Abstract
Background:
Treatment demand for cannabis use disorders is increasing in Europe. Mobile phone– and internet-based interventions for cannabis users can possibly help meet the need. The purpose of this study was to examine whether a recently developed Norwegian Cannabis Cessation app reaches a broader or different user group compared to community-based Cannabis Cessation programs (CCP, Nordic abbreviation: HAP).
Method:
The app respondents (n = 148) were recruited through an online link in the app. A comparative sample (n = 102) was recruited in three municipally based CCPs in Norway. We examined whether app users differed from the CCP population in sociodemographics, substance use, mental health, and well-being.
Result:
The app group included more women than the CCP group (46% versus 26%, χ2 = 10.9, P = .001), but otherwise the groups were similar for sociodemographic variables. Severity of cannabis use did not differ between groups, but the app sample exhibited a higher depressiveness score on the Hopkins Symptom Checklist (mean difference, 0.24; 95% CI 0.04–0.44; P = .018) and lower perceived well-being (3.4 point lower score on the Outcome Rating Scale; 95% CI −5.7 to −1.2; P = .003). Well-being was negatively associated with being in the app group, being older, and having higher levels of mental distress, and was positively associated with the perceived ability to make changes (‘self-efficacy of quitting’).
Conclusion:
The higher proportion of women in the app group indicated that the app did capture an expanded segment of the cannabis-using population. The app can be an alternative for those who are not yet prepared to seek treatment in formal healthcare services. The high level of depressive symptoms and lower levels of well-being among the app respondents suggest that some app users might need additional support.
Keywords: cannabis, cannabis use disorder, substance related disorders, mobile application, smartphone, well-being, Norway
Background
Cannabis is the regulated drug most likely to be used by European youths. In 2015, an estimated 17.2 million young adults (aged 15–34), or 14.1% of this age group, had used cannabis in the last year.1 A cannabis use disorder (CUD) may exist when use continues despite negative consequences and causes significant distress or functional impairment.2,3 Having a CUD is typically associated with a concurrent substance use disorder (SUD) diagnosis, higher levels of anxiety and depression, and lower levels of well-being.4–6 When first presenting to formal treatment services, patients with a CUD also tend to have a lower educational level and worse employment status compared to matched unaffected controls.6 In EU countries, the proportion of clients with cannabis-related problems entering specialized drug treatment increased from 20% in 2006 to one third of all drug treatment patients in 2015.1 The increase needs to be understood in the context of service provision and referral practice. However, the primary psychoactive compound tetrahydrocannabinol (THC) also may be a factor. THC content has trended upward in confiscated cannabis products in some European countries, including Norway, and the higher THC content has likely heightened the addictive potential of cannabis.7
In Norway, the prevalence of cannabis use in young adults is among the lowest in Europe, with 9% in the 15–34-year age group reporting using cannabis in the last year.8 Of concern, though, is a recent national report indicating that the rate is rising. The numbers of high school students reporting cannabis use increased from 13% in 2015 to 16% in 2017 for boys and from 8.7% to 9.3% for girls.9 In Oslo, the increase was steeper, from 10% in 2015 to 17% in 2018 among boys and from 5% to 9% for girls.10 Similar to the situation in Europe as a whole, the number of patients with a CUD as their principal diagnosis in Norwegian specialist treatment centers increased 36% during 2009–2014.7
In light of the large scale of the problem and increased treatment-seeking because of CUD, the World Health Organization has suggested that mobile phone and internet-based interventions could help mitigate the demand for formal treatment services and possibly reach groups who typically forgo formal services.11 These technology solutions offered via mobile phones are referred to as ‘m-health’ or ‘mobile-health’. They offer many obvious advantages, including easier treatment access, encouragement of self-management, and cost-effectiveness. Their efficacy in reducing alcohol and other substance use has proved promising.12 Such interventions may be effective in reducing substance abuse among people with mild to moderate problems.13,14 However, few apps for cannabis cessation are available,15 and to our knowledge, none have been previously available in Norway.
Objectives
This paper will briefly describe the development of a Norwegian smartphone app intended to help individuals reduce or quit their use of cannabis. The overall purpose was to examine whether those downloading and using the app differed in sociodemographics, substance use, mental health, and well-being compared with a sample presenting for community-based, individual therapy sessions. The results are expected to indicate whether the app reached a broader user group than does face-to-face therapy. The rationale for the comparison was that the two interventions are based on the same treatment manual, enabling us to identify delivery mode as the major difference between samples. A plausible expectation was that persons who approached face-to-face services would have more severe problems than those who sought out the app. We also examined factors associated with well-being in the sample.
