Abstract
BACKGROUND AND OBJECTIVES:
Substance use disorder (SUD) is a wide-spread problem but physicians may feel inadequately prepared to provide addiction care. We sought to assess current addiction medicine curricula in US family medicine residencies (FMRs) and evaluate barriers to improving or implementing addiction medicine curricula.
METHODS:
Questions regarding addiction medicine training were added to the December 2015 Council of Academic Family Medicine Educational Research Alliance (CERA) survey to US FMR program directors to evaluate each FMR’s curriculum, potential workforce production, perceived barriers to improving or implementing curricula and faculty training in addiction medicine.
RESULTS:
Of 461 FMR directors, 227 (49.2%) responded; 28.6% reported a required addiction medicine curricula. Regional variations of having a required curriculum ranged from 41.3% in the Northeast to 20.0% in the South (P=0.07). Of residencies, 31.2% had at least one graduate obtain a buprenorphine prescription waiver in the past year and 8.6% had at least one graduate pursue an addiction medicine fellowship in the past 5 years. Lack of faculty expertise was the most commonly cited barrier to having a curriculum, with only 36.2% of programs having at least one buprenorphine waivered faculty member, 9.4% an addiction medicine board certified faculty, and 5.5% a fellowship trained faculty.
CONCLUSIONS:
Few FMRs have addiction medicine curricula and most graduates do not seek additional training. Multifaceted efforts, including developing model national curricula, training existing faculty, and recruiting addiction trained faculty, may improve addiction medicine training in family medicine residencies to better address the growing SUD epidemic.
Substance use disorder (SUD) is a growing problem in the United States. Deaths attributed to drug overdose increased almost three fold from 16,849 in 1999 to 47,055 in 2014.1 With more than 24 million individuals dependent on or abusing illicit drugs and alcohol in 2013,2 the estimated cumulative costs of substance abuse amounts to more than $700 billion annually, taking into account costs of crime, health care, and lost work productivity.3
The provision of addiction medicine services has been historically siloed from general medical care with specialized mental health professionals assuming the majority of SUD care.4 However, significant shortages exist in the mental health workforce. In 2014, the Health Resources and Services Administration reported approximately 4,000 Mental Health, Health Professional Shortage Areas (MPSAs).5 Many of these MPSAs encompass rural and low-income communities6,7 where more primary care physicians are located.8 There are more primary care physicians than mental health providers nationally, and many MPSAs have an adequate primary care work force. Since primary care physicians frequently identify SUD,9,10 primary care has the potential to serve as an opportune existing workforce to address SUD.11
Unfortunately, research demonstrates that many primary care physicians are uncomfortable with providing SUD care.12–18 As a result, many primary care physicians do not routinely address SUD. A large national survey in 2000 reported that less than 20% of primary care physicians felt prepared to identify SUDs and more than 50% of patients with SUD felt that their primary care physician did not address their SUD.12 Meanwhile, little is known about the current state of residency training in addiction medicine. The most recent survey on addiction medicine training in primary care residencies was completed in 1997. This survey found that 75% of family medicine residencies (FMR) offered an addiction medicine curriculum with an average of 8 hours of curricular time, most of which was didactic.19, 20
Our study aimed to describe the current state of addiction medicine training in US FMRs, including the prevalence of required curricula, resident pursuit of addiction training or certification, barriers to improving curricula, and faculty addiction medicine training.
Methods
We asked FMR directors to retrospectively report on their residency’s addiction medicine curriculum as part of a larger national omnibus survey conducted by the Council of Academic Family Medicine Educational Research Alliance (CERA).21 The study was reviewed and approved by the American Academy of Family Physicians’ Institutional Review Board.
The larger CERA survey is administered biannually to all ACGME accredited US FMR program directors as identified by the Association of Family Medicine Residency Directors (n=461). The survey includes a set of recurring general questions as well as a set of invited topical questions that change with each survey. The recurring questions describe FMR characteristics including residency director gender and years in position; number of non-US graduates; whether the program was university-based or community-based; geographic region; and community size. The invited questions are proposed by family medicine faculty and selected by the CERA steering committee. The survey is sent by email via Survey Monkey and three follow-up emails are sent to nonrespondents.
