Abstract
Background
Invasive infections caused by Capnocytophaga canimorsus are rare. Immunocompromised patients, who report being bitten by or having a close contact with an animal, represent a high-risk group for this infection. There are only few dozens of infections by this bacteria manifesting as purulent meningitis reported worldwide. The reported case is a first reported case of purulent meningitis caused by by Capnocytophaga canimorsus in Czech Republic with only a limited risk factor history.
Case presentation
The patient, a 74 years old man, was referred to the infectious diseases department of a teaching hospital with clear signs of developing purulent meningitis. His anamnestic data did not show any unusual findings. He was treated for compensated diabetes mellitus type II. The blood cultures were negative and the etiological agent did not grow from the cerebrospinal fluid (CSF) on common media. Eventually, it was identified by detecting pan-bacterial DNA and DNA sequencing. Subsequently, the pathogen was confirmed by anaerobic cultivation from CSF. Only after then the patient recalled being bitten by his German shepherd puppy during play. The patient was successfully treated intravenously by ceftriaxone.
Conclusions
Purulent meningitis caused by Capnocytophaga spp. is a rare disease, but it needs to be considered in patients at risk with pre-existing conditions, who report close contact with or being bitten by an animal. It is important to test for this microbe in cases with negative microbiological results for the more common agents.
Keywords: Capnocytophaga, Purulent meningitis, Invasive infection
Background
Capnocytophaga canimorsus (genus Capnocytophaga, family Flavobacteriaceae) is a fermenting Gram-negative rod, which is commonly present in oral microflora in animals and is predominantly found in the saliva of cats and dogs. Human strains, such as C. gingivalis, C. sputigena, C. ochracea and others, are found predominantly in immunocompromised patients in gingival plaque in the periodontal disease. Infections of humans usually occur through a penetrating wound or by a skin abrasion caused by a positive animal, or by a contact of a skin wound with animal saliva [1–3]. There are several invasive forms of the C. canimorsus infection, which have been described in humans. The most common one is sepsis followed by purulent meningitis. Other, less frequently observed forms, include infections of the eye, soft tissues and bones, endocarditis, or infections affecting pregnant women, such as those of fetal membranes or gynecological infections [4]. The majority of the invasive infections have been described in immunocompromised patients or those with other serious illnesses. In healthy people these infections are rare and, usually, follow a milder course. Risk factors for the development of a serious disease include asplenism, alcohol abuse, smoking, corticosteroid therapy and hemato-oncological diseases [5].
The first infection of humans by C. canimorsus was described in 1976 [6].
Incidence rates of positive identification of C. canimorsus in animals depend on the diagnostic technique used and vary widely. Thus, Westwell et al. [7] was able to show 24% of canine samples being positive by cultivation. In the work of Umeda [8], however, when both the PCR and cultivation methods were used, C. canimorsus was identified in samples of dental plaque swabs from 69,7% of dogs and 54,8% of cats tested.
The pathogenesis of the disease was investigated in both the in vivo model and in vitro experiments on human macrophages. C. canimorsus infects the macrophages and replicates in them, but does not interact with Toll-like receptors and therefore does not induce pro-inflammatory cytokines, such as TNF- α, interleukins or IFN-γ [9]. The bacteria is also resistant to the effects of the complement and polymorphonuclear leucocytes [10]. It has been suggested, that the infection elicits only very weak inflammatory response and the bacteria can escape the immune system [11, 12]. The main invasive factors have not been fully described yet, but the lipopolysaccharide and sialidase are on top of the list [13, 14].
Only few dozens of infections by this bacteria manifesting as purulent meningitis in humans have been reported worldwide and the reported case is the first one reported in Czech Republic, which, contrary to the majority of others, had only a limited risk factor history.
