Abstract
Purpose
To explore the neuroprotective effects and mechanisms of Apelin (APLN), and to study the regulation of APLN expression by microRNA (miRNA) in epilepsy.
Materials and Methods
In vitro and in vivo epileptic models were established with hippocampal neurons and Wistar rats. Apoptosis of neurons was identified by flow cytometry. Western blotting was used to detect the expression of proteins, and quantitative reverse transcriptase polymerase chain reaction (qRT-PCR) was used to analyze the expression of miRNA and messenger RNA (mRNA). Bioinformatics software was used to predict target genes of miRNA, which were confirmed by dual-luciferase reporter gene system and functional experiments.
Results
Our study demonstrated protective effects of APLN against neuronal death in epilepsy both in vitro and in vivo. The underlying mechanisms involved are inhibiting the expression of metabotropic glutamate receptor 1 (mGluR1), Bax, and caspase-3; promoting the expression of Bcl-2; and increasing phosphorylated-AKT (p-AKT) levels in neurons. For the first time, we found that miR-182 could negatively regulate both transcriptional and translational levels of APLN, and that the up-regulation of miR-182 inhibited the expression of APLN and Bcl-2, and promoted the expression of Bax and caspase-3.
Conclusion
APLN could protect the neurons from injury in epilepsy by regulating the expression of apoptosis-associated proteins and mGluR1 and increasing p-AKT levels, which were attenuated by miR-182. Hence, miR-182/APLN may be potential targets for epilepsy control and treatment.
Keywords: epilepsy, apelin, neuroprotective effects, miR-182, regulation
Introduction
Epilepsy is a chronic and often progressive neurological disorder characterized by the recurrent, periodic, and unpredictable occurrence of epileptic seizures that affects 50–70 million people globally.1,2 Epilepsy is the most frequently occurring neurodegenerative disease after stroke; according to epidemiological studies, approximately 70–80% of patients with epilepsy achieve remission, and approximately 30% of these patients are refractory to medical treatment, show progressive cognitive impairment, and may require neurosurgical resection of the epileptic focus to alleviate seizure recurrence.1,3 Although the imbalance between excitatory and inhibitory pathways within the central nervous system may contribute to epileptogenesis, the underlying etiology and mechanisms still remain elusive.2 Over the past decade, the critical role of brain inflammation in epilepsy was highlighted.2 Increased levels of pro-inflammatory cytokines [eg, interleukin-1b (IL-1b), tumor necrosis factor-α (TNF-α), high-mobility group box protein 1 (HMGB1), S100b] and downstream inflammatory mediators (eg, prostaglandins and the complement system) have been documented in epileptogenic tissues obtained from patients with different epilepsy etiologies.2 Trauma, stroke, and infection are all related to epileptic seizures via brain inflammation.4 Inflammatory responses inducing neuronal death were demonstrated by a previous study,5 which play a crucial role in the pathogenesis and recurrence of epilepsy.6,7 Furthermore, excitotoxicity,6 ischemia/hypoxia,8 oxidative stress,1 and changes in blood–brain barrier function9 contribute to the neuronal death in epilepsy. Reducing neuronal death could alleviate pentylenetetrazol (PTZ)-10 and kainic acid-induced11 seizures. Hence, protecting neurons from death is a potential target for epilepsy control and treatment.
Apelin (APLN) is an endogenous neuropeptide and was initially isolated from bovine stomach, which is a native ligand of the Apelin (APJ) receptor.12 Some studies have found that APLN peptides could alter blood pressure, feeding behavior, and pituitary hormone release.12 APLN was reported to mediate neuroprotective effects by regulating ischemia-reperfusion injury, oxidative stress, autophagy, and neuronal apoptosis.13–16 APLN-13 could protect rat primary cortical glia-neuron co-culture against PTZ-induced toxicity17 and have anticonvulsive and neuroprotective effects against PTZ-induced seizure in rats.18 MicroRNAs are involved in post-transcriptional regulation of gene expression in multicellular organisms by affecting both the stability and translation of messenger RNAs (mRNAs).19 Although certain miRNAs that could regulate the expression of APLN gene were reported in previous studies,20,21 the mechanism by which miRNAs regulate APLN gene expression in epilepsy is not clear.
In this study, we confirmed that APLN could protect the hippocampal neurons from apoptosis in epilepsy. The underlying mechanisms involved are inhibiting the expression of pro-apoptosis proteins and metabotropic glutamate receptors (mGluR1) and increasing the expression of anti-apoptosis protein and p-AKT levels. For the first time, we found that miR-182 could negatively regulate the expression of APLN gene and that the up-regulation of miR-182 could attenuate the neuroprotective effects of APLN.
Materials and Methods
Animals and Cell Lines
Female Wistar rats (8–10-week-old) were purchased from Beijing Charles River Laboratory (SCXC-2016) and housed in specific pathogen-free conditions at the First Hospital Animal Center of Jilin University. All animal experiments were approved by the Animal Ethical committee of First Hospital of Jilin University and according to the China Laboratory Animal-Guideline for ethical review of animal welfare (GB/T 35892–2018). E18 rat primary hippocampal neurons were purchased from KangLang Biotechnology (Shanghai, China).
