Abstract
Cancer is a devastating disease that has claimed many lives. Natural bioactive agents from plants are gaining wide attention for their anticancer activities. Several studies have found that natural plant-based bioactive compounds can enhance the efficacy of chemotherapy, and in some cases ameliorate some of the side-effects of drugs used as chemotherapeutic agents. In this paper, we have reviewed the literature on the anticancer effects of four plant-based bioactive compounds namely, curcumin, myricetin, geraniin and tocotrienols (T3) to provide an overview on some of the key findings that are related to this effect. The molecular mechanisms through which the active compounds may exert their anticancer properties in cell and animal-based studies also discussed.
Keywords: bioactive compounds, anticancer, curcumin, myricetin, geraniin, tocotrienols
1. Introduction
Cancer is one of the leading causes of death in the world. Cancer burden is measured based on cancer incidence and mortality. The International Agency for Research on Cancer (IARC) reported the 5-year global cancer prevalence of worldwide burden of 27 cancers for the year 2008 to be 28.8 million with 12.7 million new cancer cases and 7.6 million cancer deaths [1]. Some of the major cancer cases reported were lung (1.61 million), breast (1.38 million) and colorectal (1.23 million) cancers [2]. In addition, it was estimated that there would be 14.1 million new cancer cases and 8.2 million deaths in 2012 worldwide [3]. According to a recent global cancer statistic, there will be 18.1 million new cancer cases and 9.6 million cancer deaths [4], with lung cancer being the leading cause of death followed by breast, colorectal, stomach and liver cancer (Table 1) [4].
Table 1.
Cancer global statistics 2018.
| Cancer Types | Deaths | New Cases |
|---|---|---|
| Lung | 1.76 million | 2.09 million |
| Stomach | 782,685 | 1.03 million |
| Liver | 781,631 | 841,080 |
| Breast | 626,679 | 2.02 million |
| Colon | 551,269 | 1.09 million |
| Esophagus | 508,585 | 572,034 |
| Pancreas | 432,242 | 458,918 |
| Prostate | 358,989 | 1.27 million |
| Source: [4] | ||
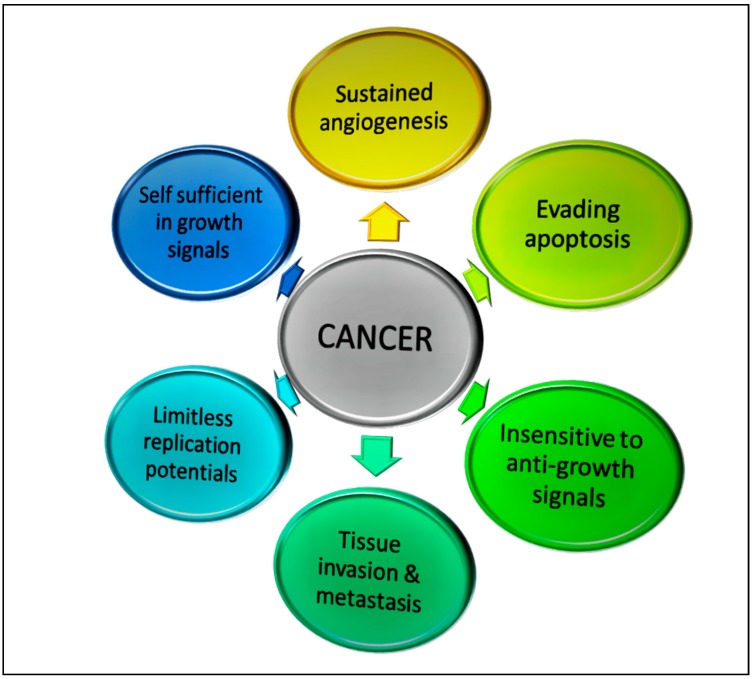
Cancers could result from inflammatory processes that are driven by rapid growth of intrinsic (self) origin. Some of the common hallmark features of cancers are shown in Figure 1. These include the ability of cancer cells to (i) evade apoptosis [5]; (ii) induce angiogenesis [6]; (iii) replicate limitlessly [7,8]; (iv) produce growth signals that are self-sufficient [9]; (v) be insensitive to anti-growth signals [10]; and (vi) invade tissue and metastasis [11,12]. These attributes allow the cancer cells to have limitless growth, prolonged survival and the ability to invade tissues. If these processes are not inhibited, the cancer cells can continue to grow and invade and eventually kill the cancer patient.
Figure 1.
Hallmark features of tumors that allow them to grow uncontrollably and metastasize.
At present, various therapeutic approaches such as surgery, chemotherapy drugs and/or radiation are used to treat cancers. Whilst the chemotherapeutic drugs used in the treatment of cancer can provide temporary relief to the cancer patients and help prolong their life [13,14,15], many of these drugs exhibit side-effects [16,17].
2. Anti-Tumor Immune Responses
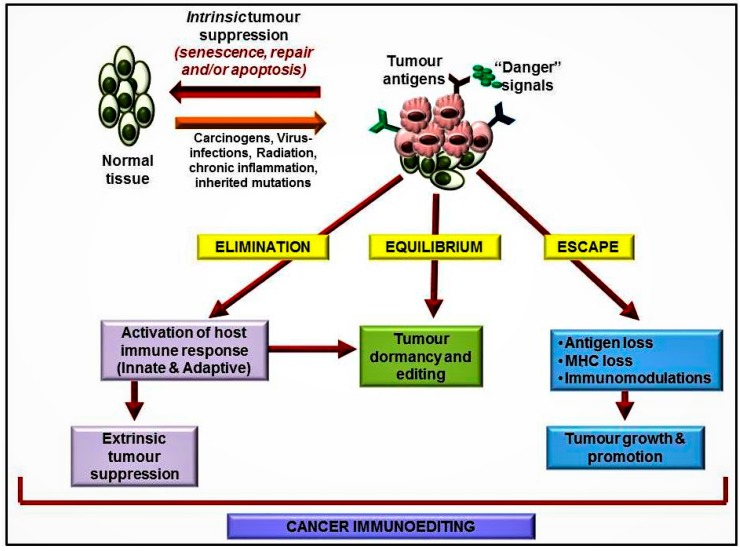
Activation of host immune system is a natural way for cancer patients to fight this disease. Several studies have shown that cells of the immune system can recognize and destroy tumor cells [18]. The process through which the immune system carries out this function is known as immunosurveillance [19]. As shown in Figure 2, continuous immunosurveillance takes place in the body to help the immune system to deal with “rogue” or abnormal cells. The outcome of this response is regulated by a process known as immunoediting. Cancer immunoediting refers to the dual role played by the immune system in host protection and promotion of tumor growth. Cancer immunoediting consists of three phases, which are elimination, equilibrium and escape [20,21]. If the immune system is appropriately activated, tumor growth can be inhibited and they can be destroyed. However, in some situations, the immune system may can promote tumor progression through chronic inflammation [22] and/or suppression of anti-tumor immune responses [23].
Figure 2.
The three phases of cancer immunoediting: elimination, equilibrium and escape.
During the elimination phase (Figure 2), the innate and adaptive arms of the host immune system work hand-in-hand to destroy cancer cells before these cells can be clinically detected [24]. Many effector T-lymphocyte subsets and cytokines play key roles in eliminating tumor cells. Tumor cells that cannot be destroyed in the elimination phase can enter the equilibrium phase. The main role of the equilibrium phase is to prevent outgrowth of the tumor by enabling editing of tumor immunogenicity. In addition, T-helper-1 (Th1) cells as well as some of the cytokines that these cells produce (e.g., interleukin-12 (IL-12) and interferon-gamma (IFN-γ)) help to maintain tumor cells in a state of immune-mediated dormancy. However, maintaining immune cells constantly in this phase may allow emergence of unstable tumor cells that can overcome some of the barriers imposed by the anticancer immune responses. One of the reasons for this could be expression of new molecules on the tumor cells due to mutations, which are no longer recognized by the receptors of these lymphocytes [25]. In addition, the tumor cells may secrete mediators that could induce an immunosuppressive state within the tumor microenvironment [26]. When this happens, the tumor cells are no longer susceptible to the host immune system, enabling them to avoid the elimination and equilibrium phases and enter the escape phase. In the escape phase, tumor progression is no longer blocked by the host immune system and the tumor can be detected clinically [27].
3. Plant-Derived Active Compounds and Their Mechanism of Action
There are several studies which have reported on various natural bioactive compounds that have anticancer [28,29,30] and/or immune-modulating effects [31,32]. Some of these anticancer agents possess mutagenic, teratogenic and/or oncogenic properties, which can impair antibody synthesis and also cell-mediated immune responses [33]. In the scientific literature, there is an increasing number of reports which show that many phenolic compounds have potential inhibitory effects on cancer invasion and metastasis [34,35,36,37]. A number of plant-based bioactive compounds with anticancer activities have been identified in the past decade (Table 2).
Table 2.
