Abstract
Background
This study was conducted among healthy adolescents to assess the effects of a yoga breathing practice (Bhramari pranayama, Bhr.P) towards cardiac autonomic function using heart rate variability (HRV) parameters.
Methods
Of the 730 eligible subjects screened, 520 healthy adolescents who met the inclusion and exclusion criteria were randomly assigned to either yoga breathing group (n = 260) or control group (n = 260). The yoga breathing group practiced Bhr.P. five days a week for a duration of six months while the control group continued with their daily routine without any intervention. Outcome measures were time and frequency domain of HRV in both groups which were assessed before and after the intervention using Lead II ECG. Linear models were used in the analysis of short term HRV.
Results
After 6 months of yoga breathing, the time domain parameters of short term HRV showed significant (P < 0.05) improvement towards the parasympathetic domain. Frequency domain parameters also showed the same direction of changes. In contrast, control group subjects showed a trend towards a sympathetic domain.
Conclusion
The present study showed a positive shift in cardiac autonomic modulation towards parasympathetic predominance after 6 months of yoga breathing practice among apparently healthy adolescents.
Keywords: Yoga, Bhramari pranayama, Autonomic function, Heart rate variability, Adolescents
Introduction
Several types of school-based stress management and wellness programs have been developed with the purpose of encouraging healthy coping strategies and resilience among adolescents.1 Adolescence is a vital period for the development of mental health, which also includes healthy coping responses to stress whereas today’s “typical child” is described as stressed out, under nourished, and sedentary.2 One promising approach for this is yoga combines physical exercises, flexibility and strength with relaxation and meditation/ mindfulness techniques.3
Practicing yoga has been associated with numerous health benefits. Bhramari pranayama (Bhr.P) adopts simple regulation of voluntary breathing and can be easily practiced by all irrespective of age or/and gender. Previous studies have mentioned that regular practice of yoga breathing practice reduces the cardiovascular reactivity to stress (cold pressor test) by inducing parasympathetic predominance and cortico- hypothalamo medullary inhibition.4, 5 Reduction of heart rate, blood pressure and autonomic function were observed immediately after 5 min of yoga breathing practice in healthy volunteers and this also shows that it produces parasympathetic domination.6 Enhanced inhibitory response and cognitive control were noted among the healthy individuals followed by 10 min of yoga breathing practice.7 Electroencephalogram (EEG) studies have shown increased theta activity and paroxysmal gamma waves, following the yoga breathing practice, inducing the positive thought and feeling of happiness.8 Yoga breathing has recently shown to improve the acoustic and aerodynamic parameters of voice in healthy subjects.9 Our previous studies on adolescents also showed improvement in cardiovascular parameters and pulmonary function test.10, 11 These are the very few studies that have been done on yoga breathing practice but majority of the studies mentioned above have not met the standard criteria in methodology, design, sample size etc.12
No studies have been done on adolescents to assess the long term practice of the yoga breathing practice on cardiac autonomic function and vagal tone. The aim of this study was to investigate the effects of 6 month practice of yoga breathing practice on cardiac autonomic function.
Participants and methods
Participants
Volunteers between the age group of 13–18 years (subjects recruited in this study are secondary school students) with no previous experience of yoga practice included for the study. Subjects those who were active athletes, smoker/alcoholic, any acute illness, recent surgery, endocrine disorders, cardiovascular disorders, COPD/Asthma, or doing any type of regular physical exercise (>1 h/day) excluded for the participation.13 Adolescent female with regular menses were enrolled into the study and HRV parameters of the subjects were recorded during the proliferative phase of the menstrual cycle of the subjects (5th–7th day of menstruation) to avoid hormonal influence on autonomic function. Out of 210 adolescent girls, 109 belong to yoga breathing group and 101 subjects to control group.
Outcome measures
Our primary outcomes measures were HRV. Linear model heart rate variability analysis was carried out in this study, analyzed in the time and frequency domain. In the time domain, the standard deviation of the NN interval (SDNN), the square root of the mean squared differences of successive NN intervals (RMSSD), the number of interval differences of successive NN intervals greater than 50 ms (NN50), and the proportion derived by dividing NN50 by the total number of NN intervals (pNN50) were used. In frequency domain power spectral density (PSD) analysis in nonparametric method (fast Fourier transform) were used. They were low frequency (LF, 0.04–0.15 Hz) and high frequency (HF, 0.15–0.40 Hz) power expressed in normalized units (LF nu and HF nu, respectively), and LF/ HF ratio.
