Abstract
Objective:
To estimate the burden of mental, neurological, substance use disorders and self-harm (MNSS) in Canada, Mexico, and the United States.
Method:
We extracted 2017 data from the Global Burden of Disease online database. Based on a previously developed framework to classify and aggregate the burden of specific disorders and symptoms, we reestimated the MNSS burden to include suicide, alcohol use, drug use, specific neurological, and painful somatic symptom disorders. We analyzed age–sex-specific patterns within and between countries.
Results:
The MNSS burden is the largest of all disorder groupings. It is lowest in Mexico, intermediate in Canada, and highest in the United States. Exceptions are alcohol use, bipolar, conduct disorders, and epilepsy, which are highest in Mexico; and painful somatic syndromes and headaches, which are highest in Canada. The burden of drug use disorders in the United States is twice the burden in Canada, and 7 times the burden in Mexico. MNSS become the most burdensome of all disorder groups by age 10, staying at the top until age 60, and show a distinct pattern across the lifetime. The top three MNSS disorders for men are a combination of substance use disorders and self-harm (United States), with the addition of painful somatic syndromes (Canada), and headaches (Mexico). For women, the top three are headaches and depression (all countries), drug use (United States), neurocognitive disorders (Mexico), and painful somatic syndromes (Canada).
Conclusion:
MNSS are the most burdensome disease grouping and should be prioritized for funding in Canada, Mexico, and the United States.
Keywords: mental health, mental disorders, substance use disorders, Global Burden of Disease, North America
Abstract
Objectif:
Estimer la charge des troubles mentaux, neurologiques, d’utilisation de substances et de l’automutilation (MNSA) au Canada, au Mexique et aux États-Unis.
Méthode:
Nous avons extrait les données de 2017 de la base de données en ligne Charge mondiale de morbidité. Selon un cadre élaboré préalablement pour classer et regrouper la charge des maladies et symptômes spécifiques, nous avons estimé de nouveau la charge des MNSA pour inclure le suicide, l’utilisation d’alcool, l’utilisation de drogues, les affections neurologiques spécifiques, et les troubles de symptômes somatiques de douleur. Nous avons analysé les modèles spécifiques selon l’âge et le sexe au sein des pays et entre eux.
Résultats:
La charge des MNSA est la plus lourde de tous les groupements de maladies. Elle est la plus faible au Mexique, intermédiaire au Canada et la plus élevée aux États-Unis. Les exceptions sont les troubles d’utilisation d’alcool, bipolaire, des conduites, et l’épilepsie, qui sont les plus élevés au Mexique; et les syndromes somatiques douloureux et les maux de tête, qui sont les plus élevés au Canada. La charge des troubles d’utilisation de drogues aux États-Unis est le double de celle du Canada, et 7 fois celle du Mexique. Les MNSA constituent la charge la plus importante de tous les groupes de maladies vers l’âge de 10 ans, et demeurent au sommet jusqu’à 60 ans, et affichent un modèle distinct durant toute la vie. Les 3 principaux troubles MNSA pour les hommes sont une combinaison de troubles d’utilisation de substances et d’automutilation (États-Unis), avec en outre les syndromes somatiques douloureux (Canada), et les maux de tête (Mexique). Pour les femmes, les 3 principaux sont les maux de tête et la dépression (tous les pays), l’utilisation de drogues (États-Unis), les troubles neurocognitifs (Mexique) et les syndromes somatiques douloureux (Canada).
Conclusion:
Les MNSA sont le groupe de maladies qui représentent la charge la plus lourde et qui devraient obtenir la priorité du financement au Canada, au Mexique et aux États-Unis.
Introduction
During the last decade, the North American region (for the purpose of this article, we include Canada, Mexico, and the United States) has reached the highest levels of longevity so far recorded, among the highest in the world.1 However, two facts cast a shadow over this trend. First, these additional years of life have been affected by increased disability and multimorbidity, driven mostly by chronic noncommunicable diseases (NCDs).2–4 Second, in the United States, this trend has flattened in 2014 and even reversed in 2016 and 2017, with a decline in life expectancy at birth.1,5 Canada seems to be following the United States with a 2-year lag: Life expectancy gains stalled from 2016 to 2017 and even reversed in some provinces, most notably British Columbia.6 Previous studies suggest that in North America, the largest proportion of the disease burden is due to mental, neurological, substance use disorders and self-harm (MNSS),7,8 which also have substantial adverse human, social, and economic consequences.9–14 Indeed, specific MNSS seem to be the main causes of the reversal in life expectancy the United States and Canada are experiencing. Case and Deaton pointed early on to the “deaths of despair” due to alcohol, drugs, and suicide.15 Similarly but more recently, statistically significant increases were detected in deaths due to suicide, overdose, liver disease, as well as neurocognitive disorders, among others.16,17 In Canada, the main causes are substance use disorders (mostly opioid but also stimulant and polysubstance use disorders), weaponized by the contamination of the illegal drug supply with fentanyl.6,18,19
Despite the disability and death toll that MNSS exact on populations, they have been neglected by policy makers and funders, arguably as a manifestation of pervasive structural stigma, lack of knowledge about preventable risk factors, and uncertainty about the availability of effective and cost-effective interventions.7,20–23 This neglect has been exacerbated by the fact that several studies have underestimated the magnitude of this burden due to their methodological limitations.9 The Global Burden of Disease (GBD) Project has developed a specific methodology to collect inputs (e.g., prevalence, mortality, etc.), model disorder-specific disease burden (years lived with disability [YLDs], years of life lost [YLLs], and disability-adjusted life years [DALYs]), and aggregate disorder-specific burden into higher level groupings. Their ad hoc methodology for aggregation, which sometimes follows the International Statistical Classification of Diseases and Related Health Problems (ICD-10) and sometimes departs from it without a clear rationale, is however enforced for all the GBD official estimates, across disorder groupings.24 We have argued that this “one size-fits-all” approach (comprising decisions made around what inputs to exclude, how to attribute mortality, and how to aggregate disorders) generates biased estimates that specifically undercount the mental health–related burden. As per our original analysis, the GBD methodology nearly halves the DALYs that should be attributed to the mental health–related burden as a fraction of total burden globally: 7% versus 13%.9 Indeed, in principle, DALYs should consist of the sum of YLDs and YLLs, which holds true for most disorders. However, for mental disorders, DALYs are in fact exclusively composed of YLDs. Zero deaths (and hence zero YLLs) have been attributed in the nearly three decades of GBD estimates to depressive disorders and bipolar disorders, for example. And as of last year, all deaths previously attributed to schizophrenia have been removed. The only YLLs included in the GBD estimates for mental disorders in 2017 globally are those resulting from 326 global deaths attributed to eating disorders. Further, as of this year, the burden resulting from substance use disorders is presented separately in a newly created Level 2 aggregation, the most recent unexplained departure from ICD methodology. And when the GBD does follow the ICD classification, it does so mechanistically, which occasionally leads to obvious misclassifications such as including suicide and intentional self-harm among ICDs “external causes of morbidity and mortality”, along with traffic accidents, war casualties, assault, and so on (the Level 1 grouping “injuries”). Although the merits of the GBD collaboration are without question, we find that these specific methodological decisions need an urgent revision, since the systematic underestimation of the burden related to mental health does a disservice to mental health epidemiology and, more importantly, to the people whose burden is minimized.
