Abstract
Aims.
Whether the public stigma associated with mental illness negatively affects an individual, largely depends on whether the person has been labelled ‘mentally ill’. For labelled individuals concealing mental illness is a common strategy to cope with mental illness stigma, despite secrecy's potential negative consequences. In addition, initial evidence points to a link between stigma and suicidality, but quantitative data from community samples are lacking.
Methods.
Based on previous literature about mental illness stigma and suicidality, as well as about the potential influence of labelling processes and secrecy, a theory-driven model linking perceived mental illness stigma and suicidal ideation by a mediation of secrecy and hopelessness was established. This model was tested separately among labelled and unlabelled persons using data derived from a Swiss cross-sectional population-based study. A large community sample of people with elevated psychiatric symptoms was examined by interviews and self-report, collecting information on perceived stigma, secrecy, hopelessness and suicidal ideation. Participants who had ever used mental health services were considered as labelled ‘mentally ill’. A descriptive analysis, stratified logistic regression models and a path analysis testing a three-path mediation effect were conducted.
Results.
While no significant differences between labelled and unlabelled participants were observed regarding perceived stigma and secrecy, labelled individuals reported significantly higher frequencies of suicidal ideation and feelings of hopelessness. More perceived stigma was associated with suicidal ideation among labelled, but not among unlabelled individuals. In the path analysis, this link was mediated by increased secrecy and hopelessness.
Conclusions.
Results from this study indicate that among persons labelled ‘mentally ill’, mental illness stigma is a contributor to suicidal ideation. One explanation for this association is the relation perceived stigma has with secrecy, which introduces negative emotional consequences. If our findings are replicated, they would suggest that programmes empowering people in treatment for mental illness to cope with anticipated and experienced discrimination as well as interventions to reduce public stigma within society could improve suicide prevention.
Key words: Hopelessness, mental illness stigma, secrecy, suicidal ideation
Introduction
People with mental disorders commonly face stigmatising stereotypes, prejudice and discrimination. The anticipation and experience of being stigmatised in one's everyday life introduce a variety of negative consequences, including low rates of help-seeking behaviour, unemployment, social isolation, impaired quality of life, low self-esteem, and feelings of shame and hopelessness (Rüsch et al. 2005; Link & Phelan, 2013).
Whether or not individuals have been labelled as ‘mentally ill’, they tend to perceive similar levels of negative attitudes or public stigma in society. However, stigma's impact varies greatly across different persons with mental health problems (Corrigan & Watson, 2002; Rüsch et al. 2006). A potential explanation for this variability is provided by the Modified Labelling Theory, developed by Link et al. (1989). The theory implies that stigmatising misconceptions present in society are only relevant for persons labelled as ‘mentally ill’. One of the most important reasons for being labelled is the use of mental health services (Link et al. 1989). While the perception of mental illness stigma is largely irrelevant for unlabelled persons, labelled individuals are likely to develop fear of social rejection and adapt coping strategies. A key strategy is to conceal one's mental illness in order to avoid the label and the resulting stigma. Even though secrecy reduces discrimination, it can be harmful, leading to increased cognitive and emotional distress in terms of self-consciousness, hypervigilance, feelings of shame, guilt, helplessness, sadness, hopelessness, fear of discovery and the decisional conflict between disclosure and non-disclosure (Link et al. 1991; Pachankis, 2007; Corrigan et al. 2013).
Many of the negative emotional consequences introduced by mental illness stigma (e.g., low self-esteem, feelings of loneliness, shame, hopelessness) are also predictors of suicidality (Rüsch et al. 2014). With globally around 1 000 000 completed suicides per year and many more attempted suicides, the topic is a major public health issue (World Health Organization, 2014). Even though suicide is a very complex phenomenon with a variety of social and individual risk factors, previous research has consistently identified psychiatric disorders to be a key determinant for suicidality (Selby et al. 2014; World Health Organization, 2014). Psychological autopsy studies showed that in around 90% of suicide victims evidence for the presence of a psychiatric disorder can be found (Cavanagh et al. 2003). However, even though mental illness is strongly associated with suicide, not everyone with a mental illness experiences suicidality (Harris & Barraclough, 1997; Bostwick & Pankratz, 2000; Miret et al. 2013). Thus, the anticipation or experience of mental illness stigma has been hypothesised as providing at least a partial explanation for the observed variability in suicide risk among persons with psychiatric disorders (Rüsch et al. 2014).
