Abstract
Background
Lethal and edema toxins are critical virulence factors of Bacillus anthracis. Few data are available on their presence in the early stage of intranasal infection.
Methods
To investigate the diffusion of edema factor (EF) and lethal factor (LF), we use sensitive quantitative methods to measure their enzymatic activities in mice intranasally challenged with a wild-type B anthracis strain or with an isogenic mutant deficient for the protective antigen.
Results
One hour after mouse challenge, although only 7% of mice presented bacteremia, LF and EF were detected in the blood of 100% and 42% of mice, respectively. Protective antigen facilitated the diffusion of LF and EF into the blood compartment. Toxins played a significant role in the systemic dissemination of B anthracis in the blood, spleen, and liver. A mouse model of intoxination further confirmed that LT and ET could diffuse rapidly in the circulation, independently of bacteria.
Conclusions
In this inhalational model, toxins have disseminated rapidly in the blood, playing a significant and novel role in the early systemic diffusion of bacteria, demonstrating that they may represent a very early target for the diagnosis and the treatment of anthrax.
Keywords: bacteria, blood, inhalational anthrax, mice, toxins
The enzymatically active components of B anthracis toxins and bacteria can diffuse very early in the blood during inhalational anthrax model, paving the way for an ultra-precocious diagnosis and the setup of an early and effective treatment.
Inhalational anthrax, due to the inhalation of Bacillus anthracis spores, a rare spontaneous disease in humans, is the most lethal and fulminant form of anthrax, with a mortality rate of 50%–90% [1].
How B anthracis spores cross the respiratory epithelial barrier is still subject to debate [2, 3]. Two main sites of entry, after deposition in the respiratory tract, have been described thus far: (1) the upper respiratory tract through nasal-associated lymphoid tissues (NALTs) [4] and (2) the lower respiratory tract within the alveoli, where alveolar macrophages (AMs) and dendritic cells (DCs) act as a “Trojan horse,” transporting inhaled spores across the lung epithelium into the draining lymph nodes (LNs) [5]. Spore capture by phagocytes is a rapid process: 10 to 35 minutes for AM [6, 7] and less than 3 minutes for DCs [8].
Germination in the lung aerial space occurs at a low level and can be detected when adequate sampling procedures are used [9, 10]. Bacterial multiplication occurs at the initial site of entry, ie, the NALT or alveolar lumen [4, 11]. After dissemination to the draining LN, the bacteria eventually enter the bloodstream via the lymphatic system. Once the bacteria reach the bloodstream, the evolution to septicemia and death is extremely rapid, as shown in mice (5 to 8 hours [12]).
Virulence is due to a poly-gamma-d-glutamic acid capsule with anti-phagocytic properties, contributing to bacterial dissemination, and 2 toxins, the lethal toxin (LT), an association of lethal factor (LF) and protective antigen (PA), and edema toxin (ET), an association of edema factor (EF) and PA. Lethal factor is a zinc-dependent metalloprotease that cleaves and inactivates most mitogen-activated protein kinase kinases [13, 14], disrupting major eukaryotic cell functions [15]. Edema factor is a calmodulin- calcium-dependent adenylylcyclase, which catalyzes the conversion of adenosine 5′-triphosphate (ATP) to cyclic adenine monophosphate (cAMP) [16, 17], inducing multiple alterations in gene expression through PKA and CREB [18–21]. Anthrax toxins play a central role in the disease pathogenesis at 2 critical stages of the infection. During the early period of infection, they specifically target innate and adaptive immune cells, paralyzing the immune response and overriding the host response. During the late stage of infection, when high levels of toxins circulate in the blood, they are responsible for high lethality by targeting specific organs [22, 23].
The fulminant character of inhalational anthrax suggests that the bacteria may act rapidly and use host mechanisms to enter the body. Indeed, we showed that LF and EF can be detected locally and in the bloodstream very early during infection with a fully virulent strain in a model of cutaneous infection [24]. Thus, we reasoned that LF and EF could also be detected early in an inhalation model of infection, because the lung is one of the most highly vascularized organs and toxins play a role in the pathophysiology of anthrax. In this study, we show the early presence of LF, EF, and bacteria in the bloodstream. We also determined the impact of the virulence factors of B anthracis in the diffusion of LF and EF and systemic dissemination of the bacteria.
METHODS
Chemicals and Reagents
Recombinant EF was obtained from Quadratech Diagnostics (Epsom Surrey, United Kingdom). Adenosine 5′-triphosphate disodium salt hydrate, adenosine 3′,5′-cyclic monophosphate, sodium periodate, and rhamnose were obtained from Sigma-Aldrich (St. Louis, MO). Human recombinant calmodulin was from Enzo Life Sciences (Villeurbanne, France). The cAMP antiserum, cAMP acetylcholinesterase enzymatic tracer, Ellman’s reagent, cAMP standard, and acetic anhydride used in the enzyme immunoassay (EIA) were from Spi-Bio (Montigny-Le-Bretonneux, France). Recombinant LF was from List Biological Laboratories (Campbell, CA). The peptide substrate cleaved by LF (H-Ser-Lys-Ala-Arg-Arg-Lys-Lys-Val-Tyr-Pro-Tyr-Pro-Met-Glu-Asn-Phe-Pro-Pro-Ser-Thr-Ala-Arg-Pro-Thr-OH), the N-terminal/C-terminal products (H-Ser-Lys-Ala-Arg-Arg-Lys-Lys-Val-Tyr-Pro and Tyr-Pro-Met-Glu-Asn-Phe-Pro-Pro-Ser-Thr-Ala-Arg-Pro-Thr-OH), and internal standards [25] were from Bachem (Basel, Switzerland).