The aim of this article is to compensate for the GBD methodological limitations noted above and to provide less biased estimates of the burden of disease related to mental health in Canada, Mexico, and the United States. The commonly used estimates3,4 were adjusted by including self-harm and suicide, providing an estimation for somatic symptom disorder with prominent pain and specific neurological disorders, and allocating somatic manifestations of alcohol use to the burden caused by alcohol use disorder. A comparative epidemiology of North America offers the unique opportunity of highlighting the similarities and differences of the disease burden related to mental health in three countries that, despite their geographic proximity and long-standing social and economic interactions, have important differences in their cultural traits, level of economic development, and health system arrangements. It also provides the opportunity to raise the issue of how underestimating the mental health–related burden poses specific, frequently different, health systems challenges in each of these three countries.
Method
The goal of our comparative epidemiology is to capture not only the mortality and nonlethal impact of the disorders of interest in these countries—traditionally captured by cause-specific mortality and prevalence rates—but the actual loss in terms of healthy life associated with each disorder. Hence, we base our analysis on publicly available disorder-specific disease burden estimates produced by the GBD project.
Estimates of global and local DALYs are produced yearly, along with the DALYs’s building blocks: YLDs plus YLLs due to premature mortality.25 The GBD Project has developed a specific methodology to (a) collect globally available inputs (e.g., prevalence, mortality, etc.), (b) adjust these inputs and model disorder-specific disease burden (YLDs, YLLs, and DALYs), and (c) aggregate disorder-specific disease burden into higher level groupings (e.g., major depressive disorder and dysthymia—Level 4 disorders—are aggregated into depressive disorders—a Level 3 grouping, which are then combined with others into mental disorders—a Level 2 grouping, which are then aggregated into NCDs—a Level 1 grouping, which combined with the two other Level 1 groupings (“injuries” and “communicable, maternal, neonatal nutritional”) represent the total disease burden.) YLLs are a mortality measure weighted by a factor given by optimized life expectancy minus age of death, and YLDs are a measure of prevalence weighted by the empirically determined perception of impairment of each health state resulting from disease.26,27 The GBD Project makes disorder-specific burden data available through the Global Health Data Exchange (ghdx.healthdata.org) and encourages the utilization, sharing, modification, and building upon their outputs and estimates by independent research groups. This “open-access” policy represents a unique and groundbreaking scientific endeavor and has allowed the collective understanding of the disease burden—in general and specifically related to mental health—to evolve throughout the years in response to the GBD’s dialogue with the scientific community. This article seeks to advance this collective goal, with a focus on our specific field of study and area of interest.
From this public repository, we extracted 2017 disaggregated sex- and age-specific country-level burden of disease data (i.e., DALYs and YLDs) for all disorders and symptoms for the three countries (published in 2018).3,4 Following the extraction of data, the mental health–related burden was reestimated with adjustments to include self-harm and suicide, specific neurological disorders, drug use disorders, alcohol use disorders and their somatic symptoms, and an estimation for somatic symptom disorder with prominent pain, which in DSM5 replaces “pain disorder” (DSM IV) and is equivalent to “persistent somatoform pain disorder” (ICD 10).24,28,29 This burden is collectively referred to as mental, neurological, substance use disorders and self-harm (MNSS), and our methodology is described in additional detail elsewhere.9
The reasons for these adjustments are both conceptual and practical. Our goal is to arrive at the best possible holistic estimate of the disease burden related to mental health in order to inform health policy and health systems planning. Other mental health–related burden estimations are guided by different goals and/or bound by specific organizational decision-making hierarchies and are sometimes unable to arrive at an estimate of minimum face validity. The arbitrary separation between disorders traditionally considered psychiatric and neurological, the separate presentation of mental and substance use disorders, the consideration of self-harm and suicide as a category unrelated to mental disorders, the conflation of painful somatization disorders with musculoskeletal disorders, the exclusion of personality disorders as such, and the inadequate consideration of the contribution of mental illness to excess deaths, all contribute in a synergistic manner to undercount the burden related to mental health.30,31 We argue that these exclusions, which lead to biased estimates, are based on technical limitations and misclassification rather than on conceptually sound decision-making. We further argue that this is not a trivial limitation: It drives policy, and by reducing the visibility of the burden related to mental health, it results in undertreatment and increased suffering, as we have argued elsewhere.7,32 With the currently available data, it is not possible to fully address these shortcomings, but it is possible to significantly remediate them: In lieu of excluding 100% of excess death due to mental disorders, we include deaths due to suicide; instead of excluding 100% of somatic symptom disorders, we include a fraction of painful somatic disorders without anatomical correlate as an estimate of somatic symptom disorder with prominent pain (usually ignored despite a prevalence that has been found to be as high as 8% of the population33,34); instead of presenting separately mental and substance use disorders, we present them together (as the ICD system does and even GBD did until last year); instead of arbitrarily separating mental and neurologic disorders, we follow the approach of the World Health Organization, the Disease Control Priorities collaboration, and also collaborators of the GBD study and add specific neurological disorders—those with prominent behavioral and cognitive presentations, namely, neurocognitive disorders, epilepsy, and headaches—to mental burden aggregations; and instead of distributing the direct somatic consequences of alcohol use disorder among multiple unrelated aggregations (liver cancer due to alcohol use is grouped by the GBD with neoplasms, alcoholic cardiomyopathy with cardiovascular disorders, and cirrhosis due to alcohol use with cirrhotic disorders), we include these causes of disability and death in the burden attributable to alcohol. In every instance in which we add the YLDs or DALYs attributed to our MNSS aggregation, we subtract them from their group in the GBD aggregation, so the overall classification remains exhaustive and mutually exclusive. Uncertainty intervals (UIs) were computed for our new age-standardized rate estimates based on the UIs of the individual disorders’ rates, applying a methodology designed to combine asymmetric errors (such as the UIs produced by the GBD methodology). Likelihood functions for distributions with asymmetric errors are approximated with a variable width Gaussian whose variance scales linearly, as per Barlow, 2004.35 These likelihood functions are combined to form a likelihood function for the sum of the values by marginalizing over the individual values while keeping their sum constant. Asymmetric errors can then be read off of the resulting likelihood for the sum.