Recent research testing this hypothesis has found initial evidence for its validity. For example, a population-based study using data from several European countries reported that national mental illness stigma levels were positively associated with national suicide rates (Schomerus et al. 2015), and two other studies found positive associations between suicidality and self-stigma, stigma stress and shame (Sharaf et al. 2012; Bryan et al. 2013). Additionally, in qualitative research, patients reported that experienced discrimination due to their mental illness contributed to their suicidal behaviour (Farrelly et al. 2015).
Even though previous studies provided interesting findings, the association and the underlying paths between mental illness stigma and suicidality remain unclear. In addition, so far research examined participants within clinical settings or data derived from representative population polls. To date, no study examined the association between perceived mental illness stigma and suicidal ideation in a community sample of persons with elevated psychiatric symptoms, investigating the influence of labelling due to mental health service use.
Aim, hypotheses and research questions
Building on previous findings highlighted in the introduction section the present study tested a theory-driven model linking perceived mental illness stigma and suicidal ideation by a mediation of secrecy and hopelessness, using data from a large community sample of people with elevated psychiatric symptoms. Based on Modified Labelling Theory, perceived mental illness stigma was expected to be positively associated with suicidal ideation among persons labelled as ‘mentally ill’ by previous mental health service use, but not among unlabelled individuals. In addition, a three-path mediation of secrecy and hopelessness was expected to at least partially explain the association between perceived mental illness stigma and suicidal ideation.
Methods
Design and participants
All data were derived from the Epidemiology survey of the ZInEP-study (Zurich Program for Sustainable Development of Mental Health Services, www.zinep.ch), a cross-sectional population-based study conducted between August 2010 and September 2012 that aimed to assess the prevalence of common mental disorders and the use of mental health care services among people living in the Canton of Zurich in Switzerland (for details see Ajdacic-Gross et al. 2014). Telephone screening interviews among a random sample of people aged 20–years drawn from the Zurich population registry were conducted (N = 9829). During the telephone interviews, Global Severity Index (GSI) scores of participants were obtained using the Symptom Checklist-27 (SCL-27) (Hardt et al. 2004). On 27 items participants indicated their level of distress due to symptoms of mental illness during the last 7 days on a five-point Likert scale. The GSI was defined as the mean score across all items, and a 75th percentile cut-off point was used to stratify the total sample into low and high scorers. Then, one random sample within each of the two groups was drawn to participate in subsequent face-to-face interviews and complete questionnaires (600 low scorers and 900 high scorers).
The present study analysed participants screened with a GSI equal or above the 75th percentile (high scorers, N = 900). Due to missing values in the questionnaire data, 681 individuals remained for the statistical analysis. For the purpose of this project, the study sample was stratified based on lifetime mental health service use to compare results among unlabelled persons (N = 252) and those labelled as ‘mentally ill’ (N = 429).
Measures
Suicidal ideation was assessed during the face-to-face interviews by two consecutive dichotomous questions (no v. yes). First, participants were asked: ‘During the past 12 months did you have the feeling you would not mind being dead, or did you have plans to hurt yourself?’ followed by the question: ‘During the past 12 months, did you experience vague or serious suicidal thoughts, death wishes, suicide attempts?’ Since sufficient severity was reflected in both questions, everyone who answered with ‘yes’ on either of the two questions was classified as having experienced suicidal ideation during the past 12 months.
Perceived mental illness stigma, or the perception of how negatively most people view individuals with a mental illness, was assessed using the 12-item Perceived Devaluation Discrimination Questionnaire (PDDQ) (Link et al. 1989). Participants rated statements reflecting typical public stereotypes from 1 (not true at all) to 6 (very true), e.g., ‘Most people believe that entering a mental hospital is a sign of personal failure’. Higher mean values indicated more perceived mental illness stigma (Cronbach's α in this study is 0.87). Secrecy was measured using the nine-item secrecy subscale of the Stigma Coping Orientation Scales (SCOS) (Link et al. 2002). Participants indicated their opinion on whether mental illness should be concealed, e.g., ‘If you have ever been in treatment for a serious mental illness, the best thing to do is to keep it a secret.’ Answers were made from 1 (not true at all) to 6 (very true) with higher mean scores indicating increased secrecy (Cronbach's α in this study is 0.89). Feelings of hopelessness were assessed during the face-to-face interviews as part of a questionnaire focusing on symptoms of major depressive disorder. Participants were asked whether they had experienced feelings of hopelessness during the past 12 months and responded on a binary scale (no v. yes). Depressive symptoms were assessed by the respective four-item subscale of the SCL-27 (Hardt et al. 2004).
