Abstract
Objective:
Successful weight loss interventions for African-Americans adolescents are lacking. Cognitive-behavioral interventions seek to develop weight loss skills (e.g., counting calories, goal setting, managing one’s environment). Little is known about how well adolescents implement such skills in their daily lives. Study aims were to (1) examine weight loss skills utilization at midpoint and end of a 6-month cognitive-behavioral/motivational interviewing weight loss sequential multiple assignment randomized trial (SMART), and (2) determine if greater skill utilization predicted weight loss at treatment end and 3 months post-treatment.
Method:
One hundred and eighty six African-Americans adolescents with obesity and their caregiver were first randomly assigned to complete 3 months of cognitive-behavioral and motivational interviewing family-based weight loss treatment in their home or in the research office (Phase 1). Nonresponders (i.e., those who lost < 3% of initial weight, n = 161) were rerandomized to 3 months of continued skills training (n = 83) or contingency management (n = 78) for Phase 2; responders were allocated to 3 months of relapse prevention (n = 20). Adolescents’ frequency of weight loss skills utilization was assessed via questionnaire at treatment midpoint and end.
Results:
Higher treatment attendance was associated with better skill utilization. Higher skill utilization was associated with more weight loss at treatment end, whereas higher baseline confidence was associated with more weight loss at follow-up.
Conclusions:
This study indicates the importance of attending weight loss intervention sessions to develop and strengthen weight loss skills in African-American adolescents with obesity, and strengthening confidence to use such skills for continued weight loss.
Keywords: African-Americans, Adolescents, Obesity, Weight loss skills, Intervention
Rates of obesity, defined as BMI at or above the 95th percentile, have risen in the last 30 years and remain higher in African-American (22.6%) than Caucasian (19.6%) adolescents [1]. Few adolescent behavioral weight control trials focus on urban and/or ethnic minority samples and the majority focus on Caucasian and/or suburban samples [2]. Of the few existing trials with African-American adolescents, most have not been successful at reducing weight or retaining adolescents in treatment [3–7], likely due to multiple system factors that influence obesity such as dealing with multiple competing priorities and low motivation for changing behavior, possibly underscored by differences in sociocultural beliefs and practices regarding eating and physical activity behaviors [8]. For example, in a culturally tailored nutrition and physical activity trial for African-American adolescent girls with obesity, delivered through local churches, structured diets with reduced caloric intake were not included as in the program because early focus groups with the target population raised opposition to their use [3]. Research to identify the best methods for promoting weight loss among African-American adolescents with obesity remains imperative to reducing pediatric obesity-related health inequities [9].
The American Academy of Pediatrics recommends the use of behavioral interventions to increase healthy eating and activity level among overweight and obese adolescents [10,11]. Such programs focus on developing a core set of empirically-supported behavioral weight loss skills including self-monitoring caloric intake and activity level, stimulus or environmental control to limit cues for unhealthy eating and sedentary activities, and goal setting. Such programs demonstrate success with weight outcomes, primarily with Caucasian samples [12–15]. In one of the few studies focusing on low income ethnic minority (most commonly African-American) children and adolescents with morbid obesity, more frequent self-monitoring was associated with greater weight loss [12]. Other research demonstrates that many African-Americans adolescents with overweight or obesity do not feel highly motivated to engage in these weight loss skills [3,16,17]. Incorporating weight loss skills into daily routines can be difficult and aversive for adults, and adolescents may face additional barriers (e.g., likely only marginal control of food options within the home, social and normative pressures to align behaviors with friends and family members). Thus, the extent to which African-American adolescents with obesity are sufficiently motivated and confident in their abilities and actually engage in core behavioral weight skills are unknown.
We conducted a sequential multiple assignment randomized trial (SMART) to optimize a 6-month family-based weight control intervention for African-Americans with obesity (FIT Families). FIT Families included teaching adolescents cognitive-behavioral weight control strategies consistent with the obesity treatment literature. Content was delivered using a motivational interviewing (MI) framework given MI’s role in improving treatment attendance [18] and lifestyle behavior changes [19] in weight control programs for African-Americans. MI is a communication style characterized by a sense of partnership between provider and patient, provider’s acceptance and compassion for the patient, and provider’s use of evocation to elicit patient’s intentions for behavior change [20]. The initial randomization was intended to test if weight loss would be maximized when the Phase 1 intervention was delivered in the natural environment (home-based, HB) versus in a clinical office (office-based, OB). HB treatment was designed to decrease barriers to accessing treatment. After 3 months of treatment, participants’ initial treatment response (degree of weight loss) was evaluated. Adolescents who lost at least 3% of their baseline weight were considered treatment responders [21]. For Phase 2, responders were allocated to relapse prevention, and nonresponders were rerandomized to either continued skills (CS) training or contingency management (CM) for weight loss. CM has been suggested by pediatric obesity experts [22] and was supported in pilot work [23]. The primary outcome papers [24,25] reported that although participants lost weight overall, weight loss at treatment-end was not associated with group assignment or attendance but was moderated by baseline confidence, executive functioning, and age.
