Abstract
Background
Certainly, there is a demand for stronger recognition of how nanoparticles can move through the cell membrane. Prostate cancer is one of the forcing sources of cancer-relevant deaths among men.
Aim of the Work
The current research studied the power of prostate cancer cells to uptake a ternary nanocomposite TNT/CuFe2O4/Zn-Fe mixed metal oxides (MMO).
Methodology
The nanocomposite was synthesized by a chemical method and characterized by a High-resolution transmission electron microscope, Field emission scanning electron microscope, X-ray diffraction, Fourier transmission infra-red, X-ray photoelectron spectroscopy, dynamic light scattering. Besides, it was implemented as an inorganic anticancer agent versus Prostate cancer PC-3 cells.
Results
The results revealed cellular uptake validity, cell viability reduction, ultra-structures alterations, morphological changes and membrane damage of PC-3 cells.
Conclusion
The prepared ternary nanocomposite was highly uptake by PC-3 cells and possessed cytotoxicity that was dose and time-dependent. To conclude, the study offered the potential of the investigated ternary nanocomposite as a promising prostate anticancer agent.
Keywords: cytotoxicity, inorganic nanomaterials, prostate cancer
Background
Investigations have indicated that 25% of men are diagnosed with prostate cancer (PCa).1 The clinical diagnostic approach is testing the prostate-specific antigen (PSA) level, where a concentration ˃ 4 ng/mL is considered a risk of biopsy.2 The routine diagnostic technique is the digital rectal examination, and Multi-parametric-magnetic resonance imaging allows the potential diagnosis of PCa.3 The distinct five stages of PCa are (zero) I, II, III, and IV,4 and most cases of prostate cancer metastasis develop in the lymph nodes and the bones.5 Choice of the treatment procedure, whatever surgery, radiation, hormone, Cryo-therapy, Vaccine, and Bone-directed treatment depends on the clinical stage, the age, and the general health of the individual.6
The potential complications of the mentioned approaches are serious to consider.7 The prostate size is the fundamental limitation of surgery, and 5 to 20% of cases suffer from stress incontinence after radical prostatectomy. Hormonal therapy leads to loss of libido, bone, and muscle mass.8 Further, 30 to 50% experience erectile dysfunction after radiation therapy,9 and urinary retention, urgency, and frequency are more common in Brachytherapy.10
Recent improvements in cancer nanomedicine have a significant consideration.11 In specific, metal and metal oxides inorganic nanoparticles (NPs) are substantial parts in the clinical progress of cancer diagnostic and therapy.12,13 For instance, Iron oxide NPs in Glioma,14 Graphite for Prostate,15 Gold in Cervical,16 Selenium/Ruthenium/copper for breast,17 Titanium peroxide with the pancreas, Platinum in the lung18 and Graphene in Non-small-cell lung carcinoma.19,20 Further, titanium dioxides TiO2 NPs have promising anticancer activities towards the breast21 and prostate.22,23 Besides, ferrites magnetic inorganic NPs are good anticancer agents, as Zinc,24,25 Nickel,26 Zinc-Nickel,27 Cobalt28 and super-paramagnetic iron oxide.29 Besides, the developed NPs target the PCa using aptamer, antibody30 and prostate-specific membrane antigen surface marker.31
However, the major drawback of inorganic NPs is their toxicity, which impairs the proteins, lipids, and DNA of the normal cell.32 In specific cases, inorganic NPs inhibit the cellular efflux pump by disturbing the Ca2+ concentration.33 So far, the researchers denoted the efficacy of inorganic NPs in cancer therapy, but the main limitation is the only concern at high concentration. Additionally, the issue of cell penetration, translocation and subsequent aggregation inside the cell, or in the cellular compartments is still a critical case.
Lately, nanostructures, such as ternary nanocomposites have potential usage in different fields since synergistic effects of their ingredients at the nanoscale domain may enhance the physical and chemical properties when compared to individual phases,34 for example, a novel sensitive photo-electrochemical ternary nanocomposite biosensor for glucose detection and sensing.35,36 Ternary nanocomposite films with different NPs exhibited superior chemical, thermal, mechanical properties, and electrochemical capacitance,37,38 a biocompatible nanocomposite of silver/gold alloy showed potential anticancer activities against liver cancer.39
To limit the cytotoxicity of the individual inorganic nanoparticles at high concentrations, the present research was planned to synthesis a ternary nanocomposite that constituted of titanate nanotubes/cupper ferrite/zinc-iron mixed metal oxides (MMO) (TNT/CuFe2O4/Zn-Fe MMO), in addition, to investigate how and to what extent the validity of prostate cancer cellular uptake in trial to achieve high efficacy with low concentration as an adequate anticancer inorganic agent versus PCa.
Materials and Methods
Materials
CuFe2O4 and Zn-Fe layered double hydroxides (LDH) were prepared using nitrate salts, Fe (NO3)3.9H2O (Alpha Chemika, India), Cu (NO3)2.3H2O (Alpha Chemika, India) and Zn (NO3)2.6H2O (Oxford Laboratory Reagent, India). Sodium hydroxide (NaOH) was purchased from Piochem for laboratory chemicals, Egypt, and hydrochloric acid (HCl) was obtained from Carlo Erba reagents. All chemicals were of reagent grade quality and used with no further purification.
Human prostate cancer PC-3 cell lines were obtained from the American-Type Culture Collection (ATCC, Rockville, MD). Mammalian cell lines: MRC-5 cells (Normal human Lung fibroblast cells) were acquired from VACSERA Tissue Culture Unit, Egypt. The used chemicals were Dimethyl sulfoxide (DMSO), MTT and trypan blue dyes were purchased from Sigma (St. Louis, Mo., USA). Fetal Bovine serum, DMEM, RPMI-1640, HEPES buffer solution, L-glutamine, gentamycin and 0.25% Trypsin-EDTA, Osmium tetroxide chemical fixes fat and sodium cacodylate buffer, Uranyl acetate staining, lead citrate phosphate-buffered saline (PBS), acetone, 4% of glutaraldehyde and 10% formalin were procured from Lonza (Belgium). Doxorubicin as a reference standard was taken from Sigma Aldrich.
Preparation of TNT/CuFe2O4/Zn-Fe MMO
Titanate nanotubes were formed in agreement with our preceding research with minor adjustments.32 Quickly, 10g of Anatase TiO2 powder was suspended in 500 mL of 10 M NaOH solution, transferred to a 1000 mL hydrothermal autoclave, and heated at 160°C for 23 hrs. TNT/CuFe2O4 with a 1:1 ratio was prepared using the co-precipitation approach. In the LDH phase, the molar ratio of Zn/Fe was 4:1.33 Originally, an aqueous solution of TNT was sonicated for 30 min in 4 M NaOH solution. Solutions of Cu2+ and Fe3+ were included drop-wise under vigorous stirring until a pH 10. The obtained precipitates were developed for 24 hrs at 70°C, filtered, washed with bi-distilled water several times, dried at 80°C overnight and calcined at 400°C for 2 hrs. To prepare the Zn-Fe MMO, the corresponding Zn-Fe LDH (1:1 by weight) was deposited over the surface of the TNT/CuFe2O4 phase through the co-precipitation of the corresponding Zn and Fe nitrate salts using sodium hydroxide as a precipitating agent. After precipitation, the powder was separated by centrifugation, washed several times and left to dry overnight at 40°C. Converting the LDH phase into the corresponding MMO was achieved through heating the dried samples at 200°C and left to cool naturally. Preparing MMO from the corresponding LDH phase is considered as a simple and economical procedure, which allows the MMO to keep the layered morphology of the original LDH phase after being heated.
