Abstract
Aims.
Few studies have examined the experiences of carers of people with psychosis using a representative sample. Aiming to obtain generalisable results concerning carers in the context of increased emphasis on involving carers in Australian mental health service delivery and policy frameworks, this study recruited carers within the second Australian national survey of psychotic disorders (Survey of High Impact Psychosis, SHIP). Given that most SHIP participants had long-term illness and extended relationships with carers, the health and wellbeing of carers as a group were expected to be relatively stable. However, since it is unknown whether carers’ health and wellbeing would change, our main aim was to explore change and stability in carers’ health and wellbeing and the relationship between any changes experienced by individual carers and corresponding SHIP participants’ functioning over time.
Methods.
Ninety-eight caregivers of SHIP participants were recruited at baseline and completed validated instruments assessing their health and wellbeing. Seventy-eight carers were re-interviewed at 1-year follow-up. Clinical factors were extracted from the SHIP database. Wilcoxon matched-pairs signed-rank test and t-test were used to analyse changes in variables over time. Cross-lagged analyses were conducted to identify possible causative relationships in changes in SHIP participant and carer variables.
Results.
A substantial percentage of carers experienced social isolation (28.6%), psychological distress (37.7%) and poorer quality of life than population norms. There were no statistically significant changes between baseline and follow-up scores for almost all carers’ health and wellbeing variables, other than a poorer perception of their quality of life in relation to their physical health after 1 year. Cross-lagged analyses suggested that poorer functioning of people with psychosis influenced carers’ social isolation, grief and psychological distress.
Conclusions.
Findings show that carers’ perception of their health and wellbeing did not improve within current mental health service delivery frameworks over time. Carer's persistently poor health and wellbeing suggests a pressing need to enhance services that improve carers’ health and wellbeing especially their physical health and the functioning of people with psychosis whom they support.
Key words: Caregivers, longitudinal study, physical health, psychotic disorders
Introduction
Caregivers of people with psychosis experience psychological distress, social isolation, poor quality of life, grief and carer burden (Awad & Voruganti, 2008; Jansen et al. 2015). However, most previous caregiving studies focus on carers alone, resulting in a gap in knowledge regarding the relationship between patient-related factors and carers’ characteristics. The other gap is a lack of longitudinal studies, as highlighted consistently in several reviews (Caqueo-Urízar et al. 2014; Jansen et al. 2015).
In most previous research, carers have been recruited through their participation in formal mental health programs or by advertising. This has yielded samples with unclear representation of the full range of carers limiting the generalisability of findings (Ohaeri, 2003). Due to the small number of longitudinal population-based caregiving studies (Szmukler et al. 1998; Train et al. 2001; van Wijngaarden et al. 2003; Shibre et al. 2012), improvement or deterioration of carers’ health and wellbeing over time is unclear (Shibre et al. 2012). There is a need for a representative longitudinal study of carers and their relatives with psychosis to provide greater understanding of their circumstances in order to improve service planning (Pirkis et al. 2010).
To the authors’ knowledge, this study is the first longitudinal study with both patient and carer data, conducted within an epidemiological framework in Australia, specifically, the second national survey of psychotic disorders (Survey of High Impact Psychosis, SHIP). The current study sought to document quality of life, social connectedness, grief and psychological health of carers of SHIP participants and to explore changes in carers’ status over time and the dynamic relationships between these and patient characteristics. Given that the majority of SHIP participants had been ill for an extended period and their carers had been providing care for some time, the health and wellbeing of carers overall was likely to be relatively stable, although individual carers might experience change due to the stress of caregiving over time. Further, there has been growing involvement of involving carers in mental health services (Department of Human Services, 2006) but no longitudinal population-based studies to evaluate the impact of this increased emphasis in policy and service delivery on carers’ health and wellbeing. Therefore, it is unknown whether the shift in policy and service delivery has directly benefited the health and wellbeing of individual caregivers of people with psychosis. Our first aim was to investigate whether SHIP participants’ functioning and their carers’ health and wellbeing changed over time. Our second aim was to explore associations between changes in the functioning of individual SHIP participants with psychosis and changes in the health and wellbeing of their carers over time.
Method
Procedures
This study used participants in SHIP as the basis to recruit carers. In SHIP, a random selection of those who screened positive for psychosis was invited to participate in an in-depth interview. Those who had poor English ability, limited capacity to give informed consent and cognitive impairment were excluded from the study. Further details of the SHIP recruitment method can be found in an earlier publication (Morgan et al. 2012).
