female. Enrollment characteristics were summarized as median (25th, 75th percentile) or count (percentage). In the subset of participants in whom duration of diabetes and blood pressure were available, racial differences in these factors were compared using the Wilcoxon rank-sum test. A cumulative (summed) score of the number of the seven modifiable risk factors was calculated for each participant. To assess incremental risk for HF associated with accumulating number of risk factors, this score was included as an ordinal variable in a multivariable Cox proportional hazard model adjusted for age, sex, race, history of MI or CABG, history of stroke or TIA, education (<high school, high school/vocational training/junior college/some college, college degree or higher), annual household income (<$15,000, $15,000-$24,999, ≥$25,000), marital status (married or living as married with partner, separated/divorced, widowed, single), and enrollment source (CHC, general population).(14) Next, the risk of incident HF associated with each of the seven modifiable risk factors was assessed using multivariable-adjusted Cox proportional hazards models using robust variance that included each of the seven modifiable risk factors and all of the aforementioned covariates. Population attributable risk (PAR) and 95% CI was calculated using the punafcc package in Stata that utilizes the multivariable-adjusted hazard ratios from the Cox models. Analyses were conducted in the cohort of 27,078 individuals and each race-sex group. Analyses were repeated after excluding participants with a history of MI or CABG at baseline. Analyses were performed using R (The R project, Vienna, Austria) or Stata v.13.0 (Stata Corp., College Station, TX).
Results
Prevalence of seven risk factors
Of the 27,078 SCCS participants included in this study, 68.8% were black, 62.6% were women, and 69.7% had an annual household income below $15,000 (Table 1). Most participants had hypertension, were overweight or obese, and were physically underactive. Other risk factors were also common, with diabetes, high cholesterol, and smoking present in 26.5%, 39.5%, and 43.4% of participants, respectively. Nearly 99% of participants had one or more of the seven modifiable risk factors, with a median number of 3 (25th to 75th percentile 3 to 4). Prevalence of the seven modifiable risk factors varied by race-sex group. Duration of diabetes was greater in black than white participants, p < 0.001. Similarly, blood pressure was greater in black compared with white participants, p < 0.001, in the subset who had this measured at enrollment (Online Table 1).
Table 1.
