Abstract
Background.
The purpose of this paper is to describe variation, over the months of the year, in major depressive episode (MDE) prevalence. This is an important aspect of the epidemiological description of MDE, and one that has received surprisingly little attention in the literature. Evidence of seasonal variation in MDE prevalence has been weak and contradictory. Most studies have sought to estimate the prevalence of seasonal affective disorder using cut-points applied to scales assessing mood seasonality rather than MDE. This approach does not align with modern classification in which seasonal depression is a diagnostic subtype of major depression rather than a distinct category. Also, some studies may have lacked power to detect seasonal differences. We addressed these limitations by examining the month-specific occurrence of conventionally defined MDE and by pooling data from large epidemiological surveys to enhance precision in the analysis.
Method.
Data from two national survey programmes (the National Population Health Survey and the Canadian Community Health Survey) were used, providing ten datasets collected between 1996 and 2013, together including over 500,000. These studies assessed MDE using a short form version of the Composite International Diagnostic Interview (CIDI) for major depression, with one exception being a 2012 survey that used a non-abbreviated version of the CIDI. The proportion of episodes occurring in each month was evaluated using items from the diagnostic modules and statistical methods addressing complex design features of these trials. Overall month-specific pooled estimates and associated confidence intervals were estimated using random effects meta-analysis and a gradient was assessed using a meta-regression model that included a quadratic term.
Results.
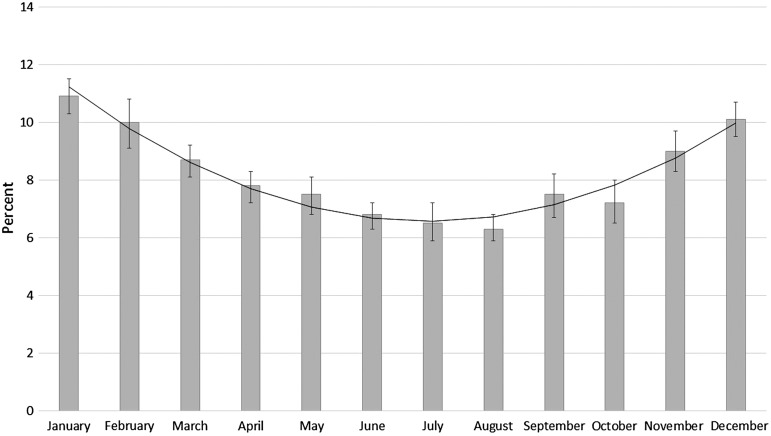
There was considerable sampling variability when the month-specific proportions were estimated from individual survey datasets. However, across the various datasets, there was sufficient homogeneity to justify the pooling of these estimated proportions, producing large gains in precision. Seasonal variation was clearly evident in the pooled data. The highest proportion of episodes occurred in December, January and February and the lowest proportions occurred in June, July and August. The proportion of respondents reporting MDE in January was 70% higher than August, suggesting an association with implications for health policy. The pattern persisted with stratification for age group, sex and latitude.
Conclusions.
Seasonal effects in MDE may have been obscured by small sample sizes in prior studies. In Canada, MDE has clear seasonal variation, yet this is not addressed in the planning of services. These results suggest that availability of depression treatment should be higher in the winter than the summer months.
Key words: Epidemiologic studies, major depressive episode, meta-analysis, meta-regression, seasonal, seasonal affective disorder, winter depression
The literature contains many attempts to estimate the prevalence of seasonal affective disorder (SAD). A systematic review of this literature published by Magnusson in 2000 concluded that seasonal variation in mood had been ‘documented thoroughly’ (Magnusson, 2000) but most of the studies identified used a measure of seasonal mood variability, or seasonality, the Seasonal Pattern Assessment Questionnaire (SPAQ) (Mersch et al. 2004) rather than an assessment of major depressive episode (MDE). Longitudinal studies have generally found that only a minority of SAD cases have a persistent seasonal pattern (Sakamoto et al. 1995; Thompson et al. 1995; Schwartz et al. 1996; Cobb et al. 2014). Furthermore, the paradigmatic treatment for SAD (light therapy) is not specific to SAD but is also efficacious in non-seasonal MDE) (Tuuanainen et al. 2004; Young, 2011). Consequently, and despite arguments encouraging its inclusion (Rosenthal, 2009), SAD does not appear in DSM-5. Rather, the seasonal pattern remains a specification code for the course of major depressive disorder (and bipolar disorder). Rosenthal's original definition required a history of major affective disorder and at least two consecutive years in which depression developed during the fall or winter and then remitted during the following spring or summer (Rosenthal et al. 1984). This definition is broader than the course specifier in DSM-5 (American Psychiatric Association, 2013), which requires that seasonal episodes (those having onset and remission at characteristic times of the year) occur in at least two consecutive years without non-seasonal episodes and also requires that, over the lifetime, seasonal episodes ‘substantially outnumber’ non-seasonal ones. With the DSM-5 specifier, seasonal episodes judged secondary to seasonal stressors (e.g. unemployment) are not counted. DSM-5 does not require fall or winter onset.