Material Characterization
The prepared nanocomposite was characterized by high-resolution transmission electron microscopy HRTEM (JEOL-JEM 2100), field emission scanning electron microscopy FESEM (Gemini, 154 Zeiss-Ultra 55, field emission high-resolution scanning electron 155 microscope), X-ray diffraction XRD, X-ray photoelectron spectroscopy XPS (Thermo-Scientific k-Alpha), Zeta sizer and zeta potential (Malvern Instruments Ltd), Fourier transformation infrared spectroscopy FTIR (Vertex 70 FTIR-FT Raman) to study the microstructure, morphology, crystallinity, quantitative elemental composition chemical state, size distribution, surface potential and the functional groups, respectively.
Testing the Cellular Uptake by TEM
The PC-3 cells were shaken well and left intact for 20 hrs, the suspension was centrifuged down to a pellet and rinsed twice with PBS and then the samples were developed adopting standard practices for transmission electron microscopy (TEM), where post-fixation was carried out in 1% osmium tetroxide in cacodylate buffer at room temperature for 1 hr. The cells were dehydrated in acetone and buried in Epon resin. Ultrathin pieces were stained with Uranyl acetate and lead citrate and later probed with a TEM (70 kV GEOL GEM-1010) at the Regional Centre for Mycology and Biotechnology (RCMB), Egypt.
Morphological Analysis
Again, the investigated PC-3 cells were incubated at 37°C for 24 hrs. After that, the cells were soaked with PBS triplicates and were prefixed with 4% of glutaraldehyde solution for overnight and laved three times with 0.1 M sodium cacodylate buffer for 10 mins. The specimens were fixed in 1% of osmium tetroxide at 4oC for 2 hrs and washed plentiful with 0.1 M sodium cacodylate buffer for 10 mins. Subsequently, the specimens were dehydrated with a series of ethanol washes (30, 50, 70, 90, and 100%); critical point dried in CO2, coated with gold, and examined with a 20 kV JEOL JSM-5500LV Scanning Electron Microscope (SEM) at RCMB.
Viable Cell Counting (Trypan Blue Assay)
The treated PC-3 with the tested nanocomposite cells were separated using 0.25% trypsin for 10 mins, then 0.50 μL of PC-3 cell suspension was placed in a cryo-vial. An equal part of 0.4% trypan blue dye was added to the cell suspension to obtain a 1 to 2 and was mixed by pipetting up and down. The mixture was incubated at room temperature for 2 mins. Later, the cells were counted with an automated cell counter (TC10 Automated Cell Counter 145–0001; Bio-Rad Laboratories, Inc., Hercules, CA, USA). The percentage of viable cells was calculated by dividing the number of viable cells by the number of total cells and multiplying by 100 or % viable cells = [1.00 – (Number of blue cells ÷ Number of total cells)] × 100.40
Antitumor Activity Assay
The procedures followed.41 First, the PC-3 cells were cultivated on RPMI-1640 medium supplemented with 10% inactivated fetal calf serum and 50 µg/mL gentamycin, kept at 37 ºC in a moistened environment with 5% CO2 and sub-cultured three times a week. For cytotoxicity evaluation using viability assay, the PC-3 cells were suspended in a medium in Corning® 96-well tissue culture plate with a concentration 5x104 cell/well and then incubated for 24 hrs. Second, sequential double-fold dilutions of the tested nanocomposite were included in a 96-well plate (three repeats). Six vehicles with media 0.5% DMSO were run as a control (untreated with the investigated nanocomposite). After incubating for 24 hrs, the numbers of viable cells were detected by the MTT test.
Shortly, the media was expelled from the well plate and recovered with 100 µL of pure culture RPMI 1640 medium, and 10 µL of the 12 mM MTT stock solution (5 mg of MTT in 1 mL of PBS) were added to each well including control and was incubated further at 37°C and 5% CO2 for 4 hrs. Finally, an 85 µL aliquot of the media was removed from the wells, and 50 µL of DMSO was included to each well and mixed thoroughly with the pipette and incubated at 37°C for 10 mins.