Methods
Development of a cannabis cessation app in Norway
The development of the cannabis cessation app (in Norwegian: HAP-app) was carried out by the City Centre Outreach Service in Oslo and the National Drug Helpline in Norway.16 The app was developed based on a manual for individual outpatient therapy, the ‘Cannabis Cessation Program’ (CCP, Nordic abbreviation: HAP), developed by Lundqvist and Ericsson.17 CCP is based on principles from cognitive therapy, motivational interviewing, and psychoeducation.18 The program period extends over the time frame of a normal withdrawal period for quitting cannabis (eight weeks) and consists of ~15 meetings. It includes medical, psychological, and social phases in which the participant is helped to recognize and address typical problems related to each phase. The CCP has been implemented as a low-threshold face-to-face community-based program from 2005 onwards in several Norwegian municipalities. Low-threshold means that participants could contact the services themselves without a formal referral, and participation is free of charge. A small pilot study reported that an encouraging 79% of completers (26 of 33) had at least a 30 days cannabis abstinence period at the end of the intervention.19 The Sørlandet Hospital has conducted a study examining the long-term effect of the program (CCP study), but the results have not yet been published.
Many of the clients in CCP sessions at the Outreach Service in Oslo reported that they had thought about seeking help long before they actually did and that they had tried to quit on their own several times. The National Drug Helpline found that callers often needed an easy-to-access alternative for gaining help with reducing or quitting their cannabis use. A low-threshold motivation program would help expand access to help. An app would be expected to provide an alternative for those who would not otherwise contact traditional services or who live where services are unavailable. In addition to individual use of the app, those who attended CCP sessions could also use it as an add-on to face-to-face treatment.
We cooperated with students from Westerdals Oslo ACT College University in constructing the app. The development of the app was based on the CCP manual.17 To adapt it to the smartphone-based interface and make it as user friendly as possible, we assembled a reference group of professionals and cannabis users as well as a participant from a user organization; the Norwegian chapter of the marijuana legalization organization (‘NORMAL’). User tests, pilots, and surveys were conducted to examine what cannabis users would need and want in an app to help quit or reduce their cannabis use. Recreational users, former users, and users who experienced problems related to present cannabis use participated. Functions in the app are as follows:
- Motivational components (e.g., positive reinforcement):20
- Daily motivation and reflection advice
- A tool to register and visualize how long the person has abstained from/reduced their cannabis use, including how much money has been saved by reducing or quitting
- Gamification elements and accomplishments (milestones in the process) to increase motivation.
- Relapse prevention components:22
- A self-assessment tool to help with mapping and recognizing triggers of craving
- Suggestion of strategies to handle craving and triggers (trigger diary)
Similar to the CCP, respondents were recommended to use the app for at least eight weeks. The cannabis cessation app was launched in June 2016 for both Android and Apple phones. The app was marketed at several conferences for professionals, on social media, to user organizations, and in direct contact with cannabis users and their relatives. The National Drug Helpline also included information about the app on their homepage, with a direct link to download it. In October 2018, the app had been downloaded more than 5,000 times. In developing the app, privacy issues were an important concern. Because app users were using an illegal drug, securing their anonymity was crucial. Thus, national guidelines on privacy and data security issues were implemented (e.g., no personal data was required when downloading the app).
Study procedures
A questionnaire similar to that used in the previous CCP study was developed to allow for comparison between the CCP group and app group. The questionnaire was pilot tested before study start, and a link to the web-based questionnaire was inserted in the app. The link was visible on the startup page of the app for seven days after downloading and a notification invited a response to the questionnaire. The data collected in the study were registered only via the web-based link and not stored in the app or phone, and the respondents remained anonymous to the researchers. Data collection began in June 2017.
Participants
The app respondents were recruited through the app. Because of an administrative problem (data on age was unfortunately missing), this study used data collected from March to October 2018 when the age question was added to the questionnaire. We did not intend to use exclusion criteria. However, we would inspect the data, for example, the open-ended comments in the questionnaire and cannabis use variables, to examine whether there were respondents who were not ‘real’ cannabis users (e.g., relatives, health workers) or who reported unrealistic data (e.g., reported cannabis use for >30 days in the last month). To make the comparison between groups reliable, we excluded those with Severity of Dependence Scale (SDS) <4 in analyses, similar to the inclusion criteria in the CCP (see below). The questionnaire included a question regarding how the respondent intended to use the app (app alone or combined with other face-to-face services).
The comparative sample was recruited in three municipally based CCP centers in Norway (Kristiansand, Oslo, and Fredrikstad) from January 2013 to December 2016. The target group was individuals who engaged in regular or daily cannabis use, and who were motivated to quit cannabis. Some participants came into contact with the centers through support services in the cities (healthcare services, social security and welfare services, child welfare services, and school healthcare services), but no formal ‘referral’ was required. Many obtained information through friends, other users, or the internet and made direct contact themselves. The main aim of the CCP was to quit cannabis smoking, and participants were advised to set a quit date during the first part of therapy. The formal inclusion criterion was SDS score ⩾4. Youths under age <16 years were excluded from the CCP study.
