Abstract
Aims.
Prevalence and covariates of subclinical psychosis have gained increased interest in the context of early identification and treatment of persons at risk for psychosis.
Methods.
We analysed 9829 adults representative of the general population within the canton of Zurich, Switzerland. Two psychosis syndromes, derived from the SCL-90-R, were applied: ‘schizotypal signs’ and ‘schizophrenia nuclear symptoms’.
Results.
Only a few subjects (13.2%) reported no schizotypal signs. While 33.2% of subjects indicated mild signs, only a small proportion (3.7%) reported severe signs. A very common outcome was no ‘schizophrenia nuclear symptoms’ (70.6%). Although 13.5% of the participants reported mild symptoms, severe nuclear symptoms were very rare (0.5%). Because these two syndromes were only moderately correlated (r = 0.43), we were able to establish sufficiently distinct symptom clusters. Schizotypal signs were more closely connected to distress than was schizophrenia nuclear symptoms, even though their distribution types were similar. Both syndromes were associated with several covariates, such as alcohol and tobacco use, being unmarried, low education level, psychopathological distress and low subjective well-being.
Conclusions.
Subclinical psychosis symptoms are quite frequent in the general population but, for the most part, are not very pronounced. In particular, our data support the notion of a continuous Wald distribution of psychotic symptoms in the general population. Our findings have enabled us to confirm the usefulness of these syndromes as previously assessed in other independent community samples. Both can appropriately be associated with well-known risk factors of schizophrenia.
Key words: Attenuated psychosis syndrome, epidemiology, schizotypy, subclinical psychosis
Introduction
Although significant variability exists between incidence and prevalence rates of schizophrenia, the average annual incidence is about 0.2 per 1000 persons, with a lifetime prevalence of 0.4–0.7% (Rössler et al. 2005). While schizophrenia can be considered a relatively rare disease, subclinical psychosis symptoms are much more frequent in the general population (Scott et al. 2006; Rössler et al. 2007) and in socio-culturally different countries (Loch et al. 2011). These symptoms are commonly referred to as psychotic-(like) experiences, proneness to psychosis, at-risk mental state, schizotypy or exceptional experiences (Fach et al. 2013). A recent systematic review of 61 reported incidence and prevalence studies of population rates for subclinical psychosis symptoms revealed a median prevalence rate of 7.2% and a median annual incidence rate of 2.5%, with significant variation detected in those rates (Linscott & van Os, 2013).
Subclinical psychosis symptoms, although not always of clinical relevance (Johns & van Os 2001), can have predictive power for the onset of clinical psychotic disorders later in life (van Os et al. 2000). As such, the topic has gained increased interest within the context of early identification and treatment of persons at risk for psychosis. Because of various early intervention programmes, a new category was proposed for introduction in DSM-5 to address this ‘psychosis risk syndrome’, which describes a condition ‘with recent onset of modest psychotic-like symptoms and clinically relevant distress and disability’ (Tsuang et al. 2013). However, the data showed that only a minority of persons develops a diagnosable psychotic disorder (Fusar-Poli et al. 2012). Another newly discussed category, the ‘attenuated psychosis syndrome’, did not necessarily imply a transition of subclinical psychosis to a full psychotic disorder. It also was discounted because certainty was lacking about its validity and reliability. Moreover, it was unclear how this attenuated psychosis syndrome could be delimited from a schizotypal personality disorder (Tsuang et al. 2013).
One explanation for the fuzziness of this concept is the ‘near Babylonian speech confusion’ within this field. Schultze-Lutter et al. (2011) have argued that this at-risk nomenclature lacks clarity with the emergence of ever-new terms and concepts. Indeed, no comprehensive picture currently describes what actually constitutes subclinical psychosis. Therefore, to reduce its heterogeneity of assessed symptoms, researchers must define more general psychopathological categories.
We have previously employed several independent community samples and populations – in particular, data from the ‘Zurich Study’ (Angst et al. 2005) – to evaluate subclinical psychosis with higher-order syndromes, as derived from the SCL-90-R. In that unique small-community sample, which we followed longitudinally over 30 years, we identified subclinical psychosis syndromes with relevant distress and functional disability (Rössler et al. 2007). Although none of those participating individuals developed a psychotic disorder, persons with persisting subclinical psychosis syndromes were found to be at risk for developing other mental disorders (Rössler et al. 2011a).
To validate some of these results, we have now conducted a cross-sectional study in which we analysed those two previously established psychosis syndromes. Here, a new, much larger sample of adults, 20–41 years old, was followed. They were considered representative of the general population of the canton of Zurich, Switzerland. Our objectives were to (i) determine the distribution of these syndromes, (ii) estimate their prevalence and comorbidity, and (iii) investigate their associations using several covariates.