Experimental procedures
All the subjects were instructed to maintain their normal sleep pattern, not ingest beverages with caffeine or alcohol, and not perform physical exercise 24 h before the evaluations. This test was conducted in morning after 2 h of light breakfast. Subjects were encouraged to void urine before commence of recording. After 15 min of supine rest on a couch, ECG was recorded for 5 min with normal breathing. For the recording of short-term HRV, recommendation of the Task Force on HRV was followed.14 For this purpose, limb Lead II ECG was acquired at a rate of 8000 samples/ second during supine rest using electrocardiogram (ECG) analog to digital converter (AD).15 Since this study includes 520 subjects, we have used five units of simple AD converter for the ECG recording to avoid time gap in pre assessment and post assessment across the groups. Ectopics and artifacts were removed from the recorded ECG after manual checking in offline mode. Thus, HRV data were excluded when recordings have more than 10% of beats were premature, or artifact time exceeded 5% of recorded time. Raw R-R interval data was obtained from simple analog- digital (A–D) converter were stored in the system separately and HRV analysis was done using kubios HRV analysis software version 2.2 (Bio‑signal Analysis group, Finland).
Sample size
The sample size for this study was calculated based on the anticipatory mean difference of 3 with standard deviation 9, alpha of 0.05, power of 0.8 and the effect size of 0.3, which makes up 230 (each group). Taking possible outliers into account, 23 respondents (10%) were added to create a total of 253 respondents so as to cater for the attritions, non-respondent and missing values.
Randomization
Of the 730 potential subjects screened, 210 did not meet the above-described eligibility criteria. All the participants (n = 520) were randomly assigned to either the yoga breathing practice group (n = 260) or no-treatment group (n = 260) by using computerized random allocation software version 1. Allocation concealment was carried out using sequentially numbered opaque sealed envelope (SNOSE), maintained by a person who was not directly involved in the project who handed over the sealed opaque envelopes to the participants.
Blinding/masking
The investigator was blinded from both the group participants. yoga breathing practice was given to the participants by a registered yoga and naturopathy medical practitioner for the entire study period. For HRV, Lead II ECG was assessed by a trained medical physiologist to avoid intra observer variability.
Intervention protocol
Yoga breathing practice (Bhr.P) was taught to the subjects by a qualified yoga and naturopathy physician as per standard method.16 They were allowed to sit in any comfortable sitting posture and with closed eyes they used index finger to close the both ears. The subjects were directed to inhale slowly up to their maximum through both the nostrils. Then, the subjects were instructed to exhale through both the nostrils slowly up to the maximum. During exhalation, the subject must chant the word "Mmmm" with a humming nasal sound mimicking the sound of a humming wasp, and it will mildly vibrate the laryngeal walls and the inner walls of the nostril. Each time when they do the pranayama, they had to do 3–6 breaths/minute for 5 min followed by 2-minute rest. This was considered as one cycle and it was repeated 5 times (5 cycles). In this way, the subjects practiced the pranayama for three days under supervision and two days at home in a week for 6 months. Control group did not do any activity other than their routine schedule for 6 months.
Follow up
Yoga breathing practice group practiced Bhr.P in the morning between 7.30 a.m. to 8.30 a.m. If they did not attend the training more than three days for two consecutive weeks they were dropped from the final analysis. Lecture on importance of yoga training and its role in cognition was delivered very often for motivation and to avoid getting boredom due to the mono training. A log book was maintained to note the timing and duration of practice per day to ensure that the entire yoga breathing group was practiced consistently. Control group subjects continued their routine works and after the post intervention period same level of training (for the period of 6 months includes three days under supervision and two days at home) was continued without any changes in the yoga training protocol.
Statistical analysis
Data is expressed as mean ± standard deviation (SD). Comparison of mean difference in between the group was done using independent t test and intra-group comparison was done using paired t-test. Significant level was set at P < 0.05. R statistical version 3.1.2 was used for the statistical analysis.
