Abstract
Aims.
Previous cross-sectional studies revealed inconsistent results regarding mental health treatment preferences among the general population. In particular, it is unclear to what extent specific age groups approve psychotherapy or psychotropic medication for the treatment of mental disorders. We explore whether treatment recommendations of either psychotherapy or psychiatric medication change over the lifespan which includes age-related effects due to increasing age of a person, cohort effects that reflect specific opinions during the time a person was born and period effects that reflect societal changes.
Methods.
Using data from three identical population surveys in Germany from 1990, 2001 and 2011 (combined n = 9046), we performed age-period-cohort analyses to determine the pure age, birth cohort and time period effects associated with the specific treatment recommendations for a person with either depression or schizophrenia, using logistic Partial Least-Squares regression models.
Results.
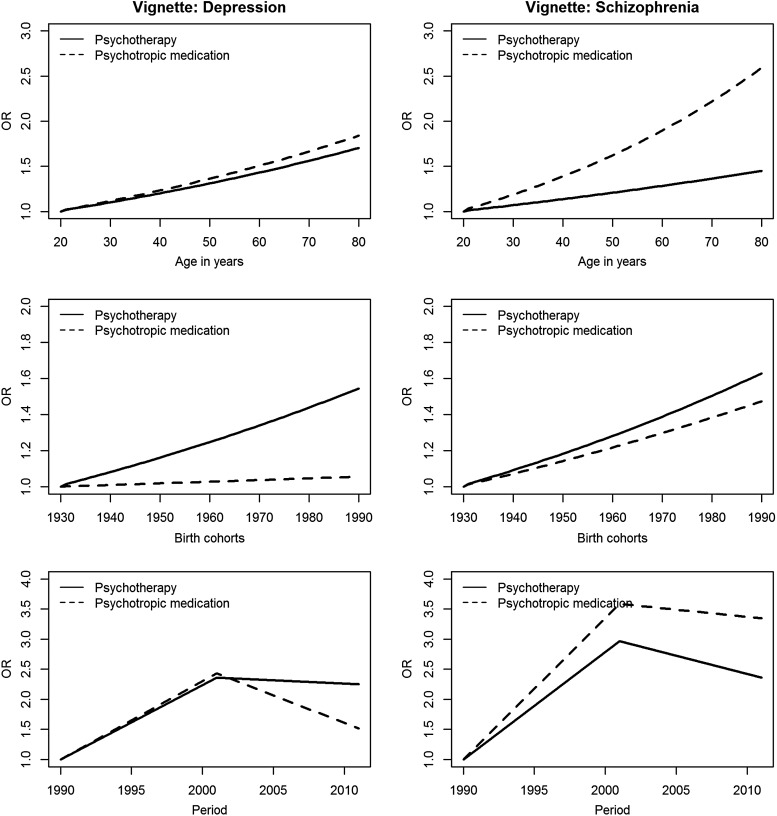
For both disorders, approval of both psychotherapy and medication for a person with mental illness increases with age. At the same time, younger cohorts showed stronger recommendations particularly for psychotherapy (OR around 1.07 per decade). The strongest effects could be observed for time period with an increase in recommendation between 1990 and 2001 with odds ratio of 2.36 in depression and 2.97 in schizophrenia, respectively. In general, the treatment option that showed the strongest increase in recommendation was medication for schizophrenia and psychotherapy for depression.
Conclusion.
Underutilisation of psychotherapy in old age seems not to reflect treatment preferences of older persons. Thus, special treatment approaches need to be offered for this group that seems to be willing for psychotherapy but do not yet use it. Cohort patterns suggest that approval of psychotherapy among older persons will likely further increase in the coming years as these people get older. Finally, strong period effects underpin the importance of changing attitudes in the society. These could reflect reporting changes about psychiatric topics in the media or a general increase in the perception of treatment options. Nevertheless, more treatment offers especially for older people are needed.
Key words: Age-period-cohort, psychotherapy in old age
Introduction
Mental disorders in old age are associated with higher general health service use (Luppa et al. 2012). Yet, the use of mental health services is often poorly matched to needs and only one-third of all older adults with mental disorders report ever seeking help for their complaints such as psychiatric medication or psychotherapy (Wittchen & Pittrow, 2002; Cepoiu et al. 2008; Busch et al. 2013). Reasons for this misallocation of health care resources are unclear: under-diagnosis of mental health problems in old age is one likely barrier to adequate treatment (Mitchell et al. 2010), but negative attitudes towards psychiatric medication or psychotherapy could also play a role. Looking specifically at attitudes towards psychotherapy and pharmacotherapy, a study among depressed primary care patients in the USA indicated a preference for counselling or psychotherapy over antidepressant medication (Gum et al. 2006), which corresponds to population studies that consistently show stronger preferences for psychotherapy over pharmacotherapy (Schomerus et al. 2012). However, only very few older persons with depression receive psychotherapy, most patients of older age receiving treatment are taking antidepressant medication (Morichi et al. 2015). On the one hand, this is simply because guidelines for geriatric depression recommend antidepressant medication as an initial treatment (Alexopoulos, 2011), probably still reflecting the false belief that older persons do not benefit from psychotherapy. On the other hand, access to psychotherapy is limited (Unützer et al. 2003) and depression in older age is often accompanied by cognitive deficits, which might result in under-diagnosis of mood disorders (Morimoto & Alexopoulos, 2013; Koethe et al. 2014).
