Abstract
HIV prevention goals in the United States include reducing new HIV infections among people in the South Census region (commonly referred as the South). Using data reported to the National HIV Surveillance System, we examined trends in HIV diagnoses in the South, including the Deep South and Other South, during 2012–2017. Although diagnosis rates declined in all regions during the time period, declines were greater in all other regions compared to the Deep South, with the exception of the West region. Moreover, the South continues to have a diagnosis rate 50% higher (65% higher in the Deep South) than that of any other region. Diagnoses in the Deep South increased among some groups, including men who have sex with men, persons aged 25–34 years and Hispanics/Latinos. These findings highlight the need to further strengthen interventions in the South, particularly among communities of color and young adults.
Keywords: HIV, United States, South Census region, Disparities
Introduction
The disproportionate impact of HIV on the South Census region of the United States (“the South”: Alabama, Arkansas, Delaware, District of Columbia, Florida, Georgia, Kentucky, Louisiana, Maryland, Mississippi, North Carolina, Oklahoma, South Carolina, Tennessee, Texas, Virginia, and West Virginia) has been well-established [1–6]. Lower rates of retention in HIV care and poorer HIV survival have also been documented in the region [5–7]. These disparities may be related to factors including increased HIV-related stigma, discrimination, and poverty, which disproportionately affects the region as a whole, and blacks/African Americans in the South in particular [2, 5, 8]. National HIV prevention goals focus on reducing new HIV infections and HIV-related disparities, and include people living in the South as a priority population [9].
Previous analyses have documented higher proportions of diagnoses in the South via heterosexual transmission, and among women and blacks/African Americans, compared to other regions [10, 11]. Several urban areas in the South, including Memphis, Miami, Atlanta, and Baltimore, have a particularly high prevalence of HIV and may in part contribute to higher rates in the region [3]. However, disparities in the region are not limited to urban areas, as HIV diagnoses have been shown to be more common in smaller metropolitan areas with < 500,000 population and nonmetropolitan areas in the South compared to areas of similar population in other regions of the United States [5]. People living in rural areas often have less access to resources and services for management of chronic illness, including HIV, than those living in nonrural areas [12].
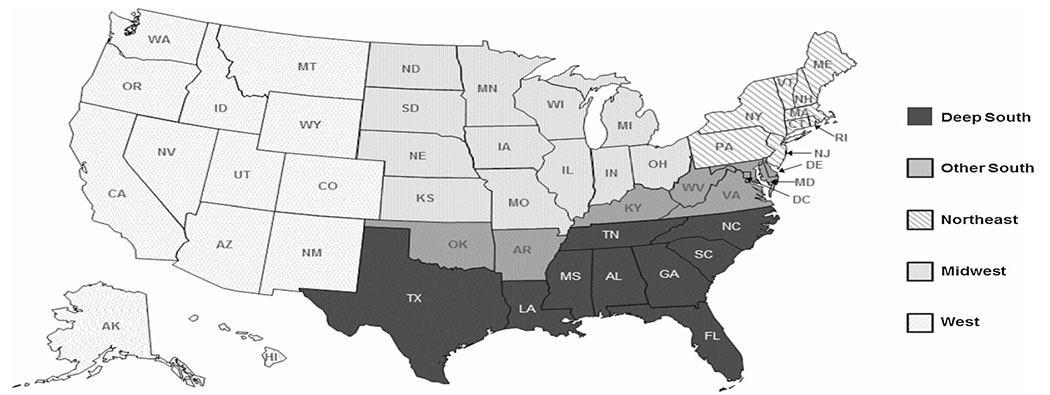
HIV diagnosis rates across the South are not homogenous, and the area considered the “Deep South” has particularly poor health outcomes for HIV as well as other health conditions [4, 13]. Reif et al. [2, 4] defined the “Deep South” as nine states (Alabama, Florida, Georgia, Louisiana, Mississippi, North Carolina, South Carolina, Tennessee and Texas) (Fig. 1). According to their findings, the HIV diagnosis rate in these Deep South states in 2014 (24 per 100,000 persons) was 45% higher than in the Other South states (Arkansas, Delaware, District of Columbia, Kentucky, Maryland, Oklahoma, Virginia, and West Virginia), which had a combined rate similar to the U.S. average (both 17 per 100,000 persons) [2].
Fig. 1.
United States by U.S. Census regions, with Deep South stratification
Though HIV diagnoses are declining overall, national HIV prevention goals will be difficult to achieve without continued progress, particularly in the South [9]. Monitoring progress toward national HIV prevention goals requires assessing progress over time. We examined trends in HIV diagnoses among persons aged 13 and older during 2012–2017 in the South region of the United States (including both Deep South and Other South) and other U.S. regions by key characteristics (age group, race/ethnicity, transmission category and urban/rural classification) using data reported to the National HIV Surveillance System (NHSS) through December 2018. This analysis provides new information on trends in HIV diagnosis in the South, enabling more focused prevention approaches.
Methods
Data Collection
This analysis used NHSS data reported to CDC as of December 31, 2018, on persons with HIV diagnosed during 2012–2017. Data were reported by surveillance programs of local, territorial, and state health departments of 50 states and the District of Columbia (D.C). Most cases are identified by health departments through routine reporting of results of laboratory test for HIV infection, and case reports are completed with demographic, risk, and clinical information. HIV surveillance records in the jurisdiction are updated as additional information is submitted to the health department in accordance with mandatory reporting regulations. De-identified data are then reported to CDC NHSS.