Ethics Statement
All animal experiments were conducted at the Institut Pasteur according to European Directive 2010/63/UE and were approved by the Institut Pasteur animal care and use committee. All efforts were made to minimize suffering. The animals were housed in animal facilities of the Institut Pasteur licensed by the French Ministry of Agriculture in compliance with European regulations. The protocols were approved by the Institut Pasteur Safety Committee and Animal Experimentation Ethics Committee (CETEA 2013-0088/MESR 01168.01).
Animal and Bacterial Strains
Female outbred OF1 mice (22 to 24 grams) were from Charles River (L’Arbresle, France). The luminescent B anthracis strains used in this study were the wild-type 9602WT-lux(EF+LF+PA+), the isogenic derivative mutants inactivated in the pagA gene, 9602P-lux(EF+LF+PA−), or lef and/or cya genes, 9602L(EF+LF-PA+), 9602C(EF-LF+PA+), and 9602LC(EF-LF-PA+), constructed as previously described [12, 26]. Isogenic derivative mutants inactivated in the cya and/or lef genes were used as negative controls for the production of EF and LF.
Mouse Infection and Intoxination
Anesthetized mice were challenged intranasally by depositing 20 µL of a spore suspension of each bacterial strain onto a nostril as previously described [4]. The inoculum size was verified retrospectively by plating 10-fold serial dilutions on brain-heart infusion (BHI) (Difco, Detroit, MI) agar plates (Table 1). For intoxination, anesthetized mice were inoculated intranasally either with 400 ng (to be close to the local concentration determined in vivo during cutaneous infection [24]) or 10 µg LF/EF and or PA in 20 µL phosphate-buffered saline.
Table 1.
Inoculated Doses of Bacteriaa
| Strain | 9602WT-lux | 9602P-lux ± PA | 9602C-lux ± EF | 9602L-lux ± LF | 9602LC ± LF, EF |
|---|---|---|---|---|---|
| CFU (log10/mL) | 5.04 ± 0.14 (5) | 5.06 ± 0.31 (12) | 5.13 ± 0.34 (7) | 5.4 ± 0.29 (6) | 4.3 ± 0.26 (5) |
Abbreviations: CFU, colony-forming units; EF, edema factor ; LF, lethal factor; PA, protective antigen; SEM, standard error of the mean.
aMice were intranasally challenged with spores of the 9602WT-lux (EF+LF+PA+), 9602P-lux (EF+LF+PA-), 9602C-lux (EF-LF+PA+), 9602L-lux (EF+LF-PA+), or 9602LC (EF-LF-PA+) strain. The inoculum size was retrospectively verified by plating 10-fold serial dilutions on brain-heart infusion agar plates. Data are expressed as the mean ± SEM, with the number of experiments (n) shown in parentheses.
One hour after challenge, blood was collected in calciparine (50 UI per mL) and 10% protease inhibitor mix (Roche). After centrifugation (7000 rpm, 4 minutes), plasma was filtered through 0.22-µm pore filters (Ultrafree-MC centrifugal units; Dominique Dutscher) and stored at −20°C. In some experiments, spleen and liver were harvested, homogenized in distilled water, and bacterial enumeration performed on BHI agar plates. Blood colony-forming units were determined before centrifugation of the sample.
Determination of Lethal Factor Enzymatic Activity by LC-MS/MS Quantification
The LF enzymatic activity was assayed as previously described [24]. In brief, standards and samples were incubated with the substrate peptide. After elimination of the proteins and solvents, the N-Ter and C-Ter peptides produced by cleavage of the substrate peptide by LF were detected and quantified using a liquid chromatography system coupled to a triple quadrupole mass spectrometer (LC-MS/MS). The results were analyzed using Thermo Scientific Xcalibur software.
Edema Factor Enzymatic Activity Assay
The adenylyl cyclase EF activity was measured by assessing production of cAMP using a competitive EIA, as previously described [24, 27]. The EF adenylyl cyclase activity was first assayed directly in the sample (plasma) by the enzymatic reaction assay. The ATP interference was then eliminated, and the sensitivity of cAMP detection increased by chemical transformation (production of acetylated cAMP), followed by the EIA assay. The absorbance was recorded at 405 nm using a spectrophotometer microplate reader Multiskan Ascent (Labsystem). No intrinsic adenylyl cyclase activity was detected in the infected samples in the absence of calmodulin, and the endogenous ATP and cAMP concentrations in the infected samples did not interfere with the EF assay.
Characterization of the Thresholds for Lethal Factor and Edema Factor Detection
The background signal and threshold for LF and EF detection were determined from plasma samples of animals 1 hour after infection with B anthracis strains devoid of LF and/or EF, as previously described [24], to follow the pathophysiological events that occur during an infection as closely as possible. The B anthracis strains used produced either no LF and EF (9602LC(EF-LF-PA+) strain), no LF (9602L-lux(EF+LF-PA+) strain), or no EF (9602C-lux(EF-LF+PA+) strain). The highest values obtained for these negative control samples were considered to be the threshold of detection for LF and EF. The detection thresholds were thus determined to be 3.1 pg/mL (n = 33) for EF and 640 pg/mL (n = 15) for LF.
For the intoxination model, the threshold was determined with EF and PA for LF quantification and LF and PA for EF quantification. The highest values obtained for these negative control samples were considered to be the threshold of detection for LF and EF. The detection thresholds were thus determined to be 9.3 pg/mL (n = 29) for EF and 200 pg/mL (n = 8) for LF.
