Abstract
Introduction
Endoscopic treatment for pilonidal disease was initially described by Meinero in 2013. This minimally invasive technique has both technical and aesthetic advantages. The diagnostic application helps identify the anatomy of the pilonidal disease and the operative phase ablates and cleans the infected cavity. Our aim was to study the short-term outcomes of endoscopic treatment for pilonidal disease and to evaluate complications and recurrence rates.
Materials and methods
A prospectively maintained database of all consecutive patients who underwent endoscopic treatment for pilonidal disease by a single surgeon in a district general hospital from 1 November 2014 to 31 March 2018 was analysed. Follow-up was available until 30 September 2018.
Results
A total of 74 patients (56 men) underwent endoscopic treatment for pilonidal disease. The median age was 21 years (range 16–62 years). All patients underwent the procedure as daycase procedures, seven under local anaesthesia. There were no immediate postoperative complications and no return to theatre or readmission within 90 days.
On a median follow-up of 52 weeks (range 2–114 weeks), 57 patients healed completely and 8 lost to follow-up. We achieved primary healing rates of 67% (44/66) and delayed healing rate of 77% (51/66).
Conclusions
Endoscopic treatment for pilonidal disease is a safe and effective minimally invasive technique that should be considered as first-line treatment in selected cases of pilonidal sinus disease, thereby reducing morbidity related to conventional procedures.
Keywords: Pilonidal sinus, Pilonidal disease, Pilonidal Abscess, Endoscopic
Introduction
Pilonidal sinus disease is most commonly seen in the sacrococcygeal area and around the natal cleft. The reported incidence is around 25 per 100,000 with a male to female ratio between three and four to one.1 There can be considerable impact on quality of life due to pain, amended activities and time off work.
The aetiology of pilonidal sinus disease is thought to be the retention of follicular hair or keratin associated with an inflammatory response. The above hypothesis was developed from the widely accepted theories of Bascom and Stelzner.2–4 This hypothesis could also explain the late recurrences due to the chronic retention of hair and the long-lasting pressure effect on the terminal saccrococcygeal hair follicles. Meinero concluded in his paper that the late recurrences could be considered to be new primary disease by extrapolating these theories.5
Surgery for pilonidal sinus disease has been in the form of excision, associated sometimes with unacceptable levels of morbidity in a very physically active young group of patients. Over the 2000s, newer minimal access approaches including sinotomy, sinusectomy and trephining has increasingly played a role in the management of these patients. By using similar principles to video-assisted anal fistula treatment, Meinero developed a new technique more recently called endoscopic pilonidal sinus treatment.6 The procedure uses endoscopic treatment of the pilonidal sinus and pilonidal fistula tracts to remove and destroy follicular hair and keratin debris. We present a single-centre experience of this new technique.
Materials and methods
All consecutive patients who underwent endoscopic pilonidal sinus treatment between 1 November 2014 to 31 March 2018 were included in the study. Patients under 16 years of age and those who had acute pilonidal abscess were excluded from this study. (A series of patients with acute pilonidal abscess who were treated endoscopically has been published previously by our department).7 Data of patient demographics, comorbidities and previous treatment of pilonidal disease were collected. Details of endoscopic pilonidal sinus procedures and postoperative events were collected from a prospectively maintained database. Patients were followed up to 30 September 2018 to study healing and recurrence rates.
Technique
This procedure can be performed under general (complex sinus disease or patient preference) or local (simple sinuses) anesthethesia. The patient is positioned in a lateral or prone position (surgeon’s preference).
Instruments
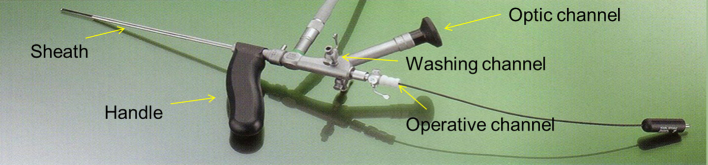
A specially designed optical 80 Meinero Fistuloscope (Fig 1) with an outer diameter of 3.4 × 4.7mm and a working length of 18cm is employed in this procedure. The fistuloscope has a working channel and an irrigation channel. Instruments that are used in the procedure include grasping forceps (double-action jaws of 2mm size and a length of 30cm), fistula brush (4–5mm outer diameter) and a monopolar coagulation electrode (‘Diathermy whip’ – 7 Fr and a length of 53cm).
