Abstract
Non-standard working hours are associated with negative health outcomes. However, little is known about the early years of exposure to non-standard work hours, or whether workers new to these work schedules perceive their work as impacting their health. This limits our ability to develop meaningful intervention strategies for transitioning into non-standard work hour schedules. This exploratory study investigated whether recent Australian graduates in various non-standard workhour schedules perceive that their work schedule negatively impacts their health. The responses of 120 graduates within four years of completing their tertiary qualification collected from an online survey were analysed. Graduates were asked whether they perceived their work arrangements as impacting their health. Significantly more of those who were engaged in non-standard work schedules or worked beyond contracted hours perceived their working arrangements as having an impact on their health. This study highlights the importance of studying workers’ perceptions of the impact of work hours on health, particularly when workers may be experiencing good global health but be at risk for negative health outcomes in future.
Keywords: Non-standard work schedules, Extended working hours, Work beyond contracted hours, Health risk perception, Australian workforce
Introduction
The Australian workforce is changing, with many workers no longer engaged in traditional models of working hours (i.e. full-time, up to 40-h working week, confined to the daylight hours, Monday to Friday1)). Non-standard work hours are increasingly common, with 16% of Australian workers engaged in shift work2), 37% regularly engaged in evening, overnight or weekend work3) and 24% working on-call4). Further, 42% of full-time workers are working more than 40 h a week5). These arrangements are all considered non-standard work schedules, as they require workers to be available beyond the traditional 9–5, Monday to Friday routine1), or beyond the recommended 38 h week6).
Non-standard work schedules are utilised by businesses as a means to operate more efficiently1). Employees seeking more flexibility to allow for other life commitments are also positive about such arrangements3). For example, an increase in women in the workforce5) has led to both men and women seeking more flexible work hours to balance child rearing and domestic tasks7, 8). Further, an increasing number of Australians are combining work with study9), thus enticing workers to adopt paid employment which accommodates their study commitments.
However, while some benefits are positive, non-standard work schedules can have negative impacts on workers’ health in the medium- to long-term. For example, night shift work has been associated with increased incidence of obesity10,11,12), coronary heart disease13, 14) and diabetes15, 16); workers in on-call working arrangements experience increased stress and decreased mental health17); weekend work has been associated with increased depressive symptoms18) and premature male cardiovascular disease morality19): and extended work hours are associated with chronic health conditions including diabetes20), obesity21), stroke22) and coronary heart disease23). Some research indicates that workers do not feel as impacted by extended hours when the hours are expected24), suggesting that working beyond contracted hours may have a different impact on workers to other non-standard schedules.
While it is evident that non-standard work schedules have an impact on workers’ health, what is not yet well understood is whether workers perceive their working arrangements as impacting their health in the early years of working such schedules. Health risk perception describes the beliefs about risk of potential health consequences and is an important component of health behaviour24). Most major health models assume an element of perceived health risk25). Specifically, to avoid negative health outcomes it is assumed a person can perceive a risk to health. Further, the ability to perceive risk of negative health outcomes is a crucial element of behavioural change26) as individuals who perceive possible health risks are more likely to participate in health protective behaviour24).
While research shows that risk perception is an important factor in predicting health behaviour, people often underestimate their risk of negative health outcomes27, 28). Increasing an individual’s knowledge of a potential risk of health consequence, through risk communication or improved health literacy, has been shown to increase the accuracy of health risk perception29,30,31,32). Thus, explorations into health risk perceptions in workers may provide insight as to whether workers are a) aware of the negative health outcomes associated with non-standard work schedules, and b) whether risk communication or improved health literacy interventions when commencing in a career with non-standard work schedules may be a viable intervention to minimise negative health outcomes.
A population of particular interest are those workers entering into non-standard work schedules as recent graduates. While duration of time spent in non-standard work schedules is associated with adverse health outcomes14, 16), relatively little is known about new graduates who are beginning careers in occupations with higher prevalence of non-standard work schedules such as nursing and paramedics. The study will determine whether workers in this transition perceive they are experiencing negative health impacts early in their post-graduate period and thus whether there is awareness and impetus for intervention to mitigate future negative health outcomes.
This exploratory study aimed to address a current gap in literature around risk perception for health in Australian workers soon after graduation, by exploring a) whether workers perceive their work schedules as impacting their health, and b) whether these perceptions differ by different work hour schedule.