Anticancer activities of selected natural bioactive compounds.
| Target Cancer | Compounds | Biological Activity | Dosage/Concentration | Ref. |
|---|---|---|---|---|
| Breast | Fucoxanthin | Anticancer | 10 µM | [38] |
| Punicalagin | Anticancer | 10 mg/mL | [39] | |
| Curcumin | Apoptosis | 5–50 µg/mL | [40] | |
| Lung | Anthocyanin | Anti-proliferative | 400 μg/mL | [41] |
| Triterpenoids | Anticancer | 22.4 μmol/L | [42] | |
| Saponin | Anticancer, apoptosis | 50 μg/mL | [43] | |
| Pancreatic | Genistein | Anticancer | 60 µM | [44] |
| Garcinol | Anti-proliferative | 7 μM | [45] | |
| Limonoids | Anti-proliferative | 18–42 µM | [46] | |
| Crocin | Apoptosis | 10 g/L | [47] | |
| Colorectal | Carotenoids | Anti-proliferative | 250 μg/mL | [48] |
| Β-sitosterol | Anticancer, apoptosis | 266.2 μM | [49] | |
| Saponin | Anticancer | 5, 10 or 20 mg/kg | [50] | |
| Genistein | Anti-proliferative | 50 μM | [51] | |
| Prostate | Gallic acid | Anticancer | 100 µg/mL | [52] |
| Neobavaisoflavone, psoralidin | Apoptosis | 50 µM | [53] | |
| Rhodioflavonoside | Apoptosis | 80 µg/mL | [54] | |
| Ovarian | Corilagin | Apoptosis | 20–40 μM | [55] |
| Gallic acid | Anti-proliferation | 40 µM | [56] | |
| Ellagic acid | Anti-metastasis | 50 mg/kg | [57] | |
| Blood | Epigallocatechin gallate | Apoptosis | 3–25 μg/mL | [58] |
| Rosavin | Anticancer | 8 µg | [59] |
In this short review, the anticancer effects of four bioactive compounds (curcumin, myricetin, geraniin and tocotrienols) will be discussed. For this review, published papers reporting on the anticancer effects of these four bioactive compounds (curcumin, myricetin, geraniin and tocotrienols) that are indexed in PubMed and/or Google Scholar were selected to be included in this review. These four bioactive compounds were chosen for this review as these compounds are the putative anticancer natural products that we are currently working with to develop bioactive cocktails that have more potent anticancer activities.
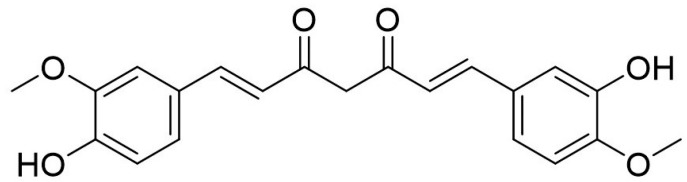
4. Curcumin
Diferuloylmethane, better known as curcumin (Figure 3) is major bioactive compound derived from an East-Indian plant known as Curcuma longa. This plant is native to the Southeast Asian region and belong to the Zingiberacae family [60]. Curcumin consists of curcuminoids compounds, which is made up from several chemicals such as curcumin, desmethoxycurcumin and bis-demethoxycurcumin [61]. Approximately 2–5% curcumin in turmeric is responsible for the yellow color as a flavoring and coloring agent in foods.
Figure 3.
Chemical structure of Curcumin.
Curcumin was found to have low bioavailability due to insufficient absorption and fast elimination from the body, which was one of the limitations of this bioactive compound. Researchers have used several approaches to increase the bioavailability of curcumin including nanoparticles [62], piperine [63], phospholipid complexes [64] and liposomes [65]. Synthetic analogs of curcumin and polyphenolic curcumin analogs have been shown to have inhibitory effects against mushroom tyrosinase [66]. Among the 61 reported curcumin compounds, four compounds (E10, F10, FN1 and FN2) were reported to inhibit prostate, pancreas and colon cancer cells with IC50 lower than 1 µM [67]. Curcumin has been shown potent anticancer properties on human cancers including lung, pancreatic, melanoma, prostate, head and neck, breast, colorectal and ovarian cancer [68,69,70,71,72,73,74,75]. Curcumin exerts anticancer effects through several mechanisms, which affect regulation of cell growth and apoptosis. For instance, curcumin can inhibit angiogenesis [76] as well as inhibit their proliferation and metastasis [77], decrease chronic inflammation [78] and combat mutated cancer cells [77]. Bisdemethoxycurcumin showed excellent inhibitory effects with an IC50 value of 23.0 µM whilst the D2 analog showed potent inhibitory effects at 8.2 µM [79]. A curcumin analog, namely CUR3d, inhibited proliferation of liver cancer cells at 100 µmol/L, which was reported to be due to downregulation of PI3K/Akt and inhibition of the NFκB pathway, which is responsible for cancer cell growth [80]. Another curcumin analog, WZ35, was reported to have potent cytotoxic effects on prostate cancer cells with a very low IC50 value (2.2 µM) when compared with curcumin (20.9 µM) [81]. In another study, curcumin at 10 μM induced apoptosis in MCF-7 human breast cancer cells, which was reported to take place via the expression of wild type p53 [82]. Exposure to curcumin, increased expression of p53 and Bax, which triggered apoptosis in these cells. In a xenograft mouse model, it was shown that a low dose of curcumin (20 μg/kg) reduced the progression of breast cancer [83]. In another study, supplementation of curcumin (1 g/kg) significantly inhibited growth and metastasis to liver of colorectal cancer cells [84]. Similar anticancer effects were also reported in aggressive papillary thyroid carcinoma, where a dose-dependent effect of curcumin was reported. Higher concentrations of curcumin (12.5, 25, 50 and 100 µM) inhibited migration of K1 papillary thyroid cancer cells by downregulating metalloproteinase-9 (MMP-9) expression [85].
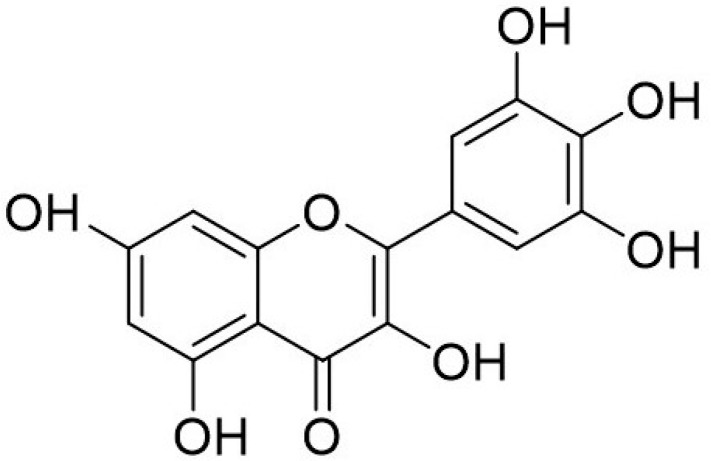
5. Myricetin
Myricetin (3,5,7,3′,4′,5′-hexahydroxyflavone cannabiscetin) is a bioflavonoid (Figure 4) widely found in food sources such as vegetables, tea, berries, red wine and medicinal plants. It was first isolated from the bark of the Myrica nagi Thunb, Myricaceae in 1896 with molecular formulae of C15H10O8 [86]. Myricetin has been credited for its therapeutic effects in cardiovascular disease [87], cancer [88], and diabetes mellitus [89,90]. Being lipophilic compounds, myricetin has poor solubility in water but can be solubilized in organic solvents such as acetone, dimethylformamide, dimethylacetamide and tetrahydrofuran.
Figure 4.
Chemical structure of Myricetin.
Myricetin is stable at pH 2 and its degradation depends on pH and temperature [91]. A recent study showed that microemulsion formulation can improve the solubility of myricetin 1225 times greater than water and also enhance its anti-proliferative activity against human liver cancer cells (HepG2) [92]. Myricetin is a promising anti-carcinogen and chemo preventive agent with therapeutic potential reported in ovarian [93], colon [94], skin [95], liver [96] and breast [97] cancers. Cell-based studies have shown that myricetin inhibited proliferation of T24 bladder cancer cells by inducing cell cycle arrest at the G2/M phase by downregulating cyclin B1 and cyclin-dependent kinase cdc2 [98]. In addition, myricetin induced apoptosis in T24 cells by modulating Bcl-2 family protein and activating caspase 3 pathways. Similar findings (i.e., cell cycle arrest and induction of apoptosis) were observed in cervical cancer cells following combination treatment with myricetin (60 μM), methyl eugenol and cisplatin [99]. In a rat model, tumor progression was inhibited when the rats were fed with 100 mg/kg of myricetin, which was found to be due to inhibition of the p21 activated kinase-1 (PAK1) [100]. A recent study showed that myricetin may exert anti-metastatic effects by downregulating the expression of MMP2 and/or MMP9 in breast cancer cells [101].