The current study is a secondary data analysis of the SMART to examine weight loss skills utilization. The primary aims were to determine (1) if frequency of weight loss skills utilization among African-American adolescents with obesity would differ by treatment arm at the end of Phase 1 (T2) and Phase 2 (T3), and (2) whether more frequent skill utilization resulted in greater weight loss at T3 and follow-up (T4). We hypothesized (H1a) that adolescents would show higher skill utilization when they were initially randomized to HB compared with OB because practicing weight loss skills in the home environment would optimize their use [26]. We hypothesized (H1b) that skill utilization in Phase 2 would be higher in CM versus CS, because skills utilization might result in weight loss and thus increase incentives earned in CM [23]. We hypothesized (H2a and H2b, respectively) that skills utilization would account for weight change from baseline to treatment end and follow-up, such that higher skill utilization at the end of treatment would be related to more weight loss at both T3 and T4, even after accounting for confidence and executive functioning [27,28].
Method
Procedure
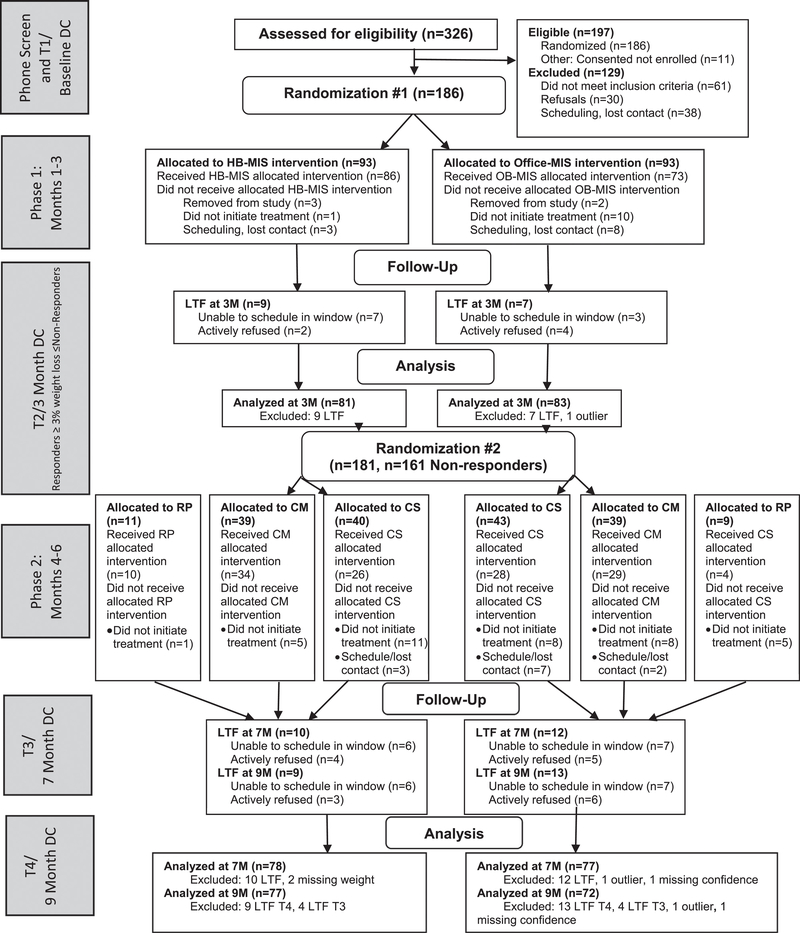
Figure 1 shows the Consolidated Standards of Reporting Trials (CONSORT) diagram of participant flow throughout the study. The study was registered with ClinicalTrials.gov (NCT01350531). All aspects of the study were approved by the university’s Institutional Review Board. Study methods have been reported elsewhere [24,25,29]. In brief, all data collections - baseline (T1), 3 months (T2), 7 months (T3), and 9 months (T4) - were completed in participants’ homes to help minimize attrition. Parental informed consent and adolescent assent were obtained at baseline.
Figure 1.
Participant flow following Consolidated Standards of Reporting Trials (CONSORT) guidelines.
Notes. CM= contingency management; CS= continued skills; DC= data collection; HB= home-based; LTF= lost to follow-up; MIS= motivational interviewing and skills; OB= office-based; RP= relapse prevention.
After baseline, the project manager randomized the family to 3 months of HB or OB treatment with groups stratified on adolescent percent overweight (high and low) and adolescent comorbidities (presence vs. absence). The T2 data collection involved adolescents’ weight measurement and assessment of adolescents’ weight loss skills utilization over the past 3 months. The project manager subsequently randomized non-responders to CS or CM, and responders to relapse prevention. Data collections then occurred at treatment end (T3) and post-treatment follow-up (T4). Research and clinical teams strived to keep research assistants blind to intervention conditions by keeping separate locked paper and password-protected computer files. Families were compensated $50 for the T1, T3, and T4 data collection and $10 for the shorter T2 data collection.