Results
Distribution of the Disease Burden in Each Country
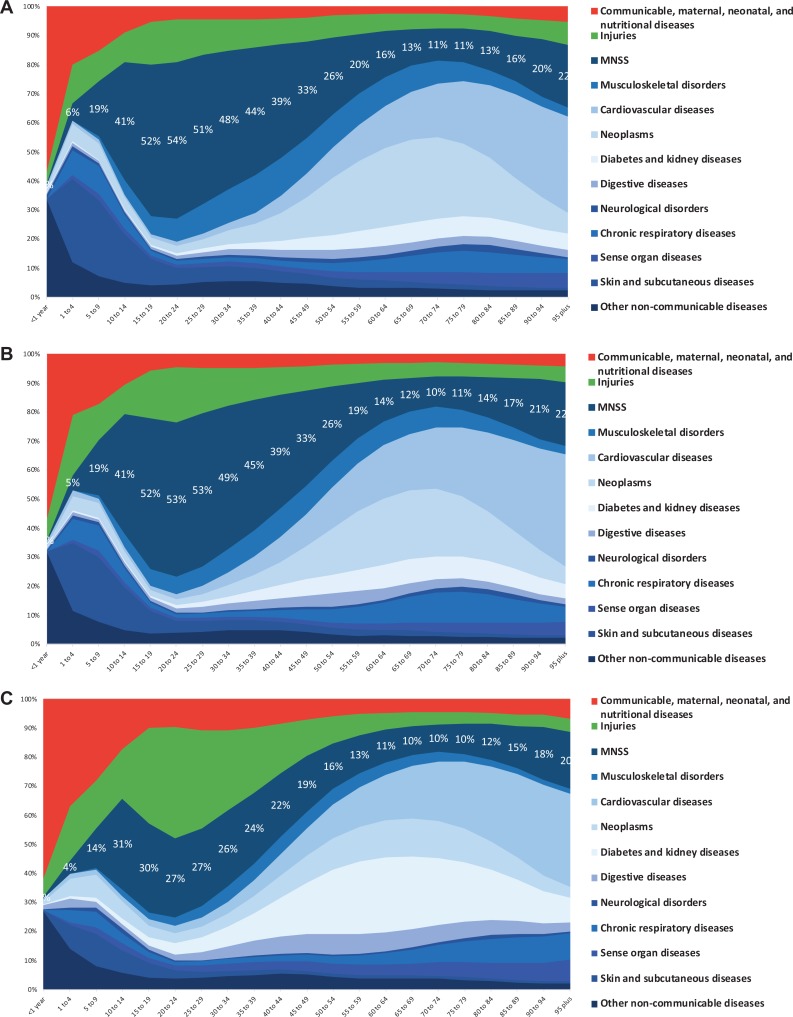
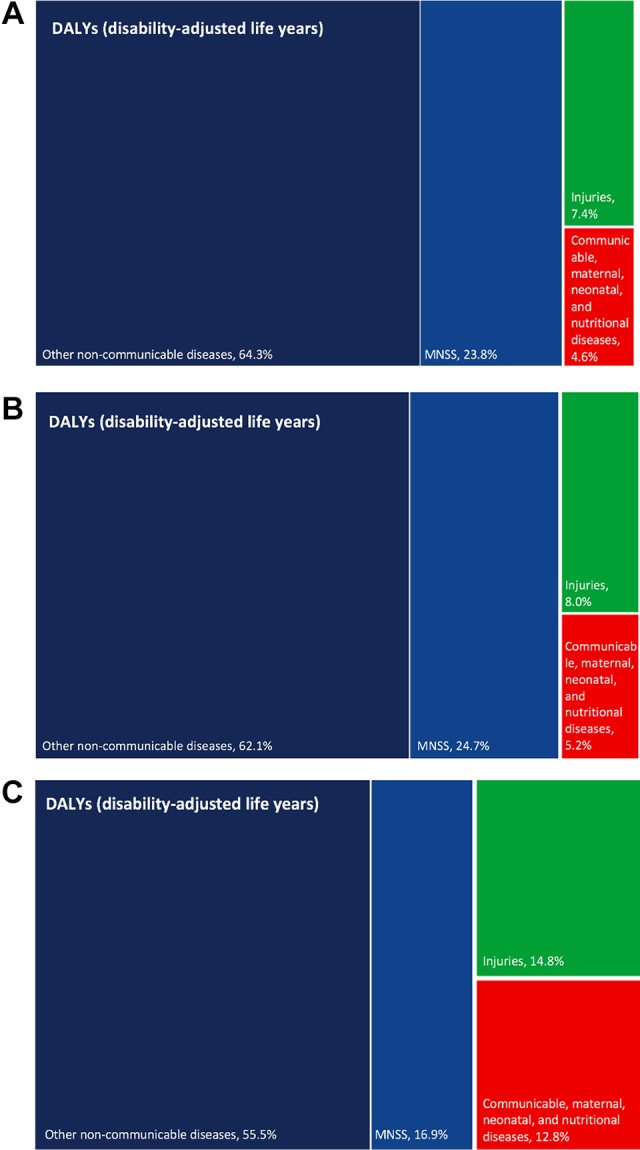
Broad overviews of the disease burden percentages in North America reveal almost identical patterns for the United States and Canada, with, respectively, 25% and 24% of overall DALY burden caused by MNSS (see Figure 1A and 1B). With respect to disability only, the United States and Canada also have similar proportions caused by MNSS: 35% and 34% of YLDs, respectively.
Figure 1.
Overall disease burden distribution in Canada, the United States, and Mexico. (A) Canada. (B) United States. (C) Mexico.
In Mexico, a larger percentage of the total disease burden than in the other two countries is caused by injuries, communicable, maternal, neonatal, and nutritional disorders, so NCDs cause a relatively smaller fraction. MNSS cause a similar percentage of the YLDs (32%) in Mexico but a lower percentage of the total DALYs (17%; Figure 1C).
In the three countries, MNSS are the largest relative cause of DALYs of all NCD groups by far, followed by neoplasms in Canada, cardiovascular disorders in the United States, and diabetes plus kidney disease in Mexico (see Figure 2A to 2C).