The optical density was measured at 590 nm with the microplate reader (SunRise, TECAN, Inc, USA) to detect the total viable cells. The percent of viability was calculated as [(ODt/ODc)] x100% where ODt is the mean optical density of treated wells and ODc is that of untreated cells. The experiments and measures were conducted three times, and the results were presented as the average±Standard Deviation. The relationship between tested nanocomposite versus inhibitory and viability percent was plotted in a bar chart using Graphpad Prism software (San Diego, CA. USA), and the 50% inhibitory concentration (IC50), which is the concentration required to cause toxic effects in 50% of intact cells was determined. The cytotoxicity of the tested nanocomposite was assessed against Mammalian cell lines: MRC-5 cells (Normal human Lung fibroblast cells). In addition, the efficacy of the tested nanocomposite was compared with a standard Doxorubicin.
Results and Discussion
Material Characterization
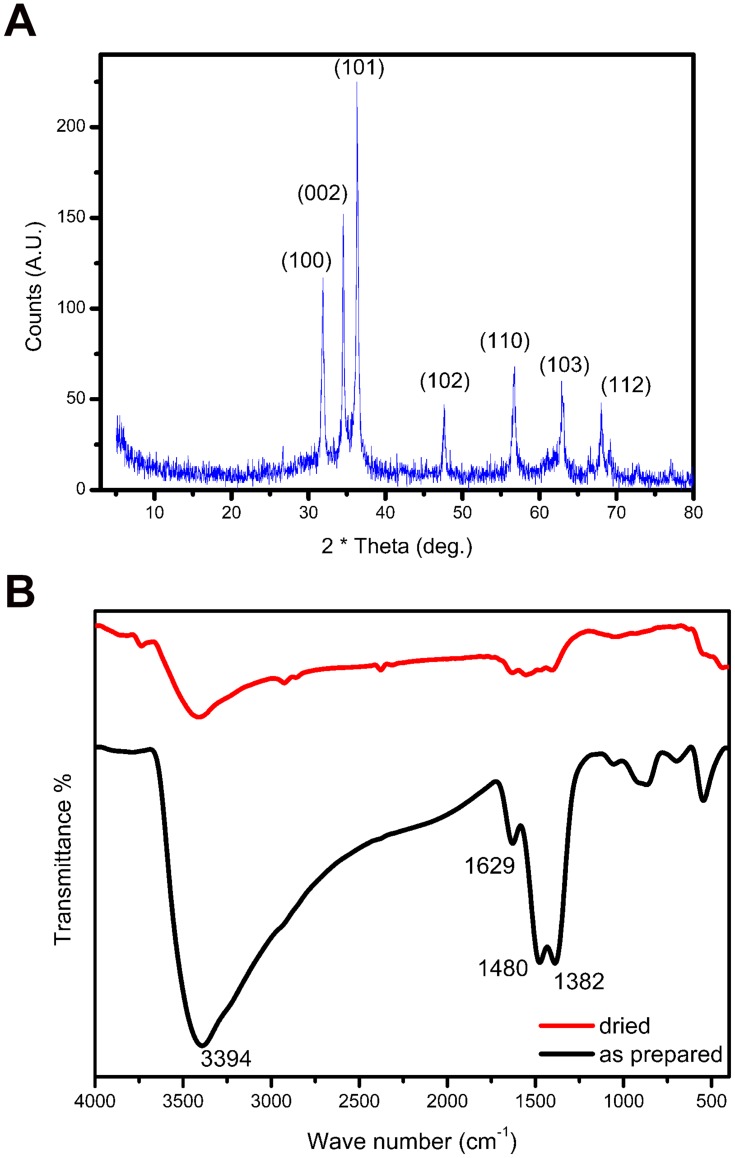
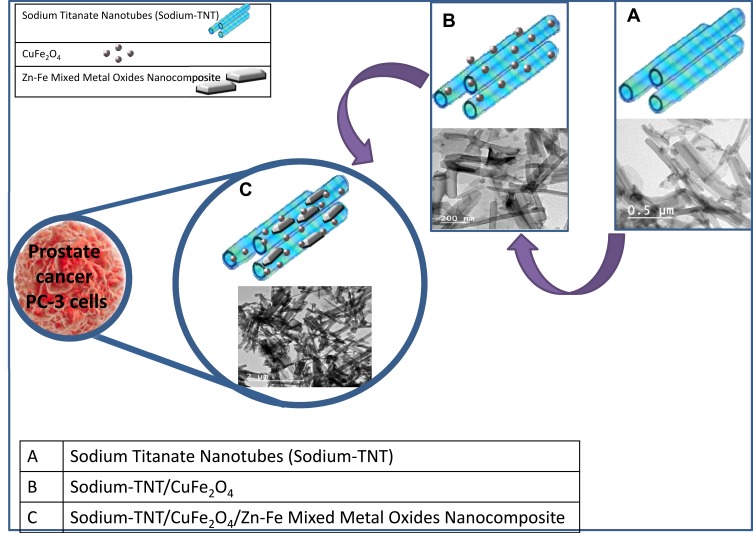
Figure 1A displays the X-ray diffraction (XRD) of the studied nanocomposite. The sharp peaks at 31.89°, 34.5°, 36.3°, 47.61°, 56.6o, 62.9°, and 68o are characteristic peaks for the (100) (002) (101) (102) (110) (103) and (112) planes, respectively, and well matched with (ICDD card number: 01-070-2551). Mild heating of the LDH phase formed the corresponding MMO of ZnO as a dominant phase with the trivalent Fe+3 cations those uniformly distributed in the oxide network. ZnFe2O4 phase was absent; its detection required heating at 600°C.42 Besides, the peaks at 31.89°, 34.5°, 36.3° and 62.9° reflected the diffraction peaks of the CuF2O4 phase (112) (103) (211) and (224) planes, respectively.43 The diffraction peak of the titanate phase was low intensities compared with the MMO and ferrite phases and could not be observed in the XRD diffractogram. The structure of the nanocomposite is further illustrated in Scheme 1.
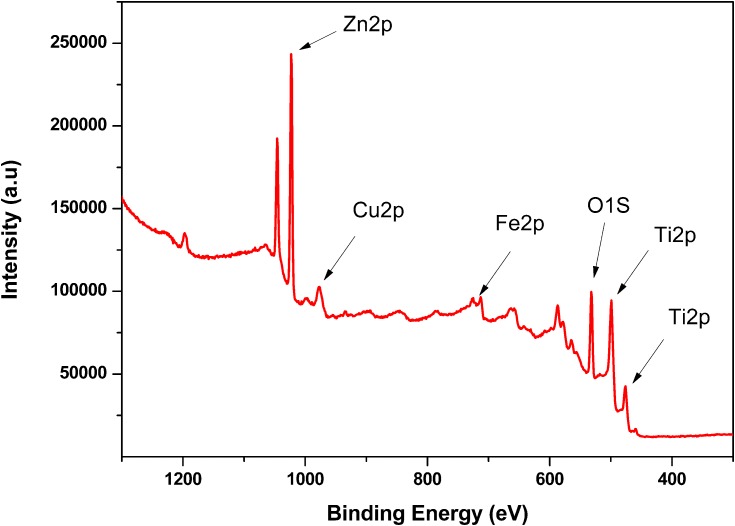
Figure 2.
XPS spectrum of titanate nanotubes/CuFe2O4/Zn-Fe MMO.
Figure 1.
(A) XRD pattern of the prepared ternary nanocomposite, (B) FTIR pattern of the prepared ternary nanocomposite.
Scheme 1.
Possible structure of the ternary nanocomposite.
Figure 1B indicates the FTIR range of the synthesized nanocomposite. The absorption peaks at 3394 cm−1 and 1629 cm−1 illustrates the OH stretching and bending, respectively, because of the adsorbed water molecules44 while the those at 1382 cm−1 and 1480 cm−1 assigned to the ν3 stretching vibration of the NO345 and carbonate46 groups, and the peaks at the low wave number attributed to the metal-oxygen bond absorption.47
X-ray photoelectron spectroscopy was performed to confirm the ingredients elemental composition of the prepared ternary nanocomposite and to determine its oxidation state. Figure 2 presents the XPS spectrum of the inorganic nanomaterials forming the ternary nanocomposite. Overall, XPS results evidenced that all the ingredients were in oxide form rather than in metallic one. The spectrum emphasizes Cu+2, Fe+3, Zn+2 and Ti+4 originating from the CuFe2O4, mixed metal oxide (Zn-Fe) and titanate phase, respectively. The Figure clarifies different peaks of various oxidation states at distinct binding energy levels; the peak of Fe 2p was detected at the binding energy 712 and 725 eV confirming the +3 oxidation state of iron and matched with the preceded study.48 The peaks at 1022.7 and 1044.72 eV attribute to the +2 oxidation state of (ZnO), similar to another research.49,53 The peak of Cu 2p appears at 932 eV specifies to Cu2+ while peaks of Ti 2p assign to Ti4+.50,54,55
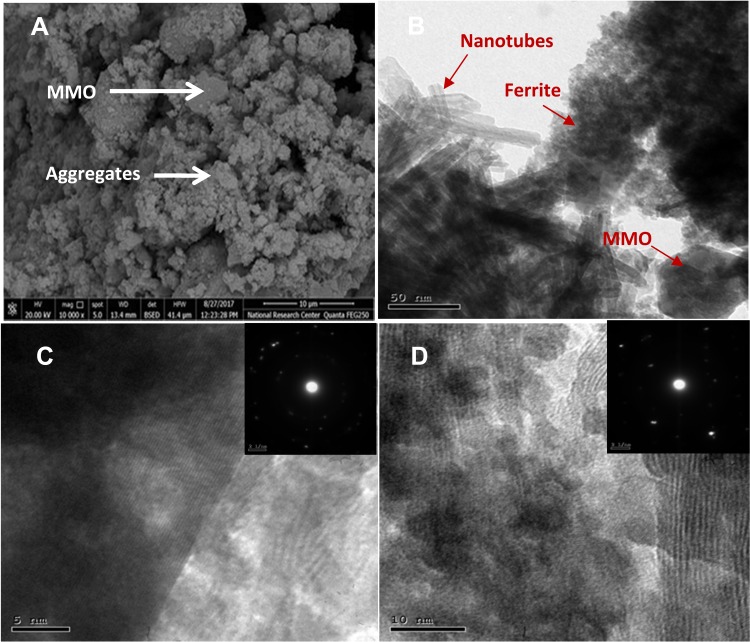
Figure 3A shows the SEM micrograph of the prepared nanocomposite; two morphologies appeared as a layered morphology of Zn-Fe MMO and fine aggregates that originated from the titanate and ferrite phases. Figure 3B is a TEM image indicating all three phases as titanate nanotubes decorated by CuFe2O4 and layered Zn-Fe MMO as illustrated in Scheme 1. TNTs have an average diameter ranging between 10–15 nm. Figure 3C reveals the formed-walls of the TNTs.
