Summary
Background
For thoracolumbar burst fractures with spinal canal compromise but no neurological deficit, is it necessary to perform additional laminectomy decompression after the currently accepted posterior pedicle-screw internal fixation?
Methods
Patients were divided into two groups: decompression group (Group A) and nondecompression group (Group B). A retrospective analysis of the posterior vertebral body height of the fractured vertebral body, the ratio of the volume of the spinal canal, and the change of the Cobb angle, relative to the corresponding preoperative values, was conducted to analyse the reasons for choosing different surgical methods.
Results
Compared the intraoperative findings after fixation with the preoperative data, in Group A, the posterior vertebral body height of the fractured vertebral body was not significantly restored, the volume ratio of the spinal canal was not significantly improved, and the Cobb angle was not significantly reduced (p > 0.05). In comparison, in Group B, the posterior vertebral body height of the fractured vertebral body was significantly restored, the volume ratio of spinal canal was significantly increased, and the Cobb angle was significantly reduced (p < 0.001).
Conclusion
For patients with thoracolumbar burst fractures with spinal canal compromise but no neurological deficit, if when the posterior intraoperative fixation is performed, the spinal canal fracture is partially recovered, the posterior vertebral body height of the injured vertebrae is significantly restored, the spinal canal volume ratio is significantly increased, and the large kyphosis is corrected, then the indirect decompression without the posterior laminectomy can be performed.
The translational potential of this article
This study contributes to offer treatment consideration for patients with thoracolumbar burst fracture without neurological symptoms.
Keywords: No neurological deficits, Spinal canal compromise, Spinal canal volume, Surgical approach, Thoracolumbar burst fracture, Vertebral body height
Introduction
Thoracolumbar is a common site for spinal fractures. Among all, the thoracolumbar burst fractures are unstable fractures caused by high-energy traumas with vertical compression, often involving the anterior or posterior column [[1], [2], [3]]. Burst thoracolumbar fractures are prone to cause spinal canal compromise and even lead to spinal cord or nerve damage. For thoracolumbar burst fractures with spinal canal compromise and neurological symptoms, timely decompression and internal fixation should be performed to restore the vertebral body height and spinal canal volume, correct kyphosis, and reconstruct spinal stability as early as possible [4,5]. Posterior decompression and pedicle-screw internal fixation have been widely used in this type of patients because of the simple operation and small trauma, and the clinical efficacy has been widely accepted by clinicians [6].
However, for patients with thoracolumbar burst fracture with no neurological symptoms, in addition to posterior pedicle-screw internal fixation, should decompression be used at the same time? What are the postoperative clinical efficacies for different surgical methods? There has been a long-standing controversy [[7], [8], [9]]. In this study, the Department of Orthopedics of the First Affiliated Hospital of Suzhou University offered different surgical treatments for patients from January 2013 to January 2015 and studied their clinical efficacies on these patients. The study is expected to provide some guidance for the treatment of such patients in the future.
Methods
General information
The clinical study was approved by the Ethics Committee of the first affiliated hospital of Soochow University, and written informed consents were obtained from all participants. From January 2013 to January 2015, there were 99 middle-aged patients with a diagnosis of thoracolumbar burst fractures who met the surgical indications, including 47 men and 52 women. The average age was 42.3 years old, and the fractured segment included 21 cases of T11, 28 cases of T12, 17 cases of L1, 19 cases of L2, and 14 cases of L3. Comprehensive preoperative examinations were conducted with X-ray, computed tomography (CT), and magnetic resonance imaging (MRI). According to the different surgical methods, whether the posterior pedicle internal fixation combined with laminectomy decompression or not, the patients were divided into two groups: decompression group (Group A) and nondecompression group (Group B).
The inclusion criteria were as follows: (1) CT and MRI confirmed fresh single thoracolumbar burst fracture, with no dislocation; (2) spinal canal compromise by bone with occupancy rates no more than 30%; (3) fracture type: AO classification of the A3 type, fresh fracture with no serious osteoporosis; (4) no spinal cord or nerve root injury before operation, with neurological function Grade E according to the American Spinal Injury Association international standards; and (5) follow-up time > 1 year and follow-up data are complete.
