Abstract
Preventing influenza infections is a national health priority, particularly among vulnerable geriatric and frail adults who reside in post-acute and long-term care (PALTC) settings. Older adults account for more than 70% of deaths from influenza, a reflection of decreased vaccine effectiveness in that age group. Annually vaccinating health care personnel (HCP) working with these vulnerable patients against influenza is critical to reducing influenza morbidity and mortality among patients. PALTC HCP have the lowest influenza vaccination rate when compared to HCP in other settings. The Advisory Committee on Immunization Practices (ACIP) recommends that all HCP receive an annual influenza vaccination, including those who do not have direct patient care responsibilities.1 Here, we discuss the importance of influenza vaccination for HCP, detail recommendations for influenza vaccination practice and procedures for PALTC settings, and offer support to PALTC settings and their staff on influenza vaccinations.
Keywords: Nursing Home, Influenza, Vaccinations, Aged, Policy
Summary of the article:
This article presents the Society for Post-Acute & Long-Term Care Medicine’s recommendations, and FAQs for influenza vaccinations for post-acute and long-term care health care personnel.
Background
Influenza has been linked to 12,000 to 56,000 deaths in the United States alone each year. Geriatric adults, those ≥ 65 years old, are the most vulnerable to severe infection and account for up to 85% of these deaths.2–4 For the 2016–2017 influenza season, the Centers for Disease Control and Prevention (CDC) estimates, influenza vaccination prevented over 5 million illnesses and prevented nearly 85,000 hospitalizations.5 Nonetheless, there were still 600,000 hospitalizations for influenza infections that year and most of those hospitalized were geriatric patients.5 The effectiveness of the influenza vaccine can vary widely from 19% to 60% over the past ten years (Table 2). This means the vaccine reduced a person’s risk of having to seek medical care by 40% in 2018, the CDC found. Even though that seems low, it is still our best way to prevent influenza and its complications.6 Residents who are cared for in post-acute and long-term care (PALTC) facilities are increased risk for exposure to influenza and more likely to have co-morbidities that increase vulnerability to poor outcome following infection.7, 8 Therefore, it is critical to maximize infection control efforts in these facilities amongst residents, staff, and visitors. Long-term care facility environments and the vulnerability of their residents provide a setting conductive to the rapid spread of influenza and other respiratory pathogens. Infections may be introduced by staff, visitors or new transferred residents, and outbreaks in such settings can have devastating consequences for individuals as well as placing extra strain on health services.9 As a result of these risks, influenza has a major impact on residents of nursing homes. Influenza attack rates typically range from 20 to 30%, and even higher rates have been documented. In addition, mortality rates during such influenza outbreaks often exceed 5%.10
TABLE 2.
Influenza Vaccine Effectiveness Over Time
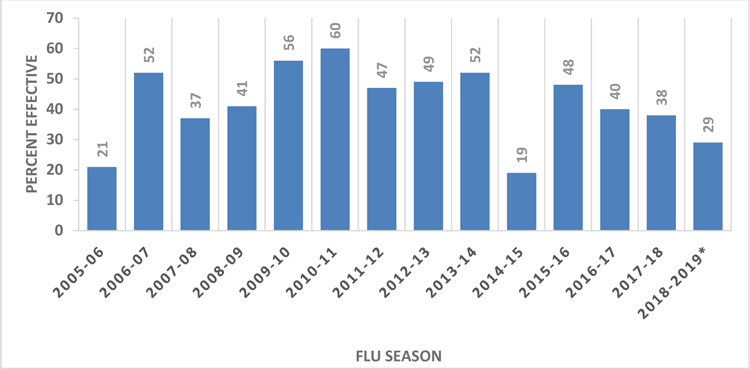 |
While CDC began estimating influenza vaccine effectiveness annually in 2004–05, this slide captures data beginning in 2008–2009 when the U.S. Influenza Vaccine Effectiveness Network (U.S. Flu VE Network) began. Earlier estimates may not have been representative because they were from only one site.
