Abstract
Introduction:
The pathophysiology of femoroacetabular impingement (FAI) remains to be better understood, including factors affecting symptom development and disease progression. The purpose of this study was to determine (1) rates of initial and subsequent symptom development in the contralateral hip of patients with symptomatic FAI and (2) to identify predictors of the development of symptomatic contralateral FAI.
Methods:
This prospective study cohort included the contralateral hip of 179 consecutive patients undergoing primary surgical treatment of FAI. At presentation and follow-up time points, patients recorded the presence of symptoms in the contralateral hip. Patients with a minimum of 1 year of follow-up were included in the final cohort. Univariate analysis compared the patient and FAI (cam and pincer) imaging characteristicsof initially asymptomatic patients developing symptoms to those who remained asymptomatic. Kaplan-Meier survival curves were calculated to demonstrate symptom development over time.
Results:
A total of 148 patients (83%) were followed for at least one year time period (mean 2.9 years). Thirty-four (23%) patients presented with initial symptoms in the contralateral hip. Twenty-seven hips (24% of the initially asymptomatic) developed symptoms during the follow-up period at an average of 2.0 years from presentation.
Head-neck offset ratio on the AP pelvis radiograph was significantly lower among hips that developed symptoms (0.163 vs. 0.153 asymptomatic group, p=0.037). Maximum alpha angle (p=0.503), lateral center edge angle (p=0.975), and crossover sign (p=0.865) were not predictive of the development of symptoms. Patients developing contralateral hip symptoms were less likely to have a UCLA activity score of 9 or 10 at presentation (18.2% vs. 43.8%, p=0.032). The total arc of rotation in flexion (IRF + ERF) was significantly decreased in hips developing symptoms (39.4º vs. 50.3º, p=0.012). Kaplan-Meier survival analysis demonstrated 72%, 67%, 56%, and 48% of all patients remaining asymptomatic at 1, 2, 3, and 4 years.
Conclusions:
Approximately one in four patients with FAI presents with symptoms in the contralateral hip and an additional one in four patients develops significant symptoms in the following four years. Several factors, including low activity level, less hip rotational motion, and decreased HNOR, were significantly associated with the development of symptoms, while the alpha angle and crossover sign was not.
Introduction
Osteoarthritis of the hip is a common and disabling condition in the Unites States that is associated with ever-increasing healthcare costs and societal burden.21,9 Over the past decade there has been a remarkable paradigm shift in the understanding of pre-arthritic hip disease with major emphasis on early detection and preventive treatment in the younger patient. Most importantly has been the recognition of femoroacetabular impingement (FAI) as a potential major etiologic factor in pre-arthritic hip dysfunction and subsequent premature osteoarthritis.5
FAI occurs as a result of abnormal bony morphology of the proximal femur and/or acetabulum that leads to repetitive abutment of the femur and acetabulum with hip flexion and rotational activities. The most common form of FAI is known as cam-type impingement, which results from a femoral-sided deformity. Cam-type impingement is commonly caused by asphericity of the anterolateral femoral head, and may result in labral pathology and chondromalacia as this femoral prominence contacts the acetabular-sided structures during activities. Pincer-type impingement occurs secondary to overcoverage of the anterosuperior acetabular rim due to focal overcoverage, acetabular retroversion, or global overcoverage. Patients with symptomatic FAI experience hip pain, diminished hip function, activity restriction, and reduced quality of life.3 In some cases, clinical symptoms worsen and premature hip degeneration ensues.5,15
Abnormal femoral bony morphologies consistent with FAI have a prevalence of 4–25% in the general population, despite only a subgroup of these individuals ever developing hip pain.7,6,1 The athletic population appears to have an even higher prevalence of bony FAI deformity,20 with 70% of professional ice-hockey players having a CAM deformity, in one study.12 Similarly, the radiographic definitions of pincer-type FAI continue to evolve and there is increased recognition that some parameters such as a positive crossover sign can occur as normal variants. 19,11,16 Despite the recent advances in understanding and treating FAI, significant controversy persists regarding the natural history of FAI, and risk factors for disease progression. The contralateral hip represents an opportunity to observe this natural history in a high-risk population for the development of hip symptoms, secondary to patient-specific factors that may have played a role in the development of ipsilateral hip symptoms. The contralateral extremity has previously been a valuable model for the natural history of various orthopaedic conditions.14,23 In addition, the risk of developing a symptomatic contralateral hip is valuable prognostic information in an elite athlete who is contemplating secondary surgery and return-to-play.