Baseline Characteristics of 27,078 Southern Community Cohort Study Participants Receiving Medicare or Medicaid, Overall and by Race and Sex
| Overall n = 27,078 |
Black Men n = 6,936 |
Black Women n = 11,688 |
White Men n = 3,202 |
White Women n = 5,252 |
|
|---|---|---|---|---|---|
| Age, years | 54 (47−65) | 53 (47−61) | 53 (45−63) | 60 (49−67) | 58 (48−66) |
| Hypertension | 62.5 | 60.5 | 67.6 | 56.7 | 57.0 |
| Diabetes mellitus | 26.5 | 23.8 | 29.8 | 23.8 | 24.3 |
| Duration of diabetes, years | 7.0 (3.0−15.0) | 7.0 (3.0−14.0) | 8.0 (3.0–16.0) | 6.0 (3.0−13.8) | 7.0 (3.0−14.0) |
| Body mass index, kg/m2 | 29.1 (24.9−34.6) | 26.6 (23.3−30.9) | 31.3 (26.6−37.1) | 27.6 (24.4−31.8) | 29.3 (24.9−35.1) |
| Body mass index ≥ 25 kg/m2 | 74.3 | 63.1 | 82.1 | 70.7 | 74.2 |
| High cholesterol | 39.5 | 31.0 | 38.0 | 47.1 | 49.5 |
| Current smoker* | 43.4 | 56.9 | 37.5 | 42.2 | 39.2 |
| Healthy eating index score | 57.9 (49.5−66.5) | 55.0 (47.6−62.7) | 59.4 (51.4−67.7) | 55.6 (46.9−64.7) | 59.9 (50.5−69.1) |
| Underactive† | 85.4 | 81.6 | 88.1 | 80.4 | 87.3 |
| Median risk score‡ | 3 (3,4) | 3 (2,4) | 4 (3, 4) | 3 (2, 4) | 3 (3, 4) |
| History of MI/CABG | 8.6 | 8.6 | 6.1 | 17.7 | 8.6 |
| History of stroke/TIA | 9.6 | 9.4 | 9.1 | 10.8 | 10.0 |
| Annual Income | |||||
| <$15,000 | 69.7 | 71.8 | 74.5 | 53.4 | 65.9 |
| $15,000-$24,999 | 18.0 | 17.9 | 18.3 | 16.9 | 18.2 |
| ≥$25,000 | 12.3 | 10.4 | 7.2 | 29.7 | 15.9 |
| Education | |||||
| Less than high school | 38.4 | 44.2 | 40.4 | 29.0 | 32.0 |
| High school/vocational training/some college | 53.1 | 49.0 | 53.1 | 53.1 | 58.7 |
| College degree | 8.5 | 6.8 | 6.5 | 17.9 | 9.4 |
| Marital Status | |||||
| Single | 21.8 | 29.6 | 25.3 | 14.5 | 7.9 |
| Widowed | 14.4 | 5.6 | 19.6 | 5.3 | 20.0 |
| Separated/divorced | 34.0 | 33.0 | 34.8 | 27.2 | 37.7 |
| Married/living as married with partner | 29.8 | 31.7 | 20.3 | 53.0 | 34.5 |
Values for binary variables are displayed as percentages, and values for continuous variables are displayed as median (25th percentile-75th percentile). Prevalence of the Life’s Simple 7 risk factors (hypertension, diabetes, BMI≥25, high cholesterol, current smoking, poor diet, and physical underactivity) was compared among the four race-sex groups using Pearson’s chi -squared tests, with all p<0.001. Healthy eating index score was the most missing variable with 6.51% missing.
Defined as smoking presently or within the past year, in accordance with the American Heart Association’s definitions of ideal cardiovascular health.(3)
Defined as <150 minutes/week of moderate exercise or <75 min/wk of vigorous exercise or <150 min/wk of combined moderate or vigorous exercise.(3)