Instruments
In addition to basic sociodemographics, the inventory included the following measures. The SDS is a 5-item questionnaire measuring the severity of dependence by users of different types of drugs, in this instance cannabis.23,24 Each of the five items is scored on a 4-point scale (0–3), and the sum score ranges from 0–15, with higher scores indicating higher levels of dependence. The SDS is a reliable and valid measure of severity of cannabis dependence among adolescents and adults, and a score ⩾4 is indicative of cannabis dependence.24 Two versions of the Hopkins Symptom Checklist (HSCL-10 and HSCL-25) were used to measure mental distress, HSCL-10 in the app group and HSCL-25 in the CCP.25 The present analysis is based on the HSCL-10 items, which are similar across the two versions. Each of the 10 items is scored on a 4-point scale (1–4), and an average score is computed, indicating a global severity index of mental distress (GSI). Four of the questions pertain anxiety and six to depression with respective sub-scales. The cut-off point for pathology is 1.85, and higher scores indicate greater distress.25 Days of cannabis use, last 30 days was collected according to the practice of the ASI questionnaire.26 Use of nicotine, alcohol and other substance use, last week was measured with separate visual analog scales in the CCP and similar ordinal scales in the app, from 0 = no use up to 10 = massive daily use. Self-efficacy of quitting and/or reducing cannabis use and the importance of quitting and/or reducing cannabis use were scored on a similar scale. A higher score represented higher self-efficacy and higher perceived importance of quitting/reducing cannabis use. General well-being was measured with the Outcome Rating Scale (ORS), which has four visual analog items on personal, interpersonal, social, and general well-being. Items are scored from 0 = bad up to 10 = good.27 Because of a technical limitation of the web-based survey, we used a Likert scale for these items in the app. The items are summed and total range is 0–40. A score <25 is indicative of scores expected in a clinical population.27
Statistical procedures
Data are presented descriptively. Across-group differences were examined using the chi-square or Student’s t-test. We did not perform Bonferroni adjustments or similar corrections because of the exploratory design.28 Multiple linear regression with simultaneous entry of variables was used to examine associations between well-being and independent variables (sociodemographic and severity variables, ie, substance use and mental health). Preliminary bivariate analyses were undertaken, and only factors with a P value below .20 were included in the multivariate analysis following the lax criterion recommended by Altman.29 Assumptions of multiple regression were met, for example, normal distribution and linearity of residuals and no multicollinearity. Results are presented with standardized and nonstandardized beta coefficients (β) with 95% confidence intervals (CIs). The R square (R2) value was used to assess the percentage of the response variable variation explained by the model. The significance level was set at P < .05. Statistical analyses were performed using SPSS version 23.0.
Results
A total of 301 respondents were included in the datasets. The app sample consisted of 185 respondents. However, 30 (16%) had an SDS score <4, and seven were not included because of information in open-ended text fields and reporting of >30 days of cannabis use in the last 30 days. The CCP sample consisted of 116 respondents. Although all of them participated in the CCP intervention, 14 of them (12%) should not have been included in the dataset because of SDS scores lower than the inclusion criterion of ⩾4. The final sample for analysis thus consisted of 250 respondents: 148 in the app group and 102 in the CCP (Table 1). The mean age was 25 years (SD 8, range 13–54 years) and was similar across groups. In the app, five respondents were under age 16 years. In the CCP, 47% had reached only secondary school, and 44% had done so in the app sample; in addition, a small percentage of these had not even completed secondary school. Slightly more than half of the respondents had at least some income from work, and one in four reported living with a partner. The app sample had a greater proportion of women (46% versus 26%; χ2 = 10.9; P = .001), but no other significant sociodemographic differences were found across groups (Table 1).
Table 1.
Sociodemographic characteristics of study respondents (N = 250), presented as N(%) or mean (SD).
| CHARACTERISTICS | CCP n = 102 |
APP n = 148 |
P a |
|---|---|---|---|
| Age, years | 25 (8) | 25 (9) | .197 |
| Gender, female (n = 247) | 26 (26) | 67 (46) | .001 |
| Relationship, living with a partner (n = 243) | 24 (24) | 34 (24) | .974 |
| Education level (n = 247) | |||
| Not completed primary | 3 (3) | 8 (6) | |
| Primary and secondary school (10 years of education) | 45 (44) | 55 (38) | .418 |
| High school (up to 13 years of education) | 44 (43) | 60 (41) | |
| University college or university (⩾ bachelor’s degree) | 10 (10) | 22 (15) | |
| Occupation | |||
| At least some income from own work (n = 230) | 48 (52) | 82 (59) | .277 |
| Working days within last 30 days | 10 (13) | 10 (9) | .876 |
Abbreviations: CCP, cannabis cessation program.
P was obtained from student’s t-test for continuous variables and chi-square test for categorical variables.
Concerning cannabis use, both groups had an average score in the mid-range on the SDS (~8; Table 2). Thus, the perceived severity of current use was similar, and so were the duration of problematic cannabis use and frequency of current use the last month (mean difference, 1.5 days; 95% CI −1.0 to 4; P = .237; Table 2). Concerning concurrent substance use, the app sample had significantly higher alcohol and other substance use. However, both groups had mean scores at the lower end of the scale. Nicotine use seemed to be quite extensive in both groups, with a score >7.
Table 2.