When looking at age-related differences in attitudes, three effects need to be distinguished. Age-effects refer to regular changes in attitudes over the lifespan, regardless of the year a person is born. Besides these changes over the lifespan, cohort effects might also cause variation in attitudes between older and younger persons. Cohort effects refer to attitudes that develop similarly in a certain birth cohort, for example, due to a shared cultural environment in childhood. The third time related effect on attitudes, changes that affect the general population regardless of age or birth cohort, is referred to as period effects. They reflect general attitude changes within a specific time frame, caused for example by economic or societal changes, but potentially also by population wide antistigma campaigns. Put briefly, age effects characterise the effect of ageing, while cohort effects characterise the effects of upbringing and period effects characterise societal changes.
So far, few studies examined attitudes of older persons towards mental health care and the existing cross-sectional studies based on population-based and clinical samples revealed inconsistent results (Leaf et al. 1987; Kessing et al. 2005). A study in Denmark found more negative attitudes towards antidepressant medication among older compared with younger adults being treated for affective disorders (Kessing et al. 2005). A population-based study in the USA of attitudes towards mental health services in 1980 found that both younger and older participants are more sceptical towards mental health care seeking compared with those aged 25–64 years (Leaf et al. 1987). In contrast, analyses of the population-based National Comorbidity Survey 1990–1992 in the USA found a positive correlation between age and willingness to seek mental health treatment (Mojtabai, 2007). So far, it is thus unclear whether attitudes towards using mental health care differ between younger and older persons.
Regarding period effects, attitudes of the general population towards psychiatric treatment have changed over the last decades. A meta-analysis of time-trend studies from several Western industrialised countries showed that in more recent surveys, more people recommended drug treatment of mental disorders than did so in earlier surveys (Schomerus et al. 2012). Accordingly, prescription rates particularly for antidepressant medication are rising. Between 1999 and 2010, antidepressant use in the USA increased from 6 to 10% of the population (Olfson & Marcus, 2009; Mojtabai & Olfson, 2014). Similarly, in OECD countries, consumption of antidepressants rose from 3 to 6 defined daily doses (DDD) per 100 inhabitants between 2000 and 2011 (OECD. Health at a Glance 2013: http://www.oecd.org/health/healthtaglance (accessed 26.5.2014)). A time trend study over 21 years from Germany showed that between 1990 and 2011, the approval rates of psychotherapy for depression rose from 57 to 71%, and for schizophrenia from 62 to 82% (Angermeyer et al. 2013a, b). A Swedish study recently reported an overall increase in more positive attitudes toward psychotherapy and medication between 1976 and 2014 (Mirnezami et al. 2015). While suggesting a strong period-effect, these studies did not investigate simultaneously the effect of age, cohort and time period on treatment approval. Hence, it is unclear to what extent age of the respondents, changes in birth cohorts, or general societal changes are responsible for the development of preferences for psychotropic medications or psychotherapy over time.
Aims of the study
In this paper, we examine age related differences in attitudes towards mental health treatment by disentangling age, cohort and period effects. In particular, we use age, period and cohort analyses based on three pooled cross-sectional studies of the German population to examine the approval of either psychiatric medication or psychotherapy for a person with either depression or schizophrenia.
Methods
Surveys
Our study is based on data from three methodologically identical population-based cross-sectional surveys among German citizens aged 18 years and older conducted in 1990, 2001 and 2011 (Angermeyer & Matschinger, 1997; Angermeyer et al. 2003, 2013a, b; Schomerus et al. 2015). Aim of these surveys was to assess various mental health-related attitudes of the general population cross-sectionally, and to enable time-trend analyses of attitudes. In all surveys, the samples were drawn using an identical random sampling procedure with the three stages sample points, households and individuals within the target households. Target households within the sample points were determined according to the random route procedure (Gabler & Hoffmeyer-Zlotnik, 1997). Target individuals within households were selected using random digits. Informed consent was considered to have been given when individuals agreed to complete the interview. Fieldwork was carried out by GETAS (Hamburg) in 1990, and by USUMA (Berlin) in 2001 and 2011. Data in 1990 were gathered in two waves, wave 1 in the old German states (April 1990) and wave 2 in the new German states (November 1990) shortly after re-unification.
