Abstract
Aims.
In low-income countries, care for people with severe mental disorders (SMDs) who manage to access treatment is usually emergency-based, intermittent or narrowly biomedical. The aim of this study was to inform development of a scalable district-level mental health care plan to meet the long-term care needs of people with SMD in rural Ethiopia.
Methods.
The present study was carried out as formative work for the Programme for Improving Mental health CarE which seeks to develop, implement and evaluate a district level model of integrating mental health care into primary care. Six focus group discussions and 25 in-depth interviews were conducted with service planners, primary care providers, traditional and religious healers, mental health service users, caregivers and community representatives. Framework analysis was used, with findings mapped onto the domains of the Innovative Care for Chronic Conditions (ICCC) framework.
Results.
Three main themes were identified. (1) Focused on ‘Restoring the person's life’, including the need for interventions to address basic needs for food, shelter and livelihoods, as well as spiritual recovery and reintegration into society. All respondents considered this to be important, but service users gave particular emphasis to this aspect of care. (2) Engaging with families, addressed the essential role of families, their need for practical and emotional support, and the importance of equipping families to provide a therapeutic environment. (3) Delivering collaborative, long-term care, focused on enhancing accessibility to biomedical mental health care, utilising community-based health workers and volunteers as an untapped resource to support adherence and engagement with services, learning from experience of service models for chronic communicable diseases (HIV and tuberculosis) and integrating the role of traditional and religious healers alongside biomedical care. Biomedical approaches were more strongly endorsed by health workers, with traditional healers, religious leaders and service users more inclined to see medication as but one component of care. The salience of poverty to service planning was cross-cutting.
Conclusions.
Stakeholders prioritised interventions to meet basic needs for survival and endorsed a multi-faceted approach to promoting recovery from SMD, including social recovery. However, sole reliance on this over-stretched community to mobilise the necessary resources may not be feasible. An adapted form of the ICCC framework appeared highly applicable to planning an acceptable, feasible and sustainable model of care.
Key words: Chronic care model, community-based rehabilitation, mental disorders, primary health care, recovery, schizophrenia, social inclusion, sub-Saharan Africa
Introduction
The treatment gap for severe mental disorders (SMDs), comprising psychotic disorders (e.g. schizophrenia) and bipolar disorder, is substantial in low- and middle-income countries (LMICs). In Ethiopia, it is estimated that around 90% of people with SMD never receive effective treatment (Kebede et al. 2004). Furthermore, the care received by the minority who do access treatment is mostly emergency-based, intermittent and narrowly biomedical. The consequences of inadequate care for people with SMDs in LMICs are substantial, including prolonged mental ill-health for the affected individual, premature mortality (Teferra et al. 2011), undernutrition (Lijalem et al. 2003), loss of productivity and functional impairment (Kebede et al. 2006; Mogga et al. 2006), economic and caregiver burden (Shibre et al. 2003; Zergaw et al. 2008), stigma, discrimination and abuse (Shibre et al. 2001).
Compelling arguments have been made for making care for people with SMDs an essential component of emerging initiatives to achieve universal health care in LMICs (Patel, 2015). The World Health Organization (WHO) launched the mental health gap action programme (mhGAP) to improve access to care by integrating mental health into primary care services (World Health Organization, 2008). The mhGAP Intervention Guide provides evidence-based, packages of care for prioritised mental, neurological and substance use disorders (Barbui et al. 2010, World Health Organization, 2010). However, at present, mhGAP does not address the issue of how these packages of mental health care can be delivered to people with SMDs who have ongoing needs for care. Furthermore, mhGAP has limited focus on how to achieve social and functional recovery in addition to clinical improvement. A systematic review of evaluations of community-based mental health care in sub-Saharan Africa revealed the paucity of data available to inform service development and implementation of care for people with SMDs in LMICs (Hanlon et al. 2010).
For long-term health conditions more generally, a ‘chronic care model’ of service delivery has been associated with improved outcomes (Wagner et al. 1996). This model has been adapted for LMICs in the Innovative Care for Chronic Conditions (ICCC) framework (Epping-Jordan et al. 2004). The ICCC framework incorporates the health system elements that support patient-centred care at micro, meso and macro levels (see Table 1). Recent interest in the integration of mental health care into existing chronic care models in LMICs (e.g. for HIV/AIDS or tuberculosis (TB)) has focused on depression and alcohol use disorders due to the high levels of co-morbidity and evidence for the effectiveness of task shared care (Patel et al. 2013). However, this strategy may not meet the needs of people with SMDs in LMICs. Integrated models for people with SMDs in high-income countries (HICs) have included resource-intensive specialist multidisciplinary teams which are unlikely to be feasible in LMICs (Lehtinen & Taipale, 2001). Contextual differences between HICs and LMICs, for example in terms of community poverty levels, literacy and social connectedness, need also to be considered. To the best of our knowledge, the ICCC framework has not been applied previously or evaluated with respect to the care of persons with SMDs in LMICs.
