Abstract
Background
Hypoalbuminemia is a marker for malnourishment and is associated with poor outcomes in the setting of hip fractures, periprosthetic joint fractures, and spine surgery. We hypothesized that hypoalbuminemia is associated with higher rates of early complication in patients undergoing surgical treatment for proximal humerus fractures.
Methods
Utilizing the ACS NSQIP database, all proximal humerus fractures treated with plate fixation were extracted from 2006 to 2015. Two cohorts were compared based on hypoalbuminemia (albumin <3.5 g/dL) versus normoalbuminemia (albumin >3.5 g/dL). Patient demographics and postoperative complications were analyzed with multivariable regression.
Results
Out of 916 patients undergoing PHF surgery, 290(31.7%) satisfied criteria for hypoalbuminemia (mean age: 65.9, female: 71%). Among 339 obese patients with BMI>30, 87 (25.7%) were hypoalbuminemic. Patients with hypoalbuminemia were overall at higher risk of any (29.7% vs 12.1%, p < 0.001), major (10.0% vs 2.4%, p < 0.001), and minor complications (24.1% vs 11.0%, p < 0.001) as well as readmissions (12.7% vs 5.1%, p < 0.001). Obese hypoalbuminemic patients had similar rates of complication as non-obese hypoalbuminemic patients. Multivariable regression showed that hypoalbuminemia had an odds ratio of 1.85(p = 0.003) for predicting any complication within 30 days of surgery.
Conclusion
Hypoalbuminemia is associated with higher risk for complications and readmission after PHFs. It occurs more frequently in patients with chronic disease and is predictive of malnourishment. Paradoxically, hypoalbuminemia is not uncommon in obese patients.
Level of evidence
III; Retrospective Cohort Study.
Keywords: Proximal humerus fractures, Malnourishment, Hypoalbuminemia, Complications, Perioperative outcomes
1. Introduction
Serum albumin (SA), an acute-phase protein, has been evaluated as a marker for malnutrition and is shown to correlate with risk for surgical complications and mortality.1,2 An estimated 20% of all patients admitted for an acute medical condition meet criteria for hypoalbuminemia, defined as SA under 3.5 g/dL.3,4 Several studies have shown that hypoalbuminemia is associated with increased short-term mortality, length of hospital stay and complications.5, 6, 7
Thus, SA levels may have utility in predicting complications among patients with traumatic orthopaedic injuries including proximal humerus fractures (PHF). In the past several decades, the incidence of PHF has significantly increased in the US and is now the third most common fracture treated by orthopedic surgeons.8,9 Established risk factors for sustaining proximal humerus fracture include advanced age, female sex, history of fractures, low bone mineral density, history of falls, poor vision, specific medical comorbidities such as insulin-dependent diabetes, and low physical activity.10, 11, 12
While previous studies have shown hypoalbuminemia to be associated with worse outcomes in orthopedic procedures including hip fractures and periprosthetic joint fractures, no study to date has assessed the impact of hypoalbuminemia on early complication rates with patients sustaining PHF.13 Thus, the purpose of this study was to define the association between hypoalbuminemia and 30-day postoperative complications in patients undergoing open reduction-internal fixation (ORIF) for PHF. We hypothesize that hypoalbuminemia will be an independent risk factor associated with increased early postoperative complications that may lead to poor outcomes.
2. Methods
Utilizing the American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) database, all PHF treated with plate fixation as defined by the Current Procedural Terminology (CPT) code 23615 (open treatment of proximal humeral fracture, includes internal fixation, when performed, includes repair of tuberosity(s) when performed) were extracted between January 1, 2006 and December 31, 2015.14 No identifiable patient information is included in the database, and was thus deemed exempt from IRB. Patients presenting to the emergency department in an urgent or emergent manner with activation of the trauma protocol were not included in the NSQIP database. Thus, all cases analyzed were elective in nature.
Exclusion criteria included any patients less than 18 years old, incomplete data or missing data on SA levels. Patients with diagnoses of pathologic fracture or cancer were also excluded. Demographic variables were collected for all patients. Demographic factors included sex, age, race, BMI, and other comorbidities. Comorbidities included history of diabetes, dyspnea, chronic obstructive pulmonary disease (COPD), smoking, chronic heart failure (CHF), dialysis, renal failure, hypertension, bleeding disorder, and steroids. Patients were stratified by albumin levels: ≥3.5 g/dL (normal) or <3.5 g/dL (hypoalbuminemic) that were obtained within 30 days of the surgical date. Patients were also characterized by American Society of Anesthesiologists (ASA) Class (Table 1).