We added to the December 2015 CERA survey 12 questions about addiction medicine residency training that aimed to address the following domains: description of current addiction medicine curricula, family physician workforce production for addiction care, description of barriers to improving or implementing residency addiction medicine training, and current state of faculty addiction training. To validate the questions, the CERA steering committee reviewed draft questions for consistency with the study aims and overall readability. Draft questions were pretested with FMR faculty who were not part of the target population. Questions were then modified based on feedback.
Curriculum Questions
To describe current addiction medicine curricula, three questions queried whether programs had (1) a required curriculum, (2) a structured addiction medicine elective for additional and/or optional training, and (3) an area of concentration or specialty training track for additional and/or optional training. Programs with required curricula were then asked to describe the training setting with choices including classroom didactics as well as provision of care in an outpatient addiction facility, outpatient primary care clinic, and/or inpatient hospital setting. These questions were similar to the questions from the 1997 addiction medicine survey.19,20 Given the variable definitions of addiction medicine, we decided in consensus not to formally define the term addiction medicine and also decided not to define what constituted a required curriculum, leaving both up to the respondents’ judgement. Program directors were then asked to select the expected competency of residency graduates in addiction medicine with options including: (a) able to screen and refer; (b) able to screen and provide brief interventions; (c) able to screen, provide brief interventions and prescribe medications for SUD treatment; and (d) able to screen, provide in-depth interventions such as counseling and prescribe medications for SUD treatment.
Workforce Questions
To assess for potential workforce production, program directors were asked whether (1) any graduating residents pursued fellowship training in addiction medicine in the past 3 years and (2) any graduating residents obtained a buprenorphine prescription waiver in the past year. We considered obtaining a buprenorphine prescribing waiver as a measurable surrogate for the future provision of addiction medicine since buprenorphine, one of the primary medications used in the treatment of opioid use disorder in primary care, requires a Drug Enforcement Agency waiver to prescribe.
Barrier Questions
To determine barriers to improving or implementing addiction medicine curricula, program directors were asked to rank the top three barriers from a multiple choice list of seven. These options were selected in consensus among co-authors. Next, respondents were asked to rank on a scale of zero to ten, with zero being not a priority and ten being a high priority, how high a priority teaching addiction medicine was for their program.
Faculty Expertise Questions
Three questions queried program directors about faculty training in addiction medicine. These questions asked whether any faculty member in their residency program had (1) board certification in addiction medicine; (2) fellowship training in addiction medicine; and (3) a buprenorphine prescribing waiver.
Data Analysis
We used SAS 9.4 for our data analysis. Categorical measurements were summarized with frequencies and proportions, and numerical measurements were summarized with means and standard deviations. Chi-square tests were used to determine if the distribution of survey responses was significantly associated with other categorical survey responses and t-tests were used to compare numerical survey responses against categorical survey responses. Logistic regression was used to calculate the odds ratio of having at least one graduate obtaining a buprenorphine prescribing waiver and at least one graduate pursuing addiction medicine fellowship training based on other categorical survey responses.
Results
Respondent Characteristics
The response rate for the overall survey and the addiction medicine subset of questions was 49.2% (227/461). Of respondents, 17.6% were at university-based programs; 65.6% at community-based, university-affiliated programs; 12.8% at community-based, non-university-affiliated programs; and 4.0% at military-based programs (Table 1). Geographically, 24.0% of respondents were in the West, 24.0% in the Midwest, 20.5% in the Northeast and 31.1% in the South.