Self-reported substance use, mental health, and well-being among study respondents (N = 250), presented as n(%) or mean (SD).
| CHARACTERISTICS | CCP n = 102 |
APP n = 148 |
P a |
|---|---|---|---|
| Substance use | |||
| Years of problematic cannabis use | 7 (6) | 6 (6) | .197 |
| Severity of dependence scale (SDS, scale 0–15) | 8.8 (2.8) | 8.3 (2.8) | .195 |
| Days of cannabis use within last 30 days | 18.8 (10.2) | 20.3 (9.7) | .237 |
| Substance use (scale 0–10) | |||
| Alcohol use | 1.6 (1.7) | 2.3 (2.5) | .017 |
| Other substance use | 0.2 (0.9) | 1.2 (2.3) | <.001 |
| Nicotine | 7.3 (3.4) | 7.4 (3.3) | .756 |
| Importance of quitting, scale 0–10b | 9.1 (1.7) | 8.7 (2.0) | .125 |
| Self-efficacy of quitting, scale 0–10b | 8.0 (2.0) | 7.5 (2.7) | .080 |
| How to use the app? (n = 121)c | |||
| On your own | 79 (65) | ||
| As an add-on to traditional therapy | 42 (35) | ||
| Mental health (mental distress, HSCL-10) | |||
| Proportion in the clinical range of distressd | 72 (71) | 104 (77) | .367 |
| Anxiety | 2.16 (0.67) | 2.20 (0.76) | .626 |
| Depressiveness | 2.40 (0.74) | 2.64 (0.80) | .018 |
| Global mental distress score (GSI) | 2.30 (0.66) | 2.47 (0.71) | .070 |
| Well-beinge | |||
| Self-reported well-being (ORS) | 22.5 (8.6) | 19.1 (8.7) | .003 |
| Proportion in the clinical range of distressf | 62 (62) | 99 (73) | .078 |
Abbreviations: CCP, cannabis cessation program; GSI, global symptom index; HSCL, hopkins symptom checklist; ORS, outcome rating scale.
P was obtained from student’s t-test for continuous variables and chi-square test for categorical variables.
In the app, the used term was ‘quitting or reducing’.
Data from the app group only.
GSI score of the HSCL-10 ⩾ 1.85, n = 237.
n = 236; 12 respondents in the app group and 2 in the CCP group had missing ORS data.
ORS score <25.
The perceived need to make changes in cannabis use as measured by the ‘importance of quitting/reducing’ question was high and at a similar level in the two groups (mean score ~9 out of 10 in both groups). The perceived self-efficacy of quitting/reducing cannabis use was somewhat lower at 7.4 in the app versus 8.0 in the CCP, but in both groups, the score still represented a positive view of the respondents’ ability to carry out the needed lifestyle changes. A total of 65% in this group reported that they planned to use the app as a self-management tool, and 35% used it as an add-on to formal therapy (Table 1). We checked whether those who planned to use the app as an adjunct to face-to-face treatment differed from the app only group, but found no differences in severity (SDS score = 8.4 versus 8.2, P = .66). Thus, a more complex analysis with sub-groups was deemed unnecessary.
Some differences appeared in the mental health and well-being scores (Table 2). App respondents had a higher HSCL-10 depressiveness score (mean difference 0.24; 95% CI 0.04–0.44; P = .018). No differences in anxiety or overall GSI score emerged. The groups did not differ concerning the proportions above the cut-off value for mental distress, but a substantial majority (74%) of all respondents had a score above this cut-off value. Accordingly, 73% in the app and 62% in the CCP were in the clinical range for distress on the well-being scale, and app respondents reported a substantial 3.4-point worse score on that scale (95% CI −5.7 to −1.2; P = .003). App participants were significantly lower in the personal, interpersonal and general domains of the ORS, with the largest differences in the personal and interpersonal domains (Figure 1).
Figure 1.
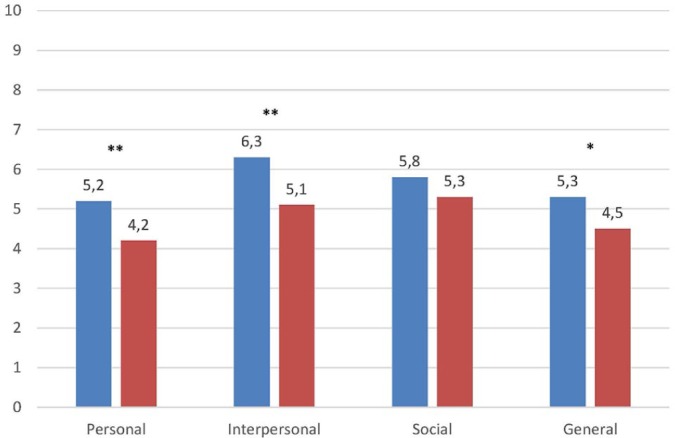
Difference between groups in each well-being domain of the outcome rating scale (ORS; n = 236). The clinical cut-off is 6.3 (below the cut-off is in the clinical range of well-being). The blue bars indicate the Cannabis Cessation Program group and the red bars the app group.
*P < .05, **P < .01.