6. Geraniin
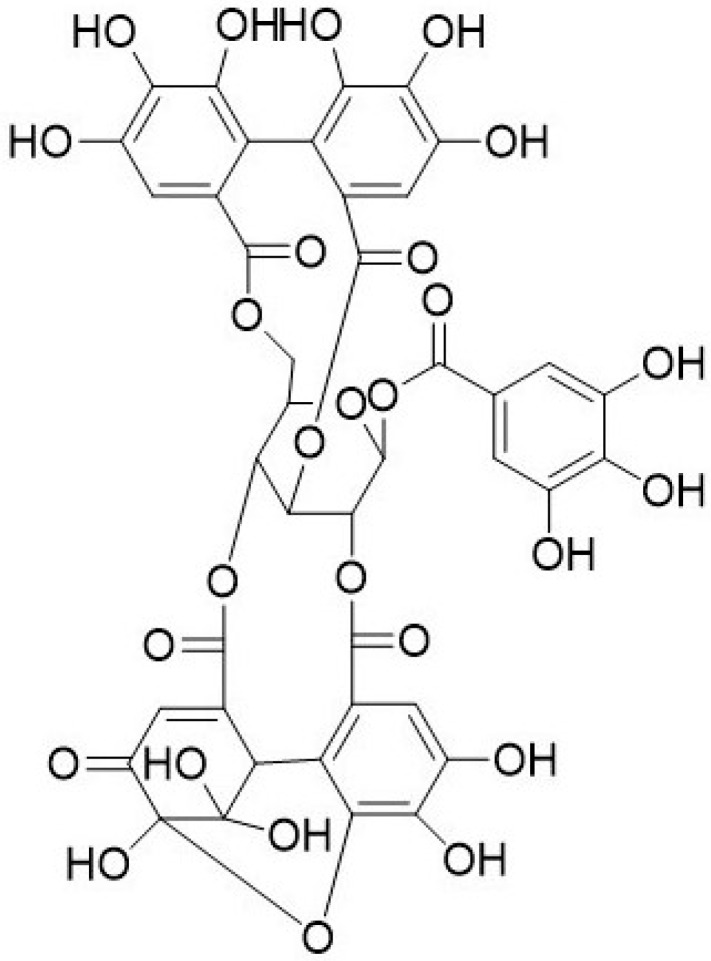
Geraniin is a dehydroellagitannin (Figure 5) found in geraniums and regarded as main active compounds in various medicinal plants. It was first identified from Geranium thunbergii [102] and belongs to the Sapindaceae, Gereniaceae, Nymphaeaceae and Elaeocarpaceae families [102,103]. Geraniin has been credited to possess high antioxidant, antibacterial, anti-hyperglycemic, anti-viral and anticancer activities [104,105,106,107,108]. The hydrolyzed compounds from geraniin were identified as gallic acid, corilagin, and ellagic acid. As shown in Figure 5, geraniin contains galloyl groups with additional hydroxyl structure to ortho-dihydroxy groups, which have high nitrogen oxide (NO) scavenging ability. Corilagin and gallic acid contain galloyl group also contribute to the intrinsic antioxidant activities of geraniin [109].
Figure 5.
Chemical structure of geraniin.
Geraniin isolated from fruit of Emblica (Phyllantus emblica L.) was found to have an anticancer effect on MCF-7 human breast cancer cells [110]. Cell-based assays using murine splenocytes showed that geraniin inhibited proliferation of MCF-7 human breast cancer cells with IC50 value of 13.2 μg/mL [110]. Similarly, geraniin extracted from Phyllanthus urinaria Linn was reported to have anti-proliferative and pro-apoptotic effects on MCF-7 cells with IC50 value 9.94 µM [111]. Geraniin triggered apoptosis by activating the p38 MAPK signaling pathway [111]. Epithelial–mesenchymal transition (EMT) is reported to play an important role in cancer metastasis [112]. Geraniin inhibited transforming growth factor beta-1 (TGF-β-1)-induced EMT in lung cancer cells by increasing the expression of E-cadherin and inhibiting expression of Snail, a transcription factor crucial for induction of EMT [113]. In addition, activation of Smad-2 was inhibited in TGF-β-1-induced EMT, suggesting that geraniin may play a role in preventing metastasis and EMT in TGF-β-1-induced signaling pathway [113].
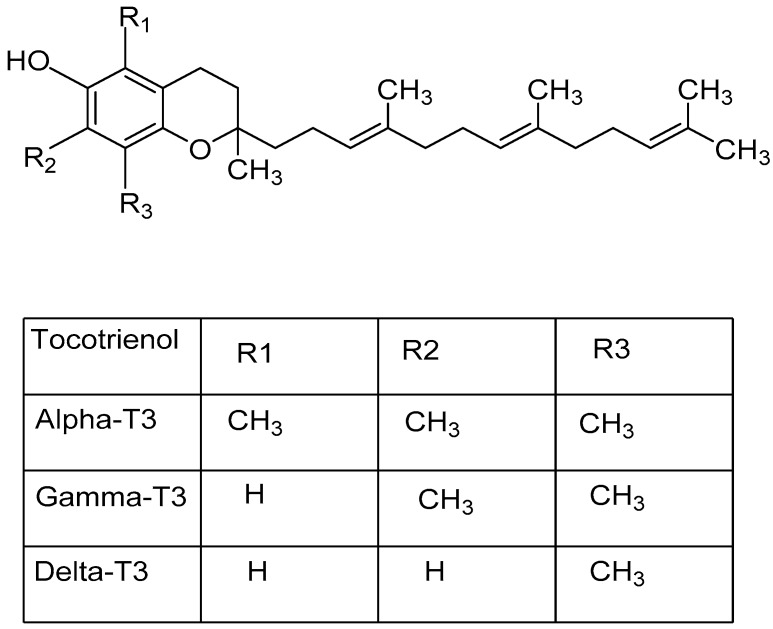
7. Tocotrienol
Vitamin E encompass two major class of fat-soluble antioxidants namely tocopherols and tocotrienols (T3) [114]. There are eight dietary components identified to be a member of the vitamin E family, which are tocopherols (α, β, γ, δ) and tocotrienols (α, β, γ, δ) [115]. The chemical structure of tocotrienols and its various isoforms are shown in Figure 6.
Figure 6.
Chemical structure of tocotrienols and its four major isoforms. (T3: Tocotrienol).
The major sources of dietary tocopherols are plant oils such as wheat-germ oil, safflower-seed oil, maize oil, soya bean oil [116], whilst the main sources of tocotrienol are palm oil, rice bran oil, and palm kernel oil [117]. Tocotrienols are main phytonutrients found in palm oil and can be found in the palm oil fraction known as tocotrienol-rich fraction (TRF) [118]. TRF contains three main isoforms of tocotrienol, which are αT3 (29%), γT3 (28%) and δT3 (14%) isomers [119]. Tocotrienols are reported to possess anti-thrombotic [120], antioxidant [121], neuroprotective [122] and cardio-protective [123] activities as well as immune modulatory [124,125] properties. Both cell-based and experimental model studies have suggested that tocotrienols also possess anti-tumor properties as these compounds can inhibit proliferation of many cancer cell lines including prostate [126], breast [127], skin [128], colon [129], stomach [130], pancreatic [131], liver [132] and lung [133] cancers. The anticancer effects induced by tocotrienol are reported to be mediated through apoptosis [134], anti-angiogenesis [135], anti-proliferative [136] and/or immunoregulation [125]. Tocotrienol isoforms inhibited proliferation of human breast cancer cells in the following order: αT3 < TRF < γT3 < δT3 [137]. In addition, daily supplementation of 1 mg of TRF was reported to inhibit tumor growth in a syngeneic murine model of breast cancer [31,124,137]. A similar observation was also reported in a xenograft athymic mouse model of breast cancer where a significant delay in the onset of breast cancer in mice fed with 1 mg TRF was observed [138]. This delay was reported to be due to down-regulation of the c-myc oncogene in the breast cancer cell and upregulation of the CD59 glycoprotein precursor gene, which was responsible for immune regulation. In another study, supplementation with δT3 inhibited proliferation and migration of lung cancer cells in a dose- and time-dependent manner [139]. This inhibition was due to inhibition of NFκB activity and signaling via the NOTCH-1 pathway by δT3. In another study, daily supplementation of 1 mg TRF was reported to inhibit growth of breast cancer in mice as well as reduce the levels of vascular endothelial growth factor (VEGF) in serum [135]. In addition, murine breast cancer cells (4T1) cells treated with TRF or δT3 were found to induce marked inhibition of IL-8 and VEGF genes, which play important roles in tumor development [140]. These findings suggest that TRF also possesses anti-angiogenesis activity. In the same mouse model of breast cancer, it was shown that daily supplementation with TRF may exert anticancer effects by upregulating the expression of the IL24 gene [140].
8. Conclusions
Natural products have the potential to serve as chemotherapeutic as well as chemopreventive agents in the treatment of cancer. The bioactive compounds derived from many natural plant sources could be a possible means to provide protection against cancer or used as a treatment approach against cancer. Curcumin and tocotrienols show much promise to be developed as chemopreventive and/or novel therapeutic agents in the fight against cancer as there are many studies that show that these bioactive agents possess potent anticancer activities. Although there are some studies that have demonstrated how these compounds exert anticancer effects, the exact target remains elusive. Hence, more work needs to be carried out to know to understand exactly how these compounds act as this information would be useful in developing therapeutic cocktails made up of various bioactive agents that can target different molecules to produce better therapeutic effects.
Acknowledgments
This review was initiated during the PhD candidature of the first author. The authors would like to thank the International Medical University and the Malaysian Palm Oil Board for support during the PhD candidature.
Author Contributions
The manuscript was written through contributions of all authors. All authors have given approval to the final version of the manuscript.