Table 1:
CERA Survey Respondents’ Residency Program Characteristics
| Respondent Residency Characteristics | Characteristics of all US Residencies | |
|---|---|---|
| Type of Residency Program | * | |
| University-Based | 40 (17.6%) | -- |
| Community-Based, University-Affiliated | 149 (65.6%) | -- |
| Community-Based, Non-affiliated | 29 (12.8%) | -- |
| Military | 9 (4.0%) | -- |
| Geographic Region | ** | |
| Puerto Rico | 1 (0.4%) | 4 (0.8%) |
| New England (NH, MA, ME, VT, RI, CT) | 11 (4.9%) | 16 (3.2%) |
| Middle Atlantic (NY, PA, NJ) | 35 (15.6%) | 67 (13.5%) |
| South Atlantic (FL, GA, SC, NC, VA, DC, WV, DE, MD) | 37 (16.4%) | 76 (15.4%) |
| East South Central (KY, TN, MS, AL) | 13 (5.8%) | 28 (5.7%) |
| East North Central (WI, MI, OH, IN, IL) | 29 (12.9%) | 95 (19.2%) |
| West South Central (OK, AR, LA, TX) | 20 (8.9%) | 53 (10.7%) |
| West North Central (ND, MN, SD, IA, NE, KS, MO) | 25 (11.1%) | 42 (8.5%) |
| Mountain (MT, ID, WY, NV, UT, AZ, CO, NM) | 16 (7.1%) | 38 (7.7%) |
| Pacific (WA, OR, CA, AK, HI) | 3 (16.9%) | 76 (15.4%) |
| Residency Community Size | * | |
| Less than 30,000 | 12 (5.4%) | -- |
| 30,000 to 74,999 | 40 (17.9%) | -- |
| 75,000 to 149,000 | 41 (18.3%) | -- |
| 150,000 to 499,999 | 62 (27.7%) | -- |
| 500,000 to 1 million | 35 (15.6%) | -- |
| >1 million | 34 (15.2%) | -- |
data for all program directors were not available
data for geographic region distribution were obtained from the 2016 CERA program directors’ survey since the geographic region distribution data were not available for the 2015 CERA program directors’ survey
Description of Addiction Medicine Training
Only 65 (28.6%) family medicine residencies have a required addiction medicine curriculum. Of those that do not have a required curriculum, an additional 28 (12.3%) offer structured elective experiences in addiction medicine (Table 2). An optional specialized area of concentration or specialty training track in addiction medicine is only offered at 27 programs (11.9%), with 10 of the 27 (37.0%) having a required curriculum. FMRs serving mid-sized communities with a population of 75,000–149,999, are most likely to have a required curriculum (46.3% vs 22.6–31.4%; P=0.03). Additionally, there was a trend, although not statistically significant, for FMRs in the Northeast to have a required curriculum (41.3% vs 20.0–33.3%; P=0.07). Furthermore, FMRs in the Northeast are significantly more likely to have a structured elective offered (54.3% vs 27.1–48.1%; P=0.02).
Table 2:
Characteristics of Addiction Medicine Curricula in Family Medicine Residencies
| Required Addiction Medicine Curriculum | Structured Addiction Medicine Elective for Additional/optional Training | Area of Concentration and/or Specialty Training Track in Addiction Medicine | ||||
|---|---|---|---|---|---|---|
| Total | 65 (28.6%) | 92 (40.5%) | 27 (11.9%) | |||
| Type of residency program | ||||||
| University-based n=40) | 11 (27.5%) | P = 0.44 | 23 (57.5%) | P = 0.02† | 7 (17.5) | P = 0.10 |
| Community-based, university-affiliated (n=149) | 47 (31.5%) | 59 (39.6%) | 14 (9.4%) | |||
| Community-based, non-affiliated (n=29) | 6 (20.7%) | 9 (31.0%) | 6 (20.7%) | |||
| Military (n=9) | 1 (11.1%) | 1 (11.1%) | 0 (0%) | |||
| Geographic Region | ||||||
| Northeast (n=46) | 19 (41.3%) | P = 0.07 | 25 (54.3%) | P = 0.02† | 9 (19.6%) | P = 0.25 |