Data on race/ethnicity were collected by health departments and reported to CDC in accordance with the Office of Management and Budget (OMB)’s 1997 Revisions to the Standards for the Classification of Federal Data on Race and Ethnicity [14]. Because of small case counts among Native Hawaiians/Other Pacific Islanders, we combined this category with the Asian race/ethnicity category into a category called “Asian/Pacific Islander”, consistent with other federal statistics [15]. Persons classified as “Hispanic/Latino” can be of any race. Persons in other categories of race/ethnicity were not known to be of Hispanic/Latino ethnicity.
Transmission category represents the risk factor by which someone most likely acquired HIV (men who have sex with men [MSM], injection drug use [IDU], MSM and IDU, heterosexual contact, or other). Persons with more than one reported risk are classified in the transmission category listed first, with the exception of men who had sexual contact with other men and injected drugs, which forms a separate category of its own; persons in this category are not counted for both MSM and IDU transmission categories separately. Multiple imputation was used to assign transmission category to cases reported without an identified risk factor [16, 17].
Cases were assigned to their county and state of residence at time of HIV diagnosis. States were classified according to the four U.S. Census regions as defined by the U.S. Census Bureau (Northeast, Midwest, South and West) [18]. Counties were classified using the 2013 National Center for Health Statistics’ Urban–Rural Classification Scheme for Counties, which assigns each county to one of six categories [19]. Four of the six county categories are considered metropolitan, as they contain Metropolitan Statistical Areas (MSAs): large central metro (counties in MSAs of one million or more population that contain at least 250,000 inhabitants of any principal city of the MSA, or have the entire population of the largest principal city of the MSA); large fringe metro (counties in MSAs of one million or more population that did not qualify as large central metro counties); medium metro (counties in MSAs of 250,000 to 999,999 persons); and small metro (counties in MSAs of less than 250,000 persons). Nonmetropolitan county categories include micropolitan (counties in micropolitan statistical areas) and noncore (nonmetropolitan counties that did not qualify as micropolitan) [20].
Data Analysis
We used national HIV case surveillance data to calculate the annual number of reported HIV diagnoses and diagnosis rates in the United States reported during 2012–2017. All rates were calculated using population denominators from the U.S. Census Bureau for 2012–2017 and were per 100,000 population. We included data for persons aged ≥ 13 years reported to CDC through December 2018. We summarized the data by U.S. Census region and further stratified the South region into Deep South (Alabama, Florida, Georgia, Louisiana, Mississippi, North Carolina, South Carolina, Tennessee and Texas) and Other South (Arkansas, D.C., Delaware, Kentucky, Maryland, Oklahoma, Virginia, and West Virginia; Fig. 1). Next, for the Deep South, we calculated HIV diagnosis rates during 2012–2017 by age at diagnosis, race/ethnicity, transmission category, and urban/rural classification. Differences in annual rates were reported when the rates differed by at least five percent.
When examining temporal trends, we determined the estimated annual percent change (EAPC) [21, 22]. We calculated the EAPC and 95% confidence intervals (CIs) in diagnosis rates by using a binomial distribution. Because of unknown population denominators, case counts (rather than rates) were used to analyze diagnoses by transmission category; the EAPC in case counts were calculated by using a Poisson distribution. We analyzed the data using SAS version 9.4 (SAS Institute, Cary NC) and considered trends statistically significant if the EAPC CI excluded 0. Trends described as stable were those not found to be statistically significant.
Results
Trends in HIV Diagnosis Rates by Region
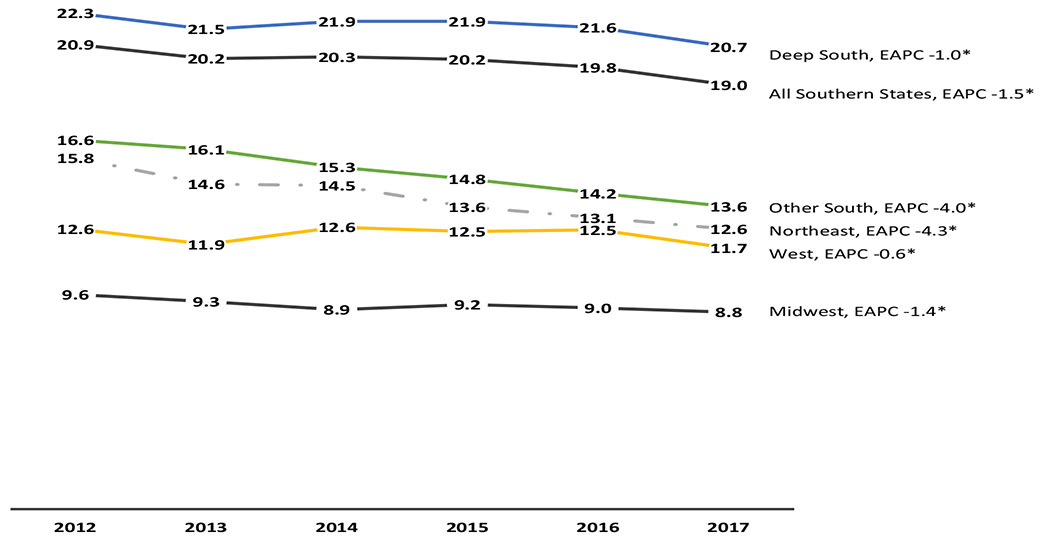
During 2012–2017, of the 237,663 persons aged 13 years and older diagnosed with HIV in the United States, 50% (120,485) resided in the South, with the nine Deep South states accounting for 82% (98,502) of diagnoses in the South and 41% overall. HIV diagnosis rates in 2017 were highest in the South (19.0 per 100,000), followed by the Northeast (12.6), West (11.7), and Midwest (8.8). Rates declined over time in all regions (Fig. 2). Declines in rates over time were most pronounced in the Northeast (EAPC − 4.3; CI − 4.8, − 3.7). Although the South experienced declines in diagnosis rates (EAPC − 1.5; CI − 1.8, − 1.2), the South had the highest rates per year (20.9 per 100,000 in 2012 and 19.0 in 2017) compared to all other regions (Fig. 2).
