Introduction
Miscarriage is the most common pregnancy complication worldwide, affecting approximately 30–50% of pregnancies, including preclinical cases.1 A miscarriage is a pregnancy loss that occurs before the fetus reaches the gestational age of 23 weeks,2 and chromosomal abnormalities are the primary cause.1 Environmental exposure to toxins and behavioral patterns, such as alcohol use are also contributing factors to pregnancy loss.2 With the exception of a few studies, however, little research has been conducted on women's perceptions of the causes and the defined period of pregnancy loss.3,4 Further research is needed as perceptions of maternal–fetal health can influence behavioral patterns in pregnancy,4,5 which can have important implications for subsequent pregnancy outcomes.
Studies conducted on the perceptions of pregnancy loss have found that women lack knowledge of evidence-based causes of early termination of pregnancy. In Malawi, researchers found that women did not know the causes of miscarriage.4 Women felt reluctant to seek medical assistance because they were fearful of the type of treatment they would receive from medical personnel. They also feared that they would be stigmatized in their community if others found out about their loss.4 In the United States, individuals had incorrect information about the causes of miscarriages; the majority of participants thought miscarriages were caused by a stressful event or by lifting heavy objects.3
Perceptions of pregnancy loss are particularly important to explore in India, where miscarriages occur at relatively high rates of 32%.6 Despite these high rates, the Indian medical community has not traditionally viewed women's experiences of pregnancy loss as a significant issue to explore,7 despite the lengths women go to protect the unborn fetus from harm.5 Recent studies, however, have pointed to the psychosocial implications of fetal and neonatal loss, such as being viewed by the family as a failure to produce viable offspring.7 As such, rural Indian women are reluctant to discuss their experiences with pregnancy loss due to fear of ridicule from family and community members since motherhood is viewed by many as the crux of womanhood.7
This pilot study was conducted to examine women's perceptions of the causes of pregnancy loss in two neighboring, but culturally distinct, populations in rural South India, where studies of the local perceptions of the causes of pregnancy loss are lacking acknowledgement. Women in this region are known to follow strict dietary norms aiming to circumvent the risk of fetal death and protect the mother from harm,5 however other beliefs of pregnancy loss are unknown. The overall aim of this research, therefore, was to generate findings that will aid local healthcare providers who educate women on the causes of pregnancy complications.
Study populations
This study was conducted with pregnant women from rural farming villages and the Jenu Kuruba tribe in Mysore district, Karnataka. Mysore is located in Southwest India at 12.30°N, 76.65°E. Mysore district has over 900,000 people living in the urban region, and over 1.6 million people residing in rural villages.8 Kannada is the official state language of Karnataka.
Women from rural farming villages are predominantly housewives or do seasonal work on either their husbands' farms or as low-paid agricultural labourers. The Jenu Kurubas are honey collectors by tradition, but currently work as daily-wage agricultural labourers.8,9 Jenu Kurubas differ from Hindu castes regarding health status, social structure, marital patterns, and gender equality.9 For instance, the sex ratio in Jenu Kurubas is higher than mainstream Hindus, indicating more gender equality, but due to isolation and discrimination, they have higher rates of malnutrition, illiteracy, and unemployment.9
Methods and analysis
Data were collected over the course of two months in 2015, and were part of a larger study that focused on dietary preferences and cultural norms in pregnancy. Pregnant participants completed an interviewer-administered structured questionnaire in the local language of Kannada. Questions included demographic information, total number of living children, miscarriages, and abortions. Women were also asked to free-list10 their perceptions of what causes pregnancy loss and to state the month of pregnancy that fetuses are at highest risk of death.
The Institutional Review Boards at Washington State University and Public Health Research Institute of India in Mysore reviewed and approved this study. Literate women provided written informed consent, and the others provided verbal consent and thumbprints to satisfy PHRII IRB requirements.
Data were analyzed using R version 3.1.2 (2014-10-31). Summary statistics were computed for demographic variables. Salience analysis was used to determine the most commonly perceived cause of pregnancy loss and the month(s) of pregnancy that fetuses are at highest risk of miscarriage. Salience analysis is used to measure the primary items within a cultural domain.10 This method computes a score that represents both the frequency of mention across participants and the order of mention. The composite salience score is calculated by adding the scores for each item across all participants.
Perceptions of pregnancy loss
Participants included pregnant women from rural farming villages (n = 72) and Jenu Kuruba haadis (n = 30). On average, participants from rural farming villages were 22 years of age (range: 18–33), and Jenu Kuruba were 23 years of age (range: 18–30).
The majority of women in the rural farming villages were primigravida (50%), 38% had one living child, and 13% had two living children (M = 0.63, range: 0–2). Fourteen rural farming women (19%) reported having at least one miscarriage or abortion (M = 0.23, range: 0–2). Rural farming women listed the following causes for their personal pregnancy losses: improper development, bleeding, lifting heavy weight, taking a long journey, and infection. One woman who took a long journey stated that her stomach banged into a cattle cart, which ultimately led to the loss of her baby.