Table 1.
Components of the ICCC framework
| Level | Explanation |
|---|---|
| Meso | At this level, the framework advocates for:
|
| Micro | This level emphasises equipping health facilities to provide continuity of care including:
|
| Macro | This level considers the contribution of a ‘positive policy environment’, including:
|
The Programme for Improving Mental Health Care (PRIME) (Lund et al. 2012) aims to produce high-quality evidence about how to implement mental health care within primary and maternal health care services in five LMICs (Ethiopia, India, Nepal, South Africa and Uganda). In this paper, we present data from formative work from the PRIME study in rural Ethiopia. Our objectives were to: (i) identify the key components of a model of long-term mental health care integrated into primary care for people with SMD in this setting and (ii) explore the acceptability, feasibility and sustainability of potential strategies to achieve long-term care with the goal of achieving recovery and social reintegration.
Methods
Study design
A qualitative study employing individual in-depth interviews (IDIs) and focus group discussions (FGDs) (Lambert & Loiselle, 2008).
Study setting
The study was carried out in Sodo District of the Gurage Zone, in the Southern Nations, Nationalities and Peoples Region of Ethiopia, located around 100 km south of the capital city, Addis Ababa. Sodo has a population of about 160 000 adults (Central Statistical Authority (CSA), 2008). The area is predominantly rural. The majority of people engage in subsistence farming.
At the time of the study, there were no mental health services within Sodo District. The nearest mental health service was a psychiatric nurse-led out-patient unit located in the General hospital in the neighbouring district of Butajira, between 30 and 50 km away. The nearest in-patient psychiatric care is available in Addis Ababa. In Sodo District, there are eight health centres delivering primary health care, mostly staffed by nurses and health officers. There are no medical doctors or hospital facilities. Linked to each health centre are paid, community-based, health extension workers (HEWs), who form the primary health care interface with the community. HEWs are all women, high school completers who are recruited from the local area and have received one year of training in health promotion and illness prevention. Most HEWs have little or no training in community-based mental health care. There is also a community network of health volunteers mobilised for health education (Donnelley, 2011).
Population and sample
A sample of key stakeholders was selected purposively, covering each of the planned levels of the PRIME mental health care intervention; health service organisation (n = 4 IDIs from the District Health Office and Federal Ministry of Health), health facility (three FGDs with PHC frontline workers and supervisors of HEWs) and community (one FGD with HEWs, one FGD with health volunteers, one FGD with families of persons with mental and developmental disorders, and IDIs with family members (n = 3) and mental health service users (n = 8), traditional and religious leaders (n = 5), community leaders (n = 3) and representatives from non-governmental organisations active in the area (n = 2). Characteristics of the participants are summarised in Table 2. FGDs were used whenever it was feasible to convene a relatively homogeneous group of respondents (e.g. primary care workers, health volunteers, family members) in order to elicit additional information about the manner in which the respondents spoke about the topic in front of one another as well as their perspectives on the topic. IDIs were used when the informants were more heterogeneous or difficult to access or, in the case of mental health service users, to avoid the potential stress of a group discussion.
Table 2.
Sociodemographic characteristics of participants
| Gender | |||||
|---|---|---|---|---|---|
| Data collection modality | Participant type | Male | Female | Age (years) | Other characteristics |
| FGD 1 | Primary Healthcare (PHC) workers | 4 | 3 | 26–39 | Nursing diploma, degree, health officer Years of experience, 1–7 |
| FGD 2 | PHC workers | 2 | 4 | 25–40 | Nursing diploma, degree, health officers Years of experience, 3–20 |
| FGD 3 | Health extension workers | 0 | 7 | 21–26 | 1 year HEW training Years of experience, 2–3 |
| FGD 4 | PHC worker supervisors | 5 | 0 | 27–39 | Nursing diploma, degree, health officers Years of experience, 2–7 |
| FGD 5 | Health volunteers | 7 | 2 | 25–38 | 5th grade, up to diploma |
| FGD 6 | Caregivers of persons with mental disorder | 2 | 8 | – | Family member with psychosis (n = 1), epilepsy (n = 4) and intellectual disability (n = 2) |
| IDIs | Traditional and religious healers | 4 | 0 | 29–52 | All literate, up to diploma |
| Community leaders | 4 | 0 | 53–70 | 4–8th grades | |
| Non-governmental organisation representatives | 2 | 0 | 32, 33 | Both degree levels | |
| Service planners and co-ordinators | 4 | 0 | – | Degree, masters, post-graduate psychiatry qualifications | |
| Service users | 4 | 5 | 25–45 | Four people who were non-literate, three able to read and write, 1 8th grade, one diploma | |
| Caregivers | 2 | 1 | 50–60 | Two people who were non-literate, one able to read and write | |
Research process
All IDIs and FGDs were conducted in Amharic, the official language of Ethiopia, by three experienced Masters’ level research assistants. The FGDs were conducted in primary health care facilities. The IDIs were carried out in a neutral central location in Sodo District, in people's homes and in the offices of policy-makers and planners who were based in the capital city, Addis Ababa. At all times privacy was ensured. Apart from service planners, all participants received remuneration for transport costs and FGD participants also received refreshments. The FGDs followed recommended methodology (Krueger & Casey, 2009). For the FGDs, a note-taker was present in addition to the facilitator, in order to observe and document non-verbal communication.
