Abstract
Context:
Efficient management and allocation of scarce medical resources can improve outcomes for victims of Mass Casualty Events (MCEs). However, the effectiveness of specific strategies has never been systematically reviewed.
Objectives:
We analyzed published evidence on strategies to optimize the management and allocation of scarce resources across a wide range of MCE contexts and study designs.
Data Sources:
Our literature search included Medline, Scopus, Embase, Cumulative Index to Nursing and Allied Health Literature, Global Health, Web of Science®, and the Cochrane Database of Systematic Reviews, from 1990 through late 2011. We also searched the grey literature using the New York Academy of Medicine’s Grey Literature Report and key websites. We included both English and foreign language articles.
Study Selection:
We included studies that evaluated strategies employed in real-world MCEs or tested through drills, exercises, or computer simulations. We excluded studies that lacked a comparison group or did not report quantitative outcomes.
Data Extraction and Synthesis:
Data extraction, quality assessment, and strength of evidence ratings were conducted by a single researcher and reviewed by a second; discrepancies were reconciled by the two reviewers. Due to heterogeneity in outcome measures, we qualitatively synthesized findings within categories of strategies.
Results:
From 5,716 potentially relevant citations, 74 studies met inclusion criteria. Strategies included: reducing demand for healthcare services (18 studies), optimizing use of existing resources (50), augmenting existing resources (5), implementing crisis standards of care (5), and multiple categories (4). The evidence was sufficient to form conclusions on two strategies, although the strength of evidence was rated as low. First, as a strategy to reduce demand for healthcare services, Points of Dispensing (PODs) can be used to efficiently distribute biological countermeasures following a bioterror attack or influenza pandemic, and their organization influences speed of distribution. Second, as a strategy to optimize use of existing resources, commonly used field triage systems do not perform consistently during actual MCEs. The number of high-quality studies addressing other strategies was insufficient to support conclusions about their effectiveness because of differences in study context, comparison groups, and outcome measures.
Limitations:
Our literature search may have missed key resource management and allocation strategies due to their extreme heterogeneity. Inter-rater reliability was not assessed for quality assessments or strength of evidence ratings. Publication bias is likely given the large number of studies reporting positive findings.
Conclusions:
The current evidence base is inadequate to inform providers and policymakers about the most effective strategies for managing or allocating scarce resources during MCEs. Consensus on methodological standards that encompass a range of study designs is needed to guide future research and strengthen the evidence base. Evidentiary standards should be developed to promote consensus interpretations of the evidence supporting individual strategies.
Introduction
Mass casualty events (MCEs) generate large numbers of acutely ill or injured people who require immediate medical and/or mental healthcare.1 MCEs may occur suddenly, as is typical of an earthquake, tornado, or bombing,2 but they may also evolve gradually over hours, days or even weeks, as is typical of a hurricane, flood, epidemic, or a chemical attack.3
For the purpose of this review, we define an MCE as an event that produces demand for medical care that may outstrip the capacity of local or even regional healthcare systems to provide conventional standards of care to the affected population.4 Because MCEs typically occur with little or no warning, providers must have contingency plans to meet exceptional demands for care. If these measures prove to be inadequate, providers may need to re-allocate resources using a fair, equitable, and transparent process—a concept known as “crisis standards of care.”5
Many strategies have been suggested to optimize management and allocation of scarce resources during an MCE, including cancelling elective admissions, conserving and reusing resources, accessing resources from stockpiles, and implementing early Intensive Care Unit discharge protocols. These examples illustrate four broad categories of strategies that providers and policymakers might use to manage and allocate scarce resources during an MCE: (1) managing or reducing less urgent demand for healthcare services, (2) optimizing use of existing resources, (3) augmenting existing resources, and (4) implementing crisis standards of care (Table 1).
Table 1.
Conceptual Framework for the Review
| Resource Management Strategies under Conventional or Contingency Conditions | Implement Strategies Consistent with Crisis Standards of Care | |||
|---|---|---|---|---|
| Manage/reduce less urgent demand for healthcare services | Maximize use of existing resources | Augment resources | ||
| Policy Makers |
|
|
|
|
| Providers |
|
|
|
|
The effectiveness of implementing specific strategies in each of these areas across a range of meaningful outcomes, particularly patients’ health, has not been systematically assessed. To help policymakers and providers identity the best options, the Office of the Assistant Secretary for Preparedness and Response (ASPR), U.S. Department of Health and Human Services, formally requested that the Agency for Healthcare Research and Quality (AHRQ) commission a systematic review of the evidence on the effectiveness of resource management and allocation strategies across a wide range of MCE contexts.
Methods
This evidence review was guided by a 2009 report issued by the Institute of Medicine (IOM) describing adaptive strategies for surge conditions arising from MCEs.5 We organized our work around the four broad categories of strategies mentioned above—a framework that accommodated the vast majority of strategies that were referenced in the IOM report. We sought to identify the best available evidence within each broad category. The full report with additional details on our methodology can be found elsewhere.6 The 27-item PRISMA Checklist guided the structure and the content of this report (See Appendix A).7
Data Sources
To identify relevant studies, we searched seven research databases, including PubMed, Scopus, Embase, Cumulative Index to Nursing and Allied Health Literature, Global Health, Web of Science®, and the Cochrane Database of Systematic Reviews, from 1990 through November 2011. To identify relevant books, we searched the National Library of Medicine’s online catalog. We supplemented these searches with a scan of the grey literature using the New York Academy of Medicine’s Grey Literature Report and websites of government agencies, provider organizations, and academic research centers. Appendix B contains a list of the literature search terms.
Study Selection
We considered both U.S. and international sources, including non-English language articles that met our two primary inclusion criteria. First, eligible studies had to prospectively assess a strategy during an actual event; document its impact in an after-action report; or test its effectiveness in an exercise, drill, or computer simulation. Second, to ensure studies met a minimum threshold of scientific rigor, they had to have compared an intervention with one or more alternative interventions, employ a control group, or use some other objective benchmark. Given the anticipated diversity of strategies, we considered a broad set of outcome measures, including health, cost, ethical, and legal outcomes, as well as process measures, such as triage accuracy rate and triage time. Because studies inconsistently reported the issuance of disaster declarations and often failed to fully characterize the extent of resource shortages, our review included both MCEs and quite likely some events that produced conditions of excessive surge that would not be classified as MCEs. Appendix C contains a list of excluded studies and the reasons for exclusion.
Data Extraction and Quality Assessment
Two researchers screened all titles. Abstracts and full-text articles underwent dual review. We resolved disagreement by consensus or when necessary, third-party reconciliation. Data were abstracted using the DistillerSR program. Core data elements included study design, geographic location, type of MCE, description of the strategy, outcomes, and facilitators and/or barriers to the implementation of each strategy.
After finding no suitable quality assessment tools in the peer-reviewed literature, we developed a 5-item scale that enabled comparisons of methodological quality across diverse types of studies. We combined key domains from three sources. From the National Registry of Evidence-based Programs and Practices (NREPP)8 quality assessment scale from the Substance Abuse and Mental Health Services Administration we used two items: (1) whether the strategy was implemented with fidelity (i.e., implemented consistently), and (2) whether the authors discussed potential confounders to the strategy’s effectiveness. The remaining three items represent core elements of two common frameworks commonly used to appraise the quality of qualitative research: those by Mays & Pope9 and Lincoln & Guba.10 These three items assessed whether or not: (1) the level of detail used to describe the resource allocation strategy was adequate, (2) data collection was systematic (and if so, whether it was retrospective or prospective), and (3) the authors assessed the generalizability of findings. Two reviewers reconciled all differences in scores for each quality item. For computer simulations, we included two items that assessed justification of model inputs and the robustness of sensitivity analyses (and eliminated the data collection item and implementation fidelity item). For systematic reviews, we used the 11-item AMSTAR instrument.11
Data Synthesis and Analysis
Because of the breadth of topics we reviewed, we conducted systematic reviews within sub-categories of resource management/allocation strategies. We combined these results into a single report because our conclusions were largely similar across most categories. The data were not amenable to quantitative synthesis because abstracted studies rarely addressed similar strategies. Moreover, when multiple studies did assess a common strategy, they typically differed widely in their settings, comparison groups, and outcome measures. Accordingly, we summarized the results qualitatively, using the four broad categories from the conceptual framework shown in Table 1 and sub-categories when clusters of related strategies emerged. Wherever possible, we summarized the degree of consistency in the magnitude and direction of the most relevant outcomes. We also highlighted contextual and methodological differences that were relevant to the interpretation of results.
