Abstract
Veterans Treatment Courts (VTCs) grew exponentially in the last decade with more than 550 courts, dockets and tracks operating in the U.S. Eligibility criteria and operating practices of VTCs vary widely. Existing logic models guide the activities of these courts, but do not explicitly address the distinct missions and priorities of different agencies that support VTCs. To facilitate communication and research to address this gap, we propose a logic model of the Department of Veterans Affairs’ (VA) role in VTCs. To construct the VA-VTC logic model, we adapted an existing logic model and held expert panels with VA staff, clinical leaders and researchers to discuss and refine the model. The VA-VTC logic model is a novel contribution to current thinking about VTCs and clarifies the potential resources, activities, outputs, outcomes and population impacts that are under the purview of the VA. Explicitly recognizing the VA as a separate partner in VTCs, this logic model can be a tool for communication with criminal justice agencies to facilitate broader discussions about the mechanisms driving VTC outcomes. This model can also be continuously updated as we learn from research and evaluation efforts about VTCs, ultimate improving the effectiveness of the VA’s role in these courts.
Keywords: Veterans, treatment courts, logic model
Introduction
Background
Since the establishment of the first two Veterans Treatment Courts (VTCs) in Anchorage, AK, in 2004 and in Buffalo, NY in 2008, these courts have grown exponentially with 551 veteran-related courts, dockets and tracks now operating in the U.S. (U.S. Department of Veterans Affairs 2018c). The VTC model is a hybrid of drug and mental health courts with 10 key components developed by the National Association of Drug Court Professionals (NADCP) and its subsidiary, Justice for Vets (Russell 2009). These components include practices such as integration of mental health and addiction treatment with justice system processing and abstinence monitoring through alcohol and drug testing. Elements of VTCs unique to veterans include peer mentoring by veteran volunteers and partnership with the U.S. Department of Veterans Affairs (VA). Partnership with the VA provides linkage to health care treatment and psychosocial support, such as housing and employment benefits. The eligibility criteria and practices of VTCs vary widely (Timko et al. 2017). For example, some courts only accept veterans with mental health conditions related to military service, combat veterans, or veterans eligible for VA services. VTCs operate independently from the VA at the county, regional or federal level; decisions made about court entry criteria and requirements for participation are at the discretion of the court.
The VA and the Veterans Justice Outreach Program
Justice-involved veterans are about 3% of the overall veteran population in the U.S. (Blue-Howells et al. 2013) Although VTCs are independent entities, a primary partner in virtually all VTCs is the VA, which is the largest integrated healthcare system in the U.S. Each year, a total of over 6 million patients are served at 172 medical centers and 1,062 community-based outreach clinics in the Veterans Health Administration (VHA) system. There are two VA programs dedicated to justice-involved veterans: The Health Care for Reentry Veterans program, which primarily serves veterans exiting state and federal prisons, and the Veterans Justice Outreach program, which primarily serves veterans who are encountered by law enforcement, in the court process, and/or exiting jails (Blue-Howells et al. 2013). The mission of VA’s Veterans Justice Programs is to identify, conduct outreach to, and connect justice-involved veterans with VA services with the vision that “Every justice-involved Veteran will have access to the care, services and other benefits to help him or her maximize their potential for success and stability in the community, including by avoiding homelessness and ending their involvement in the justice system” (p. 5; U.S. Department of Veterans Affairs 2017).
In VTCs, the VA is most frequently represented by a Veterans Justice Outreach (VJO) Specialist who typically functions as a member of the court team and liaison between the court and the VA. VJO Specialist’s roles can include providing psychosocial assessments, continuous quality improvement activities, evaluation/consultation, placement services, and referral and linkage to various community agencies for veterans who releasing from jails and/or being monitored by the courts, particularly but not limited to specialty treatment courts. The VJO Specialist’s role in court often includes reporting to the collaborative court team on veterans’ engagement with VA treatment during their period of court supervision. The VA also serves an important role in providing the majority of treatment services to veterans in VTCs. Over 90% of veterans in VTCs eligible for VA care receive some VA treatment services while under court supervision – most commonly mental health or substance use disorder treatment (Finlay 2016). However, the VA is not authorized to provide direct treatment services to veterans while incarcerated or to veterans who are ineligible for VA care. As estimated 23% of incarcerated veterans have a military discharge status that prevents them from obtaining VA benefits (Bronson et al. 2015). Although many courts can refer veterans to community health care services, there are some courts that only accept veterans eligible for and participating in VA healthcare. VTCs can also provide linkage to VA supported housing programs, therapeutic employment opportunities, and community agencies that provide additional financial support or assistance in filing disability benefits (e.g., through county Veterans Service Officers).
While the VHA is an essential partner in supporting VTCs, its staff and priorities are aligned with the broader VA system (U.S. Department of Veterans Affairs 2017). Adopted in 2011, the universal core values of the VA are summarized by the I CARE acronym, which stands for Integrity, Commitment, Advocacy, Respect, and Excellence. The Veterans Justice Programs are aligned with the I CARE values with the aim of realizing VHA’s commitment to “defining excellence in healthcare” (p. 4; U.S. Department of Veterans Affairs 2017). VA priorities may be in conflict, at times, with those of other agencies that partner in VTCs. For example, the Advocacy value is veteran-centric, emphasizing “identifying, fully considering, and appropriately advancing the interests of veterans and other beneficiaries” (p.3; U.S. Department of Veterans Affairs 2017). In VTCs, the VJO Specialists focus their advocacy on veterans’ access to services and aligning treatment recommendations with veterans’ treatment needs. In contrast, the VTCs may focus on a particular legal outcome or apply universal – rather than individually-tailored – treatment mandates for all veterans. For example, in some cases the VA’s VJO Specialists and VA providers may recommend outpatient substance use disorder care as the optimal evidence-based treatment for some patients, whereas some courts may mandate residential treatment in lieu of incarceration. Describing the VA’s role in VTCs and how these processes are aligned with the broader VA system may help to clarify communication among all VTC partners.