As mentioned earlier, persons who had ever used mental health services were considered as labelled ‘mentally ill’. People were asked about their previous and current mental health service use and classified as either ‘never used services’ (unlabelled) or ‘ever used services’ (labelled). Mental health service use was assessed via self-report and defined as having sought professional help for a mental health problem, including seeing a psychologist, psychiatrist or general practitioner.
Statistical analyses
The distributions of continuous variables in the total sample and among the two subgroups (labelled v. unlabelled) were examined visually and no violation of the normal distribution assumption was found. In addition, a correlation matrix of independent variables and the outcome was examined to rule out potential multicollinearity. Characteristics of the sample were described and t-tests (continuous variables) or chi-square (χ2) tests (categorical variables) were calculated to test for significant differences between the groups (Table 1). Bivariate associations with suicidality using point-biserial correlation for continuous independent variables and χ2 tests and phi (φ)-coefficients for categorical independent variables were estimated (Table 2). Subsequently, multiple binary logistic regression models of perceived mental illness stigma on suicidal ideation were performed (Table 3). The first model did not include any potential mediating or confounding variables; thereafter, mediators and confounders were consecutively added to the analysis.
Table 1.
Characteristics of the total sample and stratified by mental health service use. Results presented as: mean (s.d.) or % frequency
| Lifetime mental health service use | ||||
|---|---|---|---|---|
| Never | Ever | Sign.* | ||
| Variables (and range of mean scores, where appropriate) | Total sample N = 681 | N = 252 | N = 429 | |
| Suicidal ideation during the past 12 months (yes) | 20.2% | 12.3% | 24.8% | p < 0.001 |
| Perceived stigma (1–6) | 3.78 (0.87) | 3.75 (0.84) | 3.79 (0.88) | p = 0.53 |
| Secrecy (1–6) | 3.25 (1.14) | 3.32 (1.09) | 3.20 (1.16) | p = 0.20 |
| Hopelessness during the past 12 months (yes) | 37.6% | 26.8% | 43.7% | p < 0.001 |
| Depressive symptoms (1–5) | 2.35 (0.68) | 2.20 (0.58) | 2.44 (0.72) | p < 0.001 |
| Sex (female) | 53.7% | 44.6% | 58.9% | p < 0.001 |
| Age in years (21–42) | 30.00 (6.53) | 28.60 (6.54) | 30.83 (6.39) | p < 0.001 |
t-tests (continuous variables) or χ2 tests (categorical variables).
Table 2.
Bivariate associations between the independent variables and suicidal ideation (point-biserial correlation for continuous variables, as well as χ2 test and φ-coefficient for binary variables)
| Lifetime mental health service use | ||
|---|---|---|
| Never | Ever | |
| N = 252 | N = 429 | |
| Point-biserial correlation | ||
| Perceived stigma | 0.01 | 0.12* |
| Secrecy | 0.08 | 0.08 |
| Depressive symptoms | 0.26*** | 0.36*** |
| Age in years (21–42) | −0.07 | −0.03 |
| χ2 test | ||
| Hopelessness (yes) | χ2 = 17.58*** | χ2 = 73.95*** |
| φ = 0.26*** | φ = 0.41*** | |
| Sex (female) | χ2 = 0.21 | χ2 = 0.01 |
| φ = −0.03 | φ = −0.01 | |
*p < 0.05, ***p < 0.001.
Table 3.