We graded the strength of evidence using the methodology commonly employed for systematic reviews commissioned by AHRQ.12 It requires reviewers to consider four key domains: risk of bias, consistency, directness, and precision, then grade the overall strength of the evidence using a four-point scale (i.e., high, moderate, low, or insufficient). Grades were assigned by one reviewer and confirmed by a second, followed by discussion when conflicts arose. We rated the strength of evidence within the four domains for individual categories (or subcategories) of resource management/allocation strategies depending on the number of studies available. A single reviewer graded the strength of evidence for each domain within categories of strategies and overall. The ratings were then reviewed by a second researcher and differences were reconciled through discussion.
Results
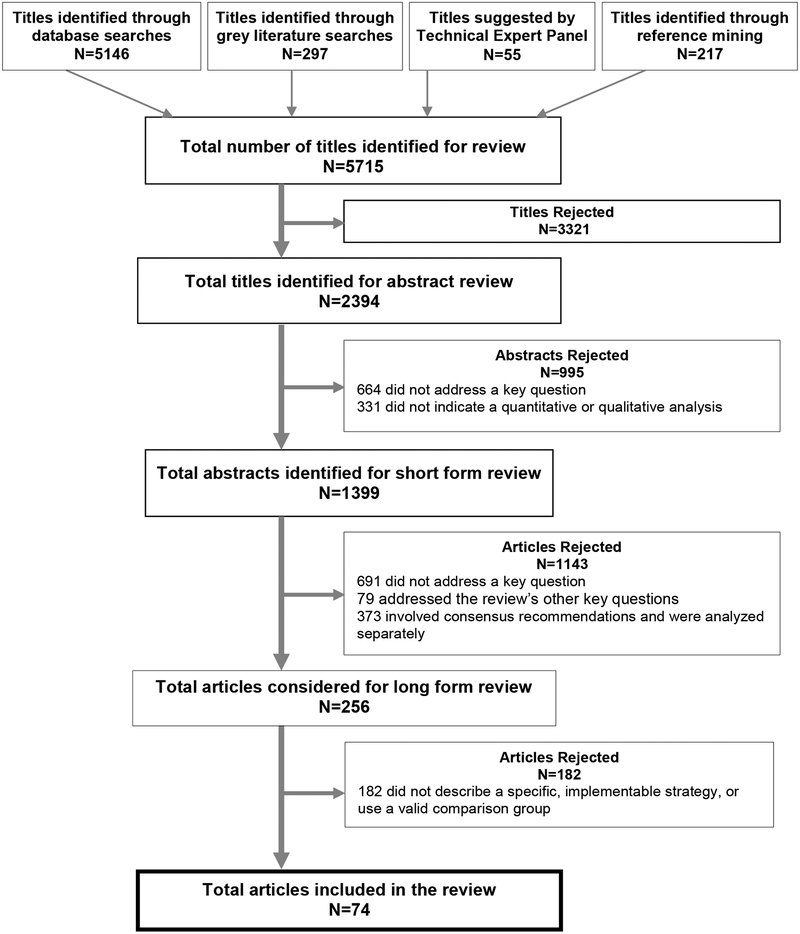
Our search strategy identified 5,716 potentially relevant citations. After applying exclusion criteria, only 74 articles underwent data extraction (Figure 1). These 74 studies comprised three main types of analyses: 48 were intervention studies (i.e., involving human subjects), including 23 that evaluated the outcomes of drills and 25 that reported findings from actual MCEs (Table 2). Nearly half of the intervention studies (25 of 48) occurred in the United States. The other 23 took place elsewhere, particularly Europe (8) and Israel (6). The remaining 26 non-intervention studies included computer simulations (17), systematic reviews (2), validation analyses (5), and laboratory studies (2).
Figure 1.
Literature flow
Table 2.
Characteristics of Studies Included in the Review
| Number of studies (Percent of all studies) | |
|---|---|
| All studies | 74 (100) |
| Study type | |
| Intervention studies* | 48 (65) |
| Drills | 23 (48) |
| Actual MCEs | 25 (52) |
| Computer simulations | 17 (23) |
| Systematic reviews | 2 (3) |
| Validation analyses | 5 (7) |
| Laboratory analyses | 2 (3) |
| Study setting** | |
| United States | 25 (52) |
| Europe | 8 (17) |
| Israel | 6 (13) |
| Asia | 3 (6) |
| Canada | 2 (4) |
| Australia | 1 (2) |
| Mexico | 1 (2) |
| Rwanda | 1 (2) |
| Haiti | 1 (2) |
| Type of event | |
| Pandemic influenza | 13 (18) |
| Explosive | 10 (14) |
| Multiple hazards | 10 (14) |
| Anthrax | 7 (9) |
| Natural disasters: earthquake | 6 (8) |
| Natural disasters: hurricane | 3 (4) |
| Nuclear/radiological events | 3 (4) |
| Transportation accidents | 3 (4) |
| Chemical events | 3 (4) |
| Smallpox | 2 (3) |
| SARS | 1 (1) |
| Other | 3 (4) |
| Unspecified events | 10 (14) |
We use the term “intervention study” to refer to any study that tested a strategy with human subjects, and includes both drills and actual MCE.
Among intervention studies only
Twenty-three studies focused on biological threats, including pandemic influenza (13), anthrax (7), smallpox (2), and SARS (1). Nine studies addressed natural disasters including 6 earthquakes (3 of which involved Hurricane Katrina). Ten reported outcomes following a terrorist attack with explosives. The remaining MCEs included: nuclear/radiological events (3), transportation accidents (3), chemical events (3), multiple hazards (10), unspecified events (10), and other types of MCEs (5).
Table 3 groups the studies according to the four broad categories of resource allocation strategies defined in our conceptual framework. In the sections that follow, we discuss only the studies relevant to distribution of “biological countermeasures” and “field triage,” the two subcategories for which the evidence was sufficient to form tentative conclusions about their effectiveness. We also summarize the available evidence on implementation of crisis standards of care—an area of particular interest to providers and policymakers. Appendix D contains detailed descriptions of each study.
Table 3.