Results
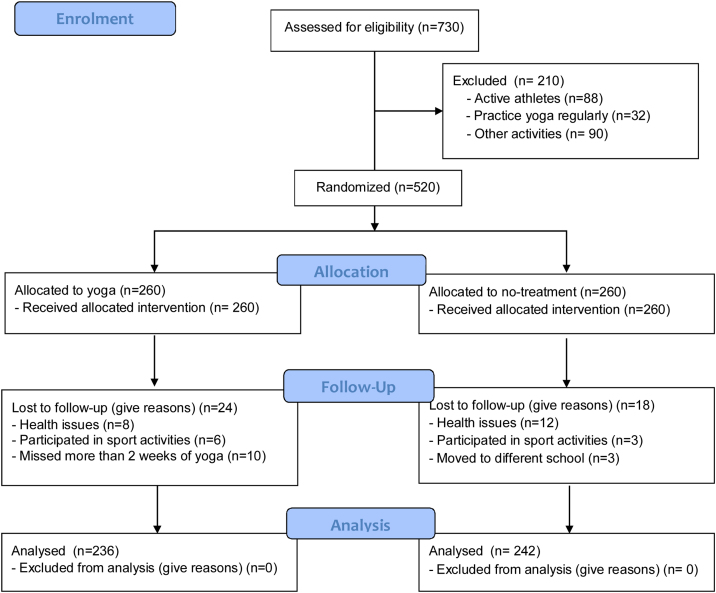
Five hundred and twenty students expressed interest in this study and were deemed eligible. They were randomly divided into two groups (yoga breathing: n = 260 and no treatment control: n = 260). Out of 260 students, eight students had health issues, six students participated in sports activities and ten students were not participated more than 2 weeks in the yoga training and dropout from the final evaluation in yoga breathing group. In control group, twelve students had health issues, three students participated in the regular sports activity and three students changed the school and did not complete the study (Fig. 1).
Fig. 1.
Subjects’ recruitment flow diagram.
Table 1 shows the anthropometry parameters in yoga breathing group and control group. In both groups, age and height, other parameters were not significantly differing. Though height differed in the baseline, BMI did not show any variation and hence we can consider taking these groups for comparison.
Table 1.
Baseline characteristics of the yoga breathing group and no-treatment control group.
| Variables | Yoga breathing (n = 236) | No treatment group (n = 242) | p-Value |
|---|---|---|---|
| Sex (M/F) | 135/101 | 138/109 | 0.480# |
| Age (yrs) | 13.4 ± 0.5 | 14.4 ± 0.6 | 0.430$ |
| Height (cm) | 157.9 ± 11.9 | 161.0 ± 8.4 | 0.010$ |
| Weight (kg) | 51.8 ± 11.5 | 53.5 ± 10.9 | 0.870$ |
| BMI (kg/m2) | 21.1 ± 6.1 | 20.7 ± 4.1 | 0.318$ |
BMI, Body mass index. Data are represented in the mean ± SD (standard deviation). P-values were calculated using unpaired t-test$ and chi-squared test#.
There are significant differences between yoga breathing and no-treatment control in all of the parameters in time domain and frequency domain (Table 2).
Table 2.
Comparison of time domain and frequency domain parameters between yoga breathing group and no-treatment control group.
| Yoga breathing group (n = 236) |
No treatment group (n = 242) |
|||||
|---|---|---|---|---|---|---|
| Before | 6 Months after | Δ Value | Before | 6 Months after | Δ Value | |
| Time domain variable | ||||||
| HR (bpm) | 74.28 ± 4.26 | 69.73 ± 5.29*** | −4.55 ± 1.40 | 73.22 ± 6.05 | 75.18 ± 5.65 | 1.96 ± 1.48† |
| R-R (msec) | 739.05 ± 53.19 | 778.98 ± 61.55*** | 39.93 ± 8.34 | 753.79 ± 48.98 | 750.57 ± 57.53 | −3.21 ± 0.90††† |
| SDNN (sec) | 80.03 ± 10.14 | 88.06 ± 14.83** | 8.03 ± 1.90 | 79.05 ± 12.71 | 77.82 ± 12.32 | −1.22 ± 0.52†† |
| RMSDD (sec) | 59.91 ± 13.50 | 62.05 ± 16.93*** | 2.13 ± 0.34 | 58.78 ± 14.27 | 58.06 ± 13.03 | −0.72 ± 1.20† |
| NN 50 (count) | 26.29 ± 10.16 | 29.68 ± 11.02*** | 3.38 ± 0.45 | 27.33 ± 10.58 | 26.70 ± 11.06 | −0.62 ± 0.92† |
| pNN 50 (%) | 11.20 ± 4.17 | 13.59 ± 7.08*** | 2.39 ± 0.93 | 11.77 ± 4.21 | 10.68 ± 4.08** | −1.08 ± 0.24†† |
| Frequency domain variable | ||||||
| LF (n.u) | 65.06 ± 11.67 | 57.02 ± 12.29*** | −4.87 ± 0.91 | 63.95 ± 11.66 | 65.86 ± 11.37*** | 1.11 ± 0.32†† |
| HF (n.u) | 40.08 ± 9.01 | 46.87 ± 11.22*** | 6.14 ± 1.20 | 40.05 ± 8.88 | 40.72 ± 8.95 | −0.02 ± 0.07†† |
| LF/HF Ratio | 1.60 ± 0.42 | 1.37 ± 0.40*** | −0.21 ± 0.02 | 1.71 ± 0.44 | 2.06 ± 0.55*** | 0.32 ± 0.11††† |
Data are represented in the mean ± SD (standard deviation). Δ (Delta), changes between before and 6-months after treatment.