Fig. 2.
Trends in HIV diagnosis, 2011–2016, United States, by region including Deep South. The Deep South is defined as Alabama, Florida, Georgia, Louisiana, Mississippi, North Carolina, South Carolina, Tennessee and Texas. Other South is defined as Arkansas, Delaware, District of Columbia, Kentucky, Maryland, Oklahoma, Virginia, and West Virginia. Rates are per 100,000 population for all persons aged 13 and older. *Denotes statistical significance (EAPC 95% confidence interval does not include 0)
Annual rates in the Deep South, while declining (EAPC − 1.0; CI − 1.3, − 0.6), were higher than rates in all other regions every year (Fig. 2). Rates in the Other South region were lower than those in the Deep South and declined more steeply (EAPC − 4.0; CI − 4.7, − 3.2), but also exceeded rates observed in all other regions.
Differences and Trends in HIV Diagnosis Rates in the Deep South
Table 1 displays HIV diagnosis rates in the Deep South during 2012–2017 by state, race/ethnicity, age, transmission category, and urban/rural category. During 2012–2017, diagnosis rates declined in Tennessee (EAPC − 4.2; 95% CI 5.8, − 2.6), Georgia (− 1.0; CI − 1.9, − 0.1), and Texas (− 1.5; CI − 2.2, − 0.8). Diagnosis rates declined among persons of multiple races (EAPC − 13.6; CI − 15.5, − 11.6), blacks/African Americans (EAPC − 1.8; CI − 2.3, − 1.3), and whites (EAPC − 0.9; CI − 1.7, − 0.2). Statistically significant increases in diagnosis rates were observed among American Indians/Alaska Natives (EAPC 12.5; CI 1.9, 24.3; results should be interpreted with caution because of small sample sizes) and Hispanic/Latinos (EAPC 0.9; CI 0.1, 1.7). HIV diagnosis rates among Asians/Pacific Islanders were stable (EAPC 0.7; CI − 2.9, 4.4). HIV diagnosis trends varied by age, with diagnosis rates increasing over the time period among those aged 25–29 (EAPC 3.5; CI 2.6, 4.4) and 30–34 (EAPC 2.6; CI 1.6, 3.7). HIV diagnosis rates declined among those aged 40–59 years (Age 40–44: EAPC 5.6; CI − 6.8, − 4.4. Age 45–49: EAPC − 6.7; CI − 7.9, 5.6. Age 50–54: EAPC − 2.3; CI − 3.7, − 1.0. Age 55–59: EAPC − 2.0; CI − 3.6, − 0.3). Trends for all other age groups were stable. By transmission category, the number of HIV diagnoses increased among men reporting MSM contact (EAPC 1.5; CI 1.0, 2.0). HIV diagnoses in the Deep South also decreased among women reporting injection drug use and heterosexual risk factors (EAPC − 2.6; CI − 5.0, − 0.1 and EAPC − 1.2; − 2.1, − 0.4, respectively). The number of diagnoses related to other transmission modes was stable. HIV diagnosis rates declined over the time period in large central and fringe metro areas (EAPC − 2.0; CI − 2.5, − 1.5 and EAPC − 0.8; CI − 1.7, − 0.0, respectively) as well as in micropolitan and noncore areas (EAPC − 2.9; CI − 4.5, 1.3, and EAPC − 2.1, CI − 4.0, − 0.2, respectively). HIV diagnosis rates in medium and small metro areas were stable.
Table 1.
