Abstract
Background.
Chinese psychiatrists have gradually started to focus on those who are deemed to be at ‘clinical high-risk (CHR)’ for psychosis; however, it is still unknown how often those individuals identified as CHR from a different country background than previously studied would transition to psychosis. The objectives of this study are to examine baseline characteristics and the timing of symptom onset, help-seeking, or transition to psychosis over a 2-year period in China.
Method.
The presence of CHR was determined with the Structured Interview for Prodromal Syndromes (SIPS) at the participants' first visit to the mental health services. A total of 86 (of 117) CHR participants completed the clinical follow-up of at least 2 years (73.5%). Conversion was determined using the criteria of presence of psychotic symptoms (in SIPS). Analyses examined baseline demographic and clinical predictors of psychosis and trajectory of symptoms over time. Survival analysis (Kaplan–Meier) methods along with Log-rank tests were performed to illustrate the relationship of baseline data to either conversion or non-conversion over time. Cox regression was performed to identify baseline predictors of conversion by the 2-year follow-up.
Results.
In total 25 (29.1%) of 86 completers transitioned to a psychotic disorder over the course of follow-up. Among the CHR sample, the mean time between attenuated symptom onset and professional help-seeking was about 4 months on average, and converters developed fully psychotic symptoms about 12 months after symptom onset. Compared with those CHR participants whose risk syndromes remitted over the course of the study, converters had significantly longer delays (p = 0.029) for their first visit to a professional in search of help. At baseline assessment, the conversion subgroup was younger, had poorer functioning, higher total SIPS positive symptom scores, longer duration of untreated prodromal symptoms, and were more often given psychosis-related diagnoses and subsequently prescribed antipsychotics in the clinic.
Conclusions.
Chinese CHR identified primarily by a novel clinical screening approach had a 2-year transition rate comparable with those of specialised help-seeking samples world-wide. Early clinical intervention with this functionally deteriorating clinical population who are suffering from attenuated psychotic symptoms, is a next step in applying the CHR construct in China.
Key words: Outpatient psychiatry, psychosis, risk factors, schizophrenia
Introduction
Unlike many other chronic medical diseases, such as diabetes or hypertension, schizophrenia and other psychotic disorders most often begin in adolescence or young adulthood (van der Werf et al. 2014), remain undetected and untreated for long periods of time (Melle et al. 2004; Perkins et al. 2005), and are often associated with functional decline (Rajji & Mulsant, 2008). Early detection and intervention offer hope for improving the course of these disorders on young lives. Researchers from around the world have contributed to the identification of early signs and symptoms suggesting a ‘prodrome’ to psychosis in the hope that early detection will minimise risk and reduce the full onset of psychotic disorders. Increased scientific interest and research have led to the development of operationally defined criteria, for identifying those at ‘clinical high risk (CHR)’ (Yung et al. 2005; McGlashan et al. 2010; Schultze-Lutter et al. 2010). These have gained wide recognition in the last decade. One concern with this effort is the fact that only a modest portion of the CHR participants transition to full psychosis (about 29%) after 2 years (Fusar-Poli et al. 2012). Therefore, more refined criteria and risk factors (clinical or biological) are needed to identify those at highest or most imminent risk, such as a study is being conducted by Cannon et al. (2008) in the North American Prodrome Longitudinal studies (NAPLS).
In China, the concept of CHR is still new to mental health professionals, with only preliminary tests of validity of this concept in a Chinese clinical setting (Zhang et al. 2014). In our first report, in a consecutive sample of 2101 outpatients, we found a 4.2% rate of CHR syndromes, mainly characterised by attenuated positive symptoms. This work confirmed that CHR subjects are not uncommon and can be accurately identified in a Chinese clinic population. The question remains as to who are at highest risk for future psychosis. Although bio-markers may facilitate identification of the progression of psychosis (Solis, 2014), implementation of these biological predictors are still not yet specific enough to be applied to current clinical practice, and we must rely on optimising easily collected clinical characteristics.
The current study builds on the prior study by examining the rate of conversion and 2-year outcomes of the full sample of Chinese psychological counseling service center patients previously identified as CHR for psychosis. As the baseline characteristics associated with 2-year outcomes of Chinese CHR samples and the timing of symptom onset, help-seeking, or conversion have not yet been characterised; we report on these analyses in this paper. We expected that the transition rate would be comparable with the results from a recent meta-analysis (Fusar-Poli et al. 2012). In addition, we are motivated to carry out this study because we believe that knowing what baseline characteristics predict subsequent conversion to psychosis would be of practical interest for clinicians beginning to develop early intervention approaches.
Methods
Sample
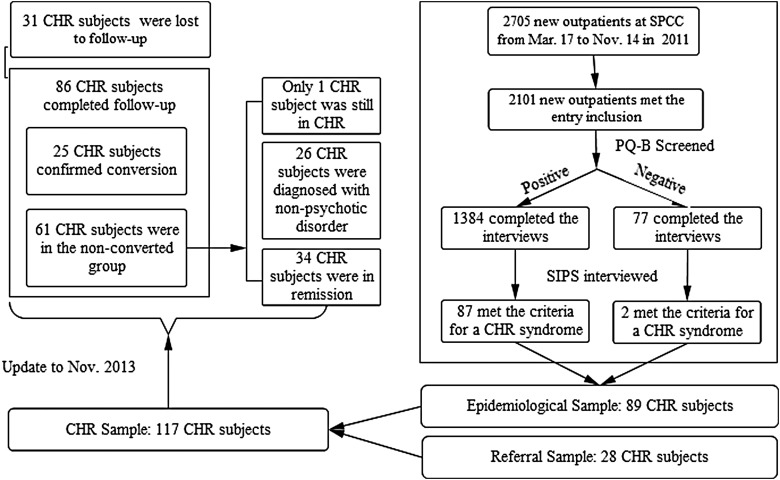
The Research Ethics Committee at the Shanghai Mental Health Center (SMHC) approved the study in 2011.The 117 participants with CHR included in this study were recruited from both clinic-wide questionnaire screening (n = 89) and clinician referrals (n = 28), all anti-psychotic naïve at baseline, and making their first visit for psychiatric treatment. In Fig. 1 below, we have included a flow chart showing enrolment in the early identification program and the 2-year follow-up of CHR participants. The CHR status was confirmed in a face-to-face interview using the Structured Interview of Prodrome Syndromes (SIPS/SOPS; Miller et al. 2003). This observational study sample was taken from the Shanghai Psychotherapy and Psychological Counseling Center (SPCC) at SMHC, which is China's largest outpatient medication-management and psychotherapy-providing mental health clinic. These help-seeking participants from different parts of the country were screened to be included in the study. At baseline, participants were between 15 and 45 years of age (Mean = 27.1; s.d. = 7.36), 44.5% male and had completed at least 6 years of primary education. They were recruited after we obtained written consent. Those younger than 18 years of age were signed up for the study by their parents, who provided consent, and the youth provided assent. The inclusion criteria were identical to the preliminary data published in the epidemiological study using a screening tool (Loewy et al. 2005). Participants had to fulfill at least one of the prodromal syndrome criteria: (1) brief intermittent psychotic syndrome, (2) attenuated positive symptom syndrome, or (3) genetic risk and deterioration syndrome (GRDS). Those with severe somatic diseases (e.g., pneumonia, cancer, or heart failure), mental retardation, or dementia were excluded.