Published estimates of SAD prevalence, usually based on the SPAQ, are organised differently than the nosology used in clinical practice since the SPAQ assesses retrospectively reported seasonality rather than MDE prevalence. Prevalence estimates based on such definitions do not provide a complete description of the epidemiological influence of season on MDE prevalence.
Another set of studies have examined seasonal variation in symptom levels using conventional instruments, with or without SPAQ ratings. Such studies, as a group, have produced inconsistent results. For example, one of the largest studies (Oyane et al. 2008) found that seasonality, as assessed by global seasonality scores from the SPAQ, was associated with elevated depressive symptom ratings irrespective of the month in which the interviews were conducted. Elevated symptoms (measured using the Hospital Anxiety and Depression Scale) were identified in the November to March interval, but only in a subgroup of respondents having low to moderate levels of seasonality. Michalak et al. (2004) used data from the ODIN study to examine seasonal variation in Beck Depression Inventory ratings. No consistent evidence of substantial seasonal variation was found in any of the participating European countries. Winthorst et al. (2011) analysed data from the NESDA study in the Netherlands, examining cross-sectional ratings collected using a variety of instruments. No prominent or consistent seasonal patterns were found. While most studies have used cross-sectional data and were thus limited in their analysis to an examination of between person effects, Kerr et al. (2013) used longitudinal data from two panel studies (called the Oregon Youth Study and the Family Transitions Project) to also examine within-person patterns. They found statistically significant within-person seasonal variation, but with a small effect size (less than half a point on the CES-D rating scale). The effect was visually imperceptable when plotted across the full range of scores.
A series of national surveys conducted by Statistics Canada since the mid-1990s examined MDE prevalence in the Canadian household population. The instrument used to assess MDE in most of these surveys was the Composite International Diagnostic Interview short form for major depression (CIDI-SFMD) (Kessler et al. 1998) with the exception of one survey conducted in 2002 (the Canadian Community Health Survey 1.2, or CCHS 1.2) which used a version of the WHO Mental Health (WMH)-CIDI (Kessler & Ustun, 2004). The CIDI-SFMD was developed using data from the National Comorbidity Survey using a receiver operator analysis designed to detect a subset of CIDI items most highly predictive of MDE. If five symptom-based CIDI-SFMD items are endorsed, the instrument has a 90% positive predictive value for MDE (Kessler et al. 1998). The WMH-CIDI is currently the most widely used fully structured diagnostic instrument in psychiatric epidemiology. Although the WMH-CIDI is more comprehensive, the two instruments produce comparable estimates although prevalence estimates arising from the CIDI-SFMD may be slightly higher (Patten et al. 2014). Both instruments included items asking about the month of occurrence of MDE. The Statistics Canada surveys had similar sampling frames, based largely on an area frame from an ongoing national survey programme called the Labour Force Survey. This, combined with the similarity of measurement strategies suggests sufficient methodological homogeneity to justify pooling of the data. This provides an opportunity to overcome the sample size limitations and imprecision of prior estimates while also applying a conventional definition of MDE to the question of seasonal variation.
The objective of this study was to precisely estimate the proportion of MDE occurring in specific months of the year in order to more decisively determine the existence of seasonal variation and, if present, to describe the magnitude of seasonal effects on MDE.