Effectiveness of Veterans Treatment Courts
Although research on the effectiveness of drug courts exists (Marlowe, Hardin, and Fox 2016), limited research to date support the effectiveness of VTCs. Studies have primarily focused on summary characteristics of courts and participants (Baldwin 2017, Timko et al. 2017), legal perspectives on the rationale for or against VTCs (Cartwright 2011, Cavanaugh 2010), and describing aspects of the courts or peer mentoring programs (Ahlin and Douds 2016, Baldwin and Rukus 2015). A few studies have examined outcomes such as recidivism, changes in mental health symptoms, substance use measured by self-report and drug testing, family functioning, and psychosocial outcomes such as employment and housing (Hartley and Baldwin 2016, Johnson et al. 2017, Johnson et al. 2015, Knudsen and Wingenfeld 2016, McCormick-Goodhart 2013, Russell 2009, Slattery et al. 2013, Smith 2012, Tsai et al. 2018, Tsai et al. 2017). However, these studies are limited by small sample sizes, exclusion or inclusion criteria for court entry that could introduce bias, follow-up times that end at the conclusion of court involvement or shortly thereafter, and/or primary reliance on court participants’ self-report or court staff reports rather than clinical treatment records (e.g., clinician diagnoses, clinical outpatient visits from electronic health records) or criminal justice data (e.g., arrest records, jail stays). Privacy concerns and other factors surrounding the sharing and matching of data from courts, correctional systems, community health systems, and VA health systems slow the conduct of careful research studies in this area. While research and evaluation efforts are in process that would provide clear direction to evidence-based practices in these courts, VTCs may benefit from logic models as tools to guide their strategic program planning and define the outcomes they anticipate among program participants. These logic models can then be adjusted to reflect research and evaluation results as they accumulate.
Logic Models
Logic models are aimed at connecting practices, products and outcomes with the theoretical assumptions underlying a program (W. K. Kellogg Foundation 2004). Mapping the available resources, planned activities, and anticipated results in a succinct and visual display allows stakeholders to communicate about their programs and provide a guide for research and evaluation efforts. The National Institute of Justice has developed a logic model for drug courts (National Institute of Justice 2018). The logic model of drug courts depicts all elements of the drug court in one model, including the criminal justice aspects (e.g., judicial interaction, recidivism), treatment and health aspects (e.g., alcohol and drug treatment services), and community aspects (e.g., public resources, employment). A logic model that combines criminal justice, healthcare and community systems may be appropriate for drug courts where aspects of the court program are under the control of and aligned with the mission of the court. For example, a judge may mandate treatment which is provided by a community healthcare agency that is contracted by the drug court. Community-based clinical staff who assess court participants and make treatment recommendations may be employees of the court or of the contracted community agency.
A logic model for VTCs has also been created, which combines the resources, activities, and outputs of criminal justice agencies, community programs, and the VA (Blackburn and Cheesman 2015). For example, under resources/inputs, the judge representing the court, a VJO Specialist representing the VA, and treatment provider representing the VA and/or community health care, are all listed as part of the VTC team along with other court team members. For processes/activities, the VTC model lists legal eligibility, which is a court activity; treatment interventions, which are either VA and/or community activities; and regular meetings with peer mentors, which may be a court or community activity. This model also includes short-term outcomes and long-term impacts that combine expectations from criminal justice, the VA and community agencies. The Blackburn and Cheesman VTC logic model, however, has an important limitation: it does not clarify that the multiple agencies functioning with the VTC context have distinct missions, visions, and priorities. Without clarifying the different priorities of and activities provided by each agency, there can be conflict or miscommunication in expectations. For VTCs to optimize their effectiveness, a mutually agreed upon goal and a clear delineation of each agency’s distinct contribution to the courts is needed.
Current Study
An important question not yet widely discussed in the literature is how the VA, the criminal justice system, and the community care system can partner together in VTCs, despite their different priorities and resources, to most effectively support justice-involved veterans. This paper proposes a logic model of the VA’s role in VTCs that aligns with the mission and priorities of the VA’s Veterans Justice Programs and the broader VA. The proposed model in the current study cannot be used to examine the overall effectiveness of VTCs because an overall logic model would require information and elements from non-VA partners. However, drawing from existing logic models and expert perspectives, this VA-facing logic model for VTCs is meant to serve as a practical tool for VA practitioners to use for program planning and implementation, to communicate with their criminal justice and community partners and with justice-involved veterans about the rationale for and functions of the VA’s role in VTCs, and to guide evaluation and research efforts that examine the impact of VA resources and activities on VA care and health outcomes among VTC participants. The methods section describes the formation of this logic model. The results section presents the logic model elements and explanations of each aspect of the model. The discussion section examines the unique contribution of this logic model to the literature and the limitations of the model.