Defined as median number of Life’s Simple 7 risk factors. Participants with missing values for any risk factor were assumed not to have that risk factor, and it was assigned a value of zero.
Heart failure risk associated with seven modifiable factors
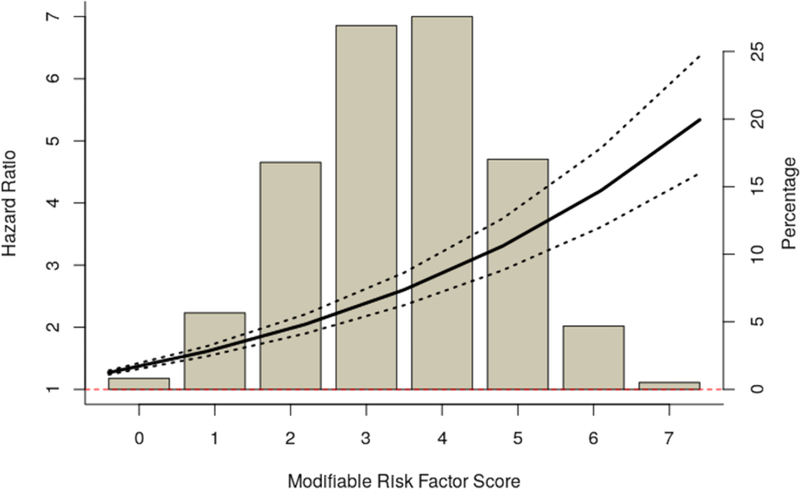
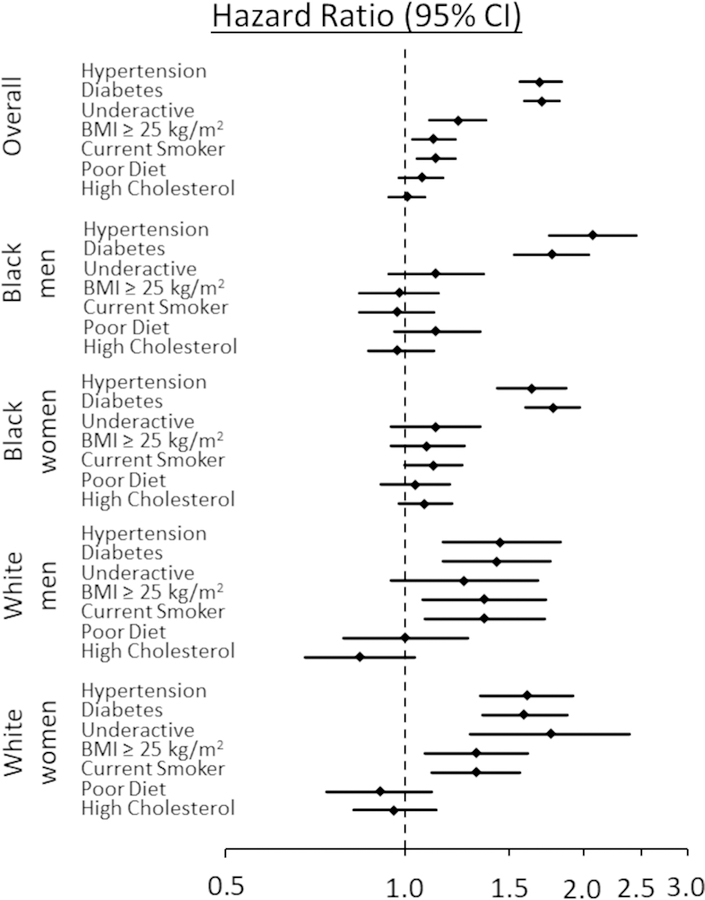
Over a median follow-up of 5.2 years (range 0.1 to 8.8 years), 4,341 (16.0%) participants developed HF. The accumulation of modifiable risk factors associated with increasing HF risk, with a 27% increase (95% CI: 24% to 30%) for every additional risk factor (Figure 1). In an analysis of the individual seven modifiable factors, hypertension and diabetes were associated with the greatest risks for HF overall, with HRs of 1.69 (95% CI: 1.56 to 1.84) and 1.70 (95% CI: 1.59 to 1.82), respectively (Figure 2 and Online Table 2). Physical underactivity, high BMI, and smoking associated with modestly increased risk for HF, while poor diet and high cholesterol did not.
Figure 1. Distribution of Risk Factor Scores and Cumulative Risk of Heart Failure Associated with Risk Factor Score.
The histogram depicts the frequency distribution of cumulative score for number of unhealthy modifiable risk factors, ranging from 0 to 7, with the percentage of individuals with each score shown on the right axis. Spline plot depicts the hazard ratio (HR, dark band) and 95% confidence interval (dashes). HRs (left axis) are from Cox models adjusted for age, race, sex, history of MI or CABG, history of stroke or TIA, education, income, marital status, and enrollment source. Missing values for any individual risk factor were assigned a value of zero.
Figure 2. Association of Modifiable Risk Factors and Incident Heart Failure, Overall and by Race-Sex Group.
Results are from Cox models adjusted for the variables shown and age, history of MI or CABG, history of stroke or TIA, education, income, marital status, and enrollment source. The model for the overall population was also race and sex adjusted.
In analyses by race-sex groups, (Figure 2 and Online Table 2), among black men and women, hypertension and diabetes were the only modifiable factors significantly associated with HF risk. In white participants, hypertension, diabetes, high BMI and smoking significantly associated with HF risk in both men and women. Physical underactivity significantly associated with HF risk in white women (HR 1.76, 95% CI: 1.29 to 2.39) and trended towards significance in white men (HR 1.26, 95% CI: 0.95 to 1.68). Consistent with the overall results, poor diet and high cholesterol did not significantly associate with HF risk in any race-sex group.