Statistical Analysis
Statistical analysis was performed using GraphPad Prism software (version 4.0; GraphPad Software, San Diego, CA). Statistical significance was determined by the Mann-Whitney test. P < .05 was set as the statistically significant threshold.
RESULTS
Lethal Factor and Edema Factor as Early Biomarkers of Inhalational Anthrax
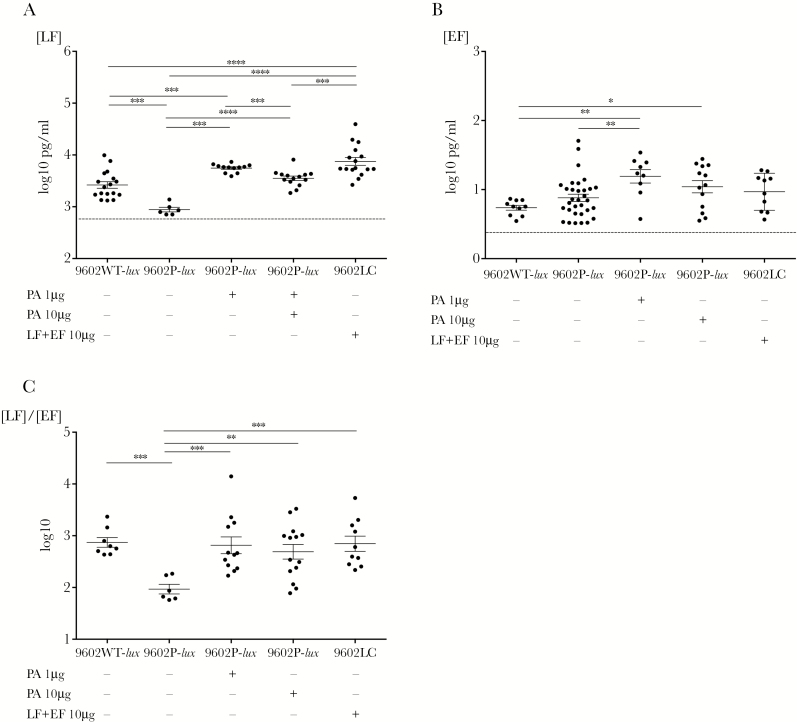
One hour after intranasal challenge with the B anthracis strain 9602WT-lux, LF was detected in the blood of all mice (n = 17 of 17) and EF in that of 41.7% (n = 10 of 24) (Table 2), showing rapid production and systemic diffusion of LF and EF. The mean plasma LF and EF levels were 2630 and 5.5 pg/mL, respectively (Table 3), corresponding to a mean LF/EF ratio of 436 (Figure 1C, Table 3).
Table 2.
Percentage of Mice Positive for LF and EF in Plasma After Intranasal Inoculation With the 9602WT-lux (EF+LF+PA+) Strain and Its Mutants 9602P-lux (EF+LF+PA-) ± PA, and 9602LC (EF-LF-PA+) ± (EF + LF), 1 Hour After Infectiona
| Strains Used for the Infection | LF | EF |
|---|---|---|
| 9602WT-lux | 100 (17/17) | 41.7 (10/24) |
| 9602P-lux | 30.4 (7/23) | 70 (28/40) |
| 9602P-lux + 1 μg PA | 100 (12/12) | 75 (9/12) |
| 9602P-lux + 10 μg PA | 100 (14/14) | 81.3 (13/16) |
| 9602LC | NC | NC |
| 9602LC + 10 μg (EF + LF) | 100 (16/16) | 62.5 (10/16) |
Abbreviations: CFU, colony-forming units; EF, edema factor; LF, lethal factor; NC, not concerned; PA, protective antigen; SEM, standard error of the mean.
aMice were intranasally challenged with spores of the 9602WT-lux (EF+LF+PA+) strain (5.04 log10 CFU ± 0.14 (n = 5), mean ± SEM, number of experiments (n) (in brackets), spores of the 9602P-lux (EF+LF+PA-) strain (5.06 ± 0.31 [n = 12]), with or without 2 different concentrations of PA (1 or 10 µg), or spores of the 9602LC (EF-LF-PA+) strain (4.3 ± 0.26 [n = 5]), with or without 10 µg of LF and EF. The percentage of mice positive for EF and LF was calculated as the number of mice showing detectable circulating levels of EF or LF relative to the total number of mice. (n), number of samples.
Table 3.
LF and EF Levels in Plasma and the Associated LF/EF Ratio During Inhalational Infection With the 9602WT-lux (EF+LF+PA+) Strain and Its Mutants 9602P-lux (EF+LF+PA-) ± PA and 9602LC (EF-LF-PA+) ± (EF + LF), 1 Hour After Infectiona
| Plasma | |||
|---|---|---|---|
| Strains Used for the Infection | LF (log10 pg/mL) | EF (log10 pg/mL) | LF/EF (log10) |
| 9602WT-lux | 3.42 ± 0.06 (17) | 0.74 ± 0.03 (10) | 2.64 ± 0.12 (8) |
| 9602P-lux | 3.01 ± 0.08 (7) | 0.86 ± 0.05 (28) | 1.97 ± 0.09 (6) |
| 9602P-lux + 1 µg PA | 3.75 ± 0.02 (12) | 1.19 ± 0.1 (9) | 2.56 ± 0.09 (9) |
| 9602P-lux + 10 µg PA | 3.55 ± 0.04 (14) | 1.04 ± 0.09 (13) | 2.52 ± 0.13 (11) |
| 9602LC +10 μg (EF + LF) | 3.88 ± 0.08 (16) | 0.97 ± 0.08 (10) | 2.85 ± 0.15 (10) |
Abbreviations: EF, edema factor; LF, lethal factor; PA, protective antigen; SEM, standard error of the mean.
aMice were intranasally challenged as described in Table 1. The EF and LF concentrations were assessed by competitive immunoassay and mass spectrometry, respectively, in the plasma 1 hour after challenge and compared with the threshold obtained with the plasma of noninfected mice. The EF and LF concentrations are expressed as the mean log10 ± SEM pg per mL in the plasma. The LF/EF ratio was calculated for each individual mouse displaying values over the thresholds for both LF and EF in the plasma. Data are expressed as the mean log10 ± SEM. (n), number of samples.