Binary logistic regression models of perceived mental illness stigma on suicidal ideation
| Lifetime mental health service use | |||||
|---|---|---|---|---|---|
| Never n = 252 | Ever n = 429 | ||||
| OR | 95% CI | OR | 95% CI | ||
| Block 1 | Perceived stigma | 1.01 | 0.64–1.60 | 1.35* | 1.05–1.73 |
| Block 2 | Perceived stigma | 0.92 | 0.57–1.47 | 1.29 | 0.99–1.68 |
| Secrecy | 1.27 | 0.87–1.86 | 1.09 | 0.89–1.32 | |
| Block 3 | Perceived stigma | 1.04 | 0.66–1.65 | 1.31* | 1.00–1.70 |
| Hopelessness (yes) | 4.88*** | 2.21–10.77 | 7.33*** | 4.45–12.01 | |
| Block 4 | Perceived stigma | 0.95 | 0.59–1.53 | 1.28 | 0.97–1.70 |
| Secrecy | 1.30 | 0.88–1.93 | 1.00 | 0.81–1.25 | |
| Hopelessness (yes) | 4.97*** | 2.24–11.02 | 7.45*** | 4.53–12.24 | |
| Block 5 | Perceived stigma | 0.97 | 0.59–1.59 | 1.21 | 0.90–1.64 |
| Secrecy | 1.25 | 0.82–1.90 | 1.07 | 0.84–1.35 | |
| Hopelessness (yes) | 2.95* | 1.20–7.24 | 5.17*** | 3.06–8.72 | |
| Depressive symptoms | 3.33** | 1.59–6.97 | 2.75*** | 1.89–4.03 | |
| Sex (female) | 0.57 | 0.24–1.35 | 0.77 | 0.54–1.56 | |
| Age in years | 0.97 | 0.91–1.04 | 0.98 | 0.94–1.02 | |
*p < 0.05, **p < 0.01, ***p < 0.001.
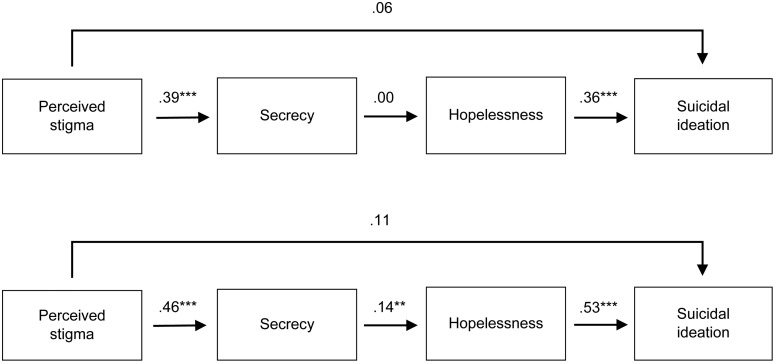
Finally, a path analysis based on the hypothesised multiple mediation model was conducted (Fig. 1). All paths were controlled for depressive symptoms, age and sex. Since a dichotomous outcome was modelled, diagonally weighted least squares (DWLS) were used as a robust alternative for the maximum likelihood estimation (Steinmetz, 2014). Thus, effects are reported as standardised probit regression coefficients, which indicate the change in the z-score (probit index) of the outcome for a one-unit change in the predictor. Acceptable model fit is indicated by a non-significant scaled χ2 statistic, a Root Mean Square Error of Approximation (RMSEA) <0.06, a Tucker Lewis Index (TLI) >0.90, a Comparative Fit Index (CFI) >0.95 and a Weighted Root Mean Square Residual (WRMR) <1.0 (Hancock & Mueller, 2013). In addition, pseudo R2 values were obtained. Indirect effects were tested using the bootstrapping approach (bootstrap replications: 1000) (Preacher & Hayes, 2008; Taylor et al. 2008). SPSS version 21 was used for analyses, except for the path analysis in R, version 3.1.2 (lavaan library).
Fig. 1.
Results obtained from the path analyses, testing the three-path mediation effect of secrecy and hopelessness among unlabelled persons (upper path diagram, N = 252, R2 = 0.19) and individuals labelled by lifetime mental health service use (lower path diagram, N = 429, R2 = 0.26). **p < 0.01, ***p < 0.001.
