Abstract
Aims.
Timely recognition and treatment of mental disorders with an onset in childhood and adolescence is paramount, as these are characterized by greater severity and longer persistence than disorders with an onset in adulthood. Studies examining time-to-treatment, also referred to as treatment delay, duration of untreated illness or latency to treatment, and defined as the time between disorder onset and initial treatment contact, are sparse and all based on adult samples. The aim of this study was to describe time-to-treatment and its correlates for any health care professional (any care) and secondary mental health care (secondary care), for a broad range of mental disorders, in adolescents.
Methods.
Data from the Dutch community-based cohort study TRacking Adolescents’ Individual Lives Survey (TRAILS; N = 2230) were used. The Composite International Diagnostic Interview (CIDI) was administered to assess DSM-IV disorders, the age of onset, and the age of initial treatment contact with any health care professional in 1584 adolescents of 18–20 years old. In total 43% of the adolescents (n = 675) were diagnosed with a lifetime DSM-IV disorder. The age of initial treatment contact with secondary care was based on administrative records from 321 adolescents without a disorder onset before the age of 10. Descriptive statistics, cumulative lifetime probability plots, and Cox regression analyses were used analyze time-to-treatment.
Results.
The proportion of adolescents who reported lifetime treatment contact with any care varied from 15% for alcohol dependence to 82% for dysthymia. Regarding secondary care, proportions of lifetime treatment contact were lower for mood disorders and higher for substance dependence. Time-to-treatment for any care varied considerably between and within diagnostic classes. The probability of lifetime treatment contact for mood disorders was above 90%, whereas for other mental disorders this was substantially lower. An earlier age of onset predicted a longer, and the presence of a co-morbid mood disorder predicted a shorter time-to-treatment in general. Disorder severity predicted a shorter time-to-treatment for any care, but not for secondary care. Time-to-treatment for secondary care was shorter for adolescents from low and middle socioeconomic background than for adolescents from a high socioeconomic background.
Conclusion.
Although the time-to-treatment was shorter for adolescents than for adults, it was still substantial, and the overall patterns were remarkably similar to those found in adults. Efforts to reduce time-to-treatment should therefore be aimed at children and adolescents. Future research should address mechanisms underlying time-to-treatment and its consequences for early-onset disorders in particular.
Key words: Adolescence, diagnosis, health service research, mental health, survival analysis
Introduction
The prevalence of mental disorders is high (Kessler et al. 2005a; Moffitt et al. 2010; de Graaf et al. 2012). Although mental disorders are associated with a tremendous disease burden (Whiteford et al. 2013), worldwide, no more than one-third of people with a mental disorder receive treatment (Kessler et al. 2005b; Thornicroft, 2012). The majority of mental disorders in adulthood have their onset in adolescence and early adulthood (Wang et al. 2005; Kessler et al. 2007; Merikangas et al. 2010; de Girolamo et al. 2012; Ormel et al. 2015), and interfere with key areas of development such as education, social relationships and the transition to work (Costello & Maughan, 2015). Timely recognition and treatment of such early-onset mental disorders is paramount, as these are characterised by greater severity and longer persistence than disorders with an onset in adulthood (Kessler et al. 1998; Korczak & Goldstein, 2009; Reef et al. 2010). However, despite the apparent need for care (Jörg et al. 2015), only a small proportion of youths actually receive timely treatment (Merikangas et al. 2011; de Girolamo et al. 2012; Jansen et al. 2013).
Studies focusing on the time between the onset of a mental disorder and initial treatment contact (time-to-treatment; also referred to as treatment delay, duration of untreated illness or latency to treatment), have mainly focused on the duration of untreated psychosis (DUP). Review studies show that a longer DUP is associated with a worse course of illness and worse outcomes (Marshall et al. 2005; Perkins et al. 2005). Studies focusing on time-to-treatment in common mental disorders are sparse (Ghio et al. 2014), but these also point towards poorer outcomes of disorders with longer time-to-treatment (Kisely et al. 2006; Dell'Osso & Altamura, 2010). Of particular interest is the finding that an earlier age of onset is associated with a longer time-to-treatment in both community (Kessler et al. 1998; Christiana et al. 2000; Wang et al. 2004, 2005, 2007; Bruffaerts et al. 2007; Korczak & Goldstein, 2009; ten Have et al. 2013a) and clinical samples (Altamura et al. 2007, 2008). Although these studies generally stress the importance of recognition and treatment of early-onset disorders in the critical age range of 10–24 years, they are all based on adult samples.
Our aim is to expand on the available literature by describing time-to-treatment and its correlates for any health care professional (hereafter referred to as any care) and secondary mental health care (hereafter referred to as secondary care), for a broad range of mental disorders, in adolescents. We will use data from the Dutch Tracking Adolescents’ Individual Lives Survey (TRAILS), a large community-based cohort study in which participants were followed from childhood into emerging adulthood (Oldehinkel et al. 2015), to do so. The Composite International Diagnostic Interview (CIDI; Kessler & Üstün, 2004) was administered to establish age of onset of mental disorders as well as age of initial treatment contact with any care. Furthermore, data from the Psychiatric Case Register North Netherlands (PCRNN) were used to establish age of initial treatment contact with secondary care.
Methods
Sample
The data used in this study were from TRAILS, a prospective population-based cohort study aimed at explaining the development of mental health from early adolescence into adulthood. The TRAILS sample, response rates and study contents have been described in detail elsewhere (de Winter et al. 2005; Nederhof et al. 2012; Oldehinkel et al. 2015). In short, after the exclusion of children whose schools refused participation (n = 338), and children with serious mental or physical health problems or language difficulties (n = 210), consent to participate in the study was obtained from 2230 (76.0%) out of 2935 eligible children and their parents. Teacher-reported levels of psychopathology did not differ between responding and non-responding children, but boys, children with a lower socioeconomic background, and children with relatively poorer school performance were more likely to be non-responders (de Winter et al. 2005).
We used data from the first and fourth assessment wave, which ran from March 2001 to July 2002 (T1), and from October 2008 to September 2010 (T4). Of the T1 participants (mean age = 11.1 years, s.d. = 0.6 years, 50.8% girls), 84.3% still participated at T4 (n = 1881, mean age = 19.1 years, s.d. = 0.6 years, 52.3% girls). Drop-out was related to being male, low intelligence, low educational level, low parental socioeconomic position (SEP), single-parent families, being bullied and parent-reported behaviour problems (Nederhof et al. 2012). As part of T4, the CIDI was completed by 1584 adolescents (response rate = 71.0%, mean age = 19.3 years, s.d. = 0.6 years, 54.0% girls) (Ormel et al. 2015).
The TRAILS data were linked to the PCRNN (hereafter referred to as the register), which covers secondary child, adolescent and adult mental health care organisations. The catchment area of the register covers 1.7 million inhabitants, and overlaps with the geographic area from which TRAILS participants were recruited. The register, which contained data from 2000 onward, did not include primary (youth) mental health care, private practices and commercial mental health care organisations. Consent to link the TRAILS database to the register was obtained from 1385 CIDI participants and their parents (87.4%). A 95% likelihood matching procedure uniquely identified 342 children with one or more records in the PCRNN (24.7%).