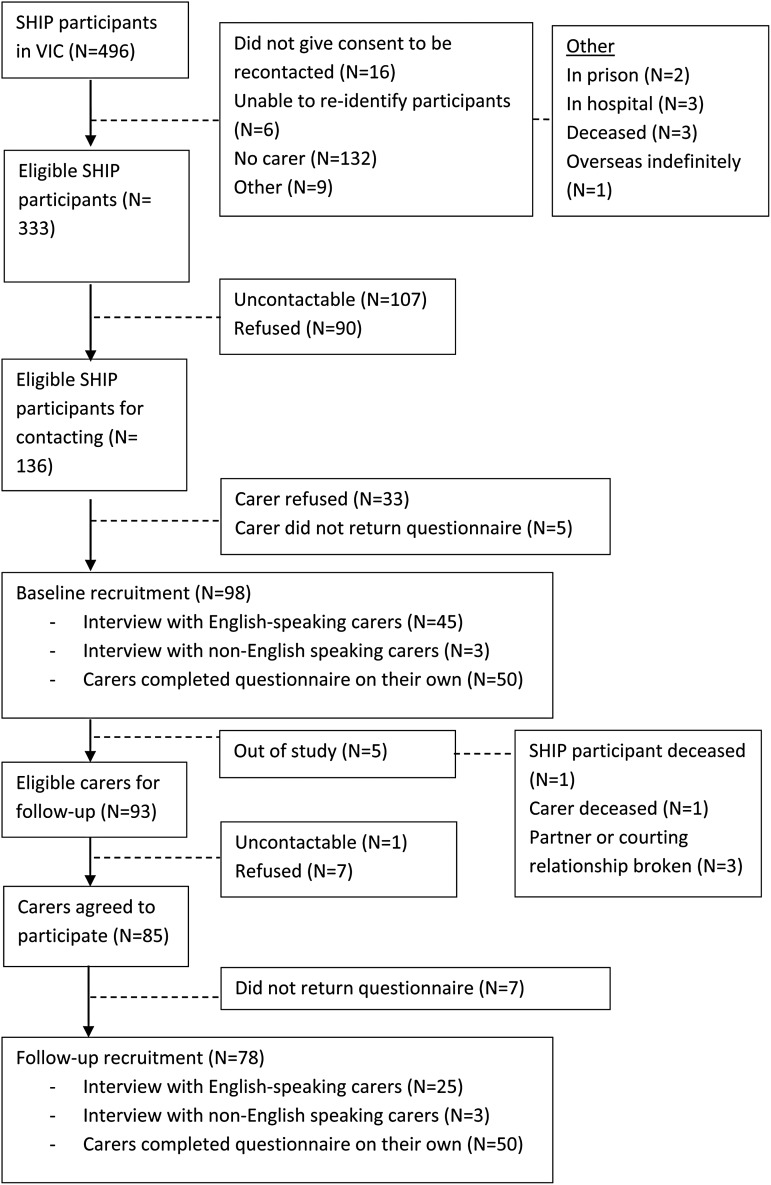
For this carer study, the first author contacted SHIP participants in two Victorian sites who nominated their carers, and sought their written consent to contact their carers. The eligible carer in this study was defined as someone (excluding paid professionals) who was responsible for looking after, helping or taking care of the SHIP participant and their needs who may or may not live with them. No carers had cognitive impairment and therefore none were excluded on these grounds. Interpreters were used as needed so that poor English ability was not an exclusion criterion for carers. Carers were contacted and provided their written consent for study participation. A face-to-face interview using validated, structured questionnaires was then sought. Questionnaires were mailed to carers unable to attend an interview and any missing responses were clarified by telephone. Approximately 1 year after the initial interview, carers who agreed to participate in the follow-up were re-interviewed. A target sample size of 100 was calculated prior to recruitment based on: (1) alpha of 0.05, (2) power of 80%, (3) effect size (f2) to be detected was set at 0.15 based on multiple correlation coefficient (R2) of 0.13 (Green, 1991). Ninety-eight carers were recruited at baseline; 78 were re-interviewed at follow-up (Fig. 1). The study was approved by Melbourne Health (Reference: 2010.011), St Vincent's Hospital (Melbourne) (Reference: 111/11) and the University of Melbourne (Reference: 1034494.1) Human Research Ethics Committees.
Fig. 1.
Recruitment chart.
Survey instruments
Socio-demographic data regarding carers were collected and validated instruments were used to assess their health and wellbeing:
-
(1)
The 10-item Kessler-10 (K10) was used to measure psychological distress of the carers. Higher scores indicate greater psychological distress (Kessler et al. 2002).
-
(2)
The Friendship Scale (FSS) was used to measure social connectedness of the carers. The 6-item FSS is validated with higher scores indicating greater social connectedness (Hawthorne, 2006).
-
(3)
The World Health Organisation Quality of Life - BREF (WHOQOL-BREF) was used to measure perceived quality of life of the carers. The 26-item WHOQOL-BREF covers four domains: Physical Health, Psychological Health, Social Relationships and Environment. Higher scores indicate better perceived quality of life (WHOQOL Group, 1998).
-
(4)
The 16-item Mental Illness Version of the Texas Inventory of Grief (MIVTIG) was used to measure feelings of grief in the carers. Higher scores indicate more prominent grief (Miller et al. 1990).
-
(5)
The Life Skills Profile-20 (LSP-20) was used to measure carers’ perception of the functioning of their relative with psychosis. The 20-item LSP-20 covers five areas of functioning: Self-care, Anti-social, Withdrawal, Bizarre and Compliance and higher scores indicate better functioning (Rosen et al. 2001).
Relevant demographic and clinical variables concerning the index SHIP participant were extracted from the SHIP database. These included: International Classification of Diseases and Related Health Problems 10th Revision (ICD-10) diagnosis, derived algorithmically using the Diagnostic Interview for Psychosis (Castle et al. 2006); current cognitive ability using the Digit Symbol Coding Test (Randolph et al. 1998); and behavioural and social aspects of functioning as well as role performance over 1 year as measured by the Personal and Social Performance Scale (PSP) (Morosini et al. 2000).
Analysis
Data were analysed using SPSS version-21 (IBM Corp, 2012). Descriptive analysis was carried out. Wilcoxon matched-pairs signed-rank test and t-tests were conducted to assess changes in carers’ health and wellbeing over time. Non-parametric tests were used for non-normal distributions. Significance level was 0.05 (two-tailed) for all statistical tests.