Table 1.
Patient demographics and characteristics.
| All Patients | Albumin: ≥3.5 | Albumin: <3.5 | P | |
|---|---|---|---|---|
| Total | 916 | 626 | 290 | |
| Demographics | ||||
| Age: years, mean (SD) | 65.9 (13.4) | 65 (13.5) | 68 (12.9) | 0.002 |
| Gender: n (%) | 0.328 | |||
| Female | 653 (71.3) | 453 (72.4) | 200 (69) | |
| Male | 263 (28.7) | 173 (27.6) | 90 (31) | |
| Race: n (%) | 0.863 | |||
| White | 793 (86.6) | 541 (86.4) | 252 (86.9) | |
| Nonwhite | 56 (6.1) | 40 (6.4) | 16 (5.5) | |
| Unknown | 67 (7.3) | 45 (7.2) | 22 (7.6) | |
| Comorbidities | ||||
| BMI: kg/m^2, mean (SD) | 29.1 (8.2) | 29.6 (7.8) | 28.0 (8.8) | 0.005 |
| Diabetes: n (%) | 0.068 | |||
| Non-insulin Dependent | 118 (12.9) | 87 (13.9) | 31 (10.7) | |
| Insulin Dependent | 96 (10.5) | 57 (9.1) | 39 (13.4) | |
| Dyspnea: n (%) | <0.001 | |||
| At rest | 6 (0.7) | 3 (0.5) | 3 (1) | |
| Moderate Exertion | 63 (6.9) | 36 (5.8) | 27 (9.3) | |
| COPD: n (%) | 87 (9.5) | 38 (6.1) | 49 (16.9) | 0.007 |
| Smoking: n (%) | 207 (22.6) | 125 (20) | 82 (28.3) | 0.556 |
| CHF: n (%) | 17 (1.9) | 10 (1.6) | 7 (2.4) | <0.001 |
| Dialysis: n (%) | 10 (1.1) | 1 (0.2) | 9 (3.1) | 0.005 |
| Renal Failure: n (%) | 7 (0.8) | 1 (0.2) | 6 (2.1) | 0.608 |
| Hypertension: n (%) | 559 (61) | 378 (60.4) | 181 (62.4) | 0.005 |
| Bleeding disorder: n (%) | 88 (9.6) | 48 (7.7) | 40 (13.8) | 0.073 |
| Steroids: n (%) | 58 (6.3) | 33 (5.3) | 25 (8.6) | <0.001 |
| ASA Class: n (%) | <0.001 | |||
| 1 | 24 (2.6) | 22 (3.5) | 2 (0.7) | |
| 2 | 286 (31.3) | 232 (37.1) | 54 (18.6) | |
| 3 | 509 (55.6) | 326 (52.2) | 183 (63.1) | |
| 4 | 96 (10.5) | 45 (7.2) | 51 (17.6) | |
| Clinical Characteristics | ||||
| Serum Albumin: mean (SD) | 3.70 (0.6) | 4.0 (0.4) | 3.0 (0.4) | <0.001 |
| Preop. Blood Transfusion: n (%) | 39 (4.3) | 12 (1.9) | 27 (9.3) | 0.02 |
| Anemia: n (%) | 538 (58.7) | 313 (50) | 225 (77.6) | <0.001 |
* BMI: Body Mass Index; COPD: Chronic Obstructive Pulmonary Disease; CHF: Congestive Heart Failure: ASA: American Society of Anesthesiology; Preop Blood Transfusion - within 48 h preoperatively.
The primary outcome measures were any major or minor complications within 30-days of surgery. Major complications included sepsis, septic shock, wound infection, pulmonary embolism, ventilator usage for greater than 48 h, reintubation, renal failure, cardiac arrest, myocardial infarction, or cerebrovascular accident. Minor complications were identified as superficial surgical site infection, pneumonia, urinary tract infection, deep vein thrombosis, bleeding requiring transfusion, and renal insufficiency. Criteria for complications are defined in the NSQIP Participant Use File available at https://www.facs.org/quality-programs/acs-nsqip/program-specifics/participant-use. Other outcomes measured included readmission to the hospital, reoperation rate, and hospital length of stay in days. Additional sub analysis was performed evaluating the prevalence of hypoalbuminemia in obese and non-obese patients, as well as complication rates in these sub-groups.