Material and methods
Data sources
This study used data from two sources. The first was the National Population Health Survey (NPHS) (Statistics Canada, 2013), a longitudinal survey that began with a sample of 17 276 in 1994 and produced cross-sectional data files in 1996 and 1998. The ability to produce cross-sectional data files from a longitudinal study arises from three factors: (1) the sample (which included respondents aged 12 and over) was ‘refreshed’ by inclusion of children aged 0–11 during initial sampling but who became old enough (age 12+) to participate by the time of a subsequent interview, (2) several provinces had expanded ‘buy-in’ samples in 1996 and (3) sampling weights and replicate bootstrap weights for variance estimation were recalculated for use in cross-sectional estimation in 1996 and 1998, ensuring representation of the national household population. A second data source was a series of general health surveys called the CCHS (Statistics Canada, 2011). The CCHS program uses cross-sectional samples representative of the national household population, producing a new dataset approximately every 2 years. As noted above, both the NPHS and CCHS used similar sampling strategies (multiple-stage, area frame supplemented by random digit dialling, clustered sampling) and measurement strategies (the CIDI-SFMD, with one exception as noted above). There were eight such CCHS surveys conducted between 2001 and 2013 that could be included in the current analysis, together with the two cross-sectional samples from the 1996 and 1998 NPHS. It is important to note that in the CCHS the CIDI-SFMD was usually included as optional content, meaning that it was included in the survey interview only in some provinces. However, we are aware of no evidence that MDE prevalence differs by province in Canada.
The CIDI-SFMD has an item that asks respondents reporting depressive symptoms about the timing of occurrence of their symptoms. This item followed the series of symptom-based items (covering the occurrence of various depressive symptoms in the same 2-week period during the prior 12-months) and had the following wording: ‘Think about the last time you felt this way for 2 weeks or more in a row. In what month was that?’ In this analysis, we restricted the assessment of month depressed to those achieving the 90% predictive probability level on the CIDI-SFMD, which means that they reported five of the nine symptom-based criteria roughly equivalent to those required by DSM-IIIR, IV and DSM-5 for major depressive episode. The relevant item in the CCHS 1.2 was preceded by this preamble: ‘In the next questions, the word ‘episode’ means a period lasting 2 weeks or longer when, nearly every day, you were (at this point the interviewer summarises key phrases) and you also had some of the other problems we just mentioned. The end of an episode is when you no longer have the problems for 2 weeks in a row. With this definition in mind, how many different episodes did you have in the past 12 months?’ When there was a single episode this was followed by ‘In what month and year did that episode start?’ If there were multiple episodes the most recent episode was referenced.
Pooled analyses of survey datasets are complicated due to the design effects that necessarily occur in large-scale population surveys. The data sources used in this study had multi-stage sampling strategies that had differing probabilities of selection and involved clustering. Replicate bootstrap sampling weights must be used to offset these effects in these datasets (Statistics Canada, 2011). Each survey estimate therefore incorporated the proper replicate bootstrap procedures and subsequently meta-analytical methods were used for pooling to improve precision.
Statistical analysis
The pooling procedure followed the following steps. First, the datasets from the individual surveys were restricted to the subset in each survey having a 90% probability of past-year MDE according to the CIDI-SFMD (or in the case of the CCHS 1.2 had a single episode of MDE in the preceding year). Next, the proportions reporting depression in each month were tabulated. These month-specific estimates were then pooled using the ‘metan’ command in Stata Corporation 13 (2013). Initially, forest plots were produced and meta-regression was used to confirm an absence of secular effects. To provide an additional perspective, time was represented in meta-regression models as years since the initial assessment of MDE prevalence in the datasets examined (which was 1996). This meant that the intercept term in this meta-regression's linear equation represented a baseline estimate (1996), and the slope term represented change per year. The statistical significance of this slope term (in a random effects meta-regression) was used to test for secular trends in prevalence. A meta-regression model containing an indicator for measurement instrument was used to assess differences due to use of the WMH-CIDI in the CCHS 1.2. Tests of homogeneity based on the I2 statistic and an associated χ2 test were used to examine heterogeneity prior to pooling. The month-specific proportions were then pooled across the ten surveys. Finally, the pooled estimates of month-specific proportions of MDE were examined using bar graphs in order to depict the pattern. The bars represented the per cent of episodes occurring in that month. 95% confidence intervals were added to the bars. As the observed pattern had a parabolic shape, its statistical significance was assessed by addition of a month2 term to a meta-regression model in which months were numbered 0 (January) to 11 (December) and a month and month2 term was included. Because two of the surveys (the 1996 and 1998) included some of the same respondents (as the NPHS was partially a longitudinal survey, about 20% of the 1996 sample were also included in 1998) a sensitivity analysis was conducted with exclusion of the 1998 dataset.