Interview guide
The IDI and FGD topic guides were developed collaboratively across the PRIME research programme consortium and tailored to the different categories of respondent and country context. The topic guide drew on our review of the literature and focused on aspects of intervention provided by the health care system (‘biomedical intervention’), especially adherence to medication, engagement in care (outreach), case management (continuity of care), as well non-health sector aspects, in particular rehabilitation, social inclusion and reintegration (countering stigma, discrimination and abuse). The topic guide explored aspects of delivery of integrated mental health care in relation to psychosis (the focus of this paper) and other disorders. Where needed, a standardised vignette for psychosis was used to orientate respondents (Wig et al. 1980; Alem et al. 1999).
Data analysis
IDIs and FGDs were audiotaped, transcribed in Amharic and then translated into English by the interviewers prior to coding. Any ambiguities or points of interest were discussed and noted within the transcripts. Analysis was carried out concurrently with data collection. Each research assistant kept field notes. After each set of data collection, C.H. discussed with the research assistants about emerging themes and unexpected findings, to inform iterative development of the topic guides and theoretical sampling. A framework analysis approach was utilised (Smith & Firth, 2011) which involved independent coding of text by S.M. and C.H. and verification meetings with the interviewers. Qualitative software was used for data management (ATLAS.ti. Version 5.0, 2003; NVivo qualitative data analysis software. Version 9, 2010).
Ethical considerations
The study was approved by the Institutional Review Board of the College of Health Sciences, Addis Ababa University and the University of Cape Town Human Research Ethics Committee. After being informed fully about the study, respondents gave voluntary consent.
Findings
The findings are structured under the following themes, which reflected the most salient domains of long-term care for people with SMD: (1) ‘restoring the person's life’; (2) engagement with families; and (3) delivering long-term, collaborative mental health care. Cutting across these themes was the salience of poverty. For full quotations grouped by theme refer to Supplementary file 1.
‘Restoring the person's life’
Respondents spoke of the complexity of the process of rehabilitation, recovery and reintegration for people with SMDs. The required interventions were considered to be those targeting basic needs for food, shelter and livelihoods support of people with SMD, overcoming social exclusion and attending to spiritual recovery. Community respondents expressed willingness to respond to the needs of those with SMDs akin to similar community mobilisation for people living with HIV/AIDS: provision of shelter and food. A local health service planner spoke positively of the community's willingness to help by providing food and economic support:
… The process of restoring the person's life will be a time taking process as this is a person who has lost many things in the course of his illness. … Our community is very cooperative. … We have ample experience with HIV where people provide each other with support.
IDI 6, Local health service planner
The need for tangible support to meet basic needs was reported across all categories of respondents, but emphasised particularly by service users and family members. Poverty alleviation was considered to be critical to the success of any intervention to help people with SMD, in terms of accessing care, being able to take medication continuously, making a full recovery and protecting against relapse in the future.
… A person may recover from his illness; but deprivation could cause him to go back to being ‘crazy’. … What is expected of us is to help create jobs for these people…. Until something is done for these people they are in danger of relapsing.
FGD 6, Health volunteers
However, recovery was considered to be about more than meeting basic needs for survival. Many respondents spoke of the need to provide moral support and encouragement, as well as attending to the person's spiritual recovery.
In helping that person to get back on track we need to provide him with a wide array of support through prayer; counselling; money and many other ways.
IDI 10, Religious leader
Some community leaders were uncomfortable with the idea of including people with SMD in positions of authority, even post-recovery. People with SMDs spoke of how such stigmatising attitudes impeded their recovery.
I have a strong interest to start working but no one understands and trusts me because I am mentally ill.
ID19, Person with SMD
However, the potential role of community members in promoting the social inclusion of those recovering from SMD was mentioned by the health volunteers and HEWs. In both instances, public contact with persons with SMDs was advocated in order to prevent discrimination.
We can establish relationships with these people; spend time with them; take them out for some tea and coffee. If we spend some time with them, we can help them make small improvements. They generally tend to feel alienated and that they are outcasts.
FGD 6, Health volunteers
HEWs expressed willingness to involve people with SMDs in the local community. Religious leaders also perceived that they had a role in overcoming negative stereotypes of people with SMD.
Currently, there is no message transmitted from the religious leaders. As a result, the community is careless towards the needs of these people. They think that the person is crazy and there is no hope afterwards. …The person's full life journey may be considered as ruined.