Interview
All interviews were conducted face-to-face using pencil and paper. In all surveys, the fully structured interview was identical regarding wording and the sequence of questions. At the beginning of the interview respondents were presented with a vignette of a diagnostically unlabelled case history depicting a person with mental illness. While several mental disorders had been studied in single surveys, vignettes on schizophrenia and major depression had been used in three consecutive surveys and could thus be subject of our age-period-cohort (APC) analysis. The symptoms described in both vignettes fulfilled the criteria of DSM-IV for schizophrenia or depression and had been validated by five experts in psychopathology blinded to the diagnosis (vignettes see supplement). While in 1990 and 2011 the sex of the individual presented in the vignettes varied at random, in 2001 only responses to a male vignette were elicited. For the present study, we thus only use responses elicited with the male vignette. We asked respondents treatment recommendation for the person described in the vignette. Presenting them with a catalogue of treatment options, we asked: ‘Although you might not be expert, you may have an idea what should best be recommended to someone with a problem described in the vignette. Please tell me for each option to what extent you would recommend it or would not recommend it.’ Eliciting treatment recommendations for a third person is an established method to assess mental health literacy (Reavley & Jorm, 2012). Recently it has been shown that treatment recommendations and personal treatment preferences are closely related (Rüsch et al. 2014). Answers were recorded using a five-point Likert scale with the anchors 1 = ‘I would strongly recommend it’ and 5 = ‘I would strongly advise against it’, plus a ‘don't know’ category. For our present analysis, we use answers to the items ‘using psychotherapy’ and ‘taking psychotropic drugs’.
Sample description
Our combined study sample from all surveys consisted of 9046 participants, 4505 subjects receiving the depression vignette and 4541 participants receiving the schizophrenia vignette. Since in both samples from 1990 the population from the old (West-)German states was underrepresented, we weighted this sample to achieve a proportion of 80:20 for old and new German states for the schizophrenia and depression sample, respectively. This is representative of the overall German population and identical to the old/new-proportions in the samples from 2001 and 2011. Participants with missing values in one of the analysed variables were excluded. To aid interpretation of results, we also excluded participants answering with ‘don't know’ (vignette: depression + recommendation: psychotherapy N = 356; vignette: depression + recommendation: psychotropic medication N = 443; vignette: schizophrenia + recommendation: psychotherapy N = 299; vignette: schizophrenia + recommendation: psychotropic medication N = 457). Our final study sample thus included N = 4120 (psychotherapy) and N = 4034 (psychotropic medication) for the depression vignette and N = 4212 (psychotherapy) and N = 4061 (psychotropic medication) for the schizophrenia vignette.
Statistical analysis
Disentangling age, cohort and period effects is methodologically challenging because of the perfect collinearity of the three time variables (period = cohort + age). To extract the ‘pure age related effect’ that is not confounded by cohort or period effects, more advanced statistical methods than simple ordinary least-squares regression are required. For each of the two disorders, we performed an APC analysis to test and separate associations of age at examination, birth cohort and time period with our two items of treatment recommendation (psychotherapy and psychotropic medication). This collinearity problem is referred to as the identification problem because only two of the three variables can be put into a regression model simultaneously. Instead, we used partial least-squares regressions (PLS), which allow using perfectly collinear variables in one regression model. In PLS components are extracted that are weighted combinations of the original variables. These components are chosen according to their relationship to the outcome variable. They seek to maximise the covariance between the outcome and those weighted components. As a result, the first component has a greater covariance with the outcome than the second and so on. In a three-dimensional space with three covariates as input variables a maximum of three PLS components can be extracted which are orthogonal to each other. The regression coefficients for the three variables can directly be obtained from their weights in each component (Tu et al. 2012; Jiang et al. 2013). For the mathematical equations see supplemental material. Bastien et al. (2005) extended the linear PLS to generalised linear models (GLM), including binary and ordinal regression. We used the R-package plsRglm that is available on the CRAN archive and maintained by Frédéric Bertrand. First, we used a GLM PLS with logit link and binomial distribution to model binary treatment recommendation for psychotherapy and psychotropic medication, respectively. We dichotomised the five-point Likert scales (1: ‘I would strongly recommend’ & ‘I would recommend’ 0: ‘I would neither recommend or advise against it’ & ‘I would advise against it’ & ‘I would strongly advise against it’). We included age at interview and birth cohort as continuous variables and two dummy variables for time period (i.e. 2011 and 2001 v. 1990) as covariates. We performed 1000 bootstrap replications to obtain 95% confidence intervals (CIs). To additionally examine non-linear relationships for age and birth cohort, we used restricted cubic splines (Harrell, 2001) in PLS regression with five knots for age at examination and birth cohort. Wald tests of coefficients of the second, third and fourth spline transformation equal to zero were used to obtain p values for nonlinearity. Wald tests indicated that age and cohort were linearly related to all outcomes. To assess the model fit of linear and non-linear PLS, we compared the pseudo R2, which is a measure of the variance of the outcome variable that can be explained by the covariates, analogous to ordinary least-squares regression. Because PLS penalises variables according to their variance when extracting the components, covariates were scaled to have unit variance and zero mean. To validate our results, we conducted two additional sensitivity analyses detailed in the supplement. First, we included those participants that had answered with the ‘don't know’ category by coding them as denial of treatment (i.e. ‘I would strongly advise against it’) in the binary logistic regression. Second, we performed an ordered logistic regression included in the plsRglm package with the five response categories of the Likert scale (setting respondents with ‘don't know’ to missing). To test the proportional odds assumption underlying the ordered logit model, we used a graphical method proposed by Harrell (2001) because other statistical tests have the tendency to reject the null hypothesis. Analyses were performed using the statistical software R (version 3.0.2).