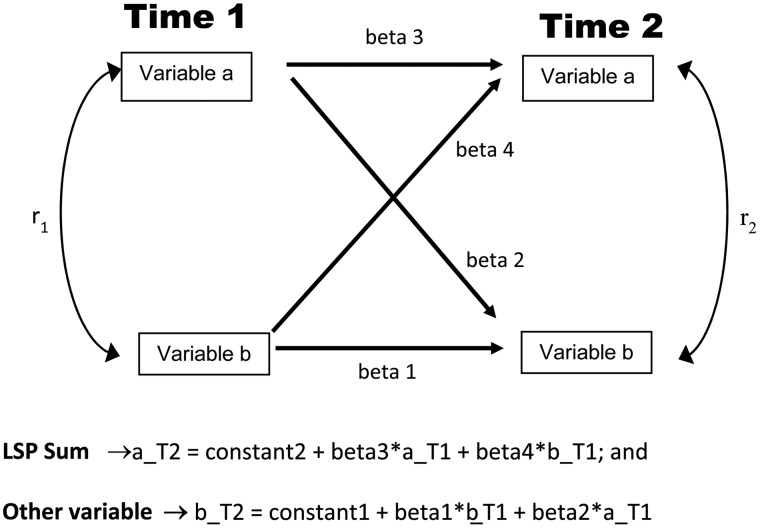
Cross-lagged analysis was conducted to explore potential causal relationships and estimate the effects of LSP total scores on the caregiving variables over time (Finkel, 1995). Using K10 score as an example, regression was first conducted to model the effect of LSP total score on K10 score after controlling for the effect of K10 score at Time 1 (T1). The second regression was conducted predicting the effect of K10 score on LSP total score after controlling for the effect of LSP total score at T1 (Fig. 2).
Fig. 2.
Model of longitudinal effects using cross-lagged analysis (Life Skills Profile (LSP) total score was used as ‘variable a’ and each of the caregiving outcome variables was used as ‘variable b’ in each analysis).
Results
Socio-demographic characteristics of carers
Most (75.5%) carers were female. Their mean age was 57.1 years (s.d. = 12.1). Most (62.2%) carers were parents of the respective SHIP participant and their mean age was 61.1 years (s.d. = 8.6). The mean age of spouses or partners who were carers (n = 15) was 49.0 years (s.d. = 14.7). Seven carers were friends or housemates and eleven were siblings of the SHIP participants. Most carers (n = 70, 71.4%) were born in Australia. For the rest (n = 28), the mean years of living in Australia was 34.5 years (s.d. = 16.7). Most (n = 86, 87.8%) carers spoke only English at home. More than half (59.2%) were married or in a de facto relationship. The highest level of education attained by the carers was: primary education (8.2%), secondary education (32.7%) and tertiary education (59.1%). One-third (36.7%) were receiving government financial support. Three-fifths (63.3%) were employed.
Socio-demographic and clinical characteristics of SHIP participants with carers
The median age of the SHIP participants was 33.0 years (range = 18–62) and 64 (65.3%) were male. Most were born in Australia (n = 78, 79.6%) and were single (72.4%). Most (73.4%) had at least secondary education and a third (30.6%) had a trade certificate. Just under half had been unemployed (46.9%) within the last 12 months.
The ICD-10 diagnoses of the SHIP participants were schizophrenia (38.8%), schizoaffective disorder (17.3%), bipolar disorder (21.4%), depressive disorders (16.3%), delusional disorders and other non-organic psychoses (5.1%) and major depression without psychosis (1.0%) assessed during SHIP interview; all were screen positive for psychosis during the SHIP census. Almost all SHIP participants had a long period of illness and the duration was distributed widely (25th percentile = 5.0, 50th percentile = 10.0, 75th percentile = 19.0 years). Reported patterns of illness were of multiple episodes of psychosis with partial recovery between episodes (n = 41, 41.8%), continuous chronic illness (n = 25, 25.6%), multiple episodes with good recovery between episodes (n = 20, 20.4%) and a single episode with good recovery (n = 12, 12.2%). The PSP was used to measure personal and social functioning of the SHIP participants. The mean score was 58.3 (s.d. = 13.7) indicating marked difficulties in one or more areas of functioning.
The characteristics of the SHIP participants in the caregiver study (n = 98) were compared with those of the eligible SHIP participants not recruited to this study (n = 235) from Victoria (Fig. 1). Most characteristics of those recruited and not recruited were comparable. One-way ANOVA showed that the differences in course of mental disorder and diagnosis of mental disorder were not statistically significant. The SHIP participants in the carer study were more likely to be living in family homes (recruited sample (RS) = 37.8%, eligible sample (ES) = 22.6%, χ2 = 8.104, df = 1, p = 0.007); to have completed Year 12 education (RS = 54.2%, ES = 35.2%, χ2 = 10.069, df = 1, p = 0.002); had better behavioural and social functioning and role performance according to the PSP (RS mean = 58.33 (s.d. = 13.68), ES mean = 54.64 (s.d. = 13.92), difference in mean (DM) = 3.688 (95% CI: 0.41, 6.96), t331 = 2.215, p = 0.027) and were more likely to be employed (RS = 43.9%, ES = 32.8%, χ2 = 4.349, df = 1, p = 0.037) than the rest of the eligible SHIP participants. However, in terms of their age, gender and current cognitive ability, both groups were alike.
Relationships between people with psychosis and their carers
Just over half (55.1%) of the carers were living with the SHIP participants. Carers who were not living with the participant had frequent contact with them. Most carers had at least weekly face-to-face (68.2%) and/or phone (77.3%) contact with them. The median period that the caregivers had been caring for the person with mental illness was 7.0 years (range = 0.1–41.0). Almost all of the spouses/partners (93.3%) were living with the SHIP participants but only around half (47.5%) of the parents were living with the SHIP participants.
Functioning level of people with psychosis over time
As SHIP was a cross-sectional study, no contemporaneous SHIP data were available at follow-up within this carer study. Therefore, the functioning level of SHIP participants at baseline and follow-up was assessed by the carers, using the LSP-20 (Rosen et al. 2001). The difference in means of the subscales and total scores of the LSP-20 at baseline and follow-up (Table 1) were not statistically significant. Comparison of percentages between baseline and follow-up scores and statistical tests indicate that the independent functioning levels of the SHIP participants were similar after 1 year.