Methods
The VA-VTC logic model was developed over a one-year period (July 2017 to July 2018) as part of a larger VA-funded project focused on evaluating healthcare outcomes of veterans’ participation in VTCs. In July 2017, the lead author reviewed the research literature on VTCs. Drawing from an extant VTC logic model (Blackburn and Cheesman 2015) and other court-specific logic models, the limited literature on outcomes among VTC participants, the broader specialty court literature (National Institute of Justice 2018), a preliminary VA-VTC logic model was developed. Aspects of Blackburn and Cheesman’s existing logic model that were specific to the VA (e.g., staff, resources, activities) were included, and additional VA resources and activities that are measurable with VA data sources were added to the model.
A series of expert panels with VJO Specialists was organized to seek expert input on positive outcomes that were expected among VTC participants. Panels of 10–12 Specialists each met twice in the fall of 2017 (September through November 2017). In total, 37 VJO Specialists participated in the panels. During the first panel call, a moderated discussion of important outcomes that should be assessed using VA data sources was held using semi-structured questions and notes were taken. During the second call, the preliminary logic model, with refinements developed based on the first panel calls, was presented and VJO Specialists offered their feedback on adding or removing model elements. Discussions about this VTC model for VA-facing elements centered around VJO Specialist and VA treatment provider processes and expected outcomes and population impacts from the VA’s role in VTCs. An additional expert panel with researchers, clinical staff, and operational leaders was held and feedback from that session was incorporated into the logic model. Development of the logic model was based on reviewing the literature and consulting experts; therefore, we did not require Institutional Review Board approval.
Results
The VA-VTC logic model (Figure 1) posits that the VA’s role in VTCs is limited to the resources and activities that are directly related to VA services, and therefore the outcomes and population impacts are aligned with the health and healthcare aspects of VTCs. The various components of the logic model are described below.
Figure 1.
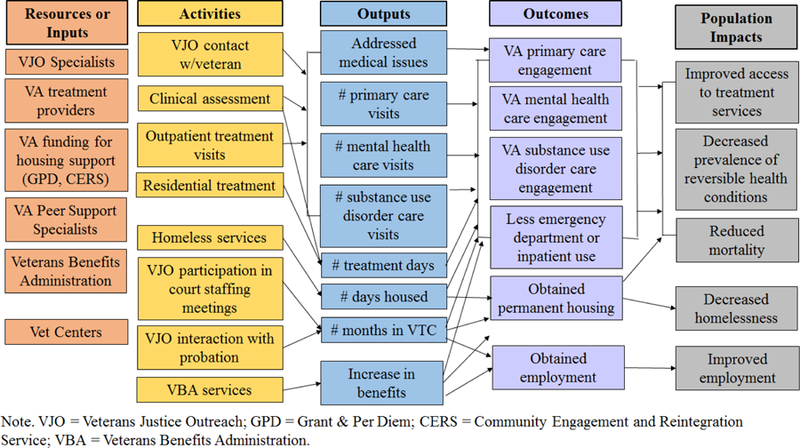
Logic Model of VA’s Role in Veterans Treatment Courts.
Resources/inputs
The VA resources that are available to VTC participants include staff, financial, and organizational inputs. The VJO Specialists who staff and support the courts are the most visible VA resource in the courtroom, but VTCs also draw heavily on treatment providers at VHA facilities and VHA Peer Support Specialists to meet the treatment and psychosocial needs of veterans in VTCs. Financial resources that are provided to veterans in VTCs may include compensation for service-connected disabilities through the Veterans Benefits Administration (VBA) , funding for education or vocational training (e.g., under the GI Bill), Supportive Services for Veteran Families (SSVF), which provides services to very low-income veteran families to support their transition to permanent housing, housing vouchers through the Housing and Urban Development Veterans Affairs Supportive Housing (HUD-VASH) program, and/or home loans (U.S. Department of Veterans Affairs 2018a, b). The VBA is a branch of the Department of Veterans Affairs separate from VHA, that primarily administers financial and other benefit support to veterans. Programs under VBA that veterans and family members can access include veterans’ compensation, veterans’ pension, survivors’ benefits, vocational rehabilitation and employment assistance, educational assistance, home lone guaranties, and life insurance. In instances when a veteran has been discharged from the military with other than honorable or bad conduct discharges, VBA makes the determination regarding whether a veteran may be eligible for VHA services.
Vet Centers, which are organizationally aligned under VHA but function as a separate entity, are available to an array of veterans, including combat veterans, veterans with post-traumatic stress disorder or military sexual trauma, and veterans with other than honorable discharge from the military. Vet Centers provide a number of treatment services, including family and couples therapy. Some services offered at Vet Centers and VHA facilities are similar. For example, there has been a surge in family and couples therapy offered at VHA facilities with the influx of newer veterans to the VHA. Data from Vet Centers cannot be linked with VA health or healthcare data, limiting statements we can make about the services provided.
The integrated health care system of the VA serves as an organizational resource. Veterans can access resources at any VA and veterans can even to travel to VA facilities in other states to access specific treatment programs (e.g., residential substance use or trauma disorder treatment) (U.S. Department of Veterans Affairs 2019). Notably, all VA staff and related programs must adhere to VA regulations and standards, which may conflict with the interests or preferences of other agencies involved in VTCs. For example, occasionally a judge will mandate a veteran to a year-long residential substance use disorder treatment program; however, residential program length within the VA is based on individual clinical need, not judicial mandate, and linked to the goals and objectives of the rehabilitation plan (Department of Veterans Affairs 2010).