Measures
Lifetime prevalence, age of onset and age of initial treatment contact of DSM-IV disorders (American Psychological Association, 1994) were established using the World Mental Health Organization (WHO) CIDI version 3.0 (Kessler & Üstün, 2004), a structured diagnostic interview that can be administered by trained lay interviewers. Clinical reappraisal studies showed generally good validity of CIDI diagnoses when compared with blinded clinical reappraisal interviews (Haro et al. 2006; Kessler et al. 2009). Disorders included in this study were mood disorders [major depressive disorder (MDD), dysthymic disorder (DYS) and bipolar disorder types I and II (BPD)); anxiety disorders (separation anxiety disorder (SAD), agoraphobia without panic disorder (AGP), generalised anxiety disorder (GAD), obsessive–compulsive disorder (OCD), panic disorder (PDS), social phobia (SO) and specific phobia (SP)]; behaviour disorders [attention deficit hyperactivity disorder (ADHD) and oppositional defiant disorder (ODD)]; and substance dependence [alcohol dependence (ALD) and drug dependence (DRD)]. Organic exclusion criteria, for disorders caused by physical illness, and diagnostic hierarchy rules, for disorders better explained by other disorders, were used where applicable.
Time-to-treatment was defined as the time in years between the age of onset, which is the age at which all DSM-IV diagnostic criteria for the index disorder were met for the first time, and the age of initial treatment contact. The age of initial treatment contact was established in two different ways: with regard to any care as assessed by the CIDI, and with regard to secondary care based on the register. In the CIDI, respondents were asked in each diagnostic section separately whether they had ever talked about the symptoms of the index disorder with a medical doctor or any other health care professional, such as psychologists, clergymen, herbalists and acupuncturists. If acknowledged, respondents were asked their age at first contact. For respondents with a record in the register, the age of initial treatment contact in secondary care was determined based on the date of the first entry in the register. Thus, in case of multiple disorders, the age of initial treatment contact could differ by disorder for any care, while it would be the same for all disorders for secondary care.
The predictor variables included sex (male; female), ethnic minority status (at least one parent born in a non-developed country; both parents born in a developed country), intelligence (IQ < 85; 85 ≤ IQ ≤ 115; IQ > 115) (Silverstein, 1975), parental SEP (lowest 25%; intermediate 50%; highest 25%) (Amone-P'Olak et al. 2010), number of biological parents in the household (none or one; two), disorder severity (mild; severe) (Merikangas et al. 2010; Ormel et al. 2015), age at onset (1–5; 6–10; 11–15; 16–20) and presence of a co-morbid disorder from another diagnostic class (no; yes). Intelligence, parental SEP, and number of biological parents in the household were assessed at T1. A disorder was considered severe if it exceeded, at any time, the impairment or distress thresholds required for the regular CIDI DSM-IV disorders. Co-morbidity was included as a time-varying covariate for each diagnostic class separately.
Analyses
For the analyses, only participants with a CIDI DSM-IV diagnosis were included, which amounted to 42.6% of all CIDI participants (n = 675). Although seemingly high, according to Ormel et al. (2015) the prevalence rates found in TRAILS are comparable with those found in similar studies. Results from prospective studies suggest that actual lifetime prevalence rates are even higher (Moffitt et al. 2010), and that emotional and behavioural problems are nearly universal in nature (Angst et al. 2016). Of the CIDI participants with consent to link their data to the register (n = 1385), 23.2% (n = 321) were included because their first disorder had an onset since 2000, whereas 19.5% (n = 270) were excluded because of a disorder onset before 2000. Cases with a disorder onset before 2000 were more often identified in the register (38 v. 26%, χ12 = 9.7, p < 0.002), and more often had disorders from multiple diagnostic classes (47 v. 28%, χ12 = 25.4, p < 0.001) than cases with a disorder onset since 2000.
The main analyses were divided into two parts. First, time-to-treatment was described using observed proportions of adolescents who made treatment contact at any point in their lives, subdivided into three groups: after initial symptoms and before, in, and after the year of onset of the full-blown disorder. Furthermore, cumulative probability curves of lifetime treatment contact were estimated using survival analysis. These curves were generated for each disorder separately using survival analysis, and showed the estimated cumulative proportion of cases that eventually make treatment contact. The actuarial method was used, because it is better suited than the Kaplan–Meier method for events for which the period rather than the exact date during which an event has occurred is known (c.f. Wang et al. 2005; Bunting et al. 2012). The results were weighted by sex, the Child Behavior Checklist total problems score (Achenbach & Rescorla, 2001), and parental SEP to account for selective non-response (Ormel et al. 2015). Second, Cox regression analyses (Kleinbaum & Klein, 2012) were used to test predictors of time-to-treatment for the four diagnostic classes, and any disorder. Cases without treatment contact were censored at the age of the interview. The analyses were performed separately for any care and for secondary care.
Additionally, we performed two sensitivity analyses on the data regarding any care. First, the Cox regression analyses were repeated while excluding cases with any disorder onset before 2000. This exclusion criterion was also used in the analyses regarding secondary care. Second, the Cox regression analyses for disorder classes were repeated using treatment for any disorder rather than disorder-specific treatment, because the register data could not be linked to any specific disorder class.
All analyses were performed with SPSS 23.0 (IBM Corp, 2015).
Results
Table 1 shows the proportions of lifetime treatment contact, subdivided into treatment contact after initial symptoms and before, in, and after the year of onset of the full-blown disorder, for any care and secondary care, among adolescents with a mental disorder according to the CIDI. The proportion of adolescents with a mental disorder who had lifetime treatment contact with any care by the age of 18–20 varied between 15% for alcohol dependence and 82% for dysthymia. Lifetime treatment rates for secondary care were considerably lower for mood disorders, and higher for substance dependence compared with any care. Notably, for secondary care the proportions of cases with treatment contact before onset of the full-blown disorder were higher than for any care.
Table 1.