Table 1.
Independent functioning levels of SHIP participants with psychotic illness using LSP-20
| SHIP participants baseline (N = 98) | SHIP participants follow-up (N = 78) | Patients with schizophrenia (Rosen et al. 2001) | |||
|---|---|---|---|---|---|
| Mean | s.d. | Mean | s.d. | Mean | |
| Anti-social (4–16) | 13.68 | 2.53 | 13.60 | 2.80 | 13.04 |
| Compliance (3–12) | 10.65 | 1.86 | 10.97 | 2.25 | 9.54 |
| Self-care (5–20) | 15.63 | 3.15 | 15.15 | 3.57 | 15.54 |
| Bizarre (3–12) | 10.73 | 1.62 | 10.56 | 1.83 | 9.80 |
| Withdrawal (5–20) | 14.50 | 3.61 | 14.62 | 3.84 | 12.37 |
| Total (20–80) | 64.94 | 9.89 | 64.91 | 11.39 | 60.30 |
LSP, life skills profile; SHIP, survey of high impact psychosis.
Health and wellbeing of carers over time
More than a quarter (28.6%) of the carers reported feeling isolated or very isolated. At follow-up, carers continued to experience social isolation; 29.5% reported being isolated or very isolated (Table 2). The Pearson correlation between baseline and follow-up FSS scores was 0.67 (p < 0.001). The average score difference between baseline and follow-up of 0.22 (95% CI: −0.68, 1.11) was not statistically significant (p = 0.630).
Table 2.
Social connectedness and psychological distress of the carers
| Social connectedness (FSS) | Caregivers baseline (N = 98) | Caregivers follow-up (N = 78) | Australian population norm (Hawthorne, 2008) | ||
|---|---|---|---|---|---|
| N | % | N | % | % | |
| Very isolated | 9 | 9.2 | 6 | 7.7 | 2 |
| Isolated | 19 | 19.4 | 17 | 21.8 | 5 |
| Some isolation | 15 | 15.3 | 10 | 12.8 | 9 |
| Connected | 24 | 24.5 | 16 | 20.5 | 25 |
| Very connected | 31 | 31.6 | 29 | 37.2 | 59 |
| Psychological distress level (K10) | Australian population norm (Australian Bureau of Statistics, 2012) | ||||
| Low (10–19) | 61 | 62.2 | 52 | 66.7 | 70.1 |
| Moderate (20–24) | 17 | 17.3 | 8 | 10.3 | 18.4 |
| High (25–29) | 16 | 16.3 | 8 | 10.3 | 7.4 |
| Very high (30–50) | 4 | 4.1 | 10 | 12.8 | 3.4 |
FSS, friendship scale.
As for psychological distress, a considerable percentage (20.4%) of the carers had a high or very high level of psychological distress (Table 2). The Wilcoxon matched-pairs signed-rank test was used as the data were skewed. The output indicated there was no statistically significant difference between baseline and follow-up median scores (baseline-median = 16.0, follow-up-median = 16.0, Z = −0.300, p = 0.767).
The carers experienced moderate grief as measured on the MIVTIG (Miller et al. 1990). The mean MIVTIG baseline score was 40.8 (s.d. = 17.3) and follow-up score was 39.8 (s.d. = 16.6). The correlation between baseline and follow-up MIVTIG scores was 0.23 (p = 0.055). The average difference between baseline and follow-up mean scores of 4.10 (95% CI: −1.04, 9.24) was not statistically significant (p = 0.116, n = 67).
There was no statistically significant difference between baseline and follow-up mean scores for carers’ perceived quality of life. However, the average difference between baseline and follow-up physical health mean scores of 4.49 (95% CI: 1.37, 7.60) was statistically significant (p = 0.005) indicating deterioration in the physical health satisfaction of the carers over time. Thus, carers’ perceived quality of life was generally unchanged after 1 year except for their perceived physical health which worsened (Table 3).
Table 3.
Perceived quality of life of the carers
| Quality of life (WHOQOL-BREF) | Caregivers baseline (N = 98) | Caregivers follow-up (N = 78) | Australian population norm (Hawthorne et al. 2006) | |||
|---|---|---|---|---|---|---|
| Mean | s.d. | Mean | s.d. | Mean | s.d. | |
| Physical health | 72.6 | 17.1 | 68.3 | 18.6 | 73.5 | 18.1 |
| Psychological health | 70.1 | 15.4 | 70.2 | 15.2 | 70.6 | 14.0 |
| Social relationships | 66.9 | 19.3 | 64.9 | 20.6 | 71.5 | 18.2 |
| Environment | 73.5 | 16.9 | 74.0 | 16.1 | 75.1 | 13.0 |
Longitudinal relationships between functioning levels of people with psychosis and their carers’ health and wellbeing
Two outliers were removed because of atypical deterioration and their influence on estimates. In the cross-lagged analysis of MIVTIG scores with LSP total scores (Table 4), given that the path from LSP total scores to MIVTIG scores was large and statistically significant in comparison with the path from MIVTIG scores to LSP total scores, the conclusion was that LSP total scores had an effect on the MIVTIG scores. Higher values of LSP total scores at T1 caused lower values of MIVTIG at T2. There was no statistically significant effect of MIVTIG scores at T1 on LSP total scores at T2. This suggests that carers’ perceptions of better functioning of the SHIP participants resulted in less grief experienced by the carers at follow-up whereas grief in the carers did not have an effect on their perceptions of the functioning of SHIP participants at follow-up.
Table 4.