Fig. 1.
Sample flow chart of enrollment and follow-up.
Assessment
Baseline CHR identification
CHR status was assessed with SIPS/SOPS (Miller et al. 2002, 2003; McGlashan et al. 2010), which was designed to assess the existence of positive prodromal symptoms and a range of other potentially prodromal phenomena, such as negative, disorganised and general symptoms. The positive symptoms (scales P1–P5) were rated to rule out psychosis and to rule in prodromal syndromes. The English version has good inter-rater reliability (IRR) and validity for predicting psychosis transition (Miller et al. 2003). The Chinese version (Zheng et al. 2012) of the SIPS/SOPS was translated and tested by our team members (detailed descriptions of this work have been published previously in Zhang et al. (2014), and demonstrated both good IRR (r = 0.96, p < 0.01 on the SOPS score) and validity (26.4%, converted to psychosis in the ensuing 2 years) with a Chinese clinical population.
The global assessment of function (GAF) (Aas, 2010) was used as a measure of the global psychological, social and occupational functioning of the patients. It had been widely used in studies of psychotic patients' outcomes. Also, the GAF is included as the measurement for assessing the functional deterioration (score relative to 12 months prior) in the SIPS/SOPS interview. It is a numeric scale with 10-point intervals and should be rated from 1 to 100. The lower the score, the poorer the individual functions. Duration of untreated prodromal symptoms (DUPrS) was assessed retrospectively, defined as the period between the onset of the first attenuated psychotic positive symptom (at least moderate level, corresponding to 3 points or higher on SOPS), based on information from the SIPS interview, and the commencement of professional help at mental health services.
Follow-up outcome measures
The major focus of this follow-up study was conversion to psychosis. Conversion was determined using the criteria of POPS (Presence of Psychotic Symptoms in SIPS/SOPS) (McGlashan et al. 2010). Participants had to demonstrate at least one psychotic level symptom [rated a ‘6’ (severe and psychotic, i.e., conviction of psychotic experiences) on at least one of the five positive symptoms (P1, unusual thought content; P2, suspiciousness; P3, grandiosity; P4, perceptual abnormalities; and P5, disorganised communication)] with either sufficient frequency and duration (at least 1 h per day, an average frequency of 4 days per week for a period of one month), or at a level that was disorganising or dangerous. Other clinical outcomes were defined in accordance with definitions from the second phase of the NAPLS 2 (Addington et al. 2015). ‘Remission’ was determined by SOPS P symptoms rated scores of 2 or less, or required the GAF to have returned to 90% of the previous best GAF for GRDS. ‘Symptomatic’ was determined by SOPS P symptoms rated scores of 3–5, but not currently meeting criteria for CHR (to meet CHR criteria, the symptom must currently rate at least one scale point higher than rated 12 months ago). As for GRDS, meaning with no change in the GAF, CHR subjects with new or worse symptoms in the year prior to follow-up were defined as having sustained CHR status. Those fulfilling criteria of other Axis I disorders, categorised as ‘other disorders’, were defined according to their medical records by clinical psychiatrists and judgments through phone conversation by research psychiatrists based on the Chinese Classification and Diagnostic Criteria of Mental Disorders (CCMD-3).
If a SIPS face-to-face interview was not possible (usually this situation occurred because the participant lived far from Shanghai and was unable to participate in the face-to-face interview during the follow-up), the diagnoses of those who either converted to a psychotic disorder or had other disorders, such as depression, were obtained by at least two senior psychiatrists in two instances using the POPS criteria or CCMD-3 criteria by a phone call.
Among the 25 converters, 19 subjects were identified according to POPS criteria by a SIPS interview: 11 were interviewed by phone and 8 through face-to-face interviews conducted by the research psychiatrists (14 of 19 diagnoses of psychotic disorders were also confirmed by their clinicians as recorded in their medical records). The remaining six converters were confirmed by interviewers according to the patient's information during the episode of psychosis offered by their family members, and also confirmed by their clinical, medical records. Although these six patients refused to talk to the interviewers, the diagnosis of psychotic conversion was reliant on both specific documentation of the clinical diagnosis, severity of symptoms and from judgments by research psychiatrists from a phone conversation with the family. As for the 61 non-converters, 25 were interviewed by phone, 28 through face-to-face interviews, and the remaining 8 were determined by interviewers according to information from family members, medical records and clinical diagnosis. Whether CHR subjects had taken their medication as prescribed by our clinicians at baseline, or took medication in an irregular way was carefully assessed in the follow-up. If CHR subjects did not follow their clinicians' prescription, they are categorised as ‘irregular or interruption of medication’.
Procedures
Full details about initial recruitment and screening are available in our prior report (Zhang et al. 2014). Two senior nurses with at least 10 years experience in a psychiatric unit who conducted the initial screenings were employed to collect all diagnostic and medication information from medical records at every follow-up visit. The four psychiatrists are qualified and well-trained (Zhang et al. 2014) and conducted the SIPS/SOPS interview at baseline and follow-up. The IRR for the SIPS/SOPS positive symptoms ranged from 0.86 (P5) to 0.98 (P4) among the four raters.
From March to November 2011, participants who met the inclusion criteria were consecutively recruited to participate in this study. They were informed that this was not a treatment study and it involved naturalistic follow-up without any extra intervention or financial remuneration. They otherwise followed the routine clinical treatment procedure at the SPCC. After consent and initial assessment, all the participants were informed that the plan was to be followed up for at least 2 years (mean period of 28.3 months for those who completed the follow-up assessment). All the CHR participants who completed the baseline assessment were followed up at least twice in either March or April 2012 and November 2013. Both the patients and their caregivers had been told that they could contact the interviewer and study clinicians anytime for questions and to provide progress reports on the patients' medical conditions during the subsequent 2 years. Except for those who did not desire any further contact, the CHR participants were re-assessed using the SIPS/SOPS on two different occasions. The conversion determination was made according to the clinical information received from clinician reports, telephone interviews of CHR individuals or their caregivers and face-to-face interviews.