Case presentation
The 74 years old male patient first reported to his general practitioner (GP) on August 24. For the last 3 days he had experienced headache and stiff neck without any fever, for which he had been taking paracetamol. On the day of his visit he started to feel nauseated and his temperature rose to 39o C. Anamnestically, the patient had been on an ongoing treatment for type II diabetes mellitus with metformin, for arterial hypertension with telmisartan/hydrochlorothiazid, for dislipidemia with atorvastatin and for liver steatosis with sillymarin. He had undergone cholecystectomia, abdominal hernia surgery and partial gastric resection for ulcer disease. He had used to work as an engineer in a factory, but he was retired at that point and lived with his wife and dog in a family house. He had had no travel history for the preceding 2 years, had never smoked, alcohol had used only occasionally and had engaged in sports.
The GP reported the following - the patient was febrile, nauseated, with normal blood pressure and pulse, pulmonary signs without pathological findings and abdominal exam showed no local resistance or pain. However an upper meningeal syndrome was present and thus the patient was immediately sent to the local infectious disease (ID) department.
There, on the admission, the patient was febrile, blood pressure and pulse were stable and Glasgow Coma Scale was 15. His laboratory showed increased inflammatory markers (leucocytosis, CRP of 176 mmol/l). Both aerobic and anaerobic blood cultivation was started. X-rays of lungs and paranasal sinuses were negative. Cerebrospinal fluid (CSF) examination showed 5524 segmented neutrophils/mm3, 1568 lymphocytes/mm3, glucose 2,98 mmol/l and protein 2,1 g/l. A combination therapy of intravenous dexamethazone (4 mg every 6 h), ceftriaxone (4 g every 24 h) and crystalline solution (500 ml applied over 4 h) was started and the patient was transported to the intensive care unit (ICU) of the ID department of the Faculty Hospital in Hradec Kralove on the same day.
At the admission there the patient was clinically stable and conscious. The neurological examination showed only a mild stiffness of his neck and a slight tremor of fingers. The CT scan of the brain and paranasal sinuses showed no pathology and the Ear-Nose and Throat specialist found no infectious foci in this area. Both aerobic and anaerobic CSF cultivation in blood culture bottles (Bactec 9240, Becton Dickinson) were started. Microscopic and agglutination analysis of the CSF were negative. The therapy with corticosteroids was continued for another 2 days. Intravenous ampicillin was added to the therapy (3 g every 6 h), but only four doses were administered, because Listeria spp. was soon ruled out as the causative agent in the next step (below). Due to the hyperglycemia, insulin was administered intravenously.
As there was no growth detected by the CSF cultivation on the second day, the cultivation analysis was continued further to the total length of 7 days and molecular diagnostic methods were implemented.
During the first step, PCR tests performed on CSF ruled out Streptococcus pneumoniae, Neisseria meningitidis, Listeria monocytogenes, Staphylococcus aureus and Haemophilus influenzae. The second day the CSF values showed a slight improvement and transoesophageal ultrasound of the heart showed no signs of endocarditis.
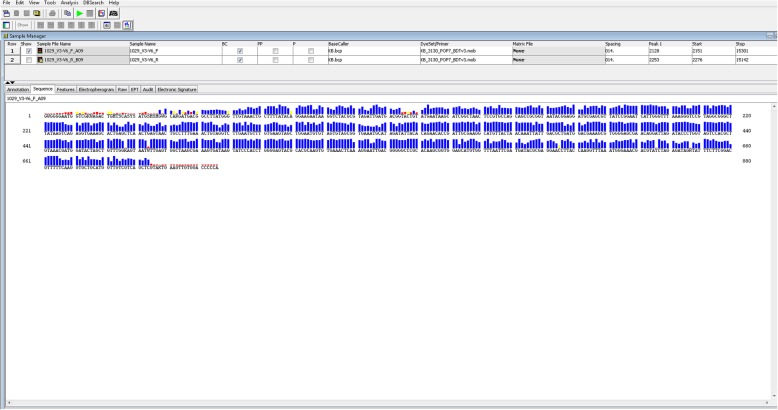
Due to the still unclear microbial diagnosis vancomycin (1 g in 250 ml intravenously every 12 h) was added to the antibiotic regimen. Since there was a strong PCR positivity for the pan-bacterial DNA from the CSF, targeted PCR for Escherichia coli and Mycobacterium tuberculosis was performed, but with negative results. However, a subsequent bacterial DNA sequencing on August 28 identified DNA of the Capnocytophaga spp. with a specificity of 99% (Fig. 1). No further specification could be achieved.
