Abstract
This study examined the incidence and trends of surfing-related and mild traumatic brain injuries that presented to United States emergency departments between 2001 and 2016. Subjects with surging-related head injuries were retrieved from the National Electronic Injury Surveillance System. A weighted total of 34,337 surfing-related head injuries were identified. The annual incidence of surfing-related head injuries insignificantly decreased from 2001 to 2016 (R2 = .119; p = .19). Most common injuries included lacerations (50.4%), blunt head injuries (25.7%), and mild traumatic brain injuries (16.1%). Mild traumatic brain injury incidence and annual percentage increased significantly during the study period (R2 = .251; p = .05 and R2 = .346; p = .02, respectively).
Keywords: Surfing, Head injury, Epidemiology, Mild traumatic brain injury, Concussion, Sports-related injury
1. Introduction
Sports-related mild traumatic brain injuries (MTBIs), also known as concussions, have garnered increased interest in both the media and literature in recent decades. MTBIs in sports are common, and appropriate diagnosis and management are critical for better long-term outcomes. In the United States (US) alone, the estimated yearly incidence of concussions sustained from competitive and recreational activities is 3.8 million.1 Although MTBI in high-impact sports such as football has been extensively studied,2 its relevance in non-contact sports and activities has grown in recent years.3,4 This includes surfing, an increasingly popular sport worldwide with limited literature on associated head injuries.
Within the last decade, surfing participation has almost tripled from 13 to 37 million surfers.5 In a recent survey, 91% of surfers admitted to sustaining a sport-related injury at some point during their career, the most common directed at the head in 37% of cases.5, 6, 7, 8 MTBIs also accounted for 37% of reported surfing-related head injuries in a recent survey-based study.3 Considering that an estimated 50% of MTBIs go unreported, the true incidence of surfing-related concussions may be even higher.1
Currently, the literature regarding surfing-mediated MTBIs is largely survey-based. To our knowledge, ED-retrieved medical data has not been thoroughly assessed. Therefore, using a US ED database, this study aimed at examining the incidence and annual trends of surfing-related head injuries with a particular emphasis on MTBIs between 2001 and 2016. We specifically evaluated the frequency of the total and most common surfing-related head injuries, as well as the proportion of MTBIs among them.
2. Materials and methods
2.1. Data source and patient selection
Between January 2001 and December 2016, general and head-related surfing injuries were identified using the National Electronic Injury Surveillance System (NEISS) Manual codes 1261 and 75, respectively. NEISS is a database operated by the US Consumer Product Safety Commission (CPSC) that collects de-identified ED data from approximately 100 participating hospitals across the country and generates a nationwide probability sample of consumer product injuries based on calculated weighted values.9 No exclusions were made based on patients’ age, gender, or race.
2.2. Outcomes
The primary outcomes assessed encompassed the frequency of the total and most common surfing-associated head injuries, as well as the proportion of MTBIs. For such purposes, the weighted values reported in the NEISS database were used. The yearly incidence of each injury type was assessed over the 15-year period between 2001 and 2016.
2.3. Data analysis
The data was compiled in a Microsoft Excel spreadsheet (Microsoft Corporation, Redmond, Washington). The incidence of surfing head injuries was determined using NEISS weighted values for each documented case. Annual trends were then computed with linear regression analysis using SPSS version 24 (IBM Corp., Armonk, New York). The threshold for statistical significance was set at p < .05.
3. Results
3.1. Study population
A total of 561 cases, corresponding to a weighted estimate of 34,337 surfing-related head injuries, were retrieved from NEISS between 2001 and 2016. Patient ages ranged between 4 and 74 years with a mean age of 25.6 years. The sample included 28,378 males (82.6%) and 5,959 females (17.4%) estimates. 76.7% of the sample were White, 4.9% Asian, 0.9% Black, 1.1% designated as “other” (predominantly Hispanic), 0.2% Native Hawaiian/Pacific Islander, and 16.1% did not have their race stated in the ED record.