Trends in HIV Diagnosis among adults and adolescents by demographic characteristics, 2012–2017, Deep South, United States
| 2012 |
2013 |
2014 |
2015 |
2016 |
2017 |
Total N | EAPC | EAPC 95% CI | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No. | Rate | No. | Rate | No. | Rate | No. | Rate | No. | Rate | No. | Rate | ||||
| Total | 16,305 | 22.3 | 15,976 | 21.5 | 16,470 | 21.9 | 16,716 | 21.9 | 16,744 | 21.6 | 16,291 | 20.7 | 98,502 | −1.0 | (−1.3, −0.6) |
| Deep south states | |||||||||||||||
| Alabama | 666 | 16.6 | 633 | 15.7 | 673 | 16.6 | 664 | 16.3 | 664 | 16.3 | 653 | 15.9 | 3953 | −0.3 | (−2.1, 1.6) |
| Florida | 4391 | 26.6 | 4302 | 25.7 | 4485 | 26.4 | 4587 | 26.5 | 4684 | 26.5 | 4590 | 25.5 | 27,039 | −0.3 | (−1.0, 0.4) |
| Georgia | 2677 | 33.0 | 2340 | 28.6 | 2385 | 28.8 | 2621 | 31.2 | 2493 | 29.3 | 2584 | 30.0 | 15,100 | −1.0 | (−1.9,−0.1) |
| Louisiana | 1024 | 27.0 | 1135 | 29.7 | 1206 | 31.4 | 1098 | 28.5 | 1118 | 28.9 | 1008 | 26.1 | 6589 | −1.0 | (−2.4, 0.4) |
| Mississippi | 445 | 18.2 | 471 | 19.1 | 477 | 19.3 | 508 | 20.6 | 422 | 17.1 | 426 | 17.2 | 2749 | −1.5 | (−3.7,0.7) |
| North Carolina | 1231 | 15.2 | 1282 | 15.6 | 1310 | 15.8 | 1324 | 15.8 | 1391 | 16.3 | 1301 | 15.1 | 7839 | 0.2 | (−1.0, 1.5) |
| South Carolina | 701 | 17.8 | 707 | 17.7 | 761 | 18.8 | 667 | 16.2 | 744 | 17.8 | 707 | 16.7 | 4287 | −1.3 | (−3.0, 0.5) |
| Tennessee | 853 | 15.9 | 770 | 14.2 | 757 | 13.8 | 742 | 13.4 | 709 | 12.7 | 713 | 12.7 | 4544 | −4.2 | (−5.8,−2.6) |
| Texas | 4317 | 20.6 | 4336 | 20.3 | 4416 | 20.3 | 4505 | 20.3 | 4519 | 20.0 | 4309 | 18.7 | 26,402 | −1.5 | (−2.2,−0.8) |
| Race/ethnicity | |||||||||||||||
| American Indian/Alaska Native | 21 | 6.7 | 7 | 2.2 | 23 | 7.1 | 30 | 9.2 | 32 | 9.6 | 26 | 7.7 | 139 | 12.5 | (1.9, 24.3) |
| Asian/Pacific Islander | 128 | 6.1 | 165 | 7.6 | 162 | 7.1 | 197 | 8.2 | 184 | 7.3 | 175 | 6.6 | 1011 | 0.7 | (−2.9, 4.4) |
| Black/African American | 8843 | 63.2 | 8504 | 59.8 | 8769 | 60.7 | 8826 | 60.1 | 8747 | 58.7 | 8534 | 56.5 | 52,223 | −1.8 | (−2.3, −1.3) |
| Hispanic/Latinoa | 3141 | 24.0 | 3251 | 24.2 | 3473 | 25.1 | 3712 | 26.0 | 3832 | 26.0 | 3711 | 24.4 | 21,120 | 0.9 | (0.1, 1.7) |
| White | 3619 | 8.4 | 3528 | 8.2 | 3564 | 8.2 | 3528 | 8.1 | 3529 | 8.0 | 3542 | 8.0 | 21,310 | −0.9 | (−1.7, −0.2) |
| Multiple races | 553 | 71.7 | 521 | 64.7 | 479 | 57.0 | 423 | 48.2 | 420 | 45.8 | 303 | 31.7 | 2699 | −13.6 | (−15.5, −11.6) |
| Age at diagnosis | |||||||||||||||
| 13–19 | 862 | 10.3 | 755 | 9.0 | 777 | 9.2 | 843 | 9.9 | 799 | 9.3 | 813 | 9.4 | 4849 | −0.8 | (−2.4, 0.9) |
| 20–24 | 3031 | 47.4 | 3021 | 46.6 | 3291 | 50.6 | 3228 | 49.9 | 3082 | 48.2 | 2818 | 44.6 | 18,471 | −0.6 | (−1.4, 0.3) |
| 25–29 | 2491 | 41.4 | 2690 | 44.3 | 3021 | 48.5 | 3181 | 49.6 | 3426 | 51.9 | 3266 | 48.4 | 18,075 | 3.5 | (2.6, 4.4) |
| 30–34 | 2021 | 34.2 | 2041 | 34.0 | 2139 | 35.1 | 2226 | 36.2 | 2369 | 38.0 | 2400 | 38.1 | 13,196 | 2.6 | (1.6, 3.7) |
| 35–39 | 1603 | 28.6 | 1605 | 28.5 | 1648 | 28.8 | 1722 | 29.4 | 1744 | 29.0 | 1801 | 29.3 | 10,123 | 0.6 | (−0.6, 1.7) |
| 40–44 | 1741 | 29.0 | 1547 | 25.7 | 1466 | 24.5 | 1386 | 23.4 | 1318 | 22.6 | 1233 | 21.2 | 8691 | −5.6 | (−6.8, −4.4) |
| 45–49 | 1698 | 28.0 | 1525 | 25.6 | 1432 | 24.3 | 1358 | 22.9 | 1247 | 20.6 | 1213 | 19.8 | 8473 | −6.7 | (−7.9, −5.6) |
| 50–54 | 1280 | 20.7 | 1223 | 19.7 | 1187 | 18.9 | 1200 | 19.2 | 1169 | 18.9 | 1098 | 18.0 | 7157 | −2.3 | (−3.7, −1.0) |
| 55–59 | 795 | 14.1 | 818 | 14.2 | 764 | 13.0 | 787 | 13.1 | 767 | 12.6 | 806 | 13.1 | 4737 | −2.0 | (−3.6, −0.3) |