Factors associated with perceived well-being
In bivariate analyses, several sociodemographic (ie, gender, relationship, educational level, and occupational level) and substance use variables (ie, alcohol and nicotine use, and ‘importance of quitting’) had P > .2 and were excluded from further analysis. The multiple regression analysis retained four significant independent variables. Well-being was negatively associated with being in the app group, higher age, and greater mental distress (Table 3), and was positively associated with the perceived ability to make changes (‘self-efficacy of quitting’). Mental distress was the strongest factor associated with well-being (β = −7.6; 95% CI −9.1 to −6.1; P < .001), as also evidenced by the strongest standardized beta (Table 3). The model explained 42% (R2) of the variance in well-being.
Table 3.
Factors associated with well-being (n = 236).a
| BETA (95% CI)b | STANDARDIZED BETA |
P | |
|---|---|---|---|
| Group and sociodemographic variables | |||
| Group (beta for app group versus CCP) | −1.9 (−3.8/−0.1) | 0.1 | .043 |
| Age | −0.1 (−0.3/−0.0) | −0.1 | .013 |
| Substance use variables | |||
| Severity of dependence scale – cannabis | 0.1 (−0.2/0.5) | 0.0 | .451 |
| Other substance use | −0.1 (−0.6/0.4) | 0.0 | .593 |
| Self-efficacy of quitting | 0.4 (0.0/0.8) | 0.1 | .047 |
| Mental health | |||
| Mental distress (HSCL-10) | −7.6 (−9.1/−6.1) | 0.8 | <.001 |
Abbreviations: CCP, cannabis cessation program; HSCL, hopkins symptom checklist
Well-being as measured with the outcome rating scale.
Multiple linear regression with simultaneous entry of variables (the ‘enter’ method); unstandardized beta coefficient with 95% confidence interval (CI). The model explained 42% (R2) of the variance in well-being.
Discussion
The app group had a greater proportion of women (46%) than the CCP (26%). Compared with the CCP, the app group had similar severity of cannabis use, in contrast to expectations. The app respondents also had higher depression scores and scored lower on the well-being scale. Being in the app group, being older, and having higher levels of mental distress were all factors negatively associated with well-being. The strongest negative factor influencing well-being was greater mental distress.
A recent national study found an average age of 27 years for persons with cannabis use as a principal problem presenting to specialist drug treatment in Norway.6 The average age in our study was 25 years, indicating that both the low-threshold CCP and the app recruited a slightly younger population. Our expectation that those seeking out the app would be younger than those presenting for CCP were not met. We note, however, that a few people under age 16 years downloaded the app.
Most cannabis users start using the drug while they are in the mid-teens.6,30 Thus, it is important to have a treatment option that is appealing to them. In Norway in 2017, 98% of the population >9 years old had a mobile phone, 91% had access to a smartphone, and 8 of 10 of those <35 years old had downloaded an app during the previous three months.31,32 Young persons who experience problems with cannabis use would therefore likely be inclined to search for and easily find apps that offer simple strategies for lifestyle changes before they seek out formal options that would likely be perceived as more cumbersome.
The gender difference is interesting in light of the fact that 75% of persons with CUD seeking treatment in specialized treatment services are males, similar to that seen in the CCP.6 More than four out of ten in the app sample were women, similar to a finding in an Australian web-based cannabis treatment intervention.33 Women are more likely than men to report feeling shame or embarrassment because they are in SUD treatment, and they generally experience more obligations and less mobility for accessing face-to-face services.34 Social obligations, such as caring for children, may be an important reason to refrain from seeking help due to the risk of interventions from child welfare services. Furthermore, women who are drug dependent experience various physical and social complications faster and more severely than men who are drug dependent.35 Thus, when women eventually enter substance abuse treatment, they typically present with a more severe clinical profile than men. Our findings on gender suggest that the app reached some people who were not as likely to attend formal services and who possibly would find it more problematic to seek out face-to-face services.
In contrast to expectations, we found similar substance use severity across groups. The importance of reducing/quitting score was also at a similarly high level in both groups (~9 of 10). Taken together with the large amount of persons who downloaded the app, this finding signifies that the app caught the attention of a considerable group who consider reducing or quitting cannabis use because they have a substantial related problem.36 Seeking out the app might have been a first step toward change. These users may not be sufficiently motivated to approach face-to-face–based services yet or may want to try to make changes on their own before eventually seeking conventional treatment.
The mental distress and the perceived well-being scores also point to the problematic symptom level in the sample. Most respondents (74%) reported mental distress above the pathological cut-off, and a corresponding 68% had scores in the clinical range of the well-being scale. The app group had a higher depressiveness score, corroborating previous findings in many large-scale studies and mental health surveys of a high prevalence of comorbid cannabis use and depression.6,37 Seeking out face-to-face services is one way of breaking out of isolation instead of trying to handle a problem alone. Thus, the lower depressiveness score in the CCP might be the result of an initiative to connect with others for support in the process of making lifestyle changes. By using the app only, participants miss the opportunity to form an alliance with a professional therapist and cannot benefit from the potential support and feedback from a face-to-face service.