Summary statistics including means, standard deviations and 95% confidence intervals were calculated for continuous variables. Categorical variables were reported in terms of frequencies and percentages. Statistical analysis was performed using the R statistical software package (R Foundation for Statistical Computing, Vienna, Austria). Student's t-test, chi-squared contingency testing, and multivariate logistic regression were conducted. All variables were controlled for in a multivariable regression analysis to identify independent variables significantly associated with 30-day complication rates. A p-value of <0.05 was deemed statistically significant.
3. Results
Out of 916 patients undergoing open reduction internal fixation for proximal humerus fractures, 290 (31.7%) satisfied criteria for hypoalbuminemia (SA <3.5 g/dL). Mean SA levels in normal patients was 4.0 (SD: 0.4) g/dL and 3.0 (0.4) g/dL in hypoalbuminemic patients (p < 0.001). The mean age for all patients was 65.9 years (standard deviation [SD]: 13.4). Patients with hypoalbuminemia were on average older than patients without hypoalbuminemia (68.0 years [SD: 13.5] vs 65.0 years old [SD: 12.9], p = 0.002). Majority of patients were female (263 or 28.7% male and 653 or 71.3% female). A summary of the other preoperative patient characteristics and comorbidities are in Table 1.
Compared to patients with normal albumin, hypoalbuminemia was found to be associated with higher rates of comorbidities including COPD (16.9% vs 6.1%, p = 0.007), chronic steroid use (8.6% vs 5.3%, p < 0.001), and preoperative anemia (77.6% vs 50.0%, p < 0.001). Overall, 80.7% of patients with hypoalbuminemia had a ASA class of 3 or 4 compared to 59.4% of normal patients (p < 0.001) (Table 1).
Patients with hypoalbuminemia were overall at higher risk of any (29.7% vs 12.1%, p < 0.001), major (10.0% vs 2.4%, p < 0.001), and minor complications (24.1% vs 11.0%, p < 0.001), readmissions (12.7% vs 5.1%, p < 0.001), and length of stay (5.9 days vs 3.5 days, p < 0.001). Significant differences in major complications included rate of sepsis (p = 0.014), ventilator usage for greater than 48 h (p = 0.036), and reintubation (p = 0.037; Table 2).
Table 2.
Association of hypoalbuminemia with complications.
| All Patients | Albumin: ≥3.5 | Albumin: <3.5 | P | |
|---|---|---|---|---|
| Total | 916 | 626 | 290 | |
| Any Complication | 162 (17.7) | 76 (12.1) | 86 (29.7) | <0.001 |
| Major Complication | 44 (4.8) | 15 (2.4) | 29 (10) | <0.001 |
| Sepsis | 6 (0.7) | 1 (0.2) | 5 (1.7) | 0.014 |
| Septic Shock | 3 (0.3) | 1 (0.2) | 2 (0.7) | 0.237 |
| Wound Infection | 5 (0.5) | 2 (0.3) | 3 (1) | 0.185 |
| Pulmonary Embolism | 6 (0.7) | 5 (0.8) | 1 (0.3) | 0.671 |
| Ventilator ≥48 h | 7 (0.8) | 2 (0.3) | 5 (1.7) | 0.036 |
| Reintubation | 5 (0.5) | 1 (0.2) | 4 (1.4) | 0.037 |
| Renal Failure | 3 (0.3) | 1 (0.2) | 2 (0.7) | 0.237 |
| Cardiac Arrest | 3 (0.3) | 1 (0.2) | 2 (0.7) | 0.237 |
| Myocardial Infarction | 2 (0.2) | 1 (0.2) | 1 (0.3) | 0.533 |
| Cerebrovascular Accident | 2 (0.2) | 1 (0.2) | 1 (0.3) | 0.533 |
| Minor Complication | 139 (15.2) | 69 (11) | 70 (24.1) | <0.001 |
| Superficial Infection | 2 (0.2) | 2 (0.3) | 0 (0) | 1 |
| Pneumonia | 19 (2.1) | 9 (1.4) | 10 (3.4) | 0.082 |
| Urinary Tract Infection | 14 (1.5) | 6 (1) | 8 (2.8) | 0.046 |
| Deep Vein Thrombosis | 8 (0.9) | 5 (0.8) | 3 (1) | 0.713 |
| Transfusion | 107 (11.7) | 51 (8.1) | 56 (19.3) | <0.001 |
| Readmission (Out of 709) | 53 (7.5) | 25 (5.1) | 28 (12.7) | <0.001 |
| Reoperation (Out of 713) | 26 (3.6) | 15 (3.1) | 11 (5) | 0.299 |
| Hospital Length of Stay: days, mean (SD) | 4.2 (14.5) | 3.5 (16.7) | 5.9 (7.6) | <0.001 |
All complications shown are reported in number of incidents followed by rate of incidence in parantheses.