Results
In the pooled cross-sectional data age at examination ranged from 18 to 93 and birth cohort from 1900 to 1993. Table 1 shows the number of individuals in each age group and stratified by type of vignette for 1990, 2001 and 2011 (see Supplementary Table S1 for the number of individuals per birth cohort). For more details on the distribution of age and birth cohort with respect to their recommendation see Supplementary Fig. S1. The mean age was 47 for both samples and mean birth cohort was 1952. The depression and schizophrenia samples had 44 and 46% males, respectively.
Table 1.
Number of subjects of each age group at each time period
| 1990 | 2001 | 2011 | 1990 | 2001 | 2011 | |
|---|---|---|---|---|---|---|
| Age | Psychotherapy | Psychotropic medication | ||||
| Depression vignette | (N = 4120) | (N = 4034) | ||||
| <30 | 270 | 417 | 76 | 263 | 413 | 72 |
| 30–39 | 231 | 508 | 87 | 223 | 487 | 87 |
| 40–49 | 196 | 430 | 113 | 194 | 417 | 105 |
| 50–59 | 192 | 335 | 106 | 199 | 336 | 98 |
| 60–69 | 176 | 411 | 88 | 170 | 419 | 78 |
| ≥70 | 103 | 279 | 102 | 105 | 278 | 90 |
| Recommending therapy | 635 (65%) | 1,793 (75%) | 433 (76%) | 263 (23%) | 995 (42%) | 205 (39%) |
| Schizophrenia vignette | (N = 4212) | (N = 4061) | ||||
| <30 | 307 | 382 | 69 | 291 | 370 | 66 |
| 30–39 | 262 | 498 | 92 | 250 | 491 | 80 |
| 40–49 | 205 | 467 | 107 | 204 | 451 | 102 |
| 50–59 | 211 | 332 | 99 | 202 | 326 | 98 |
| 60–69 | 195 | 387 | 114 | 184 | 375 | 101 |
| ≥70 | 115 | 271 | 99 | 108 | 270 | 92 |
| Recommending therapy | 883 (68%) | 2034 (87%) | 506 (87%) | 346 (28%) | 1371 (60%) | 329 (61%) |
Model fit
In all PLS analyses, a two-component model showed better model-fit than a one-component model and a similar model fit to the three-component model (see Supplementary Table S2). We thus report results for the two-components logistic PLS models only (Table 2). In depression, the two components PLS model explained 4.07% of the variance (pseudo R2) for recommending psychotherapy and 3.63% for psychotropic medication (one-component model: psychotherapy 3.74%; psychotropic medication 2.98%). In total, 69.4% of all participants would recommend psychotherapy and 36.3% psychotropic medication in case of depression irrespective of age, birth cohort or period. For schizophrenia, the model with two PLS components explained 4.85% of the variance for the treatment recommendation psychotherapy and 9.23% for psychotropic medication (one-component model: psychotherapy 4.36%; psychotropic medication 8.24%). Overall 81.3% recommend psychotherapy and 50.4% psychotropic medication as treatment for schizophrenia.
Table 2.
Treatment recommendations towards a person with schizophrenia or depression: age, period and cohort effects.
| Psychotherapy | Psychotropic medication | |||
|---|---|---|---|---|
| OR | 95% CIa | OR | 95% CIa | |
| Schizophrenia | ||||
| Age (years) | 1.006 | (1.002, 1.010) | 1.016 | (1.014, 1.018) |
| Cohort (years) | 1.008 | (1.007, 1.010) | 1.006 | (1.004, 1.009) |
| Period (1990 ref.) | ||||
| 2001 | 2.967 | (2.523, 3.466) | 3.589 | (3.176, 4.133) |
| 2011 | 2.361 | (1.708, 3.277) | 3.344 | (2.543, 4.076) |
| R2 | 4.85% | 9.23% | ||
| Depression | ||||
| Age (years) | 1.009 | (1.006, 1.012) | 1.010 | (1.008, 1.013) |
| Cohort (years) | 1.007 | (1.004, 1.009) | 1.001 | (0.999, 1.004) |
| Period (1990 ref.) | ||||
| 2001 | 2.361 | (2.068, 2.747) | 2.430 | (2.109, 2.881) |
| 2011 | 2.254 | (1.773, 2.804) | 1.517 | (1.244, 2.032) |
| R2 | 4.07% | 3.63% | ||
Logistic PLS regression with two components. Unstandardised coefficients.