Experimental Reagents
We purchased neuron culture medium and nerve growth factors from Sciencell (California, USA); MiR-182, U6, APLN, and glyceraldehyde 3-phosphate dehydrogenase (GAPDH) forward and reverse primers from Comate Bioscience (Jilin, China); TRIzol and transipid transfer reaction from Invitrogen (California, USA); SYBR Green Mix Real-time PCR, TOYOBO ReverTra Ace®qPCR from TOYOBO (Shanghai, China); DH5 α sensitive cell, endotoxin-free plasmid kit and RNA-free water purchased from Tiangen (Beijing, China); Dual-Luciferase report vector pmiR-RB REPORT from Ruibo (Guangzhou, China); Dual-luciferase reporter gene detection kit from Promega (Wisconsin, USA); fetal bovine serum, Opti MEM serum-free medium, and flow cytometry apoptosis detection kit from GBICO (New York, USA), Tuoran (Shanghai, China), and Kaiji Biology (Jiangsu, China), respectively; antibodies for APLN, Bax, Bcl-2, caspase-3, p-AKT, mGluR1, and β-actin from Abcam (Shanghai, China); and goat anti-rabbit antibody from Proteintech (Wuhan, China).
Hippocampal Neurons of Epilepsy Models
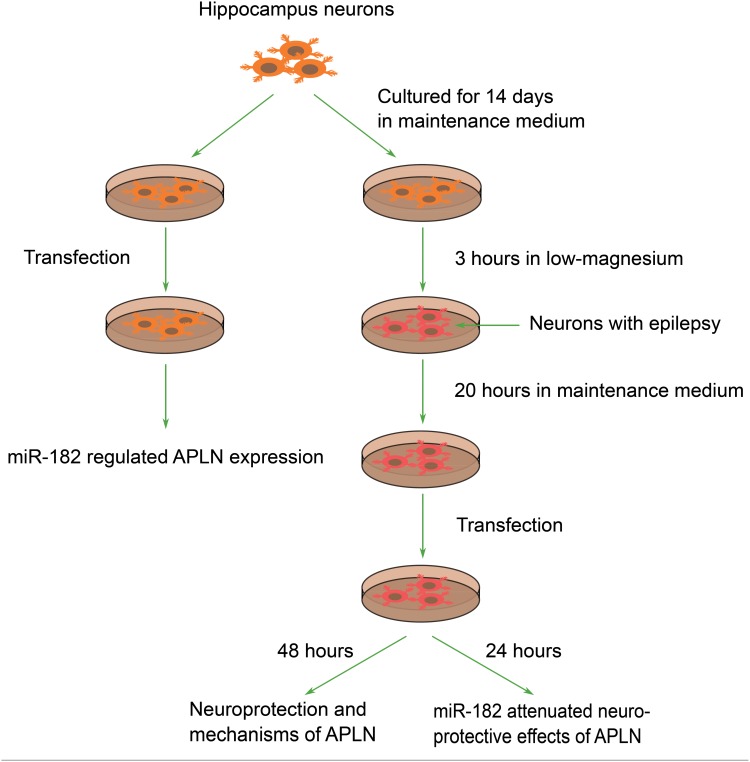
Hippocampal neurons of epilepsy models were established with a low manganese solution. Maintenance medium was dropped after the hippocampal neurons were cultured for 14 days. Then, the neurons were treated with artificial cerebrospinal fluid containing low magnesium solution for 3 hrs to generate a low-magnesium model of epilepsy. After stimulation with low magnesium solution, the neurons were cultured in maintenance medium for an additional 20 hrs. Thereafter, the neurons were transfected with different vectors for subsequent experiments, and the protocol for these experiments is presented in Figure 1. For the regulation of APLN expression, pBI-CMV3-APLN overexpression, short hairpin RNA negative control (shRNA-NC), or interference APLN shRNA plasmids were transfected into neurons. For the regulation of miR-182 expression, neurons were transfected with miR-182 mimics, miR-182 inhibitors, or miRNA negative control.
Figure 1.
Protocol used for in vitro experiments in this study.
Epileptic Rat Model Establishment
Intraperitoneal injection of 1% pentylenetetrazol (PTZ) at a dose of 3.5 mL/kg was used to induce epilepsy in rats. Five hours after the injection, behavioral changes and spontaneous seizure occurrence were recorded. The intensity of seizures was assessed by Racine scoring (0–5 points), as follows:22 stage 0, no response; stage 1, facial movements with vellication of ears and whiskers; stage 2, myoclonic jerks without rearing; stage 3, clonus of one forelimb; stage 4, rearing with bilateral forelimb clonus; stage 5, generalized tonic-clonic seizures.
Full rat kindling was achieved when the rats reached stage 4 or 5 seizures after 3 successive doses of PTZ. From the fourth day, PTZ injection was performed every other day to maintain kindled status. If epilepsy kindling was not achieved during the first 3 days, an additional dose of 10 mg/kg PTZ was injected to induce kindling every 10 min for a maximum of 4 times.
After the animal model was established, the rats were randomly divided into four groups and treated with Lipofectamine 2000 with saline (control group) or different vectors [APLN overexpression (APLN up-regulation group), APLN shRNA (APLN down-regulation group), or miR-182 agomir (miR-182 up-regulation group)] every 3 days for 4 weeks. Subsequently, the rats were sacrificed, and the hippocampus tissues were isolated and preserved in liquid nitrogen for subsequent experiments.
Cell Transfection
Twenty-four hours before transfection, rat hippocampal neurons were seeded into a 6-well culture plate. Cell transfection was performed when the cell confluence area was 80–90%. Transfection was performed using FuGene HD transfection reagents according to the manufacturers’ protocol. Culture medium containing 10% serum (150 μL), various vectors (4 μg), and FuGene HD (7.5 μL) was incubated for 15 min at room temperature. Culture medium was changed 24 hrs after transfection, and dead cells were removed.
Flow Cytometry Analysis
Twenty-four or 48 hrs after transfection, the neurons were washed twice with phosphate-buffered saline (PBS); subsequently, single-cell suspensions were prepared with a concentration of 1 × 106 cells/mL using 1× binding buffer. Cells (2×105 per tube) were stained using Annexin V and pyridinium iodide for 30 min at 4°C under dark environment.