| 60–64 | 443 | 9.0 | 429 | 8.6 | 417 | 8.1 | 437 | 8.3 | 466 | 8.6 | 467 | 8.4 | 2659 | −1.0 | (−3.1, 1.3) |
| 65+ | 340 | 2.8 | 322 | 2.6 | 328 | 2.5 | 348 | 2.6 | 357 | 2.5 | 376 | 2.6 | 2071 | −1.2 | (−3.6, 1.4) |
| Transmission category: male | |||||||||||||||
| Male-to-male sexual contact | 10,097 | – | 10,077 | – | 10,611 | – | 10,843 | – | 10,874 | – | 10,673 | – | 63,175 | 1.5 | (1.0, 2.0) |
| Injection drug use | 463 | – | 425 | – | 427 | – | 394 | – | 368 | – | 377 | – | 2453 | −4.3 | (−6.5, −2.1) |
| Male-to-male sexual contact and injection drug use | 411 | – | 431 | – | 434 | – | 444 | – | 409 | – | 399 | – | 2527 | −0.8 | (−3.0, 1.5) |
| Heterosexual contactb | 1710 | – | 1592 | – | 1613 | – | 1689 | – | 1701 | – | 1515 | – | 9820 | −1.0 | (−2.1,0.2) |
| Otherc | 17 | – | 14 | – | 13 | – | 9 | – | 10 | – | 10 | – | 73 | −11.0 | (−22.3,2.0) |
| Transmission category: female | |||||||||||||||
| Injection drug use | 393 | – | 335 | – | 339 | – | 345 | – | 340 | – | 325 | – | 2077 | −2.6 | (−5.0, −0.1) |
| Heterosexual contactb | 3206 | – | 3081 | – | 3026 | – | 2987 | – | 3032 | – | 2975 | – | 18,307 | −1.2 | (−2.1, −0.4) |
| Otherc | 10 | – | 21 | – | 7 | – | 6 | – | 11 | – | 16 | – | 71 | 0.7 | (−12.2, 15.4) |
| 2013 Urban–rural classification scheme for Counties | |||||||||||||||
| Large central metro | 7267 | 35.9 | 7043 | 34.2 | 7242 | 34.5 | 7471 | 34.9 | 7296 | 33.5 | 6955 | 31.4 | 43,274 | −2.0 | (−2.5, −1.5) |
| Large fringe metro | 2989 | 19.3 | 2898 | 18.4 | 3010 | 18.7 | 2943 | 17.8 | 3137 | 18.6 | 3150 | 18.2 | 18,127 | −0.8 | (−1.7, 0.0) |
| Medium metro | 3320 | 17.3 | 3407 | 17.6 | 3521 | 18.0 | 3443 | 17.4 | 3558 | 17.7 | 3515 | 17.3 | 20,764 | −0.1 | (−0.9, 0.7) |
| Small metro | 1076 | 15.1 | 1018 | 14.2 | 1084 | 14.9 | 1175 | 16.0 | 1144 | 15.5 | 1102 | 14.8 | 6599 | 0.7 | (−0.8, 2.1) |
| Micropolitan | 861 | 13.5 | 823 | 12.8 | 852 | 13.3 | 814 | 12.6 | 763 | 11.8 | 754 | 11.6 | 4867 | −2.9 | (−4.5, −1.3) |
| Noncore | 601 | 12.4 | 588 | 12.1 | 573 | 11.8 | 583 | 12.0 | 588 | 12.1 | 513 | 10.5 | 3446 | −2.1 | (−4.0, −0.2) |
The Deep South is defined as Alabama, Florida, Georgia, Louisiana, Mississippi, North Carolina, South Carolina, Tennessee and Texas. Other South is defined as Arkansas, Delaware, District of Columbia, Kentucky, Maryland, Oklahoma, Virginia, and West Virginia. Rates are per 100,000 population for all persons aged 13 and older. Rates are not calculated by transmission category because of the lack of denominator data
Hispanics/Latinos can be of any race
Heterosexual contact with a person known to have, or to be at high risk for, HIV infection
Includes hemophilia, blood transfusion, and risk factor not reported or not identified
Bold text indicates EAPC statistically significant (p < 0.05)
In 2017, HIV diagnosis rates in the Deep South were highest in Georgia (30.0 per 100,000 population), Louisiana (26.1), and Florida (25.5). By race/ethnicity, 2017 rates were highest among blacks/African Americans (56.5) followed by persons of multiple races (31.7) and Hispanic/Latinos (24.4). By age, the highest diagnosis rates in the Deep South during 2017 occurred among persons aged 25–29 (48.4), followed by those aged 20–24 years (44.6) and 30–34 years (38.1). Most 2017 diagnoses in the Deep South among males were attributable to MSM contact (81%) and among females, to heterosexual contact (90%). HIV diagnosis rates in the Deep South in 2017 were highest in large central metro areas (31.4), followed by large fringe (18.2) and medium metro (17.3) areas. Combined, these three categories accounted for about 80% of diagnoses in the Deep South.