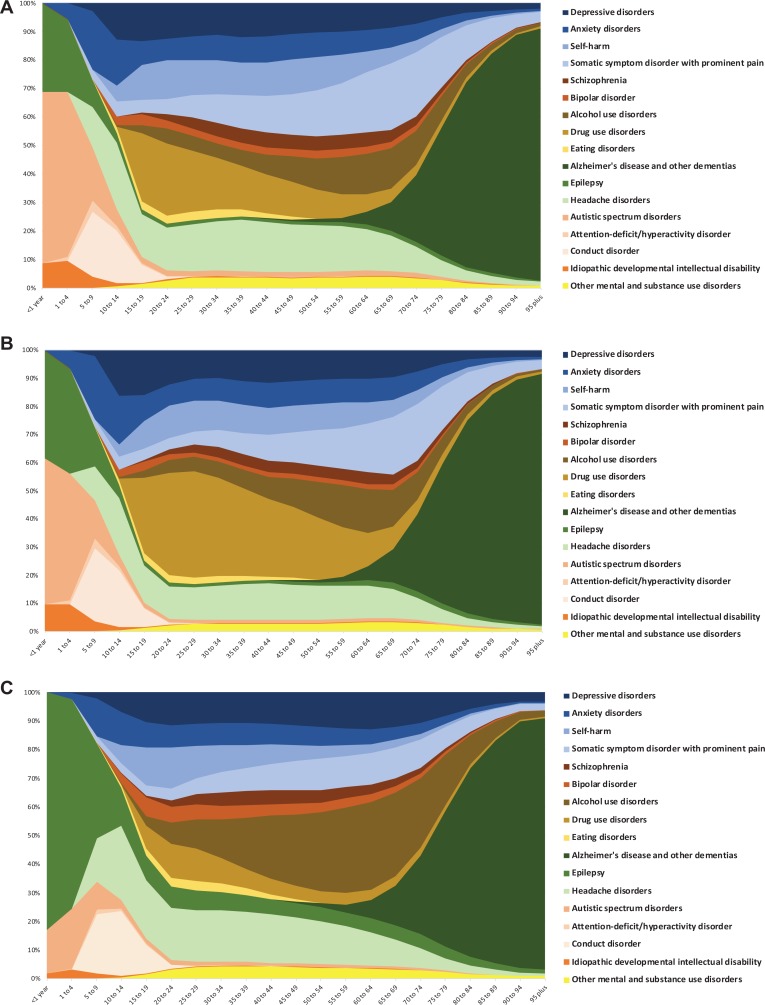
Figure 2.
Disease burden (DALYs) across the lifetime in Canada, the United States, and Mexico. (A) Canada. (B) United States. (C) Mexico. x-axis: age-group; y-axis: percentage of total DALYs in the country for both sexes. DALYs = disability-adjusted life years.
Despite the similar patterns of disease burden distribution in percentage terms in the United States and Canada, it is important to highlight that in absolute terms, the MNSS burden is lower in Canada (based on age-standardized rates, which we present in the gender-specific analysis below). This difference is mostly driven by a much lower burden of drug use disorders (less than half the DALYs for both women and men) and to a lesser extent of depression and anxiety. In the case of Mexico, the much lower overall MNSS burden is almost exclusively determined by the difference in the burden of drug use disorders, which is roughly 7 times lower both for men and women in Mexico than in the United States.
Adjusting for population size and structure, our analysis reveals a gradient of MNSS burden in North America with Mexico having the lowest burden of the three countries, Canada in an intermediate position and the United States suffering by far the highest burden for both men and women. Additional details of the magnitude and distribution of the MNSS burden are discussed below.
Distribution of the Disease Burden across the Lifetime
Examining the DALY burden across the lifetime, Canada and the United States also display similar trends. After the first year of life, NCDs—of which MNSS are a part—dominate the disease burden across age groups, reaching nearly 70% (Canada) and 60% (United States) of the total burden for the 1- to 4-year-old group (see Figure 2A and 2B). An analysis of the breakdown of these NCDs reveals that MNSS cause the highest proportion of the disease burden for those between the ages of 10 and 55, peaking at nearly 55% of the total disease burden around 25 years of age. After age 55, cancer-related mortality and cardiovascular disorders gain prominence, displacing MNSS from the top rank.
In Mexico, the pattern is different, with a larger fraction due to maternal and child disorders and an increase in violence and injuries during youth, which determines that NCDs only surpass 50% of the total burden around 5 years of age and that MNSS cause between a fifth and a third of the total burden between 10 and 50 years old (Figure 2C). Of note, interpersonal violence accounts for a third of the total disease burden in the 20- to 24-year-old group.
An analysis of how the burden specific to MNSS varies across the lifetime highlights key considerations from a population health perspective (see Figure 3 for details):
Figure 3.
Disease burden (DALYs) of MNSS across the lifetime in Canada, the United States, and Mexico. (A) Canada. (B) United States. (C) Mexico. x-axis: age-group; y-axis: percentage of total DALYs in the country for both sexes. DALYs = disability-adjusted life years.
Until 4 years of age, the MNSS burden is mostly due to epilepsy and autism, with autism comprising in this group about 50% of the MNSS burden in the United States and 60% in Canada, while epilepsy drives the MNSS burden in Mexico with well over 70%.
In the groups aged between 5 and 14 years, the burden of conduct disorders, anxiety disorders, and headaches gain prominence, accounting for (in average) nearly 60% of MNSS DALYs in Canada and the United States and 53% in Mexico.
In those aged 15 to 19 years, a pattern emerges that will remain stable throughout youth and adulthood (until around 60 years old). In Canada, common mental disorders (including anxiety, depression, self-harm, and painful somatic symptom disorders) account in average for around 45%; substance use disorders, 23%; headaches, 17%; and severe mental disorders (schizophrenia and bipolar disorders) approximately 7% of the MNSS burden. In the United States, common mental disorders account for around 40% of the MNSS burden; substance use disorders, 29%; headaches, 12%; and severe mental disorders, 5%. In Mexico, common mental disorders account for 35%; substance use, 26% (19% due to alcohol); headaches, 17%; and severe mental disorders, 8% of the MNSS burden.
Late teenage and early adulthood years show an increase in self-harm and suicide, which peaks in the United States and Canada around 13% of the MNSS burden in the early 20s. These years also show an increase in drug use disorders, which peak at 25% of the MNSS burden in Canada between the ages of 20 and 24, and at 38% of the MNSS burden in the United States between the ages of 25 and 29, reflecting the tragic outcomes of the opioid use and overdose crisis in both countries, but especially in the United States where opioid use disorders account for 15% of the total disease burden in this age-group (including here all communicable, maternal, child, NCDs, and injuries).
The adult years involve a partial switch from drug to alcohol use (especially in Mexico where it accounts for around 30% of the MNSS burden between 50 and 69 years old) and from headaches to painful somatic symptom disorders. During older adulthood neurocognitive disorders due to Alzheimer’s gain prominence: In the three countries, they reach half of MNSS DALYs at around 75 years old, 75% to 80% by 85 years old, and stay above 80% of the MNSS burden after that.
Differential Distribution of the MNSS Burden in Men and Women
If we consider all ages and both sexes, the age-standardized DALY burden of MNSS in North America is as follows: Mexico, 4,287 DALYs per 100,000 (UI = 3,944 to 4,664); Canada, 5,355 DALYs per 100,000 (UI = 4,908 to 5,840); and the United States, 6,831 DALYs per 100,000 (UI = 6,322 to 7,374). Of note, this gradient of increasing MNSS burden manifests itself not only through the DALY values but also through the UIs, which do not overlap for the three countries. The high burden found in the United States is clearly driven by the opioid use epidemic in youth and adults, which leads to the highest (by far) DALY burden of any disorder in the 15- to 50-year-old group for both sexes (10% of total disease burden) and especially for men (12% of total disease burden). It is also the most burdensome of all MNSS considering all ages together. If we consider age-standardized DALYs for men and women separately, their distribution shows both notable variations and similarities in the three countries (see Tables 1 to 3).