Activities
Multiple activities occur as part of the VA’s role in VTCs. The VJO Specialist’s primary role is to serve as a liaison between the court and the VA on behalf of veterans in VTCs. They conduct assessments of veterans to determine needed treatment services and resources, help facilitate veterans’ access to VA services, and connect them with VA and community services depending on the needs and preferences of the veteran (Department of Veterans Affairs 2017). Specialists attend court staff meetings to update the court on the veteran’s progress and advocate for the appropriate treatment services for veterans. In this function, VJO Specialists also regularly interact with probation officers, who are the primary supervisors of VTC participants. The VJO Specialist role requires extensive electronic documentation, such as entering initial assessments/updates from court and other contact with the veteran and reviewing treatment visits and progress prior to court appearances. The activities of VJO Specialists vary by VTC and VA facility. Some VTCs have multiple VJO Specialists with their time primarily dedicated to serving the court. Other VJO Specialists cover extensive geographic areas, handle multiple courts and jails, and have little additional support to meet the extensive needs of justice-involved veterans or to cultivate the relationships that ensure veterans are connecting to the care they require. The proposed logic model does not capture the nuances of each VJO Specialist’s experience in the courts.
Use of VA treatment services is an essential part of VA’s role in VTCs. Most VA-eligible veterans in VTCs use VA outpatient treatment for mental health and/or substance use disorder care and a smaller number access residential treatment services and inpatient care (Finlay 2016). Veterans in VTCs may also access primary care, specialty clinics such as infectious disease care, and other healthcare services such as surgical care. Additional services provided by the VA include homeless services, and vocational employment training (i.e., Compensated Work Therapy). VJO Specialists may assist in scheduling veterans for treatment visits or helping them with paperwork, but the majority of healthcare and psychosocial services are provided by other VA clinicians and staff.
VBA services are a VA activity, though non-VA agencies or people may be involved in supporting a veteran’s application for VBA benefits. VJO Specialists can assist veterans in identifying resources to apply for or upgrade their benefits and navigating other complexities related to their VA benefits; this is often done in partnership with VBA outreach staff at the appropriate VA Regional Office. Outside the VA, Veterans Service Officers may also interact with veterans to help them apply for benefits or file appeals. Veterans Service Officers are primarily employed by state Department of Veterans Affairs or Veteran Service Organizations (e.g., American Legion). Although VA accredits individuals to assist veterans with benefits claims, data on the services they provide are not available, as they are not part of the VA. Legal clinics and providers may also assist veterans in seeking benefit upgrades or appeals. Though the VA cannot provide legal services to veterans, there are more than 170 legal clinics hosted on VA campuses that can help address the civil legal needs, and in some cases other legal needs, of veterans. Legal clinic data that can be linked to VA health and healthcare data is not currently available. Ultimately, any decisions about VA benefits claims or appeals are made by the appropriate VA Regional Office, and/or the VA benefits appellate structure, which includes the Board of Veterans Appeals.
Outputs
The direct results of the VA activities can vary by veteran depending on their specific health care and psychosocial needs. Treatment services can be accounted for by number of outpatient visits, number of residential days, or use of medications such as pharmacotherapy for opioid use disorder (e.g., methadone). For veterans who are homeless or at-risk of homelessness, the output would be number of days in stable housing and for veterans who were unemployed and looking for work, their number of days employed. For veterans with medical conditions, the proportion who address their condition (e.g., hepatitis C pharmacotherapy is initiated, cancer is diagnosed and treatment started) would be a positive output. Other outputs include a change in VA benefits and participation in VTCs, such as number of months enrolled and graduation rates.
Outcomes
Outcomes that are the result of VA’s resources and activities in VTCs relate to healthcare and psychosocial outcomes. The expert panels indicated that a long-term positive outcome would be that a veteran continued to be connected to VA services, such as regular primary care use, and use of mental health or substance use disorder treatment/aftercare for those who needed such services. Regular use of primary care and other outpatient services make it possible to address health conditions at an early state, averting emergency department or inpatient care. Finally, positive psychosocial outcomes included obtaining permanent housing and employment.
Population Impacts
There are a number of expected population-level impacts in health that could be attributed to participation in VTCs. Improved access to treatment services is one expected impact of the outreach and referral services provided by VJO Specialists. For health conditions, there is an expected decrease in prevalence of preventable or reversible medical, mental health and substance use disorder conditions observed among justice-involved veterans as a result of the treatment services received. Mortality rates are anticipated to improve among veterans who went through VTCs with VA support. We also expect decreased rates of homelessness and improved employment rates at the population level.
Discussion
Value and Utility of the Logic Model
The VA-VTC logic model is a novel iteration in the development of logic models for VTCs because it clarifies the VA’s distinct role in these courts and the anticipated outcomes and population impacts specific to VA activities. Explicitly recognizing that the VA is a separate agency and actor partnering in in VTCs, this model lays out what the VA can contribute to these courts. Separating out the VA role is a critical next step in defining VTC logic models that reflect the reality of VTC programming. The model draws from existing literature (National Institute of Justice 2018, Blackburn and Cheesman 2015), stakeholder experiences in the field, and expert perspectives. This process began as conversations to inform analysis of outcomes among VTC participants, but grew into a framework relevant to stakeholders, including policymakers, clinical and court staff, and researchers. The VA-VTC logic model can be used to shape the VA’s role in the practice of VTCs, to evaluate the implementation and effectiveness of VA resources and activities, and as a tool to communicate about the expectations of the VA’s role and veterans’ experiences in these courts.