CI after 1000 non-parametric Bootstrap replicates.
Age effects
For the depression vignette, age was significantly associated with an increase of both treatment recommendations with similar effect sizes (psychotherapy OR per decade = 1.09; psychotropic medication OR per decades = 1.10) independent from cohort and period effects (Table 2). Over the lifespan of 60 years the odds for recommending psychotherapy increases to OR = 1.69 and to OR = 1.82 for psychotropic medication (Fig. 1). In schizophrenia, both recommendations also showed a significant age effect (Table 2). Likewise, we observed an OR of 1.06 per decade for the recommendation of psychotherapy and even higher, OR = 1.16 per decade, for recommending psychotropic medication. Over the lifespan (60 years) this cumulates to an increase of ORs to 1.44 and 2.55 for recommending psychotherapy and psychotropic medication, respectively (Fig. 1).
Fig. 1.
Cumulative effect of age, cohort and period on treatment recommendations for schizophrenia and depression.
Cohort effects
In depression, an effect of birth cohort on treatment recommendation could only be observed for psychotherapy (OR = 1.07 per decade) with greater approval in persons born in more recent birth cohorts. Over a time period from cohorts 1930 to 1990 this increases OR to 1.53.
For schizophrenia, both treatment recommendations also showed a significant cohort effect with similar effect sizes (ORs per decade of 1.08 and 1.06 for psychotherapy and medication, respectively). Participants born in later years indicated stronger recommendation for both treatment options, irrespective of age and period effects. Comparing early and most recent birth cohorts over 60 years (1930–1990), this effect cumulated to an OR = 1.62 and OR = 1.46 for psychotherapy and psychotropic medication, respectively (Fig. 1).
Taken together, age and cohort effects indicate higher attitudes both over the lifespan and in coming years, when more recent cohorts grow older.
Period effects
For time period, we calculated the effects for the three distinct time points. In depression, time period had a strong effect on treatment recommendations. Participants from more recent surveys indicated higher approval for the treatment options than the reference sample from 1990. The OR for choosing psychotherapy was 2.361 in 2001 and 2.25 in 2011, when 1990 served as reference category. For psychotropic medication, ORs were 2.43 in 2001 and 1.52 in 2011 (with 1990 as reference category). Using 2001 as reference category yielded no significant change between 2001 and 2011, neither for psychotherapy nor for psychotropic medication.
Similar to depression a significant period effect could be observed in schizophrenia for both treatment recommendations, particularly for psychotropic medication. People from the more recent surveys were more likely to recommend both treatment options. The OR for recommending psychotherapy were 2.97 in 2001 and 2.36 in 2011, compared with 1990. The decline between 2001 and 2011 was not significant when 2001 served as the reference group. For psychotropic medication the OR in 2001 was 3.59 and 3.34 in 2011, which is a relatively stable approval for this treatment between 2001 and 2011. Again, the decrease in treatment recommendation between 2001 and 2011 was not statistically significant.
Using the full sample by including the ‘don't know category’ as potential denial of treatment did not change the overall associations (Supplementary Table S3). Similarly, ordinal logistic regression on the five-point Likert scale showed overall similar results to those presented in the main analysis (Supplementary Table S4) indicating a robust model.
In summary, we found improving attitudes over time. Recommendation increases with growing age, in more recent birth cohorts, and generally improved over the last 20 years (Fig. 1). Differences in the APC pattern for treatment recommendations between schizophrenia and depression were primarily observed for recommending psychotropic medication.