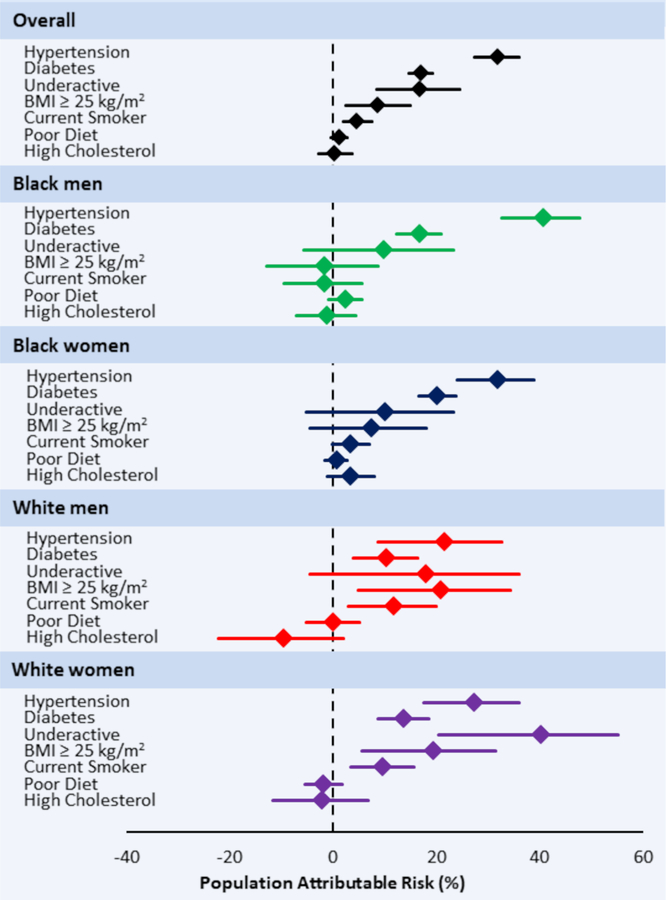
Population attributable risk for heart failure of seven risk factors
Overall, hypertension contributed the greatest population burden of incident HF, with a PAR of 31.8% (95% CI: 27.3% to 36.0%; Central Illustration and Online Table 2). Diabetes and physical underactivity contributed similarly to HF risk, with PARs of 17.0% (95% CI: 14.7% to 19.2%) and 16.9% (95% CI: 8.4% to 24.5%), respectively. High BMI and smoking accounted for a modest proportion of the population risk for HF, while poor diet and high cholesterol had nonsignificant PARs.
Central Illustration. Modifiable Risk Factors and Incident Heart Failure: Forest Plots of Population Attributable Risk Overall and by Race-Sex Group.
Population attributable risk results are calculated from risk factor prevalence and Cox models adjusted for the variables shown and age, history of MI or CABG, history of stroke or TIA, education, income, marital status, and enrollment source. The model for the overall population was also race and sex adjusted.
In all race-sex groups, hypertension and diabetes contributed significantly to the population burden of HF, and among black participants, these were the only risk factors with significant PARs. In black men and women, hypertension had the highest PAR compared with other risk factors, 40.7% (95% CI: 32.6% to 47.8%) and 31.8% (95% CI: 24.1% to 38.8%), respectively. In white men and women, high BMI accounted for a significant proportion of the population risk for HF, with respective PARs of 20.9% (95% CI: 4.8% to 34.2%) and 19.5% (5.5% to 31.4%). Among white men and women, smoking also had significant PARs of 11.9% (95% CI: 3.0% to 19.9%) and 9.7% (95% CI: 3.5% to 15.6%), respectively. Physical underactivity was significant only among white women, with a PAR of 40.2% (95% CI: 20.4% to 55.1%).
Restriction to participants without a history of MI or CABG at baseline
In the overall analysis, history of MI or CABG associated with a greater than two-fold increased risk for HF (HR of 2.06 [95% CI: 1.88 to 2.25]) (Table 2). The results did not substantially change in analyses restricted to participants without a history of MI or CABG at baseline (n = 24,689), (Online Figure 1). Hypertension and diabetes remained significantly associated with the risk of incident HF overall and in blacks and whites. Among black participants, these were the only modifiable factors associated with increased risk of incident HF. In white men and women, smoking and high BMI were also associated with higher HF risk, as was physical underactivity in white women.
Table 2.
