ABSTRACT
Introduction
Pyrethroid compounds are widely used as insecticides. These compounds not only have a versatile application, but also have favourable toxicological profiles with high selectivity and toxicity to insects and low toxicity to humans. Despite this, there have been several reports of toxicity to humans in both occupational exposure and deliberate ingestional poisoning.
Classical presentation and treatment
Two classical syndromic presentations are described. Type I syndrome is characterised predominantly by tremors and is seen with exposure to type I pyrethroids. Type II pyrethroids, which are structurally modified type I pyrethroids with the addition of a cyano group, can result in type II syndrome characterized by choreo-athetosis and salivation. Mega-dose poisoning and mixed poisoning, particularly with organophosphorus compounds, is associated with significant toxicity and death. Treatment is supportive and symptomatic. A favourable outcome can be expected in most patients.
How to cite this article
Ramchandra AM, Chacko B, Victor PJ. Pyrethroid Poisoning. Indian J Crit Care Med 2019;23(Suppl 4):S267–S271.
Keywords: Insecticides, Poisoning, Pyrethroid
INTRODUCTION
Pyrethroids account for around a fourth of the insecticide market in industrial countries. These are widely used for insect control both at home (e.g., Baygon spray, mosquito repellents, and so on) and in agricultural fields for control of insects of the orders Coleoptera, Diptera, and Hemiptera. In addition, they are used for the treatment of scabies and lice in humans.1
Synthetic pyrethroids have been in use since 1940. They are derived from pyrethrins, which are natural substances found in the extract from the flower heads of Chrysanthemum cinerariaefolium. While the inherent toxic potential of pyrethroids is high, with LD50 ranging from 0.5 mg/kg to 250 mg/kg, especially for type II compounds,2 they are generally considered safe for humans.3 Its high selectivity and knock-down effects for insects, the slow dermal absorption in humans in view of the large body surface area, and rapid metabolism to the nontoxic metabolites are factors that result in low toxicity in humans.3
Despite this, there are reports that pyrethroid compounds may not be as safe as claimed previously.4 Given its widespread use as an insecticide, it is important to understand its potential toxicity in humans. This review aims at updating the current knowledge of pyrethroid toxicity in humans.
CHEMICAL STRUCTURE
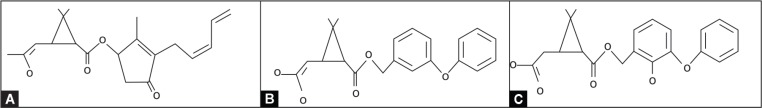
Natural pyrethrins are susceptible to destruction by light. In order to make pyrethrins more stable to light, the basic cyclopropane carboxylic ester structure of pyrethrins (Fig. 1A) was modified, resulting in the formation of synthetic pyrethroids (Fig. 1B). The addition of a cyano group to the basic structure (Fig. 1C) further enhances its insecticidal activity.3 Based on these structural differences and associated clinical manifestations, pyrethroids are categorized into two types. Type I pyrethroids are those without an alpha cyano group. Type II pyrethroids have an addition of a cyano group at the benzylic carbon atom.3 Type II pyrethroids are more potent insecticides due to the cyano group in their structure.5 Each type is associated with a distinct clinical syndrome as discussed later.
Fig. 1.
(A) Pyrethrin; (B) Type I pyrethroid without cyano group; (C) Type II pyrethroid with cyano group
MECHANISM OF ACTION
The mechanism of pyrethroid toxicity is complex due to its—action on several channels and proteins.6 Pyrethroids act mainly on sodium and chloride channels.2,7 Excitable (nerve and muscle) cells are hence the key targets of pyrethroid toxicity.