Methods
Study design and sampling
This study was conducted as part of the ‘Zurich Programme for Sustainable Development of Mental Health Services’ (ZInEP, i.e. ‘Zürcher Impulsprogramm zur nachhaltigen Entwicklung der Psychiatrie’). This broadly based public mental health research programme is located in the canton of Zurich. The Epidemiology Survey, one of six ZInEP subprojects, comprises four parts: (1) telephone screening; (2) comprehensive, semi-structured face-to-face interviews with a stratified subsample; (3) socio-physiological laboratory examination; and (4) a longitudinal survey. Its design was adapted from the longitudinal Zurich cohort-study (Angst et al. 2005). For the present analysis, we used data from the first step of the survey – the telephone screening – collected between August 2010 and May 2012.
The 9829 Swiss male and female participants were aged 20–41 years at the onset of the survey and were representative of the general population of the Zurich canton. All were screened through a computer-assisted telephone interview (CATI) that utilised the Symptom Checklist-27 (SCL-27) (Hardt et al. 2004) plus items from the psychoticism and paranoid ideation subscales of the SCL-90-R (Derogatis, 1977). Additional items included assessments of socio-demography and substance use.
Participants were randomly selected through the registration offices of all municipalities within the canton, and residents without Swiss nationality were excluded. In accordance with detailed instructions from the research team, a leading marketing and field research institute (GfK ‘Growth for Knowledge’), conducted each CATI. In all, 14 professional telephone interviewers were employed, with seven of them covering 76% of all 9829 interviews. The overall response rate was 53.6%. Reasons for non-response were no telephone connection, only telephone answering machine, incorrect telephone number, communication impossible, unavailability during the study period, or refusal by a the targeted person him/herself or a third person. In cases where potential participants were available by telephone, the response rate was 73.9%.
The Cantonal Ethics Committee (KEK) of Zurich approved the ZInEP Epidemiology Survey to fulfil all legal and data privacy protection requirements. The survey was performed in strict accordance with the Declaration of Helsinki of the World Medical Association. All participants gave their written informed consent.
Instruments and measures
The SCL-27 (Hardt et al. 2004) is a German short-form of the well-known SCL-90-R (Derogatis, 1977), which is used to report a wide variety of psychiatric symptoms over the most recent 4-week period. Subjects respond according to a five-point Likert scale that ranges from (1) ‘not at all’ to (5) ‘extremely’. Six subscales of symptoms are included: depressive, dysthymic, vegetative, agoraphobic, socio-phobic and mistrust. A total distress score similar to the GSI in the SCL-90-R is also available. Cronbach's α for the subscales are all greater 0.70 and Cronbach's α for the GSI is 0.93. The correlation between the GSI of the SCL-27 and the GSI of the SCL-90-R is r = 0.95 (Hardt et al. 2004). Here, we added items from the psychoticism and paranoid ideation subscales of the original SCL-90-R to those of the mistrust subscale. This provided two re-arranged subscales of subclinical psychosis that we had previously established in the Zurich Study (Rössler et al. 2007). The first new subscale was used to address social and interpersonal deficiencies, as evidenced by a reduced capacity for close relationships as well as ideas of reference, odd beliefs, and suspicion/paranoid ideation. As such, this factor was reminiscent of symptoms corresponding to a schizotypal personality disorder. Thus, we named this subscale ‘schizotypal signs’. The second new subscale – ‘schizophrenia nuclear symptoms’ – included items of thought insertion, thought-broadcasting, thought control and hearing voices (Table 1). Those symptoms represent attenuated forms of the nuclear symptoms of schizophrenia. A detailed description of the development of these subscales is provided elsewhere (see Rössler et al. 2007). They have also been replicated and applied in other representative samples (Breetvelt et al. 2010; Rössler et al. 2011b). Categories of distress for both subscales were defined as follows: ‘no distress’, with a mean value <1.00; ‘low distress’, 1.01–1.49; ‘moderate distress’, 1.50–1.99; ‘high distress’, 2.00–2.99; and ‘extreme distress’, with a mean value >2.99
Table 1.