Figure 3.
(A) FESEM and (B) TEM micrographs of the prepared nanocomposite. (C) HRTEM micrograph of the TNTs phase (inset: SAED pattern) and (D) HRTEM image of the ferrite phase (inset: SAED pattern).
In the inset image (selected area electron diffraction SAED), the bright spots confirmed an accepted crystallinity of the TNTs phase. Figure 3B displays a hexagonal symmetry of the MMO layers with an edge-to-edge distance of 60 nm. Figure 3D shows fine and well-dispersed CuFe2O4 spheres with diameters less than 10 nm, and inset reflected a good crystallinity of the ferrite phase.
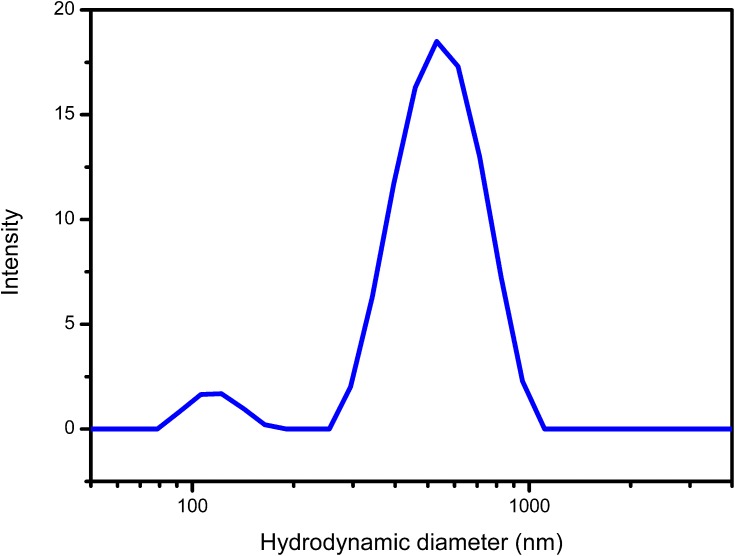
Figure 4 reveals the hydrodynamic size distribution of the prepared nanocomposite and showed two peaks at 117.7 nm and 557.4 nm, which attributed to the aggregates and layered morphologies, respectively. The reported poly distribution index PDI was 0.54 that reflected the heterogeneous distribution of the tested nanocomposite, as expected. The particles’ tendency to form aggregates or dispersed depends on the surface charge; the calculated zeta potential was −26.4 mV indicating incipient stability.
Figure 4.
Hydrodynamic size distribution of the prepared ternary nanocomposite.
Cellular Uptake
Indeed, the cellular entry of nanoparticles and their ulterior interaction with the cell’s internal structure, together with the power to envisage cultures of nanoparticles at high resolution within cells is a crucial point to infer the processes of any toxicity. It has evidenced that the imaging-based devices are worthy of investigating the nanoparticle-cell actions; the current study used electron-based imaging techniques to recognize the cellular uptake of the investigated nanocomposite.
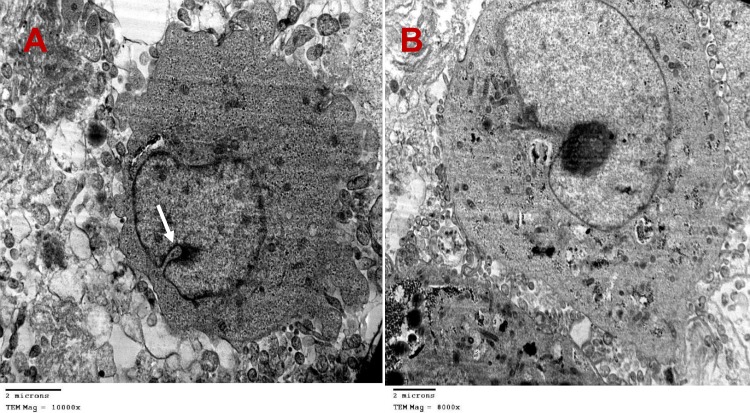
Figure 5 gives information about two different TEM images of the prostate cancer cells after incubation with the tested nanocomposite at two distinct times (a) after 24 hrs and (b) after 48 hrs. The figure proves a variation nanocomposite distribution in the extracellular and intracellular matrix, as well as in the degree of the cellular uptake. The image of Figure 5 (a) displays a lot of vacuoles and the distributed nanocomposite in the extracellular regions, also, external attachment to the cell membrane, and dissemination of the nanoparticles in the cytoplasm.
Figure 5.
Different TEM images of the PC-3 cells after incubation with the tested nanocomposite materials (IC50 = 29.8 ± 0.6 µg/mL), (A) after 24 hrs at 10,000× magnification, (B) after 48 h at 8000× magnification.
Determining the entrance mechanism is paramount; when NPs come to the surface membrane of a cell, they can connect with its ingredients or extracellular matrix, and penetrate the cell through endocytosis. Five main precise processes of endocytosis are phagocytosis, clathrin-mediated endocytosis (CME), caveolin-mediated endocytosis, clathrin/caveolae-independent endocytosis, and macro-pinocytosis.
Based on the theory of each method; the entrance pathway of the studied nanocomposite into the cells may be through Phagocytosis or CME. The first approach was not expected for reasons; Phagocytosis exists primarily in professional phagocytes as macrophages, monocytes, neutrophils, and dendritic cells that were nonexistent in the incubation media. In addition, Phagocytosis of NPs is mostly initiated by the Opsonization process, where opsonins such as immunoglobulins, complement proteins, and other blood proteins are adsorbed onto the NPs’ surface;51 these opsonins did not exist also. Further, larger micro-particles experience more efficient uptake by phagocytes while the tested composite was in nano-dimension.
Concerning the second approach, Clathrin-mediated endocytosis occurs either via receptor-specific uptake or by non-specific adsorptive uptake, which is referred to as receptor-independent CME. In receptor-independent CME, the uptake takes place without direct binding with membrane constituents through non-specific hydrophobic molecules or electrostatic interactions that initiate the uptake.
It is important to bear in mind that the surface charge has a powerful effect on the receptor-independent CME uptake mechanism and intracellular fate. For example, anionic particles showed cellular uptake in HeLa cervical cancer cells and silica nanotubes (SNTs).51 Taken into consideration the surface charge, the prepared nanocomposite bore negative charges that indicated by the zeta potential value. And as such, the suggested entrance mechanism was through electrostatic interaction between CuFe2O4/Zn-Fe and the phosphate group of the cell membrane lipid layers that caused disruption of the cell membrane integrity, created pores that boosted the entrance of TNT, and developed a tight pit on the inner surface of the plasma membrane; this pit then buds into the cell to complete a covered vesicle in the cytoplasm. The white arrow in Figure 5 illustrated the coated pits and vesicles budding in the cell’s cytoplasm, these covered pits and vesicles budding developed steadily by time after 48 hrs of incubation as presented in Figure 5B, which in turn reflected that the distributed nanocomposite in the cytoplasm indented to accumulate around the nuclear membrane, and it needed more 48 hrs of incubation to invade the nuclear envelope. In light of forgoing, the receptor-independent CME mode was the suggested mechanism of invasion and cellular uptake.