Funding
This review was written with no external funding. The article processing fee was funded by Jeffrey Cheah School of Medicine and Health Sciences, Monash University, Malaysia.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Bray F., Ren J., Masuyer E., Ferlay J. Global estimates of cancer prevalence for 27 sites in the adult population in 2008. Int. J. Cancer. 2013;132:1133–1145. doi: 10.1002/ijc.27711. [DOI] [PubMed] [Google Scholar]
- 2.Ferlay J., Shin H., Bray F., Forman D., Mathers C., Parkin D.M. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int. J. Cancer. 2010;127:2893–2917. doi: 10.1002/ijc.25516. [DOI] [PubMed] [Google Scholar]
- 3.Ferlay J., Soerjomataram I., Dikshit R., Eser S., Mathers C., Rebelo M. Cancer incidence and mortality worldwide: Sources, methods and major patterns in GLOBOCAN 2012. Int. J. Cancer. 2015;136:E359–E386. doi: 10.1002/ijc.29210. [DOI] [PubMed] [Google Scholar]
- 4.Bray F., Ferlay J., Soerjomataram I., Siegel R.L., Torre L.A., Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2018;68:394–424. doi: 10.3322/caac.21492. [DOI] [PubMed] [Google Scholar]
- 5.Snellenberg S., Cillessen S.A., Van Criekinge W., Bosch L., Meijer C.J., Snijders P.J., Steenbergen R.D. Methylation-mediated repression of PRDM14 contributes to apoptosis evasion in HPV-positive cancers. Carcinogenesis. 2014;35:2611–2618. doi: 10.1093/carcin/bgu197. [DOI] [PubMed] [Google Scholar]
- 6.Mar A.C., Chu C.H., Lee H.J., Chien C.W., Cheng J.J., Yang S.H. Interleukin-1 receptor type 2 acts with c-Fos to enhance the expression of IL-6 and VEGF-A in colon cancer cells and induce angiogenesis. J. Biol. Chem. 2015;290:22212–22224. doi: 10.1074/jbc.M115.644823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Frink R.E., Peyton M., Schiller J.H., Gazdar A.F., Shay J.W., Minna J.D. Telomerase inhibitor imetelstat has preclinical activity across the spectrum of non-small cell lung cancer oncogenotypes in a telomere length dependent manner. Oncotarget. 2016;7:31639. doi: 10.18632/oncotarget.9335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pérez A., Nogués C. Cancer Stem Cells, Reason of the Failure of Conventional Cancer Treatments. Universitat Autònoma de Barcelona; Bellaterra, Spain: 2014. [Google Scholar]
- 9.Courtnay R., Ngo D.C., Malik N., Ververis K., Tortorella S.M., Karagiannis T.C. Cancer metabolism and the Warburg effect: The role of HIF-1 and PI3K. Mol. Biol. Rep. 2015;42:841–851. doi: 10.1007/s11033-015-3858-x. [DOI] [PubMed] [Google Scholar]
- 10.Hanahan D., Weinberg R.A. Hallmarks of cancer: The next generation. Cell. 2011;144:646–674. doi: 10.1016/j.cell.2011.02.013. [DOI] [PubMed] [Google Scholar]
- 11.Merdad A., Karim S., Schulten H.J., Dallol A., Buhmeida A., Al-Thubaity F. Expression of matrix metalloproteinases (MMPs) in primary human breast cancer: MMP-9 as a potential biomarker for cancer invasion and metastasis. Anticancer Res. 2014;34:1355–1366. doi: 10.1186/1471-2407-9-188. [DOI] [PubMed] [Google Scholar]
- 12.Jiang W.G., Sanders A.J., Katoh M., Ungefroren H., Gieseler F., Prince M., Thompson S.K., Zollo M., Spano D., Dhawan P., et al. Seminars in Cancer Biology. Volume 35. Academic Press; Cambridge, MA, USA: 2015. Tissue invasion and metastasis: Molecular, biological and clinical perspectives; pp. S244–S275. [DOI] [PubMed] [Google Scholar]
- 13.Weissenstein U., Kunz M., Urech K., Baumgartner S. Interaction of standardized mistletoe (Viscum album) extracts with chemotherapeutic drugs regarding cytostatic and cytotoxic effects in vitro. BMC Complement. Altern. Med. 2014;14:6. doi: 10.1186/1472-6882-14-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fan Y., Shen B., Tan M., Mu X., Qin Y., Zhang F. Long non-coding RNA UCA1 increases chemoresistance of bladder cancer cells by regulating Wnt signaling. FEBS J. 2014;281:1750–1758. doi: 10.1111/febs.12737. [DOI] [PubMed] [Google Scholar]
- 15.Lu L., Xu X., Zhang B., Zhang R., Ji H., Wang X. Combined PD-1 blockade and GITR triggering induce a potent antitumor immunity in murine cancer models and synergizes with chemotherapeutic drugs. J. Transl. Med. 2014;12:36. doi: 10.1186/1479-5876-12-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gao W., Xiang B., Meng T.T., Liu F., Qi X.R. Chemotherapeutic drug delivery to cancer cells using a combination of folate targeting and tumor microenvironment-sensitive polypeptides. Biomaterials. 2013;34:4137–4149. doi: 10.1016/j.biomaterials.2013.02.014. [DOI] [PubMed] [Google Scholar]
- 17.Shapiro C.L., Recht A. Side effects of adjuvant treatment of breast cancer. N. Engl. J. Med. 2001;344:1997–2008. doi: 10.1056/NEJM200106283442607. [DOI] [PubMed] [Google Scholar]
- 18.Huang B., Zhao J., Li H., He K.L., Chen Y., Mayer L. Toll-like receptors on tumor cells facilitate evasion of immune surveillance. Cancer Res. 2005;65:5009–5014. doi: 10.1158/0008-5472.CAN-05-0784. [DOI] [PubMed] [Google Scholar]
- 19.Pardoll D. Cancer and the immune system: Basic concepts and targets for intervention. In: Michael B.A., Mario S., editors. Seminars in Oncology. Volume 42. Elsevier; Amsterdam, The Netherlands: 2015. pp. 523–538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Vesely M.D., Schreiber R.D. Cancer immunoediting: Antigens, mechanisms, and implications to cancer immunotherapy. Ann. N.Y. Acad. Sci. 2013;1284:1–5. doi: 10.1111/nyas.12105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mittal D., Gubin M.M., Schreiber R.D., Smyth M.J. New insights into cancer immunoediting and its three component phases—elimination, equilibrium and escape. Curr. Opin. Immunol. 2014;27:16–25. doi: 10.1016/j.coi.2014.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Macarthur M., Hold G.L., El-Omar E.M. Inflammation and Cancer II. Role of chronic inflammation and cytokine gene polymorphisms in the pathogenesis of gastrointestinal malignancy. Am. J. Physiol. Liver Physiol. 2004;286:515–520. doi: 10.1152/ajpgi.00475.2003. [DOI] [PubMed] [Google Scholar]
- 23.Sutmuller R.P.M., Van Duivenvoorde L.M., Van Elsas A., Schumacher T.N.M., Wildenberg M.E., Allison J.P. Synergism of cytotoxic T lymphocyte-associated antigen 4 blockade and depletion of CD25+ regulatory T cells in antitumor therapy reveals alternative pathways for suppression of autoreactive cytotoxic T lymphocyte responses. J. Exp. Med. 2001;194:823–832. doi: 10.1084/jem.194.6.823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gajewski T.F., Schreiber H., Fu Y.X. Innate and adaptive immune cells in the tumor microenvironment. Nat. Immunol. 2013;14:1014–1022. doi: 10.1038/ni.2703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shaw J.A., Guttery D.S., Hills A., Fernandez-Garcia D., Page K., Rosales B.M. Mutation Analysis of Cell-Free DNA and Single Circulating Tumor Cells in Metastatic Breast Cancer Patients with High Circulating Tumor Cell Counts. Clin. Cancer Res. 2017;23:88–96. doi: 10.1158/1078-0432.CCR-16-0825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kim R., Emi M., Tanabe K. Cancer immunoediting from immune surveillance to immune escape. Immunology. 2007;121:1–14. doi: 10.1111/j.1365-2567.2007.02587.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dunn G.P., Old L.J., Schreiber R.D. The three Es of cancer immunoediting. Annu. Rev. Immunol. 2004;22:329–360. doi: 10.1146/annurev.immunol.22.012703.104803. [DOI] [PubMed] [Google Scholar]