Participants
Participants (adolescents and a primary caregiver) were recruited by clinicians in pediatric clinics of a university-affiliated urban children’s hospital, via letters sent after review of hospital informatics, and from community events and inquiries. Of the 186 dyads enrolled, 5 families were removed from the study (3 were determined ineligible after enrolling and 2 due to interventionist error), resulting in data from 181 families. Briefly, adolescents were required to self-identify as African-American, be age 12 −16 years, have BMI ≥ 95th percentile for age and gender, reside within 30 miles of the hospital with a primary caregiver who was willing to participate in the intervention, and speak English. Adolescents were excluded if their obesity was secondary to another medical condition or medication, they were diagnosed with a condition causing daily fluid fluctuations or a condition preventing participation in normal exercise, or if they were pregnant, suicidal or homicidal, or had a thought disorder or serious cognitive impairment. Table 1 shows participant characteristics at baseline and follow-ups by treatment groups. Retention for follow-up visits was high; 91%, 88%, and 88% of families completed their 3-,7-, and 9-month follow-up data collection visits.
Table 1.
Unadjusted participant characteristics at baseline and follow-ups by treatment sequence
| Phase 1 treatment Group | ||||||
|---|---|---|---|---|---|---|
| Home | Office | |||||
| Age, M (SD) years | 13.64 (1.29) | 13.86 (1.41) | ||||
| Gender, N (%) girls | 67 (74.4%) | 55 (60.4%) | ||||
| T1 executive functioning, M (SD) | 123.10 (26.12) | 124.4 (29.30) | ||||
| T1 weight, M (SD) pounds | 223.04 (47.88) | 236.81 (53.55) | ||||
| T1 confidence, M (SD) | 6.62 (1.70) | 7.13 (1.69) | ||||
| T1 BMI, M (SD) kg/m2 | 37.46 (7.13) | 38.84 (7.73) | ||||
| T1 percent overweight, M (SD) | 93.75 (36.10) | 99.83 (38.97) | ||||
| P1 session attendance, M (SD) | 13.17 (5.68) | 8.62 (5.73) | ||||
| T2 skills utilization, M (SD) | 3.30 (0.68) | 3.06 (0.74) | ||||
| Phase 2 treatment group* |
||||||
| CM | CS | RP | CM | CS | RP | |
| T2 percent overweight, M (SD) | 95.48 (38.47) | 92.27 (40.27) | 74.38 (28.53) | 103.52 (44.52) | 98.63 (36.78) | 93.34 (36.72) |
| P2 session attendance, M (SD) | 17.71 (6.75) | 8.65 (6.08) | 7.95 (3.20) | 13.35 (8.47) | 7.68 (5.86) | 3.00 (3.90) |
| T3 skills utilization, M (SD) | 3.25 (0.75) | 2.84 (0.74) | 3.16 (0.87) | 2.96 (0.79) | 2.90 (0.74) | 2.46 (0.76) |
Notes: CM = contingency management; CS = continued skills; RP = relapse prevention.
T1 = baseline. T2 = 3-month follow-up (end of Phase 1 [P1]). T3 = 7-month follow-up (end of Phase 2 [P2]).
Although CM and CS both took place in participants’ homes, the 6 Phase 2 groups are shown here below the Phase 1 group in which they started (i.e., the second CM column represents teens who were first assigned to Office then to CM).
Intervention
Phase 1: Home- versus Office-based Motivational interviewing and Skills.
Sessions were conducted twice weekly by community health workers (CHWs; paraprofessional counselors). The first weekly session was 1 hour, delivered in person, and focused on teaching a weight loss skill. Adolescents also completed a weekly weigh-in, and homework was assigned (i.e., practice of the new skill that had been taught). Based on earlier work with this population and known difficulties with treatment attendance [30], OB families were given $10 gift cards in compensation for session attendance, and parking vouchers or taxi transportation were provided. The second weekly session (approximately 15–45 minutes) was a check-in with families to determine if homework (skills practice) was being implemented and address any barriers. This session was conducted over the phone for OB families and in the home for HB.
Intervention content for Phase 1 was similar irrespective of treatment delivery setting. The first week’s focus was to engage the family in treatment and to collaboratively develop treatment goals using MI. Weeks 2 and 3 focused on nutrition and physical activity education, delivered face-to-face by a registered dietitian with the CHW attending and observing most sessions. The dietitian reviewed the MyPyramid/MyPlate [31,32], tools to find calorie content in food, how to record consumption on a paper-based food log, and how to evaluate and monitor physical activity intensity. The adolescent set a treatment goal of reducing their caloric intake by 500 kcal/day or having a net intake of 1600–2000 kcal/day (based on age and gender).