The purpose of the current study was to determine rates of symptom development in the contralateral hip of FAI patients and to identify predictors of the development of these symptoms over time.
Methods
A cohort of 195 consecutive patients undergoing hip preservation surgery for symptomatic and idiopathic FAI (cam or combined cam/pincer) was prospectively enrolled in a research database of a single surgeon from 1/31/2011 – 12/31/2013. Institutional Review Board approval was obtained prior to initiation of this study. A portion of the work in this study was supported by NIH grant (UL1 TR000448). The hip that was not receiving surgery (contralateral hip) was the focus of this study. Exclusion criteria included contralateral hips that had either: previous hip surgery, significant evidence of radiographic osteoarthritis (Tonnis osteoarthritis grade ≥2) at baseline, or a history of childhood hip disorder such as Legg-Calve-Perthes disease or Slipped Capital Femoral Epiphysis.
Bony morphology of the contralateral hip was assessed with standing AP pelvis and 45-degree Dunn radiographs obtained according to standardized protocols.2 Incomplete imaging resulted in the exclusion of 16 patients (8%) [179 patients remaining]. All patients had failed a minimum three-month conservative treatment trial prior to surgical intervention. At the preoperative visit, clinical information including history, physical examination findings, sports participation, patient-rated outcome measures such as the modified Harris Hip Score and UCLA Activity score was recorded. Pain in the contralateral hip was assessed at baseline and each follow-up time point utilizing the pain component of the modified Harris hip scope specific to each hip. Routine follow-up for these patients typically occurred at 1, 2, and 5 years following the surgical intervention on the initially symptomatic hip, or at any clinical visit occurring during this time period. When clinical follow-up was not completed, phone follow-up and mailed questionnaire packets were utilized (6 cases; 4%).
At baseline and postoperative follow-up time points, patients recorded standardized outcome questionnaires, including the presence of symptoms in their contralateral hip. Pain was characterized as none, slight, mild, moderate, severe, or disabling. Significant symptoms necessitated the presence of at least moderate pain, while none, mild, or slight pain was not included. Patients developing symptoms in the contralateral hip were subclassified as having symptoms at presentation (initial symptoms) or developing symptoms during the follow-up period (developed symptoms).
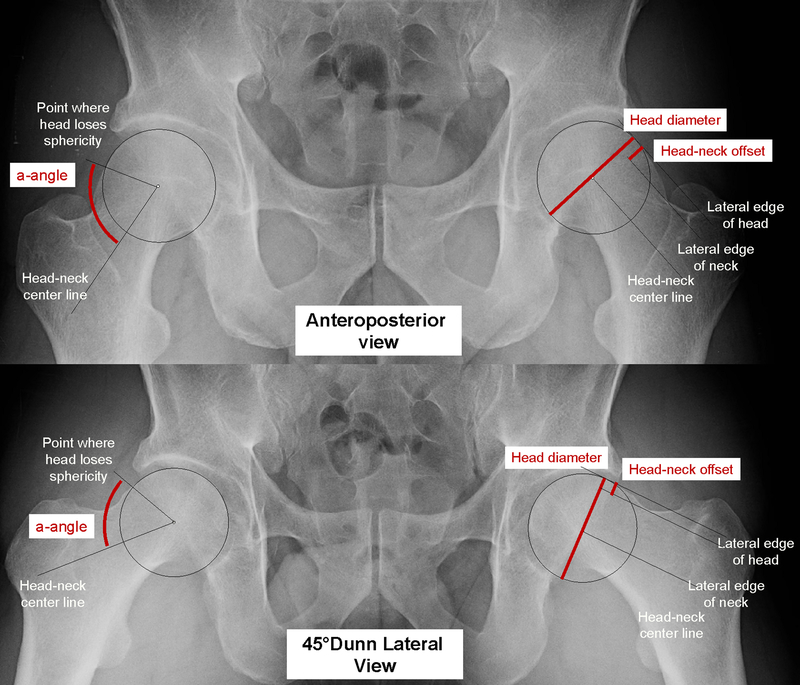
Alpha-angle of Nötzli22 and head-neck offset ratio (HNOR) were measured on the 45° Dunn and AP pelvis radiographs to characterize the severity of the femoral cam morphology (Figure 1). Additionally, the lateral center edge angle (LCEA) and acetabular inclination (AI)were assessed on AP pelvis radiographs. The presence of a positive crossover sign, LCEA ≥ 40°, or AI < 0° were assessed as markers of pincer morphology. Radiographic measurements were made using the OsiriX MD viewer (Pixmeo, Geneva Switzerland) and