| Midwest (n=54) | 18 (33.3%) | 26 (48.1%) | 6 (11.1%) | |||
| South (n=70) | 14 (20.0%) | 19 (27.1%) | 5 (7.1%) | |||
| West (n=54) | 14 (25.9%) | 22 (40.7%) | 7 (12.9%) | |||
| Community Size | ||||||
| < 30,000 (n=12) | 0 (0.0%) | P = 0.03† | 3 (25.0%) | P = 0.66 | 2 (16.7%) | P = 0.58 |
| 30,000 – 74,999 (n=39) | 11 (28.2%) | 18 (46.2%) | 7 (17.9%) | |||
| 75,000 – 149,999 (n=41) | 19 (46.3%) | 17 (41.5%) | 4 (9.8%) | |||
| 150,000 – 499,999 (n=62) | 14 (22.5%) | 21 (33.9%) | 9 (14.5%) | |||
| 500,000 – 1,000,000 (n=35) | 11 (31.4%) | 17 (48.6%) | 2 (5.7%) | |||
| > 1,000,000 (n=34) | 9 (26.5%) | 14 (41.2%) | 3 (8.8%) | |||
statistically significant result
Based on the subset of programs with a required addiction curriculum (n=65), 72.3% had class-based or online modular activities, 60.0% offered a clinical rotation at an outpatient addiction treatment facility, and 49.2% provided ongoing training integrated into the primary care office. Despite the paucity of FMRs with an addiction curriculum, 90.5% of program directors expected residents to be able to provide at least brief interventions for SUD and 41.8% expected residents to be comfortable prescribing medications for SUD. Of programs that expected residents to be comfortable prescribing medications for SUD, 38.7% had a required addiction curriculum.
Residency Graduate Outcomes
Of program directors, 8.6% reported having at least one graduate pursuing addiction medicine fellowship training in the past 5 years and 31.2% reported having at least one graduate who obtained a buprenorphine waiver in the past year upon graduation (Table 3). FMRs that required addiction training or offered additional elective opportunities or areas of concentration had higher odds of having resident graduates with buprenorphine waivers or pursuing fellowship training.
Table 3:
Odds of Residents Obtaining a Buprenorphine Waiver or Pursue Additional Training Based on Residency Addiction Medicine Curriculum**
| One or More Graduates Obtained a Buprenorphine Prescription Waiver (31.2%, n = 69) | One or More Graduates Pursued Addiction Medicine Fellowship in Past 5 Years (8.6%, n = 19) | |
|---|---|---|
| Required Addiction Curriculum (n=65) | OR = 3.05 (1.66, 5.65) † | OR = 1.17 (0.43, 3.24) |
| Elective Addiction Curriculum (n=92) | OR = 2.50 (1.40, 4.47) † | OR = 2.61 (0.99, 6.92) |
| Area of Concentration (n=27) | OR = 2.48 (1.08, 5.69) † | OR = 3.98 (1.37, 11.6) † |
reference OR = 1.00 in each scenario is not having a required addiction curriculum, an elective addiction curriculum or an area of concentration
statistically significant odds ratio
Barriers to Improving Addiction Curriculum and Faculty Training
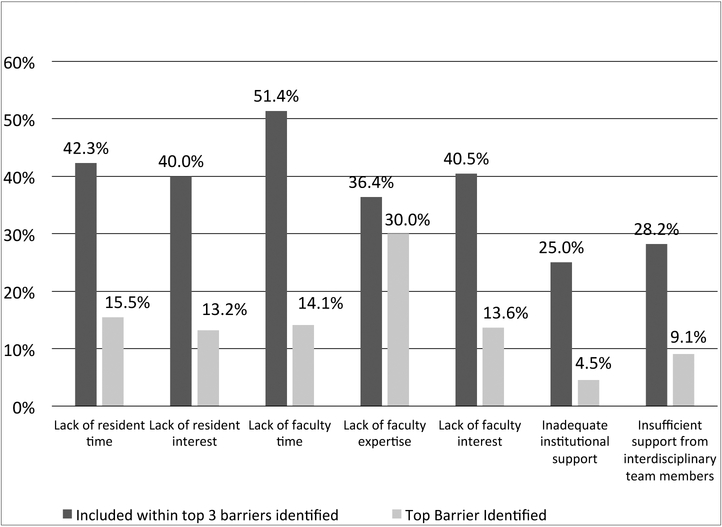
Program directors identified teaching addiction medicine in FMRs as a moderate priority (5.4 on a scale of 0–10). Lack of faculty expertise was most commonly identified as the top barrier and lack of faculty time was most commonly identified as one the top three barriers (Figure 1). Only 9.4% of FMRs have a faculty who is board certified in addiction medicine and only 5.5% have a faculty who has completed addiction medicine fellowship training. Likewise, only 36.2% of FMRs have a buprenorphine waivered faculty (Table 4). Having board-certified or buprenorphine waivered faculty was associated with higher odds of having a required or elective addiction medicine curriculum.