Results
Descriptive analysis
Comparing participants with complete data to those with missing values, we found no significant differences with regard to suicidal ideation (16.5% among non-completers and 20.2% among completers, p = 0.12), hopelessness (40.0% among non-completers and 37.6% among completers, p = 0.38), GSI-scores (mean 2.11 among non-completers and mean 2.10 among completers, p = 0.91) and depressive symptoms (mean 2.37 among completers and mean 2.35 among non-completers, p = 0.76). Non-completers were of younger age than completers (28.9 v. 30 years, respectively, p = 0.04) and showed a different gender-distribution, with 40% of non-completers being female, compared with 58.3% female participants with complete data (p < 0.001).
After the exclusion of persons with missing data, the final study sample was almost equally split in terms of gender (53.7% female) and on average about 30 years old (range 21–42). Most participants were single (78.3%, including divorced, separated or widowed), and 21.6% were married. Although 18% reported to be unemployed (including sick-leave), 82% reported to work full- or half time. When asked about education, about one-third of participants (38.2%) reported to have completed an apprenticeship, 21.6% had a university entrance certificate, 35.5% reported to possess a university diploma, and 3.8% indicated mandatory school as their highest educational degree.
Compared with the midpoint of the scales, a medium to high presence of perceived mental illness stigma, a medium level of secrecy and medium depressive symptoms were found (Table 1). About two-thirds of the participants reported having ever used mental health services and were thus classified as labelled ‘mentally ill’. Compared with the non-labelled participants, labelled participants reported significantly higher frequencies of suicidal ideation and feelings of hopelessness during the past 12 months. No significant differences between the groups were found when comparing levels of perceived mental illness stigma and secrecy. In addition, mean depressive symptoms were significantly increased among those who had ever used mental health services.
Bivariate analysis
Table 2 presents the results of the bivariate analysis testing the association between independent variables and suicidal ideation. Among participants labelled by mental health service use, a significant positive association was found between perceived mental illness stigma and suicidal ideation. In both groups, hopelessness and depressive symptoms were positively associated with suicidal ideation.
In addition, among unlabelled persons, perceived stigma was positively associated with secrecy (r = 0.32, p < 0.001), and no relationship was found between secrecy and hopelessness (r = −0.01, p = 0.88). Among labelled individuals a significant positive association was found between perceived stigma and secrecy (r = 0.37, p < 0.001) and between secrecy and hopelessness (r = 0.12, p < 0.05). Among both groups, perceived stigma was not associated with feelings of hopelessness (labelled group: r = 0.06, p = 0.19; unlabelled group: r = −0.03, p = 0.63).
Logistic regression analysis
In accordance with our hypothesis, in block 1, perceived mental illness stigma was associated with suicidal ideation among people who had ever used mental health services, but not among those who had never used such services (Table 3). When secrecy was included in the model (block 2), the previously observed positive association between perceived mental illness stigma and suicidal ideation among those labelled by service use was no longer significant. Replacing secrecy with feelings of hopelessness (block 3), a similar phenomenon was observed with a decreased but marginally significant effect of perceived stigma on suicidal ideation. Including both, secrecy and feelings of hopelessness in the same model further diminished the effects (block 4). In a last step, depressive symptoms, sex and age were included (block 5). Among both groups, a strong positive association with suicidal ideation was found for hopelessness and depressive symptoms.
Path analyses
Finally, to test the hypothesised three-path mediation of secrecy and hopelessness in the association between perceived stigma and suicidal ideation, two-path analyses were performed (Fig. 1). Analyses were done separately for the two previously established groups, comparing labelled persons who had ever used mental health services to unlabelled individuals who had never used services. Saturated models (estimated parameters = data points) were estimated for both groups, and therefore model fit could not be evaluated. Even though two degrees of freedom were present in both models, low correlations between the variables could have led to little restriction within the models, resulting in model saturation. This is clearly indicated by inflated TLI and CFI values and RMSEA equal to zero (Table 4) (Hancock & Mueller, 2013).
Table 4.
Fit indices of the path analytic models
| N | df | p (χ2)* | RMSEA* | TLI* | CFI* | WRMR* | |
|---|---|---|---|---|---|---|---|
| Service use: ever | 429 | 2 | 0.96 | 0.00 | 1.07 | 1.00 | 0.02 |
| Service use: never | 252 | 2 | 0.53 | 0.00 | 1.08 | 1.00 | 0.21 |
Good fit is indicated by a non-significant χ2, RMSEA < 0.06, TLI >0.90, CFI >0.95, WRMR < 1 (Hancock & Mueller, 2013).