Cellular Morphological Changes
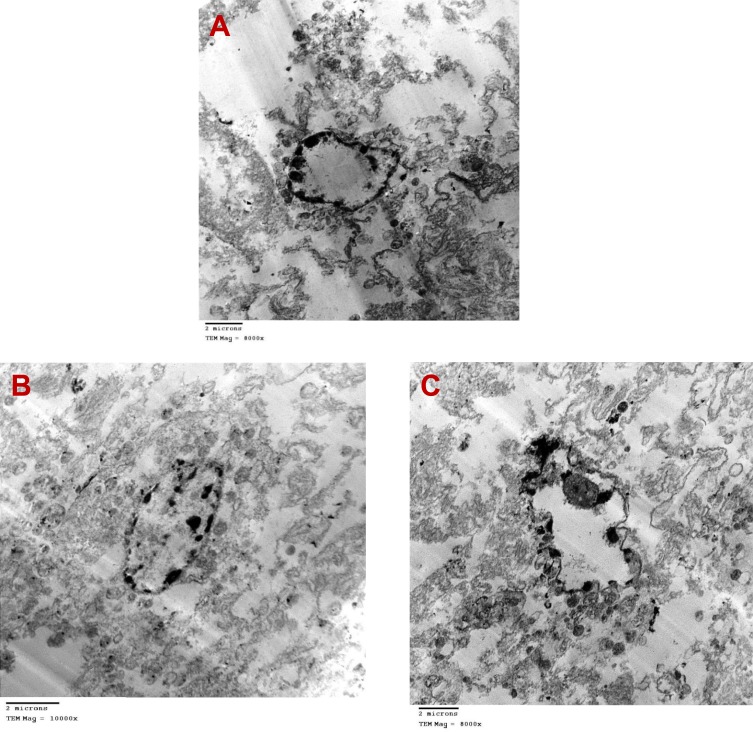
Figure 6 provides three TEM images (a, b &c) after 48 hrs of incubation. Overall, it confirmed factual details of the ultra-structural reforms of the PC-3 cells. For example, Figure 6A exhibits a heap of the nanocomposite at the internal wall of the cell membrane face to the cytoplasm. Additionally, the figure represented an alteration of the cell shape and the cell membrane with a slight elongation of the cell. This protraction increased gradually by time as confirmed in Figure 6B, and the piles of the nanocomposite still spread in the cytoplasm. Moreover, Figure 6C illustrates a sinuosity of the cell membrane; this tortuosity may increase the permeability of the membrane. Increasing permeability occurs in the cells that passed the death mechanism whatever by apoptosis or necrosis. The turban blue sassy emphasized the increased permeability. Further, the cytoplasm appeared clear in Figure 6C, reflecting the effect of the nanocomposite on the different organelles in the cytoplasm.
Figure 6.
Accurate details of the ultra-structural changes of the PC-3 treated cells with the tested nanocomposites materials (IC50 = 29.8 ± 0.6 µg/mL) after 48 hrs of incubation, (A) at 8000× magnification, (B) at 10,000× magnification and (C) at 8000× magnification.
Although the TEM reveals the intracellular distribution of the nanomaterial; nevertheless, but the quantification of the internalized nanomaterials is of fundamental concern. Up to date, there is no standardized and validated method available for this specific question because of different needs of the analytical methods depend on the particle type, the biological environment as well as the various specifications and limitations for each of the techniques.
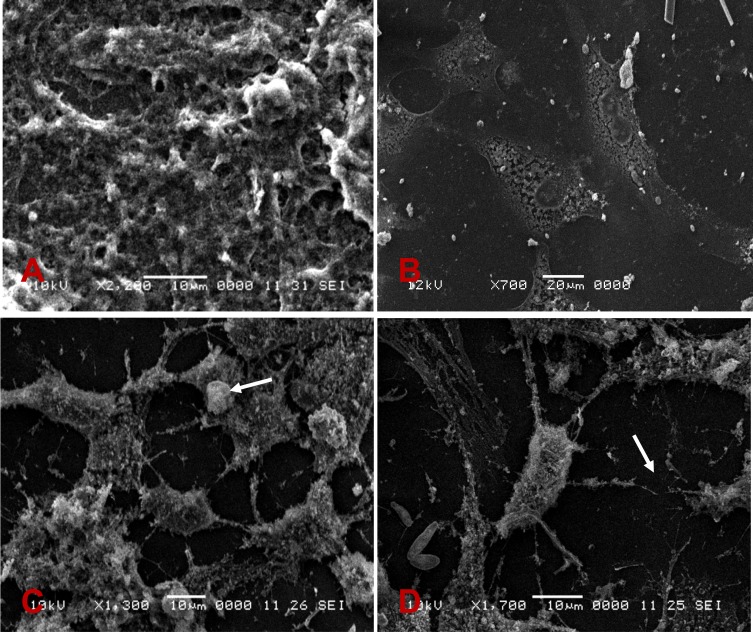
Ultimately, Figure 7 reviews four SEM images of the PC-3 cells (a, b, c & d) with different magnifications, where (a & b) without nanocomposite incubation, while (c &d) with incubation. Overall, Figure 7 describes the morphological alterations provoked by the tested nanocomposite on the PC-3 cells. Figure 7A with a large field of view paraded clusters of well-united and condensed PC-3, and revealed non-consistency grid of collagen fibers that reinforced the PC-3 cells and have a substantial part in prostate growth management. On the other hand, Figure 7B with a small and focused field of view exhibited PC-3 cells with a precise and uniform shape with a distinct cytoplasm.
Figure 7.
SEM images identify possible morphological alterations caused by the tested nanomaterials on the PC-3 cells. The white arrows refer to a concise cytoplasm and a wide cell-free zone of the treated PC-3 cells.
Regarding the treated PC-3 cells, the image of 7C exhibited a concise cytoplasm (white arrow). Moreover, Figure 7D manifests separate cells and cracker structures, leaving wide cell-free zones that illustrated in the figure as large dark signal intensity spaces (white arrows). In addition, it showed a non-uniform swelling with a fall of fragmentation of collagen tissue, in contrast, the collagen network was intensive with an increased number of fibers in non-treated PC-3 cells, as shown in Figure 7A. It is conceivable that a fraction of the proteins of the connective tissue was ruined during the incubation with the questioned nanocomposite. The morphological analysis by SEM proved variations in the basic connective tissue Stroma (which represents the principal component comprising 54% of the prostate gland), including swelling, fragmentation, and loss of collagen. The presented results were well matched with preceded study.52
Cytotoxic Assay
To confirm the implication of the inward nanocomposite; the cytotoxic effect of the tested nanocomposite versus PC-3 was investigated by the Trypan Blue dye exclusion test, which is used to determine the number of viable cells present in a cell suspension. The test is based on the principle that living cells possess intact cell membranes that exclude Trypan Blue dye, whereas Trypan Blue stain can pass through only permeable membranes of the deceased cells, altering their color into blue, which is noticeable under optical microscopy. The treated PC-3 cell suspension with the nanocomposite was mixed with the Trypan Blue dye and visually examined to determine whether cells take up or exclude dye. The cytoplasm of the treated PC-3 cells was stained by blue color while that of viable cells was clear. Overall, the incubated cell lines with the medium involving the ternary nanocomposite showed a substantial rebate in the number of viable cell contrast to the control group (p<0.05).