Figure 1:
Top Barrier and Top 3 Barriers that Residency Program Directors Report Regarding Providing and/or Improving Addiction Medicine Curriculum (n=220)**
Table 4:
Odds of Having an Addiction Medicine Curricula Based on Presence of at Least One Faculty Member With Addiction Medicine Certification/Training**
| Board Certification by ABAM* (9.4%, n=21) | Addiction Medicine Fellowship Training (5.5%, n=12) | Buprenorphine Waiver Authorization (36.2%, n=80) | |
|---|---|---|---|
| Required addiction medicine curriculum (n=65) | 3.15 (1.26, 7.85) † | 0.82 (0.22, 3.14) | 2.60 (1.42, 4.74) † |
| Elective addiction medicine curriculum (n=92) | 3.15 (1.22, 8.16) † | 2.07 (0.63, 6.73) | 2.36 (1.35, 4.15) † |
| Area of concentration (n=27) | 1.22 (0.34, 4.49) | 2.56 (0.65, 10.10) | 1.25 (0.55, 2.83) |
ABAM = American Board of Addiction Medicine
reference OR = 1.00 in each scenario is not having a faculty member with the respective certification or training
statistically significant odds ratio
Discussion
Most family medicine residencies do not have a required addiction medicine curriculum. Despite the increased national attention to the growing SUD epidemic and the multifaceted sequelae from drug abuse, program directors only rank teaching addiction medicine as a moderate priority. Nonetheless, many programs still expect residents to graduate proficient in diagnosing SUD and prescribing medications for SUD. In fact, more than 90% of program directors expect residents to be able to at least provide brief interventions for SUD, yet only a third have a required addiction medicine curriculum. Expectedly, few residency directors report that their graduates obtain buprenorphine prescribing waivers. Residency directors recognize that a lack of faculty expertise is a key barrier to improving or providing addiction training.
Multiple curricular and faculty development efforts have been attempted over the past decade to improve addiction medicine training.22–24 Most recently, in 2008, the Betty Ford Institute Consensus Conference on Graduate Medical Education (ACGME) developed a model curriculum and core competencies for family medicine substance abuse training.25 The Agency for Healthcare Research and Quality is also currently in the process of creating a report with models of integrated addiction care within primary care, which could be used to design residency training models. However, these efforts may fall short of their intended goal if family medicine faculty are not adequately trained to teach addiction medicine. Improving continuing medical education opportunities for faculty, in addition to providing technical assistance to programs that may want to start an addiction medicine curriculum, may improve training for family medicine residents and expand the workforce to care for patients with SUD.
This study has several limitations. First, the response rate of 49.2% limits generalizability, although responses were well distributed across various demographic groups and are similar to previous CERA studies.21 Responses may also be inaccurate due to recall bias, especially regarding residents obtaining buprenorphine waivers or faculty training. The survey did not define addiction medicine or describe what constituted having a curriculum (required, elective, and specialty track/area of concentration). This may have resulted in differing answers by program directors based on their perceptions of what constituted addiction medicine. Further, obtaining a buprenorphine waiver was used as a graduate outcome proxy but may not necessarily be reflective of actual provision of SUD care. Finally, the survey only assessed the state of family medicine residencies and did not include other primary care specialties.