Items for the new subscales of ‘schizophrenia nuclear symptoms’ and ‘schizotypal signs’ that replace those for the ‘paranoid ideation’ (PN) and ‘psychoticism’ (PS) subscales from the original SCL-90-R
| New SCL-90-R items | Original SCL-90-R subscalea | |
|---|---|---|
| Schizophrenia nuclear symptoms subscale | ||
| 7: | Someone else can control your thoughts | PS |
| 16: | Hearing voices other people do not hear | PS |
| 35: | Other being aware of your thoughts | PS |
| 62: | Having thoughts that are not your own | PS |
| Schizotypal signs subscale | ||
| 8: | Others are to blame for your troubles | PN |
| 18: | Feeling most people cannot be trusted | PN |
| 43: | Feeling you are watched by others | PN |
| 68: | Having ideas others do not share | PN |
| 76: | Others not giving you proper credit | PN |
| 77: | Feeling lonely even when with people | PS |
| 83: | Feeling people take advantage of you | PN |
| 88: | Never feeling close to another person | PS |
aItems excluded from the original PS subscale are 84: Thoughts about sex that bother you a lot; 85: Idea you should be punished for sins; 87: Idea something is wrong with your body; and 90: Idea something is wrong with your mind.
All other variables included in the analysis were also assessed during the CATI, with most proposing a single question and standardised response options. Topics covered alcohol use, smoking, children, civil state, housing and sex, as well as a self-evaluation of the individual's satisfaction with their mental health and a comparison with that of other persons. In addition, participants were asked about abusive drinking and level of education. The former was assessed with the question, ‘Some people may have a drink too much at a party or special occasion. Does this happen to you as well from time to time?’. Education level was defined as ‘low’ when high school or simple occupation was the highest level achieved, ‘moderate’ when college or specialised occupation was the uppermost, and ‘high’ when university was the highest degree attained.
Statistical analysis
Associations between the categories of ‘schizotypal signs’ and ‘schizophrenia nuclear symptoms’ were analysed with contingency tables and χ2 tests. Associations with the continuous psychosis subscales were examined with generalised linear models. Since both subscales were heavily peaked and right-skewed, we fitted models with an inverse Gauss distribution and log-link function. A robust estimator was used to reduce the effects of outliers and influential observations. Results were reported either with mean values when related to categorical predictors or with standardised regression coefficients (β) when related to continuous predictors. All analyses were performed with SPSS version 20 for Macintosh.
Results
The sample comprised 4908 females and 4919 males. Ranging from 20 to 41 years, the mean age was 28.9 (s.d. = 7.1). Most interviewed subjects were unmarried (66.9%), followed by married (30.9%), and separated/divorced/widowed (2.3%). A total of 2795 (28.4%) reported having children. Finally, education levels were low for 43.6% of participants, moderate for 38.0% and high for 18.4%.
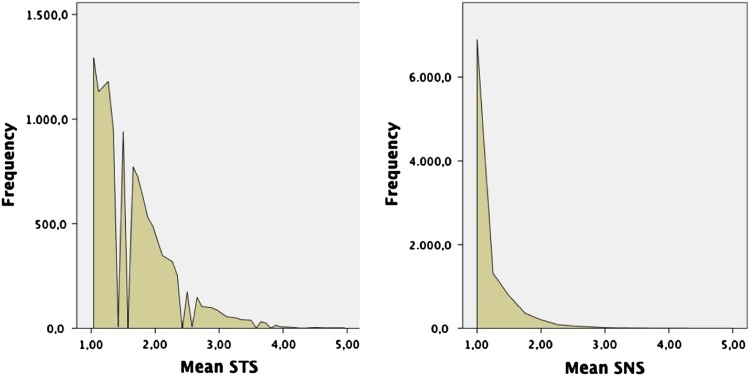
The distribution of our two psychosis subscales was inspected in detail (Fig. 1). ‘Schizotypal signs’ ranged from 1 to 5, with a mean of 1.623 (s.d. = 0.572), median of 1.5, skewness of 1.385 (s.e. = 0.025), and a kurtosis of 2.257 (s.e. = 0.049). ‘Schizophrenia nuclear symptoms’ also ranged from 1 to 5, but had a clearly lower mean of 1.159 (s.d. = 0.332), median of 1.0, skewness of 3.319 (s.e. = 0.025), and a large kurtosis of 15.989 (s.e. = 0.050). The common feature between them was their clear representation of an inverse Gaussian distribution (also known as a Wald distribution). The Spearman correlation between both syndromes was r = 0.434 (p < 0.001).
Fig. 1.
Distribution of ‘schizotypal signs’ (left) and ‘schizophrenia nuclear symptoms’ (right).
Categorisation of both subscales yielded the frequencies listed in Table 2. Most subjects reported low (33.2%) or moderate (30.2%) distress in ‘schizotypal signs’. A state of ‘no distress’ was rather uncommon (13.2%) and extreme distress was very rare (3.7%). In contrast, distress in ‘schizophrenia nuclear symptoms’ showed an exponential decline. The vast majority reported no distress (70.6%), followed by low (13.5%) and moderate (11.6%) distress. Only 0.5% reported extreme distress.
Table 2.