Association and Population Attributable Risk of History of Myocardial Infarction or Coronary Artery Bypass Graft and Incident Heart Failure
| Prevalence among HF cases, % | HR (95% CI) | P value | PAR, % (95% CI) | |
|---|---|---|---|---|
| Overall | 17.79 | 2.06 (1.88 to 2.25) | <0.001 | 9.1 (7.8 to 10.4) |
| Black men | 19.63 | 2.42 (2.04 to 2.88) | <0.001 | 11.6 (8.9 to 14.3) |
| Black women | 12.49 | 1.95 (1.68 to 2.26) | <0.001 | 6.4 (4.7 to 8.0) |
| White men | 32.29 | 1.83 (1.46 to 2.29) | <0.001 | 13.7 (8.2 to 19.0) |
| White women | 18.87 | 2.19 (1.79 to 2.68) | <0.001 | 9.9 (6.8 to 12.9) |
Results are from Cox models adjusted for all 7 modifiable risk factors as well as age, history of stroke or TIA, education, income, marital status, and enrollment source. The model for the overall population was also adjusted for race and sex. All other models were stratified by race and sex.
Discussion
In a large, low-income high-risk cohort of black and white adults from the southeastern United States, we examined the associations between seven modifiable risk factors and incident HF. While the accumulation of modifiable risk factors associated with increasing HF risk, the relative contributions of each factor to HF risk substantially varied in magnitude and by race and sex. Hypertension and diabetes were associated with increased HF risk in both black and white individuals. In black men and women, these were the only two factors significantly associated with HF risk, while in white individuals, smoking and high BMI also related to increased risk of HF. Additionally, among white women, physical underactivity was a particularly strong modifiable risk factor for HF, with a HR similar to that of hypertension and diabetes and a PAR exceeding that of diabetes. These findings may help prioritize individualized and public health interventions aimed at preventing HF, particularly in resource-limited areas with the greatest risk of HF.
The highest rates of HF in the US are in the Southeast, causing it to be known as the “HF belt.”(10,18) In the SCCS, HF incidence rates are 2 to 10 times higher than in the Cardiovascular Health Study (CHS), Multi-Ethnic Study of Atherosclerosis (MESA), ARIC study, and others, which may be attributable, in part, to a disproportionately high burden of modifiable risk factors.(14,18) For example, the prevalence of hypertension is 62.5% in the SCCS compared with 42%, 33%, and 7% in MESA, ARIC, and FHS cohorts, respectively.(14) Prior studies have shown that controlling modifiable risk factors for HF leads to a significant reduction in HF incidence.(19,20) Thus, examining the associations between modifiable risk factors and HF can inform providers’ and patients’ decisions regarding lifestyle and pharmacologic interventions targeted towards HF risk reduction. Further, examining PARs of modifiable risk factors helps prioritize public health interventions by estimating the proportion of HF cases that could be prevented if the risk factor were eliminated from a particular population. Our SCCS population included individuals and communities at highest risk for HF, including blacks and low-income individuals underrepresented in prior studies, who utilize publicly funded healthcare resources, i.e. CMS, thereby representing a group in whom personalized and population-based approaches may be most impactful.
In our study, hypertension and diabetes were equally important for individuals’ risk of HF. Hypertension contributed the greatest burden of HF at the population level, however, accounting for approximately one-third of the PAR for HF. Similarly, in 5143 FHS and Framingham Offspring Study participants, hypertension accounted for the greatest PAR for HF, 39% and 59% in men and women, respectively.(7) In 5761 National Health and Nutrition Examination Survey (NHANES) participants, hypertension also associated with the greatest risk for HF, although PAR was not estimated.(21) In a case-control study of 962 incident HF cases in Olmsted County, MN, hypertension was the modifiable risk factor with the greatest PAR in the overall population and in women, 20% and 28%, respectively; in men, smoking was the modifiable risk factor with the greatest PAR, 22%.(8) In contrast, in the ARIC study, diabetes was associated with a larger incidence rate difference (IRD) for HF than hypertension, smoking, high low-density lipoproteins (LDL), or obesity; a pattern consistent in both black and white participants.(9) In the CHS, physical underactivity, smoking, and obesity were associated with a greater risk of HF, while diet was not, consistent with our findings in white individuals.(22) Among 4195 black individuals in the Jackson Heart Study (JHS), hypertension, diabetes, physical inactivity, and smoking contributed to individuals’ risk of incident HF.(6) Socioeconomic differences between the JHS population and our study population, which had a lower average income and education level, may explain why chronic diseases have higher relative importance than other modifiable risk factors in our population.(23,24) Collectively, the variance in individual risk and PAR across studies suggests a need for risk factor modification strategies that are uniquely aligned to individual and local population characteristics.