- 28.Lee J.H., Yeon J.H., Kim H., Roh W., Chae J., Park H.O. The natural anticancer agent plumbagin induces potent cytotoxicity in MCF-7 human breast cancer cells by inhibiting a PI-5 kinase for ROS generation. PLoS ONE. 2012;7:e45023. doi: 10.1371/journal.pone.0045023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ahmed S., Othman N.H. Honey as a potential natural anticancer agent: A review of its mechanisms. Evid. Based Complement Altern. Med. 2013;2013:829070. doi: 10.1155/2013/829070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sultana N. Clinically useful anticancer, antitumor, and antiwrinkle agent, ursolic acid and related derivatives as medicinally important natural product. J. Enzyme Inhib. Med. Chem. 2011;26:616–642. doi: 10.3109/14756366.2010.546793. [DOI] [PubMed] [Google Scholar]
- 31.Hafid S.R.A., Radhakrishnan A.K., Nesaretnam K. Tocotrienols are good adjuvants for developing cancer vaccines. BMC Cancer. 2010;10:5. doi: 10.1186/1471-2407-10-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Teiten M.H., Eifes S., Dicato M., Diederich M. Curcumin—The paradigm of a multi-target natural compound with applications in cancer prevention and treatment. Toxins. 2010;2:128–162. doi: 10.3390/toxins2010128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Penn I., Starzl T.E. Immunosuppression and Cancer. Transplant. Proc. 1973;5:943–947. [PMC free article] [PubMed] [Google Scholar]
- 34.Ngamkitidechakul C., Jaijoy K., Hansakul P., Soonthornchareonnon N., Sireeratawong S. Antitumour effects of Phyllanthus emblica L.: Induction of cancer cell apoptosis and inhibition of in vivo tumour promotion and in vitro invasion of human cancer cells. Phyther. Res. 2010;24:1405–1413. doi: 10.1002/ptr.3127. [DOI] [PubMed] [Google Scholar]
- 35.Cicerale S., Lucas L., Keast R. Biological activities of phenolic compounds present in virgin olive oil. Int. J. Mol. Sci. 2010;11:458–479. doi: 10.3390/ijms11020458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wang N., Wang Z.Y., Mo S.L., Loo T.Y., Wang D.M., Luo H.B. Ellagic acid, a phenolic compound, exerts anti-angiogenesis effects via VEGFR-2 signaling pathway in breast cancer. Breast Cancer Res. Treat. 2012;134:943–955. doi: 10.1007/s10549-012-1977-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Luo K.W., Ko C.H., Yue G.G.L., Lee J.K.M., Li K.K., Lee M. Green tea (Camellia sinensis) extract inhibits both the metastasis and osteolytic components of mammary cancer 4T1 lesions in mice. J. Nutr. Biochem. 2014;25:395–403. doi: 10.1016/j.jnutbio.2013.11.013. [DOI] [PubMed] [Google Scholar]
- 38.Rwigemera A., Mamelona J., Martin L.J. Comparative effects between fucoxanthinol and its precursor fucoxanthin on viability and apoptosis of breast cancer cell lines MCF-7 and MDA-MB-231. Anticancer Res. 2015;35:207–219. [PubMed] [Google Scholar]
- 39.Shirode A.B., Bharali D.J., Nallanthighal S., Coon J.K., Mousa S.A., Reliene R. Nanoencapsulation of pomegranate bioactive compounds for breast cancer chemoprevention. Int. J. Nanomed. 2015;10:475. doi: 10.2147/IJN.S65145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Nadaf S.J., Killedar S.G. Curcumin nanocochleates: Use of design of experiments, solid state characterization, in vitro apoptosis and cytotoxicity against breast cancer MCF-7 cells. J. Drug Deliv. Sci. Technol. 2018;47:337–350. doi: 10.1016/j.jddst.2018.06.026. [DOI] [Google Scholar]
- 41.Lu J.N., Panchanathan R., Lee W.S., Kim H.J., Kim D.H., Choi Y.H. Anthocyanins from the Fruit of Vitis Coignetiae Pulliat Inhibit TNF-Augmented Cancer Proliferation, Migration, and Invasion in A549 Cells. Asian Pac. J. Cancer Prev. 2017;18:2919. doi: 10.22034/APJCP.2017.18.11.2919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Yan Z., Wang H., Liu L., Guohua D.U., Chen R. Study on in vitro anti-tumor activity of triterpenoids from Ganoderma lucidum. Int. J. Lab. Med. 2017;38:633–634. doi: 10.3969/j.issn.1673-4130.2017.05.023. [DOI] [Google Scholar]
- 43.Li T., Pan H., Feng Y., Li H., Zhao Y. Bioactivity-guided isolation of anticancer constituents from Hedera nepalensis K. Koch. South Afr. J. Bot. 2015;100:87–93. doi: 10.1016/j.sajb.2015.05.011. [DOI] [Google Scholar]
- 44.Xia J., Cheng L., Mei C., Ma J., Shi Y., Zeng F., Wang Z., Wang Z. Genistein inhibits cell growth and invasion through regulation of miR-27a in pancreatic cancer cells. Curr. Pharm. Des. 2014;20:5348–5353. doi: 10.2174/1381612820666140128215756. [DOI] [PubMed] [Google Scholar]
- 45.Parasramka M.A., Gupta S.V. Synergistic effect of garcinol and curcumin on antiproliferative and apoptotic activity in pancreatic cancer cells. J. Oncol. 2012;2012:709739. doi: 10.1155/2012/709739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Patil J.R., Jayaprakasha G.K., Murthy K.C., Chetti M.B., Patil B.S. Characterization of Citrus aurantifolia bioactive compounds and their inhibition of human pancreatic cancer cells through apoptosis. Microchem. J. 2010;94:108–117. doi: 10.1016/j.microc.2009.09.008. [DOI] [Google Scholar]
- 47.Bakshi H., Sam S., Rozati R., Sultan P., Islam T., Rathore B., Lone Z., Sharma M., Triphati J., Saxena R.C. DNA fragmentation and cell cycle arrest: A hallmark of apoptosis induced by crocin from kashmiri saffron in a human pancreatic cancer cell line. Asian Pac. J. Cancer Prev. 2010;11:675–679. [PubMed] [Google Scholar]
- 48.Castro-Puyana M., Pérez-Sánchez A., Valdés A., Ibrahim O.H.M., Suarez-Alvarez S., Ferragut J.A. Pressurized liquid extraction of Neochloris oleoabundans for the recovery of bioactive carotenoids with anti-proliferative activity against human colon cancer cells. Food Res. Int. 2017;99:1048–1055. doi: 10.1016/j.foodres.2016.05.021. [DOI] [PubMed] [Google Scholar]
- 49.Baskar A.A., Ignacimuthu S., Paulraj G.M., Al Numair K.S. Chemopreventive potential of β-sitosterol in experimental colon cancer model-an in vitro and in vivo study. BMC Complement. Altern. Med. 2010;10:24. doi: 10.1186/1472-6882-10-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Li Y., Liu C., Xiao D., Han J., Yue Z., Sun Y., Fan L., Zhang F., Meng J., Zhang R., et al. Trillium tschonoskii steroidal saponins suppress the growth of colorectal Cancer cells in vitro and in vivo. J. Ethnopharmacol. 2015;168:136–145. doi: 10.1016/j.jep.2015.03.063. [DOI] [PubMed] [Google Scholar]
- 51.Qi W., Weber C.R., Wasland K., Savkovic S.D. Genistein inhibits proliferation of colon cancer cells by attenuating a negative effect of epidermal growth factor on tumor suppressor FOXO3 activity. BMC Cancer. 2011;11:219. doi: 10.1186/1471-2407-11-219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Chen H.M., Wu Y.C., Chia Y.C., Chang F.R., Hsu H.K., Hsieh Y.C., Chen C.C., Yuan S.S. Gallic acid, a major component of Toona sinensis leaf extracts, contains a ROS-mediated anti-cancer activity in human prostate cancer cells. Cancer Lett. 2009;286:161–171. doi: 10.1016/j.canlet.2009.05.040. [DOI] [PubMed] [Google Scholar]
- 53.Szliszka E., Czuba Z.P., Sȩdek Ł., Paradysz A., Król W. Enhanced TRAIL-mediated apoptosis in prostate cancer cells by the bioactive compounds neobavaisoflavone and psoralidin isolated from Psoralea corylifolia. Pharm. Rep. 2011;63:139–148. doi: 10.1016/S1734-1140(11)70408-X. [DOI] [PubMed] [Google Scholar]
- 54.Ming D.S., Hillhouse B.J., Guns E.S., Eberding A., Xie S., Vimalanathan S., Towers G.N. Bioactive compounds from Rhodiola rosea (Crassulaceae) Phyther. Res. An. Int. J. Devoted to Pharmacol. Toxicol. Eval. Nat. Prod. Deriv. 2005;19:740–743. doi: 10.1002/ptr.1597. [DOI] [PubMed] [Google Scholar]