IV05 Religious leader
There was some evidence of social desirability affecting responses in the HEW and community health volunteer groups, as well as at the healthcare administration level, with respondents speaking positively about the community's capacity to mobilise and support vulnerable people. However, despite the enthusiastic response of these respondents, other respondents highlighted the lack of community activity to date for people with conspicuous mental illness and doubted the capacity of the community to be able to respond materially on an ongoing basis to the challenge of caring for those with long-term SMD. They explained that the successes associated with rehabilitation for those with HIV were only possible because of additional external resources. People with long-term SMDs and their caregivers spoke from their own experience.
The … problem is that it is a long-term illness. People will get tired of you if you are ill for [a] longer [period of time]… .
ID 16 Person with SMD
Engaging with families
Family members described their desperate efforts to seek effective help and ongoing care and support for their affected relatives. Many family members described crossing between two systems of healing, traditional healing and the health system, incurring substantial costs along the way. The emotional burden on family members and the need for support beyond the prescription of medication was also articulated by respondents.
It's been a year since the younger one got sick. He sleeps all day; …. I have taken him to a holy water site [Ethiopian Orthodox Church]. Recently I have become tired and I have given up altogether.
FGD 5, Family members
Religious institutions appeared to provide most of the limited support available for people with SMDs who did not have family, although community groups sometimes helped with acute crises.
Equipping families to better meet the needs of their mentally ill relatives was emphasised, particularly by community level informants and less by the facility-based health workers. Families needed to be informed about the rationale for long-term medication and the importance of engagement with health services. Beyond this, one religious healer also described how he counselled families to behave in a more therapeutic manner:
R: Yes. I beg their parents not to chain them up. I plead to treat them in a caring manner with the help of God. I told her parents not to disappoint her because that might lead to relapse. There should not be arguing with her.
IV08, Holy water attendant
R: I think the family needs more treatment and encouragement than the patient. We explain to them that there is a cure for someone who is mentally ill. Illness is always there with human beings. We tell them not to lose hope. If they help the person receive psychological treatment, if the person takes his medication properly, if he receives good care, if the person keeps time in taking his medication, that person would be important member of the family and good citizen. Therefore, we tell them this.
I: So you educate the family?
R: Yes. We tell them to be patient.
IV07 Religious healer
Delivering collaborative, long-term mental health care
The need for biomedical intervention, particularly long-term medication, for SMDs was endorsed by most participants although there were discordant views amongst some mental health service users. The proposal to integrate mental health care into primary care was welcomed as important for improving access to affordable care. However, there was recognition of the limitations of medication and facility-based care, and the need for long-term residential mental health care for people with complex and refractory illness was mentioned. Religious healers and other community-based stakeholders, including people with SMD, gave greater emphasis to medication being just one component of care rather than sufficient in itself. Traditional and religious healers were considered by many respondents to have an important ongoing role alongside biomedical care, targeting the presumed root cause of the disorder (spirit possession) and allowing for potential cure.
There are cases which can be cured by traditional and faith based healers … so for us spending time in hospital is a waste. … On the other hand there are people who can be cured by modern treatment … so it would be good if both were working together.
ID23 Person with SMD
Many family members reported, however, that despite multiple trips to holy water sites and high levels of expenditure, they saw little benefit of the holy water. Health professionals and family members tended to focus more on medication. Health professionals in particular framed the potential role of traditional and religious healers in terms of improving engagement with facility-based care and adherence to medication.
A reliable medication supply, incentivising primary health care workers, systems to enable tracking of people who default from treatment and dedicated clinics for mental disorders, akin to those used in HIV and TB care, were advocated by health care provider respondents. These providers were familiar with the challenges of providing long-term care and advocated utilising strategies that had been successful for HIV and TB care to promote medication adherence, including attending the health facility to take medication (‘Directly Observed Therapy’) and a ‘Guarantor’ model where a person takes responsibility for guaranteeing that the patient would receive the medication as prescribed. Respondents spoke of the benefits of using the new network of HEWs and the health volunteers as the mechanism for co-ordinating outreach from the health facility and long-term engagement in care.
Intervening with food or financial and psychosocial support was recommended for those persons whose adherence to medication and engagement in care might be jeopardised by extreme poverty, again drawing on the model of care employed for HIV treatment.
Discussion
In this paper, we present findings from formative work to develop a service model of long-term mental health care for people with SMDs integrated into primary care in a rural African setting. A broad range of stakeholders participated and emphasised the need for care that extended beyond the provision of medicine to also address basic needs for survival and to support social and spiritual restoration of people with SMD. The crucial role of the family and the need for accessible integrated and collaborative care were also important themes. Some religious healers and people with SMDs gave less emphasis to biomedical care. An adapted version of the ICCC framework appeared highly appropriate for structuring the approach to long-term care for people with SMD.
Restoring the person's life
Participants prioritised interventions to meet the basic survival needs of people with SMD. This resonates with a previous qualitative study from rural Ethiopia in which people with SMDs and their caregivers spoke of the difficulties adhering to psychotropic medication and attending follow-up appointments due to food insufficiency and poverty (Teferra et al. 2013). The bidirectional relationship between mental disorders and poverty is well established (Lund et al. 2011), and particularly salient in LMIC settings, where people with SMDs and their families are often among the poorest in society (Lund et al. 2011).