Method
Participants
Recent TAFE and University graduates (within four years of survey) from a regional Australian University were invited to take part in this online survey through an email distributed by the university’s alumni association in February 2018. Participants were directed to an online survey portal which provided a rationale and explanation of the study. Participation in the survey was considered consent, and participants could leave the survey at any stage. The survey was distributed via email to 4,198 Alumni, with a 27.8% open rate, slightly below industry standard of 34.0%33). Of those who opened the survey, the click through rate (CTR) for the survey was 6.0%; slightly above industry standard (5.5%)33). This study was conducted with approval from the CQUniversity Human Research Ethics Committee (Approval number-0000020931).
Measures
Demographic measures
Demographic information was collected including age (yr), gender (male, female, other), type of tertiary study completed (open response), years since graduation (yr), sleep per day (h) and annual income (income brackets). The online survey was developed using questions from the Standard Shiftwork Index34) Australian Bureau of Statistics Census35) and the Housing, Income and Labour Dynamics in Australia (HILDA) Survey36).
Self-reported general health
The self-report health measure was a five point Likert scale. Participants were asked “Would you say that in general your health is: Excellent, Very good, Good, Fair or Poor”37). Health measures were obtained prior to questions relating to work and health to avoid any influence of work related questions biasing this global health measure. For analysis the health measure was collapsed to form a binary outcome of Fair/Good and Very good/Excellent, given the limited number of poor (n=0) and fair (n=7) responses. This dichotomised measure of health was used in a previous study by Artazcoz and colleagues38).
Work Schedule Measures
Non-standard work hours
Type of work schedule was established using questions regarding time of day that participants’ work took place, whether they engaged in shift work, whether they engaged in on-call work and whether they were required to work after hours or on weekends regularly (more than once a month). Participants who indicated that they were regularly engaged in one or more of these forms of non-standard work hours were subsequently categorised as non-standard workers and compared with ‘standard’ workers as a dichotomous outcome variable.
Extended work hours
Participants were asked how many hours they were paid to work per week on average. Due to the small sample size, these hours were categorised into short/average hours (≤38 h) and extended hours (>38 h) based on the recent Fair Work Australia recommendation that working hours should not exceed 38 h per week6) and a previous study within Australian population using this cut-off showing cardiometabolic differences in young workers39). This dichotomised variable allowed sufficient power for exploration between those working the recommended full time (or less) hours and those working in excess of these hours.
Beyond contracted work hours
Participants were asked to indicate how many hours above their contracted hours they usually worked per week. Participants who indicated working any hours beyond contracted hours were considered “Working beyond contracted hours” and those who did not indicate any work beyond contracted hours were considered “Not working beyond contracted hours”.
Self-reported perceptions of work arrangements impact on health
Following the work-related questions, participants were asked how they perceived their work arrangements impacted their health on a five point Likert scale. The health risk perception question was “Do you think your work arrangements impact on your general health? Not at all, Slightly, Moderately, Quite a bit or Extremely”. The perception-based health measure was condensed to form a three category outcome (Not at all, Slightly/Moderately, Quite a bit/Extremely) given the relatively small sample size (n=120). Participants were also given the opportunity to provide a free text response to elaborate on their response to this question, which allowed us to establish that the work schedule impacts were negative rather than positive.
Data analysis
Data were analysed using IBM SPSS v2540) (IBM Corporation, Armonk, NY, USA). Exploratory investigation of the differences in the outcomes of interest by predictors were analysed using the Pearson χ2 statistic. Assumption testing was met using guidelines outlined by Field41). To meet the assumption of independence it was ensure that all entities only contributed to one cell in each analysis. Analyses were checked to ensure that they met minimum expected cell counts.
Results
After removing cases with missing data on the outcomes of interest (n=16), the final sample consisted of n=120 participants, 72.5% (n=87) female and 27.5% (n=33) male with a mean age of 35.7 yr (SD ± 12.2). Participants, on average, completed their degree within the previous 2.2 ( ± 1.0) yr. Within the sample, the range of paid work hours per week was between 2−80 h, (M ± SD = 34.8 ± 12.8) h. Work beyond contracted hours ranged from 1−60 h per week, (M ± SD = 6.4 ± 9.3). As the range was large, responses were checked with corresponding weekly paid hours reported, to ensure they did not exceed a feasible volume of work in a seven-day period. All combinations of weekly hours and work beyond contracted hours were feasible, and retained in the dataset.
Healthcare graduates (including nursing, ultrasound, and paramedic science) represented the majority of participants (61.7%), with engineering graduates (14.7%), and mental health graduates (6.7%) the other prominent groups.