Orthopaedic Studio plugin (Spectronic, Helsingborg, Sweden) by a single reader with de-identified radiographs. Intraobserver reliability was assessed by comparing the reader’s measurements made on a subset of 20 patients during two separate occasions, two weeks apart. Accuracy of radiographic measurements was determined using intraclass correlation coefficients (ICCs) for continuous measurements. ICCs were calculated using a two-way random model for single measurement with absolute testing. Intraobserver agreement was moderate to very high (ICC 0.67 and 0.91) in measurement of α-Angle on the AP and 45° Dunn view, respectively. Intraobserver agreement was high to very high (ICC 0.80 and 0.90) in measurement of HNOR on the AP and 45° Dunn view, respectively. The interobserver and intraobserver reliability of the LCEA, AI, and crossover sign has been previously established.18
Figure 1:
Demonstration of the anteroposterior (AP) and 45º Dunn radiographic views as well as the primary radiographic measurements made. Head-neck offset ratio (HNOR) is calculated as the ratio of head-neck offset to femoral head diameter.
All patients with a minimum follow-up of at least one year after presentation were included in the current study. The time to symptom development in the contralateral hip was recorded, with a time of zero indicating symptom presence in the contralateral hip at initial completion of the questionnaire. Symptom development in the contralateral hip was not considered during the initial 6 weeks of the perioperative period.
Statistics
The study cohort was characterized using standard descriptive statistics. Univariate analysis was used to determine factors significantly associated with symptom development among the group that was initially asymptomatic. Kaplan-Meier survival analysis was performed for symptom development in the contralateral hip as a function of time in years. A p-value less than 0.05 was considered significant.
Results
A total of 148 patients (83%) were followed for at least one year time period after enrollment (mean 2.9 years; range 1.0–6.6 years) and comprised the final cohort. The study cohort had a mean age of 30.9 years and included 65.2% females. The mean alpha angle of the contralateral hip on AP pelvis and 45º Dunn views was 66.4 and 61.5 degrees, respectively.
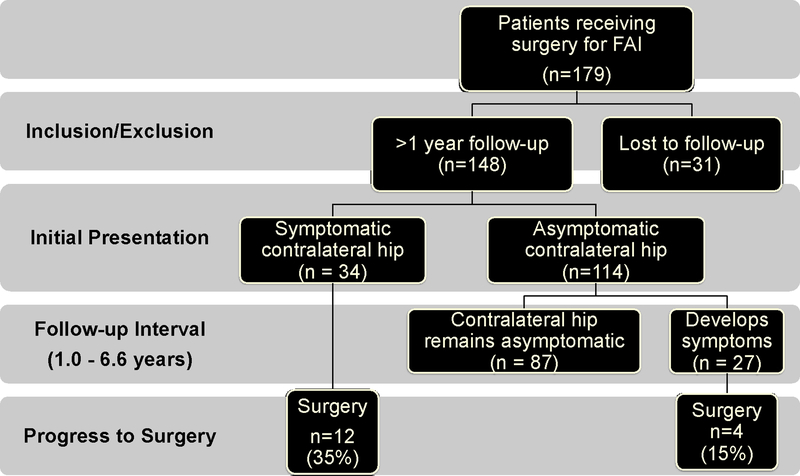
Thirty-four patients (23%) presented with initial symptoms in the contralateral hip. Figure 2 summarizes the frequency of initial symptoms and the development of symptoms over time for the entire cohort. One hundred and fourteen patients (77%) did not report significant symptoms in their contralateral hip at presentation. Twenty-seven hips (24% of the initially asymptomatic) developed symptoms during the follow-up period at an average of 2.0 years (Std Dev. 1.28 years) from presentation. Table 1 compares the subgroup of patients that developed symptoms over the course of the study to those that remained asymptomatic. Sixteen (11%) patients underwent contralateral hip procedures during the follow-up period and included 35% of those with symptoms at presentation and 15% of those that developed symptoms since presentation.