In this study, the community expressed willingness to provide support for basic needs of people with SMD, and so community mobilisation for instrumental support will form part of the planned intervention. However, the sustainability of this approach was questioned. Caregivers expressed doubts about the reliability and capacity of the community response. During scale up of access to antiretroviral therapy in persons living with HIV/AIDS, the need for externally funded food supplementation and poverty alleviation strategies was recognised and included in many programmes (Au et al. 2006, Hardon et al. 2007). The potential need for such external support to ensure successful implementation of integrated mental health care will be investigated as part of the PRIME case study (De Silva et al. 2015).
The need for rehabilitation, including opportunities for skill (re)acquisition, was recognised by respondents in the study. Raising awareness within families and the wider community about the importance of supporting people with SMDs to resume previous activities and play their part within the community was seen as an essential first step. However, our findings indicated that the community level of the ICCC framework required expansion to include livelihoods initiatives and access to paying work. This was a particularly high priority for people with SMD.
The community-based health workers and volunteers were quick to emphasise their potential role in reducing stigma by socialising with people with SMDs and including them in the community work, thus helping to restore their status. The potency of ‘direct contact’ interventions in reducing stigma has been shown in other settings (Thornicroft, 2006) and will be promoted in the PRIME intervention for SMD.
‘Engagement with families’
In relation to recovery and reintegration of people with SMD, family members were regarded as an important resource. Several respondents conceptualised the unit of intervention to be the family and not the individual with SMD, recognising their vital role in bringing a person with SMD to care and providing them with ongoing support (Thara et al. 2008). Ensuring that the family, as well as the person with SMD, is given adequate information about the nature of the condition and its treatment accords well with the ICCC framework, which broadens the notion of patient-centred care to involve other key actors.
The high level of emotional and financial burden experienced by family caregivers of people with SMD has been demonstrated previously in a rural Ethiopian setting (Shibre et al. 2003). Providing locally accessible mental health care may by itself reduce the burden substantially (Shibre et al. 2012). However, community-based self-help groups for service users and caregivers in Ghana were found to provide important benefits to caregivers in terms of both practical and emotional support (Cohen et al. 2012) and may be a feasible and useful intervention for the Ethiopia setting. Attending to the mental health of family caregivers is likely to benefit care for people with SMD, again linking with the ICCC framework approach that recognises the interconnectedness of patient and family health.
Religious healers spoke of a potential role in advising the family on how to interact with their family member with SMD; for example, to speak softly, not to argue with them, to treat them in a caring manner. In Western and some LMIC settings, familial ‘high expressed emotion’ towards a person with SMD, characterised by hostility, critical comments and emotional overinvolvement, is associated with poorer clinical outcomes (Brown et al. 1972; Leff et al. 1987). Furthermore, structured family interventions tackling these patterns of interaction reduce the risk of relapse of psychotic disorders (Pfammatter et al. 2006). Family intervention may, therefore, be a fruitful area of collaboration between the public health system and traditional and religious healers in Ethiopia. Such a community level approach to improving patient outcomes is at the heart of the ICCC framework.
Delivering long-term, collaborative mental health care
Several lessons for the delivery of long-term care for SMD were drawn from existing service models for HIV/AIDS and TB and again accord well with the ICCC framework for interventions at health organisation and community levels. Health service and system innovations used for the care of people with HIV/AIDS and TB, such as task-sharing care in primary are, maintenance of a case register to track people defaulting from care, liaison with community health workers to provide community outreach and medication adherence support over extended periods of time, were all assumed to be applicable to the delivery of mental health care. Similarly for the community-level focus on awareness-raising to reduce stigma and community mobilisation to provide support.
The recommendations for adherence support drew largely on interventions used for TB, including the Directly Observed Therapy model. This approach has been applied successfully to the care of people with SMDs in India (Farooq et al. 2011), although qualitative evaluation from another study revealed that families sometimes felt overburdened when asked to support adherence preferring involvement of non-relatives (Mall et al. 2013). This approach aligns well with the ICCC framework emphasis on community level intervention running alongside patient level care.
Service users in particular favoured involvement of traditional and religious healers. Our previous strengths-based approach to mapping community resources in the PRIME implementation district underlined the strong presence of traditional and religious healers (Selamu et al. 2015). However, this previous work also indicated that restrictive practices, such as chaining people with SMD, are widespread in such healing sites. The evidence base for collaborative care with traditional and religious healers is limited (Gureje et al. 2015). Efforts will be directed at finding a workable model of collaboration which enhances the outcomes of people with SMD.
With care of people with SMD, an additional factor to be considered is the particular vulnerability of those people whose mental state impairs their decision-making capacity with regard to treatment. In our study, some people with SMD spoke of both the benefits and harms of being treated against their will, but the issue of non-consenting patients was notably absent from the discourse of other stakeholders. In ICCC framework terms, legislative changes to protect people with SMDs who are not consenting to treatment would need to be addressed in order to provide an enabling policy and service environment for mental health care.