Path estimates obtained from the path analysis are shown in Fig. 1. Strong positive significant associations between perceived mental illness stigma and secrecy as well as between hopelessness and suicidal ideation were observed in both models. While secrecy was positively associated with hopelessness among people with a history of mental health service use, no significant association was found among persons who had never used services. To test indirect effects of mental illness stigma on suicidal ideation the bootstrapping approach was used and a significant three-path mediation effect of secrecy and hopelessness was found among people labelled as ‘mentally ill’ (p < 0.01), but not among the unlabelled persons (p = 0.98). Among the labelled participants, a pseudo R2 of 0.26 was found for suicidal ideation, compared with a pseudo R2 of 0.19 among the unlabelled persons.
Discussion
Testing a theory-driven model to explain the association between perceived mental illness stigma and suicidal ideation, increased perceived stigma was associated with suicidal ideation only among the labelled individuals. This was explained by a three-path mediation effect of secrecy and hopelessness.
Our findings add to previous research on mental illness stigma contributing to suicidality (Sharaf et al. 2012; Bryan et al. 2013; Niederkrotenthaler et al. 2014; Reynders et al. 2014; Farrelly et al. 2015; Schomerus et al. 2015). Previous studies could not clarify whether the labelling status might alter the relationship between mental illness stigma and suicidality. Consistent with Modified Labelling Theory, in the labelled and the unlabelled groups we found similar, moderately positive associations between the level of perceived stigma and the attitude that psychiatric disorders should be concealed. However, only among those labelled by previous mental health service use more perceived stigma was significantly associated with suicidal ideation. While unlabelled persons appeared to be unaffected by perceived stigma, secrecy was linked to hopelessness in the labelled group. A likely explanation is that only in the labelled group secrecy shapes individuals’ actual social behaviour and thus becomes harmful in terms of hopelessness and social isolation. This is consistent with previous findings on harmful consequences of secrecy among minority group members (Pachankis, 2007). In line with Modified Labelling Theory, our findings indicate that being labelled as ‘mentally ill’ might be a crucial factor in explaining the observed variation in the impact perceived mental illness stigma has on people with psychiatric disorders.
This study has several strengths. To the best of our knowledge, it is the first to use a large community sample with elevated psychiatric symptoms to examine a potential pathway between perceived mental illness stigma and suicidal ideation. While all participants reported elevated psychiatric symptoms, only around two-thirds had ever used mental health services and we therefore could examine the role of labelling status.
However, limitations of the study should be considered. Logistic regression modelling requires a sufficient number of cases to obtain reliable estimates (Hosmer et al. 2013). However, while earlier work recommended the 10 : 1 rule (ten events per parameter; Peduzzi et al. 1996), as illustrated by Vittinghoff & McCulloch (2007) a 5 : 1 rule is legitimate. Further, our labelling variable (lifetime mental health service use) does not identify all persons labelled as ‘mentally ill’ and thus introduces misclassification bias. Even though having never utilised mental health services, a person might still perceive herself as a member of the stigmatised group (i.e., as labelled) if other classifying attributes are present (e.g., recognising symptoms as a mental disorder). Even though the definition of the mediating variables was based on pertinent literature, other potential mediators could have been omitted and other effects of the chosen variables are possible (e.g., confounding effects). Regarding the used measures, the limited information of a binary scale must be acknowledged. In addition, underreporting of suicidal ideation is likely since suicide is a largely stigmatised topic (Sudak et al. 2008). Thus a systematic misclassification of cases is possible with people who are more aware of mental illness stigma not disclosing their suicidal ideation. As a consequence the obtained results might underestimate the true association between perceived mental illness stigma and suicidal ideation. In the path analysis, pseudo R2 values indicated small explanatory power; however, the obtained path estimates provide support for the hypothesised mediation effect. Finally, even though the analysis of mediating effects in cross-sectional data is common, the interpretation of obtained results in terms of causality demands caution as reverse causality is possible (Gu et al. 2014).
Conclusion
In summary, our results indicate that among persons labelled as ‘mentally ill’ the perception of mental illness stigma contributes to suicidal ideation, which was explained by increased secrecy and hopelessness. If replicated, our findings suggest that programmes empowering people in treatment for mental illness to cope with anticipated and experienced discrimination as well as interventions to reduce mental illness stigma within the society could improve suicide prevention.