Resource Allocation Strategies Included in the Systematic Review
| Author | Study type | MCE type | Description of Strategies | Quality Score | Summary |
|---|---|---|---|---|---|
| Strategies to reduce or manage less-urgent demand for healthcare services | |||||
| Allocation of biological counter-measures | |||||
| Arora, 201039 | Computer sim | Influenza | Optimize level of pre-allocation of antiviral stockpile and percentage allocated for prophylaxis and treatment for influenza | 4/7 | Non-comparable strategies Three different biological threats studied All studies were computer simulations Insufficient evidence |
| McCaw, 200840 | Computer sim | Influenza | Optimize the use of multiple drugs for prophylaxis and/or treatment | 7/9 | |
| Wein, 200341 | Computer sim | Anthrax | Implement prioritization policies, biosensor deployment, and/or deploy federal or military resources and volunteers | 5/9 | |
| Bravata, 200642 Zaric, 200843 |
Computer sim Computer sim |
Anthrax Anthrax |
Increase local stockpiles, deploy stockpile to targeted areas, enhance detection, or increase dispensing capacity | 7/9 3/9 |
|
| Glasser, 201044 McVernon, 201045 Medlock, 200946 |
Computer sim Computer sim Computer sim |
Influenza Influenza Influenza |
Targeting vaccination to different populations | 2/7 4/7 5/9 |
|
| Zenihana, 201047 | Computer sim | Smallpox | Mass vaccination, contact tracing, and school closure | 3/7 | |
| Distribution of biological counter-measures | |||||
| Ablah, 201013 | Exercise | Anthrax | Centralized POD system vs. hybrid (“pull” and “push” approach) | 6/8 | Mail carrier strategy may dominate centralized model Three large-scale exercises Low strength of evidence |
| Koh, 200814 | Exercise | Anthrax | Centralized POD system vs. “push” model utilizing U.S. Postal Service mail carriers | 6/8 | |
| Lee, 200615 | Exercise | Anthrax | POD operations supported by a decision-support software tool | 4/8 | |
| Hupert, 200916 | Computer sim | Anthrax | Use of dynamic staffing during POD implementation | 2/7 | |
| Erwin, 200917 | Actual MCE | Smallpox | Implementation of CDC mass vaccination protocol | 4/8 | |
| Nonbiological counter-measures | |||||
| Cahill, 200848 | Computer sim | Influenza | Distribution of surgical masks or N95 respirators to the public | 2/9 | Each study evaluated a distinct strategy Insufficient evidence |
| Schull, 200749 | Actual MCE | SARS | Restrict non-urgent demand for hospital care | 4/8 | |
| Savovia, 200950 | Exercise | Influenza | Training public health officials in their legal authority to implement strategies to limit the spread of pandemics | 4/7 | |
| Adini, 201051 | Actual MCE | All-hazards | Automated central information distribution system for families | 4/8 | |
| Strategies to optimize use of existing resources | |||||
| Field Triage studies: Implementation Tests | |||||
| Cohen, 199852 | Actual MCE | Explosive | American College of Surgeons Committee on Trauma criteria | 4/8 | Few triage systems tested during real events; Studies assessed different outcomes; Few studies tested in real MCEs assessed mortality. Low strength of evidence |
| Cone, 200818 | Exercise | Chemical | Combined trauma/CBRN-specific system | 6/8 | |
| Rodriguez-Noriega, 201020 | Actual MCE | Influenza | Influenza-Like Illness Scoring System |
5/8 | |
| Aylwin, 200631 | Actual MCE | Explosive | London transit bombings protocol | 5/8 | |
| Kuniak, 200819 | Exercise | Radiological | Radiation Injury Severity Classification | 6/8 | |
| Cone, 200953 Lerner, 201054 | Exercise Exercise |
All-hazards Explosive |
Sort- Assess- Lifesaving Interventions- Treatment/transport (SALT) protocol | 5/8 5/8 |
|
| Zoraster, 200721 Schenker, 200622 |
Actual MCE Exercise |
Transportation accident Multiple |
Simple Triage and Rapid Treatment (START) | 4/6 6/8 |
|
| Gutsch, 200655 | Exercise | Unspecified | Modified START triage algorithm (mSTART) | 4/4 | |
| Rehn, 201056 | Exercise | Transportation accident | Interdisciplinary Emergency Service Cooperation Course (TAS Triage Method) | 6/8 | |
| Cryer, 201057 | Actual MCE | Transportation accident | Los Angeles Commuter Rail accident | 5/8 | |
| Janousek, 199958 | Exercise | Multiple | NATO triage classification system | 3/7 | |
| Field Triage studies: Derivation/Validation Studies | |||||
| Adeniji, 201159 | Validation | Influenza | Simple Triage Scoring System (STSS) | 3/6 | |
| Casagrande, 201160 | Computer sim | Nuclear | Model of Resource and Time-based Triage | 6/9 | |
| Cancio, 200861 | Validation | Combat | Field Triage Score vs. Revised Trauma Score | 4/6 | |
| Guest, 200962 | Validation | Influenza | Christian et al. triage protocol | 5/7 | |
| Navin, 200925 Sacco, 200727 |
Computer sim Computer sim |
Unspecified Unspecified |
Sacco Triage method | 3/7 5/7 |
|
| Nie, 201063 | Actual MCE | Earthquake | Modified START (includes resuscitation category) | 2/8 | |
| Beyersdorf, 199664 | Actual MCE | Mass shooting | Revised Trauma Score vs. Pre-hospital Index vs. Washington state Pre-hospital Trauma Triage Procedure | 2/6 | |
| Kilner, 201023 | Sys Review | Multiple | Systematic review of triage systems | 8/8 | |
| Field Triage studies: other | |||||
| Hirshberg, 201065 | Computer sim | Explosive | Role assignment during two-stage triage system | 6/9 | |
| Romm, 201166 | Laboratory Test | Radio/Nucl | Expedited biodosimetry method | 5/5 | |
| Gao, 200767 | Exercise | Unspecified | Electronic triage tags to monitor vital signs and transmit information to first responders | 5/8 | |
| Load-sharing | |||||
| Kanter, 200728 Epley, 200668 Leiba, 200669 Raiter, 200870 Xiong, 201071 |
Computer sim Actual MCE Actual MCE Actual MCE Computer sim |
Unspecified Hurricane Explosive Explosive Earthquake |
Existing regional systems to optimize allocation of patients to hospitals |
3/9 4/8 2/8 3/8 2/7 |
Israeli home command system may not be generalizable to US Three studies provide low-applicability evidence Insufficient evidence |
| Simon, 200172 | Actual MCE | Explosive | Ad hoc incident command structures to optimize allocation of patients to hospitals | 2/8 | |
| Wolf, 200973 | Exercise | Unspecified | Load-sharing protocol for mass gatherings | 8/8 | |
| Imaging | |||||
| Beck-Razi, 200774 Sarkisian, 199175 |
Actual MCE Actual MCE |
Explosive Earthquake |
Focused assessment of sonography for trauma (FAST) for triage | 6/8 4/8 |
Sonogram studies used distinct gold standards; CT protocols tested in exercises only Insufficient evidence |
| Korner, 200676 Korner, 201177 |
Exercise Exercise |
Unspecified Unspecified |
Accelerated CT protocols |
5/7 7/8 |
|
| Medical Interventions | |||||
| Gunal, 200478 | Actual MCE | Earthquake | Medical interventions for the prevention of acute renal failure in crush victims | 6/8 | Studies addressed different topics Insufficient evidence |
| Vardi, 200479 | Exercise | Chemical | Novel drug infusion devices | 6/8 | |
| Space optimization | |||||
| Satterthwaite, 201080 Van Cleve, 201181 |
Actual MCE Actual MCE |
Explos/Trans accident Influenza |
Reverse triage to create surge capacity | 2/7 5/8 |
Only one of the two reverse triage protocols was truly tested Insufficient evidence |
| Scarfone, 201182 | Actual MCE | Influenza | Conversion of lobbies, clinics, and other units to accommodate surge | 2/8 | |
| Training | |||||
| Hsu, 200483 | Sys Review | Multiple | MCE response training (including drills, tabletop exercises, computer simulations) | 7/10 | Systematic review suggests drills are effective; Most studies reported lessons learned; Longer term effectiveness of training is unknown Insufficient evidence |
| Jarvis, 200984 | Exercise | Unspecified | Game-based training | 4/8 | |
| Andreatta, 201085 Vincent, 200886 |
Exercise Exercise |
Explosive Unspecified |
Virtual reality training | 6/6 4/7 |
|
| Vincent, 200987 | Exercise | Explosive | Podcasts and multi-manikin simulations | 3/5 | |
| Sanddal, 200488 | Exercise | Explos/Trans accident | “JumpSTART” training session followed by drill | 6/8 | |
| Other | |||||
| Einav, 200989 | Actual MCE | Explosive | Hospital-based case managers to ensure care coordination | 3/8 | Studies addressed different topics Insufficient evidence |
| Amlot, 201090 | Exercise | CBRN | Multiple strategies to increase decontamination effectiveness | 3/6 | |
| Loeb, 200937 | Actual MCE | Influenza | Influenza prophylaxis for healthcare workers: surgical masks vs. N95 respirators | 5/6 | |
| Strategies to augment existing resources | |||||
| Temporary facilities | Three studies assessing temporary facilities shared same context: hurricane. Potentially limited generalizability to other MCEs. Insufficient evidence |
||||
| Eastman, 200791 | Actual MCE | Hurricane | Alternate-site surge capacity facilities | 4/7 | |
| Blackwell, 200792 | Actual MCE | Hurricane | Deployment of mobile field hospital | 3/5 | |
| Wein, 200341 | Computer sim | Anthrax | Activating mobile provider units from other federal agencies to provide hospital surge capacity | 5/9 | |
| Other | |||||
| Arora, 201039 | Computer sim | Influenza | Mutual aid agreements for the transfer of antivirals between counties | 4/7 | |
| Corvino, 200693 | Laboratory | Chemical | Conversion between formulations of nerve agents to augment supply | 6/7 | |
| Strategies for implementing crisis standards of care | |||||
| Damage-control surgery/care | Contexts include terrorist bombing, earthquake, civil war, and unspecified. Limited measurement of patient outcomes Insufficient evidence |
||||
| Dhar, 200829 Labeeu, 199630 |
Actual MCE Actual MCE |
Earthquake Combat |
External fixation of fractures rather than definitive orthopedic care | 5/8 1/6 |
|
| Aylwin, 200631 | Actual MCE | Explosive | Limited advanced on-scene interventions, delaying non-urgent CT scans, limited use of blood typing and cross-matching | 5/8 | |
| Other | |||||
| Merin, 201032 | Actual MCE | Earthquake | Very early discharge from intensive care unit | 1/6 | |
| Kanter, 200728 | Computer sim | Unspecified | Essential interventions (unspecified) for pediatric MCE victims | 3/9 | |
Notes: Computer sim=computer simulation. The numerator of the quality score reflects the number of points achieved. The denominator reflects the total number of points for the applicable items.