Fig. 1.
Capnocytophaga canimorsus sequence obtained by DNA sequencing from CSF
Simultaneously the anaerobic CSF cultivation using the Schaedler agar (anaerobic chamber with atmosphere containing 85% nitrogen, 5% hydrogen and 10% carbon dioxide, temperature 37 °C, incubated for 7 days total) started to show small semi-transparent colonies. Microscopically they were formed by fusiformic Gram-negative small rods. MALDI-TOF (Bruker Daltonik) identified Capnocytophaga canimorsus with a score of 1,98. Blood and other biological samples were negative.
The antibiotic therapy was adjusted to intravenous ceftriaxone (4 g) only. This led to a subsequent improvement of the overall status and to a decrease of inflammatory markers. The antidiabetic therapy was converted to oral administration of metformin (500 mg daily in one dose) and, on September 8, the control exam of the CSF was negative. An examination by a stomatologist ruled out any infectious foci in the respective area.
During the subsequent days the patient recalled being bitten by his 4 months old German shepherd dog on the internal side of his right shank approximately 2 weeks before the symptoms started. The wound was not bleeding and was painless. After careful examination the attending physician discovered an almost healed wound about 5 cm long, which was not discovered during any of the physical exams before (Fig. 2). On day 14 after admission the antibiotic treatment was stopped and the patient was released from the hospital on day 15 fully recovered (Timeline in Fig. 3).
Fig. 2.

An almost healed small bruise above patient’s ankle inflicted by his puppy of the German shepherd
Fig. 3.
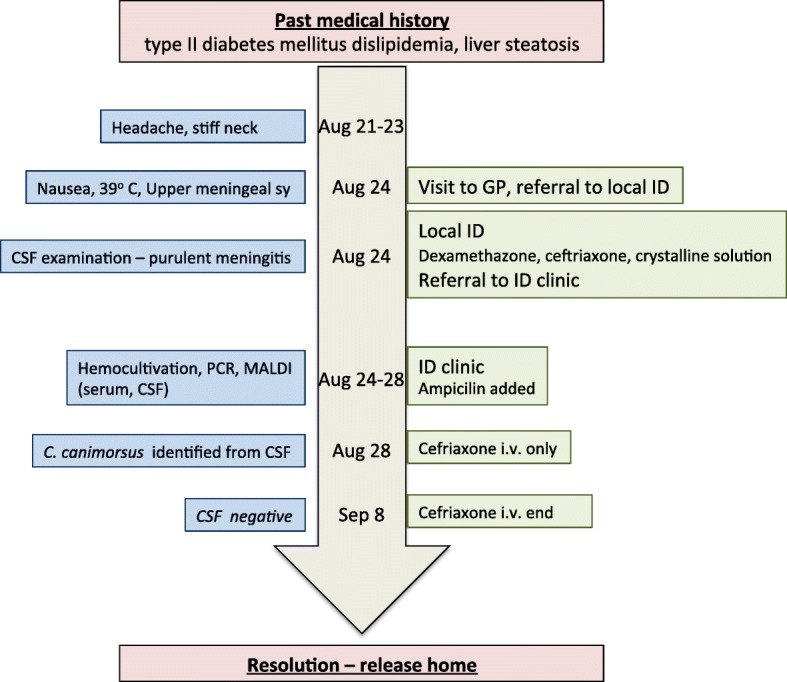
Case timeline
Discussion and conclusions
This is the second reported case of an invasive infection caused by C. canimorsus in the Czech Republic (CZ). However, the first one manifested as a severe sepsis in a woman with splenectomy [15]. Thus the patient described in this report is the first case with purulent meningitis reported in CZ. It is possible though, that the numbers of undescribed cases are likely higher in both CZ and worldwide. Butler et al. described a cohort of 484 cases of laboratory confirmed cases of Capnocytophaga spp. infections worldwide in 2015 [16]. About two thirds of these patients were men, with the age median of 55 years and mortality in this group was 26%. Clinical symptoms included severe sepsis with septic shock, gangrene, meningitis, endocarditis and eye infections. Majority of all patients reported some contact with animals as a likely source – 60% of them were bitten by a dog and another 27% recalled bruises, scratches, licking or other types of close contacts caused by cats or dogs. Meningitis (33 cases) was described mostly in older patients, often men, with longer incubation periods than in septic cases, and showed mortality rates lower than 5% [16–18]. The data from this cohort thus confirm meningitis as a relatively rare manifestation of this infection (6,8%). However, this prevalence is comparable to the rates observed for purulent meningitis in infections caused by other pathogens – e.g. Streptococcus pyogenes - 5,4 to 7,7%, Streptococcus pneumoniae and Haemophilus influenzae both around 4% [19–23]. On the other hand, the prevalence of purulent meningitis in infections caused by Neisseria meningitidis is substantially higher, between 40 and 65%, depending on individual serotypes and regional differences [24–28]. Reasons for lower mortality rates in patients with purulent meningitis (in comparison with sepsis) caused by Capnocytophaga spp. are likely similar to those in meningitis caused by meningococci (in comparison with meningococcal sepsis) – the patients are not likely to develop lethal complications of sepsis, such as disseminated intravascular coagulation, thrombocytopenia, Waterhouse-Fridrichsen syndrome and others.