The exclusion criteria were as follows: (1) multisegment fractures and multiple fractures; (2) pathological fractures; (3) fractures with ankylosing spondylitis and intervertebral disc injuries; and (4) diseases with lower limb function and paraesthesia before the injury.
Observation parameters
Statistical analysis was performed on the imaging data of all enrolled patients. According to X-ray images and three-dimensional CT reconstructions, the posterior vertebral body height of the fractured vertebral body, the volume ratio of the spinal canal, and the Cobb angle were calculated before and during the internal fixation, as well as at postoperative follow-ups. The volume ratio of the spinal canal was measured at the axial position with the most significant compromise on CT and calculated based on Li/((La + Lb)/2), where Li is the narrowest midsagittal diameter of the spinal canal at the level of the fractured vertebra, and La and Lb are the midsagittal diameters of the spinal canal at one level above and below the fractured vertebra, respectively [9]. The lower limb motor function scores of the patients were recorded both preoperatively and in postoperative follow-ups according to the American Society of Spinal Injury motor score [10].
Treatments
For each patient, the patient's spine was strictly fixed before surgery, and the patient was scheduled to undergo surgery after the patient's vital signs were stable. Under general anaesthesia, the patient was placed in a prone position with the abdomen suspended. Following routine disinfection, a posterior median incision was made, centred at the injured vertebra, to expose the upper and lower lamina, as well as the articular processes and transverse processes of the vertebral spine. The pedicle needle insertion point was determined at the injured vertebrae and adjacent superior and inferior vertebrae, and the pedicle root was opened by the opener to drill a hole. The bottom and the periphery of the channel were probed, and the positioning needle was placed in the bone tissue. After an ideal positioning of the C-arm fluoroscopic system, the pedicle screw of an appropriate length was screwed in. Subsequently, a longitudinal connecting rod with the appropriate length and angle was selected. The pedicle screw and the connecting rod were installed and then axially expanded properly to restore the height of the vertebral body, and the nut was tightened using an appropriate angle with the connecting rod to correct the kyphosis. At this time, the X-ray and CT were retaken using the C-arm and O-arm systems. The posterior vertebral body height of the fractured vertebral body, the volume ratio of the spinal canal, and the Cobb angle was measured and calculated using the picture archiving and communication system and compared with the preoperative values. If the posterior vertebral body height of the fractured vertebral body was significantly restored, the volume ratio of the spinal canal was significantly improved, and the Cobb angle was significantly decreased, then the patient would be selected for the posterior pedicle-screw fixation procedure. If there was no obvious recovery of the posterior vertebral body height of the fractured vertebral body, significant improvement of the volume ratio of the spinal canal, or significantly decreased Cobb angle, laminectomy decompression would be added on top of the posterior pedicle internal fixation. If decompression was required, a bilateral laminotomy was used. The wound was rinsed, and after the bleeding fully stopped with a vacuum suction ball placed, the incision was sutured layer by layer. After intravenous infusion of antibiotics for 3 days and routine dressing changes, the drainage tube was removed 24–48 h after surgery and the suture was removed 14 days after surgery. The recovery of fractures and related parameters was observed using X-ray and CT at 1 month, 6 months, and 12 months after surgery.
Statistical methods
Statistical software statistic package for social science (SPSS), version 18.0, was used for data processing. For the measurement data, the mean value plus standard deviation form (mean ± SD) was used. For the quantitative data analysis and the comparison between the groups, the t test and χ2 test were performed, respectively. When p < 0.05, the difference was considered to be statistically significant.