Weighteda lifetime treatment contact, subdivided into initial treatment contact after initial symptoms and before, in, or after the year of onset of the full-blown disorder. The left part of the table shows treatment contact with any health care professionalb for all adolescents with a DSM-IV disorder. The right part of the table shows treatment contact with secondary mental health carec for adolescents with a DSM-IV disorder but without any disorder onset before 2000
| Initial treatment contact with any health care professional for all adolescents with a full-blown DSM-IV disorderb | Initial treatment contact with secondary mental health care for adolescents with a full-blown DSM-IV disorder but without any disorder onset before 2000c | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Lifetime | Before year of onset | In year of onset | After year of onset | Lifetime | Before year of onset | In year of onset | After year of onset | |||
| n | % (s.e.) | % (s.e.) | % (s.e.) | % (s.e.) | n | % (s.e.) | % (s.e.) | % (s.e.) | % (s.e.) | |
| Mood disorders | ||||||||||
| Bipolar disorder | 13 | 55.4 (10.5) | 4.3 (4.3) | 21.9 (8.7) | 29.1 (9.6) | 3 | 39.5 (19.2) | 27.4 (17.5) | 0.0 (0.0) | 12.1 (12.9) |
| Major depressive disorder | 159 | 64.5 (3.1) | 7.1 (1.6) | 23.4 (2.7) | 33.9 (3.0) | 48 | 34.5 (4.0) | 10.7 (2.6) | 4.6 (1.8) | 19.3 (3.3) |
| Dysthymia | 22 | 81.7 (7.5) | 14.6 (6.9) | 26.3 (8.6) | 40.9 (9.6) | 1 | 14.1 (14.4) | 0.0 (0.0) | 0.0 (0.0) | 14.1 (14.4) |
| Any mood disorder | 175 | 63.8 (2.9) | 7.2 (1.6) | 23.4 (2.6) | 33.3 (2.9) | 51 | 34.5 (3.9) | 11.5 (2.6) | 4.3 (1.7) | 18.8 (3.2) |
| Anxiety disorders | ||||||||||
| Separation anxiety disorder | 10 | 22.5 (6.2) | 0.0 (0.0) | 10.5 (4.5) | 12.0 (4.8) | 5 | 39.4 (15.0) | 21.9 (12.7) | 8.8 (8.7) | 8.8 (8.7) |
| Agoraphobia without panic disorder | 6 | 37.8 (12.8) | 0.0 (0.0) | 18.5 (10.3) | 19.3 (10.4) | 2 | 65.9 (34.2) | 0.0 (0.0) | 34.9 (34.4) | 31.0 (33.4) |
| Generalised anxiety disorder | 27 | 58.1 (7.4) | 6.5 (3.7) | 21.3 (6.1) | 30.3 (6.9) | 9 | 43.9 (11.5) | 19.8 (9.2) | 14.3 (8.1) | 9.8 (6.9) |
| Obsessive–compulsive disorder | 28 | 30.2 (4.8) | 0.0 (0.0) | 7.6 (2.7) | 22.6 (4.3) | 11 | 28.9 (7.5) | 13.7 (5.7) | 2.4 (2.5) | 12.8 (5.5) |
| Panic disorder | 11 | 43.0 (9.9) | 0.0 (0.0) | 35.5 (9.6) | 7.6 (5.3) | 4 | 45.7 (17.8) | 22.9 (15.0) | 0.0 (0.0) | 22.8 (15.0) |
| Social phobia | 68 | 34.6 (3.4) | 0.0 (0.0) | 4.7 (1.5) | 29.9 (3.3) | 21 | 22.3 (4.3) | 5.0 (2.3) | 0.9 (1.0) | 16.3 (3.9) |
| Specific phobia | 44 | 24.1 (3.2) | 0.0 (0.0) | 2.8 (1.2) | 21.4 (3.1) | 10 | 31.2 (8.4) | 2.6 (2.9) | 3.1 (3.2) | 25.5 (7.9) |
| Any anxiety disorder | 152 | 34.6 (2.3) | 0.0 (0.0) | 5.7 (1.1) | 28.9 (2.2) | 46 | 27.3 (3.4) | 8.9 (2.2) | 1.6 (1.0) | 16.8 (2.9) |
| Behaviour disorders | ||||||||||
| Attention deficit disorder | 37 | 56.5 (6.2) | 3.4 (2.3) | 6.3 (3.1) | 46.8 (6.2) | 2 | 100.0 (0.0) | 62.8 (40.4) | 0.0 (0.0) | 37.2 (40.4) |
| Oppositional defiant disorder | 58 | 41.7 (4.2) | 5.0 (1.9) | 12.1 (2.8) | 24.6 (3.7) | 17 | 38.3 (7.4) | 7.0 (3.9) | 5.5 (3.5) | 25.8 (6.7) |
| Any behaviour disorder | 82 | 45.9 (3.7) | 4.6 (1.6) | 9.9 (2.2) | 31.4 (3.5) | 19 | 41.5 (7.3) | 9.9 (4.4) | 5.3 (3.3) | 26.4 (6.5) |
| Substance dependence | ||||||||||
| Alcohol dependence | 8 | 15.3 (5.1) | 3.7 (2.7) | 6.1 (3.4) | 5.5 (3.3) | 4 | 18.4 (8.1) | 14.6 (7.4) | 3.8 (4.0) | 0.0 (0.0) |
| Drug dependence | 18 | 25.5 (5.2) | 6.6 (2.9) | 4.0 (2.3) | 14.9 (4.2) | 13 | 37.5 (8.2) | 21.0 (6.9) | 2.8 (2.8) | 13.6 (5.8) |
| Any substance dependence | 23 | 20.3 (3.8) | 4.9 (2.1) | 3.3 (1.7) | 12.0 (3.1) | 17 | 30.0 (6.2) | 17.8 (5.2) | 3.4 (2.5) | 8.7 (3.8) |
| Total | ||||||||||
| Any disorder | 328 | 48.3 (1.9) | 2.1 (0.5) | 9.1 (1.1) | 37.2 (1.9) | 87 | 27.6 (2.5) | 9.2 (1.6) | 1.9 (0.8) | 16.5 (2.1) |
Weighted by sex, Child Behavior Checklist cut-offs (normal v. borderline clinical/clinical) and parental SEP. Cases with missing values were assigned the weight 1.
Initial treatment contact for any health care professional based on the Composite International Diagnostic Interview.
Initial treatment contact for secondary mental health care based on the Psychiatric Case Register North Netherlands. Adolescents with any disorder onset before 2000 were excluded because register data were not available before 2000.
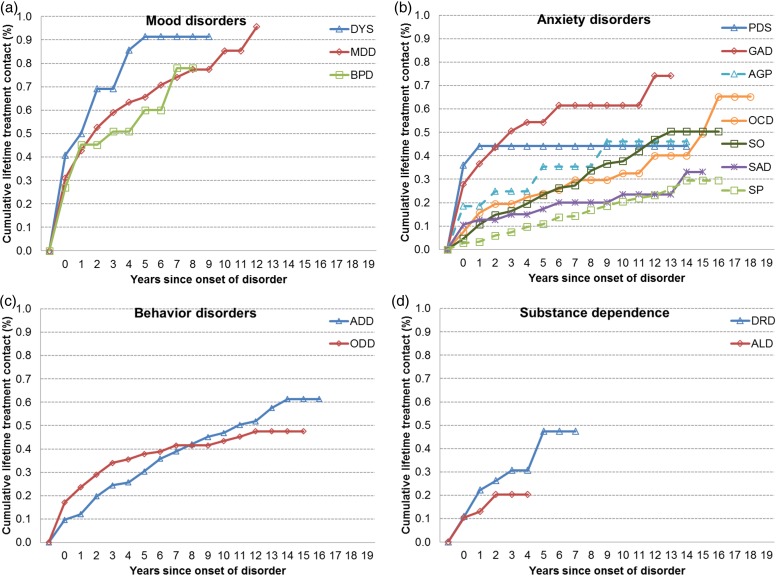
Figure 1 shows for each disorder separately the estimated cumulative proportions of adolescents who will eventually make treatment contact. Three observations stood out. First, the curves showed much variation. For mood (Fig. 1a) and behaviour disorders (Fig. 1c), the curves were comparable within their class, but differed markedly from the other class. The curves for anxiety disorders (Fig. 1b) showed much within-class variation. Curves for substance dependence (Fig. 1d) resembled those for behaviour disorders. Second, disorders with a high probability of treatment contact, such as major depression and generalised anxiety, typically had distinctly higher proportions of initial treatment contact in the first years after onset than disorders with a low probability of treatment contact, such as separation anxiety and specific phobia. Third, time-to-treatment was substantial. Time-to-treatment was shortest for mood disorders, yet the cumulative probability of treatment contact at 2 years after onset was only 50%. A cumulative probability of treatment contact of 50% for anxiety and behaviour disorders was only reached 17 and 12 years after onset, respectively.