Because the number of cases of invasive infections caused by Capnocytophaga spp. is low to begin with, the cases of purulent meningitis are very rare and thus the identification of the causative agent is difficult and complicated, since the CSF is often the only lab accessible compartment positive for this bacteria. In addition, the “classical” laboratory methods are often not reliable – conventional biochemical testing in many cases does not provide diagnostically relevant answers, the bacteria grow slowly and require specific conditions - increased CO2, the chocolate agar or selective media with antibiotics [3, 14, 17, 29] . These are all the reasons that lead to false negatives caused mostly by the cultivation of the CSF on just the basic media. Therefore, the molecular methods involving PCR represent the main tool for the successful diagnosis. Even these are not trivial and available in all hospitals, as they require the ability to amplify pan-bacterial DNA and subsequently to identify the culprit by sequencing.
It is not surprising that infections by Capnocytophaga spp occur mostly in immunocompromised patients, as the impaired immune response coincides with the ability of this microbe to evade the immune response [9–12]. However, it is “only” 29,5% of the patients with invasive forms of disease, who are immunocompromised in a more severe manner (14,2% with splenectomy or hyposplenism, 12% alcohol abuse, 1,3% hematooncologic diseases, then also HIV infection, diabetes mellitus and corticosteroid therapy) [16]. The patient described in this report was not in any clear immunosuppression. The only other comorbidity was diabetes mellitus type II treated with oral antidiabetic drugs. However, even this disease thus represents a risk factor for the infection by Capnocytophaga spp.
Antibiotics of the β-lactam structure represent a mainstream of therapy of these infections. Due to the potential of these bacteria to produce beta-lactamases, however, cephalosporins of higher generations, such as ceftriaxone or cefepime are usually administered parenterally. Amoxicilin, amoxicilin/clavulanate, piperacilin/tazobactam or chloramphenicol also show good therapeutic responses. Carbapenems are indicated for mixed soft-tissue infections or multi-resistant microbial strains. Clindamycine, doxycycline, amoxicilin/clavulanate or fluorochinolones administered orally show good results in less severe infections. On the other hand aminoglycosides, anti-staphylococcal penicillins, colistine and trimethoprim-sulfametoxazole have no therapeutic effects. The sensitivity of Capnocytophaga spp. to macrolidic antibiotics, aztreonam, phosphomycine, rifampicine and first-generation cephalosporins is questionable. In the cases of open and bleeding wounds caused by animal bites it is recommended to treat the patient with antibiotics orally and verify their tetanus vaccination history [3, 14, 16, 17, 29, 30]. The patient described in this report was successfully treated by intravenous cefriaxone.