The remaining weeks focused on building behavioral weight loss skills using the following approach. The CHW modeled the skill (e.g., keeping a food log), engaged both adolescent and caregiver in guided practice, and provided feedback regarding skill implementation. Adolescent-oriented treatment modules included self-monitoring food and physical (in)activity levels (e.g., adolescent logging food and physical activity), stimulus control of food and (in)activity triggers in and out of the home environment (e.g., adolescent making plans to change environments to optimize more healthful food and physical activity choices), and managing hunger and food cravings (e.g., adolescent learning to distinguish hunger vs. craving and developing coping strategies for managing hunger and cravings). Caregivers were encouraged to support adolescent activities and taught parenting skills (e.g., improving support, supervision, and limit setting).
Phase 2: Continued skills, contingency management, or relapse prevention.
Families generally continued working with the same CHW in Phase 2; both CS and CM were home-based. CS treatment modality was the same twice-weekly cognitive-behavioral skill building delivered using an MI framework. CS began with a reassessment of skills. Although families could also choose to repeat any sessions from Phase 1, CS was not designed to repeat Phase 1. Potential modules included managing distorted thinking regarding weight loss, reducing emotional eating, increasing planning and organizational skills, and strengthening refusal skills.
CM utilized a voucher-based system informed by our pilot work to provide incentives to both the adolescent (for weight loss) and the caregiver (for adherence to CM protocols and session attendance). Adolescents and caregivers could each earn up to $624 in vouchers for products available from amazon.com. In twice-weekly sessions, the CHW guided the caregiver’s CM administration and led discussions with family about barriers and facilitators to weight loss and meeting goals. There were no weight loss skills taught during CM. However, if families had not completed the Phase 1 educational sessions with the dietitian, those were delivered before starting CM.
Finally, for adolescents allocated to relapse prevention, treatment continued in the same location as for Phase 1 but frequency was reduced to one face-to-face session per week. Treatment modules focused on exploring values and commitment to weight loss treatment, managing slips, and maintaining dietary and physical activity changes enacted already. Families were also allowed to repeat or complete a missed Phase 1 skills module.
Quality assurance.
CHWs completed 300 hours of initial training including didactics and role plays. Throughout the study, CHWs received weekly individual supervision with a clinical supervisor (a psychologist), group supervision attended by a dietitian, weekly phone calls with an expert consultant for difficult cases, and quarterly booster trainings. HB sessions were audio-recorded and OB sessions were all video recorded, with initial sessions coded based on the Motivational Interviewing Treatment Integrity (MITI 3.1) [33] to assess MI fidelity.
Measures
Skills utilization.
The research team developed a 19-item self-report measure to assess adolescents’ utilization of weight loss skills taught in Phase 1 (available by request). At T2 and T3, adolescents self-reported their frequency of engaging in weight loss skills as part of a pencil-and-paper measures battery completed at each data collection session. Sample items include, “I counted calories.” and “I set specific goals for physical activity.” Response options were anchored by 1 (never) and 5 (all the time). Reliability was excellent; Cronbach’s αT2 = .90 and αT3 = .93. The mean score was computed at T2 and T3. On average, teens reported utilizing weight loss skills “sometimes” (MT2 = 3.18, SD T2 = 0.72; MT3 =2.97, SD T3 = 0.78).
Percent overweight.
Weight change was operationalized as change in percent overweight from baseline to the given follow-up point [34]. Percent overweight was calculated as the percentage each participant’s body mass index (BMI, in kg/m2) was above the CDC’s median BMI for age and gender.
Executive function.
Executive functioning encompasses the set of self-regulatory cognitive processes involved in inhibition, attention, set-shifting, planning, and organization. Adolescents’ executive functioning level was assessed at T1 with the Global Executive Composite score from the 86-item Behavior Rating Inventory of Executive Function - Parent Report [35]. Adolescents’ frequency of problems in the domains of inhibition, shifting situations, modulating emotions, working memory, planning/organizing, and monitoring work over the past 6 months on a 1, never, to 3, often, scale were assessed.
Motivation: Confidence.
Adolescents’ confidence/self-efficacy in making lifestyle changes was assessed with an adapted Rollnick’s Readiness Ruler [36]. Adolescents indicated how sure they felt in being able to enact 15 behaviors related to diet, physical activity, and the intervention program, on 10 cm lines anchored by not at all sure and very sure. Research assistants measured each response with a ruler and averaged for a total confidence score. Cronbach’s α = .89.
intervention-related variables.
Phase 1 (HB vs. OB) and 2 (CM vs. CS) treatment groups were included as dichotomous variables. Session attendance was measured as the number of sessions participants attended in each phase and summed for total attendance.