Fig. 1.
Weighted cumulative lifetime treatment probabilities with any health care professional for DSM-IV mood disorders (a), anxiety disorders (b), behavior disorders (c), and substance dependence (d). Notes: Weighted by sex, Child Behavior Checklist cut-offs (normal v. borderline clinical/clinical) and parental SEP. Cases with missing values were assigned the weight 1. Probabilities based on life tables using the Actuarial method. Time-to-treatment for disorders with initial treatment contact after initial symptoms and before the year of onset of the respective full-blown disorder set to 0. DYS: dysthymia; MDD: major depressive disorder; BPD: bipolar disorder types I and II; PDS: panic disorder; GAD: generalized anxiety disorder; AGP: agoraphobia; OCD: obsessive-compulsive disorder; SO: social phobia; SAD: separation anxiety disorder; SP: specific phobia; ADD: attention deficit hyperactivity disorder; ODD: oppositional defiant disorder; DRD: drug dependence; ALD: alcohol dependence.
Results from the Cox regression analyses predicting time-to-treatment are shown in Table 2 (any care) and 3 (secondary care). Age of onset predicted time-to-treatment for any disorder for both any care and secondary care. When a disorder had an earlier onset, the time-to-treatment was longer. Models analysing each of the disorder classes separately showed similar effects, although the effects were mostly non-significant for secondary care. Co-morbidity predicted time-to-treatment only in six out of the 32 possible associations reported in Tables 2 and 3; a co-morbid mood disorder in particular predicted a shorter time-to-treatment. Disorder severity predicted shorter time-to-treatment with any care, while it was not associated with secondary care. The effect of parental SEP showed a trend towards shorter time-to-treatment for secondary care for adolescents with parents from a low or middle SEP compared to adolescents with parents from a high SEP.
Table 2.
Cox regression analyses predicting time-to-treatmenta with any health care professionalb for DSM-IV disorders by disorder class and any disorder
| Any health care professionalb | |||||
|---|---|---|---|---|---|
| Mood disorders | Anxiety disorders | Behaviour disorders | Substance dependence | Any disorder | |
| HR (95 %CI) | HR (95 %CI) | HR (95 %CI) | HR (95 %CI) | HR (95 %CI) | |
| Male (ref = female) | 0.74 (0.51–1.06) | 0.90 (0.61–1.31) | 1.64 (0.97–2.77) | 0.96 (0.39–2.36) | 0.88 (0.69–1.13) |
| Ethnic minority (ref = majority) | 1.01 (0.61–1.69) | 0.50 (0.24–1.01) | 0.82 (0.29–2.27) | ‒c | 0.90 (0.59–1.36) |
| Low IQ (ref = high) | 1.46 (0.74–2.85) | 1.72 (0.88–3.39) | 1.52 (0.51–4.53) | 3.27 (0.58–18.43) | 1.37 (0.85–2.21) |
| Middle IQ (ref = high) | 1.29 (0.74–2.23) | 1.36 (0.77–2.40) | 1.73 (0.67–4.48) | 1.74 (0.37–8.20) | 1.31 (0.88–1.93) |
| Low parental SEP (ref = high) | 1.20 (0.74–1.94) | 1.08 (0.64–1.80) | 1.02 (0.53–1.98) | 1.31 (0.42–4.10) | 1.27 (0.91–1.77) |
| Middle parental SEP (ref = high) | 1.39 (0.94–2.06) | 1.04 (0.69–1.58) | 0.64 (0.34–1.18) | 1.30 (0.46–3.70) | 1.18 (0.90–1.57) |
| 0 or 1 biological parents (ref = both) | 0.97 (0.68–1.37) | 1.32 (0.93–1.88) | 1.03 (0.61–1.75) | 0.94 (0.36–2.45) | 1.28* (1.00–1.62) |
| Severe disorder (ref = mild)d | 1.73*** (1.26–2.36) | 1.94*** (1.33–2.85) | 1.98** (1.19–3.29) | ‒d | 1.57*** (1.22–2.03) |
| Age at onset 1–5 (ref = 16–20) | ‒e | 0.15*** (0.07–0.32) | 0.67 (0.35–1.30) | ‒c | 0.20*** (0.12–0.32) |
| Age at onset 6–10 (ref = 16–20) | 0.38** (0.20–0.73) | 0.23*** (0.11–0.47) | 0.41** (0.21–0.80) | ‒f | 0.26*** (0.17–0.42) |
| Age at onset 11–15 (ref = 16–20) | 0.79 (0.55–1.13) | 0.48* (0.24–0.93) | ‒g | 1.78 (0.73–4.32) | 0.58** (0.39–0.87) |
| Co-morbid mood disorder (ref = no)h | ‒i | 2.79*** (1.90–4.09) | 1.82 (0.93–3.56) | 2.43 (0.98–6.03) | 3.09*** (2.35–4.06) |
| Co-morbid anxiety disorder (ref = no)h | 1.01 (0.73–1.39) | ‒i | 0.88 (0.53–1.49) | 2.43 (0.98–6.03) | 1.09 (0.83–1.42) |
| Co-morbid behavior disorder (ref = no)h | 0.85 (0.57–1.29) | 1.49 (0.98–2.25) | ‒i | 0.60 (0.22–1.60) | 1.49** (1.11–2.01) |
| Co-morbid substance dependence (ref = no)h | 1.91* (1.12–3.27) | 0.81 (0.38–1.73) | 1.04 (0.35–3.09) | ‒i | 1.06 (0.65–1.73) |
| Chi-square | 36.3 (13)*** | 125.9 (14)*** | 24.9 (13)* | 14.9 (10) | 276.2 (15)*** |
| n events | 172 | 145 | 72 | 23 | 314 |
| n censored | 96 | 284 | 93 | 86 | 347 |
| n total | 268 | 429 | 165 | 109 | 661 |
DSM-IV, Diagnostic and Statistical Manual of Mental Disorders, fourth edition; HR, Hazard ratio; 95% CI, 95% confidence interval; IQ, intelligence quotient; SEP, socio-economic position.
Time-to-treatment for disorders with initial treatment contact after initial symptoms and before the year of onset of the respective full-blown disorder set to 0.