Characteristics of 2017 HIV Diagnoses by Region
Table 2 displays characteristics of 2017 HIV diagnosis rates and counts in the Deep South, Other South, and all other regions (hereinafter referred to as non-South). Rates were higher in the Deep South compared to rates in Other South and non-South regions among all races/ethnicities, with the exception of American Indian/Alaska Native populations, among whom rates were highest in non-South regions. For all age groups, rates were also higher in the Deep South than in Other South, and Other South had higher rates than non-South regions. A lower percentage of diagnoses in the Deep South were attributable to injection drug use compared to non-South regions (4.3 vs. 7.5%), and proportionally more HIV transmissions were attributable to heterosexual contact compared to non-South regions (11.7% among men and 89.7% among women in the Deep South, compared to 6.9% among men and 81.1% in non-South regions).
Table 2.
HIV diagnosis among adults and adolescents by demographic characteristics and region, 2017, United States
| Deep South |
Other South |
All other regions |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| No. | Rate | % | No. | Rate | % | No. | Rate | % | |
| Total | 16,291 | 20.7 | 42.6 | 3340 | 13.6 | 8.7 | 18,593 | 11.0 | 48.6 |
| Race/ethnicity | |||||||||
| American Indian/Alaska Native | 26 | 7.7 | 0.2 | 31 | 9.4 | 0.9 | 153 | 11.8 | 0.8 |
| Asian/Pacific Islander | 175 | 6.6 | 1.1 | 51 | 4.8 | 1.5 | 776 | 6.3 | 4.2 |
| Black/African American | 8534 | 56.5 | 52.4 | 1861 | 43.9 | 55.7 | 6130 | 43.8 | 33.0 |
| Hispanic/Latinoa | 3711 | 24.4 | 22.8 | 354 | 20.0 | 10.6 | 5537 | 19.7 | 29.8 |
| White | 3542 | 8.0 | 21.7 | 923 | 5.5 | 27.6 | 5455 | 4.9 | 29.3 |
| Multiple races | 303 | 31.7 | 1.9 | 120 | 23.6 | 3.6 | 542 | 17.6 | 2.9 |
| Age at diagnosis | |||||||||
| 13–19 | 813 | 9.4 | 5.0 | 163 | 6.2 | 4.9 | 799 | 4.4 | 4.3 |
| 20–24 | 2818 | 44.6 | 17.3 | 591 | 29.9 | 17.7 | 3025 | 22.0 | 16.3 |
| 25–29 | 3266 | 48.4 | 20.0 | 685 | 33.0 | 20.5 | 3746 | 25.8 | 20.1 |
| 30–34 | 2400 | 38.1 | 14.7 | 482 | 24.5 | 14.4 | 2740 | 20.0 | 14.7 |
| 35–39 | 1801 | 29.3 | 11.1 | 369 | 19.2 | 11.0 | 2112 | 16.1 | 11.4 |
| 40–44 | 1233 | 21.2 | 7.6 | 261 | 14.8 | 7.8 | 1499 | 12.5 | 8.1 |
| 45–49 | 1213 | 19.8 | 7.4 | 237 | 12.5 | 7.1 | 1499 | 11.6 | 8.1 |
| 50–54 | 1098 | 18.0 | 6.7 | 223 | 11.3 | 6.7 | 1341 | 10.1 | 7.2 |
| 55–59 | 806 | 13.1 | 4.9 | 143 | 7.1 | 4.3 | 926 | 6.7 | 5.0 |
| 60–64 | 467 | 8.4 | 2.9 | 97 | 5.3 | 2.9 | 515 | 4.1 | 2.8 |
| 65+ | 376 | 2.6 | 2.3 | 89 | 1.9 | 2.7 | 391 | 1.2 | 2.1 |
| Transmission category: male | |||||||||
| Male-to-male sexual contact | 10,673 | – | 82.3 | 2058 | – | 79.7 | 12,713 | – | 82.6 |
| Injection drug use | 377 | – | 2.9 | 116 | – | 4.5 | 821 | – | 5.3 |
| Male-to-male sexual contact and injection drug use | 399 | – | 3.1 | 126 | – | 4.9 | 766 | – | 5.0 |
| Heterosexual contactb | 1515 | – | 11.7 | 283 | – | 10.9 | 1059 | – | 6.9 |
| Otherc | 10 | – | 0.1 | 1 | – | 0.0 | 24 | – | 0.2 |
| Transmission category: female | |||||||||
| Injection drug use | 325 | – | 9.8 | 109 | – | 14.4 | 581 | – | 18.1 |
| Heterosexual contactb | 2975 | – | 89.7 | 644 | – | 85.1 | 2603 | – | 81.1 |
| Otherc | 16 | – | 0.5 | 4 | – | 0.5 | 27 | – | 0.8 |
| 2013 Urban–rural classification scheme for Counties | |||||||||
| Large central metro | 6955 | 31.4 | 43.5 | 1032 | 29.4 | 31.0 | 11,217 | 19.3 | 60.5 |
| Large fringe metro | 3150 | 18.2 | 19.7 | 1407 | 14.9 | 42.3 | 3209 | 7.8 | 17.3 |
| Medium metro | 3515 | 17.3 | 22.0 | 427 | 10.6 | 12.8 | 2488 | 7.7 | 13.4 |
| Small metro | 1102 | 14.8 | 6.9 | 177 | 7.4 | 5.3 | 912 | 6.1 | 4.9 |
| Micropolitan | 754 | 11.6 | 4.7 | 143 | 6.0 | 4.3 | 504 | 3.6 | 2.7 |
| Noncore | 513 | 10.5 | 3.2 | 138 | 4.9 | 4.2 | 218 | 2.7 | 1.2 |
The Deep South is defined as Alabama, Florida, Georgia, Louisiana, Mississippi, North Carolina, South Carolina, Tennessee and Texas. Other South is defined as Arkansas, Delaware, District of Columbia, Kentucky, Maryland, Oklahoma, Virginia, and West Virginia. Rates are per 100,000 population for all persons aged 13 and older. Rates are not calculated by transmission category because of the lack of denominator data
Hispanics/Latinos can be of any race
Heterosexual contact with a person known to have, or to be at high risk for, HIV infection
Includes hemophilia, blood transfusion, and risk factor not reported or not identified
By urban–rural classification, 37% of people living in more populated areas (large central and fringe metro areas combined) of the United States resided in the Deep South in 2017, while 54% of persons residing in less populated areas of the country (medium and small metro, micropolitan, and non-core areas) resided in the Deep South at diagnosis. Rates in large central metro areas of the Deep South were nearly twice as high, and those in large fringe metro and medium metro areas of the Deep South were more than double, compared to corresponding areas in non-South regions. In less populated micropolitan and noncore areas, differences were even more pronounced. In all urban/rural classification levels, diagnosis rates in the Other South region fell between those of the Deep South and non-South regions.