In our study, racial differences were evident in the relative contributions of modifiable risk factors to incident HF. In whites, several modifiable risk factors associated with increased risk for HF, but in blacks, hypertension and diabetes were the only risk factors which were significantly associated. This racial difference may be in part because the Life’s Simple 7 were largely derived from predominantly white cohorts, so the definitions of ideal cardiovascular health for each risk factor may be most applicable to white individuals. The observed difference may also be due to the increased severity of hypertension and earlier onset of diabetes in black compared with white participants.(25)
Among white women, physical underactivity was a particularly strong risk factor for HF, accounting for approximately 40% of the PAR. Prior studies have suggested the importance of physical underactivity as a HF risk factor in women. In the Women’s Health Initiative study of 84,537 post-menopausal, predominantly white women (nearly 85%), physical underactivity was shown to have a significant, dose-dependent association with HF risk.(26) The Swedish Mammography Cohort had similar results; namely, women who walked or bicycled for >20 minutes per day were 29% less likely to develop HF compared with women who did not.(27) In the prospective NHANES I Epidemiologic Follow-up Study, physical underactivity was associated with an increased risk for HF in women but not in men, consistent with our results.(28) These prior studies did not, however, examine the combined effect of race and sex on the association between physical activity and incident HF. We found physical underactivity was not a significant risk factor for HF among black women, even though the prevalence of physical underactivity was nearly equal (~88%) in black and white women. Our results contrast with the ARIC study in which the association between physical activity and HF incidence did not differ by race, though stratification by sex was not reported.(29)
Patients may lower their risk of HF the most through prevention and control of hypertension and diabetes. This finding appears particularly important for black individuals; however, it does not diminish the importance of other lifestyle factors, such as physical activity and a healthy diet, for maintaining health and preventing other chronic diseases. Further, our results suggest that public health measures targeting hypertension, in particular, are critical to reducing the burden of HF in our low-income high-risk population. Priority should be given to population-wide efforts to reduce the prevalence of hypertension, which accounted for nearly one-third of our population’s HF cases. Moreover, our analyses by race and sex can inform public health campaigns designed to appeal to specific subgroups. For example, measures to decrease HF incidence by promoting physical activity may be particularly effective in white women. Our results suggest that focused strategies based on prioritization of modifiable risk factors for HF in low-resource settings are needed, especially in the southeastern US, to better address the disproportionate burden of HF in this region.
Study limitations
Low-income individuals from the southeastern United States who self-identify as black or white comprised most of our study population. Results may not be generalizable to individuals of higher socioeconomic status or other racial groups. Although the presence of HF risk factors and other covariates was ascertained from participants’ self-reports, several independent validation studies have shown the reliability of self-reported variables used in the SCCS.(11,14) HF events were identified using ICD-9 codes 428.x in CMS Research Identifiable Files, as previously reported(14) and aligned with validated methods (positive predictive value > 90%) utilized in other cohort studies.(30,31) Participants receiving CMS at or within 90 days of enrollment were assumed to receive CMS throughout the study period. Though inclusion of individuals receiving CMS may result in over-representation of groups with potentially elevated HF risk, i.e. individuals aged ≥ 65 years or on dialysis, this does not negate the findings. Notably, the mean age of our subpopulation (55.5 years) was similar to the mean age of the overall SCCS (52.6 years).(14,32) Finally, residual confounding and the influence of other risk factors cannot be excluded due to the observational study design.
Conclusions
In this low-income high-risk population from the southeastern United States, the accumulation of modifiable risk factors associated with increasing HF risk, but individual risk factors had variable contributions to incident HF, with distinct race-sex differences. By defining the relative contributions of modifiable risk factors to HF by race and sex, our findings may help prioritize clinical and public health approaches to reduce the incidence of HF in this resource-limited setting.