Reduction of demand through rapid distribution of biological countermeasures.
Among the 18 studies that addressed strategies to reduce or manage demand for healthcare services, five examined the utility of “points of dispensing,” or PODs, to speed distribution of biological countermeasures. Three of the five studies used exercises to assess techniques for rapidly distributing medical countermeasures against anthrax. The first of these, an exercise conducted in Nassau County, NY, demonstrated that a traditional “centralized” POD system provided slightly faster throughput than a hybrid model. In the centralized POD model, individuals came to a fixed site to receive a medical countermeasure (a “pull” approach), whereas in the hybrid model, the “pull” approach was combined with a “push” strategy in which countermeasures were distributed to individuals at their work site.13
The second study compared a “pull” model to a different type of “push” model—one that used U.S. Postal Service mail carriers to deliver countermeasures to people’s homes.14 It found that using mail carriers served more people per hour per provider than did operating a fixed dispensing site. Although these two studies provide only limited evidence, both were relatively large-scale, high-quality exercises that were conducted in different geographic regions. Therefore, we judged them as providing highly applicable evidence.
The third study, a multi-county exercise in metropolitan Atlanta, documented that POD operations supported by a particular decision-support software tool were more efficient than traditional dispensing systems. However, the majority of findings from this study were qualitative in nature and therefore not comparable to the other results in this category.15 This same software tool was used to simulate different patient arrival patterns in another study of the effectiveness of PODs that concluded that a dynamic staffing model significantly reduces waiting times for individuals seeking countermeasures.16
The only POD study conducted during an actual MCE involved countermeasure distribution during a Hepatitis A outbreak in Eastern Tennessee. In this study, the community implemented a mass vaccination protocol originally developed by the CDC for anthrax and achieved benchmark levels of throughput.17
Although two exercise-based studies that compared different POD systems were judged to provide high-quality evidence, neither tested the approach during an actual event. Furthermore, only two of the five studies in this category were comparable, representing a very limited evidence base. Accordingly, the overall strength of evidence regarding the optimal approach to distributing biological countermeasures was rated as low.
Pre-hospital triage systems.
Among the 50 studies that evaluated strategies intended to optimize use of existing resources during an MCE, fully half focused on pre-hospital (also known as “field”) triage systems. Thirteen studies assessed the performance of responders who used these triage systems during a drill or an actual MCE, while 9 sought to validate new or existing triage systems through other design (e.g., medical record review). The other 3 examined issues related to triage, but were determined to be non-comparable. We concluded that the strength of evidence to favor use of any particular field triage system over others was low.
Implementation Tests of Triage Systems.
Thirteen studies of field triage systems examined their performance during actual (6) or simulated MCEs (7). Few of the triage tools assessed in these tests applied to pediatric victims, and only two studies addressed chemical, biological, radiological, or nuclear MCEs.18,19 Most focused on adult populations involving victims of trauma and thus used quite similar triage protocols.
The reported accuracy of these systems ranged from 62 to 100 percent across the ten studies that included this information (Table 4). Studies reporting results from actual MCEs (two terrorist bombing events, including the London Transit bombings), suggest that over-triage rates may range from 33 to 64 percent. In another study, the use of “reverse” triage among patients with low scores on an influenza-like illness scale successfully increased surge capacity in a Mexican Emergency Department during the 2009 H1N1 pandemic.20
Table 4.
Accuracy of Triage for Individual Triage Tools Reported in Ten Included Studies
| Triage system | Study Design | Under-triage rate (%) | Over-triage rate (%) | Overall Triage accuracy (%) |
|---|---|---|---|---|
| ACS Committee on Trauma criteria52 | MCE | 1* | 33 | - |
| Influenza-like Illness Scoring system20 | MCE | <1 | - | - |
| London transit bombings triage method31 | MCE | - | 64 | - |
| CBRN triage system18 | Drill | 11 | 2 | - |
| Radiation Injury Severity Classification19 | Drill | - | - | 95 |
| SALT54 | Drill | 10 | 6 | 83 |
| SALT53 | Drill | 4 | 13 | 79 |
| START22 | Drill | - | - | 70 |
| START22 | Drill | - | - | 62** |
| mSTART55 | Drill | 3 | 5 | - |
| TAS Triage method56 | Drill | 0 | 0 | 100 |
ACS=American College of Surgeons; SALT=Sort, Assess, Life-saving Interventions, Treatment/Support; Simple Triage and Rapid Treatment (START); mSTART=modified Simple Triage and Rapid Treatment; TAS=Interdisciplinary Emergency Service Cooperation Course; CBRN=Chemical/Biological/Radiological/Nuclear.
Rates moderately injured patients are reported. Under-triage rate for critical patients was 1% and for severely injured patients was 14%.
Accuracy of triage when clinical status was manipulated for 47 patients.
The seven studies that used drills to evaluate triage systems reported higher rates of accuracy than studies examining the performance of these systems in actual MCEs. Two systems associated with higher levels of performance examined triage during chemical, biological, radiological or nuclear events18 or radiological events alone.19 However, only one of these systems was developed using data from patients experiencing acute radiation syndrome; the other was based on expert opinion. Four studies, including two that evaluated the accuracy of the Sort, Assess, Life-saving interventions, Treatment/Support (SALT) triage system, were immediately preceded by a formal training program, so it is unlikely that their results will accurately predict the performance of each system during an actual MCE.
The methodological shortcomings of drills may help to explain why several studies have found that field triage systems often face challenges when implemented in practice. For example, in a commuter rail incident, use of another well-known field triage tool, Simple Triage and Rapid Treatment (START), resulted in misallocation of patients between trauma centers and community hospitals due to provider confusion about the meaning of each triage category.21 In addition, one exercise found that the START triage system is not sensitive to serious non-trauma conditions, such as a myocardial infarction or an asthma attack, and may therefore under-triage victims with these conditions.22
Non-implementation Studies Involving Triage Systems.
Nine studies reported data from validation analyses, but did not formally test one or more triage systems. One study was a systematic review comprising 11 articles on 8 triage systems.23 Only one of the 11 studies used data collected from an actual MCE in which START was used to triage patients of a transportation incident and resulted in an over-triage rate of 53%.24 The authors concluded that there is little evidence to favor one system over the others because of small sample sizes and low methodological quality of the studies, but the Sacco Triage Method (STM)25–27 was described as “promising” because it takes the available capacity at receiving hospitals into consideration.
Adding eight additional validation studies of triage systems did not change the overall conclusion from the prior systematic review. Because the vast majority of these studies did not include evidence on how these triage systems performed under real or realistically simulated conditions, we judged the collection of studies to have very limited applicability. For example, the STM requires relatively advanced health information technology and a reliable communication system to develop and transmit triage instructions to providers. The feasibility of implementing such a system in an MCE is unclear.
Crisis Standards of Care.