Western Blotting
Cells were washed three times with cold PBS, and total protein was extracted using a radioimmunoprecipitation assay (RIPA) lysis buffer on ice; protein (10 μL) and protein loading buffer (10 μL) were mixed. Proteins were separated by 10% sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE) and transferred onto 0.22 mm polyvinylidene fluoride membrane using a semi-dry transfer cell. The following antibodies were used: anti-mGluR1, anti-p-AKT, anti-Bax, anti-caspase-3, anti-Bcl-2, and anti-β-actin antibodies. The protein bands were visualized using the enhanced chemiluminescence (ECL) detection kit on the ECL detection system.
Quantitative Reverse Transcriptase Polymerase Chain Reaction (qRT-PCR)
TRIzol and RNeasy kit with DNase I digestion were used to isolate total RNA according to the manufacturers’ instructions. Reverse transcription reactions were performed using the TOYOBO ReverTra Ace®qPCR Kit, and diluted cDNA was used for qRT-PCR analysis using SYBR Premix Ex Taq II Kit. For miRNA, stem-loop reverse transcription reactions were carried out, and the 2−△Ct method was used to calculate the abundance of RNA genes relative to GAPDH or U6 expression. Sequences of reverse transcription primers and fluorescence quantitative primers are listed in Table 1.
Table 1.
Sequences of Reverse Transcription Primers and Fluorescence Quantitative Primers
| Symbol | Primer | Sequence (5ʹ-3ʹ) |
|---|---|---|
| miR-182-5p | RT-Primer | CTCAACTGGTGTCGTGGAGTCGGCAATTCAGTTGAGAGTGTGAG |
| F-Primer | TCGGCAGG TTTGGCAATGGTAGAACT | |
| R-Primer | CTCAACTGGTGTCGTGGA | |
| APLN | F-Primer | GTCTCCTCCATAGATTGGTCTGC |
| R-Primer | GGAATCATCCAAACTACAGCCAG | |
| GAPDH | F-Primer | CGGAGTCAACGGATTTGGTCGTAT |
| R-Primer | AGCCTTCTCCATGGTGGTGAAGAC | |
| U6 | RT-Primer | AACGCTTCACGAATTTGCGT |
| F-Primer | CTCGCTTCGGCAGCACA | |
| R-Primer | AACGCTTCACGAATTTGCGT |
Dual-Luciferase Reporter Gene System
Hippocampal neurons were seeded into 24-well plates. After 24 hrs, the cells were contransfected with miR-182 mimics or mimic controls (Promega) along with APLN wide-type construct or the mutant version with Lipofectamine 2000 according to the manufacturer’s protocol. The cells were cultured for 48 hrs after transfection; subsequently, the firefly and Renilla luciferase activities were quantified using the dual‐luciferase reporter assay system. The reporter activity of each well was expressed as the relative luciferase expression normalized to the Renilla activity.
Statistical Analysis
GraphPad Prism (version 7.0) was used to plot graphs and process data. Data were presented as mean ± standard errors of mean (SEM). One-way analysis of variance (ANOVA) with Scheffe post hoc test was used to find statistically significant differences among the studied groups. A two-tailed P-value <0.05 was considered statistically significant.
Results
Protective Effect of APLN on Neuronal Injury in Epilepsy
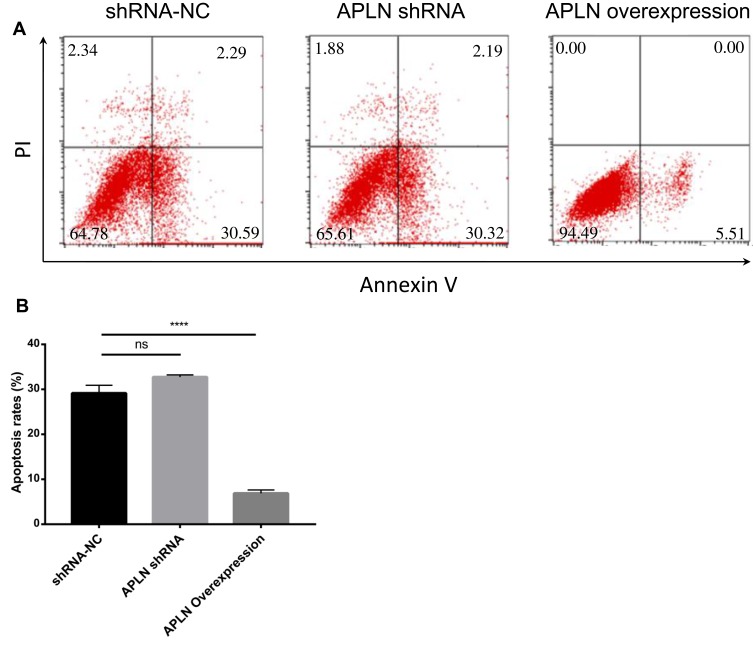
Neuronal injury plays a pivotal role in the pathogenesis of epilepsy, and APLN was reported to be a protective peptide against neuronal injury.17,18 In this study, firstly, we confirmed the neuronal protective effect of APLN on the hippocampal neurons. Forty-eight hours after transfection, the apoptosis rate of neurons decreased significantly in the APLN overexpression group than in the APLN down-regulation and control groups (Figure 2A and B). Interestingly, the neurons treated with APLN overexpression plasmid only showed early apoptosis, while those treated with control and APLN shRNA presented with both early and late apoptosis phases (Figure 2A). Although the apoptosis of neurons in the APLN overexpression group decreased significantly, it was not significantly lower in the APLN low expression group than in the control group (Figure 2B).