3.2. Incidence and trends of surfing-related head injuries
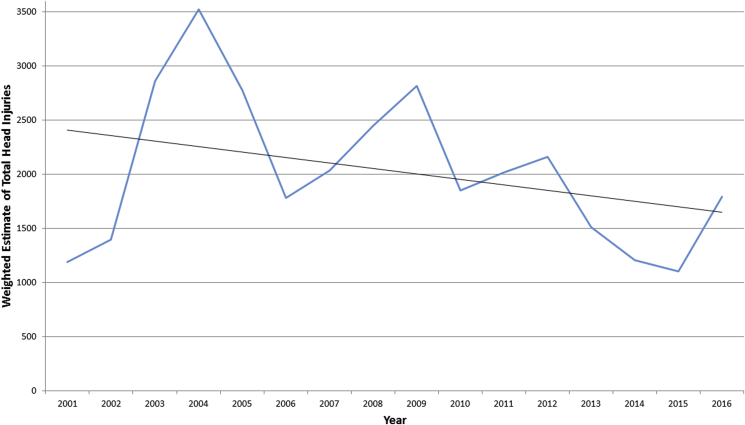
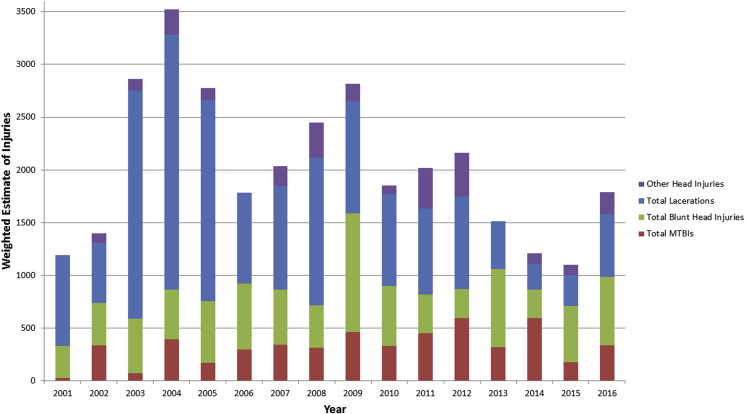
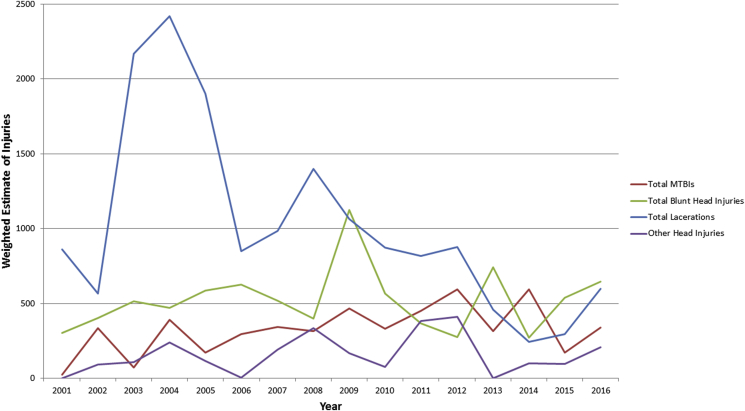
The weighted annual estimate of surfing-related head injuries varied from 1189.71 in 2001 to 1790.66 in 2016. However, the resulting trend did not reach statistical significance (R2 = .119; p = .19) (Fig. 1). Most common surfing-related head injuries included lacerations (50.4%), blunt head injuries (25.7%), and MTBIs (16.1%). Throughout the study time period, total yearly blunt head trauma injuries remained stable with weighted estimates of 305.29 and 646.55 in 2001 and 2016, respectively (R2 = .018; p = .62). Contrarily, the weighted estimate of lacerations dropped modestly from 860.44 in 2001 to 598.70 in 2016 (R2 = .351; p = .02) (Fig. 2, Fig. 3).
Fig. 1.