Participants working extended (>38) hours per week represented 29.2% (n=35) of the sample, while 70.0% (n= 84) indicated they worked beyond their contracted hours. Participants engaged in non-standard work schedules represented 60.0% (n=72) of the sample, which is similar to previous research which suggests 55% of Australian employees are engaged in some form of non-standard working time arrangement1). Participant demographic information by standard and non-standard hours is displayed in Table 1.
Table 1. Participant demographics by standard and non-standard working arrangement.
| Participant characteristics | Total | Standard hours(N=48) | Non-standard hours(N=72) | p | Works ≤38 h(N=85) | Works >38 h (N=35) | p | Works beyond contracted hours (No)(N=36) | Works beyond contracted hours (Yes)(N=84) | p | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | N | % | N | % | N | % | N | % | |||||
| Age (yr) | 0.098 | 0.066 | 0.952 | |||||||||||||||
| 18–24 | 34 | 28.3 | 19 | 39.5 | 15 | 20.8 | 22 | 25.9 | 12 | 34.3 | 11 | 30.6 | 23 | 27.4 | ||||
| 25–34 | 25 | 20.9 | 7 | 14.5 | 18 | 25.0 | 16 | 18.8 | 9 | 25.7 | 8 | 22.3 | 17 | 20.2 | ||||
| 35–44 | 27 | 22.5 | 8 | 16.6 | 19 | 26.4 | 18 | 21.2 | 9 | 25.7 | 8 | 22.3 | 19 | 22.6 | ||||
| 45+ | 34 | 28.3 | 14 | 29.2 | 20 | 27.8 | 29 | 34.1 | 5 | 14.3 | 9 | 25.0 | 25 | 29.8 | ||||
| 120 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | |||||||||||
| Gender | 0.243 | 0.001* | 0.196 | |||||||||||||||
| Female | 87 | 72.5 | 32 | 66.7 | 55 | 76.4 | 69 | 81.2 | 18 | 72.5 | 29 | 80.6 | 58 | 69.0 | ||||
| Male | 33 | 27.5 | 16 | 33.3 | 17 | 23.6 | 16 | 18.8 | 17 | 27.5 | 7 | 19.4 | 26 | 31.0 | ||||
| 120 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | |||||||||||
| Level of education | 0.354 | 0.398 | 0.102 | |||||||||||||||
| High School/TAFE | 19 | 15.9 | 8 | 16.7 | 11 | 15.3 | 11 | 12.9 | 8 | 22.9 | 7 | 19.4 | 12 | 14.3 | ||||
| Undergraduate | 78 | 65.0 | 31 | 64.6 | 47 | 65.3 | 58 | 68.3 | 20 | 57.1 | 27 | 75.0 | 51 | 60.7 | ||||
| Postgraduate | 10 | 8.3 | 6 | 12.5 | 4 | 5.5 | 8 | 9.4 | 2 | 5.7 | 1 | 2.8 | 9 | 10.7 | ||||
| Unknown/Missing | 13 | 10.8 | 3 | 6.2 | 10 | 13.9 | 8 | 9.4 | 5 | 14.3 | 1 | 2.8 | 12 | 14.3 | ||||
| 120 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | |||||||||||
| Years since graduation | 0.941 | 0.224 | 0.003* | |||||||||||||||
| 1 yr | 41 | 34.2 | 16 | 33.3 | 25 | 34.7 | 32 | 37.6 | 9 | 25.7 | 21 | 58.3 | 20 | 23.8 | ||||
| 2 yr | 34 | 28.3 | 15 | 31.3 | 19 | 26.4 | 22 | 25.9 | 12 | 34.3 | 7 | 19.4 | 27 | 32.1 | ||||
| 3 yr | 30 | 25.0 | 11 | 22.9 | 19 | 26.4 | 23 | 27.1 | 7 | 20.0 | 6 | 16.7 | 24 | 28.6 | ||||
| 4 yr + | 15 | 12.5 | 6 | 12.5 | 9 | 12.5 | 8 | 9.4 | 7 | 20.0 | 2 | 5.6 | 13 | 15.5 | ||||
| 120 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | |||||||||||
| Income (annual) | 0.152 | 0.008* | 0.002* | |||||||||||||||
| <$40,000 | 31 | 25.8 | 13 | 27.1 | 18 | 25.0 | 24 | 28.2 | 7 | 20.0 | 10 | 27.8 | 21 | 25.0 | ||||
| 40,001–60,000 | 25 | 20.9 | 8 | 16.7 | 17 | 23.6 | 19 | 22.4 | 6 | 17.1 | 5 | 13.8 | 20 | 23.8 | ||||