Pyrethroids have been found to modify the gating characteristics of voltage-sensitive sodium channels, thereby delaying their closure.2 This results in a protracted sodium influx (referred to as a sodium “tail current”), which if sufficiently large and/or long, lowers the action potential threshold, and causes repetitive firing. The amplitude of the current depends on the pyrethroid concentration and the number of affected sodium channels.2 The duration of the current however mainly depends on the type of compound; type II pyrethroids have been found to have a longer duration. At high pyrethroid concentrations, the sodium tail current may increase to the extent that it blocks further action potential generation and a “conduction block” can result. This action on the sodium channels may be the mechanism responsible for the clinical features of paraesthesia3 and proarrhythmogenic potential.8
Pyrethroids have also decreased chloride channel currents in the brain, nerves, muscles, and salivary glands.7 It is possible that these results in salivation and myotonia. Type II pyrethroids act on the voltage-dependent chloride channels and this action probably contributes significantly to the features of poisoning with type II compounds. At relatively high concentrations, pyrethroids can also act on gamma amino butyric acid (GABA)-gated chloride channels,3 which may be responsible for the seizures seen with severe type II poisoning. Ivermectin and pentobarbital, which open chloride channels, antagonize these effects and hence may be beneficial in the treatment of these effects. Further studies are however needed to better understand this action on chloride channels.6
TOXICOKINETICS
Pyrethroids are lipophilic compounds and are distributed extensively in the body in the liver, stomach, intestine, adipose tissues, nervous system, and kidneys.3 Despite its lipophilic nature, no bioaccumulation was observed after subacute dosing to mammals.9 They are generally poorly absorbed through the skin in humans and are rapidly metabolized by ester cleavage, hydroxylation, and conjugation in the liver.3 Various hydrophilic metabolites are excreted in the urine.3 In a study where cypermethrin was given to volunteers, peak excretion in the urine was found between 8 hours and 24 hours; however, reports of pyrethroid being detectable in the urine as late as 14 days have also been reported.3
As mentioned earlier, pyrethroids are generally highly selective for insects. In view of increasing insecticidal resistance, synthetic pyrethroids have been modified in ways described below. These have potentiated pyrethroids’ toxicity in humans.
Pyrethroid synergists: synthetic pyrethroids are now manufactured by combining them either with piperonyl butoxide10 or organophosphorus compounds.11 Piperonyl butoxide is a synergistic compound that inhibits the normal metabolic degradation of pyrethroids, thereby decreasing pesticide resistance. Organophosphorus compounds may enhance the toxicity of pyrethroids by inhibiting its detoxification by carboxylesterases.11 A summary of the effects of these synergists on pyrethroid absorption and metabolism is given in Table 1. These combinations not only enhance the insecticidal potency but also their toxicity in humans.
Stereoisomeric combination: pyrethroids exist in various stereoisomer forms.3 Generally, the cis-isomers are more toxic than trans-isomers.12 The insecticidal activity and human toxicity are stereospecific. In general, stereoisomers showing the highest levels of insecticidal activity are also most toxic to humans.6
Vehicle for use: the vehicle for the delivery of the pyrethroid has also been shown to impact toxicity. Pyrethroid with corn oil has been noted to have much lower LD50 than with water.13
Table 1.
Summary of the effects of synergists on pyrethroid absorption and metabolism
| Pyrethroids | Pyrethroids with piperonyl butoxide | Pyrethroids with organophosphorus (OP) compounds | |
|---|---|---|---|
| Absorption | Dermal absorption poor; maximum 1.5%;3 when orally administered, 19–50% cypermethrin absorbed | Dermal absorption increases to approximately 8%;3 following ingestion 70% or more of the administered dose absorbed | Higher absorption of ingested dose |
| Metabolism | Rapid metabolism in the liver by oxidation, hydrolysis, and conjugation reactions3 | Inhibition of CYP mono-oxygenase enzymes by up to 50% within 3 hours;3 does not return to normal until about 36 hours | OP inhibit carboxyesterases responsible for pyrethroid hydrolysis11 |
CLINICAL MANIFESTATIONS
Given the wide availability of pyrethroids in the form of household repellants and other insecticides, pyrethroid toxicity is common.