Purulent meningitis caused by Capnocytophaga spp. is a rare disease, but it needs to be considered in patients at risk with pre-existing conditions, who report close contact with or being bitten by an animal. It is important to test for this microbe in cases with negative microbiological results for the more common agents. There are hundreds of cases of invasive infections (sepsis) caused by Capnocytophaga spp. reported worldwide, but only dozens of cases of purulent meningitis. It is thus likely that the real numbers of cases of these meningitides are much higher and not diagnosed properly.
Acknowledgements
N/A
Abbreviations
- CSF
Cerebrospinal fluid
- CT
Computer tomography
- CZ
Czech Republic
- DNA
Deoxyribonucleic acid
- GP
General practitioner
- ICU
Intensive-care unit
- ID
Infectious diseases department
- IFN-γ
Interferon γ
- MALDI-TOF
Matrix assisted laser desorption/ionization- time-of-flight
- PCR
Polymerase chain reaction
- TNF-α
Tumor necrosis factor α
Authors’ contributions
PP and SP are clinicians who diagnosed the disease and administered the treatment, LR is microbiologist, who provided the laboratory diagnosis; PP prepared the initial version of the manuscript, PB is responsible data analysis, final manuscript preparation and correspondence. All authors have read and approved the manuscript.
Funding
P.B. was supported by the Long term developmental plan of the Ministry of Defence of Czech Republic. This funding is responsible for the DNA analysis and manuscript preparation.
Availability of data and materials
N/A
Ethics approval and consent to participate
The Case report is retrospective and anonymous. The patient was treated according to the best clinical practice and no additional or experimental exams or treatments were performed. Thus the ethics approval and consent was not required.
Consent for publication
Consent for publication was obtained in a written form and made available to the Journal.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Petr Prasil, Email: pprasil@seznam.cz.
Lenka Ryskova, Email: ryskoval@lfhk.cuni.cz.
Stanislav Plisek, Email: pliseks@lfhk.cuni.cz.
Pavel Bostik, Email: bostikp@lfhk.cuni.cz.
References
- 1.Brenner DJ, Hollis DG, Fanning GR, Weaver RE. Capnocytophaga canimorsus sp. nov. (formerly CDC group DF-2), a cause of septicemia following dog bite, and C. cynodegmi sp. nov., a cause of localized wound infection following dog bite. J Clin Microbiol. 1989;27(2):231–235. doi: 10.1128/JCM.27.2.231-235.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dobosz P, Martyna D, Stefaniuk E, Szczypa K, Hryniewicz W. Severe sepsis after dog bite caused by Capnocytophaga canimorsus. Polski Merkuriusz Lekarski. 2015;39(232):219–222. [PubMed] [Google Scholar]
- 3.Janda JM. 235 - Capnocytophaga. In: Bennett JE, Dolin R, Blaser MJ, editors. Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases. 8. Philadelphia: Content Repository Only!; 2015. pp. 2645–2648.e2641. [Google Scholar]
- 4.Lion C, Escande F, Burdin JC. Capnocytophaga canimorsus infections in human: review of the literature and cases report. Eur J Epidemiol. 1996;12(5):521–533. doi: 10.1007/BF00144007. [DOI] [PubMed] [Google Scholar]
- 5.Pers C, Gahrn-Hansen B, Frederiksen W. Capnocytophaga canimorsus septicemia in Denmark, 1982-1995: review of 39 cases. Clin Infect Dis. 1996;23(1):71–75. doi: 10.1093/clinids/23.1.71. [DOI] [PubMed] [Google Scholar]