Rationale for influenza vaccines among post-acute and long-term care (PALTC) staff
As people age, their immune systems become less responsive rendering vaccinations, including seasonal influenza, less effective. While vaccination is still a critical part of controlling influenza in this vulnerable population, vaccination of patients alone is not sufficient. Infection control policies and procedures must be implemented to reduce influenza exposure for these geriatric patients. This makes reducing exposure to influenza important for the health and safety of geriatric patients. This is particularly true for frail elders who live in PALTC settings as they are dependent on health care personnel (HCP) for assistance with activities of daily living and therefore have direct exposure to HCP. Any person who is infected with influenza may shed the virus for 24 hours even before developing symptoms.11 Therefore, even the most conscientious HCP may still become infected with influenza and before symptoms develop, may unintentionally expose their PALTC residents to a potentially severe infection.
Vaccinating PALTC HCP reduces has been shown to save the lives of residents from influenza and reduce hospitalizations.12,13 While the influenza vaccine has generally had a low effectiveness, it still has proven to be an effective method to reduce influenza-like illness (ILI) and deaths. Since 2008–2009 influenza season when data were more rigorously collected, the effectiveness of influenza vaccines has ranged from 19% in the 2014–2015 season to 60% in the 2010–2011 season (see table 2).14 And yet, even with low and varied rates of effectiveness, studies show the positive impact on lives. In one randomized control study of 44 nursing homes, the vaccination of healthcare personnel resulted the equivalent of preventing five deaths, two admissions to hospital with ILI, and nine cases of ILI per 100 residents during the period of influenza activity.12 Similarly striking results were found in a similar, pair-matched randomized cluster-randomized trial which led to a 20% lower mortality in intervention homes and ILI was 30% lower among residents.
Vaccinating PALTC HCP also reduces their risk for infection, presenteeism, and absenteeism. Surveys of HCP indicate 75% of HCP have worked while ill.15,16 Yet, studies also show that among HCP who reported at least 1 day absent due to sickness, vaccinated HCP were significantly less absent with influenza compared to unvaccinated HCP.17–19 A meta-analysis examining the effects effects of influenza vaccination on HCP found that absenteeism from ILI was reduced substantially (RR = 0.62) as was the duration of being absent from work (RR=0.82).20
Unfortunately, PALTC HCP have been found to consistently have lower rates of influenza vaccination than HCP in all other settings. During the 2017–2018 influenza season, the CDC found that, while 78% of HCP respondents reported receiving an influenza vaccine, HCP in PALTC had the lowest rate of only 67% vaccinated. In contrast, 92% of HCP in hospitals reported receiving an influenza vaccine.21
Potential Barriers to Vaccinating HCP Against Influenza
Similar to the general public, HCP have reported multiple concerns that lead to hesitation to receive influenza vaccination. These concerns include potential adverse reactions, perceived personal lack of susceptibility to infection, and perceived lack of vaccine effectiveness. 22–28 In addition, qualitative research has shown that nurses specifically reported a general lack of trust for influenza vaccines, stating the vaccine is not effective, may lower overall immunity, and is not needed for otherwise healthy people. Furthermore, nurses surveyed were reported to feel that mandatory influenza vaccine protocols violate personal autonomy.29
This perceived lack of vaccine effectiveness is backed up by CDCs data. Since 2008–2009 influenza season when data were more rigorously collected, the effectiveness of influenza vaccines has ranged from 19% in the 2014–2015 season to 60% in the 2010–2011 season.14 Yet, even with relatively low rates of effectiveness, studies have shown that vaccination of HCP has led to significant reductions.12,13
Mandatory Influenza Vaccination Policies
Mandatory employer-based influenza vaccination protocols for HCP in general have been shown to have influenza vaccination rates near 100%. In contrast, settings in which HCP were encouraged to get vaccinated, but vaccination is not required, promoted, or offered on-site, less than half HCP were vaccinated.21 Most United States hospitals have mandatory influenza vaccination protocols.30 However, most PALTC facilities do not have mandatory vaccination programs. Over two-thirds of hospital-based HCPs reported that their institution required an annual influenza vaccine while less than 30% of HCPs working in PALTC reported similar requirements.21 This discrepancy is a vital factor explaining the difference in rates of vaccination among hospital-based HCP and HCP in PALTC facilities.