The CIDI-SFMD item inquiring about the timing of episodes had an inherent ambiguity. The item (see above) asked about the month of a depressive episode in a way (‘last time you felt this way’) that implies the most recent, or perhaps final, part of an episode. Since many depressive episodes last longer than 1 month, the analysis was repeated with stratification by the number of reported weeks depressed in the past year: 2–4 weeks, 5–12 weeks and 13+ weeks. Since there is little ambiguity about the month of occurrence of 2–4-week episodes, this approach was used to explore whether there were differences in the patterns of the short and longer episodes.
Stratification was performed on several individual characteristics: sex (male, female), age group (12–24, 25–44, 45+), and latitude category, in approximate tertiles (42–47.9 degrees, 48–52.9 degrees and 53+ degrees). In keeping with the individual-level meta-analytical methods employed, a two-stage procedure was used in stratification. This meant that the stratification occurred with each dataset and the stratified estimates were then pooled, following the same steps described above, including the testing of a month2 term in the meta-regression analyses within the strata. All analyses were conducted in the Prairie Regional Data Centre in Calgary. Under Canadian ethical guidelines, ethical approval is not required for analyses of this type (Interagency Advisory Panel on Research Ethics (Tri-Council Panel on Ethics, 2014)).
Results
Table 1 summarises the number of available observations for each of the outcome variables in each survey cycle for the CCHS and NPHS surveys. Data from approximately half a million respondents could be included in the analysis.
Table 1.
Sample size and number with CIDI-SFMD assessments for the pooled analysis
| Survey | Total survey sample | CIDI-SFMD* |
|---|---|---|
| NPHS 1996 | 73 402 | 70 538 |
| NPHS 1998 | 15 249 | 14 781 |
| CCHS 1.1 | 131 535 | 128 182 |
| CCHS 1.2 | 36 984 | 36 789 |
| CCHS 2.1 | 135 573 | 50 751 |
| CCHS 3.1 | 132 947 | 68 389 |
| CCHS 2007/08 | 131 959 | 46 739 |
| CCHS 2009/10 | 124 870 | 58 128 |
| CCHS 2011/12 | 125 645 | 21 636 |
| CCHS 2013 | 64 346 | 20 978 |
| Total | 972 510 | 516 911 |
The CCHS 1.2 used the WMH-CIDI.
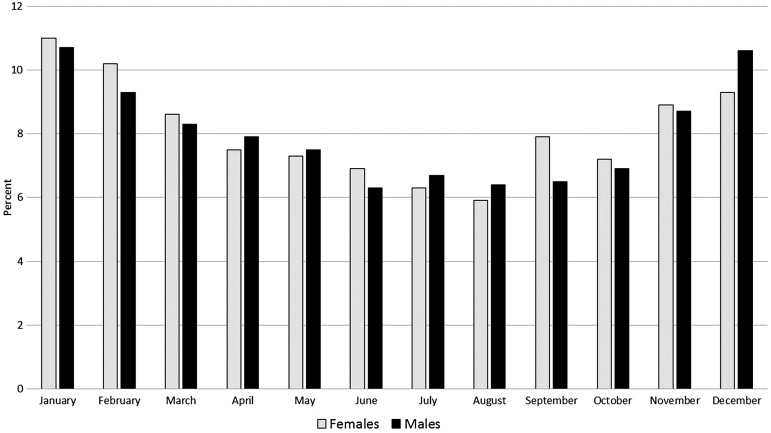
No evidence of secular trends in any of the seasonal proportions was found. The smallest p-value for trend over time (meta-regression slope, by year) was seen in the November estimates (p = 0.07) with the second smallest being that for March (p = 0.28). In the absence of any evidence of secular trends these are not discussed further in the presentation of results. Similarly, no significant differences based on measurement instrument were found in the meta-regression analyses. I2 was slightly over 50% in two of the meta-analyses: September (53%) and October (54%). The heterogeneity χ2 was significant in these same 2 months (September χ2 = 19.21, df = 9, p = 0.023; October χ2 = 19.63, df = 9, p = 0.020). The overall pooled results are displayed in Fig. 1, which depicts substantial seasonal variations. In keeping with the visual impression, a month2 meta-regression term's coefficient (0.0013) was highly significant (p < 0.001). The coefficient did not change with removal of the 1998 dataset, and it remained significant (p < 0.001). With stratification for sex, the same pattern was seen in men and women (see Fig. 2) and the month2 term was again significant in a meta-regression model both for men and women (both, p < 0.001).