Discussion
Despite public health efforts, the South continues to be disproportionately affected by HIV, with a diagnosis rate 50% higher than that of any other region. These differences are primarily driven by high rates in the nine Deep South states, which account for more than 80% of HIV diagnoses in the South. Although HIV diagnosis rates are declining in the South overall, rates among Hispanics/Latinos and American Indians/Alaska Natives are increasing in the region, and rates among blacks/African Americans and whites remain higher in the South than other regions.
HIV diagnosis rates in the Deep South were highest in metropolitan areas, but differences between diagnosis rates in less populated areas were much wider when comparing the Deep South to non-South regions, with the rate in noncore areas nearly four times as high in the Deep South as in non-South regions. The number of HIV diagnoses in less populated areas (medium and small metro areas, micropolitan areas, and noncore areas combined) of the Deep South outnumbered those in less populated areas of all other regions of the country combined. Lower rates of retention in care and viral suppression have been documented among persons with HIV living in rural areas, for reasons including lack of availability of services and support and greater stigma [12]. Poor care retention can lead to poor health outcomes, high HIV prevalence, and increased HIV transmission [23]. In the Deep South, it is particularly important that HIV prevention and care efforts have adequate reach into rural areas. Structural and relational interventions (e.g. transportation, appointment reminders, peer navigators) may help address barriers related to access and stigma [24].
CDC recommends annual (or more frequent) HIV testing for some groups, including sexually active MSM at risk for HIV infection, people who inject drugs, and those with partners with HIV [25]. Those testing positive should be linked to and retained in medical care, supporting achievement of viral suppression. People with HIV who take HIV medicines as prescribed and achieve and maintain an undetectable viral load have effectively no risk of sexually transmitting HIV to their HIV-negative sexual partners [26]. Persons at high risk who test negative for HIV should be provided prevention services, including behavioral counseling and preexposure prophylaxis (PrEP).
The findings in the report are subject to the following limitations. First, diagnoses reported may not be representative of all persons with HIV because not all infected persons have been tested, tested at a time when the infection could be detected and diagnosed, or reported to the surveillance system. Second, some HIV diagnoses are reported without an identified risk; multiple imputation was applied to correct for missing risk factor information. Third, changes in HIV diagnosis rates may reflect true changes in incidence, changes in testing, diagnosis or reporting, or a combination of factors. Future analysis to estimate incidence or to examine trends in testing behaviors may provide additional insight.
Conclusion
The South continues to be disproportionately affected by new HIV diagnoses, especially the Deep South. In addition, HIV diagnoses in the Deep South are increasing among Hispanic/Latinos, American Indians/Alaska Natives, MSM, and persons aged 25–34 years. Prevention efforts are needed to continue addressing persistent disparities in HIV diagnoses among these populations living in the Deep South. It is important that HIV prevention and care programs ensure adequate reach into rural areas of the Deep South and work to reach people where they are with interventions that address specific needs related to access and stigma (e.g. transportation, housing, appointment reminders, peer navigators). Further work to examine trends more closely by demographic groups (for instance, young MSM by race/ethnicity and geographic area) may help to identify additional specific areas of need.
Acknowledgements
We would like to acknowledge Baohua Wu for his analytic assistance and thoughtful review. We also thank the local, tribal, and state health departments.
Footnotes
Publisher's Disclaimer: Disclaimer The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Conflict of interest The authors declare that they have no conflict of interest.