The CDC’s Advisory Committee for Immunization Practices (ACIP) recommends vaccinating all individuals who work in health care settings (HCP), even including HCP without direct patient care of patients and residents.31 In addition, all of the following professional organizations recommend mandatory seasonal influenza vaccinations for HCP: Society for Healthcare Epidemiology of America (SHEA);32 Association of Professionals in Infection Control and Epidemiology (APIC);33 American Academy of Family Physicians (AAFP); American Hospital Association; Infectious Disease Society for America (IDSA); American Nurses Association and AMDA—The Society for Post-Acute and Long-Term Care.34 All mandatory vaccination programs allow for exemption. Potential acceptable exemption from mandatory influenza vaccination for HCP include medical contraindication or religious reasons.35 Less than a third of the states require influenza vaccination for PALTC HCP. States vary in their legal requirements regarding influenza vaccination for HCPs (Table 1).36, 37
TABLE 1:
Requirements for Influenza Vaccination for Healthcare Personnel (HCP) by Reporting Statesa
| Requirements | Statesb | |
|---|---|---|
| Influenza vaccine required for HCP working in post-acute/long-term care | Alabama, Arkansas, Colorado, Delaware, Kentucky, Maryland, Massachusetts, New Hampshire, New York, North Carolina, Pennsylvania, Rhode Island, South Carolina, Tennessee, Texas, District of Columbia. | |
| Required only for those with direct patient contact | South Carolina, Texas | |
| Exemptionsc | ||
| Medical | All states except Delaware, Georgia, New Hampshire | |
| Religious | Alabama, Arkansas, Illinois, Kentucky, Maine, Maryland, Massachusetts, New Hampshire, New York, North Carolina, Pennsylvania, Rhode Island, District of Columbia | |
| Philosophical | Alabama, Arkansas, California, Colorado, Delaware, Georgia, Illinois, Kentucky, Maine, Maryland, Massachusetts, Missouri, New Hampshire, New York, North Carolina, Oklahoma, Oregon, Pennsylvania, Rhode Island, South Carolina, Tennessee, Texas, Utah, District of Columbia | |
| Unspecified | New Hampshire, New York, Texas, Utah | |
Based on information obtained from Appendix 1: Influenza Vaccination Laws for Healthcare Workers (HCWs) in Long-Term Care Facilities of 1. CDC - State Long-Term Care Facility Influenza Vaccination Laws - Publications by Topic - Public Health Law. https://www.cdc.gov/phlp/publications/topic/menus/ltcinfluenza/index.html. Accessed January 31, 2019. Please check with your local and/or state department of health for current information.
Includes the District of Columbia and Puerto Rico.
Applies to HCP in long term care settings
Recommendations and Implications
AMDA—The Society for Post-Acute and Long-Term Care Medicine (The Society) strongly supports influenza vaccination of all HCP, including those who do not provide direct care. The Society also recognizes a need for continued efforts to improve influenza vaccination rates. Box 1 details a policy statement regarding influenza vaccination, which was developed by the Infection Advisory Subcommittee (IAC) and adopted by The Society. Additionally, to support improved influenza vaccination rates among PALTC HCP, the IAC developed a list of frequently asked questions (Appendix 1). Seasonal influenza vaccines are an effective way that all HCP can support the health and safety of PALTC residents.
BOX 1. AMDA - The Society for Post-Acute and Long-Term Care Medicine Policy Statement on Influenza Vaccination for Healthcare Personnel.
AMDA - The Society for Post-Acute & Long-Term Care Medicine (the Society) supports mandatory annual influenza vaccination for all post-acute and long-term care HCP unless there is a medical contraindication. All HCP should be included in mandatory influenza vaccination programs, as all HCP, even those with indirect contact, have the potential to be in close proximity with residents, which can allow for transmission of infection.
The Society supports education for HCP on the efficacy and safety of influenza vaccination in general and as an important measure to enhance resident safety. It further recommends that medical directors and other practitioners encourage professional HCP and family caregivers to obtain an annual vaccination.
In addition, the Society recommends that HCP who do not receive an influenza vaccination must wear personal-protective masks when in direct resident contact during influenza season (October through April). The Society also recommends targeted education to any HCP who do not receive an influenza vaccination.