Weighted estimates and trend of total surfing-related head injuries from 2001 to 2016.
Fig. 2.
Weighted estimates of surfing-related head injuries from 2001 to 2016 for laceration, concussion, and blunt head injury, compared to all other head injuries combined.
Fig. 3.
Annual weighted estimates and trends of the most common surfing-related head injuries between 2001 and 2016.
3.3. Surfing-related concussions
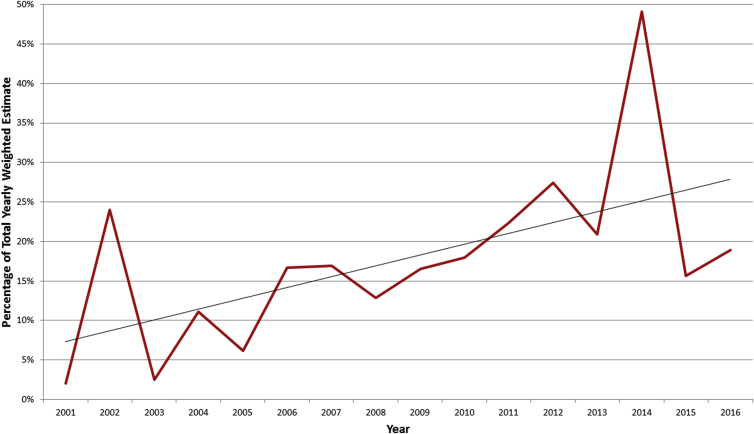
An estimated 5,128 surfing-related MTBIs were reported during the study period, making them the third most common head injury subtype, representing 16.1% of all head injuries. The 2016 incidence and percentage of MTBI were significantly higher than the ones in 2001 (R2 = .251; p = .05 and R2 = .346; p = .02, respectively) (Fig. 4).
Fig. 4.
Percentage of yearly mild traumatic brain injury weighted estimates between 2001 and 2016.
4. Discussion
Our findings corroborate the current literature, indicating that head injuries including MTBIs are relevant in surfing.3,5, 6, 7, 8 Prior to this study, the body of evidence on surfing-related head injuries and MTBIs was almost entirely survey-based. Though inexpensive and convenient, self-reported data carries inherent shortcomings including response and recall biases. Two studies have used the NEISS database to establish a more objective incidence of surfing-related injuries, but did not address specific head injury subtypes.5,10 This study constitutes an important transition from self-reported to more objective data regarding surfing-related head injuries and MTBIs.
In the current investigation, a weighted total of 34,337 surfing-related head injuries were noted between 2001 and 2016. The most common overall injuries were lacerations, followed by blunt head injuries and MTBIs. Although the incidence of all head injuries did not significantly differ between 2001 and 2016, both MTBI incidence and proportion increased significantly. Outside the acute setting, MTBIs can lead to debilitating and lifelong sequelae for patients, and recurrent episodes may increase the risk of subsequent chronic traumatic encephalopathy, cognitive impairments, and mental health issues.11,12 The relatively stable head injury incidence coupled with MTBI's significant increase over our study period raise questions about the mechanism(s) behind the increasing trends of MTBI. Has surfing as a sport become more intense or risky, or is this trend a result of increased accessibility of the sport to the general public? Alternatively, has awareness and accurate diagnosis of MTBIs among surfers and clinicians improved?