Multivariable logistic regression revealed hypoalbuminemia was independently associated with complication within 30-days of surgery (odds ratio 1.85, 95% confidence interval: 1.22–2.79; p = 0.003; Table 3). Factors such as diabetes, COPD, smoking, and hypertension were not significant predictors of hypoalbuminemia.
Table 3.
Association of hypoalbuminemia with complications.
| Adjusted OR(95%CI) | P | |
|---|---|---|
| Hypoalbuminemia (ref. = Normal) | 1.85 (1.22,2.79) | 0.003 |
| Age (cont. var.) | 1.01 (1.00,1.03) | 0.124 |
| Male (ref. = Female) | 1.06 (0.68,1.64) | 0.81 |
| Race (ref. = White) | ||
| Nonwhite | 2.21 (1.10,4.40) | 0.025 |
| Unknown | 1.09 (0.52,2.26) | 0.821 |
| BMI (cont. var.) | 1.01 (0.99,1.04) | 0.319 |
| Diabetes (ref. = Non-Diabetic) | ||
| Non-insulin Dependent | 0.62 (0.33,1.16) | 0.133 |
| Insulin Dependent | 0.72 (0.37,1.38) | 0.323 |
| Dyspnea (ref. = Non-Dyspneic) | ||
| At rest | 1.5 (0.22,10.37) | 0.681 |
| Moderate Exertion | 0.51 (0.22,1.19) | 0.12 |
| COPD | 1.07 (0.57,1.99) | 0.844 |
| Smoking | 0.97 (0.57,1.65) | 0.903 |
| CHF | 0.8 (0.22,2.88) | 0.733 |
| Dialysis | 0.35 (0.07,1.79) | 0.206 |
| Renal Failure | 1.78 (0.27,11.8) | 0.552 |
| Hypertension | 0.92 (0.59,1.46) | 0.73 |
| Bleeding Disorder | 1.31 (0.73,2.34) | 0.371 |
| Steroid Use | 1.73 (0.88,3.38) | 0.11 |
| ASA Class (ref. = ASA 1) | ||
| 2 | 0.63 (0.13,3.12) | 0.574 |
| 3 | 1.50 (0.31,7.2) | 0.611 |
| 4 | 3.62 (0.69,18.87) | 0.127 |
| Preop. Transfusion | 3.59 (1.69,7.66) | <0.001 |
| Anemia | 2.71 (1.68,4.37) | <0.001 |
OR: Odd's Ratio; CI: Confidence Interval.
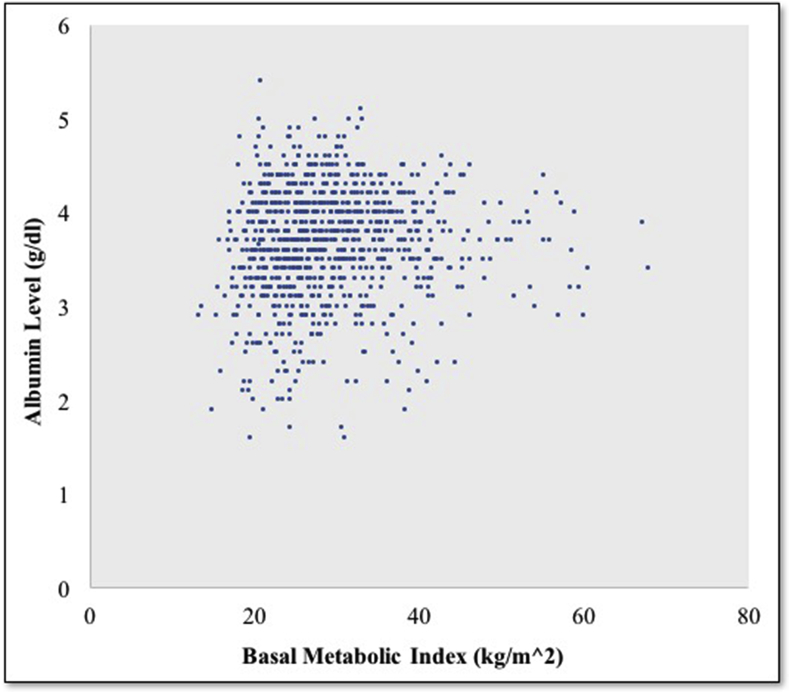
Among 339 obese patients with BMI>30, 87 (25.7%) were hypoalbuminemic. However, obese hypoalbuminemic patients had similar rates of complication compared to non-obese hypoalbuminemic patients (33.3% vs 31.0%) (Fig. 1).