Finally following Advisory Committee on Immunization Practices (ACIP) recommendations, the Society recommends annual influenza vaccinations are made available and offered at no cost to all HCP working or volunteering in post-acute and long-term care settings.
Acknowledgments
Funding Sources: This work was supported in part by funds and facilities provided by the Cleveland Geriatric Research Education and Clinical Center (GRECC) and Specialty Care Center of Innovation at the Louis Stokes Cleveland Department of Veterans Affairs (VA) (RLPJ) as well as the VA Merit Review Program (PPO 16–118-1; RLPJ), the Agency for Healthcare Research and Quality [R18 HS022465–01 A1 (DAN)] and the Pittsburgh Claude D. Pepper Older Americans Independence Center [NIH P30 AG024827 (DAN)]. The findings and conclusions in this document are those of the authors, who are responsible for its content, and do not necessarily represent the views of the VA or of the United States Government.
APPENDIX. Infections Advisory Subcommittee FAQ: Influenza Vaccinations for Health Care Providers
In 2011, the Advisory Committee for Immunization Practices recommended influenza vaccination for all health care personnel (HCP), even those without direct patient contact.1 Vaccination rates for HCP in post-acute and long-term care facilities have been shown to be the lowest of any healthcare setting. Therefore, in 2018, the Society of Post-Acute and Long-term Care recommended mandatory annual influenza vaccination for all post-acute and long-term care HCP unless there is a medical contraindication. Here are answers to some Frequently Asked Questions about influenza vaccination.
1. Who should receive influenza vaccine (“flu shot”)?
All staff, including those who do and those who do not have direct contact with residents, should receive the flu shot each year.
2. Is it important for me to get a flu shot even if I am healthy?
YES! Thousands of older and frail residents die each year from influenza or flu. Vaccinating residents is important, but it’s best when residents and staff, like you are vaccinated.
3. Why do flu shots have to be mandatory?
Voluntary programs don’t help to increase the rates of flu shots. Avoiding the flu is especially important at nursing homes, where residents are already frail. Each year, between 12,000 and 56,000 Americans die from the flu, and over two thirds of the people who die are older than 65. 2,3,38 Flu shots help prevent you from getting the flu and help the residents you care for from getting the flu.
4. Why can’t I just wash my hands and wear a mask when I am sick?
If you’ve been exposed to the flu, you can spread the virus for a whole day even before you have any symptoms. Wearing a mask with a cough is important, but even before symptoms develop, the flu shot can help protect your patients. Washing your hands properly is also an important piece of preventing spreading infections to residents.
5. How effective is the flu shot, especially since it keeps changing every year?
Public health officials predict the main flu strains each year. These strains change each year and each year the flu shot changes to protect against the common strains. The effectiveness of a flu shot also varies from year-to-year and has been less than 50% in the last few years.14 Even though the flu shot works partially well, studies have shown that vaccinations results in substantially fewer flu-related deaths and flu or flu-like illnesses.12,13 That is why you should get a flu shot every year. Even if a strain isn’t in the flu shot, getting the flu shot can make your illness from flu milder. That means you will feel less sick, miss fewer days of work, and be at lower risk for bad outcomes from flu. The flu shot is the best way to prevent influenza for you and helps the people you care for.
6. Can I get the flu from the flu shot?
NO! You can’t get the flu from the flu shot. The flu shot only has parts of the virus that don’t cause illness. You can still get a cold from other viruses–the flu shot only protects against influenza virus.
7. Will the flu shot make me feel sick?
Most people who receive the flu shot don’t feel sick. Sometimes you can have soreness, redness or swelling where the injection was given or a slight fever and body aches. Over-the-counter medicines like ibuprofen and acetaminophen can help with these side effects. These side effects can be signs that the flu shot is inducing an immune response—that is, the flu shot is working. But, if you don’t have these side effects, it doesn’t mean that the shot isn’t working. If they do occur, they start soon after you received the flu shot and typically last no more a day or two. There may be a very small increased risk of severe reactions after the flu shot. There is a 1 or 2 cases of Guillain-Barré Syndrome from the flu shot.39 As with any medicine, there is a very remote chance of the flu shot causing a severe allergic reaction, other serious injury, or death. If you think you are having an allergic reaction, get medical help immediately.
