Abstract
Purpose
This study aimed to describe the care provide by Emergency Medical Services (EMS) to severe sepsis patients being transferred between acute care hospitals and identify how that care contributes to sepsis care goals.
METHODS
This was a single-center retrospective cohort study conducted at a 60,000-visit Midwestern academic emergency department, using run reports from 13 ambulance services transferring from 9 hospitals.
RESULTS
39 patients were included in the final cohort, transferred by 13 ambulance services from 9 hospitals. Included patients were adults with severe sepsis transferred by ambulance between 2009 and 2014. Thirty-nine patients were included in this cohort. 41% (n=12) of patients received an adequate fluid bolus of 30 mL/kg (median 42.9 mL/kg crystalloid fluid, IQR 8.0 mL/kg) prior to tertiary care arrival. Seventeen percent (n=2) of patients completed the adequate bolus during transfer time. Broad-spectrum antibiotics were initiated during transfer in 2 patients.
CONCLUSIONS
EMS sepsis care during transfer was limited. EMS crews primarily continued treatments previously initiated and did not take additional steps toward resuscitation targets. Data suggests the inter-emergency department transfer period may provide an opportunity to continue working toward treatment targets, though the time is currently underutilized.
Keywords: sepsis, emergency medical services, inter-hospital transfer, emergency department, ambulance, goal-directed care
INTRODUCTION
Severe sepsis is a life-threatening condition affecting over 750,000 patients in the United States annually. [1] 59% of septic patients presenting to an emergency department (ED) in a rural state require inter-emergency department (ED) transfer and could receive inappropriate antibiotic and fluid resuscitation therapy. [2][3] Pre-hospital sepsis management has been well studied, however little is known about the care provided during inter-ED transfer. [4][5] Our study sought to describe the care delivered to sepsis patients during inter-ED transfer and determine how EMS care contributes to adherence with sepsis treatment goals. We hypothesize that patients requiring inter-ED transfer during the first three hours of health-system contact receive minimal sepsis-specific care.
METHODS
This is a single-center retrospective case series of patients with severe sepsis and septic shock transferred to a single Midwestern academic ED between May 1, 2009 and January 1, 2014. All patients were seen in a smaller community hospital, treated in the ED, and transferred to the only comprehensive academic medical center in the region for their care. In our system, all transfers originating in the ED are accepted by the tertiary ED (rather than an inpatient service), and patients were transferred by ground ambulances with advanced life support (ALS) capabilities. We included adults (age ≥ 18 years) with severe sepsis or septic shock diagnosed at the tertiary hospital by International Classification of Diseases, 9th Revision, Clinical Modification, criteria (995.91, 995.92, and 785.52) who met at least 2 systemic inflammatory response syndrome (SIRS) criteria with an infection diagnosis prior to being transferred to the academic medical center. All hypotensive patients were assumed to be in septic shock. The diagnosis codes were used for screening, but all potentially eligible patients qualified by the Sepsis-2 criteria (since this study was conducted before publication of Sepsis 3. Exclusion criteria included having an initial diagnosis other than severe sepsis or septic shock and unavailable EMS run reports. Researchers contacted ambulance services to obtain missing run reports, and the analysis includes only cases with complete data available for analysis. Transport times, vital signs, fluid type and volume, medications, and procedures were abstracted from ambulance reports by a trained, unblinded data abstractor using a standardized form. Additional data were abstracted from charts at both the transferring and tertiary hospital, but EMS interventions were only abstracted from the EMS records. Twenty-five percent of charts were independently reviewed. Reviewed charts were selected consecutively from the beginning and end of cases (listed by medical record number). The primary reviewer was not aware of the secondary review process. The institutional review boards of all participating hospitals approved the use of their information under a waiver of informed consent, and this study is reported in accordance with the Strengthening the Reporting of Observational Studies (STROBE) Statement. [6]
Time from transferring emergency department contact until arrival at the tertiary emergency department was defined as “time before tertiary care arrival”. The “3-hour sepsis window” refers to the first 3 hours after first healthcare contact, according to the time-of-onset definitions of the Center for Medicare and Medicaid Services (CMS) SEP-1 measure. [7] The “transfer before 3 hours” cohort included patients with a transferring ED length-of-stay of ≤ 3 hours. Adequate fluid bolus, as defined by the CMS SEP-1 measure and the 2012 Surviving Sepsis Guidelines, is 30 ml/kg crystalloid bolus given within the first 3 hours of presentation. [6][7] Because this study was conducted using data from 2009 to 2014, we used the international consensus Sepsis-2 definitions rather than the Sepsis-3 definition published in 2016. Data was compiled and analyzed using IBM SPSS, v. 25 (IBM, Inc., Armonk, NY).