| 60,001–80,000 | 37 | 30.8 | 16 | 33.3 | 21 | 29.2 | 30 | 35.3 | 7 | 20.0 | 11 | 30.6 | 26 | 31.0 | ||||
| >80,000 | 21 | 17.5 | 6 | 12.5 | 15 | 20.8 | 8 | 9.4 | 13 | 37.1 | 4 | 11.1 | 17 | 20.2 | ||||
| Unknown/Missing | 6 | 5.0 | 5 | 10.4 | 1 | 1.4 | 4 | 4.7 | 2 | 5.8 | 6 | 16.7 | 0 | 0 | ||||
| 120 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | |||||||||||
| Self-reported sleep per night | 0.422 | 0.674 | 0.316 | |||||||||||||||
| <7 h | 27 | 22.5 | 9 | 33.3 | 18 | 66.7 | 20 | 23.5 | 7 | 20.0 | 6 | 16.7 | 21 | 25.0 | ||||
| >7 h | 93 | 77.5 | 39 | 41.9 | 54 | 58.1 | 67 | 76.5 | 28 | 80.0 | 30 | 83.3 | 63 | 75.0 | ||||
| 120 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | |||||||||||
| Working hours per week | 0.153 | - | 0.049* | |||||||||||||||
| ≤38 h | 85 | 70.8 | 37 | 77.1 | 48 | 66.7 | - | - | - | - | 30 | 83.3 | 55 | 65.5 | ||||
| >38 h | 35 | 28.2 | 11 | 22.9 | 24 | 29.2 | - | - | - | - | 6 | 16.7 | 29 | 34.5 | ||||
| 120 | 100 | 100 | 100 | 100 | 100 | |||||||||||||
| Works beyond contracted hours | 0.061 | 0.049* | - | |||||||||||||||
| Yes | 84 | 70.0 | 29 | 60.4 | 55 | 76.4 | 30 | 35.3 | 6 | 17.1 | - | - | - | - | ||||
| No | 36 | 30.0 | 19 | 39.6 | 17 | 23.6 | 55 | 64.7 | 29 | 82.9 | - | - | - | - | ||||
| 120 | 100 | 100 | 100 | 100 | 100 | - | - | |||||||||||
| Self-reported general health | ||||||||||||||||||
| Poor | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | ||||
| Fair | 7 | 5.8 | 1 | 2.1 | 6 | 8.3 | 5 | 5.8 | 2 | 5.8 | 1 | 2.8 | 6 | 7.1 | ||||
| Good | 50 | 41.7 | 18 | 37.5 | 32 | 44.4 | 34 | 40.0 | 16 | 45.7 | 17 | 47.2 | 33 | 39.3 | ||||
| Very good | 51 | 42.5 | 24 | 50.0 | 27 | 37.6 | 40 | 47.1 | 11 | 31.4 | 16 | 44.4 | 35 | 41.7 | ||||
| Excellent | 12 | 10.0 | 5 | 10.4 | 7 | 9.7 | 6 | 7.1 | 6 | 17.1 | 2 | 5.6 | 10 | 11.9 | ||||
| 120 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | |||||||||||
*p-value signifcant at 0.05 level. ^No χ2 performed due to low cell count.
Participants reported good general health with 52.5% (n=63) of graduates reporting Fair—Good health and 47.5% (n=57) reporting Very good—Excellent health. Participants did not differ on self-reported general health outcome by age (p=0.538), gender (p=0.782) or whether they completed a healthcare degree or another degree (p=0.665).
Graduates who had studied a healthcare degree (including; nursing, paramedic science and sonography), were more likely to be engaged in non-standard work hours compared to graduates of all other study fields (χ2(1, n=120) = 13.5, p≤0.001). Graduates of healthcare degrees and graduates of all other types of degrees did not differ in their perception of work impact on health χ2(2, n=113) = 5.2, p=0.073.
Perceived impact of work on health
A significant difference was found in recent graduates’ perceptions of working arrangements impact on health when comparing those participating in standard versus non-standard work schedules overall χ2(2, n=115) = 10.22, p=0.006, see Fig. 1, Panel A.
Fig. 1.