References
- 1.Hall HI, Song R, Tang T, An Q, Prejean J, Dietz P, et al. HIV trends in the United States: diagnoses and estimated incidence. JMIR Public Health Surveill. 2017;3(1):e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Reif S, Safley D, McAllaster C, Wilson E, Whetten K. State of HIV in the US deep south. J Community Health. 2017;42(5):844–53. [DOI] [PubMed] [Google Scholar]
- 3.Gray SC, Massaro T, Chen I, Edholm CJ, Grotheer R, Zheng Y, et al. A county-level analysis of persons living with HIV in the southern United States. AIDS Care. 2016;28(2):266–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Reif S, Pence BW, Hall I, Hu X, Whetten K, Wilson E. HIV diagnoses, prevalence and outcomes in nine southern states. J Community Health. 2015;40(4):642–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Prejean J, Tang T, Hall HI. HIV diagnoses and prevalence in the southern region of the United States, 2007–2010. J Community Health. 2013;38(3):414–26. [DOI] [PubMed] [Google Scholar]
- 6.O’Leary A, Broadwell SD, Yao P, Hasin D. Major depression, alcohol and drug use disorders do not appear to account for the sexually transmitted disease and HIV epidemics in the southern United States. Sex Transm Dis. 2006;33(7 Suppl):S70–7. [DOI] [PubMed] [Google Scholar]
- 7.Rebeiro PF, Gange SJ, Horberg MA, Abraham AG, Napravnik S, Samji H, et al. Geographic variations in retention in care among HIV-infected adults in the United States. PLoS ONE. 2016;11(1):e0146119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Reif S, Mugavero M, Raper J, Thielman N, Leserman J, Whetten K, et al. Highly stressed: stressful and traumatic experiences among individuals with HIV/AIDS in the deep south. AIDS Care. 2011;23(2):152–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.National HIV/AIDS strategy for the United States: Updated to 2020. Washington, DC: The White House; 2015. [Google Scholar]
- 10.Breskin A, Adimora AA, Westreich D. Women and HIV in the United States. PLoS ONE. 2017;12(2):e0172367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Reif SS, Whetten K, Wilson ER, McAllaster C, Pence BW, Legrand S, Gong W. HIV/AIDS in the Southern USA: a disproportionate epidemic. AIDS Care. 2014;26(3):351–9. [DOI] [PubMed] [Google Scholar]
- 12.Nelson JA, Kinder A, Johnson AS, Hall HI, Hu X, Sweet D, et al. Differences in selected HIV care continuum outcomes among people residing in rural, urban, and metropolitan areas-28 US jurisdictions. J Rural Health. 2018;34(1):63–70. [DOI] [PubMed] [Google Scholar]
- 13.Kramer MR, Black NC, Matthews SA, James SA. The legacy of slavery and contemporary declines in heart disease mortality in the U.S. South. SSM Popul Health. 2017;3:609–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Office of Management and Budget. Revisions to the standards for the classification of federal data on race and ethnicity. Federal Regist. 1997;62:58782–90. [Google Scholar]
- 15.Centers for Disease Control and Prevention. Interpreting race and ethnicity in cancer data 2018. https://www.cdc.gov/cancer/uscs/technical_notes/interpreting/race.htm. Accessed 15th Oct 2018.
- 16.Harrison KM, Kajese T, Hall HI, Song R. Risk factor redistribution of the national HIV/AIDS surveillance data: an alternative approach. Public Health Rep. 2008;123(5):618–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rubin DB. Multiple imputation for nonresponse in surveys. New York: Wiley; 1987. 10.1002/9780470316696. [DOI] [Google Scholar]
- 18.U.S. Census Bureau. Census regions and divisions of the United States. https://www2.census.gov/geo/pdfs/maps-data/maps/reference/us_regdiv.pdf. Accessed 14th Oct 2018.
- 19.National Center for Health Statistics, Centers for Disease Control and Prevention. NCHS urban-rural classification scheme for counties 2017. https://www.cdc.gov/nchs/data_access/urban_rural.htm. Accessed 14th Oct 2018.
- 20.National Center for Health Statistics, Centers for Disease Control and Prevention. 2013 NCHS urban-rural classification scheme for counties. 2017. https://www.cdc.gov/nchs/data_access/urban_rural.htm. Accessed 14th Oct 2018.
- 21.Fay MP, Tiwari RC, Feuer EJ, Zou Z. Estimating average annual percent change for disease rates without assuming constant change. Biometrics. 2006;62(3):847–54. [DOI] [PubMed] [Google Scholar]
- 22.Clegg LX, Hankey BF, Tiwari R, Feuer EJ, Edwards BK. Estimating average annual per cent change in trend analysis. Stat Med. 2009;28(29):3670–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Li Z, Purcell DW, Sansom SL, Hayes D, Hall HI. Vital signs: HIV transmission along the continuum of care—United States, 2016. Morb Mortal Wkly Rep. 2019;68(11):267–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Taylor BS, Fornos L, Tarbutton J, Munoz J, Saber JA, Bullock D, et al. Improving HIV care engagement in the south from the patient and provider perspective: the role of stigma, social support, and shared decision making. AIDS Patient Care STDS. 2018;32(9):368–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dailey AF, Hoots BE, Hall HI, Song R, Hayes D, Fulton P Jr, et al. Vital signs: human immunodeficiency virus testing and diagnosis delays—United States. MMWR Morb Mortal Wkly Rep. 2017;66(47):1300–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Centers for Disease Control and Prevention. Evidence of HIV treatment and viral suppression in preventing the sexual transmission of HIV. 2018. https://www.cdc.gov/hiv/pdf/risk/art/cdc-hiv-art-viral-suppression.pdf. Accessed 8th Nov 2018.