Abstract
Improved hygiene leading to reduced exposure to microorganisms has been implicated as one possible cause for the recent “epidemic” of chronic inflammatory diseases (CIDs) in industrialized countries. That is the essence of the hygiene hypothesis that argues that rising incidence of CIDs may be, at least in part, the result of lifestyle and environmental changes that have made us too “clean” for our own good, so causing changes in our microbiota. Apart from genetic makeup and exposure to environmental triggers, inappropriate increase in intestinal permeability (which may be influenced by the composition of the gut microbiota), a “hyper-belligerent” immune system responsible for the tolerance–immune response balance, and the composition of gut microbiome and its epigenetic influence on the host genomic expression have been identified as three additional elements in causing CIDs. During the past decade, a growing number of publications have focused on human genetics, the gut microbiome, and proteomics, suggesting that loss of mucosal barrier function, particularly in the gastrointestinal tract, may substantially affect antigen trafficking, ultimately influencing the close bidirectional interaction between gut microbiome and our immune system. This cross-talk is highly influential in shaping the host gut immune system function and ultimately shifting genetic predisposition to clinical outcome. This observation led to a re-visitation of the possible causes of CIDs epidemics, suggesting a key pathogenic role of gut permeability. Pre-clinical and clinical studies have shown that the zonulin family, a group of proteins modulating gut permeability, is implicated in a variety of CIDs, including autoimmune, infective, metabolic, and tumoral diseases. These data offer novel therapeutic targets for a variety of CIDs in which the zonulin pathway is implicated in their pathogenesis.
Keywords: Chronic inflammatory diseases, Gut permeability, microbiome, zonulin
Introduction
Twenty-five hundred years ago, when Hippocrates stated that “All disease begins in the gut”, he had an incredible intuition that only recently has been fully appreciated because of new insights into the pathogenesis of many chronic inflammatory diseases (CIDs) afflicting humankind. Until 30 years ago, when the Human Genome Project was still in its planning stage, the general hypothesis was that genetic predisposition and exposure to an environmental trigger were both necessary and sufficient to develop CIDs, including infectious, allergic, neuroinflammatory/neurodegenerative, autoimmune diseases, and cancer. However, the epidemiological observation showing a major surge of CIDs during the past four decades in the Western hemisphere coincident with the declining rate of infectious diseases was at odds with the gene/environment paradigm 1, 2. This generated the hygiene hypothesis supporting the notion that we had made ourselves too clean for our own good and that people embracing a Western lifestyle would slowly die of CIDs instead of rapidly succumbing to infectious diseases as still is happening in developing countries.
What we learned when the Human Genome Project was completed is that we are genetically much more rudimentary than we had previously thought. The premise of “one gene, one protein, one disease” cannot explain the complexity of the balance between health and disease and, most definitively, the CIDs epidemics. Twenty-three thousand genes are insufficient to explain all the permutations of human pathophysiology, including if and when and why we develop diseases. Rather, it is the interplay between us as individuals and the environment in which we live that dictates our clinical destiny. This interplay is physically and mechanistically regulated by biological interfaces that divide our body from the surrounding environment. At about 8 to 9 meters in length, the human intestine provides the largest interface between our body and the outside world. Tightly packed single layers of epithelial cells cover the external surfaces of our intestinal mucosa and negotiate the interaction with the surrounding environment. Although this enormous mucosal interface (200 m 2) is not apparently visible, it plays a pivotal role through its dynamic interactions with a variety of factors coming from our surrounding environment, including microorganisms, nutrients, pollutants, and other materials. Intestinal permeability, together with luminal antigen (Ag) sampling by enterocytes via the transcellular pathway and dendritic cells, regulates molecular trafficking between the intestinal lumen and the submucosa, leading to either tolerance or immune response to non-self Ag 3– 5 ( Figure 1). Intercellular tight junctions (TJs) tightly regulate paracellular Ag trafficking. TJs are extremely dynamic structures that operate in several key functions of the intestinal epithelium under both physiological and pathological circumstances 6– 8. TJs, the most apical junctional complex of the paracellular pathway that segregates the apical and basolateral cellular compartment, were previously believed to be impermeable and static, so forming a sealing barrier. This paradigm was subverted in 1993 by the discovery of zonula occludens 1 (ZO-1) as the first component of the TJ complex 9 now being comprised of more than 150 proteins, including occludin 10, claudins 11, junctional adhesion molecules (JAMs) 12, tricellulin 13, and angulins 14. However, despite major progress in our knowledge on the composition and function of the intercellular TJ, the mechanisms by which they are regulated are still incompletely understood. One of the major breakthroughs in understanding the role of gut permeability in health and disease has been the discovery of zonulin, the only physiologic intestinal permeability modulator described so far 15, 16. Therefore, this article will focus mainly on the body of literature published on zonulin as a biomarker of gut permeability to outline the pathogenic role of a leaky gut in a variety of CIDs. However, it should be pointed out that zonulin is not involved in all CIDs and that not all CIDs have been linked to increased gut permeability.
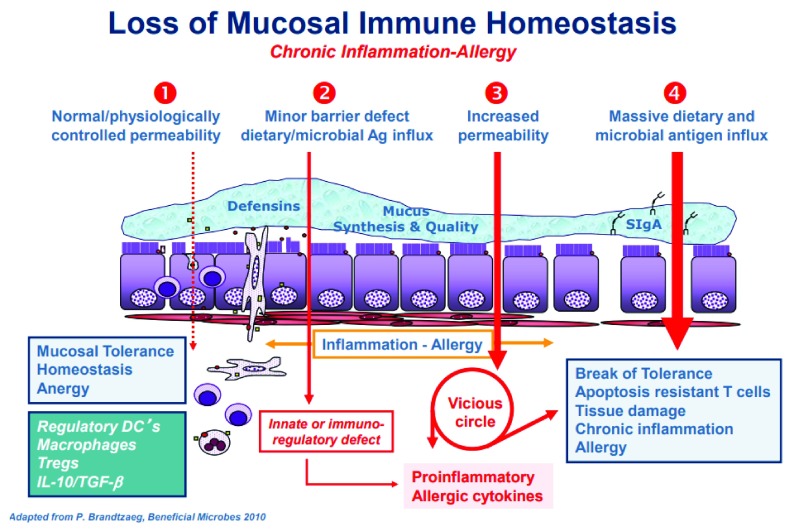
Figure 1. Proposed chain of events leading to chronic inflammatory disease.
( 1) Under physiological circumstances there is a tightly control of mucosal antigen trafficking (antigen sampling) that, in concert with specific immune cells and chemokine and cytokine mediators lead to anergy and therefore to mucosal tolerance. ( 2) Gut dysbiosis causes inappropriate production of increased amount of zonulin with subsequent functional loss of gut barrier function, followed by microbiota-derived antigen and endotoxin trafficking from the lumen to the lamina propria triggering innate and immunoregulatory responses causing a pro-inflammatory micromilieu. ( 3) If this process continues, an adaptive immune response is mounted, causing production of pro-inflammatory cytokines, including interferon gamma (IFN-γ) and tumor necrosis factor alpha (TNF-α) that cause further opening of the paracellular pathway to the passage of antigens, creating a vicious cycle. ( 4) Ultimately, these processes lead to break of tolerance with subsequent onset of chronic inflammatory disease whose nature is influenced by the specific host genetic background that dictates which organ or tissue will be targeted by the inflammatory process. DC, dendritic cell; IL-10, interleukin 10; TGF-β, transforming growth factor beta; Tregs, regulatory T cells. This figure was re-used from Zonulin, a regulator of epithelial and endothelial barrier functions, and its involvement in chronic inflammatory diseases. Tissue Barriers. doi:10.1080/21688370.2016.1251384 with permissions 17.