8. I am pregnant. Should I get the flu shot?
Yes, pregnant women should especially get a flu shot. Flu shots have been given to millions of pregnant women over many years and have been shown to be completely safe. Pregnant women should get a flu shot only but not the nasal spray flu vaccine.40 Flu shots given during pregnancy help protect both you and your baby from the flu. Flu shots have been shown to reduce the chance of flu-associated respiratory infections in pregnant women by about one-half. If you get a flu shot you are also helping to protect your baby from flu illness for the first several months after birth, when a baby is too young to get vaccinated. So getting a flu shot while you’re pregnant is even more important. According to the CDC, you can get the flu shot during any trimester of your pregnancy.
9. Is there any reason I shouldn’t get a flu shot (medical exemption)?
There are medical reasons that the flu shot is not for everybody- are called medical exemptions. You should not get the flu shot if you have a documented severe allergy to the vaccine or any vaccine component or if you have a history of Guillain-Barré Syndrome within 6 weeks of a receiving a flu shot.
Even with an egg allergy you can get a flu shot. Most flu shots and the nasal flu vaccine spray have a small amount of egg in them. However, studies have shown that severe allergic reactions in people with egg allergies are unlikely. A recent CDC study found the rate of anaphylaxis after all vaccines is 1.31 per one million vaccine doses given.41 Since 2016, the CDC and ACIP recommend that people with a history of egg allergy of any severity should receive any licensed, recommended, and age-appropriate influenza vaccine.41 Additionally, if have had severe egg allergies in the past, you can get a egg-free flu shots just to be sure.
10. Is there any reason I should avoid a flu shot (religious exemption)?
[Note: It is up to the healthcare system to determine whether or not to allow religious exemptions.] Most religions support vaccinations. Two exceptions are the Dutch Reformed Church and the Church of Christ, Scientist. 35 If you have questions, talk with your facility to learn more.
11. Is there any reason I should avoid a flu shot (philosophical exemption)?
There are philosophical reasons—personal, moral, or other beliefs—regarding the influenza vaccination. At the same time, employment in a nursing home requires other vaccinations such as vaccines against measles, mumps, and rubella, all to avoid potentially getting or infecting others with these harmful diseases. Avoiding the flu is especially important at nursing homes, where residents are already frail. Each year, between 12,000 and 56,000 Americans die from the flu, and over two-thirds of the people who die are older than 65. 2,3,38 Flu shots help prevent you from getting the flu and help the patients and residents you care for from getting the flu. If you have questions, talk with your facility to learn more.
Footnotes
Conflicts of Interest
None of the authors have relevant conflicts of interest to disclose. RLPJ and SG serve as co-chairs of the Infection Advisory Subcommittee for AMDA--The Society for Post-Acute and Long-Term Care Medicine. RLPJ is the Principal Investigator on research grants from Accelerate and Pfizer; she has also participated in advisory boards for Pfizer and Merck.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Advisory Committee on Immunization Practices, Centers for Disease Control and Prevention (CDC). Immunization of health-care personnel: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep Morb Mortal Wkly Rep Recomm Rep 2011; 60:1–45. [PubMed] [Google Scholar]
- 2.CDC. Estimates of Deaths Associated with Seasonal Influenza --- United States, 1976–2007. https://www.cdc.gov/mmwr/preview/mmwrhtml/mm5933a1.htm. Accessed January 31 2019. [PubMed]
- 3.CDC. Estimating Seasonal Influenza-Associated Deaths in the United States. https://www.cdc.gov/flu/about/disease/us_flu-related_deaths.htm. Accessed January 31, 2019.
- 4.CDC. People 65 Years and Older & Influenza. https://www.cdc.gov/flu/about/disease/65over.htm. Accessed January 31, 2019.
- 5.CDC. Estimated Influenza Illnesses, Medical visits, and Hospitalizations Averted by Vaccination in the United States. https://www.cdc.gov/flu/about/disease/2016-17.htm. Accessed January 31, 2019.
- 6.CDC Seasonal Influenza Vaccine Effectiveness, 2005–2018. Table: Adjusted Vaccine Effectiveness for Influenza Seasons from 2005–2018, February 15, 2018.