Data analysis
The distribution of demographics and clinical data at baseline was analysed using descriptive statistics. Analyses of variance (ANOVAs) were conducted to measure converter v. non-converter differences in continuous variables; and either chi-squared statistics or a Fisher's exact test were used in examining the categorical variables. We plotted the time points for symptom onset, professional help-seeking, and conversion in Excel (version 2003, Microsoft, USA). Box plot diagrams were created with SPSS version 16.0 (SPSS, Inc., Chicago, IL, USA) software, to summarise mean time to conversion and help-seeking by group. Survival analysis (Kaplan–Meier) methods and Log-rank tests were performed to illustrate the relationship of baseline data to either conversion or non-conversion over time. Converters classified with certainty and non-converters were ‘censored’. Twelve types of predictors have been chosen by median-split or conceptual/theoretical reasons in our survival analysis. Finally, Cox regression was performed to identify baseline predictors of conversion by the 2-year follow-up.
Results
Demographics and clinical characteristics at baseline
Of the 117 CHR participants enrolled in the study, 86 (73.5%) completed the follow-up, and 25 (29.1%) of these developed psychosis within 2 years. Converters were significantly younger than non-converters, and more likely to be single. However, there were significant clinical differences at baseline between the two groups in their initial diagnosis and their subsequent medication prescription rates, according to medical records. Converters were significantly more likely than non-converters to have diagnoses of possible psychotic disorders and to be treated with antipsychotics at baseline by SMHC clinicians. Socio-demographic and clinical data at baseline are listed in Table 1.
Table 1.
Baseline demographic and clinical variables, comparison between converters and non-converters
| Converters v. non-converters | ||||||
|---|---|---|---|---|---|---|
| Variables | Total CHR sample | Converters | Non-converters | Lost | F/χ2 | p value |
| Cases (n) | 117 | 25 (21.4%) | 61 (52.1%) | 31 (26.5%) | – | – |
| Age (years), [Mean (s.d.)] | 24.7 (7.6) | 20.7 (6.0) | 25.6 (7.6) | 26.0 (7.9) | 8.035 | 0.006 |
| Male [n (%)] | 56 (47.9%) | 14 (56.0%) | 24 (39.3%) | 18 (58.1%) | 2.00 | 0.158 |
| Education (years), [Mean (s.d.)] | 12.7 (3.0) | 11.6 (3.1) | 12.9 (2.8) | 13.5 (3.1) | 3.576 | 0.062 |
| Single/separated/divorced, [n (%)] | 89 (76.1%) | 24 (96.0%) | 45 (73.8%) | 20 (64.5%) | 4.21a | 0.040 |
| Birthplace (Shanghai), [n (%)] | 57 (48.7%) | 14 (56.0%) | 33 (54.1%) | 10 (32.3%) | 0.03 | 0.872 |
| Attend Class/Workb | ||||||
| (Most), [n (%)] | 79 (67.5%) | 14 (56.0) | 47 (77.0%) | 18 (58.1%) | 4.048c | 0.140c |
| (Half), [n (%)] | 22 (18.8) | 7 (28.0%) | 8 (13.1%) | 7 (22.6%) | ||
| (Less than half), [n (%)] | 16 (13.7%) | 4 (16.0%) | 6 (9.8 %) | 6 (19.4%) | ||
| Clinical diagnosis (at baseline)d | ||||||
| Psychosis-related (or suspected), [n (%)] | 43 (36.8%) | 20 (80.0%) | 15 (24.6%) | 8 (25.8%) | 23.185 | <0.001 |
| Mood/anxiety disorder-related (or suspected), [n (%)] | 57 (48.7%) | 3 (12.0%) | 38 (62.3%) | 16 (51.6%) | ||
| Others, [n (%)] | 17 (14.5%) | 2 (8.0%) | 8 (13.1%) | 7 (22.6%) | ||
| Anti-psychotic medication prescription, [n (%)] | 58 (49.6%) | 23 (92.0%) | 25 (41.0%) | 10 (32.3%) | 18.714 | <0.001 |
| Anti-depressant or mood-stabilizer prescriptione | ||||||
| (Only, without anti-psychotic medication), [n (%)] | 48 (41.0%) | 1 (4.0%) | 33 (54.1%) | 14 (45.2%) | 18.991 | <0.001 |
| (Combined with anti-psychotic medication), [n (%)] | 28 (23.9%) | 13 (52.0%) | 13 (21.3%) | 2 (6.5%) | ||
| (None), [n (%)] | 41 (35.0%) | 11 (44.0%) | 15 (24.6%) | 15 (48.4%) | ||
| (Irregular or interruption of medication), [n (%)] | – | 16 (64.0%) | 48 (78.7%) | – | 2.010 | 0.156 |
Pearson chi-square with Yates's continuity correction.
‘Attend Class/Work’ was collected from outpatients' report from question of ‘How regularly did you attend work/classes in the past 6 months’. ‘Most’ indicates ‘All or most (more than 75%) of the time’; ‘Half’ indicates ‘Half (about 50–75%) of the time’; ‘Less than half’ indicates ‘Less than half (less than 50%) of the time’.
Fisher's exact test.
‘Clinical diagnosis’ was collected from outpatients' medical records, which were created by their attending doctors according to the Chinese mental health diagnostic manual.
The information on medications taken was obtained from both clinical records and follow-up interviews, but only the information from the first visit was used in the ‘lost group’.
Attrition
In total 21 (17.9%) of the participants were lost to follow-up as of the first follow-up visit (up to March, 2012). By November, 2013, we lost contact with ten additional participants. In total, 31 (26.5%) did not complete the 2-year follow-up assessment. Participants with complete follow-up compared with those lost to attrition had no significant differences in age (F = 1.400, p = 0.239), gender (χ2 = 1.759, p = 0.185), marital status (χ2 = 3.092, p = 0.079), screening or referral method (χ2 continuity correction = 0.000, p = 1), clinical diagnosis (χ2 = 2.174, p = 0.14), family history (χ2 = 2.931, p = 0.231), current GAF score (F = 2.306, p = 0.132), or GAF drop (F = 0.502, p = 0.48). The only significant difference was that fewer local patients (those who were born in Shanghai) were lost during the follow-up (χ2 = 4.573, p = 0.032) than those who were born in other provinces, reflecting the difficulty in follow-ups with participants living far away.