Figure 2.
Protective effect of APLN against apoptosis of neurons. Hippocampal neurons of epileptic models were transfected with pBI-CMV3-APLN overexpression, short hairpin RNA negative control (shRNA-NC), or interference APLN shRNA plasmids. Forty-eight hours post-transfection, apoptosis was determined by flow cytometry. (A) Representative figure of flow cytometry; (B) Statistical results of these groups. Data are presented as mean ± SEM of three independent experiments. ns, non-significant; ****P < 0.0001.
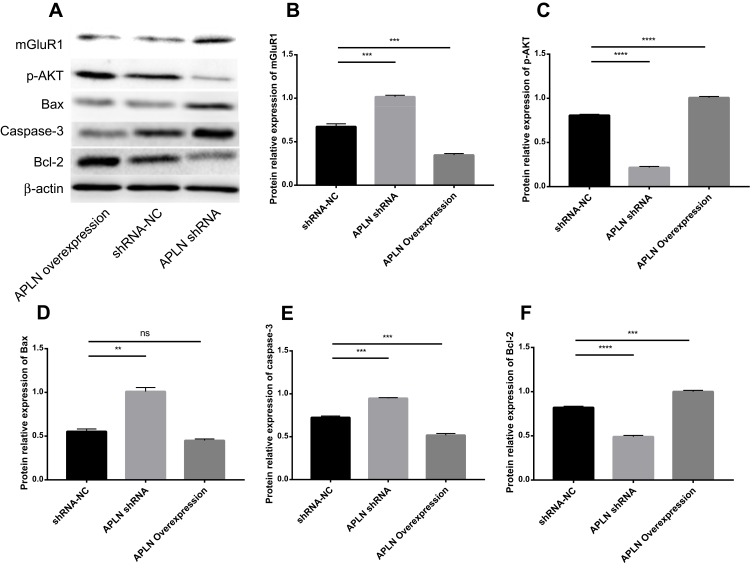
Mechanisms of Neuroprotective Effect of APLN on Neurons with Epilepsy
Metabotropic glutamate receptors (mGluR), particularly mGluR1, play very important roles in neuronal injury and the occurrence of epilepsy.23 We found that the up-regulation (down-regulation) of APLN expression could significantly decrease (increase) mGluR1 expression (Figure 3A and B). Phosphorylated AKT was an important downstream signal molecule for APLN to play a neuroprotective effect.24 Phosphorylated-AKT (p-AKT) levels were higher and lower in the up-regulation and down-regulation groups, respectively, than in the control group (Figure 3A and C). Overexpression of APLN could up-regulate Bcl-2 expression, and down-regulate caspase-3 expression (Figure 3A and D–F). Inhibiting APLN expression could down-regulate Bcl-2 expression and up-regulate caspase-3 and Bax expression (Figure 3A and 3–F). Furthermore, using the epilepsy rat model, we confirmed the above-mentioned phenomena (Supplementary Figures 1 and 2). Collectively, those results indicated that APLN could play its neuroprotective effects via inhibiting the expression of mGluR1 and pro-apoptosis proteins, promoting anti-apoptosis protein expression, and increasing p-AKT levels in neurons.
Figure 3.
Influence of APLN on the expression of apoptosis-associated proteins, mGluR1, and p-AKT levels. Hippocampus neurons of epileptic models were transfected with pBI-CMV3-APLN overexpression, short hairpin RNA negative control (shRNA-NC), or interference APLN shRNA plasmids. Forty-eight hours post-transfection, protein expression was evaluated by Western blotting. β-actin was used as a loading control. (A) Western blotting was used to examine the protein levels of mGluR1, p-AKT, Bax, caspase-3, and Bcl-2. Statistical results of mGluR1 expression (B), p-AKT levels (C), Bax expression (D), caspase-3 expression (E), and Bcl-2 expression (F) in different groups. ns, non-significant; **P < 0.01, ***P < 0.001, ****P < 0.0001.
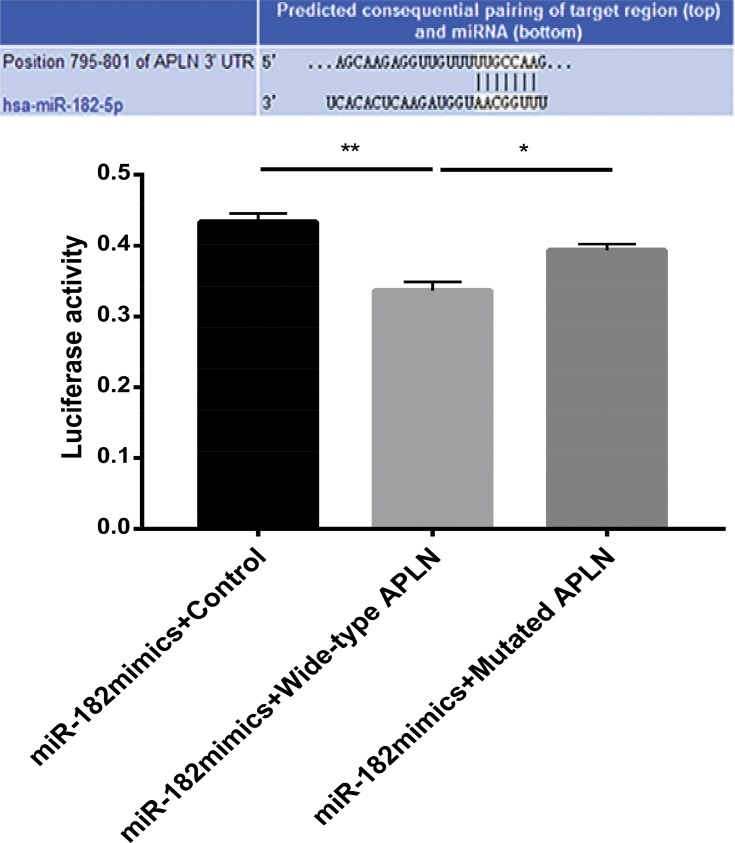
APLN Is a Target Gene for miR-182
MicroRNAs play important roles in gene expression, and miR-182 is a brain-specific miRNA, which plays a critical role in ischemia-related neuronal injuries.25,26 Using the bioinformatics software, the target genes of miR-182 were predicted. Totally, there are 1310 transcripts, including those in 1515 conservative binding sites and 558 relatively poor conservative binding sites. APLN was a target gene for miR-182; the latter can specifically bind to the sequence in 3ʹ-UTR (795-801bp) of APLN gene (Supplementary Figure 3).