- 7.Pop-Vicas A, Gravenstein S. Influenza in the elderly: a mini-review. Gerontology. 2011;57:397–404 [DOI] [PubMed] [Google Scholar]
- 8.Strausbaugh LJ, Sukumar SR, Joseph CL. Infectious disease outbreaks in nursing homes: an unappreciated hazard for frail elderly persons. Clin Infect Dis. 2003;36:870–876. [DOI] [PubMed] [Google Scholar]
- 9.Lansbury LE, Brown CS, Nguyen-Van-Tam JS. Influenza in long-term care facilities. Influenza. Other Respi Viruses. 2017; 11:356–366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bradley SF. Prevention of influenza in long-term care facilities. Long-Term Care Committee of the Society for Healthcare Epidemiology of America. Infect Control Hosp. Epidemiol. 1999;20(9):629–37. [DOI] [PubMed] [Google Scholar]
- 11.Lessler J, Reich NG, Brookmeyer R, Perl TM, Nelson KE, Cummings DAT. Incubation periods of acute respiratory viral infections: a systematic review. Lancet Infect Dis 2009; 9:291–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hayward AC, Harling R, Wetten S, et al. Effectiveness of an influenza vaccine programme for care home staff to prevent death, morbidity, and health service use among residents: cluster randomised controlled trial. BMJ 2006; 333:1241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lemaitre M, Meret T, Rothan-Tondeur M, et al. Effect of Influenza Vaccination of Nursing Home Staff on Mortality of Residents: A Cluster-Randomized Trial. J Am Geriatr Soc 2009; 57:1580–1586. [DOI] [PubMed] [Google Scholar]
- 14.CDC. Seasonal Flu Vaccine Effectiveness Studies. https://www.cdc.gov/flu/vaccines-work/effectiveness-studies.htm. Accessed November 7, 2019.
- 15.Widera E, Chang A, Chen HL. Presenteeism: a public health hazard. J Gen Intern Med 2010; 25:1244–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Weingarten S, Riedinger M, Bolton LB, et al. Barriers to influenza vaccine acceptance. A survey of physicians and nurses. Am J Infect Control 1989; 17:202–7. [DOI] [PubMed] [Google Scholar]
- 17.Frederick J, Brown AC, Cummings DA, et al. Protecting healthcare personnel in outpatient settings: the influence of mandatory versus nonmandatory influenza vaccination policies on workplace absenteeism during multiple respiratory virus seasons. Infect Control Hosp Epidemiol 2018; 39:452–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ishikane M, Kamiya H, Kawabata K, Higashihara M, Sugihara M, Tabuchi A, et al. Seasonal influenza vaccine (A/New York/39/2012) effectiveness against influenza A virus of health care workers in a long term care facility attached with the hospital, Japan, 2014/15: A cohort study. J Infect Chemother. 2016;22(11):777–9. [DOI] [PubMed] [Google Scholar]
- 19.Michiels B, Philips H, Coenen S, Yane F, Steinhauser T, Stuyck S, et al. The effect of giving influenza vaccination to general practitioners: a controlled trial []. BMC Med. 2006;4:17-. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Imai C, Toizumi M, Hall L, Lambert S, Halton K, Merollini K. A systematic review and meta-analysis of the direct epidemiological and economic effects of seasonal influenza vaccination on healthcare workers. PLoS One. 2018. June 7;13(6):e0198685. doi: 10.1371/journal.pone.0198685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Black CL. Influenza Vaccination Coverage Among Health Care Personnel — United States, 2017–18 Influenza Season. MMWR Morb Mortal Wkly Rep 2018; 67 https://www.cdc.gov/mmwr/volumes/67/wr/mm6738a2.htm. Accessed February 4, 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhang J, While AE, Norman IJ. Seasonal influenza vaccination knowledge, risk perception, health beliefs and vaccination behaviours of nurses. Epidemiol Infect 2012; 140:1569–1577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Christini AB, Shutt KA, Byers KE. Influenza vaccination rates and motivators among healthcare worker groups. Infect Control Hosp Epidemiol 2007; 28:171–177. [DOI] [PubMed] [Google Scholar]