Figure 1.
Detection of circulating plasma lethal factor (LF) and edema factor (EF) during inhalational infection with the wild-type 9602WT-lux strain and its mutants 9602P-lux (EF+LF+PA-) ± protective antigen (PA), and 9602LC (EF-LF-PA+) ± (EF + LF), 1 hour after infection. Active lethal factor ([LF] A) and edema factor ([EF] B) were quantified in the plasma, as described under Materials and Methods, 1 hour after infection with spores of the 9602WT-lux (EF+LF+PA+) strain (5.04 log10 colony-forming units ± 0.14 [n = 5], mean ± standard error of the mean, number of experiments [n] in brackets), spores of the 9602P-lux (EF+LF+PA-) strain (5.06 ± 0.31 [n = 12]), with or without 2 different concentrations of PA (1 or 10 µg), or spores of the 9602LC (EF-LF-PA+) strain (4.3 ± 0.26 [n = 5]), with or without 10 µg of LF and EF. The LF/EF ratio (C) was calculated from the LF and EF values obtained for each individual mouse. Results are expressed as picograms per milliliter; each dot represents an individual mouse, and the bar represents the mean for each mouse population for each bacterial strain. The asterisks denote statistically significant differences (Mann-Whitney test); *, P < .05, **, P < .01, ***, P < .001, and ****, P < .001.
Protective Antigen Favors Early Lethal Factor/Edema Factor Diffusion in Inhalational Anthrax
We assessed the impact of PA in early diffusion of LF and EF in the bloodstream (1 hour after challenge) by challenging mice with the PA-deficient strain, 9602P-lux, which produces only LF and EF. In the absence of PA, the percentage of mice positive for LF in the blood decreased from 100% for the 9602WT-lux strain to 30.4% (n = 7 of 23), whereas the percentage of mice positive for EF increased from 41.7% to 70% (n = 28 of 40). The mean level of LF in the positive mice was significantly lower (2.6-fold at 1023 pg/mL) (Figure 1A, Table 3), whereas the mean concentration of EF was similar, at 7.2 pg/mL (Figure 1B, Table 3). The LF/EF ratio of 93 was thus significantly lower in the absence of PA, showing a 4.7-fold decrease (Figure 1C, Table 3).
We completed the study of the role of PA during infection with the 9602WT-lux strain by instilling mice with various doses of exogenous PA and spores of the 9602P-lux strain. Concomitant instillation of PA led to restoration of only 1 parameter relative to infection with the 9602WT-lux strain: LF was detected in the blood of all infected mice. The frequency of mice positive for EF was high, reaching 75% for 1 μg of PA (Table 2). Thus, instillation of PA restored the frequency of detectable LF and increased the frequency of detectable EF to above the wild-type (WT) values. Instillation with 1 μg of PA significantly increased the mean concentrations of LF to 5623 pg/mL (2-fold increase) and EF to 15.5 pg/mL (5-fold increase) (Figure 1A and B, Table 3). However, the mean level of LF (3548 pg/mL) after instillation with 10 μg of PA was not significantly different from that observed for the WT strain, whereas the mean level of EF was still higher at 11 pg/mL (Figure 1A and B, Table 3).
When mice were cochallenged with 10 μg LF + EF and the isogenic strain 9602LC expressing PA, but not EF or LF, the mean percentage of mice positive for blood LF and EF were 100% and 62%, respectively (Table 2). The mean level of LF was significantly higher (7585 pg/mL) than that for the 9602WT-lux strain, whereas the EF level was not significantly different (Figure 1A and B, Table 3). These results confirm the important role of PA in the diffusion of LF and EF in the blood.
Diffusion of Edema Factor and Lethal Factor After Pulmonary Intoxination
Our data with the mutants of the 9602WT-lux strain showed that LF and EF were able to cross the respiratory epithelial barrier and reach the blood compartment as soon as 1 hour after infection. We further explored this intriguing phenomenon by instilling mice with the purified B anthracis toxin components LF, EF, and PA (400 ng each) and studying their diffusion at 1 hour in the bloodstream.
After instillation of LT (LF + PA) and/or ET (EF + PA), all mice were positive for blood LF and more than half for blood EF, with mean levels of 501 to 589 pg/mL for LF and 14 to 20 pg/mL for EF (Table 5). These percentages were similar to those observed during infection. The EF level was also similar to that observed during infection, whereas the LF level was lower. This result corroborates our hypothesis of the capacity of B anthracis toxins to rapidly diffuse into the bloodstream, independently of the bacteria.
Table 5.