Discussion
The first positive conclusion we can draw from our analyses is that no treatment recommendation showed a significant decrease irrespective of vignette, growing age, birth cohort or time period. The by far strongest effects were observed for time period, especially between 1990 and 2001. Obviously there has been a general rise in acceptance for professional mental health treatment, a trend that has been described and discussed previously (Angermeyer & Matschinger, 2005; Mojtabai, 2007). In our study, this trend peaked in 2001, with no significant further increase in treatment recommendations between 2001 and 2011. Disentangling this trend from any age and cohort effects, our study corroborates the notion that psychiatric treatment has generally gained acceptance over the last 20 years (Angermeyer et al. 2013b). These changes have been attributed to changes within psychiatric services following psychiatric reform, to increasing mental health literacy of the general population, but also to a more biological understanding of mental disorders (Angermeyer & Matschinger, 2005; Mojtabai, 2007; Angermeyer et al. 2013b). Since our study is the first to look at age and cohort effects in treatment recommendations for mental disorders, we will focus our discussion on this novel part of our results. Our findings show that there is no reason to suspect that particularly psychotherapy receives less support among older compared with younger persons. Especially for depression, psychotherapy as well as psychotropic medication show a similar increase in popularity with growing age. In our sample, 71.5% of the participants aged 70 years and above recom mended psychotherapy and 47.1% recommended medication. In schizophrenia, the recommendation for psychotropic medication showed a much stronger increase than psychotherapy but both treatment options are highly recommended in old age (psychotherapy 78.6% and psychotropic medication 60.2% in people of age ≥70 in our sample). The higher recommendation rates in schizophrenia could reflect the greater perceived severity of schizophrenia as depicted in our vignettes, highlighting a stronger necessity for treatment. Accordingly, the percentage of the subjects in the survey 2011 considering the person described as suffering from a ‘mental illness in a medical sense’ was 83% in schizophrenia compared with 65% in depression (Schomerus et al. 2013). If schizophrenia is more frequently seen as a medical problem, a higher rate of professional treatment recommendations seems plausible.
Depression among older persons is very common, affecting between 10 and 15% of older persons living in the community (Beekman et al. 1999). Facing the challenge of an ageing society and a rising number of geriatric patients in the future, adequate treatment options are required. Although antidepressant use especially in the elderly has increased (Olfson & Marcus, 2009), only one-third of older patients achieve remission (McGovern et al. 2014). Pharmacotherapy with antidepressants in older persons is also associated with higher all-cause mortality (Coupland et al. 2011). Older persons are more likely to exhibit adverse drug effects due to multi-morbidity and the high number of prescribed medications (Dines et al. 2014). Moreover, meta-analyses show similar effect sizes for pharmacotherapy and psychotherapy in older persons with depression (Pinquart et al. 2007). Provision of psychotherapy should thus complement pharmacotherapy or could even be a safer alternative to medication. It is becoming increasingly recognised that older people represent a suitable target group for psychotherapy due to their better emotional regulation skills, increased wisdom and resilience mechanisms accumulated over many years of experience (Laidlaw, 2013). Our findings support the willingness of this patient group to undertake psychotherapy in case of depression.
The particular merits of disentangling age, cohort and period effects are illustrated by the fact that both older age and a more recent birth cohort are associated with stronger approval of mental health treatment. This finding might level differences between older and younger respondents in cross-sectional assessments, but our analyses indicate that prospectively, the popularity of professional treatment among older persons will further increase when younger cohorts grow older. In depression, this is particularly true for psychotherapy, where younger cohorts that are even more open minded towards psychotherapy will become the new generation of older people. The strong period effects found in this study, yielding continuously higher recommendation rates for psychotherapy in more recent surveys compared with 1990, also supports this trend. Conversely, attitudes towards pharmacotherapy of depression seem to have peaked: they do not improve in younger cohorts, and between 2001 and 2011 there seems to be an overall (although insignificant) decline in approval. Generally, the strong period effects found in this study show that attitudes towards mental health treatment are changeable, which is an encouraging finding for future awareness and prevention programs.
Treatment recommendations for a person with schizophrenia also increased with age. Regarding specific treatment options for older people, this seems less important. First, approval rates for both medication and psychotherapy are generally high in schizophrenia, so age-related effects are less relevant. Second, schizophrenia mainly starts at younger age and is thus of less personal relevance for older persons. Nevertheless, our concordant findings on schizophrenia and depression suggest that greater openness particularly towards psychotherapy is not restricted to a specific diagnosis, but is reflecting a general change of mental health related attitudes. This is especially visible in the strong period effect of increased overall approval of treatment options between 1990 and 2001.
Our study has several limitations that need to be considered. First, we elicited treatment recommendations for another person, and not personal treatment preferences. However, there is evidence that recommendations for others and personal preferences are closely related (Rüsch et al. 2014). Examining recommendations is also relevant in itself, because advice from a friend or family member is one of the main sources of information in case of help seeking for psychiatric disorders (Rüsch et al. 2014). But it must also be noted that at the end the recommendation of the doctor has a great influence on treatment decision, too. Thus, it may be interesting to analyse the changes in treatment preferences of primary care physicians.
Other factors besides the three-time variables examined in this study might determine recommendations regarding mental treatment options. These may be sex, education or prior contact to people with mental disorders. This study aimed to examine and compare age relative to cohort and period effects. Future studies will help to examine whether this effects are attributable to other potential confounding, effect-modifying factors and mediators.
In summary, our study shows that both medication and psychotherapy are becoming more popular over the lifespan. Increasing the provision of psychotherapy for older persons in need would be perfectly in line with treatment preferences elicited among the general population.