In the US, the risks of acute surfing injuries increase in those who surf more than 6.5 h weekly, in large waves or over a hard seafloor, or who are able to perform aerial maneuvers.8,13,14 Such risk factors may also contribute to more serious injuries, including those to the head, MTBIs in particular. Moreover, changes in surfing equipment such as lighter, shorter, and narrower board designs enable greater speed and maneuvering capabilities, while also attributing to unpredictable changes when dislodged.15 This might explain why most common mechanisms of surfing-related injury are contact with a surfboard or with other surfers in up to 50% of cases.7,15,16
Although surfing is likely becoming riskier in recent years, the increase in MTBI diagnosis across multiple sports cannot be solely explained by surfing-related factors. Indeed, the CDC's 2011 NEISS-based report covered a time period overlapping with ours and echoed similar increasing trends in other sports-related MTBIs.17 Such trends suggest a better MTBI diagnosis at the acute care level. In fact, since its commencement in 2000, the CDC's “Heads Up” public education campaign underwent elaborate expansion into a collection of educational resources tailored for the general public, clinicians, coaches, and parents.18 Clinically, physicians exposed to this program were significantly less likely to recommend next day return to play after a MTBI compared to unexposed colleagues.19 In line with these findings, evidence-based guidelines—Task Forces on Mild Traumatic Brain Injury (MTBI) of the European Federation of Neurological Societies and the World Health Organization Collaborating Center—and diagnostic tools—Sport Concussion Assessment Tool 5 (SCAT5) and the NFL Sideline Concussion Assessment Tool—have evolved to aid with quick and accurate diagnosis.11,20,21
4.1. Study limitations
The present study has some limitations. At first, the NEISS database reports acute injuries presented to EDs only, does not account for patients seeking medical help at primary care facilities and other outpatient care clinics, and strongly relies on the weighted estimations of individual cases. Additionally, due to its retrospective nature, our analysis did only investigate the variables reported without taking into consideration other potential confounding factors, such as details regarding the circumstances and mechanisms of the injuries. Prospective studies specifically enrolling surfers while stratifying them by age, gender, geographic location, surfing experience, and type of head injury are warranted to adequately depict the epidemiology of surfing-related head injuries and their predictive factors.
5. Conclusions
The incidence of surfing-related head injuries presenting to US EDs remained stable during the 15-year study period, whereas MTBI's proportion and incidence increased significantly. Physicians, especially those with added training in sports medicine, should be aware of these insults, for a quick and accurate evaluation, diagnosis, and management. Further research is needed to isolate risk factors associated with head injuries in surfers and permit a primary prevention of these conditions.
Previous presentations
The abstract of this material has been presented at the AAPM&R Annual Assembly held in Orlando, Florida, USA, from October 25th to 28th, 2018.
Funding sources and financial disclosures
No sources of internal or external funding were sought after or utilized for completion of any aspect of this study. No conflicts of interest influenced any aspect of this study. All of the co-authors report no financial conflicts of interest to disclosure.
Declaration of competing interest
No conflicts of interest.
References
- 1.Harmon K.G., Drezner J.A., Gammons M. American Medical Society for Sports Medicine position statement: concussion in sport. Br J Sports Med. 2013;47(1):15–26. doi: 10.1136/bjsports-2012-091941. [DOI] [PubMed] [Google Scholar]
- 2.Chatterjee D., Frumberg D.B., Mulchandani N.B. Current concepts in sports-related concussion. Crit Rev Biomed Eng. 2015;43(5-6):371–383. doi: 10.1615/CritRevBiomedEng.2016016393. [DOI] [PubMed] [Google Scholar]