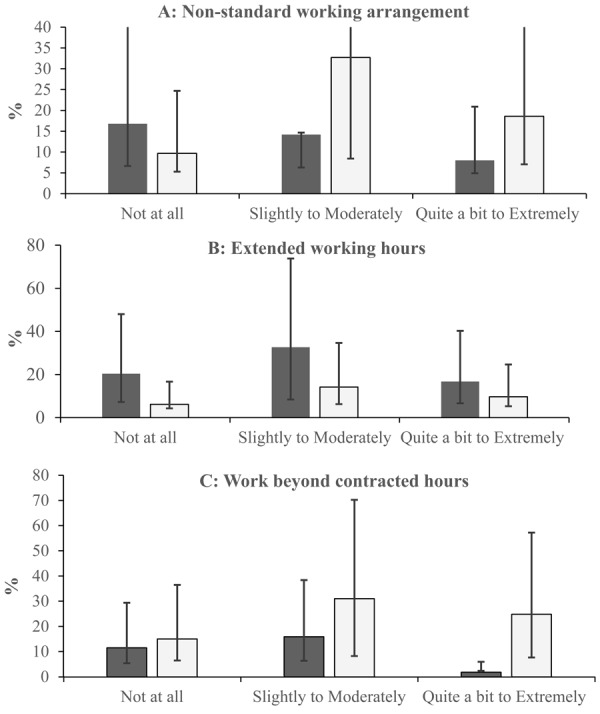
Perceived impact of work arrangement on health between forms of standard (dark grey) vs. non-standard (light grey) work schedules.
Findings are represented as percentage (%) of participants by standard (dark grey) vs. non-standard (light grey) work schedule (Panel A). Those who do not work extended hours (dark grey) vs. those working extended hours (light grey) (Panel B). Those who do not work beyond contracted hours (dark grey) vs. those working beyond contract hours (light grey) (Panel C). Error bars are representative of 95% CI’s.
Comparisons were conducted between different forms of non-standard work schedules. No significant difference in perception of work arrangements impact on health was found when comparing those working extended hours to those who did not work extended hours χ2(2, n=115) = 1.27, p=0.530, see Fig. 1, Panel B.
Graduates who reported working beyond contracted hours reported significantly more perceived impact of working arrangement on health, compared to those who did not report working beyond their contracted hours χ2(2, n=115) = 10.85, p=0.004, see Fig. 1, Panel C.
Just over half (51.6%) of the participants (n=62) within the study choose to answer the free text response to “Do you think your work arrangements impact on your general health?”. These free text responses were used to investigate whether participants had identified work arrangements as impacting their general health in a positive or negative manner. It was established that 98.4% (n=61) of respondents perceived a negative impact of work schedule on their health.
Discussion
The present study aimed to investigate graduates’ perceptions of their work schedules impact on their health, by directly asking for participant perceptions about the impact of their working arrangement on their health. General health, assessed using a standardised self-reported question, was good in this cohort of recent graduates. However, when participants were directly asked if they perceived an impact of their current work arrangements on their health, those engaged in non-standard work schedules and those working beyond contracted hours were more likely to perceive an impact of their working arrangement on their health. These findings suggest that workers are able to perceive the risk of health consequences associated with their work schedules before longer term chronic consequences10,11,12,13,14,15,16,17,18,19,20,21,22,23) emerge, and before they categorise their general health overall as poorer. The free text responses showed that an overwhelming majority of participants felt the impact of work arrangements on their health was negative.
Our findings highlight the importance of health risk perception, as even when general health is reported to be good, graduate employees perceived an impact on their health. Identifying workers early in their career who can identify that work impacts their health may offer an opportunity to intervene and provide support, possibly in the form of risk communication and strategies to mitigate risk. If workers are able to identify a health risk of their work schedule, as seen within this study, communicating the known negative outcomes and preventive actions that can be taken, will likely provide workers an opportunity to minimise the negative impacts of non-standard work schedules. Workers engaged in non-standard work hours, which are known to impact health, who do not perceive health risks may in turn benefit from programs that support the development of improved health literacy.
Graduates engaged in non-standard work schedules perceived their working arrangements as impacting their health more than those working standard schedules. While the difference could be attributed to the large proportion of these non-standard workers being engaged in the health care industry (given the common exposure to stresses and hazards42)) rather than the work schedules specifically, when healthcare graduates were compared to graduates of all other degrees, the graduates did not significantly differ on their perception of working arrangements impact on health. Thus, the relationship cannot be solely explained by being a healthcare graduate.
Graduates who worked beyond their contracted hours perceived their working arrangements as negatively impacting their health compared to graduates who did not work beyond their contracted hours. Previous findings suggest that workers do not feel that extended hours impact their health when they are expecting to work these extended hours24). This suggests that workers’ perception of control over or expectation of working hours may contribute to perceptions about working arrangements impacting their health. While the present study did not consider the degree of control over working hours, or flexibility in the job around working hours, future studies in graduates moving into non-standard work schedules could consider whether workers perceive less impact of overtime hours when they are able to control their working hours.