- 24.Rhudy LM, Tucker SJ, Ofstead CL, Poland GA. Personal Choice or Evidence-Based Nursing Intervention: Nurses’ Decision-Making about Influenza Vaccination. Worldviews Evid Based Nurs 2010; 7:111–120. [DOI] [PubMed] [Google Scholar]
- 25.Hollmeyer HG, Hayden F, Poland G, Buchholz U. Influenza vaccination of health care workers in hospitals—A review of studies on attitudes and predictors. Vaccine 2009; 27:3935–3944. [DOI] [PubMed] [Google Scholar]
- 26.Shahrabani S, Benzion U, Yom Din G. Factors affecting nurses’ decision to get the flu vaccine. Eur J Health Econ 2009; 10:227–231. [DOI] [PubMed] [Google Scholar]
- 27.Prematunge C, Corace K, McCarthy A, et al. Qualitative motivators and barriers to pandemic vs. seasonal influenza vaccination among healthcare workers: A content analysis. Vaccine 2014; 32:7128–7134. [DOI] [PubMed] [Google Scholar]
- 28.Zhang J, While AE, Norman IJ. Nurses’ knowledge and risk perception towards seasonal influenza and vaccination and their vaccination behaviours: A cross-sectional survey. Int J Nurs Stud 2011; 48:1281–1289. [DOI] [PubMed] [Google Scholar]
- 29.Pless A, McLennan SR, Nicca D, Shaw DM, Elger BS. Reasons why nurses decline influenza vaccination: a qualitative study. BMC Nurs 2017; 16:20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Greene MT, Fowler KE, Ratz D, Krein SL, Bradley SF, Saint S. Changes in Influenza Vaccination Requirements for Health Care Personnel in US Hospitals. JAMA Netw Open. 2018. June 1;1(2):e180143. doi: 10.1001/jamanetworkopen.2018.0143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.CDC. Immunization of Health-Care Personnel. https://www.cdc.gov/mmwr/preview/mmwrhtml/rr6007a1.htm. Accessed January 31, 2019.
- 32.Talbot TR, Babcock H, Caplan AL, et al. Revised SHEA Position Paper: Influenza Vaccination of Healthcare Personnel. Infect Control Hosp Epidemiol 2010; 31:987–995. [DOI] [PubMed] [Google Scholar]
- 33.APIC_Influenza_Immunization_of_HCP_12711.pdf. Available at: http://knowledgeisinfectious.com/Resource_/TinyMceFileManager/Position_Statements/APIC_Influenza_Immunization_of_HCP_12711.PDF. Accessed January 31, 2019.
- 34.Honor Roll: Mandatory Influenza Vaccination Policies for Healthcare Personnel. Available at: http://www.immunize.org/honor-roll/influenza-mandates/. Accessed January 31, 2019.
- 35.Grabenstein JD. What the World’s religions teach, applied to vaccines and immune globulins. Vaccine 2013; 31:2011–2023. [DOI] [PubMed] [Google Scholar]
- 36.CDC - State Long-Term Care Facility Influenza Vaccination Laws - Publications by Topic - Public Health Law. https://www.cdc.gov/phlp/publications/topic/menus/ltcinfluenza/index.html. Accessed January 31, 2019.
- 37.Lindley MC, Horlick GA, Shefer AM, Shaw FE, Gorji M. Assessing state immunization requirements for healthcare workers and patients. Am J Prev Med 2007; 32:459–465. [DOI] [PubMed] [Google Scholar]
- 38.CDC. People 65 Years and Older & Influenza. https://www.cdc.gov/flu/about/disease/65over.htm. Accessed January 31, 2019.
- 39.CDC. Do flu vaccines cause side effects? https://www.cdc.gov/flu/prevent/general.htm#side-effects. Accessed November 8, 2019.
- 40.CDC. Flu Vaccine Safety and Pregnancy. https://www.cdc.gov/flu/highrisk/qa_vacpregnant.htm. Accessed November 8, 2019.
- 41.CDC. Flu Vaccine and People with Egg Allergies. https://www.cdc.gov/flu/protect/vaccine/egg-allergies.htm. Accessed January 31, 2019.