Cross-lagged analysis of caregiving variables with LSP total scores
| Variables at T1 | β | s.e. | p-value | |
|---|---|---|---|---|
| Equation 1: dependent variable = FSS at T2 | FSS | 0.656 | 0.083 | <0.001 |
| LSP total | 0.194 | 0.041 | 0.023 | |
| Equation 2: dependent variable = LSP total scores at T2 | LSP total | 0.821 | 0.069 | <0.001 |
| FSS | 0.034 | 0.137 | 0.617 | |
| Equation 1: dependent variable = K10 at T2 | K10 | 0.610 | 0.108 | <0.001 |
| LSP total | −0.100 | 0.073 | 0.292 | |
| Equation 2: dependent variable = LSP total scores at T2 | LSP total | 0.817 | 0.071 | <0.001 |
| K10 | −0.036 | 0.104 | 0.600 | |
| Equation 1: dependent variable = MIVTIG at T2 | MIVTIG | 0.288 | 0.096 | 0.007 |
| LSP total | −0.489 | 0.164 | <0.001 | |
| Equation 2: dependent variable = LSP total scores at T2 | LSP total | 0.840 | 0.066 | <0.001 |
| MIVTIG | 0.032 | 0.038 | 0.625 | |
| Equation 1: dependent variable = WHOQOL physical health at T2 | Physical | 0.718 | 0.087 | <0.001 |
| LSP total | −0.008 | 0.159 | 0.920 | |
| Equation 2: dependent variable = LSP total scores at T2 | LSP total | 0.808 | 0.066 | <0.001 |
| Physical | 0.118 | 0.036 | 0.074 | |
| Equation 1: dependent variable = WHOQOL psychological health at T2 | Psychological | 0.639 | 0.085 | <0.001 |
| LSP total | 0.195 | 0.134 | 0.025 | |
| Equation 2: dependent variable = LSP total scores at T2 | LSP total | 0.809 | 0.070 | <0.001 |
| Psychological | 0.061 | 0.045 | 0.379 | |
| Equation 1: dependent variable = WHOQOL social relationships at T2 | Social | 0.633 | 0.094 | <0.001 |
| LSP total | 0.154 | 0.184 | 0.085 | |
| Equation 2: dependent variable = LSP total scores at T2 | LSP total | 0.829 | 0.070 | <0.001 |
| Social | −0.002 | 0.036 | 0.973 | |
| Equation 1: dependent variable = WHOQOL environment at T2 | Environment | 0.792 | 0.066 | <0.001 |
| LSP total | 0.099 | 0.113 | 0.154 | |
| Equation 2: dependent variable = LSP total scores at T2 | LSP total | 0.807 | 0.068 | <0.001 |
| Environment | 0.090 | 0.040 | 0.182 |
FSS, friendship scale; LSP, life skills profile; MIVTIG, mental illness version of the Texas inventory of grief; SHIP, survey of high impact psychosis.
For the cross-lagged analysis of FSS scores with LSP total scores (Table 4), as the path from LSP total scores to FSS was small and statistically significant, the conclusion was LSP total scores had an effect on the FSS scores but the effect was not large. Higher values of LSP total scores at T1 caused higher values of FSS at T2. There was no statistically significant effect of FSS scores at T1 on LSP total scores at T2. This suggests that carers’ perceptions of better functioning of the SHIP participants drive greater social connection in the carers at follow-up and conversely, social isolation in the carers did not have an effect on their perceptions of the functioning of the SHIP participants.
Similarly, the path from LSP total scores to WHOQOL-BREF Psychological Health was small and statistically significant for the cross-lagged analysis of WHOQOL-BREF Psychological Health scores with LSP total scores (Table 4). This suggests that LSP total scores had a small effect on the WHOQOL-BREF Psychological Health scores whereas the psychological health of the carers did not have an effect on their perceptions of the functioning of the SHIP participants. Thus, carers’ perceptions of higher functioning of the SHIP participants appear to result in greater satisfaction in the psychological health of the carers but satisfaction with psychological health in the carers did not have an effect on their perception of the functioning of their relatives.
For other caregiving variables, although there were strong relationships between the functioning of the SHIP participants and the caregiving outcome variables, neither of the variables appeared to have a role in causing change in the other variable.
Discussion
This study was marked by its recruitment using representative sample methods and follow-up occasion of measurement after an extended time. Previous reviewers have used a 6-month follow-up as a cut-off in categorising short and long-term intervention studies for caregivers (Yesufu-Udechuku et al. 2015), therefore, this study's 1-year follow-up may be considered reasonably lengthy in capturing changes in carers’ health and wellbeing over time. Carers reported poor psychological health, social isolation, poor quality of life and prominent grief. Their health and wellbeing did not change much over 1 year, except that satisfaction with their physical health deteriorated significantly. Carers’ perceptions of the functioning of their relative or friend with psychosis were at least partially responsible for the levels of grief, satisfaction with psychological health and social connectedness observed at the second interview. While carer's poor psychological health might have influenced their responses (Gómez-de-Regil et al. 2014), results showed that carers’ poor health and wellbeing did not affect their perception of the functioning of their relative or friend with psychosis. The relatively lower percentage of SHIP participants living with their carers compared with other caregiving studies reflected the diverse accommodation arrangements of people with psychosis in Australia (Morgan et al. 2012) as well as the varied caregiver relationships extending beyond parental-child relationships. Both these observations support the generalisability of the findings regarding carers.
Health and wellbeing of carers
A high percentage of the carers reported social isolation well above population norms as measured by FSS, also reported in another Australian study (Hayes et al. 2015). Social connectedness was poor at initial interview and remained so over time. The perceived social isolation in the carers is likely due to the responsibilities and impact of caregiving. This explanation is supported by indications of a causative relationship between lower functioning of the people with psychosis and greater social isolation in their carers and is consistent with findings of Möller-Leimkühler & Wiesheu (2012). It may be that more impaired functioning of people with psychosis requires carers to spend more time in caring and they therefore have to sacrifice their social activities (Weimand et al. 2013).