Table 1.
Distribution of the Mental, Neurological, Substance Use Disorder and Suicide Burden in the United States.
| Men | Women | ||
|---|---|---|---|
| Disorder | DALYs per 100,000 (Uncertainty Interval)a | Disorder | DALYs per 100,000 (Uncertainty Interval)a |
| MNSS (all disorders) | 7,097 (6,644 to 7,568) | MNSS (all disorders) | 6,555 (5,957 to 7,205) |
| Drug use disorders | 2,094 (1,808 to 2,380) | Drug use disorders | 1,296 (1,093 to 1,507) |
| Self-harm and suicide | 921 (858 to 963) | Headache disorders | 1,076 (706 to 1,521) |
| Alcohol use disorders | 683 (603 to 776) | Depressive disorders | 951 (673 to 1,283) |
| Headache disorders | 525 (343 to 752) | Anxiety disorders | 736 (521 to 984) |
| Depressive disorders | 523 (368 to 710) | Somatic symptom disorder with prominent pain | 653 (530 to 792) |
| Somatic symptom disorder with prominent pain | 509 (408 to 623) | Alzheimer disease and other dementias | 439 (417 to 461) |
| Anxiety disorders | 409 (290 to 551) | Self-harm and suicide | 280 (267 to 294) |
| Alzheimer disease and other dementias | 385 (365 to 405) | Alcohol use disorders | 278 (231 to 330) |
| Other mental and substance use disorders | 205 (133 to 289) | Schizophrenia | 188 (140 to 230) |
| Schizophrenia | 196 (146 to 241) | Eating disorders | 142 (93 to 209) |
| Autistic spectrum disorders | 163 (111 to 225) | Epilepsy | 123 (73 to 188) |
| Conduct disorder | 136 (82 to 214) | Bipolar disorder | 122 (79 to 181) |
| Epilepsy | 125 (77 to 186) | Other mental and substance use disorders | 112 (74 to 155) |
| Bipolar disorder | 119 (76 to 176) | Conduct disorder | 90 (55 to 143) |
| Eating disorders | 57 (35 to 84) | Autistic spectrum disorders | 39 (27 to 54) |
| Idiopathic developmental intellectual disability | 27 (10 to 49) | Idiopathic developmental intellectual disability | 22 (9 to 37) |
| Attention deficit hyperactivity disorder | 21 (12 to 33) | Attention deficit hyperactivity disorder | 8 (5 to 13) |
aAge-standardized rates.
Note. MNSS = mental, neurological, substance use disorders and suicide; DALYs = disability-adjusted life years.
Table 2.
Distribution of the Mental, Neurological, Substance Use Disorder and Suicide Burden in Canada.
| Men | Women | ||
|---|---|---|---|
| Disorder | DALYs per 100,000 (Uncertainty Interval)a | Disorder | DALYs per 100,000 (Uncertainty Interval)a |
| MNSS (all disorders) | 5,252 (4887 to 5,645) | MNSS (all disorders) | 5,451 (4,871 to 6,100) |
| Drug use disorders | 927 (755 to 1,136) | Headache disorders | 1,210 (789 to 1,727) |
| Self-harm and suicide | 779 (710 to 855) | Depressive disorders | 730 (508 to 992) |
| Somatic symptom disorder with prominent pain | 523 (404 to 671) | Somatic symptom disorder with prominent pain | 686 (538 to 864) |
| Alcohol use disorders | 512 (449 to 593) | Drug use disorders | 588 (448 to 748) |
| Headache disorders | 428 (286 to 607) | Anxiety disorders | 572 (406 to 758) |
| Depressive disorders | 416 (294 to 568) | Alzheimer disease and other dementias | 347 (318 to 380) |
| Anxiety disorders | 328 (233 to 437) | Self-harm and suicide | 300 (273 to 329) |
| Alzheimer disease and other dementias | 299 (274 to 326) | Alcohol use disorders | 215 (176 to 265) |
| Other mental and substance use disorders | 207 (135 to 292) | Schizophrenia | 180 (138 to 216) |
| Autistic spectrum disorders | 205 (139 to 281) | Bipolar disorder | 138 (86 to 206) |
| Schizophrenia | 186 (142 to 225) | Eating disorders | 134 (87 to 197) |
| Bipolar disorder | 128 (80 to 193) | Other mental and substance use disorders | 114 (74 to 160) |
| Conduct disorder | 121 (72 to 197) | Epilepsy | 86 (36 to 171) |
| Epilepsy | 92 (45 to 173) | Conduct disorder | 68 (40 to 113) |
| Eating disorders | 52 (32 to 78) | Autistic spectrum disorders | 54 (36 to 77) |
| Idiopathic developmental intellectual disability | 27 (8 to 48) | Idiopathic developmental intellectual disability | 22 (9 to 38) |
| Attention deficit hyperactivity disorder | 22 (13 to 36) | Attention deficit hyperactivity disorder | 8 (5 to 13) |
aAge-standardized rates.
Note. MNSS = mental, neurological, substance use disorders and suicide; DALYs = disability-adjusted life years.
Table 3.
Distribution of the Mental, Neurological, Substance Use Disorder and Suicide Burden in Mexico.
| Men | Women | ||
|---|---|---|---|
| Disorder | DALYs per 100,000 (Uncertainty Interval)* | Disorder | DALYs per 100,000 (Uncertainty Interval)* |
| MNSS (all disorders) | 4,599 (4,299 to 4,929) | MNSS (all disorders) | 4,001 (3,600 to 4,452) |
| Alcohol use disorders | 1,140 (1,039 to 1,253) | Headache disorders | 823 (538 to 1,174) |
| Self-harm and suicide | 485 (460 to 503) | Depressive disorders | 527 (373 to 722) |
| Headache disorders | 450 (284 to 672) | Alzheimer disease and other dementias | 401 (375 to 430) |
| Alzheimer disease and other dementias | 375 (341 to 411) | Anxiety disorders | 373 (261 to 502) |
| Depressive disorders | 350 (247 to 474) | Somatic symptom disorder with prominent pain | 349 (283 to 428) |
| Drug use disorders | 319 (241 to 407) | Epilepsy | 330 (218 to 472) |
| Epilepsy | 287 (205 to 389) | Alcohol use disorders | 281 (260 to 305) |
| Somatic symptom disorder with prominent pain | 275 (221 to 338) | Drug use disorders | 182 (133 to 236) |
| Anxiety disorders | 200 (141 to 269) | Bipolar disorder | 170 (107 to 252) |
| Other mental and substance use disorders | 161 (104 to 222) | Schizophrenia | 121 (91 to 150) |
| Bipolar disorder | 148 (93 to 218) | Self-harm and suicide | 114 (110 to 118) |
| Schizophrenia | 136 (101 to 168) | Other mental and substance use disorders | 109 (72 to 151) |
| Conduct disorder | 121 (72 to 191) | Eating disorders | 92 (59 to 137) |
| Autistic spectrum disorders | 98 (67 to 134) | Conduct disorder | 78 (46 to 127) |
| Eating disorders | 34 (21 to 50) | Autistic spectrum disorders | 35 (24 to 48) |
| Idiopathic developmental intellectual disability | 11 (2 to 23) | Idiopathic developmental intellectual disability | 12 (3 to 22) |
| Attention deficit hyperactivity disorder | 11 (7 to 17) | Attention deficit hyperactivity disorder | 4 (3 to 7) |
aAge-standardized rates.