Figure 2:
Flowchart demonstrating cohort characteristics
Table 1:
Univariate analysis of initially asymptomatic hips comparing those that develop symptoms to those that remained asymptomatic. P-values <0.05 are considered significant and are in bold.
| Symptomatic n=27 (range) | Asymptomatic n=87 (range) | P-value | |
|---|---|---|---|
| Age | 31.8 | 30.1 | 0.549 |
| Male* | 51.9% | 34.5% | 0.105 |
| BMI | 24.2 | 24.4 | 0.871 |
| Follow-up interval (years) | 2.76 | 2.78 | 0.939 |
| Radiographs | |||
| Maximum α-angle (AP or Dunn) | 70.3° (43.8–97.8°) | 72.7° (40.2–103.8°) | 0.503 |
| Head-Neck Offset Ratio AP | 0.153 | 0.163 | 0.027 |
| Head-Neck Offset Ratio Dunn | 0.149 | 0.155 | 0.209 |
| Lateral center edge angle (LCEA) | 29.3° (15.3°−44.0°) |
29.3 (14.5°−49.6°) |
0.978 |
| LCEA ≥ 40 | 7.4% | 8.0% | 1.000 |
| Acetabular inclination (AI) | 5.3° (−1.4°−18.6°) | 6.6° (−12.0°−15.8°) | 0.212 |
| AI < 0 | 7.4% | 8.0% | 1.000 |
| Crossover sign (% positive) | 25.9% | 27.6% | 0.865 |
| UCLA Activity Score ≥ 9* | 18.2% | 43.8% | 0.032 |
| Range of Motion | |||
| Total Arc of Rotation: Extension | 42.8° (10–70°) | 46.2° (20–110°) | 0.320 |
| Total Arc of Rotation: 90° Flexion | 39.4° (15–80°) | 50.4 (15–110°) | 0.012 |
| Internal Rotation in 90° Flexion | 10.7° (−5–30°) |
14.3° (0–50°) |
0.096 |
Groups compared with Student’s t-test unless otherwise noted;
Chi-squared test
Percentage of male patients did not significantly differ between symptomatic and asymptomatic groups (51.9% vs. 34.5%, respectively; 0.105). Head-neck offset ratio on the AP pelvis radiograph was significantly lower among hips that developed symptoms (0.163 vs. 0.153 asymptomatic group, p=0.037). Maximum alpha angle (either AP or Dunn) was not predictive of the development of symptoms during this timeframe (72.7º symptomatic vs. 70.3º asymptomatic; p=0.503). The lateral center edge angle (p=0.975), and crossover sign (p=0.865) were not associated with the development of symptoms. Similarly, a LCEA greater than or equal to 40 degrees or AI less than 0 (both p = 1.0) were also not associated with symptom development. Patients with a UCLA activity score of 9 or 10 at presentation were less prevalent in the symptomatic group (18.2% vs. 43.8% asymptomatic group, p=0.032). The mean hip internal rotation in 90 degrees of flexion (IRF) in hips developing symptoms was 10.7 degrees, compared to 14.3 degrees among hips remaining asymptomatic (p=0.096). The total arc of rotation in flexion (IRF + external rotation in flexion, ERF) was significantly decreased in hips developing symptoms (39.4º vs. 50.3º asymptomatic, p=0.012).