Among Jenu Kuruba women, 37% were primigravida, 33.3% had one living child, and 30% had two living children (M = 0.93, range: 0–2). Five (16.7%) reported having at least one miscarriage or abortion (M = 0.67, range: 0–2). These women felt their pregnancies were unsuccessful due to stomach pain, superstition, and heart problems. Two women were not sure what caused their miscarriages. Two women reported loss of a child of less than one year of age. One woman stated that the cause of death was ‘superstition’ and the other did not provide a cause. Many Jenu Kurubas believe that infant death can occur during the early postpartum period if the infant is not monitored at all times during the day and night.
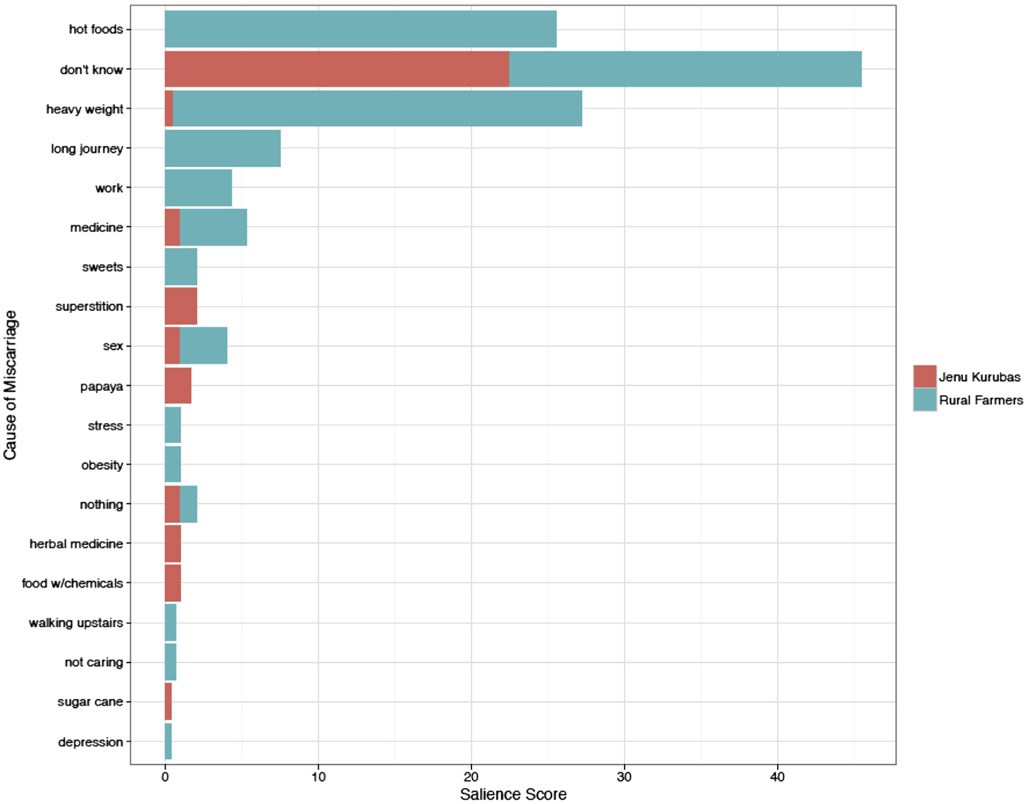
All women were asked what they think causes pregnancy loss regardless of their pregnancy histories. The most salient responses from rural farming women were: lifting heavy weight, consuming ‘hot’ foods, ‘don't know,’ going on a long journey, taking medicine, and work. Similar to the rural farming population, the majority of Jenu Kuruba women stated that they did not know the causes of pregnancy loss (73%). Two women mentioned superstition as the main cause, followed by consumption of papaya, consuming food with chemicals, taking herbal medicine, and sex. Both groups overlapped in the following responses: ‘don't know,’ carrying heavy weight, having sex, taking medicine, and ‘nothing.’ A complete list of responses and their salience scores are provided in Table 1, with a visual comparison of the two groups displayed in Fig. 1.
Table 1 –
Women's perceptions of the causes of pregnancy loss sorted by salience score.
| Cause of pregnancy loss | Salience score |
|---|---|
| Rural farmers | |
| Heavy weight | 26.68 |
| Hot foods | 25.51 |
| Don't know | 23 |
| Long journey | 7.49 |
| Work | 4.33 |
| Taking medicine | 4.33 |
| Sex | 3 |
| Eating sweets | 2 |
| Small stress | 1 |
| Nothing | 1 |
| Obesity | 1 |
| Walking upstairs | 0.67 |
| Not caring | 0.67 |
| Depression | 0.33 |
| Jenu Kuruba | |
| Don't know | 22.5 |
| Superstition (devil) | 2 |
| Papaya | 1.67 |
| Nothing | 1 |
| Sex | 1 |
| Take medicine | 1 |
| Take food with ‘chemicals’ (pesticides) | 1 |
| Herbal medicine | 1 |
| Heavy weight | 0.5 |
| Sugarcane | 0.33 |
Fig. 1 –
Distribution of salience scores for the perceived causes of miscarriage by population.