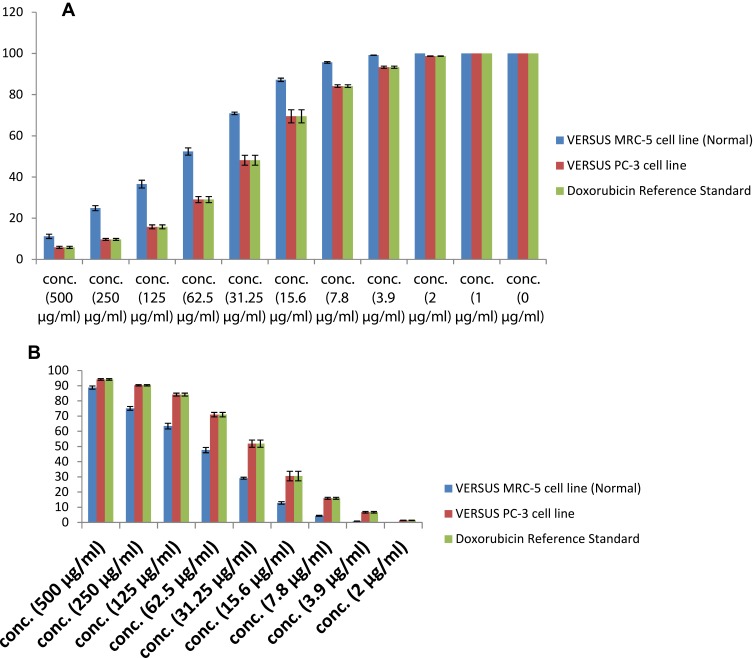
Further, Figure 8 illustrates the statistical analysis bar chart of the MTT assay measurements. Figure 8A shows the viability percent (vertical axis) of the PC-3 and MRC-5 cell line (Normal) versus the tested nanocomposite and a standard chemotherapy agent (Doxorubicin) with serial dilutions (horizontal axis). The viability percent was measured for each concentration, and the data were reported as an average ± Standard Deviation. Overall, the viability percent of the treated cells (PC-3 and MRC-5) decreased with the increase of the concentration. The lowest percent was at the maximum concentration (500ug/mL). It was below 5% of Doxorubicin and closed to 5% of the nanocomposite while the viability of the normal cells was approximately 10%. The viability of the treated PC-3 by Doxorubicin reduced rapidly while those treated by the ternary nanocomposite lessened consistently at low concentration and suddenly diminished at high concentration. The cytotoxic effect of the nanocomposite on the normal MRC-5 appeared obviously at high concentrations. On the other hand, Figure 8B is a chart clarifies the inhibitory percent of the treated cell at the same concentrations, the IC50% of the nanocomposite against PC-3 and MRC-5 was 29.8 ± 0.6 µg/mL and 71.9 ± 2.5 µg/mL, respectively, while IC50% of Doxorubicin versus PC-3 was 3.68 ± 0.2 µg/mL.
Figure 8.
The statistical analysis of the MTT assay, (A) the viability and (B) inhibitory percent of the PC-3 and MRC-5 cell line (Normal) cells treated by ternary nanocomposites and standard chemotherapy agent (Doxorubicin).
The future work of the current research will focus on twofold: performing other assays to indicate the efficiency of the tested ternary nanocomposite against specific organelles of the PC-3 cells to scout the toxicity pathways, to study the alteration in the hormonal order, to investigate special growth factors and activity of specific enzymes that affects the regulation of the PC-3 growth, and to rebate the main ingredient of the ternary nanocomposite that activate the cytotoxicity of the PC-3 cells meticulously.
To conclude, the safe treatment of inorganic NPs persists a crucial question, and many warrants are still recommended. Furthermore, recognizing the interactions of NPs with cells and how the entrance influences their cellular uptake is essential. Consequently, to limit the cytotoxicity of the individual NPs at high concentrations; the current study presented the ternary nanocomposite TNT/CuFe2O4/Zn-Fe MMO, investigated the cellular uptake versus PC-3, proposed the receptor-independent CME as an entrance mechanism, showed the intracellular distribution of the tested nanocomposite, reported a distinct alteration in the morphology and ultrastructure of the PC-3, as well as a potential toxicity of the tested ternary nanocomposite that was dose and time-dependent, which reflected a high cellular uptake. In the final, the current study suggests the capability of the tested ternary nanocomposite as a promising prostate anticancer agent.
Acknowledgments
The authors are thankful to all members at Materials Science and Nanotechnology Dept., Faculty of Postgraduate Studies for Advanced Sciences (PSAS), Beni-Suef University Egypt for supporting preparation of the nanomaterials. Also, all members at Central Lab for Characterization and Statistical unite at 57357 Children Cancer Hospital, Egypt.
Abbreviations
PCa, Prostate Cancer; MMO, Mixed Metal Oxides; LDH, Layered double hydroxide; PSA, Prostate-Specific Antigen; DRE, Digital Rectal Examination; mp-MRI, Multiparametric-magnetic resonance imaging; PSMA, Prostate-Specific Membrane Antigen; M6PR, Mannose 6-phosphate receptor; DTX, Docetaxel; TPGS, Tocopheryl polyethylene glycol succinate; CUR, DTX-curcumin; NPs, Nanoparticles; DNA, Deoxyribonucleic acid; DMSO, Dimethyl sulfoxide; PBS, Phosphate Buffered Saline; TNT, Titanate nanotubes; FESEM, Field Emission Scanning Electron Microscopy; IC50, Inhibitory concentration; TEM, Transmission Electron Microscopy; RCMB, Regional Centre for Mycology and Biotechnology; SEM, Scanning Electron Microscope; XRD, X ray Diffraction; FTIR, Fourier transformation infra-red; SAED, Selected Area Electron Diffraction; ROS, Reactive Oxygen Species.
Ethics Approval and Consent to Participate
The authors followed the ethics of research, approved and consented to participate in this study.
Consent for Publication
The authors consent this manuscript for publication.
Data Sharing Statement
The authors emphasize the availability of data and materials.
Author Contributions
Dr. Elshahawy conceived the idea for biomedical application, Dr. A.H. Zaki, Dr. Nada A. Mohamed, Dr. Yasser GadelHak, Dr. S. A. Abdelmoaty Dr. R.K. Mahmoud, and Dr. A A Farghali participated in the study design. Dr. Elshahawy conducted the bio-section, analyzed and interpreted the data. Dr. A.H. Zaki, Dr, Dr. S. A. Abdelmoaty, Dr. R.K. Mahmoud and Dr. A A Farghali prepared the materials. Dr. Yasser GadelHak investigated and Nada A. Mohamed and Dr. R.K. Mahmoud characterized the prepared materials. The authors wrote and revised the manuscript. All the authors approved the final version to be published, and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Disclosure
The authors confirm no competing interests in this work.