Dual-Luciferase reporter gene system was used to verify the interaction of miR-182 and APLN gene. MiR-182 mimics plus control (group A), APLN wide-type gene (group B), or mutated gene in miR-182 binding site (group C) reporter vectors were transfected into neurons. The luciferase activity of neurons in group B was significantly lower than those in groups A and C (both P < 0.05) (Figure 4). Furthermore, there was no significant difference between groups A and C regarding luciferase activity.
Figure 4.
Detection of luciferase activity by dual-luciferase reporter gene. Neurons were transfected with miR-182 mimics combined with control, wide-type APLN, and mutated APLN in miR-182 binding site report vectors. *P < 0.05, **P < 0.01.
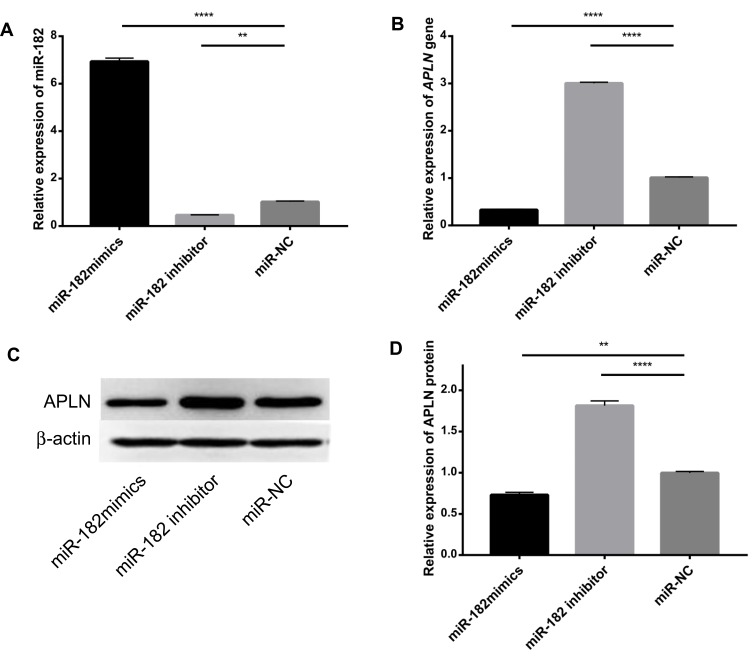
qRT-PCR showed that the expression of miR-182 increased significantly in the miR-182 mimics group and decreased in the miR-182 inhibitor group, which suggested the success of regulation of miR-182 expression (Figure 5A). mRNA of the APLN gene was significantly lower in the miR-182 mimics group and higher in the miR-182 inhibitor group than in the control group (Figure 5B). The influence of miR-182 on APLN protein expression was also confirmed by Western blotting (Figure 5C and D). These results suggested the direct binding effect of miR-182 to APLN gene and the negative regulation of APLN gene expression by miR-182.
Figure 5.
Relative expression of miR-182 and APLN in neurons. Neurons were transfected with miRNA negative control (miR-NC), miR-182 mimics, or miR-182 inhibitors. Twenty-four hours post-transfection, the expression of miR-182 was examined by qRT-PCR, and the expression of APLN was examined by qRT-PCR and Western blotting. (A) Relative expression of miR-182 determined by qRT-PCR. (B) Relative expression of APLN gene determined by qRT-PCR. (C, D) Western blotting analysis for APLN protein expression. **P < 0.01, ****P < 0.0001.
miR-182 Negatively Impacts the Neuroprotective Effect of APLN
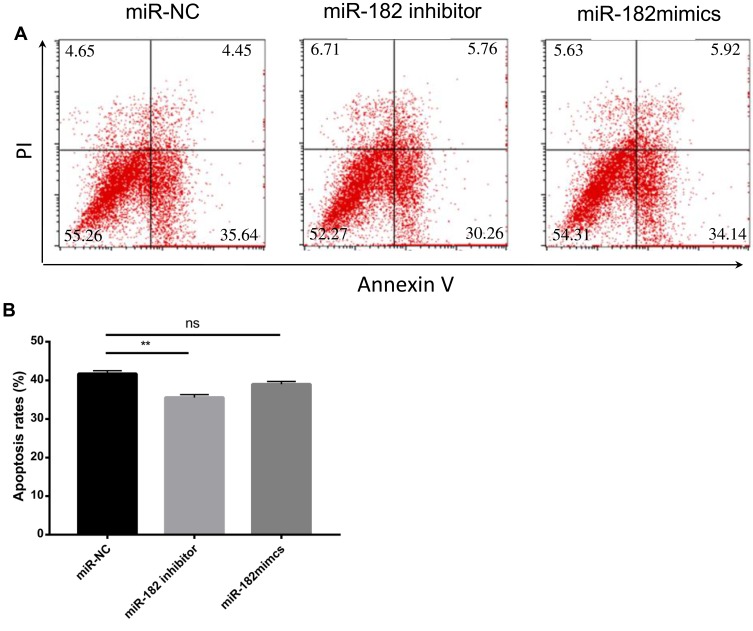
Whether the regulation of APLN gene expression by miR-182 could impact neurons was subsequently determined. Neurons of epilepsy model treated with miR-182 inhibitor showed significantly lower apoptosis rate than those treated with control and miR-182 mimics (Figure 6A and B). Down-regulation of miR-182 expression could significantly inhibit the expression of pro-apoptosis proteins, Bax, and caspase-3 and promote the anti-apoptosis protein (Bcl-2) expression (Figure 7). Such regulation effect was also confirmed by in vivo experiments (Supplementary Figure 2).