The study findings should be considered in context of certain limitations. As the study was exploratory the sample is small, impacting our ability to investigate the impact of various forms of extended/short work hours or amount of hours worked beyond contracted hours beyond associations with general health and perceived impact. The study did not ask participants how long they had been in their working arrangement and thus, was unable to rule out influences caused by the amount of time working in certain working arrangement. Another important limitation is the over-representation of healthcare graduates within the sample. The sample consisted of a high percentage of healthcare graduates, likely due to the high volume of healthcare qualifications offered by the university sampled. These graduates are more likely to be engaged in non-standard work schedules, and also exposed to other factors such as repetitive physical work and contractible illness. Further, given their healthcare knowledge, these workers are expected to have a better health literacy level and thus more likely to understand the negative impacts of non-standard work schedules. It would be beneficial to consider these hypotheses in future with a larger and more diverse sample, with concurrent measures of health literacy, to determine whether education type and level of health literacy inform worker perceptions. The study also had an over-representation of female participants, did not collect information regarding the participant’s location and current occupation and thus was unable to account for any possible influences of socio-demographic or occupation-specific risks or exposures. The self-reported perceptions of work arrangements impact on health variable used in this study did not provide participants with the opportunity to provide a direct indication of whether their work impacts their health in a positive or negative manner. While the free text option demonstrates that majority of participants indicated negative impacts on their health, this is an important consideration for the interpretation of the findings as the impact may not be negative for all respondents. For future studies, it will be important to consider the use of a continuous scale for both self-report general health and health risk perception measures, to allow for more thorough exploration including the use of other data analysis techniques and the investigation of possible covariates.
The results of this study highlight the benefit of investigating workers’ health using health risk perception methods, particularly in the post-graduation period where interventions may be viable to minimise future negative health outcomes. This may be particularly crucial while workers are still experiencing good global health but may be at risk for negative health outcomes in the future. It will be important to determine whether early perceptions of work impacts on health translate into poorer health outcomes, as this has not been considered in longitudinal studies. Health risk perceptions may provide an important area of exploration regarding non-standard workers’ health. Further studies of health risk perception in workers engaged in non-standard work schedules will be beneficial, particularly in a longitudinal context, to inform workplace and individual-level interventions for worker health and wellbeing. Importantly, further investigation may allow for development of interventions to minimise the negative health outcomes currently associated with non-standard work schedules.
References
- 1.Venn D. (2003) Non-standard work timing: evidence from the Australian Time Use Survey. Doctoral dissertation, The University of Melbourne, Melbourne, Australia. https://minerva-access.unimelb.edu.au/handle/11343/38890. Accessed June 19, 2018.
- 2.Australian Bureau of Statistics (2013) Working time arrangements, Australia, November 2012. Catalogue No. 6342.0 http://www.abs.gov.au/ausstats/abs@.nsf/Latestproducts/6342.0Main%20Features2Novemb er%202012?opendocument&tabname=Summary&prodno=6342.0&issue=November%202012&num=&view=. Accessed June 1, 2018.
- 3.Venn D, Carey G, Strazdins L, Burgess J. (2016) What explains trends in Australian working-time arrangements in the 2000s? Labour Ind 26, 138–55. [Google Scholar]
- 4.Australian Bureau of Statistics (2016) Characteristics of employment, Australia, August 2015. Catalogue no. 6333.0 http://www.abs.gov.au/ausstats/abs@.nsf/Previousproducts/6333.0Main%20Features2Augu st%202015?opendocument&tabname=Summary&prodno=6333.0&issue=August%202015&num=&view=. Accessed June 1, 2018.
- 5.Barrett S, Burgess J, Campbell I. (2005) The Australian labour market in 2004. J Ind Relat 47, 133–50. [Google Scholar]
- 6.Fair Work Ombudsman (2017). Hours of Work. https://www.fairwork.gov.au/employee-entitlements/hours-of-work-breaks-and-rosters/hours-of-work. Accessed September 14, 2018.
- 7.Siegel C. (2017) Female relative wages, household specialization and fertility. Rev Econ Dyn 24, 152–74. [Google Scholar]
- 8.Drago R, Wooden M, Black D. (2009) Who wants and gets flexibility? Changing work hours preferences and life events. Ind Labor Relat Rev 62, 394–414. [Google Scholar]
- 9.Abhayaratna J, Andrews L, Nuch H, Podbury T (2008) Part time employment: the Australian experience, staff working paper, productivity commission. https://www.pc.gov.au/research/supporting/part-time-employment Accessed November 5, 2018.