The app group also had a 3.4-point worse well-being mean score, and the difference was especially large in the personal and interpersonal domains. Previous research has found baseline ORS scores between 20 and 23 in samples with SUDs.38,39 The app sample had even lower ORS scores, almost as low as in samples with a major depression diagnosis (mean ORS = 17).38 The high level of mental distress and correspondingly low perceived well-being may have been motivating factors for contemplating behavior change and seeking out possible change strategies in the present sample, as has been seen in general SUD samples.40
In the multivariate regression analysis, the severity of the cannabis use was surprisingly not associated with well-being. After controlling for sociodemographic and severity variables (substance use and mental health), we found that the app group had an adjusted 1.9 lower well-being score. The strongest influence was mental distress; a one-point higher mental distress score resulted in a substantial 7.6 lower well-being score. The high level of mental distress corresponding with the reduced well-being seen in the app group suggest that these respondents did not have an insignificant problem. These findings are somewhat worrying. In a face-to-face treatment, the therapist can follow-up on concurrent mental distress in the treatment process. Users of the app will hopefully contact face-to-face–based services to obtain needed support if they do not achieve their goals by means of the app only.
Some of the respondents in the app group (35%) used the app as an add-on to face-to-face treatment. This proportion is much higher than that seen in an Australian study where only 4% used the web-based application in combination with face-to-face treatment.33 The high proportion in our study may be caused by an intentional recommendation in the CCP that using the app between face-to-face sessions might be useful.
Clinical implications
Our findings suggest that some users who sought out the app might have needed more support than an app can offer. SUD and mental disorders can mutually affect each other, and it is important to pay attention to both.41 The simplest implication is that there is a need to focus more on this concern in the app through a holistic approach to both SUD and mental health, in addition to giving information about where to seek help for these disorders. Furthermore, the majority of cannabis smokers in both groups also used nicotine, implying that it could be wise to address nicotine use in both forms of treatment.42
Concerning the content of the app, more interactivity might be needed, such as connecting support to the app, like a question-and-answer, chat, or mentor function. Such a tool would make it possible to contact and communicate with a therapist to obtain relevant information and support. To enable personalized feedback on mental health, one possibility would be to have a questionnaire assessing mental health (e.g., the HSCL-10) included in the app. During this study, it was included only as a separate link to the study questionnaire.
Methodological considerations
This study examined those who downloaded the app and did not include data on how much they actually used it. The usual caveat about the interpretation of causality in cross-sectional research must be kept in mind; with this design, we cannot tell whether the independent variables (e.g., mental distress) caused the reduced well-being seen in the sample. The CCP sample was recruited several years before the development of the app. However, we are not aware of any changes in treatment policy or cannabis use that may have contributed to biases due to the different data collection timeframes. As the app was developed some years after the CCP data collection, it is unlikely that the samples comprise some of the same respondents. However, we cannot rule out this possibility.
With regards to the gender difference between samples, we are not aware of any incentives of the CCP that favored men. Notably, one important recruitment area was the school system, which shows equal gender representation. A recent Norwegian report found that health workers are more concerned with the possible problems of female substance users when they approach treatment services.43 It has also been observed that women may be more likely to participate in surveys than men.44 We cannot exclude that these or other confounding factors may partly explain the observed differences between our samples.
A small proportion of the original app dataset (30 of 185, 16%) had SDS scores below the clinical cut-off. On its own, this finding could indicate that the app reached users with lower severity. However, a similar proportion (12%) in the CCP dataset also had SDS scores below the cut-off, although they perceived their cannabis use as problematic enough to participate in a CCP intervention. It seems possible to perceive having a cannabis-related problem even with SDS scores below the clinical cut-off, as previous studies have indicated.45 We did not include these individuals in our analyses because they did not meet our formal criteria of having a CUD. Because of the similar proportion excluded due to the severity score, including these respondents likely would not have altered our conclusion concerning the severity of cannabis use across groups.
Future studies should ask individuals who are receiving face-to-face treatment whether they have considered or tried the app for additional support.
Conclusion
The cannabis users who downloaded the app and responded to the survey did not have a less severe cannabis-related problem than those attending a low-threshold, face-to-face, community-based treatment service. To some degree, the app reached a broader segment of the cannabis-using population, as evidenced by the higher proportion of women. The app can be an alternative for those who are not prepared to seek treatment in formal healthcare services. However, the high level of depression and low well-being scores may imply that some users of the app might need additional support.
Footnotes
Declaration of conflicting interest:The authors declare that there is no conflict of interest.
Funding:The author(s) received no financial support for the research, authorship, and/or publication of this article.
Authors’ Contributions: All authors made substantial contributions to conception and design, acquisition of data or analysis, and interpretation of data. JKV, MR, CB, and ØK drafted the manuscript, and all authors were involved in revising it critically for important intellectual content. All authors gave approval for the final version to be published.
Ethical Approval and Consent to Participate: The Regional Committee for medical and health research ethics in Health Region South-East (REK 2012/1407) approved the study. All participants in the CCP provided written informed consent before inclusion. Data collection in the app was anonymous, and replying to the survey was considered as an implied consent.
ORCID iD: John-Kåre Vederhus  https://orcid.org/0000-0002-7341-5480
https://orcid.org/0000-0002-7341-5480
Availability of Data and Materials: The dataset used in the current analysis is available from the first author upon reasonable request.