Supplementary Material
Clinical Perspectives.
Competency in Patient Care:
Race-sex specific variation in the associations between modifiable risk factors and heart failure may inform individualized care plans aimed at heart failure risk reduction.
Competency in Systems-Based Practice:
Reducing the prevalence of hypertension should receive priority among population-wide efforts to reduce the burden of heart failure in high-risk low-income black and white individuals in the southeastern United States.
Translational Outlook:
The prevention of heart failure, and likely other chronic cardiovascular diseases, will require alignment of personalized and public health approaches with underlying race and sex-based variation in disease susceptibility.
Acknowledgements:
The authors would like to thank all SCCS participants and the SCCS research team.
Sources of Funding: The Southern Community Cohort Study is supported by the National Cancer Institute (grants R01 CA092447 and U01 CA202979) and supplemental funding from the American Recovery and Reinvestment Act (3R01 CA029447-0851). Data collection was performed by the Survey and Biospecimen Shared Resource which is supported by the Vanderbilt-Ingram Cancer Center in Nashville, TN (P30 CA68485). DKG is supported by K23 HL128928-01A1.
Abbreviations:
- BMI
body mass index
- CABG
coronary artery bypass graft
- HF
heart failure
- MI
myocardial infarction
- PAR
population attributable risk
- SCCS
Southern Community Cohort Study
- TIA
transient ischemic attack
Footnotes
Disclosures: There are no relationships with industry.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Benjamin EJ, Virani SS, Callaway CW et al. Heart Disease and Stroke Statistics-2018 Update: A Report From the American Heart Association. Circulation 2018;137:e67–e492. [DOI] [PubMed] [Google Scholar]
- 2.Heidenreich PA, Albert NM, Allen LA et al. Forecasting the impact of heart failure in the United States: a policy statement from the American Heart Association. Circulation Heart failure 2013;6:606–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lloyd-Jones DM, Hong Y, Labarthe D et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association’s strategic Impact Goal through 2020 and beyond. Circulation 2010;121:586–613. [DOI] [PubMed] [Google Scholar]
- 4.Folsom AR, Shah AM, Lutsey PL et al. American Heart Association’s Life’s Simple 7: Avoiding Heart Failure and Preserving Cardiac Structure and Function. Am J Med 2015;128:970–6 e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ogunmoroti O, Oni E, Michos ED et al. Life’s Simple 7 and Incident Heart Failure: The Multi-Ethnic Study of Atherosclerosis. J Am Heart Assoc 2017;6. [DOI] [PMC free article] [PubMed]
- 6.Spahillari A, Talegawkar S, Correa A et al. Ideal Cardiovascular Health, Cardiovascular Remodeling, and Heart Failure in Blacks: The Jackson Heart Study. Circulation Heart failure 2017;10. [DOI] [PMC free article] [PubMed]
- 7.Levy D, Larson MG, Vasan RS, Kannel WB, Ho KK. The progression from hypertension to congestive heart failure. JAMA 1996;275:1557–62. [PubMed] [Google Scholar]
- 8.Dunlay SM, Weston SA, Jacobsen SJ, Roger VL. Risk factors for heart failure: a population-based case-control study. Am J Med 2009;122:1023–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Avery CL, Loehr LR, Baggett C et al. The population burden of heart failure attributable to modifiable risk factors: the ARIC (Atherosclerosis Risk in Communities) study. J Am Coll Cardiol 2012;60:1640–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mujib M, Zhang Y, Feller MA, Ahmed A. Evidence of a “heart failure belt” in the southeastern United States. Am J Cardiol 2011;107:935–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Signorello LB, Hargreaves MK, Blot WJ. The Southern Community Cohort Study: investigating health disparities. J Health Care Poor Underserved 2010;21:26–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Buchowski MS, Matthews CE, Cohen SS et al. Evaluation of a questionnaire to assess sedentary and active behaviors in the Southern Community Cohort Study. J Phys Act Health 2012;9:765–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Signorello LB, Munro HM, Buchowski MS et al. Estimating nutrient intake from a food frequency questionnaire: incorporating the elements of race and geographic region. Am J Epidemiol 2009;170:104–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Akwo EA, Kabagambe EK, Wang TJ et al. Heart Failure Incidence and Mortality in the Southern Community Cohort Study. Circulation Heart failure 2017;10. [DOI] [PMC free article] [PubMed]