First, this logic model can be used when planning new courts. VA staff can use the model to explain the services provided by VA and the constraints of their roles in the courts. Non-VA stakeholders can develop their court policies and practices to accommodate VA standards and policies. The logic model also highlights what is not under the VA purview. For example, re-arrest and criminal recidivism are important outcomes for VTCs, but are not health outcomes; it is best understood as the product of multiple factors operating in a VTC, not ones that can be attributed to VA activities primarily. There is much more that goes into developing a VTC than what is described in this logic model, but we aim for the VA-VTC logic model to be one tool among many that is useful in conversations about VTCs.
Second, this model can be used in existing VTCs to improve program implementation (W. K. Kellogg Foundation 2004). Local resources and conditions vary for each VTC and each VA facility. This logic model can function as a starting point for conversations about the resources that can be provided and the monitoring that can occur by VA staff to ensure the VA is implementing their services as intended by the VA. This model is also congruent with Goal 5 of the Veterans Justice Programs Strategic Goals, Objectives, Actions and Measures (2017–2021) – Evaluate the effectiveness of the Veterans Justice Programs (U.S. Department of Veterans Affairs 2017). Close attention to VA activities will inform VA staff and leaders about the effects of their services and contribute to learning about what does and does not work, allowing for decisions about the effectiveness of VA’s role in VTCs. In addition to improving the VA’s activities, investigation of program implementation will also inform updates to the logic model.
Third, in both new and existing courts, use of the logic model will facilitate communication among stakeholders, including VA staff and leaders, court and other criminal justice staff, community partners, program evaluators, and funders. An explicit description of the VA’s role in these courts will help promote a shared understanding of what the VA can and cannot do to support and sustain these courts’ missions. VA’s court, criminal justice partners, and community partners may similarly decide to modify existing VTC logic models to clarify their resources, activities, outcomes and population impacts. By starting from logic models that map to the missions and priorities of each agency, we can then come together and build a meta-VTC logic model that incorporates each agency and optimizes VTCs for veterans. A preliminary hypothetical meta-VTC logic model that draws upon our VA-VTC model for the VA component and draws upon the literature for the court and community components (Blackburn and Cheesman 2015, National Institute of Justice 2018) is displayed in the supplemental appendix, but participation from key stakeholders in the court and community systems would be required to appropriately inform such a model.
Finally, this logic model can be used to guide evaluation and research efforts focused on VTCs. There are many challenges to conducting evaluation and research in VTCs, such as limitations on data sharing across agencies, a lack of clear documentation on program implementation, and different definitions for measuring aspects of the program. This model can be used as a starting point to describe the VA aspects of the VTC program and measures we plan to define and document systematically throughout the VA healthcare system. For example, metrics for outputs such as number of treatment visits and number of days in stable housing can be defined and distributed to court and community partners, which will allow us to consistently document and then systematically evaluate the impact of treatment visits on veterans’ long-term health and healthcare.
Considered but Excluded Aspects of the Logic Model
We aimed to limit this logic model to resources, activities, outputs, and outcomes that are under the purview of the VA and measurable by VA data sources. We considered existing logic models (National Institute of Justice 2018, Blackburn and Cheesman 2015), but excluded aspects of those models that were provided by or monitored by criminal justice and community agencies. From resources/inputs, we excluded partners who are members of other organizations, such as judges and court staff, probation officers, lawyers, and law enforcement. Peer mentors were excluded because the mentorship programs are organized by entities outside the VA. Funding provided by organizations other than the VA were also excluded. Activities that were not part of the VA’s role were excluded, including non-VA services, legal eligibility determination, community supervision, and meetings with a peer mentor. Random drug testing was also excluded because the requirements for random drug testing in courts were not congruent with VA’s drug screening policies and practice. Outputs that were specifically related to criminal justice, such as jail stays or probation contacts, were excluded from the model. Outcomes and population impacts were limited to outcomes that are linked to VA activities and measurable using currently available VA data sources.
Although recidivism was mentioned by VJO Specialists as an important outcome of the courts, the VA does not currently have access to recidivism data that would allow VA to measure this outcome. Similarly, treatment services that are not provided or purchased by the VA are not systematically tracked by or available in VA databases. Improvement in mental health and substance use disorder symptoms was discussed as an important outcome of VTCs, but current centralized VA data do not allow measurement of changes in symptoms. This VA-VTC logic model is reflective of the limitations of the current resources, activities, and data of the VA, but should evolve as the courts, the VA’s role in the courts, and data access and sharing expand.
Future Research and Evaluation
Moving forward with this logic model, research and evaluation studies are needed. The authors are currently examining outcomes among VTC participants with a four-year follow-up period using VA data. We are able to examine some aspects of the logic model, including outputs such as number of treatment visits and number of months in a VTC, and outcomes such as post-VTC mental health and substance use disorder treatment use at the VA. However, other outcomes and population impacts such as improved health status and decreased homelessness or unemployment are more difficult to estimate from VA data and would need to be collected from veterans who did and did not participate in VTCs.
As research and evaluation studies are conducted, methods for feeding the results back into the logic model and, more importantly, into VTCs are required. Lessons from the learning health system model (Institute of Medicine 2012) may provide insight into how to incorporate feedback into VTCs. Some VTCs may already have logic models developed for their courts, but how these models are used and what processes, if any, are in place to update the models with new information is unknown. Logic models are designed to be dynamic and responsive to programs they represent (W. K. Kellogg Foundation 2004). Therefore, a systematic process for updating the VA-VTC logic model within the VA would promote the spread of best practices.