References
- 1.Thompson B, Khan S. Aging men and prostate cancer. J Reproduktionsmedizin und Endokrinol Reprod Med Endocrinol. 2016;12:396–398. [Google Scholar]
- 2.Adhyam M, Gupta AK. A review on the clinical utility of PSA in cancer prostate. Indian J Surg Oncol. 2012;3:120–129. doi: 10.1007/s13193-012-0142-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sidhu HS, Benigno S, Ganeshan B, et al. Textural analysis of multiparametric MRI detects transition zone prostate cancer. Eur Radiol. 2017;27:2348–2358. doi: 10.1007/s00330-016-4579-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Patel KM, Gnanapragasam VJ. Novel concepts for risk stratification in prostate cancer. J Clin Urol. 2016;9:18–23. doi: 10.1177/2051415816673502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chen CP, Roach M, Kased N, et al. Management of prostate cancer patients with lymph node involvement: a rapidly evolving paradigm. Cancer Treat Rev. 2012;38:956–967. doi: 10.1016/j.ctrv.2012.05.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lakshmanan V-K. Therapeutic efficacy of nanomedicines for prostate cancer: an update. Investig Clin Urol. 2016;57:21–29. doi: 10.4111/icu.2016.57.1.21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chen Z, Penet M-F, Nimmagadda S, et al. PSMA-targeted theranostic nanoplex for prostate cancer therapy. ACS Nano. 2012;6:7752–7762. doi: 10.1021/nn301725w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Saad F, Aversa A, Isidori AM, et al. Onset of effects of testosterone treatment and time span until maximum effects are achieved. Eur J Endocrinol. 2011;165:675–685. doi: 10.1530/EJE-11-0221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pettus JA, Masterson T, Sokol A, et al. Prostate size is associated with surgical difficulty but not functional outcome at 1 year after radical prostatectomy. J Urol. 2009;182:949–955. doi: 10.1016/j.juro.2009.05.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kragelj B. Obstructive urination problems after high-dose-rate brachytherapy boost treatment for prostate cancer are avoidable. Radiol Oncol. 2016;50:94–103. doi: 10.1515/raon-2015-0010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shi J, Kantoff PW, Wooster R, Farokhzad OC. Cancer nanomedicine: progress, challenges and opportunities. Nat Rev Cancer. 2017;17:20. doi: 10.1038/nrc.2016.108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jiao M, Zhang P, Meng J, et al. Recent advancements in biocompatible inorganic nanoparticles towards biomedical applications. Biomater Sci. 2018;6:726–745. doi: 10.1039/C7BM01020F [DOI] [PubMed] [Google Scholar]
- 13.Bhattacharyya S, Kudgus RA, Bhattacharya R, Mukherjee P. Inorganic nanoparticles in cancer therapy. Pharm Res. 2011;28:237–259. doi: 10.1007/s11095-010-0318-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Silva AC, Oliveira TR, Mamani JB, et al. Application of hyperthermia induced by superparamagnetic iron oxide nanoparticles in glioma treatment. Int J Nanomedicine. 2011;6:591–603. doi: 10.2147/IJN.S14737 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ishikawa H, Tsuji H, Kamada T, et al. Carbon ion radiation therapy for prostate cancer. Int J Urol. 2012;19:296–305. doi: 10.1111/iju.2012.19.issue-4 [DOI] [PubMed] [Google Scholar]
- 16.Daduang J, Palasap A, Daduang S, et al. Gallic acid enhancement of gold nanoparticle anticancer activity in cervical cancer cells. Asian Pac J Cancer Prev. 2015;16:169–174. doi: 10.7314/APJCP.2015.16.1.169 [DOI] [PubMed] [Google Scholar]
- 17.Liao W, Yu Z, Lin Z, et al. Biofunctionalization of selenium nanoparticle with dictyophora indusiata polysaccharide and its antiproliferative activity through death-receptor and mitochondria-mediated apoptotic pathways. Sci Rep. 2015;5:18629. doi: 10.1038/srep18629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nakayama M, Sasaki R, Ogino C, et al. Titanium peroxide nanoparticles enhanced cytotoxic effects of X-ray irradiation against pancreatic cancer model through reactive oxygen species generation in vitro and in vivo. Radiat Oncol. 2016;11:91. doi: 10.1186/s13014-016-0666-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Patel SC, Lee S, Lalwani G, et al. Graphene-based platforms for cancer therapeutics. Ther Deliv. 2016;7:101–116. doi: 10.4155/tde.15.93 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Akhtar MJ, Ahamed M, Alhadlaq HA. Therapeutic targets in the selective killing of cancer cells by nanomaterials. Clin Chim Acta. 2017;469:53–62. doi: 10.1016/j.cca.2017.03.020 [DOI] [PubMed] [Google Scholar]
- 21.Sree Latha T, Reddy MC, Muthukonda SV, et al. In vitro and in vivo evaluation of anti-cancer activity: shape-dependent properties of TiO2nanostructures. Mater Sci Eng C. 2017;78:969–977. doi: 10.1016/j.msec.2017.04.011 [DOI] [PubMed] [Google Scholar]
- 22.Thurn KT, Arora H, Paunesku T, et al. Endocytosis of titanium dioxide nanoparticles in prostate cancer PC-3M cells. Nanomed Nanotechnol Biol Med. 2011;7:123–130. doi: 10.1016/j.nano.2010.09.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Thevenot P, Cho J, Wavhal D, et al. Surface chemistry influences cancer killing effect of TiO2 nanoparticles. Nanomed Nanotechnol Biol Med. 2008;4:226–236. doi: 10.1016/j.nano.2008.04.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mohammed L, Gomaa HG, Ragab D, Zhu J. Magnetic nanoparticles for environmental and biomedical applications: a review. Particuology. 2017;30:1–14. doi: 10.1016/j.partic.2016.06.001 [DOI] [Google Scholar]
- 25.Pan UN, Sanpui P, Paul A, Chattopadhyay A. Surface complexed-zinc ferrite magnetofluorescent nanoparticles for killing cancer cells and single particle level cellular imaging. ACS Appl Nano Mater. 2018;1:2496–2502. doi: 10.1021/acsanm.8b00545 [DOI] [PubMed] [Google Scholar]
- 26.Sun L, Xie S, Qi J, et al. Cell-permeable, MMP-2 activatable, nickel ferrite and his-tagged fusion protein self-assembled fluorescent nanoprobe for tumor magnetic-targeting and imaging. ACS Appl Mater Interfaces. 2017;9:39209–39222. doi: 10.1021/acsami.7b12918 [DOI] [PubMed] [Google Scholar]
- 27.Al-Qubaisi MS, Rasedee A, Flaifel MH, et al. Cytotoxicity of nickel zinc ferrite nanoparticles on cancer cells of epithelial origin. Int J Nanomedicine. 2013;8:2497. doi: 10.2147/IJN.S42367 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lojk J, Bregar VB, Strojan K, et al. Increased endocytosis of magnetic nanoparticles into cancerous urothelial cells versus normal urothelial cells. Histochem Cell Biol. 2018;149:45–59. doi: 10.1007/s00418-017-1605-1 [DOI] [PubMed] [Google Scholar]