Figure 1.
Meinero fistuloscope (courtesy of Karl Storz Endoscopy (UK) Ltd).
Diagnostic phase
The aim is to identify the anatomy of the pilonidal sinus and its secondary tracts. The existing draining sinus is opened to insert the fistuloscope and also to allow future irrigation. Irrigation channel is opened to allow glycine to display main and secondary tracts and sinuses. Tufts of hair within the tracts are then removed using grasping forceps in this phase.
Therapeutic phase
A diathermy whip is used to ablate granulation tissue in the tracts. Further hair shafts with their follicles and debris are removed at this stage. An endobrush is passed through the fistuloscope and the cavity is curetted. After curetting, meticulous attention is paid to haemostasis using diathermy, and 20ml 0.5% levobupivacaine is infiltrated after the procedure.
Postoperative advice
All patients were discharged the same day of procedure. No packing was required. Regular self-irrigation was advised for four weeks or until the wound healed. Patients were also advised to have baths or showers every day. The first follow-up was scheduled for six weeks.
Cost of endoscopic pilonidal sinus treatment
The average cost of endoscopic pilonidal sinus treatment per treatment session (excluding postoperative care) is £1,195.40, which is similar to video-assisted anal fistula treatment.8
Results
Demographics
A total of 74 (male to female ratio 56 : 18) patients underwent endoscopic pilonidal sinus treatment during the study period. The median age of the patients was 21 years (range (16–62 years). The predominant symptoms were chronic sinus (n = 43), pain (n = 13) and discharge (n = 18). Sixteen patients were smokers and two had type 2 diabetes. The majority were American Society of Anesthesiologists grade 1 (n = 54), followed by grade 2 (n = 13) and grade 3 (n = 7).
History of previous pilonidal disease
Thirty-three patients (two lost to follow-up) had endoscopic pilonidal sinus treatment as their primary procedure for pilonidal sinus. Some 22 patients (2 lost to follow-up) had at least one previous procedure and the remaining 19 (4 lost to follow-up) had 2–6 previous procedures prior to referral. Patients with acute pilonidal abscess were not included in this study, but four patients from our previous endoscopic pilonidal abscess treatment series who had recurrent symptoms were included.7 In addition, 30 patients required 63 hospital inpatient episodes due to recurrent problems.
Endoscopic pilonidal sinus treatment
All patients underwent endoscopic pilonidal sinus treatment as daycase procedures, of which seven were performed under local anaesthesia. There were no immediate postoperative complications, return to theatre or readmission within 90 days. Two patients were reviewed in the surgical assessment unit before the scheduled six-weeks-follow-up because of excessive bloodstained discharge, and were deemed to have inadequate irrigation of the sinus tracts.