Baseline SIPS/SOPS assessment
There were significant differences in current GAF score and drop in GAF score and total SOPS positive symptom score, between converters and non-converters (see Table 2). Converters had relatively low current GAF scores, and these scores were more likely to have significantly decreased in the year preceding the baseline. The total score of SOPS positive symptoms was higher for the converters group at baseline; however, the incidence rate of each positive symptom and the means of negative, disorganised and general symptom scores did not differ significantly between the two groups.
Table 2.
Baseline SIPS/SOPS variables, comparison between converters and non-converters
| Converters v. non-converters | |||||
|---|---|---|---|---|---|
| Variables | Total CHR sample (n = 117) | Converters (n = 25) | Non-converters (n = 61) | F/χ2 | p value |
| APSS, [n (%)] | 92 (78.6%) | 23 (92.0%) | 50 (82.0%) | 0.719a | 0.396 |
| GRDS, [n (%)] | 27 (23.1%) | 2 (8.0%) | 14 (23.0%) | 1.723 | 0.189 |
| BIPS, [n (%)] | 4 (3.4%) | 1 (4.0%) | 0 | – | – |
| Current GAF, [Mean (s.d.)] | 58.8 (6.4) | 55.6 (4.2) | 59.4 (6.6) | 7.278 | 0.008 |
| Drop GAFb, [Mean (s.d.)] | 21.6 (7.5) | 24.7 (5.9) | 20.7 (7.6) | 5.507 | 0.021 |
| Family history | |||||
| (None), [n (%)] | 82 (70.1%) | 21 (84.0%) | 43 (70.5%) | 1.582c | 0.455c |
| (Low-riskd), [n (%)] | 14 (12.0%) | 2 (8.0%) | 7 (11.5%) | ||
| (High-riske), [n (%)] | 21 (17.9%) | 2 (8.0%) | 11 (18.0%) | ||
| SPD, [N (%)] | 8 (6.8%) | 0 | 5 (8.2%) | – | 0.315c |
| Symptoms rating (SOPS) | |||||
| Positive symptoms, [Mean (s.d.)] | 7.1 (4.5) | 10.7 (4.0) | 6.6 (4.3) | 17.007 | <0.001 |
| P1 > 2, Unusual thought content, [n (%)] [Mean (s.d.)] |
54 (46.2%) 2.2 (1.8) |
17 (68.0%) 3.08 (1.6) |
33 (54.1%) 2.15 (1.8) |
1.408 | 0.235 |
| P2 > 2, Suspiciousness, [n (%)] [Mean (s.d.)] |
54 (46.2%) 2.3 (1.9) |
17 (68.0%) 3.6 (1.6) |
36 (59.0%) 2.0 (1.9) |
0.605 | 0.437 |
| P3 > 2, Grandiose ideas, [n (%)] [Mean (s.d.)] |
2 (1.7%) 0.1 (0.5) |
2 (8.0%) 0.4 (1.0) |
0 0.0 (0.0) |
– | 0.082c |
| P4 > 2, Perceptual abnormalities, [n (%)] [Mean (s.d.)] |
45 (38.5%) 1.8 (2.1) |
12 (48.0%) 2.2 (2.3) |
25 (41.0%) 1.7 (1.9) |
0.356 | 0.551 |
| P5 > 2, Disorganised communication, [n (%)] [Mean (s.d.)] |
7 (6.0%) 0.8 (1.0) |
4 (16.0%) 1.4 (1.3) |
3 (4.9%) 0.8 (1.0) |
1.619 | 0.203 |
| Negative symptoms, [Mean (s.d.)] | 9.4 (5.1) | 10.8 (5.3) | 9.6 (5.5) | 0.848 | 0.360 |
| Disorganised symptoms, [Mean (s.d.)] | 3.4 (2.3) | 4.0 (2.3) | 3.3 (2.3) | 1.636 | 0.204 |
| General symptoms, [Mean (s.d.)] | 8.1 (3.4) | 7.1 (3.7) | 8.6 (3.4) | 3.538 | 0.063 |
| Total score, [Mean (s.d.)] | 28.0 (10.2) | 32.6 (11.1) | 28.1 (10.2) | 3.260 | 0.075 |
APSS, attenuated positive symptom syndrome; GRDS, genetic risk and deterioration syndrome; BIPS, brief intermittent psychotic syndrome; CHR, clinical high-risk; GAF, global assessment of function; SPD, schizotypal personality disorder.
Pearson chi-square with Yates's continuity correction.
GAF drop, GAF score current from highest in past year.
Fisher's exact test.
Low-risk family history-having any family members with mental disorders or a first-degree relative with non-psychotic disorders.
High-risk family history-having at least one first-degree relative with psychosis.
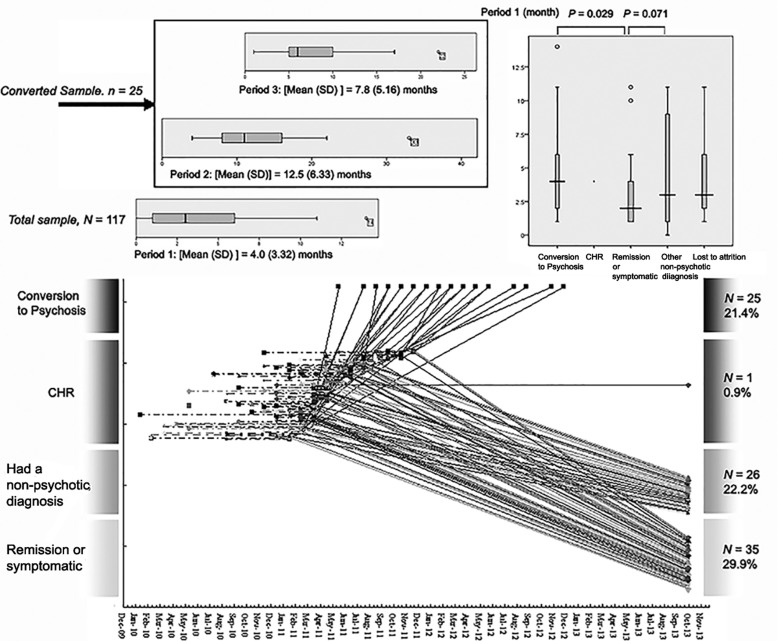
Timeline for conversion
As shown in Fig. 2, the mean time between attenuated symptom onset and professional help-seeking was approximately 4.0 ± 3.3 months for the overall CHR sample. Compared with those CHR participants whose risk syndromes remitted over the course of the study, converters had significantly longer delays (p = 0.029) between symptom onset and their first visit to a professional in search of help. On average, converters developed fully psychotic symptoms 12.5 ± 6.3 months after attenuated symptom onset.