Acute Toxicity
Pyrethroid toxicity in humans can be due to occupational exposure through skin contact or inhalation of sprays or ingestion of pyrethroid compounds. In the largest published series of 573 cases of acute pyrethroid poisoning,14 229 were due to occupational exposure and 344 were due to accidental exposure, primarily ingestion. Common reported symptoms included facial paraesthesia, skin itching, skin burning, dizziness, nausea, vomiting, and more severe cases of muscle fasciculations.14
Based on acute exposure to pyrethroids in animal studies, two distinct toxidromes (Table 2) have been identified. Exposure to type I pyrethroids results in reflex hyperexcitability and fine tremors or the T syndrome or type I syndrome.15 Incoordination, choreoathetosis, seizures, direct effects on the skeletal and cardiac muscle, and salivary gland, also known as choreoathetosis–salivation or type II syndrome is caused by type II pyrethroids.15
Table 2.
Commercially available pyrethroids and their clinical features
| Type I compounds | Type II compounds | Organophosphorus (OP)–pyrethroid combination |
| Allethrin | Cyfluthrin (Baygon) | Cypermethrin–ethion |
| Bifenthrin | Cyhalothrin | Deltamethrin–triazophos |
| Permethrin | Cypermethrin | Deltamethrin–chlorpyrifos |
| Phenothrin | Deltamethrin | Chlorpyrifos–cypermethrin |
| Prallethrin | Fenvalerate | |
| Resmethrin | Fenpropathrin | |
| Tefluthrin | Tralomethrin | |
| Teramethrin | ||
| Type I syndrome “T syndrome” | Type II syndrome “CS syndrome” | Organophosphorus–pyrethroid |
| Severe fine tremor | Choreoathetosis | Presentation depends on proportion of OP and pyrethroid |
| Marked reflex hyperexcitability sympathetic activation | Salivation | Combination associated with lower ventilator-free days compared with individual compounds |
| Paresthesia (dermal exposure) | Coarse tremor | |
| Increased extensor tone | ||
| Moderate reflex hyperexcitability sympathetic activation |
Acute poisoning rarely poses a life-threatening risk but severe poisoning with mortality risk can occur if large quantities of pyrethroid compounds are ingested. Life-threatening manifestations mentioned in the literature are seizures, coma, pulmonary edema, and hemorrhage.3
Atypical manifestations are usual in pyrethroid poisoning. In a series of 59 patients presenting to the emergency department in Korea, approximately 40% of patients had atypical manifestations.16 These included low sensorium (34%), respiratory failure requiring ventilator support (18%), acute kidney injury (11%), hypotension (10%), pneumonia (7%), and seizures (4%). Two patients in this series died. Ingestion of more than 250 mL and serum lactate of more than 3.5 mmol were found to predict atypical presentation.16 Recently, there have been increasing numbers of reports of pyrethroid poisoning presenting with status epilepticus.17 Extremely rare reports of complete heart block18 and myelopathy19 have also been published.
Hyperglycemia has been reported to be associated with adverse outcomes in pyrethroid poisoning.20 In a study on 104 patients with type II pyrethroid poisoning, hyperglycemia is associated with complications of respiratory failure, acidosis, and hypotension. Increases in adrenergic activity have been postulated to be the cause of hyperglycemia.20
Pyrethroids, when combined with organophosphorus compounds are associated with increased toxicity in human poisoning. In a study that compared the clinical profile and outcome of patients with isolated chlorpyrifos (n = 20) or cypermethrin poisoning (n = 32) with combination (cypermethrin–chlorpyrifos) poisoning (n = 32), patients with organophosphorus–pyrethroid poisoning were found to have lower ventilator-free days compared with patients with either poisoning alone.21 Mortality was not significantly different. Although the potentiation of toxicity in combination is considered due to increased toxicity of pyrethroid due to inhibition of detoxification of pyrethroid by organophosphorus compounds, the study noted that organophosphate manifestations were predominant in combined poisoning. The higher concentration of chlorpyrifos (50%) in the organophosphorus–pyrethroid combination compared with the single chlorpyrifos formulation (20%) is likely to have contributed to the predominance and persistence of cholinergic manifestations in the combination.21 In contrast, in another study that reported patients who had ingested 1:4 combination of methyl parathion (organophosphate):λ-cyhalothrin (pyrethroid), manifestations were primarily that of the pyrethroid compound.22 The predominance of cholinergic or pyrethroid symptomatology thus appears to be dependent on the proportion of organophosphorus compound and pyrethroid in the pesticide formulation.21
Chronic Exposure
In general, no chronic toxicity has been demonstrated in animal or human studies with pyrethroid exposure. Animal studies have shown that pyrethroids can affect the immune system at very high doses and can also cause neurobehavioral effects with chronic exposure. In a cross-sectional study from Bolivia of 116 pesticide sprayers, the prevalence of abnormal glucose regulation (defined as HbA1c ≥ 5.6%) was found to be higher in this pesticide sprayers compared with nonexposed controls. Among sprayers who had used only pyrethroids, a significant trend was observed between cumulative pesticide exposure and abnormal glucose regulation.23 In another study from China that included 176 children aged 0–14 years and 180 controls, those with the highest quartile of total and individual metabolites had a two-fold increase in the risk of acute lymphocytic leukemia compared with those in the lowest quartiles.24
MANAGEMENT
The diagnosis of pyrethroid poisoning is based mainly on the clinical presentation and compound identification on the container brought by the patient or relatives. The role of high-resolution gas chromatography-negative chemical ionization mass spectrometry to measure metabolites is unclear in the diagnosis of pyrethroid poisoning.