References
- 1. European Monitoring Centre for Drugs and Drug Addiction. EU Drug Report: Trends and Developments. Luxembourg: Publications Office of the European Union; 2017. [Google Scholar]
- 2. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-5. 5th ed. Washington, DC: American Psychiatric Association; 2013. [Google Scholar]
- 3. Sherman BJ, McRae-Clark AL. Treatment of cannabis use disorder: current science and future outlook. Pharmacotherapy. 2016;36(5):511–535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Lev-Ran S, Imtiaz S, Taylor BJ, Shield KD, Rehm J, Le Foll B. Gender differences in health-related quality of life among cannabis users: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Drug Alcohol Depend. 2012;123(1–3):190–200. [DOI] [PubMed] [Google Scholar]
- 5. Hayatbakhsh MR, Najman JM, Jamrozik K, Mamun AA, Alati R, Bor W. Cannabis and anxiety and depression in young adults: a large prospective study. J Am Acad Child Adolesc Psychiatry. 2007;46(3):408–417. [DOI] [PubMed] [Google Scholar]
- 6. Christiansen SG, Bretteville-Jensen AL. Who seeks treatment for cannabis use? Registered characteristics and physical, psychological and psychosocial problem indicators among cannabis patients and matched controls. BMC Public Health. 2018;18(1):780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Vindenes V, Bramness JG, Bretteville-Jensen AL, Morland J, Bachs L. [Does stronger cannabis cause more health problems?]. Tidsskr Nor Laegeforen. 2016; 136(20):1736–1738. [DOI] [PubMed] [Google Scholar]
- 8. EMCDDA. Norway - Country drug report. http://www.emcdda.europa.eu/countries/drug-reports/2018/norway_en. Accessed December 21, 2018.
- 9. Bakken A. Youth Data 2018 - National Results [Ungdata 2018 - Nasjonale resultater]. Oslo: Norwegian Social Research (NOVA); 2018. [Google Scholar]
- 10. Bakken A. Young in Oslo [Ung i Oslo 2018]. Oslo: Norwegian Social Research (NOVA); 2018. [Google Scholar]
- 11. World Health Organization. The Health and Social Effects of Nonmedical Cannabis Use. Geneva, Switzerland: World Health Organization; 2016. [Google Scholar]
- 12. Kazemi DM, Borsari B, Levine MJ, Li S, Lamberson KA, Matta LA. A systematic review of the mHealth interventions to prevent alcohol and substance abuse. J Health Commun. 2017;22(5):413–432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Gonzalez VM, Dulin PL. Comparison of a smartphone app for alcohol use disorders with an Internet-based intervention plus bibliotherapy: a pilot study. J Consult Clin Psychol. 2015;83(2):335–345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Tait RJ, Spijkerman R, Riper H. Internet and computer based interventions for cannabis use: a meta-analysis. Drug Alcohol Depend. 2013;133(2):295–304. [DOI] [PubMed] [Google Scholar]
- 15. Ramo DE, Popova L, Grana R, Zhao S, Chavez K. Cannabis mobile apps: a content analysis. JMIR Mhealth Uhealth. 2015;3(3):e81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Bjelland C, Skar AKS, Rørendal M. Cannabis cessation on the mobile [Hasjavvenning på mobilen]. Rus & samfunn. 2016;9(6):34–37. [Google Scholar]
- 17. Lundqvist T, Ericsson D. A guide for those who want to quit smoking cannabis [En guide for DEG som vil slutte med hasj]. Skien: Borgestadklinikken; 2005. [Google Scholar]
- 18. Lundqvist T, Ericsson D. The theoretical background for the cannabis cessation program [Den teoretiska bakgrunden till Haschavvänjningsprogrammet (HAP) - en metod för behandling av cannabismissbruk]. Socialmedicinsk Tidsskrift. 2007; 84(1):37–45. [Google Scholar]
- 19. Hansen AR, Ropstad G, Kristensen Ø, Clausen T. Cannabis smoking cessation courses; feasibility and follow-up results [Kurs i røykeavvenning for cannabisbrukere – en oppfølgingsstudie]. Sykepleien Forskning. 2011;6(4):368–374. [Google Scholar]
- 20. Monney G, Penzenstadler L, Dupraz O, Etter JF, Khazaal Y. mHealth app for cannabis users: satisfaction and perceived usefulness. Front Psychiatry. 2015;6:120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Budney AJ, Moore BA, Vandrey RG, Hughes JR. The time course and significance of cannabis withdrawal. J Abnorm Psychol. 2003;112(3):393–402. [DOI] [PubMed] [Google Scholar]
- 22. Hendershot CS, Witkiewitz K, George WH, Marlatt GA. Relapse prevention for addictive behaviors. Subst Abuse Treat Prev Policy. 2011;6:17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Gossop M, Best D, Marsden J, Strang J. Test-retest reliability of the severity of dependence scale. Addiction. 1997;92(3):353. [DOI] [PubMed] [Google Scholar]