Frequency of categories for ‘schizotypal signs’ and ‘schizophrenia nuclear symptoms’
| Schizotypal signs | Schizophrenia nuclear symptoms | |||
|---|---|---|---|---|
| N | % | N | % | |
| No distress | 1293 | 13.2 | 6895 | 70.6 |
| Low distress | 3266 | 33.2 | 1315 | 13.5 |
| Moderate distress | 2966 | 30.2 | 1136 | 11.6 |
| High distress | 1938 | 19.7 | 380 | 3.9 |
| Extreme distress | 364 | 3.7 | 44 | 0.5 |
| Total | 9827 | 100.0 | 9770 | 100.0 |
The contingency table for distress categories is shown in Table 3. As expected, values were statistically highly significant (Pearson χ2 = 2652.96, df = 16, p < 0.001). Interestingly, none of the subjects with extreme distress in ‘schizophrenia nuclear symptoms’ reported no, low, or moderate ‘schizotypal signs’ distress. By comparison, 877 subjects with no ‘schizophrenia nuclear symptoms’ distress also reported high ‘schizotypal signs’ distress (representing 45.5% of all subjects in that ‘schizotypal signs’ category) while 87 reported even extreme ‘schizotypal signs’ distress (24.3%).
Table 3.
Contingency table of categories for distress within ‘schizotypal signs’ and ‘schizophrenia nuclear symptoms’
| Schizophrenia nuclear symptoms distress | ||||||
|---|---|---|---|---|---|---|
| No (%) | Low (%) | Moderate (%) | High (%) | Extreme (%) | ||
| Schizotypal signs distress | No | 95.9 | 2.7 | 1.2 | 0.2 | 0.0 |
| Low | 83.7 | 10.8 | 5.1 | 0.4 | 0.0 | |
| Moderate | 67.1 | 17.6 | 12.9 | 2.4 | 0.0 | |
| High | 45.5 | 18.9 | 24.9 | 9.8 | 0.9 | |
| Extreme | 24.3 | 12.8 | 26.3 | 29.1 | 7.5 | |
Table 4 presents the various factors related to ‘schizotypal signs’ and ‘schizophrenia nuclear symptoms’. Except for sex, all variables included in this analysis had a statistically significant association with ‘schizotypal signs’. However, inspection of the effect sizes for standardised mean differences revealed that most associations were rather weak. A mean ‘schizotypal signs’ difference of 0.11 represented a small effect; 0.29, medium; and 0.45, large. Accordingly, most differences were small or small-to-medium. The largest effects with respect to ‘schizotypal signs’ were found for the mean differences between no alcohol use and daily use (mean difference = 0.21) as well as between married and separated/divorced/widowed (mean difference = 0.23). In a multivariate analyses where all predictors were entered simultaneously daily alcohol use, daily smoking and low education remained the strongest independent predictors. As for ‘schizophrenia nuclear symptoms’, abusive drinking and having children yielded no statistically significant association. Sex was statistically significant, but the effect size was marginally small and not of practical significance. Small, medium and large effects corresponding to ‘schizophrenia nuclear symptoms’ had mean differences of 0.06, 0.16 and 0.26, respectively. Thus, most statistically significant effects found for ‘schizophrenia nuclear symptoms’ represented marginally small effects (<0.06). The largest effects were found for the mean ‘schizophrenia nuclear symptoms’ difference between drinking daily v. several times per week (mean difference = 0.10) as well as between low and high education levels (mean difference = 0.10). When adjusted for each other, the strongest multivariate predictors were clearly low education and daily alcohol use. Psychopathological syndromes were all statistically significantly related to both subscales. For ‘schizotypal signs’ the effects ranged from medium (β > 0.3) to large (β > 0.5) size and they were substantially larger than the moderate effects found in ‘schizophrenia nuclear symptoms’. In each case, the strongest psychopathological association of both subscales was the socio-phobic syndrome (β = 0.70 and 0.40 for ‘schizotypal signs’ and ‘schizophrenia nuclear symptoms’, respectively).
Table 4.