- 55.Jia L., Jin H., Zhou J., Chen L., Lu Y., Ming Y., Yu Y. A potential anti-tumor herbal medicine, Corilagin, inhibits ovarian cancer cell growth through blocking the TGF-β signaling pathways. BMC Complement. Altern. Med. 2013;13:33. doi: 10.1186/1472-6882-13-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.He Z., Li B., Rankin G.O., Rojanasakul Y., Chen Y.C. Selecting bioactive phenolic compounds as potential agents to inhibit proliferation and VEGF expression in human ovarian cancer cells. Oncol. Lett. 2015;9:1444–1450. doi: 10.3892/ol.2014.2818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Liu H., Zeng Z., Wang S., Li T., Mastriani E., Li Q.H., Bao H.X., Zhou Y.J., Wang X., Liu Y., et al. Main components of pomegranate, ellagic acid and luteolin, inhibit metastasis of ovarian cancer by down-regulating MMP2 and MMP9. Cancer Biol. Ther. 2017;18:990–999. doi: 10.1080/15384047.2017.1394542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Lee Y.K., Bone N.D., Strege A.K., Shanafelt T.D., Jelinek D.F., Kay N.E. VEGF receptor phosphorylation status and apoptosis is modulated by a green tea component, epigallocatechin-3-gallate (EGCG), in B-cell chronic lymphocytic leukemia. Blood. 2004;104:788–794. doi: 10.1182/blood-2003-08-2763. [DOI] [PubMed] [Google Scholar]
- 59.Skopińska-Różewska E., Hartwich M., Siwicki A.K., Wasiutyński A.L., Sommer E., Mazurkiewicz M.I., Bany J., Skurzak H. The influence of Rhodiola rosea extracts and rosavin on cutaneous angiogenesis induced in mice after grafting of syngeneic tumor cells. Centr. Eur. J. Immunol. 2008;33:102–107. [Google Scholar]
- 60.Chattopadhyay I., Biswas K., Bandyopadhyay U., Banerjee R.K. Turmeric and curcumin: Biological actions and medicinal applications. Curr. Sci. 2004;87:44–53. [Google Scholar]
- 61.Jurenka J.S. Anti-inflammatory properties of curcumin, a major constituent of Curcuma longa: A review of preclinical and clinical research. Altern. Med. Rev. 2009;14:277. [PubMed] [Google Scholar]
- 62.Basniwal R.K., Buttar H.S., Jain V.K., Jain N. Curcumin nanoparticles: Preparation, characterization, and antimicrobial study. J. Agric. Food Chem. 2011;59:2056–2061. doi: 10.1021/jf104402t. [DOI] [PubMed] [Google Scholar]
- 63.Kakarala M., Brenner D.E., Korkaya H., Cheng C., Tazi K., Ginestier C., Liu S., Dontu G., Wicha M.S. Targeting breast stem cells with the cancer preventive compounds curcumin and piperine. Breast Cancer Res. Treat. 2010;122:777–785. doi: 10.1007/s10549-009-0612-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Giori A., Franceschi F. Phospholipid Complexes of Curcumin Having Improved Bioavailability. Application 12/281,994. U.S. Patent. 2009 May 21;
- 65.Li L., Ahmed B., Mehta K., Kurzrock R. Liposomal curcumin with and without oxaliplatin: Effects on cell growth, apoptosis, and angiogenesis in colorectal cancer. Mol. Cancer Ther. 2007;6:1276–1282. doi: 10.1158/1535-7163.MCT-06-0556. [DOI] [PubMed] [Google Scholar]
- 66.Du Z.Y., Jiang Y.F., Tang Z.K., Mo R.Q., Xue G.H., Lu Y.J., Zheng X., Dong C.Z., Zhang K. Antioxidation and tyrosinase inhibition of polyphenolic curcumin analogs. Biosci. Biotechnol. Biochem. 2011;75:2351–2358. doi: 10.1271/bbb.110547. [DOI] [PubMed] [Google Scholar]
- 67.Wei X., Du Z.Y., Zheng X., Cui X.X., Conney A.H., Zhang K. Synthesis and evaluation of curcumin-related compounds for anticancer activity. Eur. J. Med. Chem. 2012;53:235–245. doi: 10.1016/j.ejmech.2012.04.005. [DOI] [PubMed] [Google Scholar]
- 68.Wu S.H., Hang L.W., Yang J.S., Chen H.Y., Lin H.Y., Chiang J.H. Curcumin induces apoptosis in human non-small cell lung cancer NCI-H460 cells through ER stress and caspase cascade-and mitochondria-dependent pathways. Anticancer Res. 2010;30:2125–2133. [PubMed] [Google Scholar]
- 69.Kumar P., Barua C.C., Sulakhiya K., Sharma R. Curcumin ameliorates cisplatin-induced nephrotoxicity and potentiates its anticancer activity in SD rats: Potential role of curcumin in breast cancer chemotherapy. Front Pharmacol. 2017;8:132. doi: 10.3389/fphar.2017.00132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Anitha A., Deepa N., Chennazhi K.P., Lakshmanan V.K., Jayakumar R. Combinatorial anticancer effects of curcumin and 5-fluorouracil loaded thiolated chitosan nanoparticles towards colon cancer treatment. Biochim. Biophys. Acta Gen. Subj. 2014;1840:2730–2743. doi: 10.1016/j.bbagen.2014.06.004. [DOI] [PubMed] [Google Scholar]
- 71.Terlikowska K.M., Witkowska A.M., Zujko M.E., Dobrzycka B., Terlikowski S.J. Potential application of curcumin and its analogues in the treatment strategy of patients with primary epithelial ovarian cancer. Int. J. Mol. Sci. 2014;15:21703–21722. doi: 10.3390/ijms151221703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Bisht S., Schlesinger M., Rupp A., Schubert R., Nolting J., Wenzel J. A liposomal formulation of the synthetic curcumin analog EF24 (Lipo-EF24) inhibits pancreatic cancer progression: Towards future combination therapies. J. Nanobiotechnology. 2016;14:57. doi: 10.1186/s12951-016-0209-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Zhao G., Han X., Zheng S., Li Z., Sha Y., Ni J. Curcumin induces autophagy, inhibits proliferation and invasion by downregulating AKT/mTOR signaling pathway in human melanoma cells. Oncol. Rep. 2016;35:1065–1074. doi: 10.3892/or.2015.4413. [DOI] [PubMed] [Google Scholar]
- 74.Jordan B.C., Mock C.D., Thilagavathi R., Selvam C. Molecular mechanisms of curcumin and its semisynthetic analogues in prostate cancer prevention and treatment. Life Sci. 2016;152:135–144. doi: 10.1016/j.lfs.2016.03.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Basak S.K., Zinabadi A., Wu A.W., Venkatesan N., Duarte V.M., Kang J.J. Liposome encapsulated curcumin-difluorinated (CDF) inhibits the growth of cisplatin resistant head and neck cancer stem cells. Oncotarget. 2015;6:18504. doi: 10.18632/oncotarget.4181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Abusnina A., Keravis T., Zhou Q., Justiniano H., Lobstein A., Lugnier C. Tumour growth inhibition and anti-angiogenic effects using curcumin correspond to combined PDE2 and PDE4 inhibition. Thromb Haemost. 2015;113:319–328. doi: 10.1160/TH14-05-0454. [DOI] [PubMed] [Google Scholar]
- 77.Kunnumakkara A.B., Bordoloi D., Harsha C., Banik K., Gupta S.C., Aggarwal B.B. Curcumin mediates anticancer effects by modulating multiple cell signaling pathways. Clin. Sci. 2017;131:1781–1799. doi: 10.1042/CS20160935. [DOI] [PubMed] [Google Scholar]
- 78.Khan M.N., Haggag Y.A., Lane M.E., McCarron P.A., Tambuwala M.M. Polymeric Nano-Encapsulation of Curcumin Enhances its Anti-Cancer Activity in Breast (MDA-MB231) and Lung (A549) Cancer Cells Through Reduction in Expression of HIF-1α and Nuclear p65 (Rel A) Curr. Drug Deliv. 2018;15:286–295. doi: 10.2174/1567201814666171019104002. [DOI] [PubMed] [Google Scholar]
- 79.Du Z., Liu R., Shao W., Mao X., Ma L., Gu L.Q., Huang Z.S., Chan A.S. α-Glucosidase inhibition of natural curcuminoids and curcumin analogs. Eur. J. Med. Chem. 2006;41:213–218. doi: 10.1016/j.ejmech.2005.10.012. [DOI] [PubMed] [Google Scholar]
- 80.Bhullar K.S., Jha A., Rupasinghe H.P.V. Novel carbocyclic curcumin analog CUR3d modulates genes involved in multiple apoptosis pathways in human hepatocellular carcinoma cells. Chem. Biol. Interact. 2015;242:107–122. doi: 10.1016/j.cbi.2015.09.020. [DOI] [PubMed] [Google Scholar]
- 81.Zhang X., Chen M., Zou P., Kanchana K., Weng Q., Chen W., Zhong P., Ji J., Zhou H., He L., et al. Curcumin analog WZ35 induced cell death via ROS-dependent ER stress and G2/M cell cycle arrest in human prostate cancer cells. BMC Cancer. 2015;15:866. doi: 10.1186/s12885-015-1851-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Choudhuri T., Pal S., Agwarwal M.L., Das T., Sa G. Curcumin induces apoptosis in human breast cancer cells through p53-dependent Bax induction. FEBS Lett. 2002;512:334–340. doi: 10.1016/S0014-5793(02)02292-5. [DOI] [PubMed] [Google Scholar]