Figure 6.
Impact of miR-182 on apoptosis of neurons. Epileptic neurons were transfected with miR-NC, miR-182 inhibitor, and miR-182 mimics. Twenty-four hours post-transfection, apoptosis was determined by flow cytometry. (A) Representative figure of flow cytometry; (B) Statistical results of these three groups. Data are presented as mean ± SEM of three independent experiments. ns, non-significant; **P < 0.01.
Figure 7.
Influence of miR-182 on the expression of apoptosis-associated proteins. Neurons of epilepsy were transfected with control miR-NC, miR-182 inhibitor, and miR-182 mimics. Twenty-four hours post-transfection, protein expression was evaluated by Western blotting. β-actin was used as a loading control. (A) Western blotting was used to examine the protein levels of Bax, caspase-3, and Bcl-2. Statistical results of Bax expression (B), caspase-3 expression (C), Bcl-2 expression (D) in different groups. ns, non-significant; *P < 0.05, **P < 0.01, ***P < 0.001, ****P < 0.0001.
Discussion
Neuronal injury or neuronal death is involved in multiple human diseases including epilepsy.27 Although the possibility that isolated brief seizure may not induce cell death, severe and repetitive seizures can undoubtedly activate neuronal death progress.28 It is well known that repeated brief seizures lead to progressive hippocampal neuron loss and spatial memory deficits.29 It is debated whether neuronal injury is a cause or consequence of repeated seizures, but experimental data indicate that rats with seizure-induced hippocampal damage show prolonged episodes of recurrent seizures and more frequent severe epileptic seizures.30 Furthermore, seizure-induced damage should be regarded not only as neuronal loss but also as adverse long-term behavioral and cognitive consequences.31 Excitotoxicity is thought to be an important contributor for seizure-induced neuronal injury, in which excessive glutamatergic transmission leads to massive influx of calcium ions into cells, causing osmolytic stress and activation of cell death pathways, ultimately leading to the death of the neuron.6 mGluR is expressed in key regions of the cortex and the thalamus and are known to regulate spike and wave discharges.32 Up-regulation of mGluR1 mRNA and protein occurs in the hippocampus of different animal models of epilepsy, suggesting that it may be involved in the neuronal hyperexcitability, loss, and subsequent epileptogenesis at acute stages after status epilepticus or kindling.23 Stimulation of group I mGluRs elicits epileptogenesis, while group I mGluR antagonist 2-methyl-6-(phenylethynyl)-pyridine prevents status epilepticus and subsequent neuronal loss and epileptogenesis.23 Hence, targeting the cellular machinery via pharmacological or genetic ways for epilepsy control or treatment attracts tremendous interests in many studies.
APLN is a ligand of the APJ receptor that belongs to the G protein-coupled receptor family.33 APLN and APJ are widely distributed in the body and play potential physiological roles in the cytoprotection of many internal organs.33 In children with generalized epilepsy, APLN level could be significantly higher in the valproic acid (VPA) treatment group than in the control group, which suggested that VPA may play its role by regulating APLN expression.34 In patients with drug-refractory temporal lobe epilepsy, the expression of APLN in the hippocampus and adjacent cortex was significantly higher than that in a normal control, which could also be observed in rats with lithium-pilocarpine-induced epilepsy.35 Hence, a responsive increase of the APLN peptide level may be a protective mechanism against epilepsy. The neuroprotective effects of APLN in animals with epilepsy were also reported in two recent studies.17,18 In this study, we first explored the protective effects of APLN on neuronal injury in epilepsy. Both in vivo and in vitro experiments showed that APLN could significantly inhibit the apoptosis of hippocampal neurons. The mechanisms involved are the up-regulation of Bcl-2 expression and down-regulation of Bax and caspase-3 expression. For the first time, we found that APLN overexpression could inhibit the expression of mGluR1. Interestingly, up-regulation of APLN expression could significantly decrease the apoptosis of hippocampal neurons, but down-regulation of APLN expression did not obviously increase neuron apoptosis (Figures 1B and 5B). This suggested that other factors may contribute to the neuroprotective effects when APLN expression is low, and up-regulating ALPN expression was a potential intervention strategy for epilepsy.
miRNAs, as non-coding RNAs, play a regulatory role at the post-transcriptional level and are related to a variety of diseases, providing a new intervention target for disease diagnosis and treatment.19 As a specific brain miRNA, miRNA-182 is abundant in the adult and embryonic brain25,26 and participates in the transformation of neural stem cells to mature neural cells.36 In the present study, we used a bioinformatics software to predict that APLN was a target gene for miR-182, a finding that was also confirmed experimentally using the dual-luciferase reporter gene system. Function experiments showed that miR-182 could inhibit the expression of APLN gene at both mRNA and protein levels. Up-regulation of miR-182 could attenuate the protective effects of APLN on neuronal injury in epilepsy.