Fig. 2.
Conversion timeline and trajectory plots. Note: The box plot-diagram shows the descriptive statistics over time for those who made a transition to psychosis. Period 1: time between CHR symptom onset and baseline assessment; Period 2: time between CHR symptom onset and conversion; Period 3: time to conversion from the baseline assessment.
Conversion to psychosis
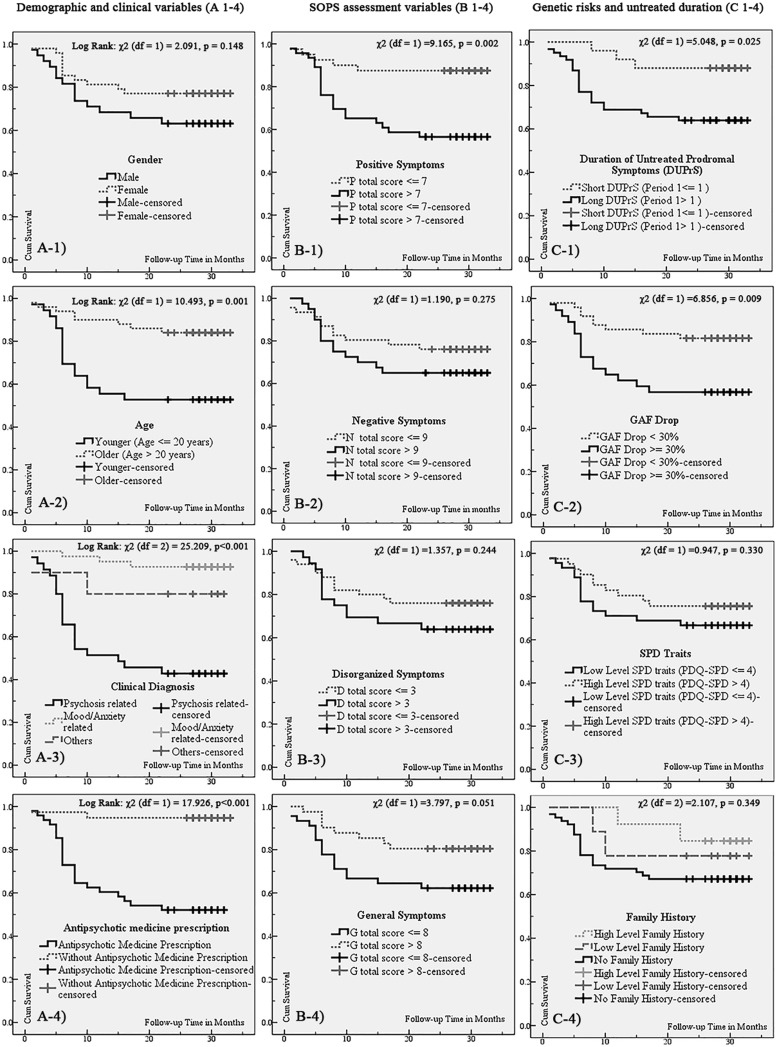
Kaplan–Meyer survival curves were constructed for 86 CHR participants (25 converters and 61 non-converters) separated by sex (male, n = 38 v. female, n = 48), age (≤20 years, n = 36 v. >20 years, n = 50), clinical diagnosis (psychosis-related, n = 35 v. mood/anxiety-related, n = 41 v. others, n = 10), antipsychotic medications prescribed (antipsychotic medications prescribed, n = 48 v. no antipsychotic medications prescribed, n = 38), total score of positive symptoms on the SOPS (≤7, n = 40 v. >7, n = 46), negative symptoms (≤9, n = 46 v. >9, n = 40), disorganised symptoms (≤3, n = 50 v. >3, n = 36), general symptoms (≤8, n = 45 v. >8, n = 41), DUPrS (≤1 month, n = 25 v. >1 month, n = 61), GAF drop (≤30%, n = 49 v. >30%, n = 37), schizotypal personality disorder (SPD) traits (PDQ-SPD ≤ 4, n = 45 v. >4, n = 41), and family history of psychosis (high level, n = 13 v. low level, n = 9 v. none, n = 64). Figure 3 shows that the conversion rate was significantly higher in those who were younger, had a psychosis-related diagnosis, had been prescribed antipsychotic medications after the baseline assessment, had a higher positive symptom score, longer delays to treatment and a lower GAF score relative to 12 months earlier.
Fig. 3.
Kaplan–Meyer survival curves for transitions to psychosis among the demographic, clinical and SIPS/SOPS assessment variables.
Prediction of conversion
Cox regression was used to evaluate the effect of demographic and clinical variables on conversion risk, including age, gender, education, marital status, character (introversion/extroversion), clinical diagnosis, antipsychotic medication prescription, irregular or interruption of medication, SIPS items (positive symptoms P1–5, P1–5 > 2), DUPrS, SPD, GAF drop. Consistently, GAF drop, clinical diagnosis and treatment decisions (i.e., antipsychotic medication prescription), and DUPrS were all found to significantly predict conversion to psychosis in this model (Table 3).
Table 3.
Cox regression for predicting the transition to psychosis
| Predictor variable | β | S.E. | OR | 95% CI | Wald statistic | p value |
|---|---|---|---|---|---|---|
| Drop in GAF | 0.116 | 0.034 | 1.123 | 1.050–1.201 | 11.417 | 0.001 |
| Clinical diagnosis (psychosis-related) | −1.822 | 0.657 | 0.162 | 0.045–0.586 | 7.684 | 0.006 |
| DUPrS | 0.132 | 0.052 | 1.142 | 1.030–1.265 | 6.413 | 0.011 |
| Antipsychotic medicine prescription | 2.254 | 1.123 | 9.527 | 1.054–86.114 | 4.027 | 0.045 |
GAF, global assessment of function; DUPrS, duration of untreated prodromal symptoms.