The zonulin pathway and its activation
Zonulin is composed of a family of related proteins 17– 19 whose first member, pre-haptoglobin 2 (HP2), the precursor of HP2, was identified almost two decades ago 20, 21. Haptoglobins evolved from a complement-associated protein (mannose-binding lectin-associated serine protease, or MASP) that lost its protease function because of mutations in the catalytic domain to then acquire new functions, including the capability to modulate intercellular TJs 18. The frequent zonulin polymorphisms secondary to high mutation rate during evolution led to a family of structurally and functionally related zonulins, including pre-HP2 and properdin, another member of the MASP family 22.
Among the several potential intestinal luminal stimuli that can stimulate zonulin release, small exposure to large amounts of bacteria (bacteria overgrowth) and gluten, the protein causing celiac disease (CD), have been identified as the two most powerful triggers 23, 24. Zonulin secretion has been shown to be MyD88-dependent 25 and is followed by an increase in gut permeability secondary to the disassembly of the protein ZO-1 from the tight junctional complex 26. Gliadin triggers zonulin release through the CXCR3 receptor activated by its engagement to MyD88 with a subsequent increase in gut permeability 27, suggesting that gluten is misinterpreted by the zonulin pathway as a potential harmful component of a microorganism. Taken together, these data suggest that the activation of the zonulin pathway may represent a defensive mechanism that “flushes out” microorganisms, contributing to the innate immune response of the host against changes in microbiome ecosystem, specifically bacterial colonization of the small intestine (small intestinal bacterial overgrowth) or changes in its composition (dysbiosis) or both. These findings are in line with the growing evidence on the role of changes in gut microbiome composition and function in causing functional changes in gut permeability, with subsequent increased Ag trafficking and break of tolerance leading to CID in genetically susceptible individuals ( Figure 1).
Pathological consequences of the activation of the zonulin pathway
Modulation of intestinal permeability, including the activation of the zonulin pathway, is part of the physiological machinery to maintain mucosal homeostasis and therefore does not always translate in clinical pathological outcomes. Indeed, studies on transgenic mice with constitutive activation of myosin light-chain kinase (MLCK), an intracellular mediator of TJ disassembly, showed increased intestinal permeability without signs of overt disease 28. Similarly, mice lacking JAM-A, a key TJ structural component, or the muscle myosin IIA heavy chain (NM IIA) showed increased intestinal permeability but only low-grade colonic inflammation and normal epithelial architecture 29, 30. Finally, zonulin transgenic mice constitutively producing high levels of zonulin showed increased gut permeability but not pathologic phenotype 31. Interestingly, zonulin transgenic, JAM-A −/−, and NM IIA −/− mice all showed increased susceptibility to chemical-induced colitis 29– 31. Together, these data suggest that gut permeability may contribute to the development of several CIDs provided that additional genetic components regulating immune response and an imbalanced microbiome are coexistent. Indeed, there is growing evidence that the additional and mutually influenced elements of the triad of gut permeability, immune system, and gut microbiome—together with genetic predisposition and exposure to environmental triggers—make the “perfect storm” for CIDs development.
Challenges in measuring zonulins with currently commercially available enzyme-linked immunosorbent assays
Several groups, including ours, have been questioning what exactly the commercially available zonulin enzyme-linked immunosorbent assay (ELISA) kits measure 22, 32. Using different approaches, both we 22 and others 32 identified complement C3 as the top match protein identified by the antibodies used for the ELISA. However, complement C3 is most likely an unspecific product overshadowing the real targets. Indeed, the respective ELISA kits did not detect any complement C proteins obtained from different suppliers when tested under native and denatured conditions, as well as when C3 was spiked in serum 22. Also, the same kit did not detect recombinant zonulin, mature HP1, or mature HP2 22. Given the additional mass spectrometric hits reported 22, 32, a few proteins stand out, although, without further validation, these data need to be interpreted with caution, since only more abundant proteins may be identified by mass spectrometric analysis, while the protein(s) of interest belonging to the zonulin family may be in low abundance in serum samples and therefore not identifiable with this approach. Keeping this in mind and the fact that the protein(s) of interest should be in the roughly 50-kDa range, combined Western blot analysis and ELISA test confirmed that the polyclonal antibodies raised against the zonulin-derived synthetic peptide AT1001 and used in the Immundiagnostik kit (Immundiagnostik AG, Bensheim, Germany) detect properdin among other proteins 22. However, when purified proteins/peptides, including the AT1001 peptide used to raise the polyclonal antibodies (internal control), were tested by ELISA, they were highly underestimated by the test. One possible explanation for these results is that zonulin as both pre-HP2 and properdin is not the main target detected by the ELISA; however, the fact that even AT1001 was underestimated seems to suggest that this hypothesis cannot entirely explain these results. Alternatively, it is possible that tertiary and quaternary (multimers) structure arrangements present in sera samples but not in recombinant proteins are necessary in order to properly detect any zonulin member by this ELISA. Given these results, it is likely that the commercially available ELISAs detect one or more members of the zonulin family that have not been discovered yet.
Alterative tests to measure gut permeability
With the appreciation that gut microbiome composition/function can affect intestinal permeability and vice versa and that loss of gut barrier function allows passage of endotoxin from gut lumen to systemic circulation, there are additional tools to be considered to monitor intestinal permeability. The presence of cytotoxic bacterial products in serum can be evaluated by using IgA/IgM responses to sonicated samples of common Gram-negative gut commensal bacteria, and assays of serum lipopolysaccharides (LPSs) and other bacterial toxins, including cytolethal distending toxin subunit B, provide good methods to screen for increased gut permeability in combination with IgM levels to zonulin and measuring gut dysbiosis 33.
Role of zonulin pathway in specific chronic inflammatory disease
Zonulin has been implicated in many CIDs ( Table 1). Independent from the CIDs considered, the steps leading to break of tolerance and subsequent development of CID seem to be similar ( Figure 1). Below, we will review some of the CIDs that have been associated with dysregulation of the zonulin pathway, and a more complete list of diseases and related references is presented in Table 1.
Table 1. Chronic inflammatory diseases in which zonulin has been linked as a biomarker of gut permeability.
| Disease | Model | References |
|---|---|---|
| Aging | Human | 37, 38 |
| Ankylosis spondylitis | Human | 39 |
| Attention deficit hyperactivity disorder | Human | 40 |
| Autism | Human | 41, 42 |
| Celiac disease | Human | 15– 20, 23– 27, 43– 48 |
| Chronic fatigue syndrome/myalgic encephalomyelitis | Human | 49 |
| Colitis – inflammatory bowel diseases | Human | 50, 51 |
| Colitis | Mouse | 52 |
| Environmental enteric dysfunction | Human | 53 |
| Gestational diabetes | Human | 54, 55 |
| Glioma | Human | 56 |
| Glioma | Cell | 57 |
| Insulin resistance | Human | 58 |
| Irritable bowel syndrome | Human | 59, 60 |
| Hyperlipidemia | Human | 61 |
| HIV | Human | 62– 66 |
| Major depressive disorders | Human | 67, 68 |
| Multiple sclerosis | Mouse | 69 |
| Multiple sclerosis | Human | 70 |
| Necrotizing enterocolitis | Rat | 71 |
| Necrotizing enterocolitis | Human | 72 |
| Non-alcoholic fatty liver disease | Human | 73– 77 |
| Non-celiac gluten sensitivity | Human | 53, 78 |
| Obesity | Human | 79– 87 |
| Schizophrenia | Human | 41, 88, 89 |
| Sepsis | Human | 90 |
| Type 1 diabetes | Rat | 91 |
| Type 1 diabetes | Human | 92, 93 |
| Type 2 diabetes | Human | 94, 95 |
Aging
Aging is the result of a constellation of cumulative changes that are deleterious, progressive, universal, and thus far irreversible. Aging damage can occur at the molecular (DNA, proteins, and lipids), cellular, or organ level (or a combination of these). Recent scientific successes in rejuvenation and extending a lifespan of model animals give hope to achieve negligible senescence, reverse aging or at least significantly delay it. Many non-mutually excluding theories have been formulated to model the senescence process, including the free radical theory 34, the cellular senescence and apoptotic theory 35, the immune system theory of aging 36, and (pertinent to this article) the intestinal permeability and aging theory. Indeed, several reports in both animal models and humans link gut permeability to non-infective chronic inflammation and metabolic changes typical of the senescence process. In fruit fly, the increase in intestinal permeability leads to systemic metabolic defects and immune changes previously linked to aging and is the best predictor of imminent death, even more than the actual age of the insect 96. In humans, it has been reported that zonulin serum concentration is higher in older adults, is positively associated with concentrations of the pro-inflammatory cytokines tumor necrosis factor alpha (TNF-α) and interleukin 6 (IL-6), and intriguingly is negatively correlated with skeletal muscle strength and habitual physical activity 37. These results suggest that zonulin-dependent gut permeability is associated with both systemic inflammation and two key indices of physical frailty associated with aging. These results have been corroborated by more recent data generated in disease-free ultra-centenarians showing lower levels of serum zonulin and endotoxemia as instigator of inflammation compared with young patients with acute myocardial infarction 38, supporting the notion that, as in the fruit fly, gut permeability may impact lifespan expectations.