Acknowledgements
We are grateful to all participants.
Financial Support
ZInEP was supported by a private donation. The donor had no further role in the experimental design, the collection, analysis, and interpretation of data, the writing of this report or the decision to submit this paper for publication. The ZInEP Epidemiology Survey, in particular research in the Center for Neurophysiology and Sociophysiology, was supported by the Swiss National Science Foundation (Grant no. 3247B0–122071). The population and education data were provided by the Swiss Federal Statistical Office.
Conflict of Interest
None.
Ethical Standard
All individuals gave their informed consent prior to their participation. The study was approved by the Cantonal Ethics Commission Zurich (Reference number: 2009-0061/3).
References
- Ajdacic-Gross V, Müller M, Rodgers S, Warnke I, Hengartner MP, Landolt K, Hagenmuller F, Meier M, Tse L-T, Aleksandrowicz A, Passardi M, Knöpfli D, Schönfelder H, Eisele J, Rüsch N, Haker H, Kawohl W, Rössler W (2014). The ZInEP epidemiology survey: background, design and methods. International Journal of Methods in Psychiatric Research 23, 451–468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bostwick JM, Pankratz VS (2000). Affective disorders and suicide risk: a reexamination. American Journal of Psychiatry 157, 1925–1932. [DOI] [PubMed] [Google Scholar]
- Bryan CJ, Ray-Sannerud B, Morrow CE, Etienne N (2013). Shame, pride, and suicidal ideation in a military clinical sample. Journal of Affective Disorders 147, 212–216. [DOI] [PubMed] [Google Scholar]
- Cavanagh JT, Carson AJ, Sharpe M, Lawrie SM (2003). Psychological autopsy studies of suicide: a systematic review. Psychological Medicine 33, 395–405. [DOI] [PubMed] [Google Scholar]
- Corrigan PW, Watson AC (2002). The paradox of self-stigma and mental illness. Clinical Psychology: Science and Practice 9, 35–53. [Google Scholar]
- Corrigan PW, Kosyluk KA, Rüsch N (2013). Reducing self-stigma by coming out proud. American Journal of Public Health 103, 794–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farrelly S, Jeffery D, Rüsch N, Williams P, Thornicroft G, Clement S (2015). The link between mental health-related discrimination and suicidality: service user perspectives. Psychological Medicine 45, 2013–2022. [DOI] [PubMed] [Google Scholar]
- Gu F, Preacher KJ, Ferrer E (2015). A state space modeling approach to mediation analysis. Journal of Education and Behavioral Statistics 39, 117–143. [Google Scholar]
- Hancock GR, Mueller RO (2013). Structural Equation Modeling: A Second Course. Iap: Greenwich. [Google Scholar]
- Hardt J, Egle UT, Kappis B, Hessel A, Brähler E (2004). Die symptom-checkliste SCL-27. Ergebnisse einer deutschen Repräsentativbefragung [Symptom Checklist SCL-27. Results of a Representative German Survey]. Psychotherapie, Psychosomatik, Medizinische Psychologie 54, 214–223. [DOI] [PubMed] [Google Scholar]
- Harris EC, Barraclough B (1997). Suicide as an outcome for mental disorders. A meta-analysis. British Journal of Psychiatry 170, 205–228. [DOI] [PubMed] [Google Scholar]
- Hosmer DW Jr., Lemeshow S, Sturdivant RX (2013). Applied Logistic Regression, Vol. 398. John Wiley & Sons: Hoboken. [Google Scholar]
- Link BG, Phelan JC (2013). Labeling and stigma In Handbook of the Sociology of Mental Health (ed. Aneshensel CS, Phelan JC and Bierman A), pp. 525–541. Springer: Dordrecht. [Google Scholar]
- Link BG, Cullen FT, Struening E, Shrout PE, Dohrenwend BP (1989). A modified labeling theory approach to mental disorders: an empirical assessment. American Sociological Review 54, 400–423. [Google Scholar]
- Link BG, Mirotznik J, Cullen FT (1991). The effectiveness of stigma coping orientations: can negative consequences of mental illness labeling be avoided? Journal of Health and Social Behavior 32, 302–320. [PubMed] [Google Scholar]