Management is largely supportive and symptomatic because there is no available antidote. Optimization of the airway, breathing, and circulation is vital, as is for any patient who comes with acute poisoning. Immediate decontamination of skin with soap and water can be considered; however, there is no evidence that it reduces toxicity. Gastric lavage is best avoided in the case of pyrethroid ingestion as the risk of aspiration pneumonia with the solvent is high.3 Evidence for the use of activated charcoal is limited; however, this can be considered if the patient presents within 1 hour of ingestion.
Seizures should be adequately controlled with antiepileptic therapy. Experimental data in mice suggest that benzodiazepines compared with phenobarbital may be more effective in controlling convulsions due to type II compared with type I compounds.2 There are reports of vitamin E is effective in the treatment of paraesthesia although the mechanism of benefit is not clear; in addition, since this symptom resolves in 12–24 hours, specific treatment is not generally required.3
Researchers have also looked at targeting pyrethroids’ effects on sodium and chloride channels. While there are data from animal studies on the benefits of lidocaine and tetracaine in antagonizing the effects on sodium channels, their use is limited by cardiac toxicity. There may be a role for phenytoin, phenobarbitone, and valproate which have also been found to act equally on the pyrethroid evoked and normal sodium currents in experimental animal model setting.25
Ivermectin, a voltage-gated chloride channel agonist, was found to control salivation and repetitive discharges in muscle in pyrethroid-poisoned rats.7 This however has limited central action given the multidrug receptor pump activity at the blood–brain barrier that largely excludes ivermectin from the brain. Although atropine may be considered to decrease salivation, it is likely to have detrimental effects because of the potential to lower the seizure threshold in patients with pyrethroid poisoning.26
Methocarbamol, a mephenesin derivative, was found to antagonize the motor signs of pyrethroid in animal studies; this however, has not been studied in humans.27 Because of its lipophilic nature, intravenous lipid emulsion has been studied in permethrin-poisoned cats and found that clinical manifestations improved earlier compared to control cats.28 This has not been studied in humans and is hence not recommended.
CONCLUSION
Pyrethroid poisoning is common in clinical practice. Given its low toxicity for humans, most patients do not manifest significant symptoms. However, in mega-dose intoxication or those with mixed poisoning, particularly in combination with organophosphorus compounds, patients may present with life-threatening manifestations that require intensive care management. Treatment is supportive and symptomatic. A favorable outcome can be expected.