This study updates for the first time in almost 20 years the state of addiction medicine training in US family medicine residencies. Interestingly, our study results are not consistent with the prior 1997 survey of primary care residencies on addiction training curriculum, which reported that 75% of FMR programs had a required curriculum. It is possible that fewer residency programs have an addiction medicine curriculum in 2015 than 1997. This potential trend toward fewer programs teaching addiction is concerning given the increase in drug overdose deaths since 1999.
Clearly, changes are needed in FMRs to better address the growing opioid epidemic. CERA survey respondents identify lack of faculty expertise as the top barrier to training residents. Efforts to recruit faculty with addiction expertise or train current faculty to teach addiction medicine will be key prerequisites to improving addiction medicine curricula in FMRs. Fundamentally, FMRs seem to have a disconnect between expectations of graduates treating SUD and how SUD is valued and prioritized. This is demonstrated by the lack of interest among faculty and residents, and the lack of required or elective addiction medicine training. Efforts may want to focus particularly on regions such as the South and West that have fewer residencies with addiction medicine curricula. Either requiring addiction medicine training or creating attractive addiction medicine electives and areas of concentration will be necessary to increase resident comfort with caring for patients with SUD. Trained faculty may create champions who have both the time and interest in promoting the value of addiction medicine. Effective curricula may change the culture and views about addiction medicine within FMRs. Future research can assist with these efforts by identifying curricular elements that best lead to graduate inclusion of addiction medicine in future practice, assess and highlight the need for addressing addiction medicine, and develop effective ways of including addiction medicine training in the full basket of residency training needs. These multifaceted efforts can help create a coordinated effort enabling today’s family physicians to better address the substance abuse epidemic.
ACKNOWLEDGEMENTS:
The authors would like to thank the CERA steering committee and the staff of the Society of Teachers of Family Medicine for their support and guidance in the development and conduct of this survey.
Footnotes
Presentations: Presented at Addiction Health Services Research Conference, Seattle, WA, October 2016; presented at North American Primary Care Research Group Annual Meeting, Colorado Springs, CO, November 2016.
References
- 1.Rudd R, Aleshire N, Zibbell J, Gladden M. Increases in Drug and Opioid Overdose Deaths - United States, 2000–2014. Centers for Disease Control and Prevention, 2016. [DOI] [PubMed] [Google Scholar]
- 2.Substance Abuse and Mental Health Services Administration. Behavioral Health Barometer: United States, 2014. Rockville, MD: Substance Abuse and Mental Health Services Administration, 2015. [Google Scholar]
- 3.National Institute on Drug Abuse. Trends and Statistics 2015. [August 20, 2015]. Available from: http://www.drugabuse.gov/related-topics/trends-statistics.
- 4.Compton WM, Blanco C, Wargo EM. Integrating addiction services into general medicine. JAMA. 2015;314(22):2401–2. [DOI] [PubMed] [Google Scholar]
- 5.Health Resources and Services Administration. Shortage Designation: Health Professional Shortage Areas & Medically Underserved Areas/Populations 2014. [August 21, 2015]. Available from: http://www.hrsa.gov/shortage/.