Associations of ‘schizotypal signs’ and ‘schizophrenia nuclear symptoms’, adjusted for sex and age. Values followed by a different superscript within a column vary significantly at corrected p < 0.05
| Schizotypal signs | Schizophrenia nuclear symptoms | ||||
|---|---|---|---|---|---|
| Mean (95% CI) | Sig.* | Mean (95% CI) | Sig.* | ||
| Alcohol use | No | 1.65a (1.62; 1.68) | 0.000 | 1.18a (1.17; 1.20) | 0.000 |
| >1 per month | 1.61b (1.59; 1.63) | 1.15b (1.14; 1.17) | |||
| >1 per week | 1.61b (1.59; 1.62) | 1.15b (1.14; 1.16) | |||
| Daily | 1.86c (1.77; 1.95) | 1.25c (1.20; 1.30) | |||
| Abusive drinking | No | 1.59a (1.57; 1.60) | 0.000 | 1.15a (1.13; 1.16) | 0.100 |
| Yes | 1.64b (1.62; 1.65) | 1.16a (1.15; 1.17) | |||
| Smoking | No | 1.57a (1.56; 1.58) | 0.000 | 1.14a (1.13; 1.15) | 0.000 |
| Occasionally | 1.67b (1.63; 1.71) | 1.17b (1.15; 1.20) | |||
| Daily | 1.76c (1.74; 1.79) | 1.21c (1.20; 1.23) | |||
| Having children | No | 1.66a (1.64; 1.67) | 0.000 | 1.16a (1.15; 1.17) | 0.058 |
| Yes | 1.54b (1.51; 1.56) | 1.15a (1.13; 1.16) | |||
| Civil state | Unmarried | 1.66a (1.65; 1.68) | 0.000 | 1.16a (1.15; 1.17) | 0.014 |
| Married | 1.53b (1.51; 1.55) | 1.14a (1.13; 1.16) | |||
| Sep/div/widowed | 1.76c (1.67; 1.85) | 1.21a (1.15; 1.27) | |||
| Housing | Alone | 1.77a (1.73; 1.80) | 0.000 | 1.19a (1.16; 1.21) | 0.005 |
| Community | 1.60b (1.59; 1.61) | 1.15b (1.15; 1.16) | |||
| Education | Low | 1.67a (1.65; 1.69) | 0.000 | 1.20a (1.19; 1.21) | 0.000 |
| Moderate | 1.60b (1.58; 1.62) | 1.14b (1.13; 1.15) | |||
| High | 1.55c (1.52; 1.57) | 1.10c (1.09; 1.12) | |||
| Sex** | Males | 1.62a (1.60; 1.63) | 0.307 | 1.15a (1.14; 1.16) | 0.012 |
| Females | 1.61a (1.61; 1.64) | 1.17b (1.16; 1.18) | |||
| β (s.e.) | Sig.* | β (s.e.) | Sig.* | ||
| Age*** | 1 s.d. increase | –0.062 (0.010) | 0.000 | –0.052 (0.010) | 0.000 |
| Depressive | 1 s.d. increase | 0.619 (0.011) | 0.000 | 0.375 (0.017) | 0.000 |
| Dysthymic | 1 s.d. increase | 0.534 (0.011) | 0.000 | 0.344 (0.016) | 0.000 |
| Vegetative | 1 s.d. increase | 0.490 (0.012) | 0.000 | 0.351 (0.019) | 0.000 |
| Agoraphobic | 1 s.d. increase | 0.489 (0.014) | 0.000 | 0.385 (0.022) | 0.000 |
| Socio-phobic | 1 s.d. increase | 0.698 (0.010) | 0.000 | 0.404 (0.017) | 0.000 |
*Test of model effect.
**Adjusted only for age.
***Adjusted only for sex.
Table 5 lists the subjective appraisal of participants' mental health. Distress in both subscales increased exponentially with higher dissatisfaction. Subjects who showed markedly increased distress in ‘schizotypal signs’ and ‘schizophrenia nuclear symptoms’ were very dissatisfied with their mental health and appraised it as being much worse compared with that of other persons. Each category differed significantly from all others. The corresponding effect sizes were large.
Table 5.
Subjective appraisal of mental health in association with ‘schizotypal signs’ and ‘schizophrenia nuclear symptoms’, adjusted for sex and age. Values followed by a different superscript within a column vary significantly at corrected p < 0.05
| Schizotypal signs | Schizophrenia nuclear symptoms | ||||
|---|---|---|---|---|---|
| Mean (s.e.) | Sig.* | Mean (s.e.) | Sig.* | ||
| Individual satisfaction with mental health | Very low | 2.71a (0.09) | 0.000 | 1.69a (0.09) | 0.000 |
| Low | 2.34b (0.04) | 1.37b (0.03) | |||
| Moderate | 1.99c (0.02) | 1.27c (0.01) | |||
| High | 1.63d (0.01) | 1.16d (0.01) | |||
| Very high | 1.40e (0.01) | 1.09e (0.00) | |||
| Comparison of mental health with others | Much worse | 2.59a (0.09) | 0.000 | 1.55a (0.09) | 0.000 |
| Worse | 2.12b (0.03) | 1.29b (0.02) | |||
| Equal | 1.67c (0.01) | 1.17c (0.01) | |||
| Better | 1.55d (0.01) | 1.14d (0.00) | |||
| Much better | 1.46e (0.01) | 1.11e (0.01) | |||
*Test of model effect.