HF, high-frequency power; HR, heart rate; LF, low-frequency power; LF/HF, ratio of low frequency to high-frequency power; NN50, number of pairs of adjacent NN intervals differing by more than 50 ms in the entire recording; n.u, normalized unit; pNN50, percentage of absolute differences between successive normal RR intervals that exceed 50 ms; RR, normal-to-normal interval; RMSSD, root-mean-square of the successive normal sinus RR interval difference; SDNN, the standard deviation of the normal-normal interval.
*p < 0.05, **P < 0.01, ***p < 0.001 compared with before and 6 months after.
†p < 0.05, ††P < 0.01, †††p < 0.001 compared with yoga and control group.
Discussion
Our study showed that yoga breathing practice may improve sympathovagal balance among the adolescents. This study has highlighted the usefulness of a simple yoga breathing technique in improving the autonomic function of adolescent children. HF power is influenced by breathing rate, so in this case, it is always better to couple with other time domain parameters supposed to index vagal tone to see which extent they correlate, for example with RMSSD that is supposed to be less affected by respiratory influences.17 We have found that a significant improvement in both RMSSD in time domain and HF power (n.u) in frequency domain parameters which gives more strength to our results.
Previous studies have been reported that long-term practice of pranayama is associated with improvement in autonomic regulation of cardiac function in both healthy and diseased population, reflected by a shift toward parasympathetic dominance.18, 19, 20 The improvement of HRV at rest after 6 months of yogic breathing would indicate greater parasympathetic nervous system activity and may reduce the risk of cardiovascular morbidity.
There are some limitations to this study which merit consideration while interpreting the outcomes. Firstly, it would have added more value if the current large sized RCT is conducted as a double-blinded study. However, it was not possible to blind the participants from the yoga intervention. Secondly, the outcome of the study was assessed only after 6 months of intervention; if the outcomes would have been measured multiple time points within the six months would be more informative for the inference. Thirdly, lack of an active control group in the study.
In conclusion, our study showed a positive shift in cardiac autonomic modulation towards parasympathetic predominance after 6 months of yoga breathing practice in healthy adolescents. However, further studies should be conducted using active control groups.
Authors’ contribution
Author KM, RP and KD conceived the study idea. AJ and SP contributed to data collection. PR and KM did data analysis. SP, KM and VV wrote the manuscript. RP did the final proof reading and corrections.
Funding
This study was sponsored by grants-in aid by Sri Ramachandra Institute of Higher Education and Research (SRIHER) for perusing Ph.D under Chancellor Sri N.P.V Ramasamy Udayar Research fellowship.
Ethical statement
This study was approved by the Ethical Committee (IEC-N1/14/JAN/38/07) of Sri Ramachandra institute for higher education and Research (SRIHER). Written permission was obtained from the school management before starting the project. The participants received explanations of the purpose and contents of the study, the voluntary nature of their participation and benefits of this yoga practice. Written consent was then obtained from each participant parents/guardians and a separate assent also obtained from the participants.
Data availability
The data that support the findings of this study are available from the corresponding author, upon request.
Conflict of interest
Authors declare no conflict of interest
Acknowledgment
We express our sincere gratitude and thanks to all our students participated in this study.