Informing a model of long-term mental health care for people with SMDs
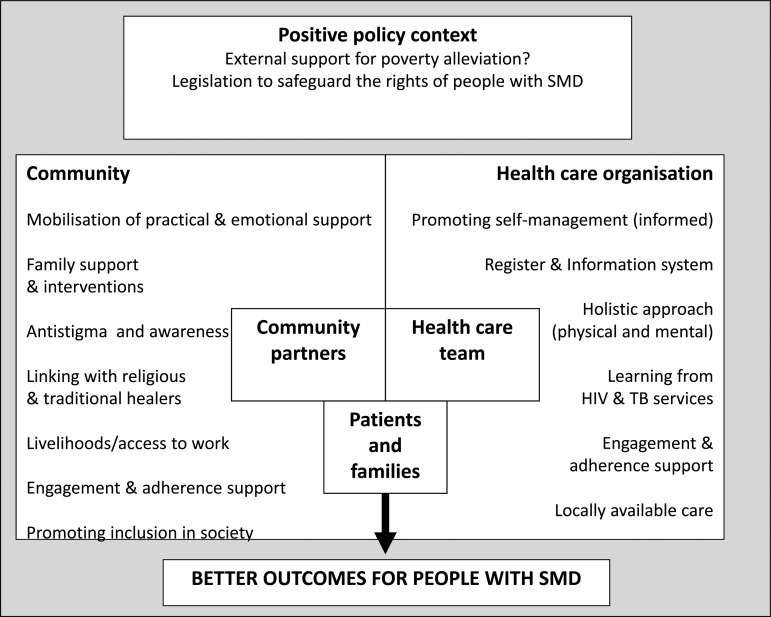
The study findings led to development of a proposed model of care for people with SMD in rural Ethiopia adapted from the ICCC framework (see Fig. 1). In keeping with the ICCC framework, the ‘micro’ level interventions emphasise the patient/family–community-health facility triad in relation to poverty alleviation, adherence support, long-term access to care, rehabilitation, reintegration and traditional/religious healing. Similarly, for the ‘meso’ level, health care organisational changes are intimately linked to community participation, for example, in facilitating adherence, engagement and improved self-management and health promotion. The ‘macro’ level was not a focus of this study, but a potential need for external resources to support poverty alleviation was clearly articulated by respondents.
Fig. 1.
An adapted ICCC framework (Epping-Jordan et al. 2004) for planning long-term care of people with severe mental disorders in rural Ethiopia.
Limitations
The study findings may not be generalisable to other settings, although are likely to be applicable to rural Ethiopian contexts.
Conclusions
In this formative study to develop a sustainable and feasible model of long-term care for people with SMD in rural Ethiopia, an adapted form of the ICCC framework appears to capture the multi-faceted and interconnected interventions needed for successful outcomes. The acceptability, feasibility and effectiveness will be evaluated as part of PRIME (De Silva et al. 2015).
Acknowledgements
The authors acknowledge gratefully the participants in the study for their valuable contributions.
Financial support
The work was supported by UK Aid from the UK Government as part of the PRIME Research Programme Consortium; however, the views expressed do not necessarily reflect the UK Government's official policies. The funders had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript.
Conflict of interest
None.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
Supplementary material
For supplementary material accompanying this paper visit http://dx.doi.org/10.1017/S2045796015001006.
click here to view supplementary material
References
- Alem A, Jacobsson L, Araya M, Kebede D, Kullgren G (1999). How are mental disorders seen and where is help sought in a rural Ethiopian community? A key informant study in Butajira, Ethiopia. Acta Psychiatrica Scandinavica (Supplementum) 397, 40–47. [DOI] [PubMed] [Google Scholar]
- ATLAS.ti. Version 5.0 (2003). Scientific Software Development GmbH: Berlin. [Google Scholar]
- Au JT, Kayitenkore K, Shutes E, Karita E, Peters PJ, Tichacek A, Allen SA (2006). Access to adequate nutrition is a major potential obstacle to antiretroviral adherence among HIV-infected individuals in Rwanda. AIDS 20, 2116–2117. [DOI] [PubMed] [Google Scholar]
- Barbui C, Dua T, van Ommeren M, Yasamy MT, Fleischmann A, Clark N, Thornicroft G, Hill S, Saxena S (2010). Challenges in developing evidence-based recommendations using the GRADE approach: the case of mental, neurological, and substance use disorders. PLoS Medicine 7, e1000322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown GW, Birley JLT, Wing JK (1972). Influence of family life on the course of schizophrenic disorders: a replication. British Journal of Psychiatry 121, 241–258. [DOI] [PubMed] [Google Scholar]
- Central Statistical Authority (CSA) (2008). Summary and Statistical Report of the 2007 Population and Housing Census. Population Size by Age and Sex. Population Census Commission, Federal Democratic Republic of Ethiopia: Addis Ababa. [Google Scholar]
- Cohen A, Raja S, Underhill C, Yaro BP, Dokurugu AY, De Silva M, Patel V (2012). Sitting with others: mental health self-help groups in northern Ghana. International Journal of Mental Health Systems 6. doi: 10.1186/1752-4458-1186-1181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Silva M, Rathod S, Hanlon C, Breuer E, Chisholm D, Fekadu A, Jordans M, Peterson I, Prince M, Shidhaye R, Thornicroft G, Kigozi F, Tomlinson M, Lund C, Patel V (2015). Cross country methods to evaluate the coverage and effectiveness of district mental health care plans in 5 low and middle income countries. British Journal of Psychiatry (Supplement). DOI: 10.1192/bjp.bp.1114.153676. [DOI] [Google Scholar]