Discussion
To our knowledge, this is the first study to systematically examine baseline characteristics and the transition rate of individuals in China at CHR over a 2-year period. According to the results from a long-term (over 10 years) follow-up study (Nelson et al. 2013) by the Personal Assessment and Crisis Evaluation (PACE) clinic, the risk for transiting to full-blown psychosis is highest in the first 2 years. Our results show that, at the end of the follow-up period, 29.1% individuals at CHR had developed a psychotic disorder. This transition rate is quite similar to the results of a recent meta-analysis (Fusar-Poli et al. 2012), although no Chinese studies were included. Our findings confirm that the CHR phenotype carries a similar and predictable risk for the future onset of psychotic disorders in a predominantly Eastern population as in Western populations. Given that China has one-fifth of the world's population and 10 million psychotic patients, this finding has major implications for psychosis prevention and early intervention.
The current study explicitly describes the differences in baseline characteristics between those participants who transited to psychosis and those who did not. Specifically, CHR participants with more severe positive symptoms and decline in functioning were more likely to transition to psychosis. These findings are largely consistent with other recent studies (Yung et al. 2004; Addington et al. 2007, 2011; Cannon et al. 2008; Lemos-Giraldez et al. 2009; Velthorst et al. 2009). Specifically, the factor of functional deterioration was identified as a potential predictor of psychosis in both NAPLS (Cannon et al. 2008) and PACE (Thompson et al. 2011) studies. In contrast with those studies, no specific positive symptoms were significantly predictive in this study. Rather, the severity of total positive symptoms was associated with higher rates of later psychosis. Our explanation for this result was that, in the SIPS/SOPS, the higher positive symptoms scores indicate the more serious psychotic experiences, and more serious impairments in the insight of those experiences. Therefore, it makes sense that those who had more serious symptoms might be more easily convinced (e.g. CHR subject had symptom as ‘hearing voices that classmates are talking on him’ [P4, perceptual abnormalities], he may become suspicious [P2, suspiciousness] on his classmates. Compared with those who had only P2 symptoms, he may be more easily convinced.). Once they are fully convinced, they will meet the criteria of full psychosis.
At present, there is no formal diagnosis corresponding to CHR syndromes in any diagnostic system. Clinicians diagnosing these individuals in a Chinese mental health clinic tended to resort to diagnoses based upon initial impressions such as ‘suspicion state,’ ‘paranoid state,’ or ‘depression state’. Although, these Chinese CHR participants may pose diagnostic challenges, psychosis-related impressions and antipsychotic medication prescriptions appear to reflect an accurate recognition of increased psychosis risk or underlying psychotic process. It seems that the Chinese clinicians perceive the risk of psychosis from their clinical evaluations. However, providing systematic and standardised evaluation methods and criteria for this work may enhance early detection and staging of treatment responses according to risk level. However, providing systematic and standardised evaluation methods and criteria for this work may enhance early detection and staging of treatment responses according to risk level. For example, although use of antipsychotic medications probably reflects accurate perception of risk of psychosis, it is not at all clear that it is optimal to use antipsychotics or when or whether it is appropriate at all for some individuals provided good psychosocial care is available. For example, in the NAPLS study sample, community clinicians provide a great deal of psychosocial care and only about 25% of CHR individuals receive antipsychotic medications (Woods et al. 2014). Moreover, a number of meta-analyses have demonstrated psychosocial treatments to be effective in reducing transition rates (van der Gaag et al. 2013).
Creating a diagnostic category of CHR or expanding awareness of risk indicators and predictive markers of imminent psychosis is urgent and crucial to the development of early psychosis identification and intervention programs in China. Although similar to findings of other follow-up studies (Broome et al. 2005; Yung et al. 2008; Simon & Umbricht, 2010; Ziermans et al. 2011) indicating that the majority of CHR participants do not actually convert to psychotic disorders, this study confirms that a sizeable percentage of non-converters still suffered with diagnosable mental health problems and functional difficulties. Even those who were remitted remained at a lower level of functioning than did the non-psychiatric participants (Addington et al. 2011). These data emphasise the importance of early detection of this syndrome. However, the new formal recognition of CHR syndromes with a less stigmatised name such as ‘psychological risk syndromes’ instead of ‘prodromal psychosis’ would be welcome in China.
Interestingly, we found that the younger participants had a significantly higher transition risk than the older ones. This result is inconsistent with many previous studies (Lemos-Giraldez et al. 2009; Fusar-Poli et al. 2012). We examined the group that was lost to follow-up and found that the oldest participants (the mean age was 26 years) were actually in this group. It is possible that our sample is a bit older than that of several foreign studies (Lemos-Giraldez et al. 2009), which might reveal that there is a peak range of psychosis onset, but not for the older participants in terms of the transition. The predictive power of family history of psychosis was not found in this study. One possible explanation for this is that information about psychosis family history may be easily overlooked or hidden (Roy et al. 1996; Milne et al. 2009) in our study participants due to the lack of mental health resources available to the older generation and the stigmatised diagnostic labels. Moreover, family history of psychosis may not predict psychosis within the time period studied.
Another important finding is that it takes approximately 4 months for CHR participants to look for professional help after becoming symptomatic, and it takes approximately 1 year to transition to psychosis after symptom onset. This implies that there is roughly an 8 month window during which to implement some possible intervention and services to prevent, make milder, or at least delay, the progress of a psychotic episode. Consistent with a long-term follow-up study (Nelson et al. 2013), the long duration of CHR symptoms is associated with a higher risk of conversion. The significant predictive factor of DUPrS found in this sample indicates the importance of early identification of CHR and leads us to call for more effective screening. Although it has been mostly argued (Larsen et al. 2001; Raven et al. 2012) that the ‘false positive’ issue may lead to unnecessary treatment and a stigmatisation label for those who are not at genuine risk, we suggest that the key point to balancing this problem is to clarify whether CHR individuals are suffering and impacted by prodromal symptoms and are looking for professional help. Thus, while screening for CHR in the general population may be currently unsupported, refining the CHR criteria in help-seeking individuals might facilitate a reduction of functional impairments and distressful experiences, and lead to a more purposeful demand for clinical intervention.