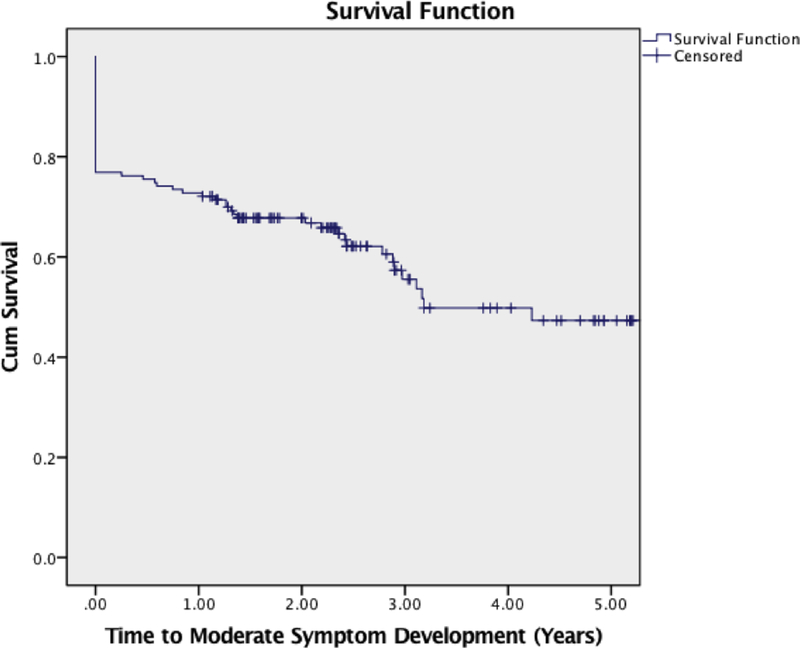
Kaplan-Meier Survival analysis (Figure 3) demonstrates the percentage of patients who remain symptom free at specified time intervals. At 1, 2, 3, and 4 years, 72%, 67%, 56%, and 48% of all patients remained asymptomatic in their contralateral hip, respectively.
Figure 3:
Kaplan-Meier analysis of symptom-free survival of the contralateral hip.
Discussion
The natural history of FAI remains to be better defined. Structural abnormalities predisposing to symptomatic FAI commonly affect both hips, although may only be associated with symptoms in one hip at the time of presentation. The prognosis of the contralateral hip is largely unknown. Athletes with bilateral deformity often inquire about their risk of contralateral FAI symptoms if they have progressed to have surgery in one hip already. Prognosis of the contralateral hip may affect timing of interventions, and in the case of professional athletes can affect contract decisions and livelihood. The current study investigated the frequency of short-term (mean 2.9, range 1.0–6.6 years) symptom development in the contralateral hip for patients who present with unilateral symptoms from FAI. Patient-specific factors such as radiographic deformity, range-of-motion, and activity level were found to influence the onset of symptoms.
Patient-specific factors affecting symptom development in FAI have not yet been well characterized. In a retrospective study of 113 patients with symptomatic FAI in one hip, Allen et al. looked at the contralateral hip and found a 78% prevalence of contralateral cam deformity, however only 26% of those patients were symptomatic at presentation.1 They found that an alpha angle > 60º (on the Dunn lateral projection) increased the chances of having a symptomatic lesion. They did not correlate symptom development to other patient factors other than radiographic deformity. In another retrospective review of over 600 patients over a 2-year period, Klingenstein et al. compared a cohort of patients receiving bilateral (staged) FAI surgery to those undergoing primary unilateral FAI surgery.10 In a multivariate logistic regression model, younger age, male patients, higher alpha angles, and decreased acetabular anteversion were associated with higher risk of bilateral surgery. Our study is limited by inability to account for symptoms in individuals that do not obtain surgery (or obtain surgery outside the study institution or time-frame). The cross-sectional nature of both these studies does not allow for evaluation of symptom development over time.