Follow-up
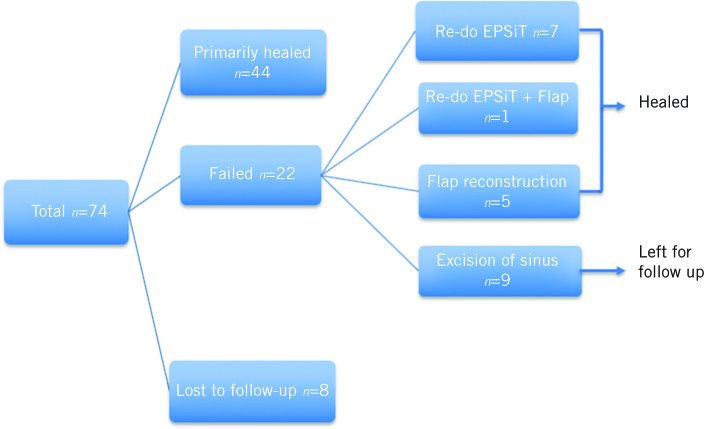
On a median follow-up of 52 weeks (range (2–114 weeks), 44 patients (67%) healed primarily after endoscopic pilonidal sinus treatment and 8 patients were lost to follow-up. Of the 22 patients who failed to heal primarily, 8 had repeat endoscopic pilonidal sinus treatment, seven of these patients healed and the other patient had a Karydakis flap and subsequently healed. Five patients had flap reconstructions, including one Karydakis flap under our team and four Lotus petal flaps under plastic surgeons. Nine patients required limited excision of superficial granulation tissue who continued to remain under follow-up. At the end of the study period we achieved a complete healing rate of 77% (51/66) after endoscopic pilonidal sinus treatment alone and 86% (57/66) with adjunct treatments (Fig 2).
Figure 2.
Follow-up outcomes after endoscopic pilonidal sinus treatment.
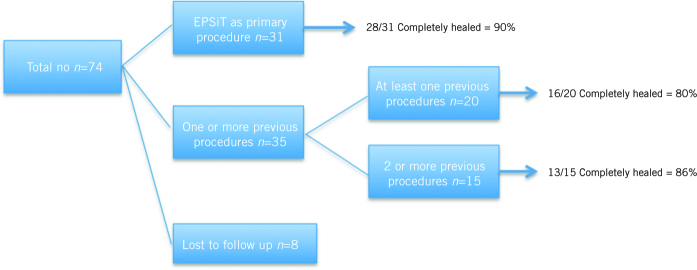
Interestingly, of those 31 patients who had endoscopic pilonidal sinus treatment as the primary treatment modality for pilonidal sinus disease, 28 achieved complete healing (90%), whereas only 29 patients of the 35 (83%) who had one or more previous procedures (endoscopic pilonidal abscess treatment, incision and drainage, excision) for pilonidal sinus disease achieved complete healing, although this did not reach statistical significance (Fig 3).
Figure 3.
Comparison of primary endoscopic pilonidal sinus treatment compared with patients who underwent previous interventions for pilonidal sinus disease.
Sixteen patients underwent laser depilation following endoscopic pilonidal sinus treatment and the impact of laser deplilation on primary healing and recurrence is being investigated in a separate study in our department. During the study period, none of the patients returned to us with recurrence of disease.
On further enquiry into the eight patients who were lost to follow up, one had complete resolution of symptoms. Three patients continued to have minor symptoms with occasional flareups that needed oral antibiotic prescriptions by the general practitioner. One patient who was deemed to have complex sinus disease with multiple previous procedures was awaiting a reconstruction procedure under plastic surgeons. Remaining three patients could not be contacted through the available contact information on the database.
Discussion
This is the first UK-based series reporting endoscopic pilonidal sinus treatment. Our findings are different from those published by Mienero et al.5 Our results suggest that endoscopic pilonidal sinus treatment is a safe procedure and can be performed in a daycase setting.
The pathogenesis of pilonidal sinus disease is thought to be a foreign body reaction secondary to hair dislocation in the natal cleft.2–4 Even though this theory has been widely accepted in men, the pathology is thought to be different in women, with hormone levels thought to play a role.9 Conventional procedures have all reported morbidity and delayed return to work secondary to wound management issues.10
Following the success of the video-assisted technique to treat perianal fistulas, the same principles were used to treat pilonidal sinus disease. The endoscopic pilonidal sinus procedure was developed to allow direct endoscopic vision of the pilonidal sinus. The direct vision achieved with the Meinero fistuloscope6 in the endoscopic procedure allows the surgeon to:
see not only the pilonidal sinus but also any possible secondary tracts or abscess cavities;
guarantee the complete destruction of the granulation tissue;
completely remove the hair follicles that are often located not only in the pilonidal sinus but also in the surrounding tissue, as previously described;
achieve effective haemostasis.