- 15.Guenther PM, Casavale KO, Reedy J et al. Update of the Healthy Eating Index: HEI-2010. J Acad Nutr Diet 2013;113:569–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yu D, Sonderman J, Buchowski MS et al. Healthy Eating and Risks of Total and Cause-Specific Death among Low-Income Populations of African-Americans and Other Adults in the Southeastern United States: A Prospective Cohort Study. PLoS Med 2015;12:e1001830; discussion e1001830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sotos-Prieto M, Bhupathiraju SN, Mattei J et al. Association of Changes in Diet Quality with Total and Cause-Specific Mortality. N Engl J Med 2017;377:143–153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Liu L, Yin X, Chen M, Jia H, Eisen HJ, Hofman A. Geographic Variation in Heart Failure Mortality and Its Association With Hypertension, Diabetes, and Behavioral-Related Risk Factors in 1,723 Counties of the United States. Front Public Health 2018;6:132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Djousse L, Driver JA, Gaziano JM. Relation between modifiable lifestyle factors and lifetime risk of heart failure. JAMA 2009;302:394–400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Grodin JL, Tang WH. Treatment strategies for the prevention of heart failure. Curr Heart Fail Rep 2013;10:331–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Komanduri S, Jadhao Y, Guduru SS, Cheriyath P, Wert Y. Prevalence and risk factors of heart failure in the USA: NHANES 2013 – 2014 epidemiological follow-up study. J Community Hosp Intern Med Perspect 2017;7:15–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Del Gobbo LC, Kalantarian S, Imamura F et al. Contribution of Major Lifestyle Risk Factors for Incident Heart Failure in Older Adults: The Cardiovascular Health Study. JACC Heart Fail 2015;3:520–528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bruce MA, Beech BM, Crook ED et al. Association of socioeconomic status and CKD among African Americans: the Jackson Heart Study. Am J Kidney Dis 2010;55:1001–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Walker RJ, Strom Williams J, Egede LE. Influence of Race, Ethnicity and Social Determinants of Health on Diabetes Outcomes. Am J Med Sci 2016;351:366–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sampson UK, Edwards TL, Jahangir E et al. Factors associated with the prevalence of hypertension in the southeastern United States: insights from 69,211 blacks and whites in the Southern Community Cohort Study. Circ Cardiovasc Qual Outcomes 2014;7:33–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Agha G, Loucks EB, Tinker LF et al. Healthy lifestyle and decreasing risk of heart failure in women: the Women’s Health Initiative observational study. J Am Coll Cardiol 2014;64:1777–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rahman I, Bellavia A, Wolk A. Relationship between physical activity and heart failure risk in women. Circulation Heart failure 2014;7:877–81. [DOI] [PubMed] [Google Scholar]
- 28.He J, Ogden LG, Bazzano LA, Vupputuri S, Loria C, Whelton PK. Risk factors for congestive heart failure in US men and women: NHANES I epidemiologic follow-up study. Arch Intern Med 2001;161:996–1002. [DOI] [PubMed] [Google Scholar]
- 29.Bell EJ, Lutsey PL, Windham BG, Folsom AR. Physical activity and cardiovascular disease in African Americans in Atherosclerosis Risk in Communities. Med Sci Sports Exerc 2013;45:901–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Saczynski JS, Andrade SE, Harrold LR et al. A systematic review of validated methods for identifying heart failure using administrative data. Pharmacoepidemiol Drug Saf 2012;21 Suppl 1:129–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rector TS, Wickstrom SL, Shah M et al. Specificity and sensitivity of claims-based algorithms for identifying members of Medicare+Choice health plans that have chronic medical conditions. Health Serv Res 2004;39:1839–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cohen SS, Signorello LB, Cope EL et al. Obesity and all-cause mortality among black adults and white adults. Am J Epidemiol 2012;176:431–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.