Autoimmune disorders
Celiac disease. Celiac disease (CD) is an autoimmune enteropathy triggered by the ingestion of gluten-containing grains in genetically susceptible individuals and can be reversed when gluten is eliminated from the diet. As mentioned above, indigestible fragments of gluten are able to bind CXCR3 and release zonulin 27. CD has been used as a model disorder to study the effect of zonulin since its involvement in the development and pathogenesis of the disease has been well documented 15– 20, 23– 27. Even if gluten can trigger zonulin release in both healthy individuals and CD subjects, the amount and duration of zonulin produced are much higher in the latter group, leading to a significant increase in gut permeability, as shown by the capability of the zonulin inhibitor AT1001 (now named larazotide acetate) to prevent the zonulin permeating activity both in ex vivo models 43, 44 and in a transgenic animal model of CD in which it prevented gluten-dependent inflammation and intestinal damage 38. Larazotide acetate has been tested in patients with CD, showing good safety and efficacy in preventing gluten-dependent inflammation 45– 48, and is now in phase III clinical trial.
Type 1 diabetes. Type 1 diabetes (T1D) is an autoimmune condition caused by the destruction of the insulin-producing β cells of the pancreas, and the pathogenesis of this disease is still not fully understood. Several studies, in both animal models and T1D patients, have shown increased intestinal permeability to precede the development of T1D 97, 98. In a recent elegant study, it was demonstrated that loss of gut barrier integrity was actually the causal factor for the microbiota-mediated T1D 99 in susceptible mice, further supporting the critical role of the gut barrier–microbiome–immune system triad in the pathogenesis of CID. BioBreeding diabetes-prone rats, which spontaneously develop T1D, have increased small intestinal permeability which precedes the loss of tolerance to glucose by at least one month 100. Oral administration of the zonulin blocker AT1001 in these rats corrected the gut barrier defect and reduced the incidence of diabetes, suggesting a mechanistic role of the zonulin-dependent gut barrier modulation in the pathogenesis of T1D 91. The involvement of zonulin in T1D was confirmed in human studies showing that about 50% of patients with T1D have increased serum zonulin levels, some of them showing these changes in the pre-diabetic phase of the disease 92. Interestingly, a subset (about 25%) of healthy first-degree relatives of patients with T1D also showed increased serum zonulin 92. Similar data were generated in children at risk of T1D in which zonulin correlated with Glo-3A antibodies (a potential biomarker of the disease) in cases (at-risk children in the pre-clinical phase [positive auto-antibodies] or overt T1D) but not in controls (at-risk children negative for auto-antibodies) 93. Combined, these data suggest that zonulin may play a role in the pathogenesis of T1D in a subset of patients.
Inflammatory bowel disease. Increased intestinal permeability has been shown to play a crucial role in the pathogenesis of inflammatory bowel diseases (IBDs) 101– 105. Arrieta et al., using the IL-10 knockout colitis mouse model, showed increased small intestinal permeability that preceded the onset of the overt colitis that can be ameliorated by oral treatment with zonulin inhibitor AT-1001 52. In humans, serum and fecal zonulin were found to be elevated in patients with active Crohn’s disease but not with ulcerative colitis 50. In a more recent study, serum zonulin concentration was found to be higher in both diseases, and an inverse correlation was observed between serum zonulin concentration and disease duration 51.
Multiple sclerosis. In the experimental autoimmune encephalomyelitis mouse model of multiple sclerosis (MS), zonulin-dependent increased intestinal permeability was shown during the pre-clinical phase of neurological symptoms, suggesting a role for zonulin in disease development 69.
It has been reported that patients affected by MS show increased permeability of both the blood–brain barrier (BBB) and the intestine. A recent report showed that zonulin concentrations were significantly higher in MS patients showing a compromised BBB as shown by magnetic resonance imaging 70. Interestingly, baseline zonulin concentrations were associated with 1-year disease progression in progressive MS and closely mirror BBB breakdown in relapsing remitting MS. Considering these results, the authors concluded that zonulin may be responsible for the breakdown of both the intestinal barrier and the BBB in gut dysbiosis, thereby explaining how the gut–brain axis modulates neuroinflammation in MS 70.
Ankylosing spondylitis. Ankylosing spondylitis (AS) is an inflammatory, autoimmune condition that typically begins in young adulthood but often gets overlooked or is incorrectly diagnosed as pain from a previous injury or aging. It is an underdiagnosed form of arthritis that creates inflammation in the spinal joints and causes chronic back pain and stiffness. Dysbiosis has recently been demonstrated in patients with AS but its implications in the modulation of intestinal immune responses have never been studied. By analyzing ileal biopsies from patients with AS, Ciccia et al. showed that the presence of adherent and invasive bacteria in the gut of patients with AS with the bacterial scores significantly correlated with gut inflammation 39. Impairment of the gut vascular barrier was also present in AS, accompanied by significant upregulation of zonulin, and was associated with high serum levels of LPS, LPS-binding protein, intestinal fatty acid–binding protein (iFABP), and zonulin 39. In in vitro studies, zonulin altered endothelial TJs while its epithelial release was modulated by isolated AS ileal bacteria. Furthermore, they provided evidence that bacterial products and zonulin influence monocyte behavior. Considering these results, the authors concluded that bacterial ileitis, increased zonulin expression, and damaged intestinal mucosal epithelial and endothelial barriers characterize the gut of patients with AS and are associated with increased blood levels of zonulin and bacterial products.
Metabolic disorders
Obesity. Obesity and its complications, including high cholesterol, type 2 diabetes (T2D), coronary heart disease, high blood pressure, and stroke, have been shown to be associated with chronic inflammation 106– 108 and frequently linked to alteration of the zonulin pathway, and more than 30 articles have been published on this topic. Several of these studies have shown elevated serum zonulin levels increased in obese versus non-obese subjects 79– 86, and there is evidence of a correlation between total bacteria and serum zonulin levels, suggesting that the gut microbiota may cause increased zonulin levels, and subsequent abnormal gut permeability to endotoxin and ultimately micro-inflammation has been reported in obesity 106. A recent report also showed that zonulin serum correlates with total calorie, protein, carbohydrate, sodium, and vitamin B 12 intake in obese women, and Ruminococcaceae and Faecalibacterium were more abundant in the low-zonulin group, suggesting that butyrate-producing gut bacteria such as Faecalibacteria could decrease gut permeability by decreasing zonulin levels and lower inflammation 87.
Other metabolic disorders. Additional evidence suggests that zonulin is associated not only with obesity but also with its metabolic complications, including insulin resistance 58, non-alcoholic fatty liver disease 73– 77, gestational diabetes 54, 55, hyperlipidemia 61, and T2D 94, 95.