Carers also reported moderate psychological distress as measured by K10, consistent with other population-based studies of carers (Szmukler et al. 1998; Train et al. 2001). Possibly reflecting the chronicity of illness of most of the SHIP participants and the close relationship between them and their carers, there was no improvement in the carers’ psychological health at follow-up within the context of SHIP participants receiving treatment from community mental health services. While comparison of the health and wellbeing of carers of people with early psychosis with carers of people with more prolonged psychotic disorders was not feasible given the sample size, a recent Australian study suggests that, over time, older carers might experience lesser burden as they have better coping abilities (Poon et al. 2015).
The longitudinal causal relationship between poor functioning of people with psychosis and their carers’ poorer perception of their psychological health as measured by WHOQOL-BREF supports the argument to improve functioning among people with psychoses to support their carers’ psychological health. In addition, there was no statistically significant change in their quality of life, except for their physical health, which carers perceived to have worsened over time. Although, one would expect some natural decline in aging carers’ physical health, however, the statistically significantly deterioration occurred in just 1 year. Therefore, it is important to assess the physical health of carers and provide them with appropriate treatment and interventions such as affordable and accessible respite services that could support their physical health (Gupta et al. 2015; Thunyadee et al. 2015).
The grief experienced by family members of people with mental illness was comparable with family members who had experienced a death in the family (Miller et al. 1990). Their grief was also stable over time. The prolonged feelings of grief in the carers are consistent with other (Godress et al. 2005). Furthermore, the results clearly indicate that the carers’ perception of the functioning of the SHIP participants is crucial in determining their levels of grief, although, professionals may fail to recognise and address this prolonged grief (Bland & Darlington, 2002). There is little emphasis on the relationship between the functioning of people with psychosis and carers’ feelings of grief in the literature. Discussions tended to focus on grief regarding parental-child relationships (Godress et al. 2005) and family interventions (Mulligan et al. 2013). This study extends this work to all carers and shows that the feelings of grief in carers are largely related to their perception of deterioration in the functioning of their relatives with psychosis. This impaired functioning indicates loss of independent living skills and an impaired societal role, with important consequences to provide effective psychiatric rehabilitation to improve the functioning of people with psychosis and to increase their ability to resume social and occupational roles.
Given the carers’ social isolation, poor quality of life, grief and psychological distress with little improvement at follow-up, current services are likely inadequate suggesting an urgent need to review them to improve the health and wellbeing of carers (Yesufu-Udechuku et al. 2015). Although there is a greater emphasis on including carers in mental health services, limited family interventions are provided to support their health and wellbeing. It is therefore questionable whether the greater emphasis on involvement of carers in mental health services will eventually lead to an overall improvement to their lives.
Carers’ perceptions of functioning levels of people with psychosis
Carers’ perceptions of the functioning of people with psychosis were found to be an important determinant of their own health and wellbeing. Although emotional impact on carers might cause their assessment of the functioning of their relatives to be biased (Parker et al. 1991), our study suggests that functioning levels had an effect on carers’ grief and psychological health instead of the converse, implying that the possibility of this subjective bias affecting carers’ assessments was unlikely. More importantly, given there are subjective biases in clinicians’ assessments of functioning of people with psychiatric illness (Trauer et al. 1995; Caqueo-Urízar et al. 2015), carers’ perceptions may be more useful in assessing their own health and wellbeing.
Strengths
This is the first Australian caregiver study to use a national prevalence study of psychosis to recruit carers in order to obtain generalisable results. Previous Australian population-based caregiver studies, such as the National Survey of Mental Health and Wellbeing, did not focus on psychosis (Pirkis et al. 2010). In addition, clinical information was unavailable in these studies and diagnoses of mental illnesses were not assigned using validated psychiatric measures by professional mental health clinicians, unlike in this caregiver study.
Limitations
The first limitation is that the percentage of recruited carers was low at 29.4% of those eligible, in spite of multiple strategies applied during recruitment. Comparison of those recruited with all eligible SHIP participants showed that there was likely no bias in the recruitment of their carers. The differences in living arrangements and employment status between the recruited sample and eligible SHIP participants may be due to the need to obtain consent of the people with psychosis before approaching carers, resulting in mainly recruiting carers who had good relationships with the SHIP participants. Although, seven carers did not return the questionnaires at follow-up, the follow-up rate was high at 84%. Those seven carers who did not return the questionnaires should be considered as refusing to participate. Although the follow-up recruitment of 1 year from the baseline recruitment was a potential limitation, the 1-year period was selected to minimise sample attrition and ensure a reasonable sample size for follow-up measurements and is supported by existing literature (Yesufu-Udechuku et al. 2015). The 1-year duration of the follow-up period is likely to have influenced the longitudinal results. A longer follow-up period would capture any slowly evolving trends. As the sample size was not large, it was not possible to define subgroups of participants to investigate factors such as the impact of early psychosis and chronic illness on the health and wellbeing of their carers.
Conclusion
Given the reciprocal relationships between carers’ health and wellbeing and functioning of those for whom they are caring, mental health service providers need to assess and support this potentially mutually beneficial relationship as a core component of service delivery (Froggat et al. 2007). Study findings suggest that current routine mental health services may not be effective in relieving the burden of caregiving or supporting the physical health of carers. Psychosocial rehabilitation for people with psychosis likely has greater potential to improve carers’ health and wellbeing over time. In addition, as carers’ perceptions of their relatives’ functioning levels were an important determinant of their own self-rated health and wellbeing, it is important for carers to complete a functioning measurement tool such as LSP-20, assessing the functioning levels of the corresponding people with psychosis. This study serves as a benchmark for a future nation-wide longitudinal study with a larger sample size and longer follow-up period to understand long-term caregiving impact and changes in carers’ health and wellbeing over time.