- 3.Swinney C. Assessing the prevalence of traumatic head injury amongst recreational surfers in the United States. Hawai‘i J Med Public Health. 2015;74(12):403–405. [PMC free article] [PubMed] [Google Scholar]
- 4.Blumenfeld R.S., Winsell J.C., Hicks J.W., Small S.L. The epidemiology of sports-related head injury and concussion in water polo. Front Neurol. 2016;7:98. doi: 10.3389/fneur.2016.00098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Klick C., Jones C.M.C., Adler D. Surfing USA: an epidemiological study of surfing injuries presenting to US EDs 2002 to 2013. Am J Emerg Med. 2016;34(8):1491–1496. doi: 10.1016/j.ajem.2016.05.008. [DOI] [PubMed] [Google Scholar]
- 6.Woodacre T., Waydia S.E., Wienand-Barnett S. Aetiology of injuries and the need for protective equipment for surfers in the UK. Injury. 2015;46(1):162–165. doi: 10.1016/j.injury.2014.07.019. [DOI] [PubMed] [Google Scholar]
- 7.Moran K., Webber J. Surfing injuries requiring first aid in New Zealand, 2007-2012. Int J Aquat Res Educ. 2013;7(3):192–203. [Google Scholar]
- 8.Nathanson A., Haynes P., Galanis D. Surfing injuries. Am J Emerg Med. 2002;20(3):155–160. doi: 10.1053/ajem.2002.32650. [DOI] [PubMed] [Google Scholar]
- 9.Schroeder T., Ault K. 2001. The NEISS Sample (Design and Implementation) 1997 to Present. Washington, D.C. [Google Scholar]
- 10.Myers S.E., Diamond P.T. Common injuries associated with long and short board surfing: a five-year analysis of emergency room visits. PM&R. 2010;1:S51. [Google Scholar]
- 11.Phillips S., Woessner D. Sports-related traumatic brain injury. Prim Care. 2015;42(2):243–248. doi: 10.1016/j.pop.2015.01.010. [DOI] [PubMed] [Google Scholar]
- 12.Manley G., Gardner A.J., Schneider K.J. A systematic review of potential long-term effects of sport-related concussion. Br J Sports Med. 2017;51(12):969–977. doi: 10.1136/bjsports-2017-097791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Furness J., Hing W., Walsh J., Abbott A., Sheppard J.M., Climstein M. Acute injuries in recreational and competitive surfers. Am J Sports Med. 2015;43(5):1246–1254. doi: 10.1177/0363546514567062. [DOI] [PubMed] [Google Scholar]
- 14.Nathanson A., Bird S., Dao L., Tam-Sing K. Competitive surfing injuries: a prospective study of surfing-related injuries among contest surfers. Am J Sports Med. 2007;35(1):113–117. doi: 10.1177/0363546506293702. [DOI] [PubMed] [Google Scholar]
- 15.Taylor D.M.D., Bennett D., Carter M., Garewal D., Finch C.F. Acute injury and chronic disability resulting from surfboard riding. J Sci Med Sport. 2004;7(4):429–437. doi: 10.1016/s1440-2440(04)80260-3. [DOI] [PubMed] [Google Scholar]
- 16.Dimmick S.J., Sheehan P.V., Gillett M., Anderson S.E. Injuries to the head and face sustained while surfboard riding. Med J Aust. 2013;198(8):419. doi: 10.5694/mja13.10006. [DOI] [PubMed] [Google Scholar]
- 17.Department of Health and Human Services C Nonfatal traumatic brain injuries related to sports and recreation activities among persons aged ≤19 years--United States, 2001-2009. MMWR Morb Mortal Wkly Rep. 2011;60(39):1337–1342. [PubMed] [Google Scholar]
- 18.Sarmiento K., Hoffman R., Dmitrovsky Z., Lee R. A 10-year review of the Centers for Disease Control and Prevention's Heads up initiatives: bringing concussion awareness to the forefront. J Saf Res. 2014;50:143–147. doi: 10.1016/j.jsr.2014.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chrisman S.P., Schiff M.A., Rivara F.P. Physician concussion knowledge and the effect of mailing the CDCs “heads up” toolkit. Clin Pediatr. 2011;50(11):1031–1039. doi: 10.1177/0009922811410970. [DOI] [PubMed] [Google Scholar]
- 20.Vos P.E., Battistin L., Birbamer G. EFNS guideline on mild traumatic brain injury: report of an EFNS task force. Eur J Neurol. 2002;9(3):207–219. doi: 10.1046/j.1468-1331.2002.00407.x. [DOI] [PubMed] [Google Scholar]
- 21.Borg J., Holm L., Cassidy J.D. Diagnostic procedures in mild traumatic brain injury: results of the WHO collaborating centre task force on mild traumatic brain injury. J Rehabil Med. 2004;43(Suppl):61–75. doi: 10.1080/16501960410023822. [DOI] [PubMed] [Google Scholar]