In our study, we examined radiographic and clinical data for patients who presented with an unaffected hip but went on to develop symptoms. It should be noted that this cohort does not represent the “general” population, as these patients are at increased risk for developing symptomatic FAI in their contralateral hip by virtue of having the disease in their other hip. However, due to the high-risk nature of our cohort, we see symptomatic “events” at a higher rate, which improves ease of study and characterization. These findings are at least applicable to patients with known FAI in their other hip, and still may have important implications for the general population
We found that structural anomalies in the femur, specifically a lack of head-neck offset (represented by decreased HNOR), was a risk factor for developing symptoms in our cohort. Ito et. al. used radial-cut MRI to characterize the femoral neck of symptomatic FAI patients and determined that decreased head-neck offset in the anterolateral aspect of the femur was commonly seen in those with labral damage.8 This seems to be a separate clinical deformity from the aspherical femoral head (as measured by the alpha angle) – though both are implicated in cam-type impingement. The aforementioned studies examining the contralateral hip in FAI patients did not measure HNOR, although both did find that an increasing alpha-angle was a risk factor for bilateral disease, with the Allen et. al. study citing a cutoff of 60 degrees.1,10 We did not find alpha-angle to be a significant determinant of symptom development in this cohort. It is possible that we were not powered to make this determination and the HNOR simply has a larger effect size and was more visible in a smaller cohort over a shorter timeframe. It is also possible that our study population, for unspecified reasons, has more severe deformities (alpha-angles averaging over 70º) such that any effect due to a small difference between cohorts is relatively muted. Additionally, parameters of pincer-type morphology, including LCEA, AI, and crossover sign, showed no association with symptom development.
Dynamic hip mechanics are thought to play a role in FAI pathology, although the exact etiologies and mechanisms are debated. This study demonstrates that a lower activity level and a decreased range of motion in 90º of flexion can be risk factors for bilateral symptom development. Range of motion in flexion is thought to be limited by the bony anatomy of the hip joint, which includes (but is not limited to) femoral head deformity, femoral neck offset, femoral version, as well as acetabular coverage and version. Therefore, a patient’s range of motion prior to abutment of the femur and acetabulum may be a reasonable surrogate for judging whether his or her anatomy, as a whole, predisposes to developing FAI. Our results would support this reasoning, as those patients with more limited motion were at-risk for symptomatic progression. Similarly, we expected that increased athletic demands on the hip would also predispose to FAI symptoms as those patients would be more likely to reach the extremes of motion that their hip joint allows. Instead, we found that high activity levels at presentation were protective of contralateral hip symptom development. It may be that the conditioning of the hip is improved in these patients, which can deter the onset of symptoms through mechanisms we do not fully understand. Another theory is that there is a subgroup of the less active patients who have sub-clinical dysfunction of their contralateral hip that is masked by their inactivity, and then later exposed once their symptomatic disease is addressed.
Despite the advantages and novelty of these findings, this study has several limitations. The short-term nature of the follow-up (1–6.6 years) makes the current study only preliminary in regards to the ultimate status of the contralateral hip. Longer-term follow-up would be useful for monitoring progression to future hip surgery or hip osteoarthritis. Additionally, we included moderate symptoms in the primary analysis, rather than including minimal or slight symptoms. These milder symptoms may resolve or indeed progress to worse symptoms at later time points. Finally, there are limitations due to our radiographic analysis techniques. Adequate visualization and measurement of proximal femur abnormalities is dependent on radiographic technique and also location of a particular morphology.2,19 Anteroposterior pelvis radiographs will better visualize morphologies located on the lateral femoral neck, whereas lateral views (such as the frog lateral) offer superior visualization of the anterior femoral neck.4 The 45º Dunn radiograph, with a position between these two extremes, has been shown to offer the best visualization of cam morphology in the characteristic anterolateral neck location and correlated well to CT imaging.13,17 Due to readily available anteroposterior and 45º Dunn views of the contralateral hip when imaging a symptomatic hip, we are able to characterize morphology in the most common locations in the contralateral hip. We also chose to focus on femoral-sided morphology with our analysis, and we did not include patients with an isolated pincer mechanism in our cohort. Primarily, we believe that pure pincer morphologies represent a smaller subgroup of overall FAI patients that may have different risk-factors for progression than those with cam FAI, and thus we chose to not study them together. In addition, consistent characterization of pincer morphology is made difficult by variations in pelvic position and technique, which would further complicate analysis.