Discussion
This study was conducted within a population deemed to be at higher risk for mental disorders, i.e. persons between the ages of 20 and 41. Our sample group was obtained from a pool of almost 10 000 persons representative of the general population in the canton of Zurich, Switzerland. Although a considerable part of the general population had indicated some kind of psychosis symptoms, only a small proportion of that was connected with severe symptoms.
The two syndromes were only moderately correlated, i.e. establishing sufficiently distinct symptom clusters. In particular, we noted that ‘schizotypal signs’ was more connected to distress than was attenuated forms of ‘schizophrenia nuclear symptoms’, even though their distribution types were similar. The only difference was that the distribution of ‘schizophrenia nuclear symptoms’ was more heavily peaked (demonstrating a higher kurtosis), meaning that more subjects were situated at the lower extreme of the distribution when compared with ‘schizotypal signs’. The typically inverse Gaussian, or Wald, distribution was to be expected for a continuously distributed symptom within the general population. We act on the assumption of a Wald distribution, i.e. continuously declining values from no/low symptom load over moderate symptom load to high/extreme symptom load. We don't find in our distribution a ‘zone of rarity’, characterised by very low values between no/low and high/extreme values, which would clearly constitute two distinct groups.
In epidemiological terms, the distribution type can give us some hints of underlying causes of the presumed continuum. Assumed that psychosis is a multifactorial disorder comparable to other chronic disorders such as diabetes, the observed distribution of the characteristic under investigation depends on the degree to which these causes interact, their prevalence and the degree to which their effect sizes differ (Johns & van Os, 2001). If the effects of the causes were moderate and contributed additively, we could expect a Gaussian distribution. If the causes contributed both independently and in interaction, we expect an inverse Gaussian distribution. We found the latter distribution type in our study.
While we found a rather broad distribution of distress in persons with ‘schizotypal signs’, an exponential decline was noted in ‘schizophrenia nuclear symptoms’. That is, most persons indicating the latter displayed no distress. This possibly meant that their ‘schizophrenia nuclear symptoms’ were rather rare events whereas ‘schizotypal signs’ were much more pervasive and, as such, more distressing.
The contingency table showed that subjects scoring high on ‘schizophrenia nuclear symptoms’ scored similarly high on ‘schizotypal signs’, whereas subjects scoring high on the latter scored rather low or moderate on the former. Again, persons who suffered primarily from ‘schizotypal signs’ might have only occasionally displayed ‘schizophrenia nuclear symptoms’, whereas those with distressing ‘schizophrenia nuclear symptoms’ in the foreground were affected pervasively in ‘schizotypal signs’.
The two syndromes were related to various covariates, although mostly rather weak. The associations with alcohol and tobacco use are replications of well-established findings (Degenhardt & Hall, 2001; Compton et al. 2009; Rössler et al. 2012a). One association with the psychopathological feature of social phobia is somewhat tautological because, by definition, ‘schizotypal signs’ are especially linked with distrust in social relationships. Nevertheless, a systematic review also provides some evidence that social and interpersonal dysfunctions may predate the onset of psychotic symptoms (Gayer-Anderson & Morgan, 2013). Interestingly we found no important sex differences even though they have long been reported in full-blown psychosis (McGrath et al. 2008). Thus, those differences in psychosis apparently manifest themselves at the high end of the continuum (full-blown schizophrenia) rather than within the subthreshold range. Here, we confirmed results from a previous analysis of the Zurich cohort study, in which we also could not identify substantial sex differences in subclinical psychosis (Rössler et al. 2012b). This finding is also in line with that from the large meta-analysis of Linscott & van Os (2013).
By focusing on subthreshold syndromes, we have provided evidence for subclinical psychosis syndromes that are quite common in the general population. This has enabled us to avoid restricting the validity of these results only to specific high-risk groups, as currently investigated in early psychosis-detection programmes. Such population-based studies will allow researchers to investigate the occurrence of psychotic symptoms before psychopathology becomes clinically relevant. Nevertheless, we could previously demonstrate that a high symptom load of the two syndromes assessed, is associated with various kinds of functional impairments (Rössler et al. 2007). Furthermore, those symptoms will be meaningful for prevention and intervention programmes, because we have already demonstrated that they may predispose a person to a wide range of mental disorders (Rössler et al. 2011a). Finally, subclinical psychosis detrimentally impacts the course and severity of affective disorders (Wigman et al. 2012), and it constitutes a risk factor for suicidal behaviour (Kelleher et al. 2012). Accordingly, we have determined in our study that the two syndromes are not meaningless for the lives of affected persons. In particular, ‘schizotypal signs’ impair the subjective well-being and satisfaction with mental health when compared with others. This is much less the case with respect to ‘schizophrenia nuclear symptoms’, probably because those symptoms are not as frequent and pervasive.