- 29.Ding C, Wu K, Wang W, et al. Synthesis of a cell penetrating peptide modified superparamagnetic iron oxide and MRI detection of bladder cancer. Oncotarget. 2016;8:4718–4729. doi: 10.18632/oncotarget.13578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Friedman D, Claypool, S AE, Liu R. The smart targeting of nanoparticles. Curr Pharm Des. 2013;19:6315–6329. doi: 10.2174/13816128113199990375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lee SS, Roche PJ, Giannopoulos PN, et al. Prostate-specific membrane antigen–directed nanoparticle targeting for extreme nearfield ablation of prostate cancer cells. Tumour Biol. 2017;39:101042831769594. doi: 10.1177/1010428317695943 [DOI] [PubMed] [Google Scholar]
- 32.Zaki AM, Zaki AH, Farghali AA, Abdel-Rahim EF. Sodium titanate-bacillus as a new nanopesticide for cotton leaf-worm. J Pure Appl Microbiol. 2017;11:725–733. doi: 10.22207/JPAM.11.2.11 [DOI] [Google Scholar]
- 33.Moaty SAA, Farghali AA, Moussa M, Khaled R. Remediation of waste water by Co–Fe layered double hydroxide and its catalytic activity. J Taiwan Inst Chem Eng. 2017;71:441–453. doi: 10.1016/j.jtice.2016.12.001 [DOI] [Google Scholar]
- 34.Ali A, Ahmed S. A review on chitosan and its nanocomposites in drug delivery. Int J Biol Macromol. 2018;109:273–286. doi: 10.1016/j.ijbiomac.2017.12.078 [DOI] [PubMed] [Google Scholar]
- 35.Wang Y, Bai L, Wang Y, et al. Ternary nanocomposites of Au/CuS/TiO 2 for an ultrasensitive photoelectrochemical non-enzymatic glucose sensor. Analyst. 2018;143:1699–1704. doi: 10.1039/C8AN00187A [DOI] [PubMed] [Google Scholar]
- 36.Silva CHB, Iliut M, Muryn C, et al. Ternary nanocomposites of reduced graphene oxide, polyaniline and hexaniobate: hierarchical architecture and high polaron formation. Beilstein J Nanotechnol. 2018;9:2936–2946. doi: 10.3762/bjnano.9.272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kumar SV, George J, Sajeevkumar VA. PVA based ternary nanocomposites with enhanced properties prepared by using a combination of rice starch nanocrystals and silver nanoparticles. J Polym Environ. 2018;26:3117–3127. doi: 10.1007/s10924-018-1200-0 [DOI] [Google Scholar]
- 38.Zhang R, Liao Y, Ye S, et al. Novel ternary nanocomposites of MWCNTs/PANI/MoS 2: preparation, characterization and enhanced electrochemical capacitance. R Soc Open Sci. 2018;5:171365. doi: 10.1098/rsos.171365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Shanmugasundaram T, Radhakrishnan M, Gopikrishnan V, et al. Biocompatible silver, gold and silver/gold alloy nanoparticles for enhanced cancer therapy: in vitro and in vivo perspectives. Nanoscale. 2017;9:16773–16790. doi: 10.1039/C7NR04979J [DOI] [PubMed] [Google Scholar]
- 40.Basso FG, Pansani TN, Oliveira CFD, et al. Cytotoxic effects of zoledronic acid on human epithelial cells and gingival fibroblasts. Braz Dent J. 2013;24:551–558. doi: 10.1590/0103-6440201302229 [DOI] [PubMed] [Google Scholar]
- 41.Gomha SM, Riyadh SM, Mahmmoud EA, Elaasser MM. Synthesis and anticancer activities of thiazoles, 1, 3-thiazines, and thiazolidine using chitosan-grafted-poly (vinylpyridine) as basic catalyst. Heterocycl Int J Rev Commun Heterocycl Chem. 2015;91:1227–1243. [Google Scholar]
- 42.Di G, Zhu Z, Zhang H, et al. Simultaneous removal of several pharmaceuticals and arsenic on Zn-Fe mixed metal oxides: combination of photocatalysis and adsorption. Chem Eng J. 2017;328:141–151. doi: 10.1016/j.cej.2017.06.112 [DOI] [Google Scholar]
- 43.Ahmed MA, Okasha N, Mansour SF, El-Dek SI. Bi-modal improvement of the physico-chemical characteristics of PEG and MFe2O4 subnanoferrite. J Alloys Compd. 2010;496:345–350. doi: 10.1016/j.jallcom.2010.02.009 [DOI] [Google Scholar]
- 44.Zhang Q, Zhang T, Wei Y, et al. Removing structural water from sodium titanate anodes towards barrier-free ion diffusion for sodium ion batteries. J Mater Chem A. 2017;5:18691–18697. doi: 10.1039/C7TA05217K [DOI] [Google Scholar]
- 45.Moaty SAA, Farghali AA, Khaled R. Preparation, characterization and antimicrobial applications of Zn-Fe LDH against MRSA. Mater Sci Eng C. 2016;68:184–193. doi: 10.1016/j.msec.2016.05.110 [DOI] [PubMed] [Google Scholar]
- 46.Jobbágy M, Blesa MA, Regazzoni AE. Homogeneous precipitation of layered Ni (II)– Cr (III) double hydroxides. J Colloid Interface Sci. 2007;309:72–77. doi: 10.1016/j.jcis.2007.01.010 [DOI] [PubMed] [Google Scholar]
- 47.Lu H, Zhu Z, Zhang H, et al. Simultaneous removal of arsenate and antimonate in simulated and practical water samples by adsorption onto Zn/Fe layered double hydroxide. Chem Eng J. 2015;276:365–375. doi: 10.1016/j.cej.2015.04.095 [DOI] [Google Scholar]
- 48.Yamashita T, Hayes P. Analysis of XPS spectra of Fe2+ and Fe3+ ions in oxide materials. Appl Surf Sci. 2008;254:2441–2449. doi: 10.1016/j.apsusc.2007.09.063 [DOI] [Google Scholar]
- 49.Wagner CD, Riggs WM, Davis LE, Moulder JF, Muilenberg GE. Handbook of X-Ray Photoelectron Spectroscopy. Eden Prairie, MN: Perkin-Elmer Corp; 1979:38. [Google Scholar]
- 50.Pineda M, Fierro JG, Palacios J, et al. Characterization of zinc oxide and zinc ferrite doped with Ti or Cu as sorbents for hot gas desulphurization. Appl Surf Sci. 1997;119:1–10. doi: 10.1016/S0169-4332(97)00183-9 [DOI] [Google Scholar]
- 51.Pašukonienė V, Mlynska A, Steponkienė S, et al. Accumulation and biological effects of cobalt ferrite nanoparticles in human pancreatic and ovarian cancer cells. Medicina (B Aires). 2014;50:237–244. doi: 10.1016/j.medici.2014.09.009 [DOI] [PubMed] [Google Scholar]
- 52.Niu Y, Xia S. Stroma – epithelium crosstalk in prostate cancer. Asian J Androl. 2009;11:28–35. doi: 10.1038/aja.2008.39 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Niu HJ, Zhang L, Feng JJ, Zhang QL, Huang H, Wang AJ. Graphene-encapsulated cobalt nanoparticles embedded in porous nitrogen-doped graphitic carbon nanosheets as efficient electrocatalysts for oxygen reduction reaction. J Colloid Interface Sci. 2019. doi: 10.1016/j.jcis.2019.05.099 [DOI] [PubMed] [Google Scholar]
- 54.Niu HJ, Chen HY, Wen GL, Feng JJ, Zhang QL, Wang AJ. One-pot solvothermal synthesis of three-dimensional hollow PtCu alloyed dodecahedron nanoframes with excellent electrocatalytic performances for hydrogen evolution and oxygen reduction. J Colloid Interface Sci. 2019;539:525–532. doi: 10.1016/j.jcis.2018.12.066 [DOI] [PubMed] [Google Scholar]
- 55.Chen HY, Jin MX, Zhang L, et al. One-pot aqueous synthesis of two-dimensional porous bimetallic PtPd alloyed nanosheets as highly active and durable electrocatalyst for boosting oxygen reduction and hydrogen evolution. J Colloid Interface Sci. 2019;543:1–8. doi: 10.1016/j.jcis.2019.01.122 [DOI] [PubMed] [Google Scholar]