Footnotes
Source of support: Nil
Conflict of interest: None
REFERENCES
- 1.Thatheyus A, Selvam G, Alexander D. Synthetic pyrethroids: toxicity and biodegradation. Appl Ecol Environ Sci. 2013;1(3):33–36. doi: 10.12691/aees-1-3-2. DOI: [DOI] [Google Scholar]
- 2.Ray DE, Forshaw PJ. Pyrethroid insecticides: poisoning syndromes, synergies, and therapy. J Toxicol Clin Toxicol. 2000;38(2):95–101. doi: 10.1081/clt-100100922. DOI: [DOI] [PubMed] [Google Scholar]
- 3.Bradberry SM, Cage SA, Proudfoot AT, Vale JA. Poisoning due to pyrethroids. Toxicol Rev. 2005;24(2):93–106. doi: 10.2165/00139709-200524020-00003. DOI: [DOI] [PubMed] [Google Scholar]
- 4.Leng G, Ranft U, Sugiri D, Hadnagy W, Berger-Preiss E, Idel H. Pyrethroids used indoors-biological monitoring of exposure to pyrethroids following an indoor pest control operation. Int J Hyg Environ Health. 2003;206(2):85–92. doi: 10.1078/1438-4639-00199. DOI: [DOI] [PubMed] [Google Scholar]
- 5.Glickman AH, Casida JE. Species and structural variations affecting pyrethroid neurotoxicity. Neurobehav Toxicol Teratol. 1982;4(6):793–799. [PubMed] [Google Scholar]
- 6.Soderlund DM. Molecular mechanisms of pyrethroid insecticide neurotoxicity: recent advances. Arch Toxicol. 2011;86(2):165–181. doi: 10.1007/s00204-011-0726-x. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Forshaw PJ, Lister T, Ray DE. The role of voltage-gated chloride channels in type II pyrethroid insecticide poisoning. Toxicol Appl Pharmacol. 2000;163(1):1–8. doi: 10.1006/taap.1999.8848. DOI: [DOI] [PubMed] [Google Scholar]
- 8.Bhaskar EM, Moorthy S, Ganeshwala G, Abraham G. Cardiac conduction disturbance due to prallethrin (pyrethroid) poisoning. J Med Toxicol. 2010;6(1):27–30. doi: 10.1007/s13181-010-0032-7. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Miyamoto J, Kaneko H, Tsuji R, Okuno Y. Pyrethroids, nerve poisons: how their risks to human health should be assessed. Toxicol Lett. 1995;82–83:933–940. doi: 10.1016/0378-4274(95)03604-0. DOI: [DOI] [PubMed] [Google Scholar]
- 10.Kumar S, Thomas A, Sahgal A, Verma A, Samuel T, Pillai MKK. Variations in the insecticide-resistance spectrum of Anopheles stephensi after selection with deltamethrin or a deltamethrin-piperonyl-butoxide combination. Ann Trop Med Parasitol. 2004;98(8):861–871. doi: 10.1179/000349804X3180. DOI: [DOI] [PubMed] [Google Scholar]
- 11.Martin T, Ochou OG, Vaissayre M, Fournier D. Organophosphorus insecticides synergize pyrethroids in the resistant strain of cotton bollworm, Helicoverpa armigera (Hübner) (Lepidoptera: Noctuidae) from West Africa. J Econ Entomol. 2003;96(2):468–474. doi: 10.1093/jee/96.2.468. DOI: [DOI] [PubMed] [Google Scholar]
- 12.Chrustek A, Hołyńska-Iwan I, Dziembowska I, Bogusiewicz J, Wróblewski M, Cwynar A, et al. Current research on the safety of pyrethroids used as insecticides. Medicina (Kaunas) 2018;54(4):E61. doi: 10.1016/j.jemermed.2017.12.056. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Crofton KM, Kehn LS, Gilbert ME. Vehicle and route dependent effects of a pyrethroid insecticide, deltamethrin, on motor function in the rat. Neurotoxicol Teratol. 1995;17(4):489–495. doi: 10.1016/0892-0362(95)00008-f. DOI: [DOI] [PubMed] [Google Scholar]
- 14.He F, Wang S, Liu L, Chen S, Zhang Z, Sun J. Clinical manifestations and diagnosis of acute pyrethroid poisoning. Arch Toxicol. 1989;63(1):54–58. doi: 10.1007/bf00334635. DOI: [DOI] [PubMed] [Google Scholar]