Fig. 1.
Albumin and BMI correlation.
4. Discussion
Management of proximal humerus fractures varies depending on patient comorbidities and severity of injury. Treatment options include nonoperative treatment, open reduction-internal fixation (ORIF), hemiarthroplasty, or total/reverse shoulder arthroplasty.15,16 Risks associated with operative treatment may predispose patients to increased short and long-term complications, thus optimizing the patient for surgery is of great importance to decrease risk of poor outcomes. Modifiable risk factors including poor nutritional status can potentially be corrected prior to surgery.17 Albumin levels are commonly used in the hospital to assess nutritional status, and thus may be prudent to analyze during routine preoperative workup. In this study, we report that an estimated 31.7% of patients undergoing open plate fixation of proximal humerus fractures are hypoalbuminemic (SA<3.5). Additionally, hypoalbuminemia was frequently associated with higher comorbidity burden and was an independent predictor for higher 30-day postoperative complications after surgery.
A surprisingly large proportion of PHF patients (31.7%) were hypoalbuminemic in our study. Comparatively, Meyer et al. reviewed 204,819 patients in the same NSQIP database undergoing one of 16 common major surgeries and found that 35,922 patients (17.54%) had preoperative hypoalbuminemia.18 Out of 85,833 general surgery patients undergoing elective operations, merely 2,088 (2.43%) of patients had low preoperative SA.19 Our cohort of patients sustaining proximal humerus fractures were much more likely to be malnourished than in other elective surgical cohorts described. PHFs are the third leading cause of all fractures and disproportionately affect women more than men, reflecting the role of osteopenia and osteoporosis in the increased rate of fragility fractures.20,21 The prevalence of protein malnutrition is common in this frail, elderly population and is associated with greater bone loss and sarcopenia. Low SA levels have also been described to be associated with fragility fractures22 This likely explains the nearly two-fold higher prevalence of hypoalbuminemia in our patient cohort compared to other common surgeries.
Risk factors for complications after ORIF of proximal humerus fractures include obesity, need for perioperative blood transfusion, late presentations or delay to surgery, and diabetes mellitus.23, 24, 25, 26 Although in elective procedures these risk factors may be modifiable over weeks to months to optimize the patient for surgery, in the setting of fracture fixation in which operative management is recommended within 1–2 weeks, drastic lifestyle changes to minimize risk may not be feasible. Thus, it is essential for the treating physician to evaluate the preoperative SA levels in these patients with PHF and address their nutritional status prior to surgery and during the perioperative period to maximize their outcome and reduce perioperative complications.
In our study, 13% of hypoalbuminemic patients were readmitted which was significantly higher than patients with normal albumin levels which had a 5% readmission rate. Further patients with normal albumin levels had a 3.5-day average length of stay while patients with low albumin levels had an average of 6 days. This outcome is consistent with other studies that demonstrate SA levels are inversely correlated with length of stay after total hip arthroplasty.27, 28, 29, 30 Del Savio et al. showed that hypoalbuminemic patients undergoing a total hip replacement procedure were twice as likely to have a prolonged hospital stay (greater than 15 days) compared to those with normal albumin levels. Comparatively, patients with low and normal albumin levels in 16 major procedures had an average length of stay of 8 and 4 days respectively.18 Additionally, hypoalbuminemic patients undergoing THA were much more likely to have an other comorbid diagnoses, including avascular necrosis of the hip.27