- 10.Antunes LC, Levandovski R, Dantas G, Caumo W, Hidalgo MP. (2010) Obesity and shift work: chronobiological aspects. Nutr Res Rev 23, 155–68. [DOI] [PubMed] [Google Scholar]
- 11.Son M, Ye BJ, Kim JI, Kang S, Jung KY. (2015) Association between shift work and obesity according to body fat percentage in Korean wage workers: data from the fourth and the fifth Korea National Health and Nutrition Examination Survey (KNHANES 2008–2011). Ann Occup Environ Med 27, 32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sun M, Feng W, Wang F, Zhang L, Wu Z, Li Z, Zhang B, He Y, Xie S, Li M, Fok JPC, Tse G, Wong MCS, Tang JL, Wong SYS, Vlaanderen J, Evans G, Vermeulen R, Tse LA. (2018) Night shift work exposure profile and obesity: baseline results from a Chinese night shift worker cohort. PLoS One 13, e0196989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Torquati L, Mielke GI, Brown WJ, Kolbe-Alexander T. (2018) Shift work and the risk of cardiovascular disease. A systematic review and meta-analysis including dose-response relationship. Scand J Work Environ Health 44, 229–38. [DOI] [PubMed] [Google Scholar]
- 14.Vetter C, Devore EE, Wegrzyn LR, Massa J, Speizer FE, Kawachi I, Rosner B, Stampfer MJ, Schernhammer ES. (2016) Association between rotating night shift work and risk of coronary heart disease among women. JAMA 315, 1726–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hansen AB, Stayner L, Hansen J, Andersen ZJ. (2016) Night shift work and incidence of diabetes in the Danish Nurse Cohort. Occup Environ Med 73, 262–8. [DOI] [PubMed] [Google Scholar]
- 16.Pan A, Schernhammer ES, Sun Q, Hu FB. (2011) Rotating night shift work and risk of type 2 diabetes: two prospective cohort studies in women. PLoS Med 8, e1001141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nicol AM, Botterill JS. (2004) On-call work and health: a review. Environ Health 3, 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lee HE, Kim HR, Kong JO, Jang TW, Myong JP, Koo JW, Kim I. (2015) Weekend work and depressive symptoms among Korean employees. Chronobiol Int 32, 262–9. [DOI] [PubMed] [Google Scholar]
- 19.Kopp M, Skrabski A, Szántó Z, Siegrist J. (2006) Psychosocial determinants of premature cardiovascular mortality differences within Hungary. J Epidemiol Community Health 60, 782–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gilbert-Ouimet M, Ma H, Glazier R, Brisson C, Mustard C, Smith PM. (2018) Adverse effect of long work hours on incident diabetes in 7065 Ontario workers followed for 12 years. BMJ Open Diabetes Res Care 6, e000496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Di Milia L, Mummery K. (2009) The association between job related factors, short sleep and obesity. Ind Health 47, 363–8. [DOI] [PubMed] [Google Scholar]
- 22.Kivimäki M, Jokela M, Nyberg ST, Singh-Manoux A, Fransson EI, Alfredsson L, Bjorner JB, Borritz M, Burr H, Casini A, Clays E, De Bacquer D, Dragano N, Erbel R, Geuskens GA, Hamer M, Hooftman WE, Houtman IL, Jöckel KH, Kittel F, Knutsson A, Koskenvuo M, Lunau T, Madsen IEH, Nielsen ML, Nordin M, Oksanen T, Pejtersen JH, Pentti J, Rugulies R, Salo P, Shipley MJ, Siegrist J, Steptoe A, Suominen SB, Theorell T, Vahtera J, Westerholm PJM, Westerlund H, O’Reilly D, Kumari M, Batty GD, Ferrie JE,, Virtanen M, IPD-Work Consortium (2015) Long working hours and risk of coronary heart disease and stroke: a systematic review and meta-analysis of published and unpublished data for 603,838 individuals. Lancet 386, 1739–46. [DOI] [PubMed] [Google Scholar]
- 23.Virtanen M, Heikkilä K, Jokela M, Ferrie JE, Batty GD, Vahtera J, Kivimäki M. (2012) Long working hours and coronary heart disease: a systematic review and meta-analysis. Am J Epidemiol 176, 586–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Payne N, Jones F, Harris PR. (2013) Employees’ perceptions of the impact of work on health behaviours. J Health Psychol 18, 887–99. [DOI] [PubMed] [Google Scholar]