Note. MNSS = mental, neurological, substance use disorders and suicide; DALYs = disability-adjusted life years.
In the United States, the MNSS burden for men is 7,097 DALYs per 100,000 (UI = 6,644 to 7,568), by far the highest of the region. They are affected mostly by drug use disorders, suicide, and alcohol use disorders, which collectively account for 52% of the MNSS DALYs. In Canada, the MNSS burden for men is 5,252 DALYs per 100,000 (UI = 4,887 to 5,645), with a similar pattern to the United States, with the exception of alcohol, which is displaced to the fourth rank order by painful somatic syndromes. In Mexico, the MNSS burden for men is lowest of the region with 4,599 DALYs per 100,000 (UI = 4299 to 4929). Mexican men are mostly affected by alcohol use disorders, suicide, and headaches.
In the United States, the MNSS burden for women is 6,555 DALYs per 100,000 (UI = 5,957 to 7,205), mostly due to drug use, headaches, and depressive disorders. In Canada, the MNSS burden for women is 5,451 DALYs per 100,000 (UI = 4,871 to 6,100), and they report mostly headaches, depression, and painful somatic syndromes. In Mexico, the MNSS burden for women is 4,001 DALYs per 100,000 (3,600 to 4452), by far the lowest of North America. Mexican women are mostly affected by headaches, depression, and Alzheimer’s disease. Additional notable trends across the three countries are the much larger burden of depression, anxiety, headaches, and eating disorders in females; and of substance use, self-harm, autism spectrum, and conduct disorders in males.
Discussion and Conclusions
Our findings show that MNSS are by far the largest absolute (adjusting for population size and structure) and relative (as a percentage) cause of DALYs and YLDs in the three North American countries studied, most notably in the United States and Canada where they amount to more than a third of the disability and a quarter of disability combined with mortality (in Mexico MNSS account for 32% of YLDs and 17% of DALYs). The burden of MNSS surpasses any other group of NCDs and also exceeds communicable, maternal, neonatal, child and nutritional disorders, and injuries, even in Mexico.
We have also found important differences between countries, including a gradient of MNSS burden which is, in absolute terms, lowest in Mexico, intermediate in Canada, and highest in the United States. Most individual disorders follow this gradient, but there are exceptions worth noting: alcohol use disorders, bipolar disorders, conduct disorders, and epilepsy are higher in Mexico than in the other two countries. Painful somatic syndromes and headaches are higher in Canada than in the United States and lower in Mexico.
With a life-course lens, we have found similarities and differences in the patterns of disease. All countries share the early rise of NCDs and MNSS in particular; the dominance of epilepsy (most notably in Mexico) and autism (in the United States and Canada) during the first years of life; the early and sustained preponderance of common mental disorders and substance use across the three countries, with particularly high impact of self-harm in Mexican youth, of drug use disorders in American and Canadian youth and adults, of alcohol use disorders in Mexican adults, and of headaches throughout adulthood, especially in Mexico and Canada; and the dominance of neurocognitive disorders after 75 years of age across countries. We have also found differential disease patterns in men and women, with men affected mostly by a combination of substance (alcohol and/or drug) use and self-harm (in the United States) plus somatic symptom disorders (in Canada) and headaches (in Mexico) as the top three disorders; and women by a combination of headaches, depression, drug use (in the United States), Alzheimer (in Mexico) and painful somatic symptom disorders (in Canada).
The key strength of this study is its grounding on a clinically and epidemiologically rational framework for attributing disease burden to disorder groupings rather than arbitrary methodological considerations. Indeed, some studies choose to present the burden resulting from MNSS in a fragmentary manner that renders the true burden invisible: Even recent studies separate the burden of mental disorders from that of suicide, neurocognitive disorders, and substance use disorders and ignore painful somatic symptom disorders.4 Spreading the mental health–related disability and mortality across a host of disparate groupings (mental, substance use, musculoskeletal, neurological, cardiovascular disorders, digestive disorders, neoplasms, and injuries) obscures the extent of the burden and may lead decision makers and the public to prioritize coverage for disease groupings which, when appropriately compared, are less burdensome. Of note, without our adjustments, a study of the disease burden related to mental health would have missed every disorder in the top three ranking for men and women in the three countries, with the exception of depression (see Online Appendix 1, Supplementary Tables 1 to 3). These blind spots, coupled with the pervasive structural stigma attached to mental health problems, arguably lead to the current global failure in providing an optimal health system response despite the availability of scalable effective and cost-effective interventions.32
This analysis also has several limitations. First, burden calculations are based on existing prevalence and mortality estimates, and the quality of the data varies among countries. These three countries, however, have a substantial amount of locally produced high-quality estimates, so this should be less of a concern. Second, different countries and cultures conceptualize, understand, and deal with mental and substance disorders differently, and despite the fact that all the studies pooled in the GBD database use standardized diagnostic criteria (i.e., DSM or ICD diagnoses), social and cultural differences can determine (through stigma and availability of services, for example) a lower detection capacity for specific disorders, regions, or countries. Third, the GBD framework to estimate disorder severity and resulting disability does not factor in availability or quality of coverage and assigns the same severity distribution to each disorder irrespective of country income level and health systems considerations. This severity distribution is based on surveys conducted in high-income countries so, arguably, it results in an underestimation of the disability in countries of lower income and coverage.
Notwithstanding these limitations, the findings have important policy implications. A more granular understanding of the disease burden of MNSS in these three countries can strengthen evidence-based policy-making and needs-based planning of services. Traditional health systems planning and policy-making is frequently driven by historic utilization of services plus a measure of advocacy and lobbying, which explains why many health systems (particularly in developing or newly industrialized countries) are still structured to address the societal challenges of maternal and child health and infectious diseases, but not of chronic diseases including MNSS. Even in industrialized countries, the lack of optimal evidence-based needs assessments and prioritization may explain the persistent imbalance in funding and gaps in coverage for MNSS.