- 24. Martin G, Copeland J, Gates P, Gilmour S. The Severity of Dependence Scale (SDS) in an adolescent population of cannabis users: reliability, validity and diagnostic cut-off. Drug Alcohol Depend. 2006;83(1):90–93. [DOI] [PubMed] [Google Scholar]
- 25. Strand BH, Dalgard OS, Tambs K, Rognerud M. Measuring the mental health status of the Norwegian population: a comparison of the instruments SCL-25, SCL-10, SCL-5 and MHI-5 (SF-36). Nord J Psychiatry. 2003;57(2):113–118. [DOI] [PubMed] [Google Scholar]
- 26. McLellan AT, Cacciola JC, Alterman AI, Rikoon SH, Carise C. The addiction severity index at 25: origins, contributions and transitions. Am J Addict. 2006;15(2):113–124. [DOI] [PubMed] [Google Scholar]
- 27. Miller SD, Duncan BL. The outcome rating scale: a preliminary study of the reliability, validity, and feasibility of a brief visual analog measure. Journal of Brief Therapy. 2003;2(2):91–100. [Google Scholar]
- 28. Perneger TV. What’s wrong with Bonferroni adjustments. BMJ. 1998;316(7139):1236–1238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Altman DG. Practical Statistics for Medical Research. London: Chapman & Hall/CRC; 1991. [Google Scholar]
- 30. Degenhardt L, Ferrari AJ, Calabria B, et al. The global epidemiology and contribution of cannabis use and dependence to the global burden of disease: results from the GBD 2010 study. PLoS One. 2013;8(10):e76635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Statistics Norway (SSB). Facts about internet and mobile phone use. https://www.ssb.no/teknologi-og-innovasjon/faktaside#blokk-2. Accessed February 6, 2019.
- 32. Statistics Norway (SSB). Digital competence in Norway. https://www.ssb.no/teknologi-og-innovasjon/artikler-og-publikasjoner/unge-og-hoyt-utdannede-er-flinkest-foran-pc-en?tabell=308098. Accessed February 6, 2019.
- 33. Rooke SE, Gates PJ, Norberg MM, Copeland J. Applying technology to the treatment of cannabis use disorder: comparing telephone versus Internet delivery using data from two completed trials. J Subst Abuse Treat. 2014;46(1):78–84. [DOI] [PubMed] [Google Scholar]
- 34. Thom B. Sex differences in help-seeking for alcohol problems–2. Entry into treatment. Br J Addict. 1987;82(9):989–997. [DOI] [PubMed] [Google Scholar]
- 35. Greenfield SF, Back SE, Lawson K, Brady KT. Substance abuse in women. Psychiatr Clin North Am. 2010;33(2):339–355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Prochaska JO, DiClemente CC, Norcross JC. In search of how people change. Applications to addictive behaviors. Am Psychol. 1992;47(9):1102–1114. [DOI] [PubMed] [Google Scholar]
- 37. Swift W, Hall W, Teesson M. Cannabis use and dependence among Australian adults: results from the National Survey of Mental Health and Wellbeing. Addiction. 2001;96(5):737–748. [DOI] [PubMed] [Google Scholar]
- 38. Reese RJ, Duncan BL, Bohanske RT, Owen JJ, Minami T. Benchmarking outcomes in a public behavioral health setting: feedback as a quality improvement strategy. J Consult Clin Psychol. 2014;82(4):731–742. [DOI] [PubMed] [Google Scholar]
- 39. Schuman DL, Slone NC, Reese RJ, Duncan B. Efficacy of client feedback in group psychotherapy with soldiers referred for substance abuse treatment. Psychother Res. 2015;25(4):396–407. [DOI] [PubMed] [Google Scholar]
- 40. Marlowe DB, Merikle EP, Kirby KC, Festinger DS, McLellan AT. Multidimensional assessment of perceived treatment-entry pressures among substance abusers. Psychol Addict Behav. 2001;15(2):97–108. [DOI] [PubMed] [Google Scholar]
- 41. Mueser KT, Noordsy DL, Drake RE, Fox L. Integrated Treatment for Dual Disorders: A Guide to Effective Practice. New York: Guilford Press; 2003. [Google Scholar]
- 42. Kelly JF, Greene MC, Bergman B, Hoeppner B. Smoking cessation in the context of recovery from drug and alcohol problems: prevalence, predictors, and cohort effects in a national U.S. sample. Drug Alcohol Depend. 2019;195:6–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Lundeberg IR, Mjåland K, Søvig KH, Nilssen E, Ravneberg B. Coercion in Addiction Treatment [Tvang overfor rusmiddelavhengige]. Bergen: Uni Rokkansenteret; 2010. [Google Scholar]
- 44. Moore D, Tarnai J. Evaluating nonresponse error in mail surveys. In: Groves RM, Dillman DA, Eltinge JL, Little A. (eds) Survey Nonresponse. New York: Wiley; 2001:197–211. [Google Scholar]
- 45. Steiner S, Baumeister SE, Kraus L. Severity of dependence scale: establishing a cut-off point for cannabis dependence in the German adult population. Sucht: Zeitschrift fur Wissenschaft und Praxis. 2008;54(suppl 1):S57–S63. [Google Scholar]