Supplementary material
For supplementary material accompanying this paper visit http://dx.doi.org/10.1017/S2045796015001134.
click here to view supplementary material
References
- Alexopoulos GS (2011). Pharmacotherapy for late-life depression. The Journal of Clinical Psychiatry 72, e04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Angermeyer MC, Matschinger H (1997). Social distance towards the mentally ill: results of representative surveys in the Federal Republic of Germany. Psychological Medicine 27, 131–141. [DOI] [PubMed] [Google Scholar]
- Angermeyer MC, Matschinger H (2005). Have there been any changes in the public's attitudes towards psychiatric treatment? Results from representative population surveys in Germany in the years 1990 and 2001. Acta Psychiatrica Scandinavica 111, 68–73. [DOI] [PubMed] [Google Scholar]
- Angermeyer MC, Beck M, Matschinger H (2003). Determinants of the public's preference for social distance from people with schizophrenia. Canadian Journal of Psychiatry. Revue canadienne de psychiatrie 48, 663–668. [DOI] [PubMed] [Google Scholar]
- Angermeyer MC, Matschinger H, Schomerus G (2013a). Attitudes towards psychiatric treatment and people with mental illness: changes over two decades. The British Journal of Psychiatry: The Journal of Mental Science 203, 146–151. [DOI] [PubMed] [Google Scholar]
- Angermeyer MC, Matschinger H, Schomerus G (2013b). Has the public taken notice of psychiatric reform? The image of psychiatric hospitals in Germany 1990–2011. Social Psychiatry and Psychiatric Epidemiology 48, 1629–1635. [DOI] [PubMed] [Google Scholar]
- Bastien P, Esposito-Vinzi V, Tenenhaus M (2005). PLS generalized linear regression. Computational Statistics & Data Analysis 48, 17–46. [Google Scholar]
- Beekman AT, Copeland JR, Prince MJ (1999). Review of Community Prevalence of depression in later life. British Journal of Psychiatry 174, 307–311. [DOI] [PubMed] [Google Scholar]
- Busch MA, Neuner B, Aichberger MC, Hapke U, Riedel-Heller SG, Luppa M (2013). Depressive Symptomatik und Inanspruchnahme von Gesundheits- und Pflegeleistungen bei Personen im Alter ab 50 Jahren in Deutschland. Ergebnisse einer bevölkerungsbasierten Querschnittstudie [Depressive symptoms and health service utilisation among persons 50 years or older in Germany. A population-based cross-sectional study]. Psychiatrische Praxis 40, 214–219. [DOI] [PubMed] [Google Scholar]
- Cepoiu M, McCusker J, Cole MG, Sewitch M, Belzile E, Ciampi A (2008). Recognition of depression by non-psychiatric physicians – a systematic literature review and meta-analysis. Journal of General Internal Medicine 23, 25–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coupland C, Dhiman P, Morriss R, Arthur A, Barton G, Hippisley-Cox J (2011). Antidepressant use and risk of adverse outcomes in older people: population based cohort study. BMJ 343, d4551. doi: 10.1136/bmj.d4551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dines P, Hu W, Sajatovic M (2014). Depression in later-life: an overview of assessment and management. Psychiatria Danubina 26 (Suppl. 1), 78–84. [PubMed] [Google Scholar]
- Gabler S, Hoffmeyer-Zlotnik JH (1997). Stichproben in der Umfragepraxis. Westdeutscher Verlag: Opladen. [Google Scholar]
- Gum AM, Arean PA, Hunkeler E, Tang L, Katon W, Hitchcock P, Steffens DC, Dickens J, Unutzer J (2006). Depression treatment preferences in older primary care patients. The Gerontologist 46, 14–22. [DOI] [PubMed] [Google Scholar]
- Harrell FE Jr. (2001). Regression Modeling Strategies. With Applications to Linear Models, Logistic Regression, and Survival Analysis. Springer: New York. [Google Scholar]
- Jiang T, Gilthorpe MS, Shiely F, Harrington JM, Perry IJ, Kelleher CC, Tu Y-K (2013). Age-period-cohort analysis for trends in body mass index in Ireland. BMC Public Health 13, 889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessing LV, Hansen HV, Demyttenaere K, Bech P (2005). Depressive and bipolar disorders: patients’ attitudes and beliefs towards depression and antidepressants. Psychological Medicine 35, 1205–1213. [DOI] [PubMed] [Google Scholar]
- Koethe D, Mattern M, Herpertz SC (2014). Psychotherapeutische Arbeit mit älteren Patienten. Der Nervenarzt 85, 1345–1351. [DOI] [PubMed] [Google Scholar]
- Laidlaw K (2013). A deficit in psychotherapeutic care for older people with depression and anxiety. Gerontology 59, 549–556. [DOI] [PubMed] [Google Scholar]
- Leaf PJ, Bruce ML, Tischler GL, Holzer CE III (1987). The relationship between demographic factors and attitudes toward mental health services. Journal of Community Psychology 15, 275–284. [DOI] [PubMed] [Google Scholar]