Results
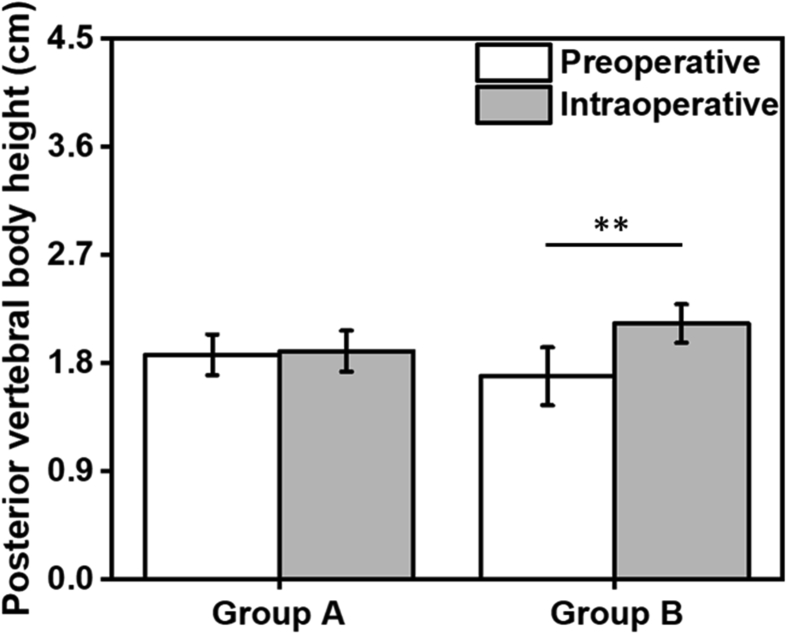
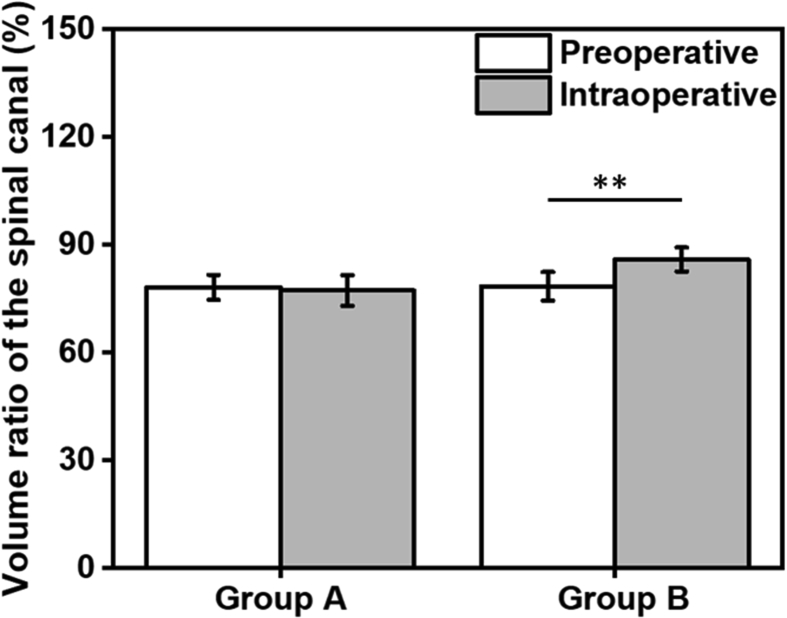
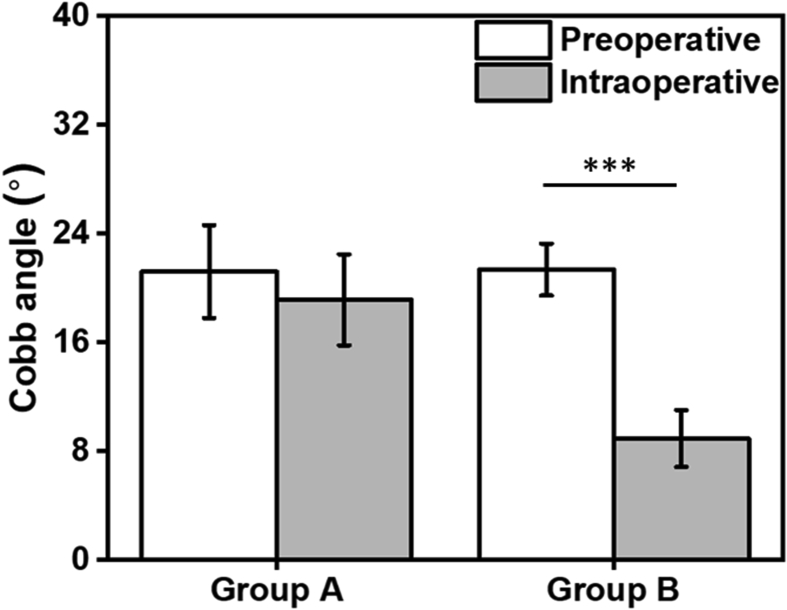
All patients in this study experienced no complications such as wound infection or internal fixation failure. And all patients had normal fracture healing, with no bone nonunion or delayed nerve injury. The basic data of the two groups of patients are shown in Table 1, including age, gender, and fracture type. The data of the two groups were comparable and showed no statistically significant difference in the fractured vertebral body. The intraoperative vertebral posterior height, the volume ratio of the spinal canal, and the Cobb angle were also compared with the preoperative data for the two groups of patients, as can be seen in Table 2. From Table 2 and Figure 1, Figure 2, Figure 3, it can be seen that, compared with the preoperative data, in Group A (decompression group), the posterior vertebral body height of the fractured vertebral body did not significantly recover, the volume ratio of the spinal canal did not significantly improve, and there was no significant decrease in the Cobb angle (p > 0.05); whereas in Group B (nondecompression group), the posterior margin of the vertebral body was significantly restored, the volume ratio of the spinal canal was significantly increased, and the Cobb angle was significantly decreased (p < 0.001). In the late follow-up, there were no significant changes in the posterior margin height, spinal canal volume ratio, Cobb angle, and American Society of Spinal Injury motor score parameters (see Table 3).