Lifetime treatment contact and age of initial treatment contact for any health care professional based on the Composite International Diagnostic Interview.
Covariate excluded due to insufficient cases.
All substance dependence diagnoses were considered severe.
Combined with age of onset 6–10 years due to insufficient cases.
Combined with age of onset 11–15 years due to insufficient cases.
Combined with age of onset 16–20 years (reference category) due to insufficient cases in the reference category.
Time-dependent covariate.
Disorder class is the dependent variable.
*p < 0.05 **p < 0.01 ***p < 0.001.
Table 3.
Cox regression analyses predicting time-to-treatmenta with secondary mental health careb for DSM-IV disorders by disorder class and any disorder for adolescents without any disorder onset before 2000
| Secondary mental health careb | |||||
|---|---|---|---|---|---|
| Mood disorders | Anxiety disorders | Behaviour disorders | Substance dependence | Any disorder | |
| HR (95% CI) | HR (95% CI) | HR (95% CI) | HR (95% CI) | HR (95% CI) | |
| Male (ref = female) | 1.31 (0.66–2.63) | 0.73 (0.33–1.62) | 1.54 (0.35–6.73) | 1.81 (0.49–6.76) | 1.09 (0.67–1.77) |
| Ethnic minority (ref = majority) | 0.53 (0.15–1.91) | ‒c | 23.12* (1.32–403.92) | ‒c | 0.89 (0.35–2.30) |
| Low IQ (ref = high) | 1.84 (0.59–5.74) | 1.12 (0.38–3.29) | 1.19 (0.17–8.17) | 0.90 (0.12–6.78) | 1.81 (0.77–4.25) |
| Middle IQ (ref = high) | 1.15 (0.43–3.05) | 0.96 (0.38–2.40) | 0.51 (0.09–2.75) | 0.47 (0.10–2.13) | 1.12 (0.55–2.29) |
| Low parental SEP (ref = high) | 1.71 (0.65–4.48) | 3.08 (0.98–9.70) | 6.82 (0.69–67.49) | 3.32 (0.63–17.45) | 1.66 (0.81–3.41) |
| Middle parental SEP (ref = high) | 2.09 (0.96–4.53) | 3.49* (1.25–9.74) | 5.49 (0.59–51.45) | 1.47 (0.39–5.53) | 1.85* (1.03–3.32) |
| 0 or 1 biological parents (ref = both) | 1.50 (0.78–2.90) | 1.54 (0.78–3.05) | 1.55 (0.40–5.99) | 0.61 (0.18–2.14) | 1.42 (0.88–2.28) |
| Severe disorder (ref = mild)d | 1.39 (0.78–2.50) | 1.44 (0.69–3.03) | 0.70 (0.21–2.38) | ‒d | 1.20 (0.71–2.02) |
| Age at onset 1–5 (ref = 16–20) | ‒e | ‒e | ‒e | ‒e | ‒e |
| Age at onset 6–10 (ref = 16–20) | 0.17 (0.02–1.33) | 0.41 (0.12–1.45) | 0.54 (0.11–2.59) | ‒f | 0.34** (0.15–0.77) |
| Age at onset 11–15 (ref = 16–20) | 0.71 (0.37–1.37) | 0.54 (0.20–1.47) | ‒g | 0.54 (0.13–2.30) | 0.58 (0.31–1.09) |
| Co-morbid mood disorder (ref = no)h | ‒i | 4.30*** (2.23–8.28) | 1.65 (0.38–7.04) | 2.35 (0.72–7.60) | 2.13** (1.24–3.67) |
| Co-morbid anxiety disorder (ref = no)h | 1.82 (0.99–3.33) | ‒i | 1.09 (0.29–4.06) | 1.60 (0.45–5.67) | 1.18 (0.69–2.04) |
| Co-morbid behavior disorder (ref = no)h | 1.54 (0.65–3.67) | 1.54 (0.63–3.75) | ‒i | 2.15 (0.60–7.70) | 1.60 (0.79–3.23) |
| Co-morbid substance dependence (ref = no)h | 1.63 (0.59–4.47) | 1.89 (0.64–5.59) | 1.31 (0.17–10.12) | ‒i | 1.40 (0.62–3.14) |
| Chi-square | 20.3 (13) | 63.1 (12)*** | 14.9 (12) | 10.0 (10) | 41.3 (14)*** |
| n events | 50 | 44 | 17 | 16 | 83 |
| n censored | 89 | 117 | 27 | 37 | 216 |
| n total | 139 | 161 | 44 | 53 | 299 |
DSM-IV, Diagnostic and Statistical Manual of Mental Disorders, fourth edition; HR, Hazard ratio; 95%CI, 95% confidence interval; IQ, intelligence quotient; SEP, socio-economic position.
Time-to-treatment for disorders with initial treatment contact before the year of onset of the respective disorder set to 0.
Lifetime treatment contact and age of initial treatment contact for secondary mental health care based on the Psychiatric Case Register North Netherlands.
Covariate excluded due to insufficient cases.
All substance dependence diagnoses were considered severe.
No cases, because adolescents with any disorder onset before 2000 were excluded.
Combined with age of onset 11–15 years due to insufficient cases.
Combined with age of onset 16–20 years (reference category) due to insufficient cases in the reference category.
Time-dependent covariate.
Disorder class is the dependent variable.
*p < 0.05 **p < 0.01 ***p < 0.001.
Two sensitivity analyses for any care were performed (available as online supplementary material). When excluding adolescents with any disorder onset before 2000 (appendix table 1), age at onset effects were often no longer statistically significant, although hazard ratios remained similar, and disorder severity no longer significantly predicted a shorter time-to-treatment for anxiety and behaviour disorders. When considering any treatment contact rather than disorder-specific treatment contact (appendix table 2), co-morbidity more often predicted a shorter time-to-treatment.
Conclusion
The time-to-treatment with any care for adolescents varied considerably across disorders, but was substantial even for mood disorders, which in general showed the shortest time-to-treatment. Cox regression analyses showed that the time-to-treatment was longer as the onset was earlier. Furthermore, the time-to-treatment was shorter for severe compared with mild disorders, and for disorders with a co-morbid mood disorder. These results were replicated for secondary care, with the exception that disorder severity was not related to time-to-treatment.
Limitations
The results need to be interpreted considering three limitations. The first limitation is recall bias (e.g., Wang et al. 2005; Altamura et al. 2010). Respondents may forget about or downplay mental health problems for which they did not seek treatment, which would lead to overestimated proportions of treatment contact. Recall bias may also cause respondents to remember past events as more recent than they actually took place (telescoping). Since onset usually occurs years before initial treatment contact, the probability of telescoping is likely larger for age of onset than for age of initial treatment contact. The time-to-treatment is therefore possibly underestimated. Our study, however, had two advantages over previous studies (Wang et al. 2004; Bruffaerts et al. 2007; Bunting et al. 2012; ten Have et al. 2013a), which probably limited recall bias. First, the diagnostic interview was administered at the age of 18–20 years rather than up to 60 years and older, so the recall period was much shorter than in previous studies. Second, administrative records are considered more reliable than self-reported treatment seeking (Wang et al. 2004; Olfson et al. 2012).