- 6.Bobo RA, Newton EJ. A previously undescribed gram-negative bacillus causing septicemia and meningitis. Am J Clin Pathol. 1976;65(4):564–569. doi: 10.1093/ajcp/65.4.564. [DOI] [PubMed] [Google Scholar]
- 7.Westwell AJ, Kerr K, Spencer MB, Hutchinson DN. DF-2 infection. Bmj. 1989;298(6666):116–117. doi: 10.1136/bmj.298.6666.116-c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Umeda K, Hatakeyama R, Abe T, Takakura K, Wada T, Ogasawara J, Sanada S, Hase A. Distribution of Capnocytophaga canimorsus in dogs and cats with genetic characterization of isolates. Vet Microbiol. 2014;171(1–2):153–159. doi: 10.1016/j.vetmic.2014.03.023. [DOI] [PubMed] [Google Scholar]
- 9.Shin H, Mally M, Kuhn M, Paroz C, Cornelis GR. Escape from immune surveillance by Capnocytophaga canimorsus. J Infect Dis. 2007;195(3):375–386. doi: 10.1086/510243. [DOI] [PubMed] [Google Scholar]
- 10.Meyer S, Shin H, Cornelis GR. Capnocytophaga canimorsus resists phagocytosis by macrophages and blocks the ability of macrophages to kill other bacteria. Immunobiology. 2008;213(9–10):805–814. doi: 10.1016/j.imbio.2008.07.019. [DOI] [PubMed] [Google Scholar]
- 11.Gaastra W, Lipman LJ. Capnocytophaga canimorsus. Vet Microbiol. 2010;140(3–4):339–346. doi: 10.1016/j.vetmic.2009.01.040. [DOI] [PubMed] [Google Scholar]
- 12.Shin H, Mally M, Meyer S, Fiechter C, Paroz C, Zaehringer U, Cornelis GR. Resistance of Capnocytophaga canimorsus to killing by human complement and polymorphonuclear leukocytes. Infect Immun. 2009;77(6):2262–2271. doi: 10.1128/IAI.01324-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ittig S, Lindner B, Stenta M, Manfredi P, Zdorovenko E, Knirel YA, dal Peraro M, Cornelis GR, Zahringer U. The lipopolysaccharide from Capnocytophaga canimorsus reveals an unexpected role of the core-oligosaccharide in MD-2 binding. PLoS Pathog. 2012;8(5):e1002667. doi: 10.1371/journal.ppat.1002667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mally M, Paroz C, Shin H, Meyer S, Soussoula LV, Schmiediger U, Saillen-Paroz C, Cornelis GR. Prevalence of Capnocytophaga canimorsus in dogs and occurrence of potential virulence factors. Microbes Infect. 2009;11(4):509–514. doi: 10.1016/j.micinf.2009.02.005. [DOI] [PubMed] [Google Scholar]
- 15.Hloch O, Mokra D, Masopust J, Hasa J, Charvat J. Antibiotic treatment following a dog bite in an immunocompromized patient in order to prevent Capnocytophaga canimorsus infection: a case report. BMC Res Notes. 2014;7:432. doi: 10.1186/1756-0500-7-432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Butler T. Capnocytophaga canimorsus: an emerging cause of sepsis, meningitis, and post-splenectomy infection after dog bites. Eur J Clin Microbiol Infect Dis. 2015;34(7):1271–1280. doi: 10.1007/s10096-015-2360-7. [DOI] [PubMed] [Google Scholar]
- 17.Le Moal G, Landron C, Grollier G, Robert R, Burucoa C. Meningitis due to Capnocytophaga canimorsus after receipt of a dog bite: case report and review of the literature. Clin Infect Dis. 2003;36(3):e42–e46. doi: 10.1086/345477. [DOI] [PubMed] [Google Scholar]
- 18.van Samkar A, Brouwer MC, Schultsz C, van der Ende A, van de Beek D. Capnocytophaga canimorsus meningitis: three cases and a review of the literature. Zoonoses Public Health. 2016;63(6):442–448. doi: 10.1111/zph.12248. [DOI] [PubMed] [Google Scholar]