- Donnelley J (2011). Ethiopia gears up for more major health reforms. Lancet 377, 1907–1908. [DOI] [PubMed] [Google Scholar]
- Epping-Jordan JE, Pruitt SD, Bengoa R, Wagner EH (2004). Improving the quality of health care for chronic conditions. Quality and Safety in Health Care 13, 299–305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farooq S, Nazar Z, Irfan M, Akhter J, Gul E, Irfan U, Naeem F (2011). Schizophrenia medication adherence in a resource-poor setting: randomised controlled trial of supervised treatment in out-patients for schizophrenia (STOPS). British Journal of Psychiatry 199, 467–472. [DOI] [PubMed] [Google Scholar]
- Gureje O, Nortje G, Makanjuola V, Oladeji BD, Seedat S, Jenkins R (2015). The role of global traditional and complementary systems of medicine in the treatment of mental health disorders. Lancet Psychiatry 2, 168–177. [DOI] [PubMed] [Google Scholar]
- Hanlon C, Wondimagegn D, Alem A (2010). Lessons learned in developing community mental health care in Africa. World Psychiatry 9, 185–189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hardon AP, Akurut D, Comoro C, Ekezie C, Irunde HF, Gerrits T, Kglatwane J, Kinsman J, Kwasa R, Maridadi J, Moroka TM, Moyo S, Nakiyemba A, Nsimba S, Ogenyi R, Oyabba T, Temu F, Laing R (2007). Hunger, waiting time and transport costs: time to confront challenges to ART adherence in Africa. AIDS Care: Psychological and Socio-medical Aspects of AIDS/HIV 19, 658–665. [DOI] [PubMed] [Google Scholar]
- Kebede D, Alem A, Shibre T, Negash A, Deyassa N, Beyero T (2004). The sociodemographic correlates of schizophrenia in Butajira, rural Ethiopia. Schizophrenia Research 69, 133–141. [DOI] [PubMed] [Google Scholar]
- Kebede D, Alem A, Shibre T, Deyassa N, Negash A, Beyero T, Medhin G, Fekadu A (2006). Symptomatic and functional outcome of bipolar disorder in Butajira, Ethiopia. Journal of Affective Disorders 90, 239–249. [DOI] [PubMed] [Google Scholar]
- Krueger RA, Casey MA (2009). Focus Groups: A Practical Guide for Applied Research, 4th Edition SAGE Publications: Los Angeles. [Google Scholar]
- Lambert SD, Loiselle CG (2008). Combining individual interviews and focus groups to enhance data richness. Journal of Advanced Nursing 62, 228–237. [DOI] [PubMed] [Google Scholar]
- Leff J, Wig NN, Ghosh A, Bedi H, Menon K, Kuipers L, Korten A, Ernberg G, Day R, Sartorius N (1987). Influence of relatives’ expressed emotion on the course of schizophrenia in Chandigarh. British Journal of Psychiatry 151, 166–173. [DOI] [PubMed] [Google Scholar]
- Lehtinen V, Taipale V (2001). Integrating mental health services: the Finnish experience. International Journal of Integrated Care 1, 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lijalem M, Tesfaye F, Alem A, Kumie A, Kebede D (2003). Nutrition Status of Cases of Schizophrenia and Bipolar Disorders in Butajira, Rural Ethiopia. Addis Ababa University: Addis Ababa. [Google Scholar]
- Lund C, De Silva M, Plagerson S, Cooper S, Chisholm D, Das J, Knapp M, Patel V (2011). Poverty and mental disorders: breaking the cycle in low-income and middle-income countries. The Lancet. DOI: 10.1016/S0140-6736(1011)60754-X. [DOI] [PubMed] [Google Scholar]
- Lund C, Tomlinson T, De Silva M, Fekadu A, Shidhaye R, Jordans M, Petersen I, Bhana A, Kigozi F, Prince M, Thornicroft G, Hanlon C, Kakuma R, McDaid D, Saxena S, Chisholm D, Raja S, Kippen-Wood S, Honikman S, Fairall L, Patel V (2012). PRIME: A programme to reduce the treatment gap for mental disorders in five low- and middle-income countries. PLoS Medicine 9, e1001359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mall S, Sibeko G, Temmingh H, Stein D, Milligan P, Lund C (2013). Using a treatment partner and text messaging to improve adherence to psychotropic medication: a qualitative formative study of service users and caregivers in Cape Town, South Africa. African Journal of Psychiatry 16, 364–370. [DOI] [PubMed] [Google Scholar]
- Mogga S, Prince M, Alem A, Kebede D, Stewart R, Glozier N, Hotopf M (2006). Outcome of major depression in Ethiopia: population-based study. British Journal of Psychiatry 189, 241–246. [DOI] [PubMed] [Google Scholar]
- NVivo qualitative data analysis software. Version 9 (2010). QSR International Pty Ltd.