References
- 1.Kraag G., Zeegers M.P., Kok G., Hosman C., Abu-Saad H.H. School programs targeting stress management in children and adolescents: a meta-analysis. J Sch Psychol. 2006;44:449–472. [Google Scholar]
- 2.Stueck M., Gloeckner N. Yoga for children in the mirror of the science: working spectrum and practice fields of the training of relaxation with elements of yoga for children. Early Child Dev Care. 2005;175:371–377. [Google Scholar]
- 3.Salmon P., Lush E., Jablonski M., Sephton S.E. Yoga and mindfulness: clinical aspects of an ancient mind/body practice. Cogn Behav Pract. 2009;16:59–72. [Google Scholar]
- 4.Jain G., Rajak C., Rampalliwar S. Effect of bhramari pranayama on volunteers having cardiovascular hyper-reactivity to cold pressor test. J Yoga Phys Ther. 2011;1:102. [Google Scholar]
- 5.Rampalliwar S., Rajak C., Arjariya R., Poonia M., Bajpai R. The effect of bhramari pranayama on pregnant women having cardiovascular hyper-reactivity to cold pressor. Natl J Physiol Pharm Pharmacol. 2013;3:128–133. [Google Scholar]
- 6.Pramanik T., Pudasaini B., Prajapati R. Immediate effect of a slow pace breathing exercise Bhramari pranayama on blood pressure and heart rate. Nepal Med Coll J. 2010;12:154–157. [PubMed] [Google Scholar]
- 7.Rajesh S.K., Ilavarasu J.V., Srinivasan T.M. Effect of Bhramari Pranayama on response inhibition: evidence from the stop signal task. Int J Yoga. 2014;7:138. doi: 10.4103/0973-6131.133896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vialatte F.B., Bakardjian H., Prasad R., Cichocki A. EEG paroxysmal gamma waves during Bhramari Pranayama: a yoga breathing technique. Conscious Cogn. 2009;18:977–988. doi: 10.1016/j.concog.2008.01.004. [DOI] [PubMed] [Google Scholar]
- 9.Manjunatha U., Bhat J.S., Radish K.B., Bajaj G., Shruthi P., Nayak P.S. Effect of Bhramari Pranayama on the acoustic and aerodynamic parameters of voice in normophonic females. Evid-Based Complementary Altern Med. 2018;2018 doi: 10.1155/2018/4176803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kuppusamy M., Dilara K., Ravishankar P., Julius A. Effect of bhrāmarī Prāṇāyāma practice on pulmonary function in healthy adolescents: a randomized control study. Anc Sci Life. 2017;36:196. doi: 10.4103/asl.ASL_220_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kuppusamy M., Kamaldeen D., Pitani R., Amaldas J. Immediate effects of Bhramari pranayama on resting cardiovascular parameters in healthy adolescents. J Clin Diagn Res. 2016;10 doi: 10.7860/JCDR/2016/19202.7894. CC17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kuppusamy M., Kamaldeen D., Pitani R., Amaldas J., Shanmugam P. Effects of Bhramari Pranayama on health–A systematic review. J Tradit Complement Med. 2017;18(8):11–16. doi: 10.1016/j.jtcme.2017.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tucker J.M., Welk G.J., Beyler N.K. Physical activity in US adults: compliance with the physical activity guidelines for Americans. Am J Prev Med. 2011;40:454–461. doi: 10.1016/j.amepre.2010.12.016. [DOI] [PubMed] [Google Scholar]
- 14.Cardiology ESo. the North American Society of Pacing and Electrophysiology Heart rate variability: standards of measurement, physiological interpretation, and clinical use; Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Circulation. 1996;93:1043–1065. [PubMed] [Google Scholar]
- 15.Maheshkumar K., Dilara K., Maruthy K., Sundareswaren L. Validation of PC-based sound card with biopac for digitalization of ECG recording in short-term HRV analysis. N Am J Med Sci. 2016;8(7):307. doi: 10.4103/1947-2714.187150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Saraswati S.S., Hiti J.K. Bihar Yoga Bharati; 1996. Asana pranayama mudra bandha. [Google Scholar]
- 17.Stevenson I., Ripley H.S. Variations in respiration and in respiratory symptoms during changes in emotion. Psychosom Med. 1952;14:476–490. doi: 10.1097/00006842-195211000-00006. [DOI] [PubMed] [Google Scholar]
- 18.Hill L., Siebenbrock A., Sollers J., Thayer J.F. Are all measures created equal? Heart rate variability and respiration. Biomed Sci Instrum. 2009;45:71–76. [PubMed] [Google Scholar]
- 19.Khattab K., Khattab A.A., Ortak J., Richardt G., Bonnemeier H. Iyengar yoga increases cardiac parasympathetic nervous modulation among healthy yoga practitioners. Evid.-Based Complementary Altern Med. 2007;4:511–517. doi: 10.1093/ecam/nem087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Satyapriya M., Nagendra H.R., Nagarathna R., Padmalatha V. Effect of integrated yoga on stress and heart rate variability in pregnant women. Int J Gynaecol Obstet. 2009;104:218–222. doi: 10.1016/j.ijgo.2008.11.013. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author, upon request.