RESULTS
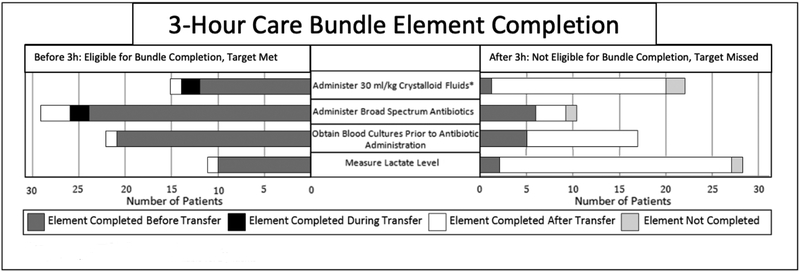
Thirty-nine patients and 14 EMS services were included in the final cohort, and our patient population has been described previously [2][3]. Twenty-nine patients (74%) had a time before tertiary arrival ≥ 3 hours, and the median time before tertiary arrival in that cohort was 4.9 h (IQR 2.1 h). Eleven patients (28%) had contact with EMS before the three-hour mark. No lactate levels were measured during transfer. Among patients with tertiary arrival ≥ 3 hours, 12 (41%) received an adequate fluid bolus (median 42.9 mL/kg crystalloid, IQR 8.0 mL/kg), with 2 (17%) patients receiving it during their transfer period. Of the 11 patients who were transferred before 3 hours, only 27% (n=3) met fluid administration targets. One patient was treated with vasopressor therapy, initiated by the transferring hospital. Antibiotics were started prior to transfer in 77% (n=30) patients and during transfer in 5% (n=2) of patients. Total completion of bundle elements in all stages of transfer is shown in Figure 1.
Figure 1. 3-hour care bundle element completion.
Administration time data not fully available for 2 patients.
DISCUSSION
Pre-hospital EMS care is a key element of sepsis treatment. [9] The role of EMS in improving clinical outcomes during inter-ED transfer is less defined. EMS providers are able to administer fluids, vasopressors, and antibiotics, pending local medical director approval. We do not have data on which services (if any) had existing sepsis protocols during this period. Our study demonstrates EMS providers have the opportunity to continue sepsis treatment within 3-hours for patients transferred very early in the course of disease..
Prior studies have shown transfer patients have associated delays in care and increased mortality. [2][3] Some delays may be due to the cumbersome nature of the transfer process. [10] Significant delays in care are attributed to preparing the patient for transfer, which in turn may prevent achieving time-sensitive resuscitation goals. [11] Because sepsis requires time sensitive treatment process and worsening clinical outcomes attributed to delays, systems should be developed to speed the transfer process and provide ongoing care throughout the process. While transferred patients are not included in current hospital-based quality reporting initiatives, the patients included in this study would qualify for components of CMS sepsis metrics by severity of illness criteria.
Although there are some limitations on EMS interventions, existing skills such as fluid and vasopressor administration can be leveraged to improve adherence rates to 3-hour care bundle goals. [12] Field lactate measurement devices provide a quick and accurate way for EMS providers to quantify an important, often unavailable data point. [13][14] The use of broad-spectrum antibiotics by EMS services will allow crews to improve antibiotic administration. Pre-hospital antibiotic administration protocols have been developed, improving the timeliness in early sepsis recognition and treatment. These protocols could be utilized during transfer to improve antibiotic administration rates. While antibiotic administration was high in our cohort, some of the patients transferred early had not received antibiotics, which could be an opportunity for improving care during transfer. [15] Standardized transfer protocols for ongoing medical control and communication between all care providers can improve patient outcomes, reduce medical error, and streamline the transfer process.
This study used a single tertiary care center and patients transferred from rural hospitals, potentially limiting the external validity. The cohort did include multiple hospitals and EMS services, however, so our findings remain generalizeable. As a retrospective study, the data available were limited to parameters documented accurately in the medical record.
CONCLUSION
Sepsis care during the inter-ED transfer period was limited, but data suggests an opportunity to improve sepsis resuscitation care. Many transferred patients are treated early in their disease, and EMS care may be an opportunity for improving early sepsis resuscitation. Future studies should explore how new technology, EMS antibiotic initiation, and telemedicine can increase the utilization of the inter-hospital transfer time and improve 3-hour treatment goal adherence.
ACKNOWLEDGEMENTS
The authors would like to acknowledge the following institutions that provided data for the conduct of this study: Unity Point Health - Allen Hospital, Washington County Hospitals and Clinics, Keokuk Area Hospital, Mercy Medical Center - Clinton, Broadlawns Medical Center, Genesis Medical Center, Covenant Medical Center, Henry County Health Center, Trinity Muscatine. We also acknowledge University of Iowa Healthcare Information Systems (Keith Burrell) and the University of Iowa Carver College of Medicine for providing the data and funding for this study.
Dr. Mohr is additionally supported by grant number K08HS025753 from the Agency for Healthcare Research and Quality. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality.
Supported, in part, by the University of Iowa Department of Emergency Medicine.