- 83.Choi Y.E., Park E. Curcumin enhances poly (ADP-ribose) polymerase inhibitor sensitivity to chemotherapy in breast cancer cells. J. Nutr. Biochem. 2015;26:1442–1447. doi: 10.1016/j.jnutbio.2015.07.015. [DOI] [PubMed] [Google Scholar]
- 84.Chen C.C., Sureshbabul M., Chen H.W., Lin Y.S., Lee J.Y., Hong Q.S., Yang Y.C., Yu S.L. Curcumin suppresses metastasis via Sp-1, FAK inhibition, and E-cadherin upregulation in colorectal cancer. Evid. Based Complement Altern. Med. 2013;2013:541695. doi: 10.1155/2013/541695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Zhang C.Y., Zhang L., Yu H.X., Bao J.D., Lu R.R. Curcumin inhibits the metastasis of K1 papillary thyroid cancer cells via modulating E-cadherin and matrix metalloproteinase-9 expression. Biotechnol. Lett. 2013;35:995–1000. doi: 10.1007/s10529-013-1173-y. [DOI] [PubMed] [Google Scholar]
- 86.Perkin A.G., Hummel J.J. The colouring principle contained in the bark of Myrica nagi. Part, I. J. Chem. Soc. Trans. 1896;69:1287–1294. doi: 10.1039/CT8966901287. [DOI] [Google Scholar]
- 87.Chang C.J., Tzeng T.F., Liou S., Chang Y.S., Liu I.M. Myricetin increases hepatic peroxisome proliferator-activated receptor α protein expression and decreases plasma lipids and adiposity in rats. Evid. Based Complement Altern. Med. 2012;2012:787152. doi: 10.1155/2012/787152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Lu J., Papp L.V., Fang J., Rodriguez-Nieto S., Zhivotovsky B., Holmgren A. Inhibition of mammalian thioredoxin reductase by some flavonoids: Implications for myricetin and quercetin anticancer activity. Cancer Res. 2006;66:4410–4418. doi: 10.1158/0008-5472.CAN-05-3310. [DOI] [PubMed] [Google Scholar]
- 89.Ozcan F., Ozmen A., Akkaya B., Aliciguzel Y., Aslan M. Beneficial effect of myricetin on renal functions in streptozotocin-induced diabetes. Clin. Exp. Med. 2012;12:265–272. doi: 10.1007/s10238-011-0167-0. [DOI] [PubMed] [Google Scholar]
- 90.Liu I.M., Liou S.S., Lan T.W., Hsu F.L., Cheng J.T. Myricetin as the active principle of Abelmoschus moschatus to lower plasma glucose in streptozotocin-induced diabetic rats. Planta. Med. 2005;71:617–721. doi: 10.1055/s-2005-871266. [DOI] [PubMed] [Google Scholar]
- 91.Yao Y., Lin G., Xie Y., Ma P., Li G., Meng Q., Wu T. Preformulation studies of myricetin: A natural antioxidant flavonoid. Die Pharm. Int. J. Pharm. Sci. 2014;69:19–26. doi: 10.1691/ph.2014.3076. [DOI] [PubMed] [Google Scholar]
- 92.Guo R.X., Fu X., Chen J., Zhou L., Chen G. Preparation and characterization of microemulsions of myricetin for improving its antiproliferative and antioxidative activities and oral bioavailability. J. Agric. Food Chem. 2016;64:6286–6294. doi: 10.1021/acs.jafc.6b02184. [DOI] [PubMed] [Google Scholar]
- 93.Xu Y., Xie Q., Wu S., Yi D., Yu Y., Liu S. Myricetin induces apoptosis via endoplasmic reticulum stress and DNA double-strand breaks in human ovarian cancer cells. Mol. Med. Rep. 2016;13:2094–2100. doi: 10.3892/mmr.2016.4763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Kim M.E., Ha T.K., Yoon J.H., Lee J.S. Myricetin induces cell death of human colon cancer cells via BAX/BCL2-dependent pathway. Anticancer Res. 2014;34:701–706. [PubMed] [Google Scholar]
- 95.Cijo George V., Vijayakumaran Vijesh V., Inoka Madumani Amararathna D., Ayshwarya Lakshmi C., Anbarasu K., Ragupathi Naveen Kumar D. Mechanism of action of flavonoids in prevention of inflammation-associated skin cancer. Curr. Med. Chem. 2016;23:3697–3716. doi: 10.2174/0929867323666160627110342. [DOI] [PubMed] [Google Scholar]
- 96.Sangwan V., Banerjee S., Jensen K., Chen Z., Chugh R., Dudeja V. Primary and liver metastasis-derived cell lines from KrasG12D.; T.rp53R172H.; P.dx-1 Cre animals undergo apoptosis in response to triptolide. Pancreas. 2015;44:583. doi: 10.1097/MPA.0000000000000317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Jayakumar J.K., Nirmala P., Kumar B.A.P., Kumar A.P. Evaluation of protective effect of myricetin, a bioflavonoid in dimethyl benzanthracene-induced breast cancer in female Wistar rats. South Asian J. Cancer. 2014;3:107. doi: 10.4103/2278-330X.130443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Sun F., Zheng X.Y., Ye J., Wu T.T., Wang J.L., Chen W. Potential anticancer activity of myricetin in human T24 bladder cancer cells both in vitro and in vivo. Nutr. Cancer. 2012;64:599–606. doi: 10.1080/01635581.2012.665564. [DOI] [PubMed] [Google Scholar]
- 99.Yi J.L., Shi S., Shen Y.L., Wang L., Chen H.Y., Zhu J. Myricetin and methyl eugenol combination enhances the anticancer activity, cell cycle arrest and apoptosis induction of cis-platin against HeLa cervical cancer cell lines. Int. J. Clin. Exp. Pathol. 2015;8:1116. [PMC free article] [PubMed] [Google Scholar]
- 100.Iyer S.C., Gopal A., Halagowder D. Myricetin induces apoptosis by inhibiting P21 activated kinase 1 (PAK1) signaling cascade in hepatocellular carcinoma. Mol. Cell Biochem. 2015;407:223–237. doi: 10.1007/s11010-015-2471-6. [DOI] [PubMed] [Google Scholar]
- 101.Ci Y., Zhang Y., Liu Y., Lu S., Cao J., Li H. Myricetin suppresses breast cancer metastasis through down-regulating the activity of matrix metalloproteinase (MMP)-2/9. Phyther. Res. 2018;32:1373–1381. doi: 10.1002/ptr.6071. [DOI] [PubMed] [Google Scholar]
- 102.Okuda K., Mori K., Terayama K., Higuchi T.H. Isolation of geraniin from plants of Geranium and Euphorbiaceae (author’s transl) J. Pharm. Soc. Jpn. 1979;99:543–555. doi: 10.1248/yakushi1947.99.5_543. [DOI] [PubMed] [Google Scholar]
- 103.Okuda T., Yoshida T., Hatano T. Constituents of Geranium thunbergii Sieb. et Zucc. Part 12. Hydrated stereostructure and equilibration of geraniin. J. Chem. Soc. Perkin. Trans. 1982;1:9–14. doi: 10.1039/p19820000009. [DOI] [Google Scholar]
- 104.Palanisamy U.D., Ling L.T., Manaharan T., Appleton D. Rapid isolation of geraniin from Nephelium lappaceum rind waste and its anti-hyperglycemic activity. Food Chem. 2011;127:21–27. doi: 10.1016/j.foodchem.2010.12.070. [DOI] [Google Scholar]
- 105.Agyare C., Lechtenberg M., Deters A., Petereit F., Hensel A. Ellagitannins from Phyllanthus muellerianus (Kuntze) Exell.: Geraniin and furosin stimulate cellular activity, differentiation and collagen synthesis of human skin keratinocytes and dermal fibroblasts. Phytomedicine. 2011;18:617–624. doi: 10.1016/j.phymed.2010.08.020. [DOI] [PubMed] [Google Scholar]
- 106.Ito H. Metabolites of the ellagitannin geraniin and their antioxidant activities. Planta. Med. 2011;77:1110–1115. doi: 10.1055/s-0030-1270749. [DOI] [PubMed] [Google Scholar]
- 107.Yang Y., Zhang L., Fan X., Qin C., Liu J. Antiviral effect of geraniin on human enterovirus 71 in vitro and in vivo. Bioorg. Med. Chem. Lett. 2012;22:2209–2211. doi: 10.1016/j.bmcl.2012.01.102. [DOI] [PubMed] [Google Scholar]
- 108.Ren Z., Zou W., Cui J., Liu L., Qing Y., Li Y. Geraniin suppresses tumor cell growth and triggers apoptosis in human glioma via inhibition of STAT3 signaling. Cytotechnology. 2017;69:765–773. doi: 10.1007/s10616-017-0085-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Perera A., Ton S.H., Palanisamy U.D. Perspectives on geraniin, a multifunctional natural bioactive compound. Trends Food Sci. Technol. 2015;44:243–257. doi: 10.1016/j.tifs.2015.04.010. [DOI] [Google Scholar]
- 110.Liu X., Zhao M., Wu K., Chai X., Yu H., Tao Z. Immunomodulatory and anticancer activities of phenolics from emblica fruit (Phyllanthus emblica L.) Food Chem. 2012;131:685–690. doi: 10.1016/j.foodchem.2011.09.063. [DOI] [Google Scholar]
- 111.Zhai J.W., Gao C., Ma W.D., Wang W., Yao L.P., Xia X.X., Luo M., Zu Y.G., Fu Y.J. Geraniin induces apoptosis of human breast cancer cells MCF-7 via ROS-mediated stimulation of p38 MAPK. Toxicol. Mech. Methods. 2016;26:311–318. doi: 10.3109/15376516.2016.1139025. [DOI] [PubMed] [Google Scholar]