In summary, our description of these two sufficiently discrete syndromes can reduce the heterogeneity of symptoms associated with subclinical psychosis. In this study we verified the usefulness of those syndromes as previously assessed in other representative samples (Rössler et al. 2007, 2011b; Breetvelt et al. 2010). Both syndromes feature similar syndromes that are used to characterise full-blown psychosis. Therefore, they are particularly appropriate for describing the psychosis continuum.
However, the present study did involve some limitations. The telephone interviews were conducted by laypersons, and the assessed variables were quite restricted in number and detail. Nevertheless, we were able to canvass a large representative sample when compared with most other investigations that have focused on subclinical psychosis within a general population. Information about service use was not available for this large screening sample. Therefore, we do not know how professional treatment may eventually have affected our results.
In addition to the more specific limitations of our study, there are some more general concerns about assessment approaches in psychiatric epidemiology. Firstly, the content of the described phenomena can never go beyond the actually assessed symptoms or signs. That is to say that we cannot definitely decide if the two syndromes identified are natural entities or resulting from the structure of our questionnaires. As such the applied questionnaires determine the content and the distribution type of the epidemiological findings. Additionally, the fewer items assessed the more rough the estimates will be.
Concerning our research question we find two types of items, the ones representing the same symptoms as seen in manifest psychosis, i.e. schizophrenia nuclear symptoms but less pronounced in intensity and quantity and attenuated psychosis symptoms, i.e. weaker as described in ‘schizotypal signs’ compared with full-blown symptoms. The former type of symptoms suggests that this type of symptom only turns into a disorder, e.g. depending on the degree of subjective distress or in a certain cultural context implying various levels of societal tolerance. The latter type of symptoms (schizotypal signs) is an attenuated form with varying degrees of severity along a continuum, i.e. precursors of a psychotic disorder. The continuity of symptoms is implied as on inspection the values of our scale are continuously decreasing from ‘no/low’ to ‘high/extreme’. But we cannot hypothesise a continuum from normal experiences to clinical phenomena, as we did not assess manifest psychosis in our sample.
Acknowledgements
We thank Professor Jules Angst for his continuing and encouraging support of our epidemiological studies.
Financial Support
ZInEP was supported by a private Foundation. The Foundation had no further role in the design of the study; the collection, analysis and interpretation of data; the writing of this report; or the decision to submit this paper for publication.
Conflict of Interest
None.
Ethical standard
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
References
- Angst J, Gamma A, Neuenschwander M, Ajdacic-Gross V, Eich D, Rössler W, Merikangas KR (2005). Prevalence of mental disorders in the Zurich cohort study: a twenty year prospective study. Epidemiologia e Psichiatria Sociale 14, 68–76. [DOI] [PubMed] [Google Scholar]
- Breetvelt EJ, Boks MP, Numans ME, Selten JP, Sommer IE, Grobbee DE, Kahn RS, Geerlings MI (2010). Schizophrenia risk factors constitute general risk factors for psychiatric symptoms in the population. Schizophrenia Research 120, 184–190. [DOI] [PubMed] [Google Scholar]
- Compton MT, Kelley ME, Ramsay CE, Pringle M, Goulding SM, Esterberg ML, Stewart T, Walker EF (2009). Association of pre-onset cannabis, alcohol, and tobacco use with age at onset of prodrome and age at onset of psychosis in first-episode patients. American Journal of Psychiatry 166, 1251–1257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Degenhardt L, Hall W (2001). The association between psychosis and problematical drug use among Australian adults: findings from the National Survey of Mental Health and Well-Being. Psychological Medicine 31, 659–668. [DOI] [PubMed] [Google Scholar]
- Derogatis LR (1977). Symptom Checklist 90, R-Version Manual I: Scoring, Administration, and Procedures for the SCL-90. Johns Hopkins Press: Baltimore, MD. [Google Scholar]