Table 1.
Basic preoperative information of patients for both decompression and nondecompression groups (mean ± SD).
| Description | Group A | Group B | p |
|---|---|---|---|
| Age (years) | 41.2 ± 5.96 | 43.06 ± 6.55 | 0.16 |
| Gender (male/female) | 22/25 | 25/27 | 0.78 |
| Type of fracture (A3.1/A3.2/A3.3) | 28/13/6 | 32/15/5 | 0.68 |
| Fractured vertebral body (T11/T12/L1/L2/L3) | 10/13/8/9/7 | 11/15/9/10/7 | 0.53 |
SD = standard deviation.
Table 2.
Preoperative and intraoperative parameter comparison for both groups (mean ± SD).
| Parameter | Group A (preoperative/intraoperative) | p | Group B (preoperative/intraoperative) | p |
|---|---|---|---|---|
| Posterior vertebral body height (cm) | 1.87 ± 0.17/1.90 ± 0.17 | 0.72 | 1.69 ± 0.24/2.13 ± 0.16 | <0.001 |
| Volume ratio of the spinal canal(%) | 78.18 ± 3.49/77.27 ± 4.27 | 0.59 | 78.45 ± 3.98/85.91 ± 3.33 | 0.0001 |
| Cobb angle(°) | 21.21 ± 3.42/19.14 ± 3.35 | 0.12 | 21.36 ± 1.91/8.93 ± 2.09 | <0.0001 |
SD = standard deviation.
Figure 1.
Comparison of preoperative and intraoperative posterior vertebral body heights of the fractured vertebral body. (**) indicates p < 0.001.
Figure 2.
Comparison of preoperative and intraoperative spinal canal volume ratio. (**) indicates p < 0.001.
Figure 3.
Comparison of preoperative and intraoperative Cobb angles. (***) indicates p < 0.0001.
Table 3.