Data analysis plan
To address Aim 1a, Phase 1 effects at T2 were investigated using analysis of covariance to control for attendance. To address Aim 1b, utilization of weight loss skills at T3 was evaluated with a Generalized Estimating Equation (GEE), an extension of the Generalized Linear Model, itself an extension of the General Linear Model. GEEs are appropriate for normal and non-normal data, nested data, longitudinal designs, and otherwise correlated data whether linearly or nonlinearly linked. The GEE included Phases 1 and 2 conditions and total session attendance.
Aim 2 was also analyzed using GEEs. The outcome variable was change in percent overweight from baseline to the time point evaluated. Prior to specifying the models, we examined bivariate correlations between potential demographic and individual difference predictors (age, gender, treatment attendance, executive functioning, confidence, and skills utilization) and change in percent overweight at the two time points. Age, gender, and treatment attendance were not significantly bivariately related to weight change at T3 or T3; therefore, they were not included in the final models. We thus included Phase 1 and 2 treatment groups and sequence, baseline confidence and executive functioning, and skills utilization in the models. Confidence, executive functioning, and skills utilization were treated as continuous variables. All analyses were conducted with SPSS version 24.
Data file structure and weighting.
We followed the weighting and replication method described by the developers of the SMART methodology [37,38]. In this approach, responders’ data are considered to be consistent with each of the Phase 2 arms that their sequence originated from (i.e., HB or OB followed by either CS or CM) and is, thus, assigned to both Phase 2 arms originating from the same Phase 1 arm. To make population-level inferences, each participant’s data were then weighted as the inverse of their selection probability. Responders were assigned a weight of 2; nonresponders were assigned a weight of 4. Robust (sandwich) errors were estimated to account for repeated measures. Power and planned sample size for the SMART were conservatively based on the Phase 2 between-groups comparison because nonresponders were rerandomized in the second phase [39]. A sample size of 180 has 80% power to detect a 3.5% difference in percent overweight in a two-side independent samples t-test with Type-I error rate of 5%. Participants who were lost at follow-up, missing specified variables, or were identified as a multivariate outlier were excluded from analysis.
Results
Effects of treatment condition on skills utilization (Aim 1)
In initial support of H1a (N = 164), adolescents who received HB intervention for Phase 1 reported significantly higher use of weight loss skills at T2 (M = 3.30, 95% confidence interval [CI 3.15,3.45]) than teens who received OB intervention (M = 3.08, 95% CI [2.93,3.23]), F(1,162) = 4.04, p = .046, partial η2 = 0.024. However, the treatment group effect was eliminated, F(1,161) = 0.26, p = .61, when controlling for session attendance (F[1,161] =43.35, p < .001, partial η2 = 0.21). The more Phase 1 sessions attended, the higher the use of weight loss skills at T2.
Hypothesis H1b was not supported (N = 158). There were no significant effects of treatment assignment for either Phase 1 or Phase 2 on weight loss skills at T3 (both Wald χ2 [df = 1] < 3.32, p’s ≥ .07). Treatment attendance was a significant covariate; the more treatment sessions participants attended, the higher their use of weight loss skills at T3 (B = 0.03,95% CI [0.02, 0.04], Wald χ2 [df=1] = 26.69, p < .001).
Effects of skill utilization on weight loss (Aim 2)
In support of H2a, weight loss skills utilization was significantly related to weight change at T3 (Table 2). The higher the skill utilization, the greater the reduction in percent overweight.
Table 2.
Results of generalized estimating equations showing effects of skills utilization on change in percent overweight at treatment end (T3)
| Parameter | B | SE | 95% CI | Wald χ2 (df =1) |
|---|---|---|---|---|
| Phase 1 condition | −1.22 | 1.97 | [−5.09,2.65] | 0.01 |
| Phase 2 condition | −1.59 | 1.79 | [−5.10,1.91] | 0.06 |
| Treatment sequence | 2.50 | 2.65 | [−2.70, 7.69] | 0.89 |
| Executive functioning | 0.03 | 0.03 | [−0.02,0.08] | 1.54 |
| Skills utilization | −2.46 | 1.19 | [−4.80, −0.13] | 4.27* |
| Confidence | −0.58 | 0.44 | [−1.44,0.27] | 1.78 |
Notes: Phase 1 treatment conditions compares families randomly assigned to home (1) vs. office (2). Phase 2 treatment condition compares contingency management (1) with continued skills (2).
p < .05.
H2b was not supported (Table 3). T3 weight loss skills utilization was not significantly related to T4 weight change. However, baseline confidence was significantly associated with weight change at T4. The higher the adolescents’ confidence in their abilities to engage in such skills at the start of treatment, the greater their reduction in percent overweight 9 months later.
Table 3.