Fig. 1.
Proportion of MDE by month, data pooled over 10 surveys. Error bars are 95% confidence intervals. The black line is a meta-regression model: prevalence of MDE = 0.112 + 0.0157*month + 0.00132*month2 where month is numbered 0 (January) to 11 (December).
Fig. 2.
Proportion of MDE by month, data pooled over 10 surveys and stratified by weeks depressed in the past year.
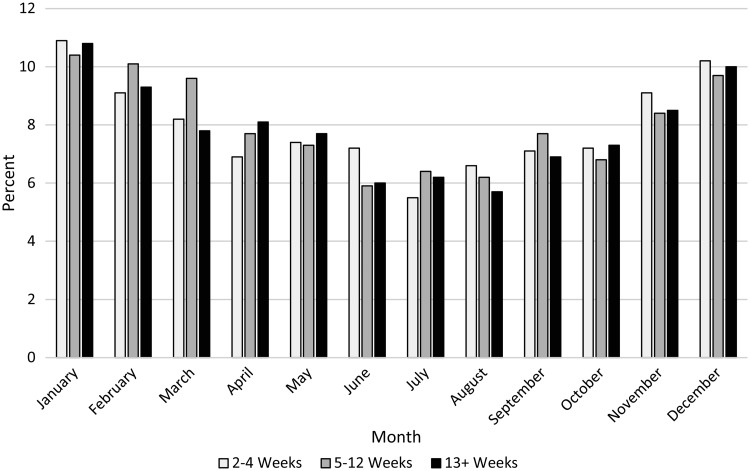
Figure 2 was reproduced with stratification by weeks depressed in the last year. Three strata were used: 2–4 weeks, 5–12 weeks and 13+ weeks. The results are presented in Fig. 3. A very similar pattern is seen irrespective of the reported duration of symptoms, and the statistical significance of the quadratic meta-regression model term remained in each of the three strata, all p-values <0.001 (Fig. 3).
Fig. 3.
Proportion of MDE by month, data pooled over 10 surveys and stratified by weeks depressed in the past year.
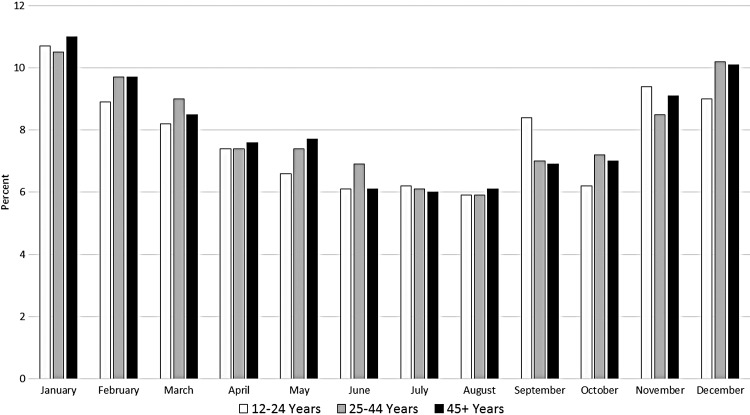
A very similar pattern was also seen in three age strata (see Fig. 4). Again, each of the quadratic terms was highly significant (both p < 0.001).
Fig. 4.
Proportion of MDE by month, data pooled over 10 surveys and stratified into three age groups.