The three countries we have studied present important differences in terms of economic development, health systems preparedness, and treatment coverage. A recent study has quantified the imbalance in public mental health spending by ascertaining the ratio of MNSS burden to effectively allocated government spending on mental health for 30 countries in the Americas and found that, in average, the burden of MNSS is 32 times the efficiently allocated spending. Of note, in Mexico, the burden of MNSS is 40 times the spending, while in the United States and Canada, the burden is 3 times the spending, the lowest regional imbalance by far.7 As could be expected from these results, coverage for MNSS in Mexico is very low, with recent studies indicating that only 6% of people with depression and 2.6% of people with substance use disorders receive minimally adequate care.36,37
In the United States, which spends much more on MNSS than Mexico, both in absolute and relative terms, only 26% of people in need get minimally adequate care for depression and 17% for substance use disorders. Despite the Mental Health Parity and Addiction Equity Act and the Affordable Care Act (which seek to increase coverage in general and specifically for MNSS), there is still a majority of Americans who do not have effective mental health coverage.38 The lack of effective coverage is particularly problematic for opioid use disorders, the top cause of DALYs among all MNSS both for men and women. Our findings evoke the phenomenon described by Case and Deaton in 2015, which they poignantly labeled “deaths of despair”: the increasing mortality of White middle-aged men without a college degree.15 Although the GBD data and our analysis do not capture ethnicity nor focus on sociodemographic variables, this increased mortality (which didn’t affect any other demographic group at the time) was caused by drug and alcohol poisoning, cirrhosis and liver disease, and suicide, which map directly to the three causes we identified as carrying the highest disease burden for all men in the United States: drug use disorders, self-harm, and alcohol use disorders. Indeed, a recently released report from the United States Senate reanalyzing the Case and Deaton data confirms these raising mortality trends for suicide, drug, and alcohol-related disorders and finds that they surpass by far “anything seen in America since the dawn of the 20th century,” even removing the deaths due to drug overdose.17
Canada shares these disorders at or near the top of the MNSS disease burden, and though it does provide “universal” medical coverage to its residents, this coverage does not include many mental health treatments including pharmacology and psychotherapy for common mental disorders, such as depression, anxiety, self-harmful behaviors, and painful somatic syndromes, despite the fact that these problems also populate the top disease burden ranking for both men and women in Canada.39 Those without supplemental employment-based private insurance (approximately one-third of the population40) face high barriers in accessing mental health services for these disorders that make up 45% of the MNSS burden during the working years. With respect to drug use disorders, Canada offers much broader coverage when compared to the United States—mainly due to lower financial and regulatory barriers41,42—and the burden is less than half for both men and women, adjusting for population size and structure. Still, the unprecedented impact opioid use disorder is having in the United States (reversing life expectancy gains at the country level) should encourage decision makers in Canada to further increase coverage, mainly by enhancing accessibility and acceptability of treatment options, and by curbing the contamination of the drug supply with fentanyl.
This comparative analysis of the mental health–related disease burden in Canada, Mexico, and the United States seeks to provide policy and decision makers with an evidence-based, clinically informed, epidemiologically meaningful picture that can guide health systems planning to address the most pressing needs of their people. Also, to contribute to the ongoing global endeavor of developing the best possible framework to understand and address mental health problems and disorders.
Supplemental Material
Supplementary_Appendix for Burden of Mental, Neurological, Substance Use Disorders and Self-Harm in North America: A Comparative Epidemiology of Canada, Mexico, and the United States by Daniel Vigo, Laura Jones, Graham Thornicroft and Rifat Atun in The Canadian Journal of Psychiatry
Acknowledgments
We want to acknowledge the contribution of Professor Scott Oser who provided the rationale and the computations required for the propagation of asymmetric errors.
Authors’ Note: All raw data used in this research can be found at: http://ghdx.healthdata.org/gbd-results-tool.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: DV received support from Saint Paul’s Hospital Foundation, the Pan-American Health Organization, and the World Health Organization, as well as from the University of British Columbia and Harvard Medical School. GT is supported by the National Institute for Health Research (NIHR) Collaboration for Leadership in Applied Health Research and Care South London at King’s College London NHS Foundation Trust, and the NIHR Asset Global Health Unit award. The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health and Social Care or other funders. GT receives support from the National Institute of Mental Health of the National Institutes of Health under award number R01MH100470 (Cobalt study). GT is supported by the UK Medical Research Council in relation to the Emilia (MR/S001255/1) and Indigo Partnership (MR/R023697/1) awards. RA and LJ received no specific funding for this research.
ORCID iD: Daniel Vigo, MD, Lic Psych, DrPH  https://orcid.org/0000-0002-4445-4122
https://orcid.org/0000-0002-4445-4122
Supplemental Material: Supplemental material for this article is available online.