Five studies evaluated resource allocation strategies that might be implemented under crisis standards of care. Three examined “damage-control surgery”—an approach to initial surgical treatment that strictly focuses on initial stabilization, with definitive repair deferred to a later time. The fourth study examined the usefulness of modified ICU admission and discharge policies. The fifth and final study in this subcategory used computer simulation to model the potential impact of restricting care to only “essential interventions,” but did not specify them.28
Two of the damage-control surgery studies focused on orthopedic surgery, while the third examined trauma surgery more broadly. The first study reported that hospitals implementing “damage control” orthopedic surgery in the aftermath of an earthquake in Kashmir in 2008 expanded operating room capacity by 37 percent, with minimal impact on patient outcomes one year after the earthquake.29 The second found that under battlefield conditions, early use of external fixation improves throughput but at the cost of a higher rate of complications, particularly surgical infections.30 The third study noted that use of damage control surgery boosted surge capacity in the hospitals that received a sudden influx of complex trauma victims from the 2005 London transit bombings.31
The study that focused on ICU admission and discharge policies described the experience of the Israeli Defense Force field hospital, which cared for numerous victims of the 2010 Haiti earthquake.32 Faced with extraordinary demand, the hospital prioritized its ICU beds for patients who could be stabilized within 24 hours, and adopted a policy of accelerated discharge from intensive care. Although the authors concluded that these policies enabled them to treat a substantially larger number of victims than would otherwise have been possible, they did not systematically assess how the policies affected patient outcomes.
Limitations
To accommodate the vast and heterogeneous body of literature on this topic, we were obliged to make several methodological trade-offs. First, as the objective of our study was to conduct the first systematic review on the most effective resource management and allocation strategies during MCEs, we were unable to specify more precise research questions. For example, while we might have included only those studies that used a narrow set of outcome measures, such as survival, we erred on the side of being more inclusive. Second, because we were asked to identify resource allocation strategies across the full spectrum of preparedness and response options, we used a broad set of search terms to scan the literature. It is possible that our approach did not identify every important strategy or every key study for the strategies included in the review, because they were not specified as formal search terms. Third, in recognition that the evidence was likely to be sparse in many areas, we elected not to use exclusion criteria relating to study type. As a result, two existing systematic reviews were included in the review. Fourth, to accommodate a broad range of study types, we developed a quality assessment scale. While we did not calculate the inter-rater reliability of quality scores, the incidence of discrepant scores that required reconciliation between reviewers was frequent enough to suggest that the scale could be further refined. The scale should also undergo validity testing. Fourth, although the scope of our review was broad, it did not address every aspect of the management of MCEs, such as detailed clinical treatment and the technical considerations involved in inter-facility transport of critically ill and injured patients. Finally, although we did not conduct a formal assessment of publication bias, the majority of studies we found reported positive findings, suggesting that publication bias may be a factor
Discussion
In 2009, the IOM Committee on Guidance for Establishing Standards of Care for Use in Disaster Situations published a Letter Report recommending that healthcare providers, organizations, government officials, and the public approach the challenge of allocating scarce resources in a thoughtful and proactive way.5 Building on that report, the IOM recently described the core functions of stakeholders engaged in preparedness and response to MCEs, and enumerated specific tasks to help ensure that each stakeholder successfully fulfills these core functions.33 To complement the IOM’s work, we undertook this systematic review to compile, for the first time, the best available evidence on strategies to manage and allocate scarce medical resources during MCEs. Our hope was that the resulting evidence base might be sufficient to improve existing disaster response plans and more closely align them within the IOM’s disaster response framework.5,33
The need for better evidence is clear. It is only a matter of time before the United States will experience another natural or man-made disaster, a pandemic, or a terrorist attack that outstrips the capacity of our healthcare system to respond. When it occurs, healthcare workers and the policymakers that support them will be forced to make difficult decisions under highly demanding and generally quite public circumstances. Because resource allocation decisions are fraught with clinical, legal, and ethical implications, they should be grounded in rigorous evidence.
Unfortunately, our review found limited evidence to help providers and policymakers make such decisions. Within all but a few categories, individual strategies were evaluated by no more than three studies. Most of the studies we reviewed were prone to at least a moderate level of bias, and many had serious methodological flaws. Most relied on process measures (such as patient throughput) to assess their effectiveness rather than the intervention’s impact on patient health. The few that did report outcomes generally did so over a very short timeframe. Only one-third of the studies that met our generous inclusion criteria used data from actual MCEs. This is problematic, because simulations and drills may not adequately replicate the physical conditions and emotional stress of responding to an actual disaster. In all but two areas, the evidence was insufficient to draw conclusions about the effectiveness of specific resource management or allocation strategies.
By their nature, MCEs are both uncommon and unpredictable. Conducting health services research in such a context presents extraordinary challenges. The rarity of MCEs necessitates use of study designs—such as computer simulations, drills, and quasi-experimental studies involving actual MCEs, all of which are commonly regarded as producing inferior evidence to prospective, randomized trials. Computer simulations and staged drills can accommodate the design features of experiments, such as prospective recruitment of participants and random allocation of strategies, but they raise significant concerns about fidelity and validity. Consensus is urgently needed to establish acceptable methodological and evidentiary standards for future research in disaster preparedness and response, particularly regarding studies that use drills, computer simulations, and prospective evaluation of strategies implemented during an actual MCE. For example, experts might consider process measures sufficient to evaluate a field triage system, but outcome measures should be collected to assess the impact of an accelerated discharge policy.
Given the practical and ethical challenges of conducting prospective studies during MCEs, federal agencies should proactively work with experts in the field to create “research preparedness” – the capacity to rapidly generate useful empirical observations and conduct urgently-needed studies during unfolding MCEs.34 Useful steps might include a standardized, “Utstein style” approach to documenting essential information about the immediate medical response to disasters and large scale acts of terrorism,35 a more standardized approach to the selection of comparison groups, a thoughtful approach to the ethics of disaster research, including the potential for pre-approved protocols sanctioned by national institutional review boards,36 and contingent grant awards to provide the necessary funding required to immediately deploy a research team to a future MCE. Such innovations could quickly build a reasonably rigorous evidence base to inform policy and practice.
Even if a research infrastructure can be established, one vexing question remains: How much evidence is sufficient to support conclusions about the effectiveness of a particular resource management or allocation strategy? For example, one high-quality study included in the review—not summarized above—reported the results of a policy restricting ambulatory and inpatient care of non-urgent cases among 32 hospitals in the greater Toronto area during the 2003 SARS epidemic.37 Can a single study, no matter how compelling, constitute sufficient evidence to support conclusions about the value of a particular policy? In the absence of consensus evidence hierarchies or other rubrics specific to MCEs, providers and policymakers may interpret evidence differently and therefore reach different conclusions. Developing evidentiary standards through consensus among relevant experts could promote swift adoption of effective strategies into disaster planning.
Given the near certainty that large scale MCEs will continue to occur, and the high cost and relative scarcity of healthcare services on a typical day, it is deeply concerning how little high-quality evidence is available to help policymakers, healthcare providers, and the public determine the best course of action during MCEs. Although we identified findings that support the utility of a few interventions, the overall body of evidence is far from definitive. Because MCEs do not lend themselves to gold-standard randomized controlled trials, non-experimental study designs must be employed. However, the absence of methodological and evidentiary standards, the challenges of conducting ethical research during an MCE, and competing funding priorities at the federal, state, and local levels, create formidable barriers to advancing the research in this area. Nevertheless, we believe our findings can serve as a key starting point for disaster researchers, first responders, and program evaluators across the nation.
In summary, the current evidence base appears inadequate to inform providers and policymakers about the most effective strategies for managing or allocating scarce resources during MCEs. Very limited evidence suggests that Points of Dispensing (PODs) can be used to efficiently distribute biological countermeasures following a bioterror attack or influenza pandemic, and different models may vary in their effectiveness. Some evidence also suggests that commonly used field triage systems do not perform consistently during actual MCEs. Few strategies were evaluated in more than two studies, and heterogeneity in outcome measures and context prevented quantitative synthesis of results. Improving the evidence base will require a diverse group of policy makers, funders, and non-governmental experts to come together to craft a well-organized and coordinated program of applied research38 that adheres to appropriate ethical and methodological standards.