- 19.Arias-Constanti V, de la Maza Trenchs-Sainz V, Sanz-Marcos NE, Guitart-Pardellans C, Gene-Giralt A, Luaces-Cubells C. Invasive disease by streptococcus pyogenes: patients hospitalized for 6 years. Enferm Infecc Microbiol Clin. 2018;36(6):352–356. doi: 10.1016/j.eimc.2017.06.005. [DOI] [PubMed] [Google Scholar]
- 20.Imohl M, Fitzner C, Perniciaro S, van der Linden M. Epidemiology and distribution of 10 superantigens among invasive streptococcus pyogenes disease in Germany from 2009 to 2014. PLoS One. 2017;12(7):e0180757. doi: 10.1371/journal.pone.0180757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Oligbu G, Collins S, Sheppard CL, Fry NK, Slack M, Borrow R, Ladhani SN. Childhood deaths attributable to invasive pneumococcal disease in England and Wales, 2006-2014. Clin Infect Dis. 2017;65(2):308–314. doi: 10.1093/cid/cix310. [DOI] [PubMed] [Google Scholar]
- 22.Polkowska A, Toropainen M, Ollgren J, Lyytikainen O, Nuorti JP. Bacterial meningitis in Finland, 1995-2014: a population-based observational study. BMJ Open. 2017;7(5):e015080. doi: 10.1136/bmjopen-2016-015080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Que Y-A, Moreillon P. 196 - Staphylococcus aureus (Including Staphylococcal Toxic Shock Syndrome) In: Bennett JE, Dolin R, Blaser MJ, editors. Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases. 8. Philadelphia: Content Repository Only!; 2015. p. 2237. [Google Scholar]
- 24.Arakaki L, Ngai S, Weiss D. Completeness of Neisseria meningitidis reporting in New York City, 1989-2010. Epidemiol Infect. 2016;144(11):2374–2381. doi: 10.1017/S0950268816000406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fukusumi M, Kamiya H, Takahashi H, Kanai M, Hachisu Y, Saitoh T, Ohnishi M, Oishi K, Sunagawa T. National surveillance for meningococcal disease in Japan, 1999-2014. Vaccine. 2016;34(34):4068–4071. doi: 10.1016/j.vaccine.2016.06.018. [DOI] [PubMed] [Google Scholar]
- 26.Rivero-Calle I, Vilanova-Trillo L, Pardo-Seco J, Salvado LB, Quinteiro LI, Martinon-Torres F, Network MR. The burden of pediatric invasive meningococcal disease in Spain (2008-2013) Pediatr Infect Dis J. 2016;35(4):407–413. doi: 10.1097/INF.0000000000001048. [DOI] [PubMed] [Google Scholar]
- 27.Sall O, Stenmark B, Glimaker M, Jacobsson S, Molling P, Olcen P, Fredlund H. Clinical presentation of invasive disease caused by Neisseria meningitidis serogroup Y in Sweden, 1995 to 2012. Epidemiol Infect. 2017;145(10):2137–2143. doi: 10.1017/S0950268817000929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Stephens DS, Apicella MA. In: 213 - Neisseria meningitidis. In: Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases. 8. Bennett JE, Dolin R, Blaser MJ, editors. Philadelphia: Content Repository Only!; 2015. pp. 2425–2445.e2426. [Google Scholar]
- 29.Zajkowska J, Krol M, Falkowski D, Syed N, Kamienska A. Capnocytophaga canimorsus - an underestimated danger after dog or cat bite - review of literature. Przegl Epidemiol. 2016;70(2):289–295. [PubMed] [Google Scholar]
- 30.Ehrmann E, Handal T, Tamanai-Shacoori Z, Bonnaure-Mallet M, Fosse T. High prevalence of beta-lactam and macrolide resistance genes in human oral Capnocytophaga species. J Antimicrob Chemother. 2014;69(2):381–384. doi: 10.1093/jac/dkt350. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
N/A