- 112.Kudo-Saito C., Shirako H., Takeuchi T., Kawakami Y. Cancer metastasis is accelerated through immunosuppression during Snail-induced EMT of cancer cells. Cancer Cell. 2009;15:195–206. doi: 10.1016/j.ccr.2009.01.023. [DOI] [PubMed] [Google Scholar]
- 113.Ko H. Geraniin inhibits TGF-β1-induced epithelial–mesenchymal transition and suppresses A549 lung cancer migration, invasion and anoikis resistance. Bioorg. Med. Chem. Lett. 2015;25:3529–3534. doi: 10.1016/j.bmcl.2015.06.093. [DOI] [PubMed] [Google Scholar]
- 114.Traber M.G., Packer L. Vitamin E: Beyond antioxidant function. Am. J. Clin. Nutr. 1995;62:1501S–1509S. doi: 10.1093/ajcn/62.6.1501S. [DOI] [PubMed] [Google Scholar]
- 115.Mène-Saffrané L., DellaPenna D. Biosynthesis, regulation and functions of tocochromanols in plants. Plant Physiol. Biochem. 2010;48:301–309. doi: 10.1016/j.plaphy.2009.11.004. [DOI] [PubMed] [Google Scholar]
- 116.Wong R.S.Y., Radhakrishnan A.K. Tocotrienol research: Past into present. Nutr. Rev. 2012;70:483–490. doi: 10.1111/j.1753-4887.2012.00512.x. [DOI] [PubMed] [Google Scholar]
- 117.Aggarwal B.B., Sundaram C., Prasad S., Kannappan R. Tocotrienols, the vitamin E of the 21st century: Its potential against cancer and other chronic diseases. Biochem. Pharmacol. 2010;80:1613–1631. doi: 10.1016/j.bcp.2010.07.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Ong A.S.H., Goh S.H. Palm oil: A healthful and cost-effective dietary component. Food Nutr. Bull. 2002;23:11–22. doi: 10.1177/156482650202300102. [DOI] [PubMed] [Google Scholar]
- 119.Sundram K., Sambanthamurthi R., Tan Y.A. Palm fruit chemistry and nutrition. Asia Pac. J. Clin. Nutr. 2003;12:355–362. [PubMed] [Google Scholar]
- 120.Mensink R.P., van Houwelingen A.C., Kromhout D., Hornstra G.A. Vitamin E concentrate rich in tocotrienols had no effect on serum lipids, lipoproteins, or platelet function in men with mildly elevated serum lipid concentrations. Am. J. Clin. Nutr. 1999;69:213–219. doi: 10.1093/ajcn/69.2.213. [DOI] [PubMed] [Google Scholar]
- 121.Packer L., Weber S.U., Rimbach G. Molecular aspects of α-tocotrienol antioxidant action and cell signalling. J. Nutr. 2001;131:369S–373S. doi: 10.1093/jn/131.2.369S. [DOI] [PubMed] [Google Scholar]
- 122.Frank J., Chin X.W.D., Schrader C., Eckert G.P., Rimbach G. Do tocotrienols have potential as neuroprotective dietary factors? Ageing Res. Rev. 2012;11:163–180. doi: 10.1016/j.arr.2011.06.006. [DOI] [PubMed] [Google Scholar]
- 123.Das S., Nesaretnam K., Das D.K. Tocotrienols in cardioprotection. Vitam. Horm. 2007;75:285–299. doi: 10.1016/S0083-6729(06)75011-7. [DOI] [PubMed] [Google Scholar]
- 124.Abdul Hafid S.R., Chakravarthi S., Nesaretnam K., Radhakrishnan A.K. Tocotrienol-Adjuvanted Dendritic Cells Inhibit Tumor Growth and Metastasis: A Murine Model of Breast Cancer. PLoS ONE. 2013;8:e74753. doi: 10.1371/journal.pone.0074753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Radhakrishnan A.K., Mahalingam D., Selvaduray K.R., Nesaretnam K. Supplementation with natural forms of vitamin e augments antigen-specific Th1-type immune response to tetanus toxoid. Biomed. Res. Int. 2013 doi: 10.1155/2013/782067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Huang Y., Wu R., Su Z.Y., Guo Y., Zheng X., Yang C.S. A naturally occurring mixture of tocotrienols inhibits the growth of human prostate tumor, associated with epigenetic modifications of cyclin-dependent kinase inhibitors p21 and p27. J. Nutr. Biochem. 2017;40:155–163. doi: 10.1016/j.jnutbio.2016.10.019. [DOI] [PubMed] [Google Scholar]
- 127.Tran A.T., Ramalinga M., Kedir H., Clarke R., Kumar D. Autophagy inhibitor 3-methyladenine potentiates apoptosis induced by dietary tocotrienols in breast cancer cells. Eur. J. Nutr. 2015;54:265–272. doi: 10.1007/s00394-014-0707-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Korać R.R., Khambholja K.M. Potential of herbs in skin protection from ultraviolet radiation. Pharmacogn. Rev. 2011;5:164. doi: 10.4103/0973-7847.91114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Zhang J.S., Zhang S.J., Li Q., Liu Y.H., He N., Zhang J., Zhou P.H., Li M., Guan T., Liu J.R. Tocotrienol-rich fraction (TRF) suppresses the growth of human colon cancer xenografts in Balb/C nude mice by the Wnt pathway. PLoS ONE. 2015;10:e0122175. doi: 10.1371/journal.pone.0122175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Manu K.A., Shanmugam M.K., Ramachandran L., Li F., Fong C.W., Kumar A.P. First evidence that γ-tocotrienol inhibits the growth of human gastric cancer and chemosensitizes it to capecitabine in a xenograft mouse model through the modulation of NF-κB pathway. Clin. Cancer Res. 2012;18:2220–2229. doi: 10.1158/1078-0432.CCR-11-2470. [DOI] [PubMed] [Google Scholar]
- 131.Husain K., Centeno B.A., Chen D.T., Hingorani S.R., Sebti S.M., Malafa M.P. Vitamin E δ-tocotrienol prolongs survival in the LSL-KrasG12D/+; LSL-Trp53R172H/+; Pdx-1-Cre (KPC) transgenic mouse model of pancreatic cancer. Cancer Prev. Res. 2013;6:1074–1083. doi: 10.1158/1940-6207.CAPR-13-0157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Chang C., Lee S.O., Yeh S., Chang T.M. Androgen receptor (AR) differential roles in hormone-related tumors including prostate, bladder, kidney, lung, breast and liver. Oncogene. 2014;33:3225–3234. doi: 10.1038/onc.2013.274. [DOI] [PubMed] [Google Scholar]
- 133.Rajasinghe L., Pindiprolu R., Razalli N., Wu Y., Gupta S. Delta Tocotrienol Inhibits MMP-9 Dependent Invasion and Metastasis of Non-Small Cell Lung Cancer (NSCLC) Cell by Suppressing Notch-1 Mediated NF-κb and uPA Pathways. FASEB J. 2015;29:718–752. [Google Scholar]
- 134.Jiang Q., Rao X., Kim C.Y., Freiser H., Zhang Q., Jiang Z. Gamma-tocotrienol induces apoptosis and autophagy in prostate cancer cells by increasing intracellular dihydrosphingosine and dihydroceramide. Int. J. Cancer. 2012;130:685–693. doi: 10.1002/ijc.26054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Weng-Yew W., Selvaduray K.R., Ming C.H., Nesaretnam K. Suppression of tumor growth by palm tocotrienols via the attenuation of angiogenesis. Nutr. Cancer. 2009;61:367–373. doi: 10.1080/01635580802582736. [DOI] [PubMed] [Google Scholar]
- 136.Wali V.B., Sylvester P.W. Synergistic antiproliferative effects of γ-tocotrienol and statin treatment on mammary tumor cells. Lipids. 2007;42:1113–1123. doi: 10.1007/s11745-007-3102-0. [DOI] [PubMed] [Google Scholar]
- 137.Selvaduray K.R., Radhakrishnan A.K., Kutty M.K., Nesaretnam K. Palm tocotrienols inhibit proliferation of murine mammary cancer cells and induce expression of interleukin-24 mRNA. J. Interf. Cytokine Res. 2010;30:909–916. doi: 10.1089/jir.2010.0021. [DOI] [PubMed] [Google Scholar]
- 138.Nesaretnam K., Ambra R., Selvaduray K.R., Radhakrishnan A., Reimann K., Razak G. Tocotrienol-rich fraction from palm oil affects gene expression in tumors resulting from MCF-7 cell inoculation in athymic mice. Lipids. 2004;39:459–467. doi: 10.1007/s11745-004-1251-1. [DOI] [PubMed] [Google Scholar]
- 139.Ji X., Wang Z., Geamanu A., Sarkar F.H., Gupta S.V. Inhibition of cell growth and induction of apoptosis in non-small cell lung cancer cells by delta-tocotrienol is associated with notch-1 down-regulation. J. Cell Biochem. 2011;112:2773–2783. doi: 10.1002/jcb.23184. [DOI] [PubMed] [Google Scholar]
- 140.Selvaduray K.R., Radhakrishnan A.K., Kutty M.K., Nesaretnam K. Palm tocotrienols decrease levels of pro-angiogenic markers in human umbilical vein endothelial cells (HUVEC) and murine mammary cancer Cells. Genes Nutr. 2012;7:53–61. doi: 10.1007/s12263-011-0223-0. [DOI] [PMC free article] [PubMed] [Google Scholar]