The second limitation is that most predictors of time-to-treatment were not assessed over time. Intelligence, parental SEP, and the number of biological parents in the household were only assessed when the participants were 10–12 years old. For the majority of adolescents, however, these are likely to be stable factors. Furthermore, disorder severity could only be assessed lifetime, rather than at the moment of initial treatment contact. Therefore, assuming symptom recognition and treatment seeking are more likely when disorders are severe than when they are mild (Merikangas et al. 2011; ten Have et al. 2013b) the effect of disorder severity on time-to-treatment could have been underestimated.
The third limitation of this study concerns the coverage of the PCRNN. First, this register does not cover primary (youth) mental health care, private practices, and commercial mental health care organisations. Nevertheless, the register still covers an estimated 75% of all mental health treatment trajectories for children and adolescents in secondary care (Jörg et al. 2015). Second, this register does not include data prior to 2000, which corresponds approximately to the age of ten in our sample. Both lead to an underestimation of the proportion of secondary care users. Additionally, time-to-treatment for secondary care is likely to be underestimated considerably, because cases with early-onset disorders, who typically had the longest time-to-treatment, had to be excluded from the secondary care analyses.
Time-to-treatment
A comparison between our findings on time-to-treatment for mental disorders in adolescents and prior studies conducted in adults yields two main observations. First, the time-to-treatment was shorter in our adolescent sample than in comparable adult samples (Wang et al. 2004, 2005, 2007; Bruffaerts et al. 2007; ten Have et al. 2013a). However, estimates of time-to-treatment are highly dependent on follow-up time, which was substantially shorter in our sample of adolescents than in the adult samples. Second, the patterns of time-to-treatment in adolescents are remarkably similar to those found in Dutch (ten Have et al. 2013a), Belgian (Bruffaerts et al. 2007), Northern Irish (Bunting et al. 2012), and American (Wang et al. 2005) adults. For instance, mood disorders are characterised by high proportions of lifetime treatment contact and a relatively short time-to-treatment in all ages, while within the class of anxiety disorders initial treatment contact is made most and fastest for panic disorder, and least and slowest for specific phobia. Although differences among countries do exist (Wang et al. 2007), we expect to find highly similar patterns of time-to-treatment in adolescents from other countries as well.
Predictors of time-to-treatment
Following studies using adult community samples (Kessler et al. 1998; Wang et al. 2004, 2005, 2007; Bruffaerts et al. 2007; Korczak & Goldstein, 2009; ten Have et al. 2013a), we found that time-to-treatment is longer when disorders have an onset earlier in life. We were able to confirm a robust association between earlier onset and a longer time-to-treatment. An important reason for this age of onset-effect is that children's access to mental health care depends on recognition and help-seeking by their parents or teachers (Wang et al. 2005; Bruffaerts et al. 2007; ten Have et al. 2013a). Symptoms from early-onset disorders may not be recognised because they may be considered as being a part of a child's identity, are not severe enough, or are not disturbing enough to the social environment (Wang et al. 2005; ten Have et al. 2013a; Jörg et al. 2015), potentially resulting in unmet need. The development of coping strategies may mitigate or even eliminate the need for treatment, at least in the short term, until adolescents enter a life phase during which they have to be more self-reliant. In adults, early-onset disorders have been associated with a time-to-treatment of decades (Kessler et al. 1998; Christiana et al. 2000; Wang et al. 2004, 2005; Bunting et al. 2012). This at least raises the questions of how potentially harmful a long time-to-treatment for early-onset disorders is, and whether prevention and early intervention programmes aimed specifically at children and adolescents should be employed (Merikangas et al. 2010; Bunting et al. 2012; de Girolamo et al. 2012; Thornicroft, 2012; Ghio et al. 2014).
The current study added to the literature by including severity and co-morbidity as predictors of time-to-treatment. Co-morbid mood disorders most often predicted shorter time-to-treatment, but co-morbidity from other classes was mostly unrelated to time-to-treatment for any care. Maybe only co-morbid disorders with a short time-to-treatment themselves, such as dysthymia and panic disorder, accelerate the time-to-treatment for other disorders, as opposed to for instance social and specific phobia (Olfson et al. 2012). Alternatively, perhaps the onset of a co-morbid disorder prompts treatment seeking for the co-morbid disorder, rather than for the index disorder (Chapman et al. 2015). That co-morbidity tended to be a stronger predictor for secondary care than for any care, was probably because treatment contact in secondary care could not be attributed to any disorder in particular.
Disorder severity, operationalised in this study as high levels of impairment or distress, predicted shorter time-to-treatment for any care. This is largely in line with a previous finding that symptoms of functional impairment predicted shorter time-to-treatment for alcohol dependence, whereas the number of dependence symptoms did not (Chapman et al. 2015). Unexpectedly, disorder severity was not associated with time-to-treatment for secondary care. Adolescents whose first disorder had an onset approximately before the age of 10 did not have a severe disorder more often than did adolescents whose first disorder had an onset later in life. They did have treatment contact with secondary care more often, and they showed more signs of multimorbidity. This might indicate that the time-to-treatment with secondary care is reduced by the complexity of psychopathology, rather than the levels of impairment or distress.
Secondary care
The results for second are care were largely similar to those for any care. The sensitivity analyses for any care shared many characteristics with the Cox regression analyses for secondary care, and lead to the same substantive conclusions. We therefore think that the latter suffered from reduced statistical power, but not reduced precision of estimates.
An interesting finding was that time-to-treatment for secondary care was shorter for adolescents from a low or middle than for adolescents from a high socioeconomic background, while no such pattern was found for any care. As a high socioeconomic background has been associated with more parent reported specialist mental health care use (Amone-P'Olak et al. 2010), parents from a high socioeconomic background may prefer to send their children to other types of care, such as private practices.
Concluding remark
This study is, as far as we know, the first to describe time-to-treatment and its correlates for lifetime mental disorders in a large cohort of adolescents. The differentiation between any care and secondary care, and the inclusion of disorder severity and co-morbidity as predictors of time-to-treatment add further relevance to this study. Time-to-treatment is already substantial in adolescence, and shows patterns highly similar to those observed in adult samples, which confirms the importance of focusing on childhood and adolescence for the reduction of time-to-treatment. Next to age of onset, only disorder severity and co-morbidity are consistently related to time-to-treatment. This suggests that the characteristics of psychopathology are more important correlates of time-to-treatment than the background variables that are generally included yet hardly produce consistent findings, such as family characteristics. For a better comprehension of time-to-treatment, future studies should ideally address theoretical explanations of time-to-treatment, such as parental recognition, coping and unmet need, as well as the outcomes of time-to-treatment, such as social functioning and educational attainment.
Acknowledgements
This research is part of the TRacking Adolescents’ Individual Lives Survey (TRAILS). Participating centres of TRAILS include the University Medical Center and University of Groningen, the Erasmus University Medical Center Rotterdam, the University of Utrecht, the Radboud Medical Center Nijmegen, and the Parnassia Bavo group, all in the Netherlands. We are grateful to everyone who participated in this research or worked on this project to make it possible.