- 25.Brewer NT, Chapman GB, Gibbons FX, Gerrard M, McCaul KD, Weinstein ND. (2007) Meta-analysis of the relationship between risk perception and health behavior: the example of vaccination. Health Psychol 26, 136–45. [DOI] [PubMed] [Google Scholar]
- 26.Weinstein ND. (1993) Testing four competing theories of health-protective behavior. Health Psychol 12, 324–33. [DOI] [PubMed] [Google Scholar]
- 27.Leventhal H, Leventhal EA, Cameron L .(2001) Representations, procedures, and affect in illness self-regulation: a perceptual-cognitive model. In: Handbook of health psychology. Baum A, Revenson TA, Singer JE (Eds.), LEA, New Jersey London. [Google Scholar]
- 28.Hwang WJ, Hong O, Kim MJ. (2012) Factors associated with blue-collar workers’ risk perception of cardiovascular disease. J Korean Acad Nurs 42, 1095–104. [DOI] [PubMed] [Google Scholar]
- 29.Winter J, Wuppermann A. (2014) Do they know what is at risk? Health risk perception among the obese. Health Econ 23, 564–85. [DOI] [PubMed] [Google Scholar]
- 30.Cho YJ, Thrasher JF, Swayampakala K, Lipkus I, Hammond D, Cummings KM, Borland R, Yong HH, Hardin JW. (2018) Does adding information on toxic constituents to cigarette pack warnings increase smokers’ perceptions about the health risks of smoking? A longitudinal study in Australia, Canada, Mexico, and the United States. Health Educ Behav 45, 32–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kreuter MW, Strecher VJ. (1995) Changing inaccurate perceptions of health risk: results from a randomized trial. Health Psychol 14, 56–63. [DOI] [PubMed] [Google Scholar]
- 32.Keohane D, Lehane E, Rutherford E, Livingstone V, Kelly L, Kaimkhani S, O’Connell F, Redmond HP, Corrigan MA. (2017) Can an educational application increase risk perception accuracy amongst patients attending a high-risk breast cancer clinic? Breast 32, 192–8. [DOI] [PubMed] [Google Scholar]
- 33.Vision6 Marketing. Email Marketing Metrics Report. https://www.vision6.com.au/metrics/. Accessed May 20, 2019.
- 34.Barton J, Spelten E, Totterdell P, Smith L, Folkard S, Costa G. (1995) The Standard Shiftwork Index: a battery of questionnaires for assessing shiftwork-related problems. Work Stress 9, 4–30. [Google Scholar]
- 35.Australian Bureau of Statistics (2011) Australian labour market statistics, Oct 2010. Catalogue No. 6105.0 http://www.abs.gov.au/ausstats/abs@.nsf/featurearticlesbytitle/67AB5016DD143FA6CA25 8680014A9D9?OpenDocument. Accessed June 19, 2018.
- 36.Drago R, Black W, Wooden D .(2005) The existence and persistence of long work hours https://melbourneinstitute.unimelb.edu.au/assets/documents/hilda-bibliography/working -discussion-research-papers/2005/drago_etal_long_work_hours_IZA.pdf. Accessed July 12, 2018.
- 37.Ware JE, Jr, Gandek B. (1998) Overview of SF-36 health survey and the international quality of life assessment (IQOLA) project. J Clin Epidemiol 51, 903–12. [DOI] [PubMed] [Google Scholar]
- 38.Artazcoz L, Cortès I, Escribà-Agüir V, Cascant L, Villegas R. (2009) Understanding the relationship of long working hours with health status and health-related behaviours. J Epidemiol Community Health 63, 521–7. [DOI] [PubMed] [Google Scholar]
- 39.Reynolds AC, Bucks RS, Paterson JL, Ferguson SA, Mori TA, McArdle N, Straker L, Beilin LJ, Eastwood PR. (2018) Working (longer than) 9 to 5: are there cardiometabolic health risks for young Australian workers who report longer than 38-h working weeks? Int Arch Occup Environ Health 91, 403–12. [DOI] [PubMed] [Google Scholar]
- 40.IBM Corp. (2017) IBM SPSS Statistics for Windows, Version 25.0. IBM Corp, Armonk. [Google Scholar]
- 41.Field AP .(2014) Categorical data. In: Discovering statistics using SPSS (and sex and drugs and rock ‘n’ roll), 4th Ed., SAGE, Los Angeles. [Google Scholar]
- 42.McGrath A, Reid N, Boore J. (2003) Occupational stress in nursing. Int J Nurs Stud 40, 555–65, discussion 567–9. [DOI] [PubMed] [Google Scholar]