Acknowledgements
This publication is based on data (patient-related) collected in the framework of the 2010 Australian National Survey of High Impact Psychosis. The members of the Survey of High Impact Psychosis Study Group are: V. Morgan (National Project Director), A. Jablensky (Chief Scientific Advisor), A. Waterreus (National Project Coordinator), R. Bush, V. Carr, D. Castle, M. Cohen, C. Galletly, C. Harvey, B. Hocking, A. Mackinnon, P. McGorry, J. McGrath, A. Neil, S. Saw, H. Stain. Ethics approvals for the SHIP study were obtained from relevant institutional human research ethics committees. The SHIP study was funded by the Australian Government Department of Health and Ageing. This report acknowledges all the effort and hard work by the local site coordinators. We would also like to thank mental health professionals who participated in the preparation and conduct of the survey and the many Australians with psychotic disorders and their caregivers who gave their time and whose responses form the basis of this publication.
Financial Support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Conflict of Interest
None.
Ethical Standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
References
- Australian Bureau of Statistics (2012). Australian Health Survey: First Results. Government of Australia. http://www.abs.gov.au/ausstats/abs@.nsf/Lookup/4338.0main+features42011-13
- Awad AG, Voruganti LNP (2008). The burden of schizophrenia on caregivers: a review. Pharmacoeconomics 26, 149–162. [DOI] [PubMed] [Google Scholar]
- Bland R, Darlington Y (2002). The nature and sources of hope: perspectives of family caregivers of people with serious mental illness. Perspectives in Psychiatric Care 38, 61–68. [DOI] [PubMed] [Google Scholar]
- Caqueo-Urízar A, Miranda-Castillo C, Lemos Giráldez S, Lee Maturana S-L, Ramírez Pérez M, Mascayano Tapia F (2014). An updated review on burden on caregivers of schizophrenia patients. Psicothema 26, 235–243. [DOI] [PubMed] [Google Scholar]
- Caqueo-Urízar A, Boyer L, Baumstarck K, Gilman S (2015). Subjective perceptions of cognitive deficits and their influences on quality of life among patients with schizophrenia. Quality of Life Research 24, 2753–2760. [DOI] [PubMed] [Google Scholar]
- Castle DJ, Jablensky A, McGrath JJ, Carr V, Morgan V, Waterreus A, Stain H, McGuffin P, Farmer A (2006). The diagnostic interview for psychoses (DIP): development, reliability and applications. Psychological Medicine 36, 69–80. [DOI] [PubMed] [Google Scholar]
- Department of Human Services (2006). Caring Together: An Action Plan for Carer Involvement in Victorian Public Mental Health Services. Mental Health Branch, Victorian Government Department of Human Services, Melbourne Victoria: Melbourne. [Google Scholar]
- Finkel SE (1995). Causal Analysis with Panel Data. SAGE: Thousand Oaks, CA. [Google Scholar]
- Froggat D, Fadden G, Johnson DL, Leggatt M, Shankar R (2007). Families as Partners in Mental Health Care: A Guidebook for Implementing Family Work. World Fellowship for Schizophrenia and Allied Disorders: Toronto. [Google Scholar]
- Godress J, Ozgul S, Owen C, Foley Evans L (2005). Grief experiences of parents whose children suffer from mental illness. Australian and New Zealand Journal of Psychiatry 39, 88–94. [DOI] [PubMed] [Google Scholar]
- Gómez-de-Regil L, Kwapil TR, Barrantes-Vidal N (2014). Predictors of expressed emotion, burden and quality of life in relatives of Mexican patients with psychosis. Journal of Psychiatric and Mental Health Nursing 21, 170–179. [DOI] [PubMed] [Google Scholar]
- Green SB (1991). How many subjects does it take to do a regression analysis. Multivariate Behavioral Research 26, 499–510. [DOI] [PubMed] [Google Scholar]
- Gupta S, Isherwood G, Jones K, Van Impe K (2015). Assessing health status in informal schizophrenia caregivers compared with health status in non-caregivers and caregivers of other conditions. BMC Psychiatry 15, 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawthorne G (2006). Measuring social isolation in older adults: development and initial validation of the friendship scale. Social Indicators Research 77, 521–548. [Google Scholar]
- Hawthorne G (2008). Perceived social isolation in a community sample: its prevalence and correlates with aspects of peoples' lives. Social Psychiatry and Psychiatric Epidemiology 43, 140–150. [DOI] [PubMed] [Google Scholar]
- Hawthorne G, Herrman H, Murphy B (2006). Interpreting the WHOQOL-Bref: preliminary population norms and effect sizes. Social Indicators Research 77, 37–59. [Google Scholar]
- Hayes L, Hawthorne G, Farhall J, O'Hanlon B, Harvey C (2015). Quality of life and social isolation among caregivers of adults with schizophrenia: policy and outcomes. Community and Mental Health Journal 51, 591–597. [DOI] [PubMed] [Google Scholar]
- IBM Corp (2012). IBM SPSS Statistics for Windows. IBM Corp: Armonk, NK. [Google Scholar]
- Jansen JE, Gleeson J, Cotton S (2015). Towards a better understanding of caregiver distress in early psychosis: a systematic review of the psychological factors involved. Clinical Psychology Review 35, 56–66. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Andrews G, Colpe LJ, Hiripi E, Mroczek DK, Normand SLT, Walters EE, Zaslavsky AM (2002). Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychological Medicine 32, 959–976. [DOI] [PubMed] [Google Scholar]