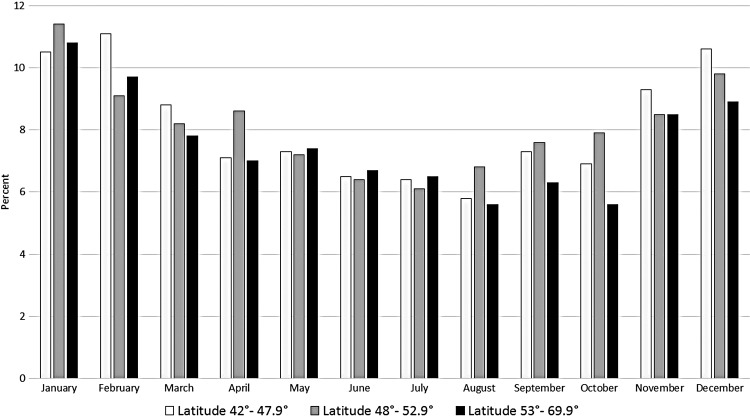
Because of the possibility that seasonal variations might be more pronounced at higher latitudes, the estimates were stratified according to latitude as well. Again, a similar pattern was seen in each of the three latitude strata examined; see Fig. 5. The figure provides no suggestion of a steeper seasonal gradient in more northerly latitudes, although for reasons of precision, the strata are broad, for example, Edmonton is located at 53.5° latitude and therefore falls into the most northerly stratum; yet, Edmonton is not located in the far north. Again, the quadratic meta-regression term was significant in each stratum (all p < 0.001, except for the most northerly stratum, where p = 0.001).
Fig. 5.
Proportion of MDE by month, data pooled over 10 surveys and stratified into three latitude categories.
Discussion
The substantial seasonal variation seen in this study suggests that the burden of MDE is greater in the winter months than in the summer months in Canada. The results appear to apply equally to men and women, and across several age strata. The lack of association with latitude is surprising since seasonal effects are believed due to a lack of light in winter (Magnusson, 2000). However, due to the clustering of the Canadian population in a relatively narrow band along the southern part of the country, the analysis may have lacked power to detect latitude-related effects. These findings add to a literature of related studies documenting seasonal variation in depressive episodes. For example, an analysis of Collaborative Depression Study data found a small seasonal variation in symptom burden and time of relapse in a clinical cohort of 298 patients diagnosed with unipolar depression according to Research Diagnostic Criteria and followed over 10 years (Cobb et al. 2014). In related analysis, similar results were reported for Bipolar disorders, although they were only significant for the Bipolar I subtype (Akhter et al. 2013). Another study by Schwartz et al. (1996) found a u-shaped pattern of mood ratings in a clinical sample with SAD.
The main implications of these findings pertain to the availability of clinical services for MDE. Although there is no tradition of offering seasonal mental health services, at least not in Canada, these data suggest that a greater volume of services may be needed to meet these needs in the winter as opposed to the summer months. This kind of statement is more strongly supported by the current analysis than by SPAQ studies of seasonal mood variation since the latter are less closely aligned with conventional clinical definitions such as that for MDE. The ratio of the highest proportion (January, 10.9%) to the lowest proportion (August 6.3%) is 1.7. Assuming a 2% overall point prevalence (Patten et al. 2006), these ratios imply a point prevalence of 2.7% in January compared with 1.5% in August. The small peak in prevalence in the 12–24-year-old age group in September (see Fig. 4) may potentially represent stresses associated with the start of the school year.
This study has several strengths including its use of ten different samples, each representative of the national household population. These surveys used similar methods of assessment of MDE, which is also a strength. The procedures used to pool these estimates are widely used and are able to accommodate the complex design features of these studies. The extent of heterogeneity could was accommodated using a random effects approach.
There are several limitations to the reported analysis. First, the surveys in question used a short-form version of a fully structured diagnostic interview, which is likely to be less accurate than the full version of the CIDI, and certainly less accurate than a detailed clinical assessment. However, the CIDI-SFMD produces realistic prevalence estimates, generally only slightly higher than the full CIDI (Patten et al. 2014). Also the basis of the 90% predictive probability on this instrument is the endorsement of five depressive symptoms occurring in the same 2-week period in the past year, roughly, mapping to the DSM ‘A’ criterion. This supports its face validity. The CIDI-SFMD was not administered to all provinces in each survey. However, in the absence of firm evidence of inter-provincial differences in depression prevalence this is unlikely to act as a confounding variable. Another limitation is that the available data do not allow estimation of prevalence by month. Rather, the surveys assessed the proportion of those depressed in each year who reported that their depression occurred in a specific month. It may be noted that the two datasets arising from the NPHS are not entirely independent of one another since they included some of the same people; however, repeating the analysis without the 1998 dataset did not change the results. The 1996 cross-sectional NPHS file had a large buy-in component resulting in a larger sample size (see Table 1) so the two datasets are actually largely independent of one another. All of the CCHS surveys used independent samples. Finally, the CIDI-SFMD does not distinguish between situations in which there are single or multiple past-year episodes.