- Patel V (2015). Universal health care for schizophrenia: a global mental health priority (Editorial). Schizophrenia Bulletin. doi: 10.1093/schbul/sbv1107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel V, Belkin GS, Chockalingam A, Cooper J, Saxena S, Unützer J (2013). Grand challenges: integrating mental health services into priority health care platforms. PLoS Medicine 10, e1001448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfammatter M, Junghan UM, Brenner HD (2006). Efficacy of psychological therapy in schizophrenia: conclusions from meta-analyses. Schizophrenia Bulletin 32, S64–S80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Selamu M, Asher L, Hanlon C, Medhin G, Hailemariam M, Patel V, Thornicroft G, Fekadu A (2015). Beyond the biomedical: community resources for mental health care in rural Ethiopia the role of resource mapping in developing a mental health care plan in a low-income setting. PLoS ONE 10(15), e0126666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shibre T, Negash A, Kullgren G, Kebede D, Alem A, Fekadu A, Fekadu D, Medhin G, Jacobsson L (2001). Perception of stigma among family members of individuals with schizophrenia and major affective disorders in rural Ethiopia. Social Psychiatry and Psychiatric Epidemiology 36, 299–303. [DOI] [PubMed] [Google Scholar]
- Shibre T, Kebede D, Alem A, Negash A, Deyassa N, Fekadu A, Fekadu D, Jacobsson L, Kullgren G (2003). Schizophrenia: illness impact on family members in a traditional society – rural Ethiopia. Social Psychiatry and Psychiatric Epidemiology 38, 27–34. [DOI] [PubMed] [Google Scholar]
- Shibre T, Medhin G, Teferra S, Wakwoya A, Berhanu E, Abdulahi A, Alem A, Fekadu A (2012). Predictors of carer burden in schizophrenia: a five year follow-up study in Butajira, Ethiopia. Ethiopian Medical Journal 50, 125–133. [PubMed] [Google Scholar]
- Smith J, Firth J (2011). Qualitative data analysis: the framework approach. Nurse Researcher 18, 52–62. [DOI] [PubMed] [Google Scholar]
- Teferra S, Shibre T, Fekadu A, Medhin G, Wakwoya A, Alem A, Kullgren G, Jacobsson L (2011). Five-year mortality in a cohort of people with schizophrenia in Ethiopia. BMC Psychiatry 11, doi: 10.1186/1471-1244X-1111-1165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teferra S, Hanlon C, Beyero T, Jacobsson L, Shibre T (2013). Perspectives on reasons for non-adherence to medication in persons with schizophrenia in Ethiopia: a qualitative study of patients, caregivers and health workers. BMC Psychiatry 13, 168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thara R, Padmavati R, Aynkran JR, John S (2008). Community mental health in India: a rethink. International Journal of Mental Health Systems 2. doi: 10.1186/1752-4458-1182-1111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thornicroft G (2006). Shunned: Discrimination Against People with Mental Illness. Oxford University press: Oxford. [Google Scholar]
- Wagner EH, Austin BT, Von Korff M (1996). Organizing care for patients with chronic illness. Milbank Quarterly 74, 511–544. [PubMed] [Google Scholar]
- Wig NN, Suleiman MA, Routledge R, Srinivasa Murthy R, Ladrido-Ignacio L, Ibrahim HHA, Harding TW (1980). Community reactions to mental illness. A key informant study in three developing countries. Acta Psychiatrica Scandinavica 61, 111–126. [DOI] [PubMed] [Google Scholar]
- World Health Organization (2008). Mental Health Gap Action Programme (mhGAP): Scaling up Care for Mental, Neurological, and Substance use Disorders. WHO: Geneva. [PubMed] [Google Scholar]
- World Health Organization (2010). Mental Health Gap Action Programme Intervention Guide (mhGAP-IG) for Mental, Neurological and Substance use Disorders in Non-Specialized Health Settings. WHO: Geneva. [PubMed] [Google Scholar]
- Zergaw A, Hailemariam D, Alem A, Kebede D (2008). A longitudinal comparative analysis of economic and family caregiver burden due to bipolar disorder. African Journal of Psychiatry 11, 191–198. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
For supplementary material accompanying this paper visit http://dx.doi.org/10.1017/S2045796015001006.
click here to view supplementary material