Results of generalized estimating equations showing effects of skills utilization on change in percent overweight at treatment follow-up (T4)
| Parameter | B | SE | 95% CI | Wald χ2 (df =1) |
|---|---|---|---|---|
| Phase 1 condition | −1.41 | 2.21 | [−5.73,2.92] | 0.46 |
| Phase 2 condition | −0.33 | 2.15 | [−4.54,3.88] | 0.01 |
| Treatment sequence | 0.62 | 3.01 | [−5.28,6.51] | 0.04 |
| Executive functioning | 0.03 | 0.03 | [−0.03,0.09] | 1.01 |
| Skills utilization | −1.94 | 1.36 | [−4.61,0.73] | 2.03 |
| Confidence | −0.88 | 0.44 | [−1.74, −0.02] | 4.02* |
Notes: Phase 1 treatment conditions compares families randomly assigned to home (1) vs. office (2). Phase 2 treatment condition compares contingency management (1) with continued skills (2).
p < .05.
Discussion
The current study examined weight loss skills utilization in a sample of African-American adolescents with obesity enrolled in a weight loss SMART. The more treatment sessions adolescents attended, the more frequent their reported use of evidence-based weight loss skills at treatment midpoint and end. In turn, the more frequently adolescents used the skills, the more weight loss, as previously found with samples of predominantly Caucasian adolescents [10–15]. Developing weight management skills, such as setting goals for eating and physical activity, measuring portions, counting calories, and reading food labels, are a key part of cognitive-behavioral skill-building interventions. Although previous researchers recorded low motivation to engage in such skills among African-American adolescents [3,16,17], this study demonstrates that it is feasible to foster these skills, that enacting such skills consistently translates to greater weight loss, and that feeling more confident and self-efficacious to engage in such skills at treatment initiation may help carry adolescents through their weight loss journey.
Our findings that better attendance was related to more frequent skill utilization corroborate previously identified treatment engagement issues for African-American adolescents [5] and highlight the need to improve treatment attendance among this population. Families faced considerable challenges to treatment attendance (e.g., adolescents and/or caregivers balancing multiple jobs and school, needs of other children/family members). Providing home-based treatment and incentivizing caregivers’ attendance helped with engagement but were insufficient for significant weight loss and imply that more potent interventions are needed. That sustained weight loss, 3 months after treatment ended, was predicted by higher early confidence suggests that boosting confidence before treatment starts may be one way to improve future interventions [17,24].
The current study is not without limitations. The skills utilization measure was not given at baseline, so we were not able to compare changes in skills utilization from baseline to treatment completion. The decision to not assess baseline skills utilization was based on the assumption that skill utilization before treatment would be essentially “never/rarely;” although without assessment we cannot test that assumption. Future research is needed to determine the extent to which adolescents use such skills prior to entering treatment and then how utilization changes over time. The skills utilization measure was self-report, covered a relatively large window of time, and was not explicitly validated. The study’s SMART design, although not a limitation in and of itself, is not a randomized controlled trial but rather a developmental study design to suggest key components for a future trial. Relatedly, although all treatment arms lasted 3 months, there was variability in the number of expected sessions for the Phase 2 arms, which may complicate the relationship between dose and treatment effects. Although potentially balanced by utilizing lower cost CHWs (compared with graduate-level interventionists), the potentially costly CM structure may limit enthusiasm for scalability; however, a full cost effectiveness analysis is an important future step.
The current study demonstrates that among a high-risk group (African-American adolescents with obesity), modest weight loss is feasible through engaging in weight loss skills. Although these skills may fade over time without support, starting with a strong sense of confidence that the skills can be mastered may provide the needed internal motivation for adolescents to keep pursuing their weight loss goals. The challenge for providers and interventionists will be to develop more potent methods to cultivate that confidence early and encourage continued use of skills over time once the primary support ends, potentially through the use of peer support, text messages, or mobile apps [40].
IMPLICATIONS AND CONTRIBUTION.
Among African-American adolescents with obesity, use of evidence-based weight loss skills predicted weight loss at treatment end. Baseline confidence in engaging in such skills predicted sustained weight loss. Together, these findings suggest the need to strengthen confidence early and develop such skills over the course of weight loss treatment.
Acknowledgments
Funding
This work was supported by the National Heart, Lung, and Blood Institute and the Eunice Kennedy Shriver National Institute of Child Health and Human Development (grant number U01HL097889) and by the National Institute of Alcohol Abuse and Alcoholism (grant number K01AA024500). The National Institutes of Health had no role in the study design; data collection, analysis, or interpretation; writing this manuscript; or the decision to submit the manuscript.
Footnotes
Conflict of interest: The authors do not have any potential, perceived, or real conflict of interest. A.J. Jacques-Tiura wrote the first draft of the manuscript; all authors contributed to study conception and manuscript editing, and all authors approve of the final draft. S. Naar is now at Florida State University.
This trial was registered with ClinicalTrials.gov:NCT01350531.