The current study prospectively investigates the development of symptoms in the contralateral hip of patients with symptomatic FAI undergoing surgical intervention. Approximately 23% of patients report moderate contralateral symptoms at the time of presentation. Over the following four years, an additional 29% (total 52%) develop moderate contralateral symptoms. Patients with higher activity levels, a larger arc of motion in flexion, and with increased offset (HNOR) as measured on AP pelvis radiographs were less likely to develop symptoms during the study period. These results can assist both the clinician and patient with short-term and mid-term prognostic information and may facilitate treatment decision-making for the contralateral asymptomatic hip. Further research into the associated risk factors could offer insight into pathophysiology of symptom development as well as inform prevention strategies.
What Is Known About This Subject:
Cam-type FAI has been demonstrated to be a risk factor for hip osteoarthritis, but many patients with underlying cam morphology will never develop hip symptoms. Very little is known regarding the role of patient-specific characteristics on the pathophysiology of FAI.
What This Study Adds To Existing Knowledge:
The current prospective study demonstrates that 23% of FAI patients present with symptoms in the contralateral hip, while an additional 29% will develop significant symptoms over the next 4 years. Patient-specific factors including activity level, amount of hip rotation, and head-neck offset appear to play a role in the development of symptoms.
References
- 1.Allen D, Beaulé PE, Ramadan O, Doucette S. Prevalence of associated deformities and hip pain in patients with cam-type femoroacetabular impingement. J Bone Joint Surg Br. 2009;91(5):589–594. doi: 10.1302/0301-620X.91B5.22028. [DOI] [PubMed] [Google Scholar]
- 2.Clohisy JC, Carlisle JC, Beaulé PE, et al. A systematic approach to the plain radiographic evaluation of the young adult hip. J Bone Joint Surg Am. 2008;90 Suppl 4:47–66. doi: 10.2106/JBJS.H.00756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Clohisy JC, Knaus ER, Hunt DM, Lesher JM, Harris-Hayes M, Prather H. Clinical presentation of patients with symptomatic anterior hip impingement. Clin Orthop. 2009;467(3):638–644. doi: 10.1007/s11999-008-0680-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Clohisy JC, Nunley RM, Otto RJ, Schoenecker PL. The frog-leg lateral radiograph accurately visualized hip cam impingement abnormalities. Clin Orthop. 2007;462:115–121. doi: 10.1097/BLO.0b013e3180f60b53. [DOI] [PubMed] [Google Scholar]
- 5.Ganz R, Parvizi J, Beck M, Leunig M, Nötzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop. 2003;(417):112–120. doi: 10.1097/01.blo.0000096804.78689.c2. [DOI] [PubMed] [Google Scholar]
- 6.Gosvig KK, Jacobsen S, Sonne-Holm S, Gebuhr P. The prevalence of cam-type deformity of the hip joint: a survey of 4151 subjects of the Copenhagen Osteoarthritis Study. Acta Radiol Stockh Swed 1987. 2008;49(4):436–441. doi: 10.1080/02841850801935567. [DOI] [PubMed] [Google Scholar]
- 7.Hack K, Di Primio G, Rakhra K, Beaulé PE. Prevalence of cam-type femoroacetabular impingement morphology in asymptomatic volunteers. J Bone Joint Surg Am. 2010;92(14):2436–2444. doi: 10.2106/JBJS.J.01280. [DOI] [PubMed] [Google Scholar]
- 8.Ito K, Minka-II M-A, Leunig M, Werlen S, Ganz R. Femoroacetabular impingement and the cam-effect. Bone Jt J. 2001;83-B(2):171–176. doi: 10.1302/0301-620X.83B2.11092. [DOI] [PubMed] [Google Scholar]