Percentage of Mice Positive for EF or LF in Plasma 1 Hour After Intoxination of Mice With LF/EF and PA and LF and EF Quantificationa
| Percentage of Mice Positive for | Plasma | |||
|---|---|---|---|---|
| Components Used for the Intoxination | EF | LF | EF (log10 pg/mL) | LF (log10 pg/mL) |
| LF + PA | NA | 100 (4/4) | NA | 2.77 ± 0.04 (4) |
| EF + PA | 53 (9/17) | NA | 1.31 ± 0.07 (8) | NA |
| LF + EF + PA | 67 (10/15) | 100 (4/4) | 1.15 ± 0.05 (9) | 2.7 ± 0.08 (4) |
Abbreviations: EF, edema factor; LF, lethal factor; NA, not applicable; PA, protective antigen; SEM, standard error of the mean.
aMice were intranasally intoxinated with 400 ng of the factors constituting the toxins of Bacillus anthracis: LF + PA, EF + PA, LF + EF + PA. The percentage of mice positive for LF and/or EF was calculated as the number of mice showing detectable LF and/or EF in their blood 1 hour after challenge. The EF and LF concentrations were assessed through a competitive immunoassay and mass spectrometry, respectively, in the plasma 1 hour after challenge. The EF and LF concentrations were expressed as mean log10 ± SEM pg per mL in the plasma, number of samples (n) in parentheses.
Protective Antigen Influences the Systemic Dissemination of Bacteria
We determined whether diffusion of the B anthracis toxin components was associated with systemic dissemination of bacteria by evaluating the blood bacterial load for the 9602WT-lux strain and the bacterial load in blood, liver, and spleen for its mutants 1 hour after intranasal challenge.
Only 6.9% of mice showed bacteria in their circulation after intranasal challenge with the B anthracis strain 9602WT-lux (Table 4). Thus, bacterial dissemination cannot explain the presence of LF in the plasma of all mice.
Table 4.
Percentage of Mice Positive For Bacteria in the Blood, Liver, and Spleen and Total Systemic Dissemination After Intranasal Inoculation With the 9602WT-lux Strain and Its Mutants, 9602P-lux (EF+LF+PA-) ± PA and 9602LC (EF-LF-PA+) ± (EF + LF), 1 Hour After Infectiona
| Infection With | Blood | Liver | Spleen | Total Systemic Dissemination |
|---|---|---|---|---|
| 9602WT-lux | 6.9 (2/29) | ND | ND | |
| 9602P-lux | 37.3 (22/59) | 25 (11/44) | 2 (1/44) | 61 (36/59) |
| 9602P-lux + 1 μg PA | 41.7 (5/12) | 25 (3/12) | 17 (2/12) | 66.7 (8/12) |
| 9602P-lux + 10 μg PA | 81.3 (13/16) | 6 (1/16) | 0 (0/16) | 81.3 (13/16) |
| 9602LC | 25.9 (7/27) | 7 (2/28) | 7 (2/28) | 37.9 (11/29) |
| 9602LC+ 10 μg (LF + EF) | 18.8 (3/16) | 0 (0/16) | 0 (0/16) | 18.8 (3/16) |
Abbreviations: EF, edema factor; LF, lethal factor; ND, not determined; PA, protective antigen.
aMice were intranasally challenged as described in Table 1. The percentage of mice positive for bacteria was calculated as the number of mice showing bacteria in their blood, liver, or spleen relative to the total number of mice. (n), number of samples.
The percentage was higher for the PA-deleted strain 9602P-lux, with 37.3% (n = 22 of 59) of the mice showing bacteria in the blood (Table 4). The total percentage of mice exhibiting systemic bacterial dissemination was 61% (n = 36 of 59), because bacteria were also detected in liver and spleen.
Cochallenge with the 9602P-lux strain and 1 μg of PA did not markedly change this percentage. However, there was greater total systemic dissemination when mice were cochallenged with 10 μg of PA. A 2-fold higher percentage of mice showed bacteria in the blood, ie, 81.3% (n = 13 of 16) (Table 4). Only 1 mouse showed bacteria in the liver.
The percentage of mice showing systemic bacterial dissemination was 37.9% (n = 11 of 29) after infection with the isogenic 9602LC strain (Table 4), the blood still being the major compartment showing the presence of the bacteria. No bacteria were present in the liver or spleen after coinstillation of 10 μg LF and EF with this strain, and only blood showed the presence of bacteria, with 18.8% of the mice being positive (n = 3 of 16).
DISCUSSION
In this study, we show rapid production and very early diffusion of enzymatically active components of the toxins of B anthracis in an animal model of inhalational anthrax. We detected LF and EF in the plasma 1 hour after instillation of spores of a WT strain using sensitive and specific techniques; all mice were positive for LF and 42% were positive for EF.
Diffusion of LF and EF was partially independent of PA and thus also of the toxic enzymatic activities mediated through intracytosolic translocation of LF and EF via PA binding, because infection with a PA-deficient strain (9602P-lux) still led to the detection of LF and EF in the plasma of 30% and 70% of mice, respectively, 1 hour after inoculation. Coinstillation of 1 or 10 µg of PA with the PA-deficient strain increased the percentage of mice positive for LF and EF to 100% and 75% to 81%, respectively. Furthermore, diffusion of LF and EF was still observed in the absence of an infectious process, because intranasal instillation of LT and/or ET led to detection of LF and EF in the plasma of 100% and more than 50% of the mice, respectively, 1 hour after instillation.
Thus, these data raise questions concerning the mechanisms of transport of LF and EF across the lung epithelial barrier. Multiple transport pathways have been described for physiological protein translocation through the pulmonary epithelium: either paracellular or transcellular via caveolae [28, 29].