Financial Support
TRAILS has been financially supported by various grants from the Netherlands Organization for Scientific Research NWO (Medical Research Council program grant GB-MW 940-38-011; ZonMW Brainpower grant 100-001-004; ZonMw Risk Behavior and Dependence grants 60-60600-97-118; ZonMw Culture and Health grant 261-98-710; Social Sciences Council medium-sized investment grants GB-MaGW 480-01-006 and GB-MaGW 480-07-001; Social Sciences Council project grants GB-MaGW 452-04-314 and GB-MaGW 452-06-004; NWO large-sized investment grant 175.010.2003.005; NWO Longitudinal Survey and Panel Funding 481-08-013 and 481-11-001), the Dutch Ministry of Justice (WODC), the European Science Foundation (EuroSTRESS project FP-006), Biobanking and Biomolecular Resources Research Infrastructure BBMRI-NL (CP 32), and the participating universities.
Conflict of Interest
None.
Ethical Standard
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
Supplementary material
For supplementary material accompanying this paper visit http://dx.doi.org/10.1017/S2045796016000226.
click here to view supplementary material
References
- Achenbach TM, Rescorla LA (2001). Manual for the ASEBA School-Age Forms & Profiles. University of Vermont, Research Center for Children, Youth, & Families: Burlington, VT. [Google Scholar]
- Altamura AC, Dell'Osso B, Mundo E, Dell'Osso L (2007). Duration of untreated illness in major depressive disorder: a naturalistic study. International Journal of Clinical Practice 61, 1697–1700. [DOI] [PubMed] [Google Scholar]
- Altamura AC, Dell'Osso B, Vismara S, Mundo E (2008). May duration of untreated illness influence the long-term course of major depressive disorder? European Psychiatry 23, 92–96. [DOI] [PubMed] [Google Scholar]
- Altamura AC, Buoli M, Albano A, Dell'Osso B (2010). Age at onset and latency to treatment (duration of untreated illness) in patients with mood and anxiety disorders: a naturalistic study. International Clinical Psychopharmacology 25, 172–179. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association (1994). Diagnostic and Statistical Manual of Mental Disorders, 4th edn APA: Washington, DC. [Google Scholar]
- Amone-P'Olak K, Ormel J, Oldehinkel AJ, Reijneveld SA, Verhulst FC, Burger H (2010). Socioeconomic position predicts specialty mental health service use independent of clinical severity: the TRAILS study. Journal of the American Academy of Child and Adolescent Psychiatry 49, 647–655. [DOI] [PubMed] [Google Scholar]
- Angst J, Paksarian D, Cui L, Merikangas KR, Hengartner MP, Ajdacic-Gross V, Rössler W (2016). The epidemiology of common mental disorders from age 20 to 50: results from the prospective Zurich Cohort Study. Epidemiology and Psychiatric Sciences 25, 24–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruffaerts R, Bonnewyn A, Demyttenaere K (2007). Delays in seeking treatment for mental disorders in the Belgian general population. Social Psychiatry and Psychiatric Epidemiology 42, 937–944. [DOI] [PubMed] [Google Scholar]
- Bunting BP, Murphy SD, O'Neill SM, Ferry FR (2012). Lifetime prevalence of mental health disorders and delay in treatment following initial onset: evidence from the Northern Ireland Study of Health and Stress. Psychological Medicine 42, 1727–1739. [DOI] [PubMed] [Google Scholar]
- Chapman C, Slade T, Hunt C, Teesson M (2015). Delay to first treatment contact for alcohol use disorder. Drug and Alcohol Dependence 147, 116–121. [DOI] [PubMed] [Google Scholar]
- Christiana JM, Gilman SE, Guardino M, Mickelson K, Morselli PL, Olfson M, Kessler RC (2000). Duration between onset and time of obtaining initial treatment among people with anxiety and mood disorders: an international survey of members of mental health patient advocate groups. Psychological Medicine 30, 693–703. [DOI] [PubMed] [Google Scholar]
- Costello EJ, Maughan B (2015). Annual research review: optimal outcomes of child and adolescent mental illness. Journal of Child Psychology and Psychiatry 56, 324–341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Girolamo G, Dagani J, Purcell R, Cocchi A, McGorry PD (2012). Age of onset of mental disorders and use of mental health services: needs, opportunities and obstacles. Epidemiology and Psychiatric Sciences 21, 47–57. [DOI] [PubMed] [Google Scholar]
- de Graaf R, ten Have M, van Gool C, van Dorsselaer S (2012). Prevalence of mental disorders and trends from 1996 to 2009. Results from the Netherlands Mental Health Survey and Incidence Study-2. Social Psychiatry and Psychiatric Epidemiology 47, 203–213. [DOI] [PubMed] [Google Scholar]
- Dell'Osso B, Altamura AC (2010). Duration of untreated psychosis and duration of untreated illness: new vistas. CNS Spectrums 15, 238–246. [DOI] [PubMed] [Google Scholar]
- de Winter AF, Oldehinkel AJ, Veenstra R, Brunnekreef JA, Verhulst FC, Ormel J (2005). Evaluation of non-response bias in mental health determinants and outcomes in a large sample of pre-adolescents. European Journal of Epidemiology 20, 173–181. [DOI] [PubMed] [Google Scholar]
- Ghio L, Gotelli S, Marcenaro M, Amore M, Natta W (2014). Duration of untreated illness and outcomes in unipolar depression: a systematic review and meta-analysis. Journal of Affective Disorders 152–154, 45–51. [DOI] [PubMed] [Google Scholar]
- Haro JM, Arbabzadeh-Bouchez S, Brugha TS, De Girolamo G, Guyer ME, Jin R, Lepine JP, Mazzi F, Reneses B, Vilagut G, Sampson NA, Kessler RC (2006). Concordance of the Composite International Diagnostic Interview Version 3.0 (CIDI 3.0) with standardized clinical assessments in the WHO World Mental Health Surveys. International Journal of Methods in Psychiatric Research 15, 167–180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- IBM Corp (2015). IBM SPSS Statistics for Windows, Version 23.0. IBM Corp: Armonk, NY, 23.0. [Google Scholar]
- Jansen DEMC, Wiegersma P, Ormel J, Verhulst FC, Vollebergh WAM, Reijneveld SA (2013). Need for mental health care in adolescents and its determinants: the TRAILS Study. European Journal of Public Health 23, 236–241. [DOI] [PubMed] [Google Scholar]