- Link BG, Struening EL, Neese-Todd S, Asmussen S, Phelan JC (2002). On describing and seeking to change the experience of stigma. Psychiatric Rehabilitation Skills 6, 201–231. [Google Scholar]
- Miret M, Ayuso-Mateos JL, Sanchez-Moreno J, Vieta E (2013). Depressive disorders and suicide: epidemiology, risk factors, and burden. Neuroscience and Biobehavioral Reviews 37, 2372–2374. [DOI] [PubMed] [Google Scholar]
- Niederkrotenthaler T, Reidenberg DJ, Till B, Gould MS (2014). Increasing help-seeking and referrals for individuals at risk for suicide by decreasing stigma: the role of mass media. American Journal of Preventive Medicine 47, 235–243. [DOI] [PubMed] [Google Scholar]
- Pachankis JE (2007). The psychological implications of concealing a stigma: a cognitive-affective-behavioral model. Psychological Bulletin 133, 328–345. [DOI] [PubMed] [Google Scholar]
- Peduzzi P, Concato J, Kemper E, Holford TR, Feinstein AR (1996). A simulation study of the number of events per variable in logistic regression analysis. Journal of Clinical Epidemiology 49, 1373–1379. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF (2008). Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods 40, 879–891. [DOI] [PubMed] [Google Scholar]
- Reynders A, Kerkhof AJFM, Molenberghs G, Van Audenhove C (2014). Attitudes and stigma in relation to help-seeking intentions for psychological problems in low and high suicide rate regions. Social Psychiatry and Psychiatric Epidemiology 49, 231–239. [DOI] [PubMed] [Google Scholar]
- Rüsch N, Angermeyer MC, Corrigan PW (2005). Mental illness stigma: concepts, consequences, and initiatives to reduce stigma. European Psychiatry 20, 529–539. [DOI] [PubMed] [Google Scholar]
- Rüsch N, Lieb K, Bohus M, Corrigan PW (2006). Self-stigma, empowerment, and perceived legitimacy of discrimination among women with mental illness. Psychiatric Services 57, 399–402. [DOI] [PubMed] [Google Scholar]
- Rüsch N, Zlati A, Black G, Thornicroft G (2014). Does the stigma of mental illness contribute to suicidality? British Journal of Psychiatry 205, 257–259. [DOI] [PubMed] [Google Scholar]
- Schomerus G, Evans-Lacko S, Rüsch N, Mojtabai R, Angermeyer MC, Thornicroft G (2015). Collective levels of stigma and national suicide rates in 25 European countries. Epidemiology and Psychiatric Sciences 24, 166–171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Selby E, Joiner TE, Ribeiro JD (2014). Comprehensive theories of suicidal behaviors In The Oxford Handbook of Suicide and Self-Injury (ed. Nock MK), pp. 286–308. Oxford University Press: Oxford, UK. [Google Scholar]
- Sharaf AY, Ossman LH, Lachine OA (2012). A cross-sectional study of the relationships between illness insight, internalized stigma, and suicide risk in individuals with schizophrenia. International Journal of Nursing Studies 49, 1512–1520. [DOI] [PubMed] [Google Scholar]
- Steinmetz H (2014). Lineare Strukturgleichungsmodelle – Eine Einführung mit R, Vol. 9 Sozialwissenschaftfliche Forschungsmethoden. Rainer Hampp Verlag: Mering. [Google Scholar]
- Sudak H, Maxim K, Carpenter M (2008). Suicide and stigma: a review of the literature and personal reflections. Academic Psychiatry 32, 136–142. [DOI] [PubMed] [Google Scholar]
- Taylor AB, MacKinnon DP, Tein J-Y (2008). Tests of the three-path mediated effect. Organizational Research Methods 11, 241–269. [Google Scholar]
- Vittinghoff E, McCulloch CE (2007). Relaxing the rule of ten events per variable in logistic and Cox regression. American Journal of Epidemiology 165, 710–718. [DOI] [PubMed] [Google Scholar]
- World Health Organization (2014). Preventing suicide: a global imperative. Retrieved 4 May 2015 from http://www.who.int/mental_health/suicide-prevention/world_report_2014/en/