The strengths of this study include its longitudinal design, and the fact that it is the first 2-year follow-up of a Chinese CHR cohort. We had a relatively large sample size with a 2-year follow-up and were able to examine both demographic and clinical factors associated with risk of psychosis. One of the limitations of our study is that we did not have follow-up data on help-seeking individuals who did not meet CHR criteria at baseline; thus, the relative risk of CHR status above and beyond new help-seeking status is unknown. A second limitation is that the Axis I diagnosis was based on clinical judgments and doctors' medical records instead of structured interview; thus, we missed some of the details of comorbid non-psychotic disorders. Third, the information of a drop in GAF at baseline was based on retrospective ratings, which may cause over-reporting or under-reporting of functional deterioration due to recall bias. Fourth, there was a potential bias caused by the various follow-up durations among our sample due to the fixed follow-up assessment for all without considering their recruitment time, Only two follow-up assessments over a 2-year study period increases the chance of bias in recall when dating conversion; thus our results should be interpreted with caution. Furthermore, 26% attrition could introduce significant bias in the outcomes, and only 36 subjects completed the follow-up through face-to-face interviews. It is unknown if phone interviews are as valid as are face-to-face interviews. Future work needs to be based on household investigations instead of phone calls for the long-term follow-up. Finally, this sample received a naturalistic treatment, mainly the approximately 50% of the sample who were taking antipsychotics, with different compliance, and this factor may have confounded the conversion rates, limiting the generality to CHR subjects who have not taken any treatment.
Conclusions
In summary, the present findings provide evidence showing that CHR syndromes can be identified in China with a 2-year transition rate very comparable with that found in other countries. Several factors, such as functional deterioration, the severity of overall positive symptoms, DUPrS and clinical impressions of emerging psychosis may be helpful in predicting, which CHR participants are more likely to develop full psychosis. Future studies should determine whether any biomarker holds promise for predicting upcoming psychotic onset, as well as suggesting or developing possible special interventions or services specifically for this at-risk group.
Acknowledgement
None.
Financial Support
This study was supported by National Natural Science Foundation of China (81201043, 81171267, 81171280, 81261120410, 81361120403), Shanghai Science and Technology Committee (15411967200, 14411961400), National Key Clinical Disciplines at Shanghai Mental Health Center (OMA-MH, 2011-873), Shanghai Key Laboratory of Psychotic Disorders (13dz2260500), Shanghai Jiao Tong University Foundation (14JCRY04, YG2014MS40) and by a Fogarty and National Institutes of Mental Health grant (1R21 MH093294-01A1) from the USA. It was also supported by SHSMU-ION Research Center for Brain Disorders (2015NKX001), Program of Shanghai Academic Research Leader (16XD1402400) and Shanghai health system advanced appropriate technology (2013SY003).
Conflict of Interest
There are no conflicts of interest to report.
Ethical Standard
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. The project received prior approval (1978) from the Ethical Committee of the Zurich University Psychiatric Hospital.
References
- Aas IH (2010). Global assessment of functioning (GAF): properties and frontier of current knowledge. Annals of General Psychiatry 9, 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Addington J, Cadenhead KS, Cannon TD, Cornblatt B, McGlashan TH, Perkins DO, Seidman LJ, Tsuang M, Walker EF, Woods SW, Heinssen R (2007). North American Prodrome Longitudinal Study: a collaborative multisite approach to prodromal schizophrenia research. Schizophrenia Bulletin 33, 665–672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Addington J, Cornblatt BA, Cadenhead KS, Cannon TD, McGlashan TH, Perkins DO, Seidman LJ, Tsuang MT, Walker EF, Woods SW, Heinssen R (2011). At clinical high risk for psychosis: outcome for nonconverters. The American Journal of Psychiatry 168, 800–805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Addington J, Liu L, Buchy L, Cadenhead KS, Cannon TD, Cornblatt BA, Perkins DO, Seidman LJ, Tsuang MT, Walker EF, Woods SW, Bearden CE, Mathalon DH, McGlashan TH (2015). North American Prodrome Longitudinal Study (NAPLS 2): the prodromal symptoms. The Journal of Nervous and Mental Disease 203, 328–335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Broome MR, Woolley JB, Johns LC, Valmaggia LR, Tabraham P, Gafoor R, Bramon E, McGuire PK (2005). Outreach and support in south London (OASIS): implementation of a clinical service for prodromal psychosis and the at risk mental state. European Psychiatry 20, 372–378. [DOI] [PubMed] [Google Scholar]
- Cannon TD, Cadenhead K, Cornblatt B, Woods SW, Addington J, Walker E, Seidman LJ, Perkins D, Tsuang M, McGlashan T, Heinssen R (2008). Prediction of psychosis in youth at high clinical risk: a multisite longitudinal study in North America. Archives of General Psychiatry 65, 28–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fusar-Poli P, Bonoldi I, Yung AR, Borgwardt S, Kempton MJ, Valmaggia L, Barale F, Caverzasi E, McGuire P (2012). Predicting psychosis: meta-analysis of transition outcomes in individuals at high clinical risk. Archives of General Psychiatry 69, 220–229. [DOI] [PubMed] [Google Scholar]
- Larsen TK, Friis S, Haahr U, Joa I, Johannessen JO, Melle I, Opjordsmoen S, Simonsen E, Vaglum P (2001). Early detection and intervention in first-episode schizophrenia: a critical review. Acta Psychiatrica Scandinavica 103, 323–334. [DOI] [PubMed] [Google Scholar]
- Lemos-Giraldez S, Vallina-Fernandez O, Fernandez-Iglesias P, Vallejo-Seco G, Fonseca-Pedrero E, Paino-Pineiro M, Sierra-Baigrie S, Garcia-Pelayo P, Pedrejon-Molino C, Alonso-Bada S, Gutierrez-Perez A, Ortega-Ferrandez JA (2009). Symptomatic and functional outcome in youth at ultra-high risk for psychosis: a longitudinal study. Schizophrenia Research 115, 121–129. [DOI] [PubMed] [Google Scholar]