Conclusions
APLN mediated its protective effects against neuronal injury in epilepsy via regulating apoptosis-associated protein expression, inhibiting mGluR1 pathway, and increasing p-AKT level in neurons. Moreover, we found that miR-182 could negatively regulate the expression of APLN and influence its neuroprotective effects. As a result, miR-182/APLN is a potential target for epilepsy control or treatment.
Acknowledgments
We thank the Department of Geriatric Medicine, The First Hospital of Jilin University, for their assistance in this work. This work was supported by the Youth Developmental Foundation of First Hospital of Jilin University (No. JDYY92018033).
Disclosure
The authors declare no conflicts of interest.
References
- 1.Méndez-Armenta M, Nava-Ruíz C, Juárez-Rebollar D, Rodríguez-Martínez E, Gómez PY. Oxidative stress associated with neuronal apoptosis in experimental models of epilepsy. Oxid Med Cell Longev. 2014;2014:293689. doi: 10.1155/2014/293689 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Paudel YN, Semple BD, Jones NC, Othman I, Shaikh MF. High mobility group box 1 (HMGB1) as a novel frontier in epileptogenesis: from pathogenesis to therapeutic approaches. J Neurochem. 2019;151(5):542–557. doi: 10.1111/jnc.v151.5 [DOI] [PubMed] [Google Scholar]
- 3.Rana A, Musto AE. The role of inflammation in the development of epilepsy. J Neuroinflammation. 2018;15(1):144. doi: 10.1186/s12974-018-1192-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pitkänen A, Sutula TP. Is epilepsy a progressive disorder? Prospects for new therapeutic approaches in temporal-lobe epilepsy. Lancet Neurol. 2002;1(3):173–181. doi: 10.1016/S1474-4422(02)00073-X [DOI] [PubMed] [Google Scholar]
- 5.Voutsinos-Porche B, Koning E, Kaplan H, et al. Temporal patterns of the cerebral inflammatory response in the rat lithium-pilocarpine model of temporal lobe epilepsy. Neurobiol Dis. 2004;17(3):385–402. doi: 10.1016/j.nbd.2004.07.023 [DOI] [PubMed] [Google Scholar]
- 6.Henshall DC. Apoptosis signalling pathways in seizure-induced neuronal death and epilepsy. Biochem Soc Trans. 2007;35(Pt 2):421–423. doi: 10.1042/BST0350421 [DOI] [PubMed] [Google Scholar]
- 7.Farrell JS, Wolff MD, Teskey GC. Neurodegeneration and pathology in epilepsy: clinical and basic perspectives. Adv Neurobiol. 2017;15:317–334. [DOI] [PubMed] [Google Scholar]
- 8.Hossain MA. Molecular mediators of hypoxic-ischemic injury and implications for epilepsy in the developing brain. Epilepsy Behav. 2005;7(2):204–213. doi: 10.1016/j.yebeh.2005.05.015 [DOI] [PubMed] [Google Scholar]
- 9.Yan BC, Xu P, Gao M, et al. Changes in the blood-brain barrier function are associated with hippocampal neuron death in a kainic acid mouse model of epilepsy. Front Neurol. 2018;9:775. doi: 10.3389/fneur.2018.00775 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhang SH, Liu D, Hu Q, Zhu J, Wang S, Zhou S. Ferulic acid ameliorates pentylenetetrazol-induced seizures by reducing neuron cell death. Epilepsy Res. 2019;156:106183. doi: 10.1016/j.eplepsyres.2019.106183 [DOI] [PubMed] [Google Scholar]
- 11.Chen C, Mei Q, Wang L, et al. TIGAR suppresses seizures induced by kainic acid through inhibiting oxidative stress and neuronal apoptosis. Biochem Biophys Res Commun. 2019;515(3):436–441. doi: 10.1016/j.bbrc.2019.05.156 [DOI] [PubMed] [Google Scholar]
- 12.Cheng B, Chen J, Bai B, Xin Q. Neuroprotection of apelin and its signaling pathway. Peptides. 2012;37(1):171–173. doi: 10.1016/j.peptides.2012.07.012 [DOI] [PubMed] [Google Scholar]
- 13.Liu DR, Hu W, Chen GZ. Apelin-12 exerts neuroprotective effect against ischemia-reperfusion injury by inhibiting JNK and P38MAPK signaling pathway in mouse. Eur Rev Med Pharmacol Sci. 2018;22(12):3888–3895. doi: 10.26355/eurrev_201806_15273 [DOI] [PubMed] [Google Scholar]
- 14.Duan J, Cui J, Yang Z, et al. Neuroprotective effect of Apelin 13 on ischemic stroke by activating AMPK/GSK-3β/Nrf2 signaling. J Neuroinflammation. 2019;16(1):24. doi: 10.1186/s12974-019-1406-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Foroughi K, Khaksari M, Rahmati M, Bitaraf FS, Shayannia A. Apelin-13 protects PC12 cells against methamphetamine-induced oxidative stress, autophagy and apoptosis. Neurochem Res. 2019;44(9):2103–2112. doi: 10.1007/s11064-019-02847-9 [DOI] [PubMed] [Google Scholar]
- 16.Zhu J, Gao W, Shan X, et al. Apelin-36 mediates neuroprotective effects by regulating oxidative stress, autophagy and apoptosis in MPTP-induced Parkinson’s disease model mice. Brain Res. 2019;1726:146493. doi: 10.1016/j.brainres.2019.146493 [DOI] [PubMed] [Google Scholar]