- Miller FE, Dworkin J, Ward M, Barone D (1990). A preliminary study of unresolved grief in families of seriously mentally ill patients. Hospital & Community Psychiatry 41, 1321–1325. [DOI] [PubMed] [Google Scholar]
- Möller-Leimkühler A, Wiesheu A (2012). Caregiver burden in chronic mental illness: the role of patient and caregiver characteristics. European Archives of Psychiatry and Clinical Neuroscience 262, 157–166. [DOI] [PubMed] [Google Scholar]
- Morgan VA, Waterreus A, Jablensky A, Mackinnon A, McGrath JJ, Carr V, Bush R, Castle D, Cohen M, Harvey C, Galletly C, Stain HJ, Neil AL, McGorry P, Hocking B, Shah S, Saw S (2012). People living with psychotic illness in 2010: the second Australian national survey of psychosis. Australian and New Zealand Journal of Psychiatry 46, 735–752. [DOI] [PubMed] [Google Scholar]
- Morosini PL, Magliano L, Brambilla L, Ugolini S, Pioli R (2000). Development, reliability and acceptability of a new version of the DSM-IV Social and Occupational Functioning Assessment Scale (SOFAS) to assess routine social functioning. Acta Psychiatrica Scandinavica 101, 323–329. [PubMed] [Google Scholar]
- Mulligan J, Sellwood W, Reid GS, Riddell S, Andy N (2013). Informal caregivers in early psychosis: evaluation of need for psychosocial intervention and unresolved grief. Early Intervention in Psychiatry 7, 291–299. [DOI] [PubMed] [Google Scholar]
- Ohaeri JU (2003). The burden of caregiving in families with a mental illness: a review of 2002. Current Opinion in Psychiatry 16, 457–465. [Google Scholar]
- Parker G, Rosen A, Emdur N, Hadzi-Pavlov D (1991). The Life Skills Profile: psychometric properties of a measure assessing function and disability in schizophrenia. Acta Psychiatrica Scandinavica 83, 145–152. [DOI] [PubMed] [Google Scholar]
- Pirkis J, Burgess P, Hardy J, Harris M, Slade T, Johnston A (2010). Who cares? A profile of people who care for relatives with a mental disorder. Australian and New Zealand Journal of Psychiatry 44, 929–937. [DOI] [PubMed] [Google Scholar]
- Poon WC, Joubert L, Harvey C (2015). A longitudinal study of the health and wellbeing of culturally and linguistically diverse carers of people with psychosis. International Journal of Social Psychiatry 61, 743–753. [DOI] [PubMed] [Google Scholar]
- Randolph C, Tierney MC, Mohr E, Chase TN (1998). The repeatable battery for the assessment of neuropsychological status (RBANS): preliminary clinical validity. Journal of Clinical Experimental and Neuropsychology 20, 310–319. [DOI] [PubMed] [Google Scholar]
- Rosen A, Trauer T, Hadzi-Pavlovic D, Parker G (2001). Development of a brief form of the Life Skills Profile: the LSP-20. Australian and New Zealand Journal of Psychiatry 35, 677–683. [DOI] [PubMed] [Google Scholar]
- Shibre T, Medhin G, Teferra S, Wakwoya A, Berhanu E, Abdulahi A, Alem A, Fekadu A (2012). Predictors of carer-burden in schizophrenia: a five year follow-up study in Butajira, Ethiopia. Ethiopian Medical Journal 50, 125–133. [PubMed] [Google Scholar]
- Szmukler GI, Wykes T, Parkman S (1998). Caregiving and the impact on carers of a community mental health service. The British Journal of Psychiatry 173, 399–403. [DOI] [PubMed] [Google Scholar]
- Thunyadee C, Sitthimongkol Y, Sangon S, Chai-Aroon T, Hegadoren KM (2015). Predictors of depressive symptoms and physical health in caregivers of individuals with schizophrenia. Nursing & Health Sciences 17, 412–419. [DOI] [PubMed] [Google Scholar]
- Train GH, Livingston G, Manela M (2001). Addressing the needs of carers of older people: the Islington study. International Journal of Geriatric Psychiatry 17, 85–86. [DOI] [PubMed] [Google Scholar]
- Trauer T, Duckmanton RA, Chiu E (1995). The Life Skills Profile: a study of its psychometric properties. Australian and New Zealand Journal of Psychiatry 29, 492–499. [DOI] [PubMed] [Google Scholar]
- van Wijngaarden B, Schene A, Koeter M, Becker T, Knapp M, Knudsen HC, Tansella M, Thornicroft G, Vázquez-Barquero J-L, Lasalvia A, Leese M, Epsilon study group (2003). People with schizophrenia in five countries: conceptual similarities and intercultural differences in family caregiving. Schizophrenia Bulletin 29, 573–586. [DOI] [PubMed] [Google Scholar]
- Weimand BM, Hall-Lord ML, Sällström C, Hedelin B (2013). Life-sharing experiences of relatives of persons with severe mental illness - a phenomenographic study. Scandinavian Journal of Caring Sciences 27, 99–107. [DOI] [PubMed] [Google Scholar]
- WHOQOL Group (1998). Development of the World Health Organization WHOQOL-BREF quality of life assessment. Psychological Medicine 28, 551–558. [DOI] [PubMed] [Google Scholar]
- Yesufu-Udechuku A, Harrison B, Mayo-Wilson E, Young N, Woodhams P, Shiers D, Kuipers E, Kendall T (2015). Interventions to improve the experience of caring for people with severe mental illness: systematic review and meta-analysis. The British Journal of Psychiatry 206, 268–274. [DOI] [PubMed] [Google Scholar]