- Loewy RL, Bearden CE, Johnson JK, Raine A, Cannon TD (2005). The prodromal questionnaire (PQ): preliminary validation of a self-report screening measure for prodromal and psychotic syndromes. Schizophrenia Research 79, 117–125. [PubMed] [Google Scholar]
- McGlashan T, Walsh B, Woods S (2010). The Psychosis-Risk Syndrome: Handbook for Diagnosis and Follow-up. Oxford University Press: New York. [Google Scholar]
- Melle I, Larsen TK, Haahr U, Friis S, Johannessen JO, Opjordsmoen S, Simonsen E, Rund BR, Vaglum P, McGlashan T (2004). Reducing the duration of untreated first-episode psychosis: effects on clinical presentation. Archives of General Psychiatry 61, 143–150. [DOI] [PubMed] [Google Scholar]
- Miller TJ, McGlashan TH, Rosen JL, Somjee L, Markovich PJ, Stein K, Woods SW (2002). Prospective diagnosis of the initial prodrome for schizophrenia based on the Structured Interview for Prodromal Syndromes: preliminary evidence of interrater reliability and predictive validity. The American Journal of Psychiatry 159, 863–865. [DOI] [PubMed] [Google Scholar]
- Miller TJ, McGlashan TH, Rosen JL, Cadenhead K, Cannon T, Ventura J, McFarlane W, Perkins DO, Pearlson GD, Woods SW (2003). Prodromal assessment with the structured interview for prodromal syndromes and the scale of prodromal symptoms: predictive validity, interrater reliability, and training to reliability. Schizophrenia Bulletin 29, 703–715. [DOI] [PubMed] [Google Scholar]
- Milne BJ, Caspi A, Crump R, Poulton R, Rutter M, Sears MR, Moffitt TE (2009). The validity of the family history screen for assessing family history of mental disorders. American Journal of Medical Genetics. Part B, Neuropsychiatric Genetics 150B, 41–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson B, Yuen HP, Wood SJ, Lin A, Spiliotacopoulos D, Bruxner A, Broussard C, Simmons M, Foley DL, Brewer WJ, Francey SM, Amminger GP, Thompson A, McGorry PD, Yung AR (2013). Long-term follow-up of a group at ultra high risk (“prodromal”) for psychosis: the PACE 400 study. JAMA Psychiatry 70, 793–802. [DOI] [PubMed] [Google Scholar]
- Perkins DO, Gu H, Boteva K, Lieberman JA (2005). Relationship between duration of untreated psychosis and outcome in first-episode schizophrenia: a critical review and meta-analysis. The American Journal of Psychiatry 162, 1785–1804. [DOI] [PubMed] [Google Scholar]
- Rajji TK, Mulsant BH (2008). Nature and course of cognitive function in late-life schizophrenia: a systematic review. Schizophrenia Research 102, 122–140. [DOI] [PubMed] [Google Scholar]
- Raven M, Stuart GW, Jureidini J (2012). ‘Prodromal’ diagnosis of psychosis: ethical problems in research and clinical practice. The Australian and New Zealand Journal of Psychiatry 46, 64–65. [DOI] [PubMed] [Google Scholar]
- Roy MA, Walsh D, Kendler KS (1996). Accuracies and inaccuracies of the family history method: a multivariate approach. Acta Psychiatrica Scandinavica 93, 224–234. [DOI] [PubMed] [Google Scholar]
- Schultze-Lutter F, Ruhrmann S, Berning J, Maier W, Klosterkotter J (2010). Basic symptoms and ultrahigh risk criteria: symptom development in the initial prodromal state. Schizophrenia Bulletin 36, 182–191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simon AE, Umbricht D (2010). High remission rates from an initial ultra-high risk state for psychosis. Schizophrenia Research 116, 168–172. [DOI] [PubMed] [Google Scholar]
- Solis M (2014). Prevention: before the break. Nature 508, S12–S13. [DOI] [PubMed] [Google Scholar]
- Thompson A, Nelson B, Yung A (2011). Predictive validity of clinical variables in the “at risk” for psychosis population: international comparison with results from the North American Prodrome Longitudinal Study. Schizophrenia Research 126, 51–57. [DOI] [PubMed] [Google Scholar]
- van der Gaag M, Smit F, Bechdolf A, French P, Linszen DH, Yung AR, McGorry P, Cuijpers P (2013). Preventing a first episode of psychosis: meta-analysis of randomized controlled prevention trials of 12 month and longer-term follow-ups. Schizophrenia Research 149, 56–62. [DOI] [PubMed] [Google Scholar]
- van der Werf M, Hanssen M, Kohler S, Verkaaik M, Verhey FR, van Winkel R, van Os J, Allardyce J (2014). Systematic review and collaborative recalculation of 133,693 incident cases of schizophrenia. Psychological Medicine 44, 9–16. [DOI] [PubMed] [Google Scholar]
- Velthorst E, Nieman DH, Becker HE, van de Fliert R, Dingemans PM, Klaassen R, de Haan L, van Amelsvoort T, Linszen DH (2009). Baseline differences in clinical symptomatology between ultra high risk subjects with and without a transition to psychosis. Schizophrenia Research 109, 60–65. [DOI] [PubMed] [Google Scholar]
- Woods SW, Walsh BC, Addington J, Cadenhead KS, Cannon TD, Cornblatt BA, Heinssen R, Perkins DO, Seidman LJ, Tarbox SI, Tsuang MT, Walker EF, McGlashan TH (2014). Current status specifiers for patients at clinical high risk for psychosis. Schizophrenia Research 158, 69–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yung AR, Phillips LJ, Yuen HP, McGorry PD (2004). Risk factors for psychosis in an ultra high-risk group: psychopathology and clinical features. Schizophrenia Research 67, 131–142. [DOI] [PubMed] [Google Scholar]
- Yung AR, Yuen HP, McGorry PD, Phillips LJ, Kelly D, Dell'Olio M, Francey SM, Cosgrave EM, Killackey E, Stanford C, Godfrey K, Buckby J (2005). Mapping the onset of psychosis: the comprehensive assessment of at-risk mental states. The Australian and New Zealand Journal of Psychiatry 39, 964–971. [DOI] [PubMed] [Google Scholar]
- Yung AR, Nelson B, Stanford C, Simmons MB, Cosgrave EM, Killackey E, Phillips LJ, Bechdolf A, Buckby J, McGorry PD (2008). Validation of “prodromal” criteria to detect individuals at ultra high risk of psychosis: 2 year follow-up. Schizophrenia Research 105, 10–17. [DOI] [PubMed] [Google Scholar]
- Zhang T, Li H, Woodberry KA, Seidman LJ, Zheng L, Zhao S, Tang Y, Guo Q, Lu X, Zhuo K, Qian Z, Chow A, Li C, Jiang K, Xiao Z, Wang J (2014). Prodromal psychosis detection in a counseling center population in China: an epidemiological and clinical study. Schizophrenia Research 152, 391–399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng L, Wang J, Zhang T, Li H, Li C, Jiang K (2012). The Chinese version of the SIPS/SOPS: a pilot study of reliability and validity. Chinese Mental Health Journal 26, 571–576. [Google Scholar]
- Ziermans TB, Schothorst PF, Sprong M, van Engeland H (2011). Transition and remission in adolescents at ultra-high risk for psychosis. Schizophrenia Research 126, 58–64. [DOI] [PubMed] [Google Scholar]