- 17.Kalantaripour TP, Esmaeili-Mahani S, Sheibani V, Najafipour H, Asadi-Shekaari M. Apelin-13 protects rat primary cortical glia-neuron co-culture against pentylenetetrazole-induced toxicity. Biomed Pharmacother. 2017;87:661–668. doi: 10.1016/j.biopha.2016.12.131 [DOI] [PubMed] [Google Scholar]
- 18.Kalantaripour TP, Esmaeili-Mahani S, Sheibani V, Asadi-Shekaari M, Pasban-Aliabadi H. Anticonvulsant and neuroprotective effects of apelin-13 on pentylenetetrazole-induced seizures in male rats. Biomed Pharmacother. 2016;84:258–263. doi: 10.1016/j.biopha.2016.09.048 [DOI] [PubMed] [Google Scholar]
- 19.Mohr AM, Mott JL. Overview of microRNA biology. Semin Liver Dis. 2015;35(1):3–11. doi: 10.1055/s-00000069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Liao YC, Wang YS, Hsi E, Chang MH, You YZ, Juo SH. MicroRNA-765 influences arterial stiffness through modulating apelin expression. Mol Cell Endocrinol. 2015;411:11–19. doi: 10.1016/j.mce.2015.04.006 [DOI] [PubMed] [Google Scholar]
- 21.Zhou Y, Zhao M, Du Y, et al. MicroRNA-195 suppresses the progression of lung adenocarcinoma by directly targeting apelin. Thorac Cancer. 2019;10(6):1419–1430. doi: 10.1111/1759-7714.13087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Racine RJ. Modification of seizure activity by electrical stimulation. II. Motor seizure. Electroencephalogr Clin Neurophysiol. 1972;32(3):281–294. doi: 10.1016/0013-4694(72)90177-0 [DOI] [PubMed] [Google Scholar]
- 23.Qian F, Tang FR. Metabotropic glutamate receptors and interacting proteins in epileptogenesis. Curr Neuropharmacol. 2016;14(5):551–562. doi: 10.2174/1570159X14666160331142228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wang C, Wen J, Zhou Y, et al. Apelin induces vascular smooth muscle cells migration via a PI3K/Akt/FoxO3a/MMP-2 pathway. Int J Biochem Cell Biol. 2015;69:173–182. doi: 10.1016/j.biocel.2015.10.015 [DOI] [PubMed] [Google Scholar]
- 25.Ding X, Sun B, Huang J, et al. The role of miR-182 in regulating pineal CLOCK expression after hypoxia-ischemia brain injury in neonatal rats. Neurosci Lett. 2015;591:75–80. doi: 10.1016/j.neulet.2015.02.026 [DOI] [PubMed] [Google Scholar]
- 26.Kouri FM, Hurley LA, Daniel WL, et al. miR-182 integrates apoptosis, growth, and differentiation programs in glioblastoma. Genes Dev. 2015;29(7):732–745. doi: 10.1101/gad.257394.114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mao XY, Zhou HH, Jin WL. Redox-related neuronal death and crosstalk as drug targets: focus on epilepsy. Front Neurosci. 2019;13:512. doi: 10.3389/fnins.2019.00512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dingledine R, Varvel NH, Dudek FE. When and how do seizures kill neurons, and is cell death relevant to epileptogenesis? Adv Exp Med Biol. 2014;813:109–122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kotloski R, Lynch M, Lauersdorf S, Sutula T. Repeated brief seizures induce progressive hippocampal neuron loss and memory deficits. Prog Brain Res. 2002;135:95–110. [DOI] [PubMed] [Google Scholar]
- 30.Zhang X, Cui SS, Wallace AE, et al. Relations between brain pathology and temporal lobe epilepsy. J Neurosci. 2002;22(14):6052–6061. doi: 10.1523/JNEUROSCI.22-14-06052.2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yang W, Li J, Shang Y, et al. HMGB1-TLR4 axis plays a regulatory role in the pathogenesis of mesial temporal lobe epilepsy in immature rat model and children via the p38MAPK signaling pathway. Neurochem Res. 2017;42(4):1179–1190. doi: 10.1007/s11064-016-2153-0 [DOI] [PubMed] [Google Scholar]
- 32.Ngomba RT, van Luijtelaar G. Metabotropic glutamate receptors as drug targets for the treatment of absence epilepsy. Curr Opin Pharmacol. 2018;38:43–50. doi: 10.1016/j.coph.2018.01.012 [DOI] [PubMed] [Google Scholar]
- 33.Antushevich H, Wójcik M. Review: apelin in disease. Clin Chim Acta. 2018;483:241–248. doi: 10.1016/j.cca.2018.05.012 [DOI] [PubMed] [Google Scholar]
- 34.Meral C, Cekmez F, Vurucu S, et al. New adipocytokines (vaspin, apelin, visfatin, adiponectin) levels in children treated with valproic acid. Eur Cytokine Netw. 2011;22(2):118–122. doi: 10.1684/ecn.2011.0284 [DOI] [PubMed] [Google Scholar]
- 35.Zhang X, Peng X, Fang M, et al. Up-regulation of apelin in brain tissue of patients with epilepsy and an epileptic rat model. Peptides. 2011;32(9):1793–1799. doi: 10.1016/j.peptides.2011.08.006 [DOI] [PubMed] [Google Scholar]
- 36.Busskamp V, Krol J, Nelidova D, et al. miRNAs 182 and 183 are necessary to maintain adult cone photoreceptor outer segments and visual function. Neuron. 2014;83(3):586–600. doi: 10.1016/j.neuron.2014.06.020 [DOI] [PubMed] [Google Scholar]