- Fach W, Atmanspacher H, Landolt K, Wyss T, Rössler W (2013). A comparative study of exceptional experiences of clients seeking advice and of subjects in an ordinary population. Frontiers in Psychology 4, 65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fusar-Poli P, Bonoldi I, Yung AR, Borgwardt S, Kempton MJ, Valmaggia L, Barale F, Caverzasi E, McGuire P (2012). Predicting psychosis: meta-analysis of transition outcomes in individuals at high clinical risk. Archives of General Psychiatry 69, 220–229. [DOI] [PubMed] [Google Scholar]
- Gayer-Anderson C, Morgan C (2013). Social networks, support and early psychosis: a systematic review. Epidemiology and Psychiatric Sciences 22, 131–146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hardt J, Egle UT, Kappis B, Hessel A, Brahler E (2004). Symptom Checklist SCL-27: results of a representative German survey. Psychotherapie Psychosomatik Medizinische Psychologie 54, 214–223. [DOI] [PubMed] [Google Scholar]
- Johns LC, van Os J (2001). The continuity of psychotic experiences in the general population. Clinical Psychology Review 21, 1125–1141. [DOI] [PubMed] [Google Scholar]
- Kelleher I, Lynch F, Harley M, Molloy C, Roddy S, Fitzpatrick C, Cannon M (2012). Psychotic symptoms in adolescence index risk for suicidal behavior: findings from 2 population-based case-control clinical interview studies. Archives of General Psychiatry 69, 1277–1283. [DOI] [PubMed] [Google Scholar]
- Linscott RJ, van Os J (2013). An updated and conservative systematic review and meta-analysis of epidemiological evidence on psychotic experiences in children and adults: on the pathway from proneness to persistence to dimensional expression across mental disorders. Psychological Medicine 43, 1133–1149. [DOI] [PubMed] [Google Scholar]
- Loch AA, Wang YP, Rössler W, Tofoli LF, Silveira CM, Andrade LH (2011). The psychosis continuum in the general population: findings from the Sao Paulo Epidemiologic Catchment Area Study. European Archives of Psychiatry and Clinical Neuroscience 261, 519–527. [DOI] [PubMed] [Google Scholar]
- McGrath J, Saha S, Chant D, Welham J (2008). Schizophrenia: a concise overview of incidence, prevalence, and mortality. Epidemiologic Reviews 30, 67–76. [DOI] [PubMed] [Google Scholar]
- Rössler W, Salize HJ, van Os J, Riecher-Rössler A (2005). Size of burden of schizophrenia and psychotic disorders. European Neuropsychopharmacology 15, 399–409. [DOI] [PubMed] [Google Scholar]
- Rössler W, Riecher-Rössler A, Angst J, Murray R, Gamma A, Eich D, van Os J, Gross VA (2007). Psychotic experiences in the general population: a twenty-year prospective community study. Schizophrenia Research 92, 1–14. [DOI] [PubMed] [Google Scholar]
- Rössler W, Hengartner MP, Ajdacic-Gross V, Haker H, Gamma A, Angst J (2011a). Sub-clinical psychosis symptoms in young adults are risk factors for subsequent common mental disorders. Schizophrenia Research 131, 18–23. [DOI] [PubMed] [Google Scholar]
- Rössler W, Vetter S, Mueller M, Gallo WT, Haker H, Kawohl W, Lupi G, Ajdacic-Gross V (2011b). Risk factors at the low end of the psychosis continuum: much the same as at the upper end? Psychiatry Research 189, 77–81. [DOI] [PubMed] [Google Scholar]
- Rössler W, Hengartner MP, Angst J, Ajdacic-Gross V (2012a). Linking substance use with symptoms of sub-clinical psychosis in a community cohort over 30 years. Addiction 107, 1174–1184. [DOI] [PubMed] [Google Scholar]
- Rössler W, Hengartner MP, Ajdacic-Gross V, Haker H, Angst J (2012b). Sex differences in sub-clinical psychosis – results from a community study over 30 years. Schizophrenia Research 139, 176–182. [DOI] [PubMed] [Google Scholar]
- Schultze-Lutter F, Schimmelmann BG, Ruhrmann S (2011). The near Babylonian speech confusion in early detection of psychosis. Schizophrenia Bulletin 37, 653–655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott J, Chant D, Andrews G, McGrath J (2006). Psychotic-like experiences in the general community: the correlates of CIDI psychosis screen items in an Australian sample. Psychological Medicine 36, 231–238. [DOI] [PubMed] [Google Scholar]
- Tsuang MT, van Os J, Tandon R, Barch DM, Bustillo J, Gaebel W, Gur RE, Heckers S, Malaspina D, Owen MJ, Schultz S, Carpenter W (2013). Attenuated psychosis syndrome in DSM-5. Schizophrenia Research 150, 21–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Os J, Hanssen M, Bijl RV, Ravelli A (2000). Strauss (1969) revisited: a psychosis continuum in the general population? Schizophrenia Research 45, 11–20. [DOI] [PubMed] [Google Scholar]
- Wigman JT, van Nierop M, Vollebergh WA, Lieb R, Beesdo-Baum K, Wittchen HU, van Os J (2012). Evidence that psychotic symptoms are prevalent in disorders of anxiety and depression, impacting on illness onset, risk, and severity–implications for diagnosis and ultra-high risk research. Schizophrenia Bulletin 38, 247–257. [DOI] [PMC free article] [PubMed] [Google Scholar]