Previous studies have highlighted the disruption of the alveolar epithelial barrier and the adjacent endothelium, which could facilitate toxin diffusion. Thus, ET could lead to the formation of transcellular macroaperture tunnels via cAMP signaling pathways, as shown in endothelial cells [30]. The LT provokes barrier dysfunction both in primary human alveolar epithelial cells [31, 32] and primary human lung microvascular endothelial cells [33, 34]; such disruption of the epithelial and endothelial barriers would thus facilitate LF and EF diffusion. Also of note, no decrease of cell viability was detected in primary human alveolar epithelial cells [31], confirming previous observations that no macroscopic cytotoxic effects occurred in the epithelium lining the alveoli, although microcolonies of LT- and ET-secreting bacteria filled the alveolar spaces [4]. Protective antigen alone had similar effects on barrier dysfunction, suggesting that pore formation could also by itself be the triggering factor [31].
Our data show that there are differences in the diffusion mechanisms between LF and EF, because the absence of PA did not modify EF plasma levels, while significantly decreasing LF levels. The involvement of PA in one of the diffusion mechanisms was further confirmed through the ability of local PA addition to markedly increase both LF and EF plasma levels to even higher values than those observed during infection with the WT strain. This increase could raise the formation of TEM tunnels and the disorganization of the lung barrier, permitting the passage of more toxins and bacteria.
Our data on LF and EF presence in plasma 1 hour after spore inoculation support the hypothesis of in situ germination in the lung aerial space, with very rapid kinetics of spore germination and toxin production and diffusion. This is a crucial element in the initiation of pulmonary anthrax, because germination in lung tissue occurs at a low level [9, 10].
Our results also raised the possibility of early bacterial dissemination from the lung aerial space into the infected host; LF/EF detection in the plasma could thus originate from their production by these bacteria. Indeed, we observed systemic dissemination in at least 1 of the 3 main target compartments tested (blood, spleen, and liver) in 61% of the mice 1 hour after spore inoculation, with 37% positive in the blood, even in the absence of PA (infection with the PA-deficient strain). This observation is consistent with those of a previous report showing that primary human small airway epithelial cells bind, internalize, and translocate B anthracis spores without disrupting barrier integrity in vitro [35]. Ross [7] reported that spores can often be seen lying in close apposition to the lining of the alveolar ducts and alveoli, and they are thus prone to interaction with epithelial cells. Bacillus anthracis also produces proteases that are involved in host tissue degradation [36], which could contribute to bacterial dissemination.
Coinstillation of 10 µg of PA showed an increase in bacterial detection, mainly in blood, with 81% of mice positive. This is associated with an increase in diffusion and level of EF in blood. These results suggest that PA, although not the main actor in early systemic bacterial dissemination, still plays a facilitating role, most likely through provoking barrier dysfunction in both alveolar epithelial and endothelial cells [30–34], as mentioned above. A higher level of ET could play a predominant role by preventing bacterial growth in the nasopharynx and the draining LNs as previously described [26] and extend bacteria circulation in blood by inducing bradycardia and hypotension [37], thus explaining the presence of bacteria primarily in the blood.
In addition to disruption of the epithelial and endothelial barriers, another process could play a role in early dissemination of bacteria. An in vivo and in vitro study highlighted the capture of spores by lung DCs after 30 minutes in a mouse model of inhalational infection [6, 8]. Interstitial lung DCs have been shown to transport spores into the thoracic LNs from 30 minutes to 1.5-hour postintranasal infection [6, 38], in accordance with another study showing that DCs can reach regional LNs from the alveolar space within 30 minutes after bacterial challenge [39].
It is interesting to note that the level of bacterial dissemination in the 3 compartments tested was lower (38% of mice) after infection with the LF/EF-deficient 9602LC strain. Coinstillation of LF + EF at the time of challenge with the 9602LC strain further reduced the percentage of mice positive for bacteria to 19%, all in the blood.
In this study, we provide evidence for the early diffusion of active LF and EF, the enzymatic toxic moieties of B anthracis toxins, in as little as 1 hour after exposure to spores by inhalation in a mouse model. Diagnosing inhalational anthrax at this early time point, if reported on a human time scale, can surely make a decisive difference for the setup of an early and effective treatment. Thus, detection of the toxin enzymatic activities is a very interesting alternative for an ultra-precocious diagnosis. Our data show that 2 types of mechanisms are involved: one involving protein crossing the epithelial barrier through PA-independent and -dependent pathways, and the other associated with early bacterial dissemination. We were able to reveal this early phenomenon through the use of highly sensitive techniques for LF and EF detection, based on amplification of the signal due to their enzymatic activities [24, 27]. Such an ultrasensitive assay is not yet available for the detection of PA at such an early time point. It is indeed possible that the 3 components of the toxins can cross the lung epithelium, and thus fully active toxins could be generated early during the infection; this could play a significant role in the pathophysiology of the initial steps of anthrax.
Our study exemplifies the importance of early detection of LF and EF; LF was a highly sensitive biomarker for initial intranasal infection and substantiated by EF detection in 42% of the animals, thus increasing the robustness of detection and diagnosis. This is supported by studies on rhesus macaques with inhalation anthrax showing that LF and EF measurements may indicate the stage of infection and, consequently, the need of treatment [40–43]. Early detection of LF and EF could help in choosing the therapeutic arsenal at a time when the toxic effects of the toxins are low and could still be curtailed by appropriate treatment, such as the administration of anti-PA monoclonal antibodies (mAbs), before the irreversible disruption of cellular metabolism. Such an approach could help to more precisely define the time window of efficient mAb administration and increase its efficacy [44–46].
Notes
Disclaimer. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Financial support. This work was funded by the Joint Ministerial Program of R&D against CBRNE risks (NRBC H1.11).