Intestinal diseases
Irritable bowel syndrome. Increased gut permeability has also been linked to the pathogenesis of irritable bowel syndrome (IBS) 59. Specifically, patients with diarrhea-associated IBS showed increased serum zonulin levels 60 and involvement of the protease-activated receptor 2 (PAR2) 109, 110, the zonulin target receptor 23.
Non-celiac gluten sensitivity. Non-celiac gluten sensitivity (NCGS) is a clinical entity triggered by gluten as in CD but without autoimmune enteropathy 111. It has been shown that patients with NCGS may have increased serum zonulin levels and increased intestinal permeability following gluten exposure 60, 78.
Environmental enteric dysfunction. Environmental enteric dysfunction (EED) is a chronic disease affecting mainly the proximal intestine. It is characterized by loss of barrier function, bacterial overgrowth in the small intestine, and low-grade intestinal inflammation leading to small intestinal villous atrophy that, in some aspects, resembles CD enteropathy. The potential developmental consequences of EE/EED can be devastating to the full physical and neurocognitive development in one third of the world’s children growing up in impoverished areas. It was recently reported that serum zonulin levels and other markers of barrier dysfunction were correlated with stunted growth in patients with EED 53.
Cancer
There is growing evidence in the literature that Ag trafficking can also be involved in the immune component leading to the onset of a variety of cancers. Here are reported those conditions in which zonulin as a biomarker of epithelial and endothelial permeability has been associated with cancer.
Glioma. Zonulin has also been shown to be involved brain tumors, mainly gliomas 56, 57. Increased zonulin expression of zonulin in gliomas correlated with the degree of malignancy and degradation of the BBB 56. In vitro studies on a glioma cell line showed that zonulin was expressed in high amounts compared with non-glioma control cells 57. Additionally, zonulin has been shown to induce transmigration of neuronal progenitor cells across the BBB 57.
Hepatocellular carcinoma. Hepatocellular carcinoma (HCC) globally ranks fifth for incidence and third for mortality among all malignant tumors. Although some progress has been made in exploring the pathological mechanisms and interventions of chronic liver diseases, there are still no effective biomarkers for the prediction and prevention of the progression of chronic liver diseases. Wang et al. recently reported that serum zonulin levels were significantly higher in patients with HCC compared with patients with liver cirrhosis or chronic hepatitis B or healthy subjects 112. Moreover, the zonulin levels were increased in the advanced stage of liver cirrhosis and HCC.
Neuroinflammatory diseases
Loss of gut barrier function (evaluated by serum IgG/IgA/IgM responses to occludin and zonulin and IgA responses to actomyosin) with subsequent increased serum levels of microbiota-derived molecules (assayed by testing serum lipopolysaccharides and bacterial toxins, including cytolethal distending toxin) and activation of the immune system (increased cytokines production) leading to neuroinflammation has been described in many neuroimmune disorders, including chronic fatigue syndrome, autism spectrum disorder (ASD), major depressive disorders (MDDs), and schizophrenia 32.
Autism spectrum disorder. Increased serum zonulin that positively correlated with the Childhood Autism Rating Scale score has been reported in children with ASD 41. In autism, as in other neuroinflammatory disorders, changes in zonulin-mediated gut permeability lead to pro-inflammatory status characterized by increased levels of mucosal pro-inflammatory cytokines (IL-5, IL-15, and IL-17) and decreased anti-inflammatory cytokines (transforming growth factor beta 1, or TGFβ1) detected mainly in ASD children experiencing gastrointestinal (GI) symptoms 42.
Schizophrenia. Increased plasma IgA/IgM responses to Gram-negative bacteria have been reported in deficit schizophrenia 112 indicating leaky gut and gut dysbiosis. These results were confirmed more recently by Maes et al., who reported that the ratio of IgM to zonulin + occludin/talin + actin + viculin was significantly greater in patients with deficit schizophrenia than in those with non-deficit schizophrenia and higher in patients with schizophrenia than in controls and was significantly associated with increased IgA responses to Gram-negative bacteria 88. IgM responses to zonulin were positively associated with schizophrenia (versus controls), whereas IgM to occludin was significantly associated with deficit schizophrenia (versus non-deficit schizophrenia and controls) 88. The results show an upregulated paracellular pathway with breakdown of the tight and adherens junctions and increased bacterial translocation in deficit schizophrenia, suggesting their mechanistic role in causing neuroinflammation typical of the disease. These data were recently confirmed by our group 89.
Major depressive disorders. Gut dysbiosis consistent with pathophysiological gut metagenomic signatures (upregulation LPS biosynthesis genes and deleterious metabolism of mood neurotransmitter pathways and host intestinal protective glycosaminoglycan mucins) different when compared with normal controls has been described in MDD 67. Parallel to these changes, subjects affected by MDD showed increased plasma levels of LPS, zonulin, and FABP2 67. Additionally, it has been demonstrated that, in patients with MDD, zonulin-mediated increased gut permeability causing increased bacterial translocation leads to marked alteration in circulating monocytes, with an expansion of the intermediate subset with increased frequency of IL-1β– and IL-6–producing cells. These changes are associated with a systemic pro-inflammatory state characterized by the enhanced serum TNF-α and IL-1β levels compared with those in the healthy controls 68.
Chronic fatigue syndrome or myalgic encephalomyelitis. Chronic fatigue syndrome/myalgic encephalomyelitis (CFS/ME) is an illness characterized by profound and pervasive fatigue in addition to a heterogeneous constellation of symptoms. The etiology of this condition remains unknown; however, it has been suggested that enteric dysbiosis is implicated in the pathogenesis of CFS/ME 49. In a systemic review, the microbiome composition of patients with CFS/ME was compared with that of healthy controls, showing statistically differences in some studies but with inconsistent findings in the studies considered 49. Nevertheless, evidence of loss of barrier function in CFS/ME 32 is consistent with the overall theme of mutual influence between gut dysbiosis and intestinal barrier function.
Conclusions
Besides genetic predisposition and exposure to environmental triggers, the pathogenesis of a variety of CIDs seems to involve mutually influenced changes in gut permeability/Ag trafficking, immune activation, and changes in composition/function of the gut microbiome. Zonulin is a modulator of both epithelial and endothelial barrier functions and its role in health and disease remains an object of active research. Gut dysbiosis may cause the release of zonulin leading to the passage of luminal contents across the epithelial barrier causing the release of pro-inflammatory cytokines that themselves cause increased permeability establishing a vicious loop leading to massive influx of dietary and microbial Ags triggering the activation of T cells. Depending on the host genetic makeup, activated T cells may remain within the GI tract, causing CID of the gut (IBD, IBS, CD, and EED), or migrate to several different organs to cause systemic CID. The effect of the zonulin inhibitor larazotide acetate in mitigating inflammation both in animal models and in human clinical trials not only confirms the pathogenic role of zonulin in many CIDs but also opens the possibility of targeting gut permeability in a variety of CIDs in which a pathogenic role for zonulin has been hypothesized or proven.
Abbreviations
Ag, antigen; AS, ankylosing spondylitis; ASD, autism spectrum disorder; BBB, blood–brain barrier; CD, celiac disease; CFS/ME, chronic fatigue syndrome/myalgic encephalomyelitis; CID, chronic inflammatory disease; EED, environmental enteric dysfunction; ELISA, enzyme-linked immunosorbent assay; GI, gastrointestinal; HCC, hepatocellular carcinoma; HP, haptoglobin; IBD, inflammatory bowel disease; IBS, irritable bowel syndrome; IL, interleukin; JAM, junctional adhesion molecule; LPS, lipopolysaccharide; MASP, mannose-binding lectin-associated serine protease; MDD, major depressive disorder; MS, multiple sclerosis; NCGS, non-celiac gluten sensitivity; T1D, type 1 diabetes; T2D, type 2 diabetes; TJ, tight junction; TNF-α, tumor necrosis factor alpha; ZO-1, zonula occludens 1
Editorial Note on the Review Process
F1000 Faculty Reviews are commissioned from members of the prestigious F1000 Faculty and are edited as a service to readers. In order to make these reviews as comprehensive and accessible as possible, the referees provide input before publication and only the final, revised version is published. The referees who approved the final version are listed with their names and affiliations but without their reports on earlier versions (any comments will already have been addressed in the published version).