In general, these results are consistent with the idea that the sample size limitations and consequent imprecision has created a difficulty discerning seasonal patterns when conventional measurement strategies are used. Nevertheless, a clear pattern emerged with pooling of the different surveys. Other approaches that provide access to large samples, such as studies of hospital admissions (Suhail & Cochrane, 1998) or Google searches (Yang et al. 2010) have identified seasonal trends, partially corroborating these results.
Finally, it should be acknowledged that since these are cross-sectional estimates, they do not necessarily reflect differences in risk. Prevalence is approximately equal to the product of incidence and mean duration. As a result, the pattern could conceivably represent seasonal differences in prognosis rather than risk. Aetiological implications of these findings should also be a focus of future studies since the seasonal variation may reflect biological, psychological or social determinants of MDE.
Acknowledgements
Dr Patten is a Senior Health Scholar with Alberta Innovates, Health Solutions (AIHS). Dr Fiest is supported by a CIHR post-doctoral fellowship award. The estimates reported in this paper derive used data collected by Statistics Canada, but the analysis and results are the sole responsibility of the authors and do not reflect the views of Statistics Canada.
Financial support
This work was supported by an operating grant from the Canadian Institutes of Health Research (MOP-130415) and by the Hotchkiss Brain Institute.
Conflicts of Interest
None.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. Under Canadian ethical standards (TCPS-2) this project did not require approval from an ethical review board.
References
- Akhter A, Fiedorowicz JG, Zhang T, Potash JB, Cavanaugh J, Solomon DA, Coryell WH (2013). Seasonal variation of manic and depressive symptoms in bipolar disorder. Bipolar Disorders 15, 377–384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association (2013). Diagnostic and Statistical Manual of Mental Disorders (DSM-5). American Psychiatric Publishing: Washington, DC. [Google Scholar]
- Cobb BS, Coryell WH, Cavanaugh J, Keller M, Solomon DA, Endicott J, Potash JB, Fiedorowicz JG (2014). Seasonal variation of depressive symptoms in unipolar major depressive disorder. Comprehensive Psychiatry 55, 1891–1899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerr DC, Shaman J, Washburn IJ, Vuchinich S, Neppl TK, Capaldi DM, Conger RD (2013). Two longterm studies of seasonal variation in depressive symptoms among community participants. Journal of Affective Disorders 151, 837–842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Ustun TB (2004). The world mental health (WMH) survey initiative version of the world health organization (WHO) composite international diagnostic interview (CIDI). International Journal of Methods in Psychiatric Research 13, 83–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Andrews G, Mroczek D, Ustun B, Wittchen HU (1998). The world health organization composite international diagnostic interview short-form (CIDI-SF). International Journal of Methods in Psychiatric Research 7, 171–185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magnusson A (2000). An overview of epidemiological studies on seasonal affective disorder. Acta Psychiatrica Scandinavica 101, 176–184. [PubMed] [Google Scholar]
- Mersch PP, Vastenburg NC, Meesters Y, Bouhuys AL, Beersma DG, Van Den Hoofdakker RH, Den Boer JA (2004). The reliability and validity of the seasonal pattern assessment questionnaire: a comparison between patient groups. Journal of Affective Disorders 80, 209–219. [DOI] [PubMed] [Google Scholar]
- Michalak EE, Murray G, Wilkinson C, Dowrick C, Lasa L, Lehtinen V, Dalgard OS, Ayuso-Mateos JL, Vazquez-Barquero JL, Casey P, the ODIN Group (2004). Estimating depression prevalence from the beck depression inventory: is season of administration a moderator? Psychiatry Research 129, 99–106. [DOI] [PubMed] [Google Scholar]