Parameter changes during follow-up in each group (mean ± SD).
| Parameter | 1 month (Group A/Group B) | 6 month (Group A/Group B) | 12 month (Group A/Group B) |
|---|---|---|---|
| Posterior vertebral body height (cm) | 2.08 ± 0.21/2.17 ± 0.17 | 2.10 ± 0.19/2.15 ± 0.17 | 2.08 ± 0.18/2.14 ± 0.16 |
| Volume ratio of the spinal canal (%) | 88.64 ± 2.66/86.27 ± 3.74 | 89.09 ± 3.65/86.55 ± 3.53 | 88.91 ± 2.77/86.82 ± 3.06 |
| Cobb angle (°) | 7.36 ± 1.86/7.93 ± 1.64 | 7.21 ± 1.67/8.07 ± 1.69 | 7.43 ± 1.83/8.21 ± 1.67 |
| AMS | 72.25 ± 7.30/76.83 ± 9.53 | 79.67 ± 8.81/82.83 ± 11.75 | 82.58 ± 8.08/84.83 ± 10.24 |
AMS = American Society of Spinal Injury motor score; SD = standard deviation.
A typical case
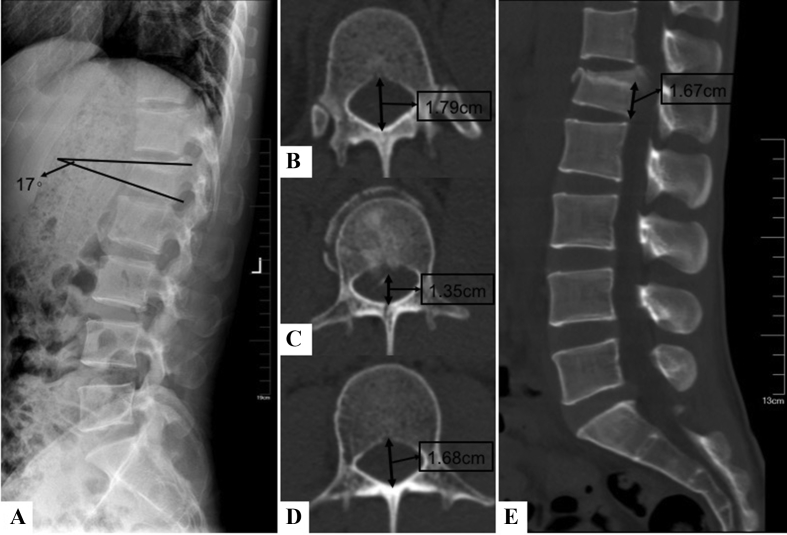
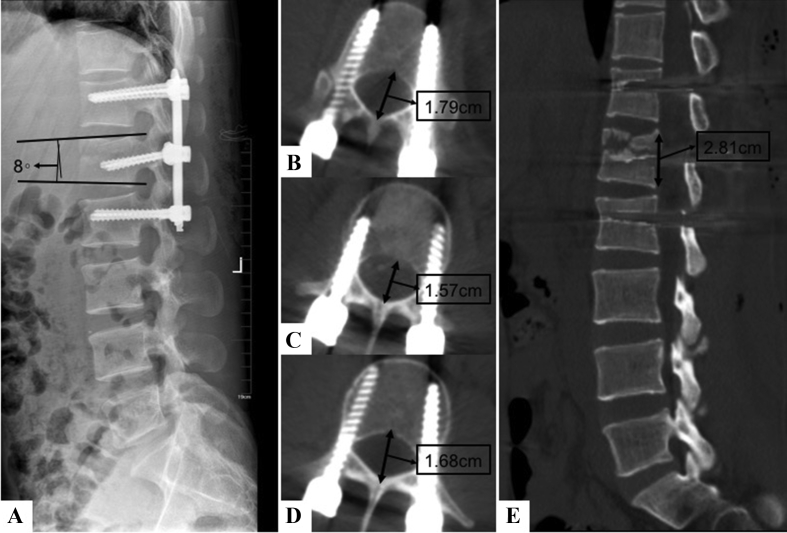
A 31-year-old male patient (Mr. Li), who suffered a fall from height 3 days ago, was diagnosed L1 vertebral burst fracture with a fracture type of A3.1 at the time of admission. Before surgery, the muscles of the lower extremities were normal. The preoperative X-ray showed that the Cobb angle of the L1 vertebral body was 17° (Figure 4A) and posterior vertebral body height of the L1 vertebral body was 1.67 cm (Figure 4E). The volume ratio of the spinal canal was calculated as 1.35/((1.79 + 1.68)/2) = 77.81% (Figures 4B–4D). After the posterior indirect reduction and pedicle internal fixation, under intraoperative C-arm and O-arm imaging, the posterior vertebral body height was found to have been significantly restored (2.81 cm, Figure 5E), the spinal canal volume ratio was improved (1.57/((1.79 + 1.68)/2) = 90.49%, Figures 5B–5D), and the Cobb angle of the L1 vertebral body was significantly corrected (8°, Figure 5A). Therefore, the patient only needed the posterior indirect reduction and pedicle internal fixation, which could achieve the clinical effect of restoring the posterior vertebral body height, improving the volume of the spinal canal, and significantly correcting the kyphosis, without the need for laminectomy decompression. During the follow-up period, the patient showed no delayed neurological symptoms, and there was no significant change in the posterior vertebral body height, the volume ratio of the spinal canal, or the Cobb angle.
Figure 4.
The preoperative X-ray and CT of Cobb angle (A), spinal canal volume of the injured and adjacent vertebrae at T12 (B), L1 (C) L2 (D), and posterior vertebral body height (E) for the typical patient case.
Figure 5.
The intraoperative X-ray and CT of Cobb angle (A), spinal canal volume of the injured and adjacent vertebrae at T12 (B), L1 (C) L2 (D), and posterior vertebral body height (E) for the typical patient case.
Discussion