The referees who approved this article are:
Arul Jayaraman, Department of Microbial Pathogenesis and Immunology, Texas A&M Health Science Center, Bryan, TX, USA
Michael Maes, Department of Psychiatry, Faculty of Medicine, Chulalongkorn University, Bangkok, Thailand
Xin M. Luo, Department of Biomedical Sciences and Pathobiology, College of Veterinary Medicine, Virginia Tech, Blacksburg, VA, USA
Funding Statement
The author declared that the following grants were involved in generating some of the data presented in this manuscript: National Institutes of Health (NIH) NIH DK104344 and NIH U19AI082655. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
[version 1; peer review: 3 approved]
References
- 1. Ege MJ: The Hygiene Hypothesis in the Age of the Microbiome. Ann Am Thorac Soc. 2017;14(Supplement_5):S348–S353. 10.1513/AnnalsATS.201702-139AW [DOI] [PubMed] [Google Scholar]
- 2. Haahtela T: A biodiversity hypothesis. Allergy. 2019;74(8):1445–56. 10.1111/all.13763 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 3. Chieppa M, Rescigno M, Huang AY, et al. : Dynamic imaging of dendritic cell extension into the small bowel lumen in response to epithelial cell TLR engagement. J Exp Med. 2006;203(13):2841–52. 10.1084/jem.20061884 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 4. Mowat AM, Millington OR, Chirdo FG: Anatomical and cellular basis of immunity and tolerance in the intestine. J Pediatr Gastroenterol Nutr. 2004;39 Suppl 3:S723–4. 10.1097/00005176-200406003-00003 [DOI] [PubMed] [Google Scholar]
- 5. Rescigno M, Lopatin U, Chieppa M: Interactions among dendritic cells, macrophages, and epithelial cells in the gut: implications for immune tolerance. Curr Opin Immunol. 2008;20(6):669–75. 10.1016/j.coi.2008.09.007 [DOI] [PubMed] [Google Scholar]
- 6. Arrieta MC, Bistritz L, Meddings JB: Alterations in intestinal permeability. Gut. 2006;55(1):1512–20. 10.1136/gut.2005.085373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Fasano A, Shea-Donohue T: Mechanisms of disease: the role of intestinal barrier function in the pathogenesis of gastrointestinal autoimmune diseases. Nat Clin Pract Gastroenterol Hepatol. 2005;2(9):416–22. 10.1038/ncpgasthep0259 [DOI] [PubMed] [Google Scholar]
- 8. Turner JR: Intestinal mucosal barrier function in health and disease. Nat Rev Immunol. 2009;9(11):799–809. 10.1038/nri2653 [DOI] [PubMed] [Google Scholar]
- 9. Itoh M, Nagafuchi A, Yonemura S, et al. : The 220-kD protein colocalizing with cadherins in non-epithelial cells is identical to ZO-1, a tight junction-associated protein in epithelial cells: cDNA cloning and immunoelectron microscopy. J Cell Biol. 1993;121(3):491–502. 10.1083/jcb.121.3.491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Furuse M, Hirase T, Itoh M, et al. : Occludin: a novel integral membrane protein localizing at tight junctions. J Cell Biol. 1993;123(6 Pt 2):1777–88. 10.1083/jcb.123.6.1777 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Furuse M, Fujita K, Hiiragi T, et al. : Claudin-1 and -2: novel integral membrane proteins localizing at tight junctions with no sequence similarity to occludin. J Cell Biol. 1998;141(7):1539–50. 10.1083/jcb.141.7.1539 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Martìn-Padura I, Lostaglio S, Schneemann M, et al. : Junctional adhesion molecule, a novel member of the immunoglobulin superfamily that distributes at intercellular junctions and modulates monocyte transmigration. J Cell Biol. 1998;142(1):117–27. 10.1083/jcb.142.1.117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Ikenouchi J, Furuse M, Furuse K, et al. : Tricellulin constitutes a novel barrier at tricellular contacts of epithelial cells. J Cell Biol. 2005;171(6):939–45. 10.1083/jcb.200510043 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 14. Higashi T, Tokuda S, Kitajiri S, et al. : Analysis of the 'angulin' proteins LSR, ILDR1 and ILDR2--tricellulin recruitment, epithelial barrier function and implication in deafness pathogenesis. J Cell Sci. 2013;126(Pt 4):966–77. 10.1242/jcs.116442 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 15. Fasano A, Not T, Wang W, et al. : Zonulin, a newly discovered modulator of intestinal permeability, and its expression in coeliac disease. Lancet. 2000;355(9214):1518–9. 10.1016/S0140-6736(00)02169-3 [DOI] [PubMed] [Google Scholar]
- 16. Wang W, Uzzau S, Goldblum SE, et al. : Human zonulin, a potential modulator of intestinal tight junctions. J Cell Sci. 2000;113 Pt 24:4435–40. [DOI] [PubMed] [Google Scholar]
- 17. Sturgeon C, Fasano A: Zonulin, a regulator of epithelial and endothelial barrier functions, and its involvement in chronic inflammatory diseases. Tissue Barriers. 2016;4(4):e1251384. 10.1080/21688370.2016.1251384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Fasano A: Zonulin and its regulation of intestinal barrier function: the biological door to inflammation, autoimmunity, and cancer. Physiol Rev. 2011;91(1):151–75. 10.1152/physrev.00003.2008 [DOI] [PubMed] [Google Scholar]
- 19. Valitutti F, Fasano A: Breaking Down Barriers: How Understanding Celiac Disease Pathogenesis Informed the Development of Novel Treatments. Dig Dis Sci. 2019;64(7):1748–58. 10.1007/s10620-019-05646-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Tripathi A, Lammers KM, Goldblum S, et al. : Identification of human zonulin, a physiological modulator of tight junctions, as prehaptoglobin-2. Proc Natl Acad Sci U S A. 2009;106(39):16799–804. 10.1073/pnas.0906773106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Rittirsch D, Flierl MA, Nadeau BA, et al. : Zonulin as prehaptoglobin2 regulates lung permeability and activates the complement system. Am J Physiol Lung Cell Mol Physiol. 2013;304(12):L863–72. 10.1152/ajplung.00196.2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Scheffler L, Crane A, Heyne H, et al. : Widely Used Commercial ELISA Does Not Detect Precursor of Haptoglobin2, but Recognizes Properdin as a Potential Second Member of the Zonulin Family. Front Endocrinol (Lausanne). 2018;9:22. 10.3389/fendo.2018.00022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. El Asmar R, Panigrahi P, Bamford P, et al. : Host-dependent zonulin secretion causes the impairment of the small intestine barrier function after bacterial exposure. Gastroenterology. 2002;123(5):1607–15. 10.1053/gast.2002.36578 [DOI] [PubMed] [Google Scholar]
- 24. Drago S, El Asmar R, Di Pierro M, et al. : Gliadin, zonulin and gut permeability: Effects on celiac and non-celiac intestinal mucosa and intestinal cell lines. Scand J Gastroenterol. 2006;41(4):408–19. 10.1080/00365520500235334 [DOI] [PubMed] [Google Scholar]
- 25. Thomas KE, Sapone A, Fasano A, et al. : Gliadin stimulation of murine macrophage inflammatory gene expression and intestinal permeability are MyD88-dependent: role of the innate immune response in Celiac disease. J Immunol. 2006;176(4):2512–21. 10.4049/jimmunol.176.4.2512 [DOI] [PubMed] [Google Scholar]