- Oyane NM, Bjelland I, Pallesen S, Holsten F, Bjorvatn B (2008). Seasonality is associated with anxiety and depression: the Hordaland health study. Journal of Affective Disorders 105, 147–155. [DOI] [PubMed] [Google Scholar]
- Patten SB, Wang JL, Williams JV, Currie S, Beck CA, Maxwell CJ, El-Guebaly N (2006). Descriptive epidemiology of major depression in Canada. Canadian Journal of Psychiatry 51, 84–90. [DOI] [PubMed] [Google Scholar]
- Patten SB, Williams JVA, Lavorato D, Fiest KM, Bulloch AGM, Wang JL (2014). The prevalence of major depression is not changing. Canadian Journal of Psychiatry 60, 31–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenthal NE (2009). Issues for DSM-V: seasonal affective disorder and seasonality. American Journal of Psychiatry 166, 852–853. [DOI] [PubMed] [Google Scholar]
- Rosenthal NE, Sack DA, Gillin JC, Lewy AJ, Goodwin FK, Davenport Y, Mueller PS, Newsome DA, Wehr TA (1984). Seasonal affective disorder. A description of the syndrome and preliminary findings with light therapy. Archives of General Psychiatry 41, 72–80. [DOI] [PubMed] [Google Scholar]
- Sakamoto K, Nakadaira S, Kamo K, Kamo T, Takahashi K (1995). A longitudinal follow-up study of seasonal affective disorder. American Journal of Psychiatry 152, 862–868. [DOI] [PubMed] [Google Scholar]
- Schwartz PJ, Brown C, Wehr TA, Rosenthal NE (1996). Winter seasonal affective disorder: a follow-up study of the first 59 patients of the National Institute of Mental Health Seasonal Studies Program. American Journal of Psychiatry 153, 1028–1036. [DOI] [PubMed] [Google Scholar]
- Stata Corporation (2013). Stata (version 13). College Station: TX, Stata Corporation. [Google Scholar]
- Statistics Canada (2011). Canadian Community Health Survey – Annual Component (CCHS). Statistics Canada: Ottawa: Retrieved 24 April 2015 from http://www.statcan.gc.ca/cgi-bin/imdb/p2SV.pl?Function=getSurvey&SDDS=3226&lang=en&db=imdb&adm=8&dis=2 [Google Scholar]
- Statistics Canada (2013). National Population Health Survey – Household Component – Cross-Sectional (NPHS). Retrieved 30 December 2013 from http://www23.statcan.gc.ca/imdb/p2SV.pl?Function=getSurvey&SDDS=3236&lang=en&db=imdb&adm=8&dis=2
- Suhail K, Cochrane R (1998). Seasonal variations in hospital admissions for affective disorders by gender and ethnicity. Social Psychiatry & Psychiatric Epidemiology 33, 211–217. [DOI] [PubMed] [Google Scholar]
- Thompson C, Raheja SK, King EA (1995). A follow-up study of seasonal affective disorder. British Journal of Psychiatry 167, 380–384. [DOI] [PubMed] [Google Scholar]
- Tri-Council Panel on Ethics (2014). TCPS 2—2nd edition of Tri-Council Policy Statement: Ethical Conduct for Research Involving Humans. Panel on Research Ethics: Ottawa: Retrieved 24 April 2015 from http://www.pre.ethics.gc.ca/eng/policy-politique/initiatives/tcps2-eptc2/Default/ [Google Scholar]
- Tuuanainen A, Kripke DF, Endo T (2004). Light therapy for non-seasonal depression. Cochrane Library, Art. No.: CD004050. DOI: 10.1002/14651858.CD004050.pub2. [DOI] [PMC free article] [PubMed]
- Winthorst WH, Post WJ, Meesters Y, Penninx BW, Nolen WA (2011). Seasonality in depressive and anxiety symptoms among primary care patients and in patients with depressive and anxiety disorders; results from the Netherlands study of depression and Anxiety. BMC Psychiatry 11, 198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang AC, Huang NE, Peng CK, Tsai SJ (2010). Do seasons have an influence on the incidence of depression? The use of an internet search engine query data as a proxy of human affect. PLoS ONE 5, e13728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young SN (2011). Bright light for nonseasonal depression? Journal of Psychiatry & Neuroscience 36, E37–E38. [DOI] [PMC free article] [PubMed] [Google Scholar]