- Luppa M, Sikorski C, Motzek T, Konnopka A, Konig H-H, Riedel-Heller SG (2012). Health service utilization and costs of depressive symptoms in late life – a systematic review. Current Pharmaceutical Design 18, 5936–5957. [DOI] [PubMed] [Google Scholar]
- McGovern AR, Kiosses DN, Raue PJ, Wilkins VM, Alexopoulos GS (2014). Psychotherapies for late-life depression. Psychiatric Annals 44, 147–152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mirnezami HF, Jacobsson L, Edin-Liljegren A (2015). Changes in attitudes towards mental disorders and psychiatric treatment 1976–2014 in a Swedish population. Nordic Journal of Psychiatry 70, 38–44. [DOI] [PubMed] [Google Scholar]
- Mitchell AJ, Rao S, Vaze A (2010). Do primary care physicians have particular difficulty identifying late-life depression? A meta-analysis stratified by age. Psychotherapy and Psychosomatics 79, 285–294. [DOI] [PubMed] [Google Scholar]
- Mojtabai R (2007). Americans’ attitudes toward mental health treatment seeking: 1990–2003. Psychiatric Services (Washington, DC) 58, 642–651. [DOI] [PubMed] [Google Scholar]
- Mojtabai R, Olfson M (2014). National trends in long-term use of antidepressant medications: results from the U.S. National Health and Nutrition Examination Survey. The Journal of Clinical Psychiatry 75, 169–177. [DOI] [PubMed] [Google Scholar]
- Morichi V, Dell'Aquila G, Trotta F, Belluigi A, Lattanzio F, Cherubini A (2015). Diagnosing and treating depression in older and oldest old. Current Pharmaceutical Design 21, 1690–1698. [DOI] [PubMed] [Google Scholar]
- Morimoto SS, Alexopoulos GS (2013). Cognitive deficits in geriatric depression: clinical correlates and implications for current and future treatment. The Psychiatric Clinics of North America 36, 517–531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olfson M, Marcus SC (2009). National patterns in antidepressant medication treatment. Archives of General Psychiatry 66, 848–856. [DOI] [PubMed] [Google Scholar]
- Pinquart M, Duberstein P, Lyness J (2007). Effects of psychotherapy and other behavioural interventions on clinically depressed older adults: a meta-analysis. Aging and Mental Health 11, 645–657. [DOI] [PubMed] [Google Scholar]
- Reavley NJ, Jorm AF (2012). Public recognition of mental disorders and beliefs about treatment: changes in Australia over 16 years. The British Journal of Psychiatry: The Journal of Mental Science 200, 419–425. [DOI] [PubMed] [Google Scholar]
- Rüsch N, Müller M, Ajdacic-Gross V, Rodgers S, Corrigan PW, Rössler W (2014). Shame, perceived knowledge and satisfaction associated with mental health as predictors of attitude patterns towards help-seeking. Epidemiology and Psychiatric Sciences 23, 177–187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schomerus G, Matschinger H, Angermeyer MC (2013). Continuum beliefs and stigmatizing attitudes towards persons with schizophrenia, depression and alcohol dependence. Psychiatry Research 209, 665–669. [DOI] [PubMed] [Google Scholar]
- Schomerus G, Schwahn C, Holzinger A, Corrigan PW, Grabe HJ, Carta MG, Angermeyer MC (2012). Evolution of public attitudes about mental illness: a systematic review and meta-analysis. Acta Psychiatrica Scandinavica 125, 440–452. [DOI] [PubMed] [Google Scholar]
- Schomerus G, Van der Auwera S, Matschinger H, Baumeister SE, Angermeyer MC (2015). Do attitudes towards persons with mental illness worsen during the course of life? An age-period-cohort analysis. Acta Psychiatrica Scandinavica 132, 357–364. [DOI] [PubMed] [Google Scholar]
- Tu Y-K, Krämer N, Lee W-C (2012). Addressing the identification problem in age-period-cohort analysis: a tutorial on the use of partial least squares and principal components analysis. Epidemiology (Cambridge, MA) 23, 583–593. [DOI] [PubMed] [Google Scholar]
- Unützer J, Katon W, Callahan CM, Williams JW, Hunkeler E, Harpole L, Hoffing M, Della Penna RD, Noel PH, Lin EHB, Tang L, Oishi S (2003). Depression treatment in a sample of 1801 depressed older adults in primary care. Journal of the American Geriatrics Society 51, 505–514. [DOI] [PubMed] [Google Scholar]
- Wittchen H-U, Pittrow D (2002). Prevalence, recognition and management of depression in primary care in Germany: the Depression 2000 study. Human Psychopharmacology 17 (Suppl. 1), S1–S11. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
For supplementary material accompanying this paper visit http://dx.doi.org/10.1017/S2045796015001134.
click here to view supplementary material