Potential conflicts of interest. All authors: no reported conflicts. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest.
Disclosure of Potential Conflicts of Interest.
Presented in part: International Conference on Bacillus anthracis, B. cereus, and B. thuringiensis, 2017, Victoria, Canada, 1–5 October.
References
- 1. Dixon TC, Meselson M, Guillemin J, Hanna PC. Anthrax. N Engl J Med 1999; 341:815–26. [DOI] [PubMed] [Google Scholar]
- 2. Weiner ZP, Glomski IJ. Updating perspectives on the initiation of Bacillus anthracis growth and dissemination through its host. Infect Immun 2012; 80:1626–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Goossens PL, Tournier JN. Crossing of the epithelial barriers by Bacillus anthracis: the known and the unknown. Front Microbiol 2015; 6:1122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Glomski IJ, Dumetz F, Jouvion G, Huerre MR, Mock M, Goossens PL. Inhaled non-capsulated Bacillus anthracis in A/J mice: nasopharynx and alveolar space as dual portals of entry, delayed dissemination, and specific organ targeting. Microbes Infect 2008; 10:1398–404. [DOI] [PubMed] [Google Scholar]
- 5. Guidi-Rontani C. The alveolar macrophage: the Trojan Horse of Bacillus anthracis. Trends Microbiol 2002; 10:405–9. [DOI] [PubMed] [Google Scholar]
- 6. Cleret A, Quesnel-Hellmann A, Vallon-Eberhard A, et al. Lung dendritic cells rapidly mediate anthrax spore entry through the pulmonary route. J Immunol 2007; 178:7994–8001. [DOI] [PubMed] [Google Scholar]
- 7. Ross JM. The pathogenesis of anthrax following the administration of spores by the respiratory route. J Pathol Bacteriol 1957; 73:485–94. [Google Scholar]
- 8. Fiole D, Douady J, Vial JC, Quesnel-Hellmann A, Tournier JN. Dynamics of rapid spore capture by dendritic cells in the lung alveolus. Am J Respir Crit Care Med 2012; 186:e2–3. [DOI] [PubMed] [Google Scholar]
- 9. Guidi-Rontani C, Weber-Levy M, Labruyère E, Mock M. Germination of Bacillus anthracis spores within alveolar macrophages. Mol Microbiol 1999; 31:9–17. [DOI] [PubMed] [Google Scholar]
- 10. Cote CK, Van Rooijen N, Welkos SL. Roles of macrophages and neutrophils in the early host response to Bacillus anthracis spores in a mouse model of infection. Infect Immun 2006; 74:469–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Sanz P, Teel LD, Alem F, Carvalho HM, Darnell SC, O’Brien AD. Detection of Bacillus anthracis spore germination in vivo by bioluminescence imaging. Infect Immun 2008; 76:1036–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Glomski IJ, Piris-Gimenez A, Huerre M, Mock M, Goossens PL. Primary involvement of pharynx and peyer’s patch in inhalational and intestinal anthrax. PLoS Pathog 2007; 3:e76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Vitale G, Pellizzari R, Recchi C, Napolitani G, Mock M, Montecucco C. Anthrax lethal factor cleaves the N-terminus of MAPKKs and induces tyrosine/threonine phosphorylation of MAPKs in cultured macrophages. Biochem Biophys Res Commun 1998; 248:706–11. [DOI] [PubMed] [Google Scholar]
- 14. Duesbery NS, Webb CP, Leppla SH, et al. Proteolytic inactivation of MAP-kinase-kinase by anthrax lethal factor. Science 1998; 280:734–7. [DOI] [PubMed] [Google Scholar]
- 15. Tonello F, Montecucco C. The anthrax lethal factor and its MAPK kinase-specific metalloprotease activity. Mol Aspects Med 2009; 30:431–8. [DOI] [PubMed] [Google Scholar]
- 16. Leppla SH. Anthrax toxin edema factor: a bacterial adenylate cyclase that increases cyclic AMP concentrations of eukaryotic cells. Proc Natl Acad Sci U S A 1982; 79:3162–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Drum CL, Yan SZ, Bard J, et al. Structural basis for the activation of anthrax adenylyl cyclase exotoxin by calmodulin. Nature 2002; 415:396–402. [DOI] [PubMed] [Google Scholar]
- 18. Puhar A, Dal Molin F, Horvath S, Ladant D, Ladants D, Montecucco C. Anthrax edema toxin modulates PKA- and CREB-dependent signaling in two phases. PLoS One 2008; 3:e3564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kim C, Wilcox-Adelman S, Sano Y, Tang WJ, Collier RJ, Park JM. Antiinflammatory cAMP signaling and cell migration genes co-opted by the anthrax bacillus. Proc Natl Acad Sci U S A 2008; 105:6150–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Park JM, Greten FR, Wong A, et al. Signaling pathways and genes that inhibit pathogen-induced macrophage apoptosis–CREB and NF-kappaB as key regulators. Immunity 2005; 23:319–29. [DOI] [PubMed] [Google Scholar]
- 21. Raymond B, Leduc D, Ravaux L, et al. Edema toxin impairs anthracidal phospholipase A2 expression by alveolar macrophages. PLoS Pathog 2007; 3:e187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Tournier JN, Rossi Paccani S, Quesnel-Hellmann A, Baldari CT. Anthrax toxins: a weapon to systematically dismantle the host immune defenses. Mol Aspects Med 2009; 30:456–66. [DOI] [PubMed] [Google Scholar]