- 15.Dorman DC, Beasley VR. Neurotoxicology of pyrethrin and the pyrethroid insecticides. Vet Hum Toxicol. 1991;33(3):238–243. [PubMed] [Google Scholar]
- 16.Cha YS, Kim H, Cho NH, Jung WJ, Kim YW, Kim TH, et al. Pyrethroid poisoning: features and predictors of atypical presentations. Emerg Med J. 2014;31(11):899–903. doi: 10.1136/emermed-2013-202908. DOI: [DOI] [PubMed] [Google Scholar]
- 17.Panwar M, Usha G, Kumath M. Status epilepticus: an association with pyrethroid poisoning. Indian J Crit Care Med. 2013;17(2):119–120. doi: 10.4103/0972-5229.114825. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Singh H, Luni FK, Marwaha B, Ali SS, Alo M. Transient complete heart block secondary to bed bug insecticide: a case of pyrethroid cardiac toxicity. Cardiology. 2016;135(3):160–163. doi: 10.1159/000446574. DOI: [DOI] [PubMed] [Google Scholar]
- 19.Mugundhan K, Iyer RS. Myelopathy following cypermethrin poisoning. J Assoc Physicians India. 2016;64(9):85–86. [PubMed] [Google Scholar]
- 20.Kim D, Moon J, Chun B. The initial hyperglycemia in acute type II pyrethroid poisoning. J Korean Med Sci. 2015;30(4):365–370. doi: 10.3346/jkms.2015.30.4.365. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Iyyadurai R, Peter JV, Immanuel S, Begum A, Zachariah A, Jasmine S, et al. Organophosphate-pyrethroid combination pesticides may be associated with increased toxicity in human poisoning compared to either pesticide alone. Clin Toxicol (Phila) 2014;52(5):538–541. doi: 10.3109/15563650.2014.909933. DOI: [DOI] [PubMed] [Google Scholar]
- 22.Tripathi M, Pandey R, Ambesh SP, Pandey M. A mixture of organophosphate and pyrethroid intoxication requiring intensive care unit admission: a diagnostic dilemma and therapeutic approach. Anesth Analg. 2006;103(2):410–412. doi: 10.1213/01.ane.0000222470.89210.5a. DOI: [DOI] [PubMed] [Google Scholar]
- 23.Hansen MR, Jørs E, Lander F, Condarco G, Schlünssen V. Is cumulated pyrethroid exposure associated with prediabetes? A cross-sectional study. J Agromedicine. 2014;19(4):417–426. doi: 10.1080/1059924X.2014.945708. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ding G, Shi R, Gao Y, Zhang Y, Kamijima M, Sakai K, et al. Pyrethroid pesticide exposure and risk of childhood acute lymphocytic leukemia in Shanghai. Environ Sci Technol. 2012;46(24):13480–13487. doi: 10.1021/es303362a. DOI: [DOI] [PubMed] [Google Scholar]
- 25.Oortgiesen M, van Kleef RGDM, Vijverberg HPM. Block of deltamethrin-modified sodium current in cultured mouse neuroblastoma cells: local anesthetics as potential antidotes. Brain Res. 1990;518(1–2):11–18. doi: 10.1016/0006-8993(94)90814-1. DOI: [DOI] [PubMed] [Google Scholar]
- 26.Drago B, Shah NS, Shah SH. Acute permethrin neurotoxicity: variable presentations, high index of suspicion. Toxicol Rep. 2014;1:1026–1028. doi: 10.1016/j.toxrep.2014.09.007. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hiromori T, Nakanishi T, Kawaguchi S, Sako H, Suzuki T, Miyamoto J. Therapeutic effects of methocarbamol on acute intoxication by pyrethroids in rats. J Pestic Sci. 1986;11(1):9–14. doi: 10.1584/jpestics.11.9. DOI: [DOI] [Google Scholar]
- 28.Peacock RE, Hosgood G, Swindells KL, Smart L. A randomized, controlled clinical trial of intravenous lipid emulsion as an adjunctive treatment for permethrin toxicosis in cats. J Vet Emerg Crit Care (San Antonio) 2015;25(5):597–605. doi: 10.1111/vec.12322. DOI: [DOI] [PubMed] [Google Scholar]