- 9.Jordan JM, Helmick CG, Renner JB, et al. Prevalence of hip symptoms and radiographic and symptomatic hip osteoarthritis in African Americans and Caucasians: the Johnston County Osteoarthritis Project. J Rheumatol. 2009;36(4):809–815. doi: 10.3899/jrheum.080677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Klingenstein GG, Zbeda RM, Bedi A, Magennis E, Kelly BT. Prevalence and preoperative demographic and radiographic predictors of bilateral femoroacetabular impingement. Am J Sports Med. 2013;41(4):762–768. doi: 10.1177/0363546513476854. [DOI] [PubMed] [Google Scholar]
- 11.Larson CM, Moreau-Gaudry A, Kelly BT, Byrd JW, Tonetti J, Lavalee S, Chabanas L, Barrier G, Bedi A. Are normal hips being labeled as pathologic? A CT-based method for defining normal acetabular coverage. Clin Orthop Relat Res. 2015;473(4):1247–1254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lerebours F, Robertson W, Neri B, Schulz B, Youm T, Limpisvasti O. Prevalence of Cam-Type Morphology in Elite Ice Hockey Players. Am J Sports Med. 2016;44(4):1024–1030. doi: 10.1177/0363546515624671. [DOI] [PubMed] [Google Scholar]
- 13.Meyer DC, Beck M, Ellis T, Ganz R, Leunig M. Comparison of six radiographic projections to assess femoral head/neck asphericity. Clin Orthop. 2006;445:181–185. doi: 10.1097/01.blo.0000201168.72388.24. [DOI] [PubMed] [Google Scholar]
- 14.Murphy SB, Ganz R, Müller ME. The prognosis in untreated dysplasia of the hip. A study of radiographic factors that predict the outcome. J Bone Joint Surg Am. 1995;77(7):985–989. [DOI] [PubMed] [Google Scholar]
- 15.Nepple JJ, Carlisle JC, Nunley RM, Clohisy JC. Clinical and radiographic predictors of intra-articular hip disease in arthroscopy. Am J Sports Med. 2011;39(2):296–303. doi: 10.1177/0363546510384787. [DOI] [PubMed] [Google Scholar]
- 16.Nepple JJ, Lehmann CL, Ross JR, Schoenecker PL, Clohisy JC. Coxa profunda is not a useful radiographic parameter for diagnosing pincer-type femoroacetabular impingement. J Bone Joint Surg. 2013;95(5):417–423. [DOI] [PubMed] [Google Scholar]
- 17.Nepple JJ, Martell JM, Kim YJ, Zaltz I., Clohisy JC, ANCHOR Study Group.. Do plain radiographs correlate with CT for imaging of cam-type femoroacetabular impingement? Clinical Orthopaedics and Related Research®, 470(12), 3313–3320. 10.1007/s11999-012-2510-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nepple JJ, Martell JM, Kim YJ, Zaltz I, Millis MB, Podeszwa DA, Sucato DJ, Sink EL, Clohisy JC, ANCHOR Study Group. Interobserver and intraobserver reliability of the radiographic analysis of femoroacetabular impingement and dysplasia using computer-assisted measurements. Am J Sports Med. 2014;42(10):2393–2401. [DOI] [PubMed] [Google Scholar]
- 19.Nepple JJ, Prather H, Trousdale RT, et al. Diagnostic imaging of femoroacetabular impingement. J Am Acad Orthop Surg. 2013;21 Suppl 1:S20–S26. doi: 10.5435/JAAOS-21-07-S20. [DOI] [PubMed] [Google Scholar]
- 20.Nepple JJ, Vigdorchik JM, Clohisy JC. What Is the Association Between Sports Participation and the Development of Proximal Femoral Cam Deformity? A Systematic Review and Meta-analysis. Am J Sports Med. 2015;43(11):2833–2840. doi: 10.1177/0363546514563909. [DOI] [PubMed] [Google Scholar]
- 21.Nho SJ, Kymes SM, Callaghan JJ, Felson DT. The Burden of Hip Osteoarthritis in the United States: Epidemiologic and Economic Considerations. J Am Acad Orthop Surg. 2013;21(suppl):S1–S6. doi: 10.5435/JAAOS-21-07-S1. [DOI] [PubMed] [Google Scholar]
- 22.Nötzli HP, Wyss TF, Stoecklin CH, Schmid MR, Treiber K, Hodler J. The contour of the femoral head-neck junction as a predictor for the risk of anterior impingement. J Bone Joint Surg Br. 2002;84(4):556–560. [DOI] [PubMed] [Google Scholar]
- 23.Yamaguchi K, Tetro AM, Blam O, Evanoff BA, Teefey SA, Middleton WD. Natural history of asymptomatic rotator cuff tears: a longitudinal analysis of asymptomatic tears detected sonographically. J Shoulder Elbow Surg. 2001;10(3):199–203. doi: 10.1067/mse.2001.113086. [DOI] [PubMed] [Google Scholar]