- 23. Liu S, Moayeri M, Leppla SH. Anthrax lethal and edema toxins in anthrax pathogenesis. Trends Microbiol 2014; 22:317–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Rougeaux C, Becher F, Ezan E, Tournier JN, Goossens PL. In vivo dynamics of active edema and lethal factors during anthrax. Sci Rep 2016; 6:23346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Boyer AE, Quinn CP, Woolfitt AR, et al. Detection and quantification of anthrax lethal factor in serum by mass spectrometry. Anal Chem 2007; 79:8463–70. [DOI] [PubMed] [Google Scholar]
- 26. Dumetz F, Jouvion G, Khun H, et al. Noninvasive imaging technologies reveal edema toxin as a key virulence factor in anthrax. Am J Pathol 2011; 178:2523–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Duriez E, Goossens PL, Becher F, Ezan E. Femtomolar detection of the anthrax edema factor in human and animal plasma. Anal Chem 2009; 81:5935–41. [DOI] [PubMed] [Google Scholar]
- 28. Gumbleton M. Caveolae as potential macromolecule trafficking compartments within alveolar epithelium. Adv Drug Deliv Rev 2001; 49:281–300. [DOI] [PubMed] [Google Scholar]
- 29. Hastings RH, Folkesson HG, Matthay MA. Mechanisms of alveolar protein clearance in the intact lung. Am J Physiol Lung Cell Mol Physiol 2004; 286:L679–89. [DOI] [PubMed] [Google Scholar]
- 30. Maddugoda MP, Stefani C, Gonzalez-Rodriguez D, et al. cAMP signaling by anthrax edema toxin induces transendothelial cell tunnels, which are resealed by MIM via Arp2/3-driven actin polymerization. Cell Host Microbe 2011; 10:464–74. [DOI] [PubMed] [Google Scholar]
- 31. Langer M, Duggan ES, Booth JL, et al. Bacillus anthracis lethal toxin reduces human alveolar epithelial barrier function. Infect Immun 2012; 80:4374–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Lehmann M, Noack D, Wood M, Perego M, Knaus UG. Lung epithelial injury by B. anthracis lethal toxin is caused by MKK-dependent loss of cytoskeletal integrity. PLoS One 2009; 4:e4755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Warfel JM, Steele AD, D’Agnillo F. Anthrax lethal toxin induces endothelial barrier dysfunction. Am J Pathol 2005; 166:1871–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Rolando M, Stefani C, Flatau G, et al. Transcriptome dysregulation by anthrax lethal toxin plays a key role in induction of human endothelial cell cytotoxicity. Cell Microbiol 2010; 12:891–905. [DOI] [PubMed] [Google Scholar]
- 35. Russell BH, Vasan R, Keene DR, Koehler TM, Xu Y. Potential dissemination of Bacillus anthracis utilizing human lung epithelial cells. Cell Microbiol 2008; 10:945–57. [DOI] [PubMed] [Google Scholar]
- 36. Popov SG, Popova TG, Hopkins S, et al. Effective antiprotease-antibiotic treatment of experimental anthrax. BMC Infect Dis 2005; 5:25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Firoved AM, Miller GF, Moayeri M, et al. Bacillus anthracis edema toxin causes extensive tissue lesions and rapid lethality in mice. Am J Pathol 2005; 167:1309–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Shetron-Rama LM, Herring-Palmer AC, Huffnagle GB, Hanna P. Transport of Bacillus anthracis from the lungs to the draining lymph nodes is a rapid process facilitated by CD11c+ cells. Microb Pathog 2010; 49:38–46. [DOI] [PubMed] [Google Scholar]
- 39. Jahnsen FL, Strickland DH, Thomas JA, et al. Accelerated antigen sampling and transport by airway mucosal dendritic cells following inhalation of a bacterial stimulus. J Immunol 2006; 177:5861–7. [DOI] [PubMed] [Google Scholar]
- 40. Gallegos-Candela M, Boyer AE, Woolfitt AR, et al. Validated MALDI-TOF-MS method for anthrax lethal factor provides early diagnosis and evaluation of therapeutics. Anal Biochem 2018; 543:97–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. A. Woolfitt AB, Gallegos-Candela M, Lins R, et al. Development of anthrax toxemia in New Zealand white rabbits developing systemic anthrax after exposure to low-dose ames spores. In: The International Conference on Bacillus anthracis, B cereus and B thuringiensis, Vicotria, British Columbia, Canada, 1–5 October 2017.
- 42. A.E. Boyer CPQ, Sanford D, Stark G, et al. Toxin levels predict survival with antimicrobial treatment in nonhuman primate models of inhalation anthrax. In: The International Conference on Bacillus anthracis, B cereus and B thuringiensis, Vicotria, British Columbia, Canada, 1–5 October 2017.
- 43. Lins RC, Boyer AE, Kuklenyik Z, et al. Zeptomole per milliliter detection and quantification of edema factor in plasma by LC-MS/MS yields insights into toxemia and the progression of inhalation Anthrax. Anal Bioanal Chem 2019; 411:2493–509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Xu W, Ohanjanian L, Sun J, et al. Correction: A systematic review and meta-analysis of preclinical trials testing anti-toxin therapies for B. anthracis infection: a need for more robust study designs and results. PLoS One 2017; 12:e0189239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Vietri NJ. Does anthrax antitoxin therapy have a role in the treatment of inhalational anthrax? Curr Opin Infect Dis 2018; 31:257–62. [DOI] [PubMed] [Google Scholar]
- 46. Huang E, Pillai SK, Bower WA, et al. Antitoxin treatment of inhalation anthrax: a systematic review. Health Secur 2015; 13:365–77. [DOI] [PMC free article] [PubMed] [Google Scholar]