Overall thirty-day rate of any complication in our study cohort was 17.7%, with the subcohort of hypoalbuminemic patients experiencing 29.7% risk of complication compared to 12.1% in normo-albuminemic patients. These complication rates are similar to the 10.8% for normo-albuminemic and 28.9% for hypoalbuminemic patients reported by Dietch et al. who evaluated 85,833 patients undergoing elective surgical procedures.19 In comparison, our study cohort had on average a higher baseline ASA class, indicating patients sustaining proximal humerus fractures also have greater baseline medical comorbidities. In a study conducted by Nussenbaum et al. elective total hip or knee arthroplasty patients were separated into two groups based on those with body mass index ≤35 and albumin ≥3.5. The total complication rates was 35.4% in the hypoalbuminemic patients compared to 14.8% in those with normal albumin levels (P < 0.01).31
One interesting finding in our study was the association of obesity and hypoalbuminemia on complication rates after PHF surgery. Studies have shown overweight and obese patients may have paradoxical malnutrition from eating high calorie foods that lack sufficient nutrition content.32, 33, 34 Thus oftentimes malnutrition is under-recognized and untreated in obese patients. While both malnutrition and obesity may be considered modifiable risk factors, obesity is notoriously difficult for patients to modify.30 Kaidar et al. investigated the prevalence of vitamin deficiencies in the morbidly obese population before undergoing bariatric surgery and found that it is higher and more significant than expected.34 Using the NSQIP database in 2011, Dietch et al. showed that hypoalbuminemia is disproportionately associated with adverse outcomes in obese elective surgical patients.19 Our results show that obese hypoalbuminemic PHF patients had the highest complication rates of 33.3%, suggesting obesity and hypoalbuminemia together may pose a double risk for poor surgical outcomes likely by impeding wound healing. Thus, it appears that nutritional counseling may be of similar importance to weight loss in reducing the risk of postsurgical complications. Because there were no treatments evaluated in this study, no specific recommendations can be made for future treatment options. However, studying the effect of improving nutritional status prior to surgery on postoperative outcomes would be very helpful. Evidence in colorectal surgery has shown that treating malnutrition preoperatively leads to better results.35
Limitations of this study include those of a retrospective review in which individual patient information cannot be identified and accurate surgeon documentation in the electronic medical record is assumed. Other limitations include that not all hospitals collected data on albumin levels so the sample of hospitals in this study was smaller than all hospitals participating in NSQIP. The timing of albumin levels relative to the initial trauma is not available and hence it is unclear when the timing of low albumin levels may affect wound healing. In recognizing these limitations inherent to the NSQIP, the large sample size over a study span of 9 years is advantageous in studying uncommon events such as readmissions, and the random sampling methodology reduces selection bias. Lastly it is unclear whether surgeons chose to treat malnutrition in hypoalbuminemic patients with supplementation or protein shakes and whether or not this affects patient outcome. These aspects of perioperative care remain to be studied and future prospective trials designed to investigate the role of optimizing nutritional status may greatly affect standard of care with regards to preoperative workup. Despite these limitations, it is difficult to track patients in the early postoperative period and thus the 30-day tracking of patients over time is a valuable component of the NSQIP.
5. Conclusion
In this analysis of 916 patients undergoing ORIF for proximal humerus fractures, 31.7% satisfied criteria for hypoalbuminemia. Hypoalbuminemia was independently associated with significantly increased complications and readmissions within 30 days of surgery. Patients who were both obese and hypoalbuminemic were at greatest risk of complication compared to all other analyzed subcohorts.
Declaration of competing interest
No authors report conflicts of interest related to this submission.
References
- 1.Lyons O., Whelan B., Bennett K., O'Riordan D., Silke B. Serum albumin as an outcome predictor in hospital emergency medical admissions. Eur J Intern Med. 2010;21(1):17–20. doi: 10.1016/j.ejim.2009.10.010. [DOI] [PubMed] [Google Scholar]