Thoracic and lumbar vertebrae are the most common sites of spinal fractures. Thoracolumbar burst fractures are common in high-energy injuries. The anterior column and middle column of the vertebral body are frequently damaged. In severe cases, the posterior column can also be involved [[1], [2], [3]]. Because posterior surgery has the characteristics of simple operation, less bleeding and less trauma, clinical posterior pedicle-screw fixation is widely used to treat thoracolumbar burst fractures [6]. It should be emphasised that the thoracolumbar burst fracture not only destroys the stability of the spine but also causes the fracture block to easily protrude into the spinal canal, causing the spinal canal to compromise, leading to spinal nerve injury and affecting the limb functions of the patient. For patients with spinal canal compromise and limb nerve function loss, the addition of spinal canal enlargement and decompression on top of posterior pedicle internal fixation has been recognised by clinicians [11,12]. This additional treatment aims to restore the vertebral body height and the cross-sectional area of the affected spinal canal, correct kyphosis, relieve the nerve compression, and maintain the stability of the spinal cord. However, for the thoracolumbar burst fractures with canal compromise but no neurological symptoms, there has been a long-standing controversy whether it is necessary to perform laminectomy in addition to posterior pedicle internal fixation [[7], [8], [9]]. In other words, there are still different opinions on whether to choose the indirect decompression or the direct decompression, and there is no definitive standard to guide when the direct decompression is needed. Yang et al. [13] believed that for any type of thoracolumbar burst fracture with an intact posterior longitudinal ligament, simple posterior pedicle-screw fixation could be used to complete the indirect reduction, regardless of the proportion of the spinal canal. Patel et al. [14] found that when the spinal canal was occupied by 34–66%, simple posterior internal fixation could be used to complete the indirect decompression, but additional anterior or posterior decompression surgery would be needed when the spinal canal occupancy exceeded 67%. Ye Peng et al. pointed out that the position of the fracture block in the spinal canal could determine whether direct decompression was needed: When the bone in the spinal canal was located in the uncovered area of the posterior longitudinal ligament, the effect of indirect reduction was poor, and additional posterior incision for direct decompression would be required [12]. Peng et al. [12] also found that when the width of the spinal canal reached more than 75% of the transverse diameter of the spinal canal or the height of the bone exceeded 47% of the height of the posterior wall of the injured vertebrae, direct posterior laminectomy and decompression would be needed. On the other hand, there are other authors who hold different opinions. Aebli et al. believed that, as long as there was a fracture block into the spinal canal compressing the spinal cord or the nerve, direct decompression with laminectomy would be needed even if there were no neurological symptoms [15].