As research accumulates and the model is revised, determining the core elements of the model that must exist in all VTCs and what aspects can be modified for local VA and non-VA resources and conditions will help ensure the VA’s roles and responsibilities in VTCs are effective. Documenting the modifications will allow us to examine progress in real-world settings and the effect such modifications have on the impact of these courts. VTCs are highly complex programs and there may be any number of modifications and adaptations to the model. As the logic model and VTCs continue to evolve, feedback on what does and does not work from multiple stakeholders will allow us to continue to shape this model to be maximally usable to the field.
Limitations
There are several limitations to the VA-VTC logic model. First, most elements of the model are untested. Although there have been some studies examining summary characteristics of VTCs, court processes, or outcomes among VTC participants, there are no studies with long-term follow-up. Other aspects of the model, such as the processes of VJO Specialists, VA Peer Support Specialists, or Veterans Benefits support in VTCs, the process of linkage and referral, and population impacts should also be examined along with veteran outcomes.
Second, this logic model represents the VA’s role in VTC program activities and outcomes, but does not include a theory of change. Expanding this model to include the theoretical causal pathways and scientific evidence in support of these causal pathways would improve the value of this model. Program evaluation and research efforts are needed to inform the model and ensure VTCs are having their intended effect without unintended consequences.
Third, our model does not include specifications for any of the included elements, such as definitions of clinical assessment or electronic documentation activities or specifications for outcomes of obtaining permanent housing or employment, and does not specify the direct link between each element. By itself, this logic model cannot be used for program planning or evaluation. Expanding this model to explain how the program works with input from stakeholders, testing elements of the model, and feeding this information back into future iterations of the model is needed to develop a robust logic model that serves stakeholders, similar to methods that are used to develop quality measures in health care (e.g., Harris et al. 2016).
Fourth, the logic model does not include the broader social and political milieu in which VTCs exist. Healthcare is only one piece of the puzzle in working with justice-involved veterans. Broader social forces also influence criminal justice involvement, such as criminalization of homelessness, law or policies that disproportionately target certain neighborhoods or communities, and economic forces that limit legal job prospects. Explicitly recognizing the broader context in logic models of VTCs provides a more complete picture of the challenges faced by justice-involved veterans and allows users of the logic model to assess whether the model could be adopted in their VTC. For example, a VTC located in a community with strict laws related to homelessness and a shortage of housing may need to adapt their logic model to realistically anticipate that recidivism may be higher due to persistent homelessness. We did not include the broader milieu in this version of the VA-VTC logic model because many of these forces are not addressable with VA services, but we plan to include the broader context as we continue to revise and expand the model.
Finally, we do not include details on the many challenges faced by veterans involved in VTCs or examine the efforts and processes required to create a court. Justice-involved veterans may be engaged in other court proceedings or face difficulties such as paying for child support or other family issues. Many of these challenges are beyond the scope of the VA’s role in these courts, particularly civil legal issues that are outside the VJO Specialists’ focus on criminal legal issues. Services for justice-involved veterans who are not eligible for VA care is beyond the scope of this logic model. As these courts continue to expand, studies that examine challenges experienced by justice-involved veterans, both eligible and ineligible for VA care, will inform the VA as well as the research field more broadly. Creating a VTC requires numerous other processes and coordination between the VA, criminal justice agencies, and community agencies. The focus of this study is solely on the VA’s role in these courts and we are therefore limited in describing the efforts of non-VA agencies in court development. Future studies that comprehensively describe the efforts of non-VA partners in the development of these courts would be beneficial to understanding the roles and responsibilities of each agency and aid in communication among all partners.
Conclusions
The VA-VTC logic model is a novel contribution to current thinking about VTCs that explicitly recognizes the VA as a separate agency partnering in these courts. As the number of VTCs continues to grow, this logic model can be used as a tool in developing new courts and communicating the priorities and expectations of the VA’s role in VTCs. Although there is a dearth of research on the effectiveness of VTCs, this model can be used to guide future studies on VA’s role in these courts and should evolve as evidence accumulates and consensus is built among all partners who support VTCs.
Supplementary Material
Value Statement.
This study proposes a logic model of the Department of Veterans Affairs’ (VA) role in Veterans Treatment Courts (VTCs). The model clarifies the resources, activities, outputs and outcomes of services provided to veterans eligible for VA healthcare. The VA-VTC logic model is a tool for VA staff to communicate with criminal justice and community partners about their role in these treatment courts and can guide evaluation efforts.
Acknowledgments
This work was funded in part by the Department of Veterans Affairs (VA) Health Services Research & Development (HSR&D) supplemental award to Dr. Finlay (CIN 14–238; PI: Dr. Steven Asch). Dr. Finlay was supported by a VA HSR&D Career Development Award (CDA 13–279). Dr. Harris was funded as a VA HSR&D Research Career Scientist (RCS 14–232). The views expressed in this article are those of the authors and do not necessarily reflect the position nor policy of the Department of Veterans Affairs (VA) or the United States government. The VA had no role in the study design; in the collection, analysis and interpretation of data; in the writing of the report; or in the decision to submit the paper for publication.