- 2.Adogwa O., Martin J.R., Huang K. Preoperative serum albumin level as a predictor of postoperative complication after spine fusion. Spine (Phila Pa. 1976;39(18):1513–1519. doi: 10.1097/BRS.0000000000000450. 2014. [DOI] [PubMed] [Google Scholar]
- 3.Gatta A., Verardo A., Bolognesi M. Hypoalbuminemia. Intern Emerg Med. 2012;7(SUPPL. 3):193–199. doi: 10.1007/s11739-012-0802-0. [DOI] [PubMed] [Google Scholar]
- 4.Herrmann F.R., Safran C., Levkoff S.E., Minaker K.L. Serum albumin level on admission as a predictor of death, length of stay, and readmission. Arch Intern Med. 1992;152(1):125–130. [PubMed] [Google Scholar]
- 5.Jellinge M.E., Henriksen D.P., Hallas P., Brabrand M. Hypoalbuminemia is a strong predictor of 30-day all-cause mortality in acutely admitted medical patients: a prospective, observational, cohort study. PLoS One. 2014;9(8) doi: 10.1371/journal.pone.0105983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zusman N.L., Ching A.C., Hart R a, Yoo J.U. Incidence of second cervical vertebral fractures far surpassed the rate predicted by the changing age distribution and growth among elderly United States' persons (2005-2008) Spine. 2012;38(9):1. doi: 10.1097/BRS.0b013e31827ab62a. [DOI] [PubMed] [Google Scholar]
- 7.Cooper B.A., Penne E.L., Bartlett L.H., Pollock C.A. Protein malnutrition and hypoalbuminemia as predictors of vascular events and mortality in ESRD. Am J Kidney Dis. 2004;43(1):61–66. doi: 10.1053/j.ajkd.2003.08.045. [DOI] [PubMed] [Google Scholar]
- 8.Launonen A.P., Lepola V., Saranko A., Flinkkilä T., Laitinen M., Mattila V.M. Epidemiology of proximal humerus fractures. Arch Osteoporos. 2015;10:209. doi: 10.1007/s11657-015-0209-4. [DOI] [PubMed] [Google Scholar]
- 9.Kim S.H., Szabo R.M., Marder R.A. Epidemiology of humerus fractures in the United States: nationwide emergency department sample, 2008. Arthritis Care Res. 2012;64(3):407–414. doi: 10.1002/acr.21563. [DOI] [PubMed] [Google Scholar]
- 10.Chu S.P., Kelsey J.L., Keegan T.H.M. Risk factors for proximal humerus fracture. Am J Epidemiol. 2004;160(4):360–367. doi: 10.1093/aje/kwh224. [DOI] [PubMed] [Google Scholar]
- 11.Kelsey J.L., Browner W.S., Seeley D.G., Nevitt M.C., Cummings S.R. Risk factors for fractures of the distal forearm and proximal humerus. The Study of Osteoporotic Fractures Research Group. Am J Epidemiol. 1992;135:477–489. doi: 10.1093/oxfordjournals.aje.a116314. [DOI] [PubMed] [Google Scholar]
- 12.Lee S.H., Dargent-Molina P., Bréart G. Risk factors for fractures of the proximal humerus: results from the EPIDOS prospective study. J Bone Miner Res. 2002;17(5):817–825. doi: 10.1359/jbmr.2002.17.5.817. [DOI] [PubMed] [Google Scholar]
- 13.Helal B., Su W.S., Churchill D.N., Gangji A.S. Relative hypoparathyroidism and hypoalbuminemia are associated with hip fracture in hemodialysis patients. Clin Nephrol. 2010;73(2):88–93. doi: 10.5414/cnp73088. [DOI] [PubMed] [Google Scholar]
- 14.ACS National Surgical Quality Improvement Program (ACS NSQIP) 2017. American College of Surgeons.https://www.facs.org/quality-programs/acs-nsqip [Google Scholar]
- 15.Garrigues G.E., Johnston P.S., Pepe M.D., Tucker B.S., Ramsey M.L., Austin L.S. Hemiarthroplasty versus reverse total shoulder arthroplasty for acute proximal humerus fractures in elderly patients. Orthopedics. 2012;35(5):e703–e708. doi: 10.3928/01477447-20120426-25. [DOI] [PubMed] [Google Scholar]
- 16.Zhang A.L., Schairer W.W., Feeley B.T. Hospital readmissions after surgical treatment of proximal humerus fractures: is arthroplasty safer than open reduction internal fixation? Clin Orthop Relat Res. 2014;472(8):2317–2324. doi: 10.1007/s11999-014-3613-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McLaughlin M.A., Orosz G.M., Magaziner J. Preoperative status and risk of complications in patients with hip fracture. J Gen Intern Med. 2006;21(3):219–225. doi: 10.1111/j.1525-1497.2006.00318.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Meyer C.P., Rios-Diaz A.J., Dalela D. The association of hypoalbuminemia with early perioperative outcomes - a comprehensive assessment across 16 major procedures. Am J Surg. 2017;214(5):871–883. doi: 10.1016/j.amjsurg.2016.11.023. [DOI] [PubMed] [Google Scholar]