In view of the aforemntioned disagreements, the authors retrospectively analysed their patients, describing the basis of the clinical decision of whether to perform direct decompression and reporting the results of follow-up data. It was found that for these patients, after posterior fixation, from intraoperative X-ray and O-arm imaging, if the fracture block protruding into the spinal canal was retracted, the posterior vertebral body height of the fractured vertebral body was significantly restored, the canal volume ratio was increased, and the Cobb angle was significantly improved, then the posterior pedicle-screw fixation could be performed without direct decompression using laminectomy (Group B). From the intraoperative imaging, if the retraction of the fracture block was not obvious, there was no obvious recovery of the posterior vertebral body height of the fractured vertebral body, the volume ratio of the spinal canal did not significantly increase or even decrease, or the Cobb angle was not significantly improved, then additional vertebral plate decompression (Group A) should be performed on top of the pedicle internal fixation. After an average of one year of follow-up, no delayed neurological symptoms were observed in any patient, and there was no statistical difference in the lower limb function between these two groups. The authors believe that it is important to note that although the posterior pedicle-screw fixation cannot completely retract the fracture block from the spinal canal, the degree of posterior protrusion into the spinal canal cannot be used as a standard for choosing direct decompression with laminectomy [16]. Although the residual part of fracture block may still compromise the spinal canal, as long as the patient's injured vertebral body height recovers, the spinal canal volume improves, and kyphosis correction is achieved, a more traumatic laminectomy that would more seriously undermine the spinal stability is not necessary. In addition, the partially restored bone block in the spinal canal can be reabsorbed during the long process of fracture healing and will not cause serious spinal stenosis.
Of course, there are still some limitations to this study. First, the number of patients was relatively small, and the follow-up time was short. More large-scale studies with mid- and long-term follow-up are still needed for further investigation. Secondly, in the recommended workflow, O-arm fluoroscopy is required during the operation to determine whether to perform laminectomy direct decompression, which may impose a high demand on hospital facilities.
Conclusions
In conclusion, for surgical patients of thoracolumbar burst fractures with spinal canal compromise but no neurological deficit, if the fracture protrusion into the spinal canal is seen returned intraoperatively, even if the return is incomplete, the posterior laminectomy for direct decompression is unnecessary as long as the posterior vertebral body height is significantly restored, the volume ratio of the spinal canal is significantly increased, and the kyphosis is corrected. The posterior pedicle-screw internal fixation with indirect decompression, which introduces less trauma and less spinal stability loss, could be selected instead. These patients, compared with patients who undergo direct decompression with laminectomy, show no significant difference in follow-up results and both groups can achieve good clinical results.
Conflict of interest
The authors have no conflicts of interest to disclose in relation to this article.
Acknowledgements
The authors have no acknowledgements to disclose and they received no funding for the work described in this article.