Supplementary Material
Acknowledgments
This study was conducted by the Southern California Evidence-based Practice Center under Contract No. 290–2007-10062-I from the Agency for Healthcare Research and Quality, with funding support from the U.S. Department of Health and Human Services’ Office of the Assistant Secretary for Preparedness and Response (ASPR). Representatives of ASPR developed the research questions and contributed to the final manuscript.
References
- 1.Health Systems Research Inc. Altered Standards of Care in Mass Casualty Events, AHRQ Publication No. 05–0043. Rockville, MD: Agency for Healthcare Research and Quality;2005. AHRQ Publication No. 05–0043. [Google Scholar]
- 2.National Center for Injury Prevention and Control. In a Moment’s Notice Surge Capacity for Terrorist Bombings. Atlanta (GA): Centers for Disease Control and Prevention; 2007. [Google Scholar]
- 3.Kaji AH, Koenig KL, Lewis RJ. Current hospital disaster preparedness. Jama-Journal of the American Medical Association. November 2007;298(18):2188–2190. [DOI] [PubMed] [Google Scholar]
- 4.Salinsky E Strong as the Weakest Link: Medical Response to a Catastrophic Event. National Health Policy Forum Background Paper – No. 65. August 8, 2008. [Google Scholar]
- 5.Altevogt BM, Institute of Medicine (U.S.) Committee on Guidance for Establishing Standards of Care for Use in Disaster Situations Guidance for establishing crisis standards of care for use in disaster situations a letter report / [electronic resource] Washington, DC: National Academies Press; 2009. [PubMed] [Google Scholar]
- 6.Timbie JW, Ringel JS, Fox DS, et al. Allocation of Scarce Resources During Mass Casualty Events. Rockville, MD: Agency for Healthcare Research and Quality;2012. [PMC free article] [PubMed] [Google Scholar]
- 7.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. August 18 2009;151(4):264–269, W264. [DOI] [PubMed] [Google Scholar]
- 8.NREPP, SAMHSA’s National Registry of Evidence-based Programs and Practices. Quality of Research available at: http://nrepp.samhsa.gov/ReviewQOR.aspx.
- 9.Mays N, Pope C. Qualitative research in health care. Assessing quality in qualitative research. BMJ January 1 2000;320(7226):50–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lincoln YS, Guba EG. Naturalistic Inquiry. Newbury Park, CA: Sage Publications; 1985. [Google Scholar]
- 11.Shea BJ, Grimshaw JM, Wells GA, et al. Development of AMSTAR: a measurement tool to assess the methodological quality of systematic reviews. BMC Med Res Methodol. 2007;7:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Owens DK, Lohr KN, Atkins D, et al. AHRQ series paper 5: grading the strength of a body of evidence when comparing medical interventions--agency for healthcare research and quality and the effective health-care program. J Clin Epidemiol. May 2010;63(5):513–523. [DOI] [PubMed] [Google Scholar]
- 13.Ablah E, Scanlon E, Konda K, Tinius A, Gebbie KM. A large-scale points-of-dispensing exercise for first responders and first receivers in Nassau County, New York. Biosecur Bioterror. March 2010;8(1):25–35. [DOI] [PubMed] [Google Scholar]
- 14.Koh HK, Elqura LJ, Judge CM, et al. Implementing the cities readiness initiative: lessons learned from Boston. Disaster Med Public Health Prep. March 2008;2(1):40–49. [DOI] [PubMed] [Google Scholar]
- 15.Lee EK, Maheshwary S, Mason J, Glisson W. Large-scale dispensing for emergency response to bioterrorism and infectious-disease outbreak. Interfaces. Nov-Dec 2006;36(6):591–607. [Google Scholar]
- 16.Hupert N, Xiong W, King K, et al. Uncertainty and operational considerations in mass prophylaxis workforce planning. Disaster Medicine and Public Health Preparedness. 2009;SO- <VO> 3(Suppl. 2):S121–S131. [DOI] [PubMed] [Google Scholar]
- 17.Erwin PC, Sheeler L, Lott JM. A shot in the rear, not a shot in the dark: application of a mass clinic framework in a public health emergency. Public Health Reports. 2009;SO- <VO> 124(2):212–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cone DC, MacMillan DS, Parwani V, Van Gelder C. Pilot test of a proposed chemical/biological/radiation/nuclear-capable mass casualty triage system. Prehosp Emerg Care. Apr-Jun 2008;12(2):236–240. [DOI] [PubMed] [Google Scholar]
- 19.Kuniak M, Azizova T, Day R, et al. The Radiation Injury Severity Classification system: an early injury assessment tool for the frontline health-care provider. Br J Radiol. March 2008;81(963):232–243. [DOI] [PubMed] [Google Scholar]
- 20.Rodriguez-Noriega E, Gonzalez-Diaz E, Morfin-Otero R, et al. Hospital Triage System for Adult Patients Using an Influenza-Like Illness Scoring System during the 2009 Pandemic-Mexico. PLoS One. May 2010;5(5). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zoraster RM, Chidester C, Koenig W. Field triage and patient maldistribution in a mass-casualty incident. Prehosp Disaster Med. May-Jun 2007;22(3):224–229. [DOI] [PubMed] [Google Scholar]
- 22.Schenker JD, Goldstein S, Braun J, et al. Triage accuracy at a multiple casualty incident disaster drill: The Emergency Medical Service, Fire Department of New York City experience. Journal of Burn Care and Research. 2006;27(5):570–575. [DOI] [PubMed] [Google Scholar]
- 23.Kilner TM, Brace SJ, Cooke MW, Stallard N, Bleetman A, Perkins GD. In ‘big bang’ major incidents do triage tools accurately predict clinical priority?: A systematic review of the literature. Injury. December 2 2010. [DOI] [PubMed] [Google Scholar]
- 24.Kahn CA, Schultz CH, Miller KT, Anderson CL. Does START triage work? An outcomes assessment after a disaster. Annals of Emergency Medicine. September 2009;54(3):424–430, 430 e421. [DOI] [PubMed] [Google Scholar]
- 25.Navin DM, Sacco WJ, McGili G. Application of a new resource-constrained Triage method to military-age victims. Military Medicine. 2009;174(12):1247–1255. [DOI] [PubMed] [Google Scholar]
- 26.Sacco WJ, Navin DM, Fiedler KE, Waddell RK 2nd, Long WB, Buckman RF Jr. Precise formulation and evidence-based application of resource-constrained triage. Acad Emerg Med. August 2005;12(8):759–770. [DOI] [PubMed] [Google Scholar]
- 27.Sacco WJ, Navin DM, Waddell RK 2nd, Fiedler KE, Long WB, Buckman RF Jr. A new resource-constrained triage method applied to victims of penetrating injury. J Trauma. August 2007;63(2):316–325. [DOI] [PubMed] [Google Scholar]
- 28.Kanter RK. Strategies to improve pediatric disaster surge response: potential mortality reduction and tradeoffs. Crit Care Med. December 2007;35(12):2837–2842. [DOI] [PubMed] [Google Scholar]
- 29.Dhar SA, Bhat MI, Mustafa A, et al. ‘Damage control orthopaedics’ in patients with delayed referral to a tertiary care center: experience from a place where Composite Trauma Centers do not exist. J Trauma Manag Outcomes. 2008;2:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Labeeu F, Pasuch M, Toussaint P, Van Erps S. External fixation in war traumatology: report from the Rwandese war (October 1, 1990 to August 1, 1993). J Trauma. March 1996;40(3 Suppl):S223–227. [DOI] [PubMed] [Google Scholar]
- 31.Aylwin CJ, Konig TC, Brennan NW, et al. Reduction in critical mortality in urban mass casualty incidents: analysis of triage, surge, and resource use after the London bombings on July 7, 2005. Lancet. December 23 2006;368(9554):2219–2225. [DOI] [PubMed] [Google Scholar]