Footnotes
Conflicts of interest and source funding: The authors report that that they have no financial conflicts of interest.
Institution Where the Work was Performed: University of Iowa Carver College of Medicine, Iowa City, Iowa
References
- [1].Angus DC, Linde-Zwirble WT, Lidicker J, Clermont G, Carcillo J, Pinsky MR. Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Crit Care Med. 2001;29(7):1303–1310. [DOI] [PubMed] [Google Scholar]
- [2].Mohr NM, Harland KK, Shane DM, Ahmed A, Fuller BM, Torner JC. Inter-hospital transfer is associated with increased mortality and costs in severe sepsis and septic shock: An instrumental variables approach. Journal of critical care. 2016;36:187–194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Faine BA, Noack JM, Wong T, Messerly JT, Ahmed A, Fuller BM, Mohr NM. Interhospital Transfer Delays Appropriate Treatment for Patients With Severe Sepsis and Septic Shock: A Retrospective Cohort Study. Critical Care Medicine. 2015;43(12):2589–2596. [DOI] [PubMed] [Google Scholar]
- [4].Seymour CW, Rea TD, Kahn JM, Walkey AJ, Yealy DM, Angus DC. Severe Sepsis in Pre-Hospital Emergency Care: Analysis of Incidence, Care, and Outcome. American Journal of Res[oratpru amd Critical Care Medicine. 2012;186(12):1264–1271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Jouffroy R, Saade A, Muret A, Philippe P, Michaloux M, Carli P, Vivien B. Fluid resuscitation in pre-hospital management of septic shock. American Journal of Emergency Medicine. 2018;36(10):1754–1758. [DOI] [PubMed] [Google Scholar]
- [6].von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61(4):344–349. [DOI] [PubMed] [Google Scholar]
- [7].“Early Management Bundle, Severe Sepsis/Septic Shock.” Specifications Manual for National Hospital Inpatient Quality Measures, 5th ed., The Joint Commission, 2017, pp. SEP-1–1–SEP-1–54. [Google Scholar]
- [8].Rhodes A, Evans LE, Alhazzani W, Levy M, Antonelli M, Ferrer R, Kumar A, Sevransky JE, Sprung CL, Nunnally ME, Rochwerg B, Rubenfeld GD, Angus DC, Annane D, Beale RJ, Bellinghan GJ, Bernard GR, Chiche JD, Coopersmith C, De Backer DP, French CJ, Fujishima S, Gerlach H, Hidalgo JL, Hollenberg SM, Jones AE Karnad DR, Kleinpell RM, Koh Y, Lisboa TC, Machado FR, Marini JJ, Marshall JC, Mazuski JE, McIntyre LA, McLean AS Mehta S, Moreno RP, Myburgh J, Navalesi P, Nishia O, Osborn TM, Perner A, Plunkett CM, Ranirn M, Schorr CA, Seckel MA, Seymour CW, Shieh L, Shukri KA, Simpson SQ, Singer M, Thompson BT, Townsend SR, Van der Poll T, Vincent JL, Wiersinga WJ, Zimmerman JL, Dellinger RP. Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock: 2016. Intensive Care Med. 2017;43(3):304–377. [DOI] [PubMed] [Google Scholar]
- [9].Studnek JR, Artho MR, Garner CL, Jones AE. The impact of emergency medical services on the ED care of severe sepsis. The American Journal of Emergency Medicine. 2012;30(1):51–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Kereiakes DJ. Specialized centers and systems for heart attack care. Am Heart Hosp J. 2008;6(1):14–20. [DOI] [PubMed] [Google Scholar]
- [11].Newgard CD, McConnell KJ, Hedges JR, Mullins RJ. The benefit of higher level of care transfer of injured patients from nontertiary hospital emergency departments. J Trauma. 2007;63(5):965–971. [DOI] [PubMed] [Google Scholar]
- [12].Wang HE, Weaver MD, Shapiro NI, Yealy DM. Opportunities for emergency medical care of sepsis. Resuscitation. 2010;81:193–197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Shapiro NI, Fisher C, Donnino M, Cataldo L, Tang A, Trzeciak S, Horowitz G, Wolfe RE. The feasibility and accuracy of point-of-care lactate measurement in emergency department patients with suspected infection. The Journal of Emergency Medicine. 2010;39(1):89–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Boland LL, Hokanson JS, Fernstrom KM, Kinzy TG, Lick CJ, Satterlee PA, LaCroix BK. Prehospital lactate measurement by emergency medical services in patients meeting sepsis criteria. Western Journal of Emergency Medicine. 2016;17(5):648–655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Seymour CW, Kahn JM, Martin-Gill C, Callaway CW, Yealy DM, Scales D, Angus DC. Delays from first medical contact to antibiotic administration for sepsis. Critical Care Medicine. 2017; 45(5): 759–765. [DOI] [PMC free article] [PubMed] [Google Scholar]