- 26. Clemente MG, De Virgiliis S, Kang JS, et al. : Early effects of gliadin on enterocyte intracellular signalling involved in intestinal barrier function. Gut. 2003;52(2):218–23. 10.1136/gut.52.2.218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Lammers KM, Lu R, Brownley J, et al. : Gliadin induces an increase in intestinal permeability and zonulin release by binding to the chemokine receptor CXCR3. Gastroenterology. 2008;135(1):194–204.e3. 10.1053/j.gastro.2008.03.023 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 28. Su L, Le Shen, Clayburgh DR, et al. : Targeted epithelial tight junction dysfunction causes immune activation and contributes to development of experimental colitis. Gastroenterology. 2009;136(2):551–63. 10.1053/j.gastro.2008.10.081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Laukoetter MG, Nava P, Lee WY, et al. : JAM-A regulates permeability and inflammation in the intestine in vivo. J Exp Med. 2007;204(13):3067–76. 10.1084/jem.20071416 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 30. Naydenov NG, Feygin A, Wang D, et al. : Nonmuscle Myosin IIA Regulates Intestinal Epithelial Barrier in vivo and Plays a Protective Role During Experimental Colitis. Sci Rep. 2016;6:24161. 10.1038/srep24161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Sturgeon C, Lan J, Fasano A: Zonulin transgenic mice show altered gut permeability and increased morbidity/mortality in the DSS colitis model. Ann N Y Acad Sci. 2017;1397(1):130–42. 10.1111/nyas.13343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Ajamian M, Steer D, Rosella G, et al. : Serum zonulin as a marker of intestinal mucosal barrier function: May not be what it seems. PLoS One. 2019;14(1):e0210728. 10.1371/journal.pone.0210728 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 33. Simeonova D, Ivanovska M, Murdjeva M, et al. : Recognizing the Leaky Gut as a Trans-diagnostic Target for Neuroimmune Disorders Using Clinical Chemistry and Molecular Immunology Assays. Curr Top Med Chem. 2018;18(19):1641–55. 10.2174/1568026618666181115100610 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 34. Dodig S, Čepelak I, Pavić I: Hallmarks of senescence and aging. Biochem Med (Zagreb). 2019;29(3):030501. 10.11613/BM.2019.030501 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 35. Soto-Gamez A, Quax WJ, Demaria M: Regulation of Survival Networks in Senescent Cells: From Mechanisms to Interventions. J Mol Biol. 2019;431(15):2629–43. 10.1016/j.jmb.2019.05.036 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 36. Prieto LI, Baker DJ: Cellular Senescence and the Immune System in Cancer. Gerontology. 2019;65(5):505–12. 10.1159/000500683 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 37. Qi Y, Goel R, Kim S, et al. : Intestinal Permeability Biomarker Zonulin is Elevated in Healthy Aging. J Am Med Dir Assoc. 2017;18(9):810.e1–810.e4. 10.1016/j.jamda.2017.05.018 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 38. Carrera-Bastos P, Picazo Ó, Fontes-Villalba M, et al. : Serum Zonulin and Endotoxin Levels in Exceptional Longevity versus Precocious Myocardial Infarction. Aging Dis. 2018;9(2):317–321. 10.14336/AD.2017.0630 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 39. Ciccia F, Guggino G, Rizzo A, et al. : Dysbiosis and zonulin upregulation alter gut epithelial and vascular barriers in patients with ankylosing spondylitis. Ann Rheum Dis. 2017;76(6):1123–32. 10.1136/annrheumdis-2016-210000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Özyurt G, Öztürk Y, Appak YÇ, et al. : Increased zonulin is associated with hyperactivity and social dysfunctions in children with attention deficit hyperactivity disorder. Compr Psychiatry. 2018;87:138–42. 10.1016/j.comppsych.2018.10.006 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 41. Esnafoglu E, Cırrık S, Ayyıldız SN, et al. : Increased Serum Zonulin Levels as an Intestinal Permeability Marker in Autistic Subjects. J Pediatr. 2017;188:240–4. 10.1016/j.jpeds.2017.04.004 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 42. Rose DR, Yang H, Serena G, et al. : Differential immune responses and microbiota profiles in children with autism spectrum disorders and co-morbid gastrointestinal symptoms. Brain Behav Immun. 2018;70:354–68. 10.1016/j.bbi.2018.03.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Gopalakrishnan S, Tripathi A, Tamiz AP, et al. : Larazotide acetate promotes tight junction assembly in epithelial cells. Peptides. 2012;35(1):95–101. 10.1016/j.peptides.2012.02.016 [DOI] [PubMed] [Google Scholar]
- 44. Gopalakrishnan S, Durai M, Kitchens K, et al. : Larazotide acetate regulates epithelial tight junctions in vitro and in vivo. Peptides. 2012;35(1):86–94. 10.1016/j.peptides.2012.02.015 [DOI] [PubMed] [Google Scholar]
- 45. Paterson BM, Lammers KM, Arrieta MC, et al. : The safety, tolerance, pharmacokinetic and pharmacodynamic effects of single doses of AT-1001 in coeliac disease subjects: a proof of concept study. Aliment Pharmacol Ther. 2007;26(5):757–66. 10.1111/j.1365-2036.2007.03413.x [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 46. Kelly CP, Green PH, Murray JA, et al. : Larazotide acetate in patients with coeliac disease undergoing a gluten challenge: a randomised placebo-controlled study. Aliment Pharmacol Ther. 2013;37(2):252–62. 10.1111/apt.12147 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 47. Leffler DA, Kelly CP, Abdallah HZ, et al. : A randomized, double-blind study of larazotide acetate to prevent the activation of celiac disease during gluten challenge. Am J Gastroenterol. 2012;107(10):1554–62. 10.1038/ajg.2012.211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Leffler DA, Kelly CP, Green PH, et al. : Larazotide acetate for persistent symptoms of celiac disease despite a gluten-free diet: a randomized controlled trial. Gastroenterology. 2015;148(7):1311–9.e6. 10.1053/j.gastro.2015.02.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Du Preez S, Corbitt M, Cabanas H, et al. : A systematic review of enteric dysbiosis in chronic fatigue syndrome/myalgic encephalomyelitis. Syst Rev. 2018;7(1):241. 10.1186/s13643-018-0909-0 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 50. Malíčková K, Francová I, Lukáš M, et al. : Fecal zonulin is elevated in Crohn's disease and in cigarette smokers. Pract Lab Med. 2017;9:39–44. 10.1016/j.plabm.2017.09.001 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 51. Caviglia GP, Dughera F, Ribaldone DG, et al. : Serum zonulin in patients with inflammatory bowel disease: a pilot study. Minerva Med. 2019;110(2):95–100. 10.23736/S0026-4806.18.05787-7 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 52. Arrieta MC, Madsen K, Doyle J, et al. : Reducing small intestinal permeability attenuates colitis in the IL10 gene-deficient mouse. Gut. 2009;58(1):41–8. 10.1136/gut.2008.150888 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Guerrant RL, Leite AM, Pinkerton R, et al. : Biomarkers of Environmental Enteropathy, Inflammation, Stunting, and Impaired Growth in Children in Northeast Brazil. PLoS One. 2016;11(9):e0158772. 10.1371/journal.pone.0158772 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Mokkala K, Tertti K, Rönnemaa T, et al. : Evaluation of serum zonulin for use as an early predictor for gestational diabetes. Nutr Diabetes. 2017;7(3):e253. 10.1038/nutd.2017.9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Demir E, Ozkan H, Seckin KD, et al. : Plasma Zonulin Levels as a Non-Invasive Biomarker of Intestinal Permeability in Women with Gestational Diabetes Mellitus. Biomolecules. 2019;9(1): pii: E24. 10.3390/biom9010024 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 56. Skardelly M, Armbruster FP, Meixensberger J, et al. : Expression of Zonulin, c-kit, and Glial Fibrillary Acidic Protein in Human Gliomas. Transl Oncol. 2009;2(3):117–20. 10.1593/tlo.09115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Díaz-Coránguez M, Segovia J, López-Ornelas A, et al. : Transmigration of neural stem cells across the blood brain barrier induced by glioma cells. PLoS One. 2013;8(4):e60655. 10.1371/journal.pone.0060655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Moreno-Navarrete JM, Sabater M, Ortega F, et al. : Circulating zonulin, a marker of intestinal permeability, is increased in association with obesity-associated insulin resistance. PLoS One. 2012;7(5):e37160. 10.1371/journal.pone.0037160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Camilleri M, Gorman H: Intestinal permeability and irritable bowel syndrome. Neurogastroenterol Motil. 2007;19(7):545–52. 10.1111/j.1365-2982.2007.00925.x [DOI] [PubMed] [Google Scholar]