References
- 1.Kraemer W.J., Schemitsch E.H., Lever J., McBroom R.J., McKee M.D., Waddell J.P. Functional outcome of thoracolumbar burst fractures without neurological deficit. J Orthop Trauma. 1996;10(8):541–544. doi: 10.1097/00005131-199611000-00006. [DOI] [PubMed] [Google Scholar]
- 2.Esses S.I., Botsford D.J., Kostuik J.P. Evaluation of surgical treatment for burst fractures. Spine. 1990;15(7):667–673. doi: 10.1097/00007632-199007000-00010. [DOI] [PubMed] [Google Scholar]
- 3.Müller U., Berlemann U., Sledge J., Schwarzenbach O. Treatment of thoracolumbar burst fractures without neurologic deficit by indirect reduction and posterior instrumentation: bisegmental stabilization with monosegmental fusion. Eur Spine J. 1999;8(4):284–289. doi: 10.1007/s005860050175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tonn J.C., Schichor C., Schnell O., Zausinger S., Uhl E., Morhard D. Intraoperative computed tomography. Acta Neurochir Suppl. 2011;109(109):163–167. doi: 10.1007/978-3-211-99651-5_25. [DOI] [PubMed] [Google Scholar]
- 5.Leferink V., Nijboer J., Zimmerman K., Veldhuis E., ten Vergert E., ten Duis H. Burst fractures of the thoracolumbar spine: changes of the spinal canal during operative treatment and follow-up. Eur Spine J. 2003;12(3):255–260. doi: 10.1007/s00586-002-0499-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Haiyun Y., Rui G., Shucai D., Zhanhua J., Xiaolin Z., Xin L. Three-column reconstruction through single posterior approach for the treatment of unstable thoracolumbar fracture. Spine. 2010;35(8):295–302. doi: 10.1097/BRS.0b013e3181c392b9. [DOI] [PubMed] [Google Scholar]
- 7.Rajasekaran S. Thoracolumbar burst fractures without neurological deficit: the role for conservative treatment. Eur Spine J. 2010;19(Suppl. 1):40–47. doi: 10.1007/s00586-009-1122-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Won-Ju J., Joon-Woo K., Dong-Kyo S., Hyun-Joo L., Jun-Young K., Jong Pil Y. Efficiency of ligamentotaxis using PLL for thoracic and lumbar burst fractures in the load-sharing classification. Orthopedics. 2013;36(5):E567–E574. doi: 10.3928/01477447-20130426-17. [DOI] [PubMed] [Google Scholar]
- 9.Shen J., Xu L., Zhang B., Hu Z. Risk factors for the failure of spinal burst fractures treated conservatively according to the Thoracolumbar Injury Classification and Severity Score (TLICS): a retrospective cohort trial. PLoS One. 2015;10(8) doi: 10.1371/journal.pone.0135735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Toh E., Arima T., Mochida J., Omata M., Matsui S. Functional evaluation using motor scores after cervical spinal cord injuries. Spinal Cord. 1998;36(7):491–496. doi: 10.1038/sj.sc.3100606. [DOI] [PubMed] [Google Scholar]
- 11.Mahar A., Kim C., Wedemeyer M., Mitsunaga L., Odell T., Johnson B. Short-segment fixation of lumbar burst fractures using pedicle fixation at the level of the fracture. Spine. 2007;32(14):1503–1507. doi: 10.1097/BRS.0b013e318067dd24. [DOI] [PubMed] [Google Scholar]
- 12.Peng Y., Zhang L., Shi T., Lyu H., Zhang L., Tang P. Relationship between fracture-relevant parameters of thoracolumbar burst fractures and the reduction of intra-canal fracture fragment. J Orthop Surg Res. 2015;10(1):1–9. doi: 10.1186/s13018-015-0260-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yang H., Shi J.H., Ebraheim M., Ebaheim M., Liu X., Konrad J. Outcome of thoracolumbar burst fractures treated with indirect reduction and fixation without fusion. Eur Spine J. 2011;20(3):380–386. doi: 10.1007/s00586-010-1542-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Patel A., Brown Z., Whang P.G. Thoracolumbar spine trauma. Oper Tech Orthop. 2007;17(3):190–198. [Google Scholar]
- 15.Aebli N., Kaiser T., Moulin P., Krebs J. Short-segment posterior instrumentation combined with anterior spondylodesis using an autologous rib graft in thoracolumbar burst fractures. Acta Orthop. 2014;85(1):84–90. doi: 10.3109/17453674.2013.871137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Limb D., Shaw D.L., Dickson R.A. Neurological injury in thoracolumbar burst fractures. J Bone Joint Surg Br. 1995;77(5):774–777. [PubMed] [Google Scholar]