Author Bios
Andrea Finlay, PhD, is a Research Health Scientist at the VA Health Services Research & Development Center for Innovation to Implementation, VA Palo Alto Health Care System, and an Affiliated Researcher with the VA National Center on Homelessness Among Veterans. Her research focuses on identifying and addressing gaps in access and engagement in health care among justice-involved Veterans.
Sean Clark, JD, is the National Coordinator for the Veterans Justice Outreach program at the U.S. Department of Veterans Affairs. Veterans Justice Outreach is a program that provides outreach and linkage to VA services for veterans in contact with law enforcement, jails and courts. Mr. Clark earned his J.D. from William & Mary School of Law.
Jessica Blue-Howells, MSW, is the National Coordinator for the Health Care for Reentry Veterans program and the National Coordinator of Project CHALENG – Community Homelessness Assessment, Local Education and Networking Groups. Ms. Blue-Howells serves as the operational partner for research focused on Veterans’ access to health services and implementation of peer initiatives.
Sherri Claudio, MSW, is a Homeless Program Supervisor and former Veterans Justice Outreach Specialist at the Orlando VA Medical Center.
Matthew Stimmel, PhD, is a Veterans Justice Outreach Specialist at the VA Palo Alto Health Care System. His research focuses on trauma and post-traumatic stress disorder among veterans involved in the criminal justice system.
Jack Tsai, PhD is a Core Investigator of the VA New England Mental Illness Research, Education, and Clinical Center and Director of Research at the VA Errera Community Care Center. He also serves as Associate Professor of Psychiatry at Yale School of Medicine and Director of the Yale Division of Mental Health Services Research.
Alec Buchanan, MD, PhD, is a forensic psychiatrist, Professor of Psychiatry with Yale School of Medicine and Associate Chief of the Mental Health Service Line at the VA Connecticut Healthcare System. His empirical and theoretical research focuses on the intersection of mental illness and criminal behavior.
Joel Rosenthal, PhD, received his Ph.D. in Clinical Psychology from Georgia State University in 1988 and has been a licensed practicing clinical psychologist in California since 1990. He retired in 2017 at the conclusion of a 31-year career with the U.S. Department of Veterans Affairs. This included 24 years providing direct clinical care and program leadership at the VA Palo Alto Health Care System followed by seven years as National Training Director of VA’s Veterans Justice Programs.
Alex H. S. Harris, PhD, MS, is a Research Career Scientist at the VA Health Services Research & Development Center for Innovation to Implementation, VA Palo Alto Health Care System, and an Associate Professor at the Department of Surgery, Stanford University School of Medicine. He is an expert in substance use disorder treatment, quality measures, and implementation science.
Susan Frayne, MD, MPH, is a General Internist and Core Investigator at the VA Health Services Research & Development Center for Innovation to Implementation at the VA Palo Alto Health Care System, and a Professor of Medicine in the Division of Primary Care and Population Health at the Stanford University School of Medicine. She is also the Director of the VA Women’s Health Evaluation Initiative and the Director of the VA Women’s Health Practice-Based Research Network Coordinating Center at the VA Palo Alto Health Care System.
References
- Ahlin EM, and Douds AS. “Military socialization: A motivating factor for seeking treatment in a Veterans’ Treatment Court.” American Journal of Criminal Justice 41, (2016):83–96. 10.1177/0306624X17723626 [DOI] [Google Scholar]
- Baldwin JM ”Whom do they serve? A national examination of Veterans Treatment Court participants and their challenges.” Criminal Justice Policy Review 28, no. 6 (2017):515–554. doi: 10.1177/0887403415606184. [DOI] [Google Scholar]
- Baldwin JM, and Rukus J. “Healing the wounds: An examination of Veterans Treatment Courts in the context of restorative justice.” Criminal Justice Policy Review 26 no. 2 (2015):183–207. doi: 10.1177/0887403413520002. [DOI] [Google Scholar]
- Blackburn PK, and Cheesman F.”Veterans Treatment Court Performance Measures” 2015. Vet Court Con, Washington, DC. [Google Scholar]
- Blue-Howells JH, Clark SC, van den Berk-Clark C, and McGuire JF. “The U.S. Department of Veterans Affairs Veterans Justice Programs and the sequential intercept model: Case examples in national dissemination of intervention for justice-involved veterans.” Psychological Services 10, no.1 (2013):48–53. doi: 10.1037/a0029652. [DOI] [PubMed] [Google Scholar]
- Bronson J, Carson EA, Noonan M, and Berzofsky M. “Veterans in prison and jail, 2011–12.” 2015. Bureau of Justice Statistics https://www.bjs.gov/content/pub/pdf/vpj1112.pdf [Google Scholar]
- Cartwright T ”To care for him who shall have borne the battle: The recent development of Veterans Treatment Courts in America.” Stanford Law & Policy Review no 22 (2011): 295–316. https://law.stanford.edu/publications/care-shall-borne-battle-recent-development-veterans-treatment-courts-america/ [Google Scholar]
- Cavanaugh JM “Helping those who serve: Veterans treatment courts foster rehabilitation and reduce recividism for offending combat veterans.” New England Law Review 45 (2010):463–487. [Google Scholar]