References
- [1].Ogden CL, Carroll MD, Lawman HG, et al. Trends in obesity prevalence among children and adolescents in the United States 1988–1994 through 2013–2014. JAMA 2016;315:2292–9. 10.1001/jama.2016.6361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Janicke DM, Steele RG, Gayes LA, et al. Systematic review and meta-analysis of comprehensive behavioral family lifestyle interventions addressing pediatric obesity. J Pediatr Psychol 2014;39:809–25. 10.1093/jpepsy/jsu023. [DOI] [PubMed] [Google Scholar]
- [3].Resnicow K, Taylor R, Baskin M, McCarty F. Results of go girls: A weight control program for overweight African-American adolescent females. Obes Res 2005;13:1739–48. 10.1038/oby.2005.212. [DOI] [PubMed] [Google Scholar]
- [4].Williamson DA, Walden HM, White MA, et al. Two-year Internet-based randomized controlled trial for weight loss in African-American girls. Obesity (Silver Spring) 2006;14:1231–43. 10.1038/oby.2006.140. [DOI] [PubMed] [Google Scholar]
- [5].Jelalian E, Hart CN, Mehlenbeck RS, et al. Predictors of attrition and weight loss in an adolescent weight control program. Obesity 2008;16:1318–23. 10.1038/oby.2008.51. [DOI] [PubMed] [Google Scholar]
- [6].Tershakovec AM, Kuppler K. Ethnicity, insurance type, and follow-up in a pediatric weight management program. Obes Res 2003;11:17–20. 10.1038/oby.2003.4. [DOI] [PubMed] [Google Scholar]
- [7].Zeller M, Kirk S, Claytor R, et al. Predictors of attrition from a pediatric weight management program. J Pediatr 2004;144:466–70. 10.1016/j.jpeds.2003.12.031. [DOI] [PubMed] [Google Scholar]
- [8].Kumanyika S. The sociocultural context for obesity prevention and treatment in children and adolescents: Influences of ethnicity and gender In: Freemark M, ed. Pediatric Obesity: Etiology, Pathogenesis, and Treatment, 2nd Ed. Contemporary Endocrinology. Cham, Switzerland: Humana Press, Springer International Publishing; 2018:696–713. 10.1007/978-3-319-68192-4_40. [DOI] [Google Scholar]
- [9].Barr-Anderson DJ, Adams-Wynn AW, DiSantis KI, Kumanyika S. Family-focused physical activity, diet and obesity interventions in African-American girls: A systematic review. Obes Rev 2013;14:29–51. 10.1111/j.1467-789X.2012.01043.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Spear BA, Barlow SE, Ervin C, et al. Recommendations for treatment of child and adolescent overweight and obesity. Pediatrics 2007;120:S254–88. 10.1542/peds.2007-2329F. [DOI] [PubMed] [Google Scholar]
- [11].US Preventive Services Task Force. Screening for obesity in children and adolescents: US Preventive Services Task Force Recommendation Statement. JAMA 2017;317:2417–26. 10.1001/jama.2017.6803. [DOI] [PubMed] [Google Scholar]
- [12].Germann JN, Kirschenbaum DS, Rich BH. Child and parental self-monitoring as determinants of success in the treatment of morbid obesity in low-income minority children. J Pediatr 2007;32:111–21. 10.1093/jpepsy/jsl007. [DOI] [PubMed] [Google Scholar]
- [13].Mockus DS, Macera CA, Wingard DL, et al. Dietary self-monitoring and its impact on weight loss in overweight children. Int J Pediatr Obes 2011;6:197–205. 10.3109/17477166.2011.590196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Saelens BE, McGrath AM. Self-monitoring adherence and adolescent weight control efficacy. Children’s Health Care 2003;32:137–52. 10.1207/S15326888CHC3202_5. [DOI] [Google Scholar]
- [15].Theim KR, Sinton MM, Goldschmidt AB, et al. Adherence to behavioral targets and treatment attendance during a pediatric weight control trial. Obesity (Silver Spring) 2013;21:394–7. 10.1002/oby.20281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Savoye M, Shaw M, Dziura J, et al. Effects of a weight management program on body composition and metabolic parameters in overweight children: A randomized controlled trial. JAMA 2007;297:2697–704. [DOI] [PubMed] [Google Scholar]
- [17].MacDonell K, Ellis D, Naar-King S, Cunningham P. Predictors of home-based obesity treatment efficacy for African American youth. Child Health Care 2010;39:1–14. [Google Scholar]
- [18].Bean MK, Powell P, Quinoy A, et al. Motivational interviewing targeting diet and physical activity improves adherence to paediatric obesity treatment: results from the MI Values randomized controlled trial. Pediatr Obes 2014;10:118–25. 10.1111/j.2047-6310.2014.226.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].MacDonell K, Brogan K, Naar-King S, et al. A pilot study of motivational interviewing targeting weight-related behaviors in overweight or obese African American adolescents. J Adolesc Health 2012;50:201–3. 10.1016/j.jadohealth.2011.04.018. [DOI] [PubMed] [Google Scholar]