- 32.Merin O, Ash N, Levy G, Schwaber MJ, Kreiss Y. The Israeli field hospital in Haiti--ethical dilemmas in early disaster response. N Engl J Med. March 18 2010;362(11):e38. [DOI] [PubMed] [Google Scholar]
- 33.Hanfling DG, Altevogt B, Viswanathan K, Gostin L, Committee on Guidance for Establishing Crisis Standards of Care for Use in Disaster Situations; Institute of Medicine, eds Crisis Standards of Care: A Systems Framework for Catastrophic Disaster Response. Washington, DC: National Academies Press; 2012. [PubMed] [Google Scholar]
- 34.Lurie N A Vision for Science Response. Paper presented at: Dynamics of Preparedness: A Public Health Systems Conference2010; University of Pittsburgh, Pittsburgh, PA. [Google Scholar]
- 35.Debacker M, Hubloue I, Dhondt E, et al. Utstein-style template for uniform data reporting of acute medical response in disasters. PLoS Curr. 2012;4:e4f6cf3e8df15a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sumathipala A, Jafarey A, de Castro L, et al. The Draft Statement/Guidelines for Disaster Research. 2011; http://globalhealthtrials.tghn.org/articles/draft-statementguidelines-disaster-research/. [Google Scholar]
- 37.Loeb M, Dafoe N, Mahony J, et al. Surgical mask vs N95 respirator for preventing influenza among health care workers: a randomized trial. JAMA, Journal of the American Medical Association. 2009;SO- <VO> 302(17):1865–1871. [DOI] [PubMed] [Google Scholar]
- 38.Shelton SR, Connor K, Uscher-Pines L, Pillemer FM, Mullikin JM, Kellermann AL. Bioterrorism and biological threats dominate federal health security research; other priorities get scant attention. Health Aff (Millwood). December 2012;31(12):2755–2763. [DOI] [PubMed] [Google Scholar]
- 39.Arora N, Raghu TS, Vinze A. Resource allocation for demand surge mitigation during disaster response. Decision Support Systems. December 2010;50(1):304–315. [Google Scholar]
- 40.McCaw JM, Wood JG, McCaw CT, McVernon J. Impact of emerging antiviral drug resistance on influenza containment and spread: influence of subclinical infection and strategic use of a stockpile containing one or two drugs. PLoS One. 2008(June):e2362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wein LM, Craft DL, Kaplan EH. Emergency response to an anthrax attack. Proc Natl Acad Sci U S A. April 1 2003;100(7):4346–4351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bravata DM, Zaric GS, Holty JEC, et al. Reducing mortality from anthrax bioterrorism: Strategies for stockpiling and dispensing medical and pharmaceutical supplies. Biosecurity and Bioterrorism-Biodefense Strategy Practice and Science. 2006;4(3):244–262. [DOI] [PubMed] [Google Scholar]
- 43.Zaric GS, Bravata DM, Cleophas Holty JE, McDonald KM, Owens DK, Brandeau ML. Modeling the logistics of response to anthrax bioterrorism. Medical Decision Making. 2008;28(3):332–350. [DOI] [PubMed] [Google Scholar]
- 44.Glasser J, Taneri D, Feng ZL, et al. Evaluation of Targeted Influenza Vaccination Strategies via Population Modeling. PLoS One. September 2010;5(9). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.McVernon J, McCaw JM, Nolan TM. Modelling strategic use of the national antiviral stockpile during the CONTAIN and SUSTAIN phases of an Australian pandemic influenza response. Australian and New Zealand Journal of Public Health. April 2010;34(2):113–119. [DOI] [PubMed] [Google Scholar]
- 46.Medlock J, Galvani AP. Optimizing influenza vaccine distribution. Science (Washington). 2009;SO- <VO> 325(5948):1705–1708. [DOI] [PubMed] [Google Scholar]
- 47.Zenihana T, Ishikawa H. Effectiveness assessment of countermeasures against bioterrorist smallpox attacks in Japan using an individual-based model. Environmental Health and Preventive Medicine. 2010;15(2):84–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Cahill BP, Collins RD, Jurko RC, et al. Collaborative risk-based preparedness for pandemic influenza in Southeastern Virginia. 2008. Systems and Information Engineering Design Symposium. 2008:323–328. [Google Scholar]
- 49.Schull MJ, Stukel TA, Vermeulen MJ, et al. Effect of widespread restrictions on the use of hospital services during an outbreak of severe acute respiratory syndrome. CMAJ. June 19 2007;176(13):1827–1832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Savoia E, Biddinger PD, Fox P, Levin DE, Stone L, Stoto MA. Impact of tabletop exercises on participants’ knowledge of and confidence in legal authorities for infectious disease emergencies. Disaster Med Public Health Prep. June 2009;3(2):104–110. [DOI] [PubMed] [Google Scholar]
- 51.Adini B, Peleg K, Cohen R, Laor D. A national system for disseminating information on victims during mass casualty incidents. Disasters. April 2010;34(2):542–551. [DOI] [PubMed] [Google Scholar]
- 52.Cohen M, Kluger Y, Klausner J, Avital S, Shafir R. Recommended guidelines for optimal design of a plastic surgery service during mass casualty events. J Trauma. November 1998;45(5):960–968. [DOI] [PubMed] [Google Scholar]
- 53.Cone DC, Serra J, Burns K, MacMillan DS, Kurland L, Van Gelder C. Pilot test of the SALT mass casualty triage system. Prehosp Emerg Care. Oct-Dec 2009;13(4):536–540. [DOI] [PubMed] [Google Scholar]
- 54.Lerner EB, Schwartz RB, Coule PL, Pirrallo RG. Use of SALT triage in a simulated mass-casualty incident. Prehosp Emerg Care. Jan-Mar 2010;14(1):21–25. [DOI] [PubMed] [Google Scholar]
- 55.Gutsch W, Huppertz T, Zollner C, et al. Results of the mSTaRT triage from mass casualty incident exercises. Initiale sichtung durch rettungsassistenten: Ergebnisse bei übungen zum massenanfall von verletzten. 2006;9(4):384–388. [Google Scholar]
- 56.Rehn M, Andersen JE, Vigerust T, Kruger AJ, Lossius HM. A concept for major incident triage: full-scaled simulation feasibility study. BMC Emerg Med. 2010;10:17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Cryer HG, Hiatt JR, Eckstein M, et al. Improved trauma system multicasualty incident response: Comparison of two train crash disasters. Journal of Trauma - Injury, Infection and Critical Care. 2010;68(4):783–788. [DOI] [PubMed] [Google Scholar]
- 58.Janousek JT, Jackson DE, De Lorenzo RA, Coppola M. Mass casualty triage knowledge of military medical personnel. Mil Med. May 1999;164(5):332–335. [PubMed] [Google Scholar]
- 59.Adeniji KA, Cusack R. The Simple Triage Scoring System (STSS) successfully predicts mortality and critical care resource utilization in H1N1 pandemic flu: A retrospective analysis. Critical Care. 2011;15(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Casagrande R, Wills N, Kramer E, et al. Using the Model of Resource and Time-Based Triage (MORTT) to Guide Scarce Resource Allocation in the Aftermath of a Nuclear Detonation. Disaster Medicine and Public Health Preparedness. March 2011;5:S98–S110. [DOI] [PubMed] [Google Scholar]
- 61.Cancio LC, Wade CE, West SA, Holcomb JB. Prediction of mortality and of the need for massive transfusion in casualties arriving at combat support hospitals in Iraq. The Journal of trauma. 2008;64(2 Suppl):S51–55; discussion S55–56. [DOI] [PubMed] [Google Scholar]
- 62.Guest T, Tantam G, Donlin N, Tantam K, McMillan H, Tillyard A. An observational cohort study of triage for critical care provision during pandemic influenza: ‘clipboard physicians’ or ‘evidenced based medicine’? Anaesthesia. November 2009;64(11):1199–1206. [DOI] [PubMed] [Google Scholar]