- Jörg F, Visser E, Ormel J, Reijneveld SA, Hartman CA, Oldehinkel AJ (2015). Mental health care use in adolescents with and without mental disorders. European Child and Adolescent Psychiatry, 1–8. Advance online publication. doi: 10.1007/s00787-015-0754-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Üstün TB (2004). The World Mental Health (WMH) Survey Initiative version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI). International Journal or Methods in Psychiatric Research 13, 93–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Olfson M, Berglund PA (1998). Patterns and predictors of treatment contact after first onset of psychiatric disorders. American Journal of Psychiatry 155, 62–69. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE (2005a). Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry 62, 593–602. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Demler O, Frank RG, Olfson M, Pincus HA, Walters EE, Wang P, Wells KB, Zaslavsky AM (2005b). Prevalence and Treatment of Mental Disorders, 1990 to 2003. New England Journal of Medicine 352, 2515–2523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Amminger GP, Aguilar-Gaxiola S, Alonso J, Lee S, Ustün TB (2007). Age of onset of mental disorders: a review of recent literature. Current Opinion in Psychiatry 20, 359–364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Avenevoli S, Green J, Gruber MJ, Guyer M, He Y, Jin R, Kaufman J, Sampson NA, Zaslavsky AM (2009). National comorbidity survey replication adolescent supplement (NCS-A): III. Concordance of DSM-IV/CIDI diagnoses with clinical reassessments. Journal of the American Academy of Child and Adolescent Psychiatry 48, 386–399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kisely S, Scott A, Denney J, Simon G (2006). Duration of untreated symptoms in common mental disorders: association with outcomes. British Journal of Psychiatry 189, 79–80. [DOI] [PubMed] [Google Scholar]
- Kleinbaum DG, Klein M (2012). Survival Analysis, 3rd edn Springer-Verlag New York: New York, NY. [Google Scholar]
- Korczak DJ, Goldstein BI (2009). Childhood onset major depressive disorder: course of illness and psychiatric comorbidity in a community sample. Journal of Pediatrics 155, 118–123. [DOI] [PubMed] [Google Scholar]
- Marshall M, Lewis S, Lockwood A, Drake R, Jones P, Croudace T (2005). Association between duration of untreated psychosis and outcome in cohorts of first-episode patients. A systematic review. Archives of General Psychiatry 62, 975–983. [DOI] [PubMed] [Google Scholar]
- Merikangas KR, He J-P, Burstein M, Swanson SA, Avenevoli S, Cui L, Benjet C, Georgiades K, Swendsen J (2010). Lifetime prevalence of mental disorders in U.S. adolescents: results from the National Comorbidity Survey Replication – Adolescent Supplement (NCS-A). Journal of the American Academy of Child and Adolescent Psychiatry 49, 980–989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merikangas KR, He J-P, Burstein M, Swendsen J, Avenevoli S, Case B, Georgiades K, Heaton L, Swanson S, Olfson M (2011). Service utilization for lifetime mental disorders in U.S. adolescents: results of the National Comorbidity Survey-Adolescent Supplement (NCS-A). Journal of the American Academy of Child and Adolescent Psychiatry 50, 32–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moffitt TE, Caspi A, Taylor A, Kokaua J, Milne BJ, Polanczyk G, Poulton R (2010). How common are common mental disorders? Evidence that lifetime prevalence rates are doubled by prospective versus retrospective ascertainment. Psychological Medicine 40, 899–909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nederhof E, Jörg F, Raven D, Veenstra R, Verhulst FC, Ormel J, Oldehinkel AJ (2012). Benefits of extensive recruitment effort persist during follow-ups and are consistent across age group and survey method. The TRAILS study. BMC Medical Research Methodology 12, 93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oldehinkel AJ, Rosmalen JGM, Buitelaar JK, Hoek HW, Ormel J, Raven D, Reijneveld SA, Veenstra R, Verhulst FC, Vollebergh WAM, Hartman CA (2015). Cohort profile update: the TRacking Adolescents’ Individual Lives Survey (TRAILS). International Journal of Epidemiology 44, 76–76n. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olfson M, Liu S-M, Grant BF, Blanco C (2012). Influence of comorbid mental disorders on time to seeking treatment for major depressive disorder. Medical Care 50, 227–232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ormel J, Raven D, van Oort F, Hartman CA, Reijneveld SA, Veenstra R, Vollebergh WAM, Buitelaar J, Verhulst FC, Oldehinkel AJ (2015). Mental health in Dutch adolescents: a TRAILS report on prevalence, severity, age of onset, continuity and co-morbidity of DSM disorders. Psychological Medicine 45, 345–360. [DOI] [PubMed] [Google Scholar]
- Perkins DO, Gu H, Boteva K, Lieberman JA (2005). Relationship between duration of untreated psychosis and outcome in first-episode schizophrenia: a critical review and meta-analysis. American Journal of Psychiatry 162, 1785–1804. [DOI] [PubMed] [Google Scholar]
- Reef J, van Meurs I, Verhulst FC, van der Ende J (2010). Children's problems predict adults’ DSM-IV disorders across 24 years. Journal of the American Academy of Child and Adolescent Psychiatry 49, 1117–1124. [DOI] [PubMed] [Google Scholar]
- Silverstein AB (1975). Validity of WISC-R short forms. Journal of Clinical Psychology 31, 696–697. [Google Scholar]
- ten Have M, de Graaf R, van Dorsselaer S, Beekman A (2013a). Lifetime treatment contact and delay in treatment seeking after first onset of a mental disorder. Psychiatric Services 64, 981–989. [DOI] [PubMed] [Google Scholar]
- ten Have M, Nuyen J, Beekman A, de Graaf R (2013b). Common mental disorder severity and its association with treatment contact and treatment intensity for mental health problems. Psychological Medicine 43, 2203–2213. [DOI] [PubMed] [Google Scholar]
- Thornicroft G (2012). No time to lose: onset and treatment delay for mental disorders. Epidemiology and Psychiatric Sciences 21, 59–61. [DOI] [PubMed] [Google Scholar]
- Wang PS, Berglund PA, Olfson M, Kessler RC (2004). Delays in initial treatment contact after first onset of a mental disorder. Health Services Research 39, 393–415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang PS, Berglund P, Olfson M, Pincus HA, Wells KB, Kessler RC (2005). Failure and delay in initial treatment contact after first onset of mental disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry 62, 603–613. [DOI] [PubMed] [Google Scholar]
- Wang PS, Angermeyer M, Borges G, Bruffaerts R, Tat Chiu W, de Girolamo G, Fayyad J, Gureje O, Haro JM, Huang Y, Kessler RC, Kovess V, Levinson D, Nakane Y, Oakley Brown MA, Ormel J, Posada-Villa J, Aguilar-Gaxiola S, Alonso J, Lee S, Heeringa S, Pennell B-E, Chatterji S, Ustün TB (2007). Delay and failure in treatment seeking after first onset of mental disorders in the World Health Organization's World Mental Health Survey Initiative. World Psychiatry 6, 177–185. [PMC free article] [PubMed] [Google Scholar]
- Whiteford HA, Degenhardt L, Rehm J, Baxter AJ, Ferrari AJ, Erskine HE, Charlson FJ, Norman RE, Flaxman AD, Johns N, Burstein R, Murray CJL, Vos T (2013). Global burden of disease attributable to mental and substance use disorders: findings from the Global Burden of Disease Study 2010. Lancet 6736, 1–12. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
For supplementary material accompanying this paper visit http://dx.doi.org/10.1017/S2045796016000226.
click here to view supplementary material