- Department of Veterans Affairs. Mental health residential rehabilitation treatment program (MH RRTP) Washington, DC: Veterans Health Administration. 2010. [Google Scholar]
- Department of Veterans Affairs. Veterans Justice Programs (VJP) Washington, DC: Veterans Health Administration.2017. [Google Scholar]
- Finlay AK “Mental health and substance use disorder diagnoses and treatment use among veterans in Veterans Treatment Courts - Identification of Treatment Needs and Interventions “ 2016. Vet Court Con, Anaheim, CA, June 1, 2018. [Google Scholar]
- Harris AHS, Weisner CM, Chalk M, Capoccia V, Chen C, and Thomas CP. “Specifying and pilot testing quality measures for the American Society of Addiction Medicine’s standards of care.” Journal of Addiction Medicine 10, no. 3 (2016):148–55. doi: 10.1097/ADM.0000000000000203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartley RD, and Baldwin JM. “Waging war on recidivism among justice-involved veterans: An impact evaluation of a large urban Veterans Treatment Court.” Criminal Justice Policy Review, (2016):1–27. doi: 10.1177/0887403416650490. [DOI] [Google Scholar]
- Institute of Medicine. Best care at lower cost: The path to continuously learning health care in America Washington, DC: National Academies Press. 2012. https://www.nap.edu/catalog/13444/best-care-at-lower-cost-the-path-to-continuously-learning [PubMed] [Google Scholar]
- Johnson RS, Stolar AG, McGuire JF, Mittakanti K, Clark S, Coonan LA, and Graham DP. “Predictors of incarceration of veterans participating in U.S. Veterans’ Courts.” Psychiatr Serv 68, no. 2 (2017) :144–150. doi: 10.1176/appi.ps.201500266. [DOI] [PubMed] [Google Scholar]
- Johnson RS, Stolar AG, Wu E, Coonan LA, and Graham DP.”An analysis of successful outcomes and associated contributing factors in veterans’ court.” Bulletin of the Menninger Clinic 79, no.2 (2015):166–73. doi: 10.1521/bumc.2015.79.2.166. [DOI] [PubMed] [Google Scholar]
- Knudsen KJ, and Wingenfeld S. “A specialized treatment court for veterans with trauma exposure: Implications for the field.” Community Mental Health Journal 52, (2015):127–135. doi: 10.1007/s10597-015-9845-9. [DOI] [PubMed] [Google Scholar]
- Marlowe DB, Hardin CD, and Fox CL. Painting the current picture: A national report on drug courts and other problem-solving courts National Drug Court Institute. 2016. http://www.ndci.org/wp-content/uploads/2016/05/Painting-the-Current-Picture-2016.pdf [Google Scholar]
- McCormick-Goodhart MA ” Leaving no veteran behind: Policies and perspectives on combat trauma, veterans courts, and the rehabilitative approach to criminal behavior.” Penn State Law Review 117 (2016): 895–926. [Google Scholar]
- National Institute of Justice. “Adult Drug Court Program Logic Model” 2018. http://www.nij.gov/topics/courts/drugcourts/pages/measures-evaluation.aspx#performancemeasures.
- Russell RT “Veterans Treatment Court: A proactice approach.” New England Journal on Criminal and Civil Confinement 35 (2009) :357–372. [Google Scholar]
- Slattery M, Dugger MT, Lamb TA, and Williams L.”Catch, treat, and release: Veteran Treatment Courts address the challenges of returning home.” Substance Use & Misuse 48 no.10 (2013):922–32. doi: 10.3109/10826084.2013.797468. [DOI] [PubMed] [Google Scholar]
- Smith JW “The Anchorage, Alaska veterans court and recidivism.” July 6, 2004 – December 31, 2010.” Alaska Law Review 29 (2012):93–111. [Google Scholar]
- Timko Christine, Flatley Bessie, Tjemsland Amanda, McGuire Jim, Clark Sean, Blue-Howells Jessica, Blonigen Daniel M., Rosenthal Joel, and Finlay Andrea. “A Longitudinal Examination of Veterans Treatment Courts’ Characteristics and Eligibility Criteria.” Justice Research and Policy 17, no. 2 (December 2016): 123–36. doi: 10.1177/1525107117740087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai J, Finlay A, Flatley B, Kasprow WJ, and Clark S. “A national study of Veterans Treatment Court participants: Who benefits and who recidivates.” Adm Policy Ment Health 45, no.2 (2018):236–244. doi: 10.1007/s10488-017-0816-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai J, Flatley B, Kasprow WJ, Clark S, and Finlay A. 2017. “Diversion of veterans with criminal justice involvement to treatment courts: Participant characteristics and outcomes.” Psychiatr Serv 68, no.4 (2017):375–383. doi: 10.1176/appi.ps.201600233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Veterans Affairs. 2017. Veterans Justice Programs Strategic Plan 2017–2021 Washington, DC: Author. [Google Scholar]
- U.S. Department of Veterans Affairs. 2018a. VA benefits for service members [Google Scholar]
- U.S. Department of Veterans Affairs. 2018b. VA programs for homeless veterans [Google Scholar]
- U.S. Department of Veterans Affairs. 2018c. Veterans Treatment Courts and other Veteran-focused courts served by VA Veterans Justice Outreach Specialists [Fact Sheet] [Google Scholar]
- U.S. Department of Veterans Affairs. 2019. “Where you’ll go for care.” https://www.va.gov/health-care/about-va-health-benefits/where-you-go-for-care/. [Google Scholar]
- W. K. Kellogg Foundation. ”Using logic models to bring together planning, evaluation, and action: Logic model development guide.” 2004. https://www.wkkf.org/resource-directory/resource/2006/02/wk-kellogg-foundation-logic-model-development-guide.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