Women were asked to state the gestational period that fetuses are at highest risk of miscarriage. Among rural farming women, 40% did not know when fetuses are at highest risk of death, 14% stated that fetuses are at greatest risk during the third and fourth months, 10% stated that months three to five pose the highest risk, and another 10% stated that the first three months was the most vulnerable period. The majority of Jenu Kuruba women did not know when fetuses are at the greatest risk of miscarriage (77%). Two women (7%) stated that the period of two to four months poses the highest risk. Others provided time periods that covered anywhere from the first month to seven months gestation.
Conclusion
This pilot study explored perceptions of pregnancy loss among women from rural farming villages and the Jenu Kuruba tribe located in Mysore, India. Similar to women and men in the US,3 rural farming women associated miscarriage with lifting heaving weights, a behavioral cause, but also stated biological causes (e.g. heavy bleeding). Avoidance of ‘hot’ foods during pregnancy is common in South Asia because according to Ayurvedic theory, pregnancy increases heat in the body. To regain balance, women should consume cooling food items (e.g. curd and coconut).5 Jenu Kuruba women's perceived causes of loss included biological, behavioral, and supernatural causes. The inclusion of sugarcane by Jenu Kuruba women is not entirely clear and warrants further investigation. A large proportion of women from both groups did not know the causes of miscarriage, which justifies the need for public health education programmes that focus on pregnancy loss. Finally, there was no consensus across both groups of women regarding the gestation period that fetuses are at greatest vulnerability of death.
This study was limited in that the population of pregnant Jenu Kuruba women was fewer than women residing in rural farming villages. Also, these results might not generalize to other populations of tribal and rural farming women in India. Women in this study might have experienced recollection bias in attempting to identify the causes of their pregnancy loss. Future research will include a more in-depth qualitative assessment of local definitions of miscarriage and stillbirth and quantitatively assess the risk factors and psychosocial health outcomes of women who experience pregnancy loss.
This qualitative pilot study identified women's perceived causes of pregnancy loss and the differences in knowledge between two neighboring populations in Mysore district. Women's perceptions in these regions do not reflect evidence-based understanding of the causes of pregnancy loss; however, their perceptions should not be disregarded without further research. Regardless, these groups would benefit from public health interventions that provide education on evidence-based causes of pregnancy loss.
Acknowledgements
The authors would like to thank the participants for taking part in the study. The authors would also like to thank Edward Hagen for assistance in early phases of research design. A special thank-you is owed to Fazila, Lakshmana, and the remaining employees at the Public Health Research Institute of India for assisting with project implementation.
Funding
Research reported in this publication was supported by the Meyer Award and Mini Grant from Washington State University and the Fogarty International Center of the National Institutes of Health [training grant # TW009338]. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Competing interests
None declared.
Ethical approval
Ethical approval for this study was obtained from Washington State University and the Public Health Research Institute of India.
REFERENCES
- 1.Stephenson MD. Recurrent early pregnancy loss. Semin Reprod Med 2011;29:461–2. [DOI] [PubMed] [Google Scholar]
- 2.Kruger TF, Botha MH. Clinical gynaecology. Juta and Company Ltd; 2007. [Google Scholar]
- 3.Bardos J, Hercz D, Friedenthal J, Missmer SA, Williams Z. A national survey on public perceptions of miscarriage. Obstet Gynecol 2015;125:1313–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lake S, Rhodes H, Waite S, Fox C, Lissauer D, Makanani B, et al. Women attending hospital in Malawi for miscarriage: a qualitative study of perceptions of miscarriage. Brit J Med Med Res 2014;4:699. [Google Scholar]
- 5.Placek CD, Hagen EH. Fetal Protection. Hum Nat 2015;26(3):255–76. [DOI] [PubMed] [Google Scholar]
- 6.Patki A, Chauhan N. An epidemiology study to determine the prevalence and risk factors associated with recurrent spontaneous miscarriage in India. J Obstet Gynec India 2016:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Roberts LR, Montgomery S, Lee JW, Anderson BA. Social and cultural factors associated with perinatal grief in Chhattisgarh, India. J Comm Health 2012;37:572–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Census of India. Census of India: Census Data Online, c2011. [cited 2016 Nov 15]. Available from: http://censusindia.gov.in/2011-common/censusdataonline.html?drpQuick=&drpQuickSelect=&q=jenukuruba.
- 9.Roy S, Hegde HV, Bhattacharya D, Upadhya V, Kholkute SD. Tribes in Karnataka: status of health research. Ind J Med Res 2015;141:673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Quinlan M Considerations for collecting freelists in the field: examples from ethnobotany. Field Methods 2005;17:219–34. [Google Scholar]