- 6.Substance Abuse and Mental Health Services Administration. An Action Plan for Behavioral Health Workforce Development. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2007. [Google Scholar]
- 7.Thomas KC, Ellis AR, Konrad TR, Holzer CE, Morrissey JP. County-level estimates of mental health professional shortage in the United States. Psychiatric services (Washington, DC). 2009;60(10):1323–8. [DOI] [PubMed] [Google Scholar]
- 8.Xierali IM, Tong ST, Petterson SM, Puffer JC, Phillips RL, Bazemore AW. Family physicians are essential for mental health care delivery. J Am Board Fam Med. 2013;26(2):114–5. [DOI] [PubMed] [Google Scholar]
- 9.Fleming MF. Screening and brief intervention in primary care settings. Alcohol Res Health. 2004;28(2):57. [PMC free article] [PubMed] [Google Scholar]
- 10.Friedmann PD, McCullough D, Chin MH, Saitz R. Screening and intervention for alcohol problems. J Gen Intern Med. 2000;15(2):84–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Samet JH, Friedmann P, Saitz R. Benefits of linking primary medical care and substance abuse services: Patient, provider, and societal perspectives. Arch Intern Med. 2001;161(1):85–91. [DOI] [PubMed] [Google Scholar]
- 12.Survey Research Laboratory. Missed Opportunity: National Survey of Primary Care Physicians and Patients on Substance Abuse. Chicago, IL: University of Illinois at Chicago, 2000. [Google Scholar]
- 13.Miller NS, Sheppard LM, Colenda CC, Magen J. Why physicians are unprepared to treat patients who have alcohol- and drug-related disorders. Acad Med. 2001;76(5):410–8. [DOI] [PubMed] [Google Scholar]
- 14.Wakeman SE, Pham-Kanter G, Donelan K. Attitudes, practices, and preparedness to care for patients with substance use disorder: results from a survey of general internists. Subst Abus. 2016:37(4):635–41. [DOI] [PubMed] [Google Scholar]
- 15.Shapiro B, Coffa D, McCance-Katz EF. A primary care approach to substance misuse. Am Fam Physician. 2013;88(2):113–21. [PubMed] [Google Scholar]
- 16.Van Hook S, Harris SK, Brooks T, et al. The “Six T’s”: barriers to screening teens for substance abuse in primary care. J Adolesc Health. 2007;40(5):456–61. [DOI] [PubMed] [Google Scholar]
- 17.Urada D, Teruya C, Gelberg L, Rawson R. Integration of substance use disorder services with primary care: health center surveys and qualitative interviews. Substance abuse treatment, prevention, and policy. 2014;9:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Barry DT, Irwin KS, Jones ES, et al. Integrating buprenorphine treatment into office-based practice: a qualitative study. J Gen Intern Med. 2009;24(2):218–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Isaacson JH, Fleming M, Kraus M, Kahn R, Mundt M. A national survey of training in substance use disorders in residency programs. J Stud Alcohol. 2000;61(6):912–5. [DOI] [PubMed] [Google Scholar]
- 20.Fleming MF, Manwell LB, Kraus M, Isaacson JH, Kahn R, Stauffacher EA. Who teaches residents about the prevention and treatment of substance use disorders? A national survey. J Fam Pract. 1999;48(9):725–9. [PubMed] [Google Scholar]
- 21.Mainous III AG, Seehusen D, Shokar N. CAFM Educational Research Alliance (CERA) 2011 Residency Director Survey. Fam Med. 2012;44(10):691–3. [PubMed] [Google Scholar]
- 22.Wakeman SE, Baggett MV, Pham-Kanter G, Campbell EG. Internal medicine residents’ training in substance use disorders: a survey of the quality of instruction and residents’ self-perceived preparedness to diagnose and treat addiction. Subst Abus. 2013;34(4):363–70. [DOI] [PubMed] [Google Scholar]
- 23.Wakeman SE, Pham-Kanter G, Baggett MV, Campbell EG. Medicine resident preparedness to diagnose and treat substance use disorders: Impact of an enhanced curriculum. Subst Abus. 2015;36(4):427–33. [DOI] [PubMed] [Google Scholar]
- 24.O’Connor PG, Nyquist JG, McLellan AT. Integrating addiction medicine into graduate medical education in primary care: the time has come. Ann Intern Med. 2011;154(1):56–9. [DOI] [PubMed] [Google Scholar]
- 25.Seale JP, Shellenberger S, Clark DC. Providing competency-based family medicine residency training in substance abuse in the new millennium: a model curriculum. BMC Med Educ. 2010;10:33. [DOI] [PMC free article] [PubMed] [Google Scholar]