During the procedure, debris and hair can be easily identified and removed.
Compared with the existing literature, our study demonstrated healing rates of 77% (51/66) using endoscopic pilonidal sinus treatment as the only procedure. Meinero et al demonstrated a 94.8% healing rate in 250 patients using endoscopic pilonidal sinus treatment.5 They also demonstrated that an incomplete healing rate was related to the number of external openings, which we have not studied in our series. However, we did identify that endoscopic pilonidal sinus treatment can be successfully used as a first-line treatment for pilonidal disease in selected patients and with adjunct procedures healing rates of 86% (57/66) was achieved in our series (Fig 1). In our practice, we also observed that pilonidal sinus disease with no previous interventions such as excision, and therefore minimal scarring or tissue loss in that area, seem to respond favourably to endoscopic pilonidal sinus treatment. However, further follow-up and assessment is required to arrive at this conclusion.
A study from Turkey using endoscopic pilonidal sinus treatment and crystallised phenol showed a success of 100% in their study group.10 Even though the sample size was smaller, the findings are significant. Thus, such hybrid techniques might be able to improve the primary healing rates even further.
Although the present study has the limitation of the absence of a long-term follow-up period, the endoscopic pilonidal sinus treatment technique appears to offer adequate and effective outcomes. In addition, when pilonidal sinus disease was persistent, re-do endoscopic pilonidal sinus treatment was able to efficiently and successfully treat the disease in seven patients. Our practice is to consider flap reconstructions early, as some patients might not be suitable for endoscopic pilonidal sinus treatment due to body habitus and previous multiple procedures leading to tissue loss and scarring. This was the case in this series, where six patients required flap reconstructions.
Conclusion
Endoscopic pilonidal sinus treatment is a safe, effective, minimally invasive technique to manage pilonidal disease. This should be considered as first-line treatment in selected patients thereby reducing morbidity related to conventional procedures.
References
- 1.Sondenaa K, Andersen E et al. Patient characteristics and symptoms in chronic pilonidal disease. Int J Colorectal Dis 1995; : 39–42. [DOI] [PubMed] [Google Scholar]
- 2.Bascom J. Pilonidal disease: origin from follicles of hairs and results of follicle removal as treatment. Surgery 1980; : 567–572. [PubMed] [Google Scholar]
- 3.Bascom J. Pilonidal disease: long-term results of follicle removal. Dis Colon Rectum. 1983; : 800–807. [DOI] [PubMed] [Google Scholar]
- 4.Stelzner F. Causes of pilonidal sinus and pyoderma fistulans sinifica. Langenbecks Arch Chir 1984; : 105–118. [DOI] [PubMed] [Google Scholar]
- 5.Meinero P, Stazi A, Carbone A et al. Endoscopic pilonidal sinus treatment: a prospective multicentre trial. Colorectal Dis 2016; : 164–170. [DOI] [PubMed] [Google Scholar]
- 6.Meinero P, Mori L, Gasloli G. Endoscopic pilonidal sinus treatment (E.P.Si.T.). Tech Coloproctol 2014; : 389–392. [DOI] [PubMed] [Google Scholar]
- 7.Jain Y, Javed M A, Singh S et al. Endoscopic pilonidal abscess treatment: a novel approach for the treatment of pilonidal abscess. Ann R Coll Surg Engl 2017; : 134–136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.National Institute for Health and Care Excellence VAAFT for Treating Anal Fistulae (Medtech Innovation Briefing). London: NICE; 2017. [Google Scholar]
- 9.Ozkan Z, Aksoy N, Emir S et al. Investigation of the relationship between serum hormones and pilonidal sinus disease: a cross-sectional study. Colorectal Dis 2014; : 311–314. [DOI] [PubMed] [Google Scholar]
- 10.Gecim IE, Goktug UU, Celasin H. Endoscopic pilonidal sinus treatment combined with crystalized phenol application may prevent recurrence. Dis Colon Rectum 2017; : 405–407. [DOI] [PubMed] [Google Scholar]