- 19.Dietch Z.C., Guidry C.A., Davies S.W., Sawyer R.G. vol. 11. 2015. Hypoalbuminemia is disproportionately associated with adverse outcomes in obese elective surgical patients; pp. 912–919. (Surgery for Obesity and Related Diseases). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Han R.J., Sing D.C., Feeley B.T., Ma C.B., Zhang A.L. Proximal humerus fragility fractures: recent trends in nonoperative and operative treatment in the Medicare population. J Shoulder Elb Surg. 2016;25(2):256–261. doi: 10.1016/j.jse.2015.07.015. [DOI] [PubMed] [Google Scholar]
- 21.Kannus P., Palvanen M., Niemi S., Parkkari J., Järvinen M., Vuori I. Osteoporotic fractures of the proximal humerus in elderly Finnish persons: sharp increase in 1970-1998 and alarming projections for the new millennium. Acta Orthop Scand. 2000;71(5):465–470. doi: 10.1080/000164700317381144. [DOI] [PubMed] [Google Scholar]
- 22.Chen L.-Y., Liu C.-L., Peng L.-N., Lin M.-H., Chen L.-K. Associative factors of existing fragility fractures among elderly medical inpatients: a hospital-based study. J Clin Gerontol Geriatr. 2012;3(3):94–96. [Google Scholar]
- 23.Berkes M.B., Little M.T.M., Lorich D.G. Open reduction internal fixation of proximal humerus fractures. Curr Rev Musculoskelet Med. 2013;6(1):47–56. doi: 10.1007/s12178-012-9150-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Drosdowech D.S., Faber K.J., Athwal G.S. Open reduction and internal fixation of proximal humerus fractures. Orthop Clin N Am. 2008;39(4):429–439. doi: 10.1016/j.ocl.2008.06.003. [DOI] [PubMed] [Google Scholar]
- 25.Goel D.P., Pike J.M., Athwal G.S. Open reduction and internal fixation of distal humerus fractures. Oper Tech Orthop. 2010;20(1):24–33. [Google Scholar]
- 26.Gerber C., Werner C.M.L., Vienne P. Internal fixation of complex fractures of the proximal humerus. J Bone Joint Surg Br. 2004;86(6):848–855. doi: 10.1302/0301-620x.86b6.14577. [DOI] [PubMed] [Google Scholar]
- 27.Savio G.C., Zelicof S.B., Wexler L.M. Preoperative nutritional status and outcome of elective total hip replacement. Clin Orthop Relat Res. 1996;326:153–161. doi: 10.1097/00003086-199605000-00018. http://www.ncbi.nlm.nih.gov/pubmed/8620636 [DOI] [PubMed] [Google Scholar]
- 28.Nicholson J.A., Dowrick A.S., Liew S.M. Nutritional status and short-term outcome of hip arthroplasty. J Orthop Surg. 2012;20(3):331–335. doi: 10.1177/230949901202000313. [DOI] [PubMed] [Google Scholar]
- 29.Rich M.W., Keller A.J., Schechtman K.B., Marshall W.G., Kouchoukos N.T. Increased complications and prolonged hospital stay in elderly cardiac surgical patients with low serum albumin. Am J Cardiol. 1989;63(11):714–718. doi: 10.1016/0002-9149(89)90257-9. http://www.ncbi.nlm.nih.gov/pubmed/2923060 [DOI] [PubMed] [Google Scholar]
- 30.Ellsworth B., Kamath A.F. Malnutrition and total joint arthroplasty. J Nat Sci. 2016;2(3) http://www.ncbi.nlm.nih.gov/pubmed/27376151%0Ahttp://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=PMC4926871 [PMC free article] [PubMed] [Google Scholar]
- 31.Nussenbaum F.D., Rodriguez-Quintana D., Fish S.M., Green D.M., Cahill C.W. Implementation of preoperative screening criteria lowers infection and complication rates following elective total hip arthroplasty and total knee arthroplasty in a veteran population. J Arthroplast. 2018;33(1):10–13. doi: 10.1016/j.arth.2017.07.031. [DOI] [PubMed] [Google Scholar]
- 32.Markovic T.P., Natoli S.J. Paradoxical nutritional deficiency in overweight and obesity: the importance of nutrient density. Med J Aust. 2009;190(3):149–151. doi: 10.5694/j.1326-5377.2009.tb02319.x. doi:mar10613_fm [pii] [DOI] [PubMed] [Google Scholar]
- 33.Kaidar-Person O., Rosenthal R.J. Malnutrition in morbidly obese patients: fact or fiction? Minerva Chir. 2009;64(3):297–302. [PubMed] [Google Scholar]
- 34.Kaidar-Person O., Person B., Szomstein S., Rosenthal R.J. Nutritional deficiencies in morbidly obese patients: a new form of malnutrition? Part A: Vitamins. Obes Surg. 2008;18(7):870–876. doi: 10.1007/s11695-007-9349-y. [DOI] [PubMed] [Google Scholar]
- 35.Håkonsen S.J., Pedersen P.U., Thomsen T., Bath-Hextall F., Kirkpatrick P., Christensen B.N. Diagnostic accuracy of a validated screening tool for monitoring nutritional status in patients with colorectal cancer: a systematic review protocol. JBI Database Syst Rev Implement Reports. 2013;11(8):186–198. [Google Scholar]