- [20].Miller WR, Rollnick S. Motivational interviewing: Preparing people for change. New York: Guilford, 2013. [Google Scholar]
- [21].Clinical Guidelines on the Identification, Evaluation and Treatment of Overweight and Obesity in Adults. NHLBI Obesity Education Initiative. Bethesda, MD: National Institutes of Health, 2000. [Google Scholar]
- [22].Barlow SE. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: Summary report. Pediatrics 2007;120:S164–92. 10.1542/peds.2007-2329C. [DOI] [PubMed] [Google Scholar]
- [23].Hartlieb KB, Naar S, Ledgerwood DM, et al. Contingency management adapted for African American adolescents with obesity enhances youth weight loss with caregiver participation: A multiple baseline pilot study. Int J Adolesc Med Health 2015;29:1–5. 10.1515/ijamh-2015-0091. [DOI] [PubMed] [Google Scholar]
- [24].Naar S, Ellis D, Idalski Carcone A, et al. Outcomes from a sequential multiple assignment randomized trial (SMART) of weight loss strategies for African American adolescents with obesity. Ann Beh Med 2018. Manuscript in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Naar-King S, Ellis DA, Idalski Carcone A, et al. Sequential multiple assignment randomized trial (SMART) to construct weight loss interventions for African American adolescents. J Clin Child Adolesc Psychol 2016;45:428–41. 10.1080/15374416.2014.971459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Appelhans BM, Moss OA, Cerwinske LA. Systematic review of paediatric weight management interventions delivered in the home setting. Obes Rev 2016;17:977–88. 10.1111/obr.12427. [DOI] [PubMed] [Google Scholar]
- [27].Reinert KR, Po’e EK, Barkin SL. The relationship between executive function and obesity in children and adolescents: A systematic literature review. J Obes 2013;2013:1–10. 10.1155/2013/820956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Smith E, Hay P, Campbell L, Trollor JN. A review of the association between obesity and cognitive function across the lifespan: Implications for novel approaches to prevention and treatment. Obes Rev 2011;12:740–55. 10.1111/j.1467-789X.2011.00920.x. [DOI] [PubMed] [Google Scholar]
- [29].Brogan Hartleib K, Jacques-Tiura AJ, Naar-King S, et al. Clinical, informatics, and community recruitment strategies are valuable for the retention of urban minority youth with obesity in clinical trials. Prev Chronic Dis 2015;12:140409. 10.5888/pcd12.140409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Naar-King S, Ellis D, Kolmodin K, et al. A randomized pilot study of multisystemic therapy targeting obesity in African-American adolescents. J Adolesc Health 2009;45:417–9. 10.1016/jjadohealth.2009.03.022. [DOI] [PubMed] [Google Scholar]
- [31].MyPlate/MiPlato. US Department of Agriculture. Available at: https://www.cnpp.usda.gov/MyPlate Accessed March 9,2018.
- [32].MyPyramid. US Department of Agriculture. Available at: https://www.cnpp.usda.gov/mypyramid Accessed February 9, 2018.
- [33].Moyers TB, Martin T, Manuel JK, et al. Assessing competence in the use of motivational interviewing. J Subst Abuse Treat 2005;28:19–26. 10.1016/j.jsat.2004.11.001. [DOI] [PubMed] [Google Scholar]
- [34].Paluch RA, Epstein LH, Roemmich JN. Comparison of methods to evaluate changes in relative body mass index in pediatric weight control. Am J Hum Biol 2007;19:487–94. 10.1002/ajhb.20608. [DOI] [PubMed] [Google Scholar]
- [35].Gioia GA, Isquith PK, Guy SC, Kenworthy L. Behavior rating inventory of executive function professional manual. Lutz, FL: PAR, 2000. [Google Scholar]
- [36].Rollnick S, Heather N, Gold R, Hall W. Development of a short readiness to change questionnaire for use in brief, opportunistic interventions among excessive drinkers. Br J Addict 1992;87:743–54. [DOI] [PubMed] [Google Scholar]
- [37].Nahum-Shani I, Qian M, Almirall D, et al. Experimental design and primary data analysis methods for comparing adaptive interventions. Psychol Methods 2012a;17:457–77. 10.1037/a0029372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Nahum-Shani I, Qian M, Almirall D, et al. Q-learning: A data analysis method for constructing adaptive interventions. Psychol Methods 2012b;17:478–94. 10.1037/a0029373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Murphy SA. An experimental design for the development of adaptive treatment strategies. Stat Med 2005;24:1455–81. 10.1002/sim.2022. [DOI] [PubMed] [Google Scholar]
- [40].Nollen NL, Mayo MS, Carlson SE, et al. Mobile technology for obesity prevention: A randomized pilot study in racial- and ethnic-minority girls. Am J Prev Med 2014;46:404–8. 10.1016/j.amepre.2013.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]