- 63.Nie H, Tang SY, Lau WB, et al. Triage during the week of the Sichuan earthquake: a review of utilized patient triage, care, and disposition procedures. Injury. July 2010;41(7):866–871. [DOI] [PubMed] [Google Scholar]
- 64.Beyersdorf SR, Nania JN, Luna GK. Community medical response to the Fairchild mass casualty event. Am J Surg. May 1996;171(5):467–470. [DOI] [PubMed] [Google Scholar]
- 65.Hirshberg A, Frykberg ER, Mattox KL, Stein M. Triage and trauma workload in mass casualty: a computer model. J Trauma. November 2010;69(5):1074–1081; discussion 1081–1072. [DOI] [PubMed] [Google Scholar]
- 66.Romm H, Wilkins RC, Coleman CN, et al. Biological Dosimetry by the Triage Dicentric Chromosome Assay: Potential Implications for Treatment of Acute Radiation Syndrome in Radiological Mass Casualties. Radiat Res. January 4 2011. [DOI] [PubMed] [Google Scholar]
- 67.Gao T, Massey T, Selavo L, et al. The Advanced Health and Disaster Aid Network: A Light-Weight Wireless Medical System for Triage. Ieee Transactions on Biomedical Circuits and Systems. September 2007;1(3):203–216. [DOI] [PubMed] [Google Scholar]
- 68.Epley EE, Stewart RM, Love P, et al. A regional medical operations center improves disaster response and inter-hospital trauma transfers. Am J Surg. December 2006;192(6):853–859. [DOI] [PubMed] [Google Scholar]
- 69.Leiba A, Halpern P, Priel IE, et al. A Terrorist Suicide Bombing at a Nightclub in Tel Aviv: Analyzing Response to a Nighttime, Weekend, Multi-Casualty Incident. Journal of Emergency Nursing. 2006;32(4):294–298. [DOI] [PubMed] [Google Scholar]
- 70.Raiter Y, Farfel A, Lehavi O, et al. Mass casualty incident management, triage, injury distribution of casualties and rate of arrival of casualties at the hospitals: lessons from a suicide bomber attack in downtown Tel Aviv. Emerg Med J. April 2008;25(4):225–229. [DOI] [PubMed] [Google Scholar]
- 71.Xiong W, Bair A, Sandrock C, Wang S, Siddiqui J, Hupert N. Implementing Telemedicine in Medical Emergency Response: Concept of Operation for a Regional Telemedicine Hub. J Med Syst. December 14 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Simon R, Teperman S. The World Trade Center attack. Lessons for disaster management. Crit Care. December 2001;5(6):318–320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Wolf S, Partenheimer A, Voigt C, Kunze R, Adams HA, Lill H. [Primary care hospital for a mass disaster MANV IV. Experience from a mock disaster exercise]. Unfallchirurg. June 2009;112(6):565–574. [DOI] [PubMed] [Google Scholar]
- 74.Beck-Razi N, Fischer D, Michaelson M, Engel A, Gaitini D. The utility of focused assessment with sonography for trauma as a triage tool in multiple-casualty incidents during the second Lebanon war. Journal of Ultrasound in Medicine. 2007;26(9):1149–1156. [DOI] [PubMed] [Google Scholar]
- 75.Sarkisian AE, Khondkarian RA, Amirbekian NM, Bagdasarian NB, Khojayan RL, Oganesian YT. Sonographic screening of mass casualties for abdominal and renal injuries following the 1988 Armenian earthquake. J Trauma. February 1991;31(2):247–250. [PubMed] [Google Scholar]
- 76.Korner M, Krotz M, Kanz KG, Pfeifer KJ, Reiser M, Linsenmaier U. Development of an accelerated MSCT protocol (Triage MSCT) for mass casualty incidents: comparison to MSCT for single-trauma patients. Emerg Radiol. July 2006;12(5):203–209. [DOI] [PubMed] [Google Scholar]
- 77.Korner M, Geyer LL, Wirth S, Reiser MF, Linsenmaier U. 64-MDCT in Mass Casualty Incidents: Volume Image Reading Boosts Radiological Workflow. American Journal of Roentgenology. September 2011;197(3):W399–W404. [DOI] [PubMed] [Google Scholar]
- 78.Gunal AI, Celiker H, Dogukan A, et al. Early and vigorous fluid resuscitation prevents acute renal failure in the crush victims of catastrophic earthquakes. J Am Soc Nephrol. July 2004;15(7):1862–1867. [DOI] [PubMed] [Google Scholar]
- 79.Vardi A, Berkenstadt H, Levin I, Bentencur A, Ziv A. Intraosseous vascular access in the treatment of chemical warfare casualties assessed by advanced simulation: proposed alteration of treatment protocol. Anesth Analg. June 2004;98(6):1753–1758, table of contents. [DOI] [PubMed] [Google Scholar]
- 80.Satterthwaite PS, Atkinson CJ. Using ‘reverse triage’ to create hospital surge capacity: Royal Darwin Hospital’s response to the Ashmore Reef disaster. Emerg Med J. October 28 2010. [DOI] [PubMed] [Google Scholar]
- 81.Van Cleve WC, Hagan P, Lozano P, Mangione-Smith R. Investigating a pediatric hospital’s response to an inpatient census surge during the 2009 H1N1 influenza pandemic. Joint Commission Journal on Quality and Patient Safety. 2011;37(8):376–382. [DOI] [PubMed] [Google Scholar]
- 82.Scarfone RJ, Coffin S, Fieldston ES, Falkowski G, Cooney MG, Grenfell S. Hospital-based pandemic influenza preparedness and response: strategies to increase surge capacity. Pediatr Emerg Care. June 2011;27(6):565–572. [DOI] [PubMed] [Google Scholar]
- 83.Hsu EB, Jenckes MW, Catlett CL, et al. Training to hospital staff to respond to a mass casualty incident. Evid Rep Technol Assess (Summ). April 2004(95):1–3. [PMC free article] [PubMed] [Google Scholar]
- 84.Jarvis S, de Freitas S. Evaluation of an Immersive Learning Programme to Support Triage Training In-game Feedback and its effect on Learning Transfer. Proceedings of the Ieee Virtual Worlds for Serious Applications. 2009:117–122. [Google Scholar]
- 85.Andreatta PB, Maslowski E, Petty S, et al. Virtual reality triage training provides a viable solution for disaster-preparedness. Academic Emergency Medicine. 2010;SO- <VO> 17(8). [DOI] [PubMed] [Google Scholar]
- 86.Vincent DS, Sherstyuk A, Burgess L, Connolly KK. Teaching mass casualty triage skills using immersive three-dimensional virtual reality. Acad Emerg Med. November 2008;15(11):1160–1165. [DOI] [PubMed] [Google Scholar]
- 87.Vincent DS, Burgess L, Berg BW, Connolly KK. Teaching mass casualty triage skills using iterative multimanikin simulations. Prehosp Emerg Care. Apr-Jun 2009;13(2):241–246. [DOI] [PubMed] [Google Scholar]
- 88.Sanddal TL, Loyacono T, Sanddal ND. Effect of JumpSTART training on immediate and short-term pediatric triage performance. Pediatric Emergency Care. 2004;20(11):749–753. [DOI] [PubMed] [Google Scholar]
- 89.Einav S, Schecter WP, Matot I, et al. Case managers in mass casualty incidents. Ann Surg. March 2009;249(3):496–501. [DOI] [PubMed] [Google Scholar]
- 90.Amlot R, Larner J, Matar H, et al. Comparative analysis of showering protocols for mass-casualty decontamination. Prehosp Disaster Med. Sep-Oct 2010;25(5):435–439. [DOI] [PubMed] [Google Scholar]
- 91.Eastman AL, Rinnert KJ, Nemeth IR, Fowler RL, Minei JP. Alternate site surge capacity in times of public health disaster maintains trauma center and emergency department integrity: Hurricane Katrina. J Trauma. August 2007;63(2):253–257. [DOI] [PubMed] [Google Scholar]
- 92.Blackwell T, Bosse M. Use of an innovative design mobile hospital in the medical response to Hurricane Katrina. Ann Emerg Med. May 2007;49(5):580–588. [DOI] [PubMed] [Google Scholar]
- 93.Corvino TF, Nahata MC, Angelos MG, et al. Availability, stability, and sterility of pralidoxime for mass casualty use. Ann Emerg Med. March 2006;47(3):272–277. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.