References
- 1. World Health Organization. Global Health Observatory (GHO) Data; 2019. Available from: https://apps.who.int/gho/data/node.main.688. [Google Scholar]
- 2. Atun R. Transitioning health systems for multimorbidity. Lancet. 2015;386(9995):721–722. [DOI] [PubMed] [Google Scholar]
- 3. GBD 2017 DALYs and HALE Collaborators. Global, regional, and national disability-adjusted life-years (DALYs) for 359 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1859–1922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. GBD 2017 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1789–1858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Centers for Disease Control and Prevention. National Center for Health Statistics. Available from: https://www.cdc.gov/nchs/hus/contents2017.htm?search=Life_expectancy. [Google Scholar]
- 6. Statistics Canada. Changes in life expectancy by selected causes of death, 2017. The Daily. 2019 May 30. [Google Scholar]
- 7. Vigo DV, Kestel D, Pendakur K, Thornicroft G, Atun R. Disease burden and government spending on mental, neurological, and substance use disorders, and self-harm: cross-sectional, ecological study of health system response in the Americas. Lancet Public Heal. 2019;4(2):e89–e96. [DOI] [PubMed] [Google Scholar]
- 8. Pan American Health Organization. The burden of mental disorders in the region of the Americas. Washington (DC); 2018. [Google Scholar]
- 9. Vigo D, Thornicroft G, Atun R. Estimating the true global burden of mental illness. Lancet Psychiatry. 2016;3(2):171–178. [DOI] [PubMed] [Google Scholar]
- 10. Prince M, Patel V, Saxena S, et al. No health without mental health. Lancet. 2007;370(9590):859–877. [DOI] [PubMed] [Google Scholar]
- 11. Bloom DE, Cafiero E, Jané-Llopis E, et al. The global economic burden of noncommunicable diseases. Geneva: World Economic Forum; 2011. Available from: http://www3.weforum.org/docs/WEF_Harvard_HE_GlobalEconomicBurdenNonCommunicableDiseases_2011.pdf. [Google Scholar]
- 12. Trautmann S, Rehm J, Wittchen HU. The economic costs of mental disorders: do our societies react appropriately to the burden of mental disorders? EMBO Rep. 2016;17(9):1245–1249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Lim KL, Jacobs P, Ohinmaa A, Schopflocher D, Dewa CS. A new population-based measure of the economic burden of mental illness in Canada. Chronic Dis Can. 2008;28(3):92–98. [PubMed] [Google Scholar]
- 14. Mnookin S. Out of the shadows: Making mental health a global development priority. Washington (DC): World Bank Group; 2016. [Google Scholar]
- 15. Case A, Deaton A. Rising morbidity and mortality in midlife among white non-Hispanic Americans in the 21st century. Proc Natl Acad Sci. 2015;111(49):15078–15083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Dyer O. US life expectancy falls for third year in a row. BMJ. 2018;363:k5118. [DOI] [PubMed] [Google Scholar]
- 17. Joint Economic Committee United States Senate. Long-term trends in deaths of despair. Washington (DC): Joint Economic Committee United States Senate; 2019. [Google Scholar]
- 18. BC Centre for Disease Control. The BC public health opioid overdose emergency. Obs Popul Public Heal. 2017. [Google Scholar]
- 19. Slaunwhite A, Chloé X. Preliminary results from the 2017 B.C. Provincial Overdose Cohort Refresh. 2009. Available from: http://www.bccdc.ca/resource-gallery/Documents/StatisticsandResearch/StatisticsandReports/Overdose/20190531_BCCDCKnowledgeUpdate_2017CohortRefresh_final.pdf. [Google Scholar]
- 20. Saxena S, Thornicroft G, Knapp M, Whiteford H. Resources for mental health: scarcity, inequity, and inefficiency. Lancet. 2007;370(9590):878–889. [DOI] [PubMed] [Google Scholar]
- 21. Henderson C, Noblett J, Parke H, et al. Mental health-related stigma in health care and mental health-care settings. Lancet Psychiatry. 2014; 1(6):467–482. [DOI] [PubMed] [Google Scholar]
- 22. Lasalvia A., Zoppei S, Van Bortel T, et al. Global pattern of experienced and anticipated discrimination reported by people with major depressive disorder: a cross-sectional survey. Lancet (London, England). 2013;381(9860):55–62. [DOI] [PubMed] [Google Scholar]
- 23. Thornicroft G, Brohan E, Rose D, Sartorius N, Leese M. Global pattern of experienced and anticipated discrimination against people with schizophrenia: a cross-sectional survey. Lancet. 2009;373(9661):408–415. [DOI] [PubMed] [Google Scholar]
- 24. World Health Organization. International Classification of Diseases, Tenth Revision (ICD-10). Geneva, Switzerland; 2010. [Google Scholar]
- 25. Murray CJ, Ezzati M, Flaxman AD, et al. GBD 2010: Design, definitions, and metrics. Lancet. 2012;380(9859):2063–2066. [DOI] [PubMed] [Google Scholar]
- 26. Salomon JA, Haagsma JA, Davis A, et al. Disability weights for the Global Burden of Disease 2013 study. Lancet Glob Heal. 2015;3(11):e712–723. [DOI] [PubMed] [Google Scholar]
- 27. Salomon JA, Vos T, Hogan DR, et al. Common values in assessing health outcomes from disease and injury: disability weights measurement study for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2129–2143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. American Psychiatric Association. Diagnostic and statistical manual of mental disorders, fifth revision, (DSM-5). Washington (DC); 2013. [Google Scholar]
- 29. American Psychiatric Association. Diagnostic and statistical manual of mental disorders, fourth revision, text revision (DSM-IV-TR). Washington (DC); 2000. [Google Scholar]
- 30. Whiteford HA, Degenhardt L, Rehm J, et al. Global burden of disease attributable to mental and substance use disorders: findings from the Global Burden of Disease Study 2010. Lancet. 2013;382(9904):1575–1586. [DOI] [PubMed] [Google Scholar]
- 31. Lang JJ, Alam S, Cahill LE, et al. Global burden of disease study trends for Canada from 1990 to 2016. Can Med Assoc J. 2018;190(44):E1296–E1304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Vigo DV, Patel V, Becker A, et al. A partnership for transforming mental health globally. Lancet Psychiatry. 2019;6(4):350–356. [DOI] [PubMed] [Google Scholar]
- 33. Fröhlich C, Jacobi F, Wittchen HU. DSM-IV pain disorder in the general population. An exploration of the structure and threshold of medically unexplained pain symptoms. Eur Arch Psychiatry Clin Neurosci. 2006;256(3):187–196. [DOI] [PubMed] [Google Scholar]
- 34. Vigo DV, Selle V, Baldessarini R., Enduring pain I. Nosology and epidemiology. Vertex. 2013;24(111):345–350. [PubMed] [Google Scholar]
- 35. Roger Barlow. Asymmetric Statistical Errors. arXiv: physics/0406120v1 [physics.data-an] [Google Scholar]
- 36. Degenhardt L, Glantz M, Evans-Lacko S, et al. Estimating treatment coverage for people with substance use disorders: an analysis of data from the World Mental Health Surveys. World Psychiatry. 2017;16(3):299–307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Thornicroft G, Chatterji S, Evans-Lacko S, et al. Undertreatment of people with major depressive disorder in 21 countries. Br J Psychiatry. 2016;210(2):119–124. doi:10.1192/bjp.bp.116.188078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Berchick E, Hood E, Barnett E. Health insurance coverage in the United States: 2017 Report Number P60-264. 2018. [Google Scholar]
- 39. Martin D, Miller AP, Quesnel-Vallée A, Caron NR, Vissandjée B, Marchildon GP. Canada’s universal health-care system: achieving its potential. Lancet. 2018;391(10131):1718–1735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Mossialos E, Wenzl M, Osborn R, Sarnak D. (Eds.). 2015 International Profiles of Health Care Systems. The Commonwealth Fund, January 2016; 2016. [Google Scholar]
- 41. Priest KC, Gorfinkel L, Klimas J, Jones AA, Fairbairn N, McCarty D. Comparing Canadian and United States opioid agonist therapy policies. Int J Drug Policy. 2019. doi:10.1016/j.drugpo.2019.01.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Sharma A, Kelly SM, Mitchell SG, Gryczynski J, O’Grady KE, Schwartz RP. Update on barriers to pharmacotherapy for opioid use disorders. Curr Psychiatry Rep. 2017;19(6):35. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary_Appendix for Burden of Mental, Neurological, Substance Use Disorders and Self-Harm in North America: A Comparative Epidemiology of Canada, Mexico, and the United States by Daniel Vigo, Laura Jones, Graham Thornicroft and Rifat Atun in The Canadian Journal of Psychiatry