- 60. Barbaro MR, Cremon C, Caio G, et al. : The role of zonulin in non-celiac gluten sensitivity and irritable bowel syndrome. United Euro Gastroenterol J. 2015;3:A87 Reference Source [Google Scholar]
- 61. Ohlsson B, Orho-Melander M, Nilsson P: Higher Levels of Serum Zonulin May Rather Be Associated with Increased Risk of Obesity and Hyperlipidemia, Than with Gastrointestinal Symptoms or Disease Manifestations. Int J Mol Sci. 2017;18(3): pii: E582. 10.3390/ijms18030582 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Funderburg N, Boucher M, Sattar A, et al. : Rosuvastatin Decreases Intestinal Fatty Acid Binding Protein (I-FABP), but Does Not Alter Zonulin or Lipopolysaccharide Binding Protein (LBP) Levels, in HIV-Infected Subjects on Antiretroviral Therapy. Pathog Immun. 2016;1(1):118–128. 10.20411/pai.v1i1.124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Koay WLA, Lindsey JC, Uprety P, et al. : Intestinal Integrity Biomarkers in Early Antiretroviral-Treated Perinatally HIV-1-Infected Infants. J Infect Dis. 2018;218(7):1085–9. 10.1093/infdis/jiy271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Utay NS, Somasunderam A, Hinkle JE, et al. : Serum Bovine Immunoglobulins Improve Inflammation and Gut Barrier Function in Persons with HIV and Enteropathy on Suppressive ART. Pathog Immun. 2019;4(1):124–46. 10.20411/pai.v4i1.276 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 65. Pastor L, Langhorst J, Schröder D, et al. : Different pattern of stool and plasma gastrointestinal damage biomarkers during primary and chronic HIV infection. PLoS One. 2019;14(6):e0218000. 10.1371/journal.pone.0218000 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 66. Dirajlal-Fargo S, El-Kamari V, Weiner L, et al. : Altered intestinal permeability and fungal translocation in Ugandan children with HIV. Clin Infect Dis. 2019;pii: ciz561. 10.1093/cid/ciz561 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 67. Stevens BR, Goel R, Seungbum K, et al. : Increased human intestinal barrier permeability plasma biomarkers zonulin and FABP2 correlated with plasma LPS and altered gut microbiome in anxiety or depression. Gut. 2018;67(8):1555–1557. 10.1136/gutjnl-2017-314759 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 68. Alvarez-Mon MA, Gómez AM, Orozco A, et al. : Abnormal Distribution and Function of Circulating Monocytes and Enhanced Bacterial Translocation in Major Depressive Disorder. Front Psychiatry. 2019;10:812. 10.3389/fpsyt.2019.00812 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 69. Nouri M, Bredberg A, Weström B, et al. : Intestinal barrier dysfunction develops at the onset of experimental autoimmune encephalomyelitis, and can be induced by adoptive transfer of auto-reactive T cells. PLoS One. 2014;9(9):e106335. 10.1371/journal.pone.0106335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Camara-Lemarroy CR, Silva C, Greenfield J, et al. : Biomarkers of intestinal barrier function in multiple sclerosis are associated with disease activity. Mult Scler. 2019:1352458519863133. 10.1177/1352458519863133 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 71. Ling X, Linglong P, Weixia D, et al. : Protective Effects of Bifidobacterium on Intestinal Barrier Function in LPS-Induced Enterocyte Barrier Injury of Caco-2 Monolayers and in a Rat NEC Model. PLoS One. 2016;11(8):e0161635. 10.1371/journal.pone.0161635 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Tarko A, Suchojad A, Michalec M, et al. : Zonulin: A Potential Marker of Intestine Injury in Newborns. Dis Markers. 2017;2017:2413437. 10.1155/2017/2413437 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Pacifico L, Bonci E, Marandola L, et al. : Increased circulating zonulin in children with biopsy-proven nonalcoholic fatty liver disease. World J Gastroenterol. 2014;20(45):17107–14. 10.3748/wjg.v20.i45.17107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Cakir M, Aksel İşbilen A, Eyüpoğlu İ, et al. : Effects of long-term synbiotic supplementation in addition to lifestyle changes in children with obesity-related non-alcoholic fatty liver disease. Turk J Gastroenterol. 2017;28(5):377–83. 10.5152/tjg.2017.17084 [DOI] [PubMed] [Google Scholar]
- 75. Kim JH, Heo JS, Baek KS, et al. : Zonulin level, a marker of intestinal permeability, is increased in association with liver enzymes in young adolescents. Clin Chim Acta. 2018;481:218–24. 10.1016/j.cca.2018.03.005 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 76. Kim AS, Ko HJ: Plasma concentrations of zonulin are elevated in obese men with fatty liver disease. Diabetes Metab Syndr Obes. 2018;11:149–57. 10.2147/DMSO.S163062 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 77. Kwon JH, Lee HG, Seo KH, et al. : Combination of Whole Grapeseed Flour and Newly Isolated Kefir Lactic Acid Bacteria Reduces High-Fat-Induced Hepatic Steatosis. Mol Nutr Food Res. 2019;63(4):e1801040. 10.1002/mnfr.201801040 [DOI] [PubMed] [Google Scholar]
- 78. Volta U, Caio G, Tovoli F, et al. : Non-celiac gluten sensitivity: Questions still to be answered despite increasing awareness. Cell Mol Immunol. 2013;10(5):383–92. 10.1038/cmi.2013.28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Zak-Gołąb A, Kocełak P, Aptekorz M, et al. : Gut microbiota, microinflammation, metabolic profile, and zonulin concentration in obese and normal weight subjects. Int J Endocrinol. 2013;2013:674106. 10.1155/2013/674106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Kuzma JN, Cromer G, Hagman DK, et al. : No differential effect of beverages sweetened with fructose, high-fructose corn syrup, or glucose on systemic or adipose tissue inflammation in normal-weight to obese adults: a randomized controlled trial. Am J Clin Nutr. 2016;104(2):306–14. 10.3945/ajcn.115.129650 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Mokkala K, Röytiö H, Munukka E, et al. : Gut Microbiota Richness and Composition and Dietary Intake of Overweight Pregnant Women Are Related to Serum Zonulin Concentration, a Marker for Intestinal Permeability. J Nutr. 2016;146(9):1694–700. 10.3945/jn.116.235358 [DOI] [PubMed] [Google Scholar]
- 82. Stenman LK, Lehtinen MJ, Meland N, et al. : Probiotic With or Without Fiber Controls Body Fat Mass, Associated With Serum Zonulin, in Overweight and Obese Adults—Randomized Controlled Trial. EBioMedicine. 2016;13:190–200. 10.1016/j.ebiom.2016.10.036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Gil-Cardoso K, Ginés I, Pinent M, et al. : Effects of flavonoids on intestinal inflammation, barrier integrity and changes in gut microbiota during diet-induced obesity. Nutr Res Rev. 2016;29(2):234–48. 10.1017/S0954422416000159 [DOI] [PubMed] [Google Scholar]
- 84. Küme T, Acar S, Tuhan H, et al. : The Relationship between Serum Zonulin Level and Clinical and Laboratory Parameters of Childhood Obesity. J Clin Res Pediatr Endocrinol. 2017;9(1):31–8. 10.4274/jcrpe.3682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Houttu N, Mokkala K, Laitinen K: Overweight and obesity status in pregnant women are related to intestinal microbiota and serum metabolic and inflammatory profiles. Clin Nutr. 2018;37(6 Pt A):1955–66. 10.1016/j.clnu.2017.12.013 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 86. Kuzma JN, Hagman DK, Cromer G, et al. : Intraindividual Variation in Markers of Intestinal Permeability and Adipose Tissue Inflammation in Healthy Normal-Weight to Obese Adults. Cancer Epidemiol Biomarkers Prev. 2019;28(3):610–5. 10.1158/1055-9965.EPI-18-0641 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 87. Mörkl S, Lackner S, Meinitzer A, et al. : Gut microbiota, dietary intakes and intestinal permeability reflected by serum zonulin in women. Eur J Nutr. 2018;57(8):2985–97. 10.1007/s00394-018-1784-0 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 88. Maes M, Sirivichayakul S, Kanchanatawan B, et al. : Upregulation of the Intestinal Paracellular Pathway with Breakdown of Tight and Adherens Junctions in Deficit Schizophrenia. Mol Neurobiol. 2019;56(10):7056–73. 10.1007/s12035-019-1578-2 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 89. Barber GS, Sturgeon C, Fasano A, et al. : Elevated zonulin, a measure of tight-junction permeability, may be implicated in schizophrenia. Schizophr Res. 2019;211:111–2. 10.1016/j.schres.2019.07.006 [DOI] [PubMed] [Google Scholar]
- 90. Klaus DA, Motal MC, Burger-Klepp U, et al. : Increased plasma zonulin in patients with sepsis. Biochem Med (Zagreb). 2013;23(1):107–11. 10.11613/bm.2013.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Watts T, Berti I, Sapone A, et al. : Role of the intestinal tight junction modulator zonulin in the pathogenesis of type I diabetes in BB diabetic-prone rats. Proc Natl Acad Sci U S A. 2005;102(8):2916–21. 10.1073/pnas.0500178102 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 92. Sapone A, de Magistris L, Pietzak M, et al. : Zonulin upregulation is associated with increased gut permeability in subjects with type 1 diabetes and their relatives. Diabetes. 2006;55(5):1443–9. 10.2337/db05-1593 [DOI] [PubMed] [Google Scholar]
- 93. Simpson M, Mojibian M, Barriga K, et al. : An exploration of Glo-3A antibody levels in children at increased risk for type 1 diabetes mellitus. Pediatr Diabetes. 2009;10(8):563–72. 10.1111/j.1399-5448.2009.00541.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Zhang D, Zhang L, Zheng Y, et al. : Circulating zonulin levels in newly diagnosed Chinese type 2 diabetes patients. Diabetes Res Clin Pract. 2014;106(2):312–8. 10.1016/j.diabres.2014.08.017 [DOI] [PubMed] [Google Scholar]
- 95. Jayashree B, Bibin YS, Prabhu D, et al. : Increased circulatory levels of lipopolysaccharide (LPS) and zonulin signify novel biomarkers of proinflammation in patients with type 2 diabetes. Mol Cell Biochem. 2014;388(1–2):203–10. 10.1007/s11010-013-1911-4 [DOI] [PubMed] [Google Scholar]
- 96. Rera M, Clark RI, Walker DW: Intestinal barrier dysfunction links metabolic and inflammatory markers of aging to death in Drosophila. Proc Natl Acad Sci U S A. 2012;109(52):21528–33. 10.1073/pnas.1215849110 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 97. Carratù R, Secondulfo M, de Magistris L, et al. : Altered intestinal permeability to mannitol in diabetes mellitus type I. J Pediatr Gastroenterol Nutr. 1999;28(3):264–9. 10.1097/00005176-199903000-00010 [DOI] [PubMed] [Google Scholar]
- 98. De Magistris L, Secondulfo M, Iafusco D, et al. : Altered mannitol absorption in diabetic children. Ital J Gastroenterol. 1996;28(6):367. [PubMed] [Google Scholar]
- 99. Sorini C, Cosorich I, Lo Conte M, et al. : Loss of gut barrier integrity triggers activation of islet-reactive T cells and autoimmune diabetes. Proc Natl Acad Sci U S A. 2019;116(30):15140–9. 10.1073/pnas.1814558116 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 100. Meddings JB, Jarand J, Urbanski SJ, et al. : Increased gastrointestinal permeability is an early lesion in the spontaneously diabetic BB rat. Am J Physiol. 1999;276(4):G951–7. 10.1152/ajpgi.1999.276.4.G951 [DOI] [PubMed] [Google Scholar]
- 101. Buhner S, Buning C, Genschel J, et al. : Genetic basis for increased intestinal permeability in families with Crohn's disease: role of CARD15 3020insC mutation? Gut. 2006;55(3):342–7. 10.1136/gut.2005.065557 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 102. Büning C, Geissler N, Prager M, et al. : Increased small intestinal permeability in ulcerative colitis: rather genetic than environmental and a risk factor for extensive disease? Inflamm Bowel Dis. 2012;18(10):1932–9. 10.1002/ibd.22909 [DOI] [PubMed] [Google Scholar]
- 103. Peeters M, Geypens B, Claus D, et al. : Clustering of increased small intestinal permeability in families with Crohn's disease. Gastroenterology. 1997;113(3):802–7. 10.1016/s0016-5085(97)70174-4 [DOI] [PubMed] [Google Scholar]
- 104. Teahon K, Smethurst P, Levi AJ, et al. : Intestinal permeability in patients with Crohn's disease and their first degree relatives. Gut. 1992;33(3):320–3. 10.1136/gut.33.3.320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Wyatt J, Vogelsang H, Hübl W, et al. : Intestinal permeability and the prediction of relapse in Crohn's disease. Lancet. 1993;341(8858):1437–9. 10.1016/0140-6736(93)90882-h [DOI] [PubMed] [Google Scholar]
- 106. Olszanecka-Glinianowicz M, Chudek J, Kocełak P, et al. : Body fat changes and activity of tumor necrosis factor α system--a 5-year follow-up study. Metabolism. 2011;60(4):531–6. 10.1016/j.metabol.2010.04.023 [DOI] [PubMed] [Google Scholar]
- 107. Olszanecka-Glinianowicz M, Zahorska-Markiewicz B, Janowska J, et al. : Serum concentrations of nitric oxide, tumor necrosis factor (TNF)-alpha and TNF soluble receptors in women with overweight and obesity. Metabolism. 2004;53(10):1268–73. 10.1016/j.metabol.2004.07.001 [DOI] [PubMed] [Google Scholar]
- 108. Zahorska-Markiewicz B, Janowska J, Olszanecka-Glinianowicz M, et al. : Serum concentrations of TNF-alpha and soluble TNF-alpha receptors in obesity. Int J Obes Relat Metab Disord. 2000;24(11):1392–5. 10.1038/sj.ijo.0801398 [DOI] [PubMed] [Google Scholar]
- 109. Linsalata M, Riezzo G, D’Attoma B, et al. : Noninvasive biomarkers of gut barrier function identify two subtypes of patients suffering from diarrhoea predominant-IBS: a case-control study. BMC Gastroenterol. 2018;18(1):167. 10.1186/s12876-018-0888-6 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 110. Singh P, Silvester J, Chen X, et al. : Serum zonulin is elevated in IBS and correlates with stool frequency in IBS-D. United European Gastroenterol J. 2019;7(5):709–15. 10.1177/2050640619826419 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 111. Bueno L: Protease activated receptor 2: a new target for IBS treatment. Eur Rev Med Pharmacol Sci. 2008;12 Suppl 1:95–102. [PubMed] [Google Scholar]
- 112. Wang X, Li Mm, Niu Y, et al. : Serum Zonulin in HBV-Associated Chronic Hepatitis, Liver Cirrhosis, and Hepatocellular Carcinoma. Dis Markers. 2019;2019:5945721. 10.1155/2019/5945721 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation