Abstract
Aims.
A subset of people with co-occurring substance use and mental disorders require coordinated support from health, social welfare and justice agencies to achieve diversion from homelessness, criminal recidivism and further health and social harms. Integrated models of care are typically concentrated in large urban centres. The present study aimed to empirically measure the prevalence and distribution of complex co-occurring disorders (CCD) in a large geographic region that includes urban as well as rural and remote settings.
Methods.
Linked data were examined in a population of roughly 3.7 million adults. Inclusion criteria for the CCD subpopulation were: physician diagnosed substance use and mental disorders; psychiatric hospitalisation; shelter assistance; and criminal convictions. Prevalence per 100 000 was calculated in 91 small areas representing urban, rural and remote settings.
Results.
2202 individuals met our inclusion criteria for CCD. Participants had high rates of hospitalisation (8.2 admissions), criminal convictions (8.6 sentences) and social assistance payments (over $36 000 CDN) in the past 5 years. There was wide variability in the geographic distribution of people with CCD, with high prevalence rates in rural and remote settings.
Conclusions.
People with CCD are not restricted to areas with large populations or to urban settings. The highest per capita rates of CCD were observed in relatively remote locations, where mental health and substance use services are typically in limited supply. Empirically supported interventions must be adapted to meet the needs of people living outside of urban settings with high rates of CCD.
Key words: Epidemiology, forensic psychiatry, health service research, psychoactive substance use disorder
Introduction
The co-occurrence of mental illness and substance use is associated with increased risk of criminal conviction (Baillargeon et al. 2009a; Ruiz et al. 2012; Rezansoff et al. 2013), unemployment (Visher et al. 2005), as well as poverty and homelessness (Fazel et al. 2014). The prevalence of co-occurring substance use and mental disorders is 2.5% in the general US population (SAMHSA, 2007) but 49% in US jails (James & Glaze, 2006). Criminality and co-occurring disorders are often mutually exacerbating and together they contribute to additional risks, including suicide (Baillargeon et al. 2009b) and mortality on release from prison (Kariminia et al. 2007).
An important subpopulation experiences the confluence of mental illness, substance dependence, corrections involvement and homelessness (or precarious housing) and can be described as having complex co-occurring disorders (CCD). Individuals with CCD require coordinated professional supports in order to address inter-dependent medical, psychiatric, housing, social and legal issues. Service models that have empirical support for people with CCD include specialised courts, such as mental health (McNiel & Binder, 2007) and drug treatment court (Somers et al. 2012, 2013b), Forensic Assertive Community Treatment (Cusack et al. 2010) and certain models of supported housing such as Housing First (Tsemberis et al. 2012; Somers et al. 2013a). In each case, these service models involve collaborative care spanning diverse professional and community resources.
Front-line service providers (e.g., police and clinicians) have sounded alarm that the number of individuals with CCD is increasing (Szkopek-Szkopowski et al. 2013). In the absence of sufficient appropriate resources, the justice system can be the primary point of engagement in the lives of people with CCD (Steadman et al. 2009). There are few empirically derived estimates of the prevalence and geographic distribution of CCD. Previous research has found that people with severe mental illnesses are more likely to change their location than individuals with serious physical illnesses (Lix et al. 2006), and that people with mental illness often move to locations where they have previously received care (Lamont et al. 2000). Several studies have reported concentrations of people with CCD in urban centres (Culhane et al. 1996; Luciano et al. 2014). But it is not clear how people with CCD are distributed over large regions, and if they are relatively less prevalent in rural and remote settings compared with urban centres. This information has crucial implications for the location and delivery of relevant interventions. In order to add to this area of knowledge, the present study examined the prevalence and geographic distribution of CCD in a large Canadian province (over 900 000 km2) with an adult population of approximately 3.7 million people. The goal of this study was to empirically estimate the rate and geographic distribution of individuals with CCD.
Method
Data sources
We examined linked administrative data spanning three provincial government ministries: justice, health services, and social development and social innovation. The respective ministries are responsible for comprehensive health, justice and social services to the entire adult population in the province of British Columbia (BC), Canada. The completeness of these data reflects the central organisational and funding role provided by the provincial government in the administration of these various services.
Non-identifying data were provided by the Government of BC through the Inter-Ministry Research Initiative (IMRI)
The purpose of the IMRI is to produce knowledge that supports the development and evaluation of multi-agency programmes involving the health and justice sectors. The IMRI is governed by Information Sharing Agreements between the partnering ministries and the host university. Planned analyses were reviewed and developed by a Steering Committee with representatives from each of the partnering institutions. Access to data is restricted to a designated secure off-line environment and is subject to police security clearance and other provisions to protect privacy. The present analysis used de-identified linked data spanning from 1997 to 2012.
Study population
The population available for analysis consisted of all individuals who had at least one conviction (including bail) between April 1st 1997 and March 31st 2012. We included only those individuals who were at least 18 years of age as of April 1st 2007, and who were not deceased prior to March 31st 2012 (the 5-year period used for observations in this study). Only individuals with linkable health records were included.
Variable details
Residents of BC are required to enrol with the Provincial Medical Services Plan (MSP). Hospital admissions and physician services are reported to the Provincial Ministry of Health, along with diagnostic details related to each admission or outpatient visit. The Ministry of Social Development and Social Innovation administers and records financial support to citizens based on demonstration of need, including shelter payments for those in need of housing. Details related to criminal convictions, including length of sentence in custody or community, are retained by the Ministry of Justice.
MSP records based on the International Classification of Diseases, 9th edition (ICD-9) were examined for physician diagnosed mental disorders between April 1st, 2007 and March 31st, 2012. All disorders were included within the ICD-9 range of 290–319 (mental disorders). Substance-related disorders were identified using the three-digit codes of 291, 292, 303, 304 and 305. Non-substance-related disorders consisted of all other codes within the range identified. Further details concerning these variables are described elsewhere (Rezansoff et al. 2013; Somers et al. 2013a, b).
CCD inclusion criteria
Integrating the domains of health, social assistance and criminality, we selected the following criteria to define the CCD sub-population. The date range for all sources of data was between April 1st, 2007 and March 31st, 2012:
-
(1)
At least one psychiatric hospitalisation (including substance-related admissions);
-
(2)
And at least two MSP encounters involving diagnoses of mental disorders (excluding substance use disorders);
-
(3)
And at least two MSP encounters involving diagnoses of substance use disorders;
-
(4)
And at least two convictions (delivered by any Provincial Court);
-
(5)
And at least $5000 (CAD) in shelter payments.
Analysis
We first identified the total number of individuals meeting CCD inclusion criteria (above). Socio-demographic and service use characteristics were compared between the CCD sub-population and the remainder of the eligible offender population. Parametric tests (e.g., Student's t test) were used to compare continuous variables among groups. Chi-square tests (non-parametric) were used to examine relationships between categorical variables (such as gender and ethnicity) and the CCD groups. The regional distribution of the CCD sub-population was tabulated and examined at four geographic levels of increasing size: local health area (LHA); health service delivery area (HSDA); regional health authority (HA); total province (see maps in Appendices 1–3). For each individual, location was based on the most recent year of observation. For each region, the rate of CCD was estimated using the total number of CCD cases divided by the total adult population and expressed as a rate per 100 000. The adult population included all individuals who were at least 20 years of age or older in 2012. Population estimates (as of 2012) for the entire province as well as for each geographical area were obtained from BCStats (2013).
Results
Characteristics of the overall offender population (n = 188 625) alongside the CCD sub-population (n = 2202) are listed in Table 1. Significance tests were conducted comparing those who met the CCD inclusion criteria with all other offenders (non-CCD participants). Results indicate that CCD and non-CCD individuals differed significantly on all variables examined. Compared with the non-CCD population, those who met the CCD criteria were younger, less well educated, more likely to be female, more likely to be aboriginal (descendants of original inhabitants) and less likely to be of other (i.e., neither white nor aboriginal) ethnicity. Members of the CCD sample were ten times more likely than others to have been diagnosed with Schizophrenia (41% v. 4%) and personality disorders (30% v. 3%) and six times more likely to have been diagnosed with drug dependence (86% v. 14%) and alcohol dependence (58% v. 9%). Those in the CCD subsample had eight times as many sentences as other offenders (8.6 v. 1.1), six times as many violent offences (1.2 v. 0.2) and nearly 50 times the number of psychiatric admissions (4.9 v. 0.1). Finally, those in the CCD group received approximately four times as much financial support as other offenders for shelter (19 155 v. 4968) and in total (36 258 v. 8798). Although our inclusion criteria included at least one psychiatric hospitalisation and at least two criminal convictions, the observed amounts greatly exceeded our minimal inclusion levels (means of 4.9 and 8.6, respectively). As appropriate, the values presented in Table 1 are either means with standard deviations (s.d.), or numbers of participants (n) with percentages (%) represented by each category.
Table 1.
Comparisons of socio-demographic and other related characteristics between CCD clients and non-CCD clients
| Variablesa | All participants (n = 188 625) Mean (s.d.) or n (%) | Non-CCD participants (n = 186 423) Mean (s.d.) or n (%) | CCD participants (n = 2202) Mean (s.d.) or n (%) | P value |
|---|---|---|---|---|
| Age at enrolment in yearsb | ||||
| Mean (s.d.) | 37.7 (11.8) | 37.7 (11.8) | 34.0 (9.5) | <0.001 |
| Gender* | ||||
| Male | 154 290 (82) | 152 721 (82) | 1569 (71) | <0.001 |
| Female | 34 305 (18) | 33 672 (18) | 633 (29) | |
| Ethnicity* | ||||
| Caucasian | 115 639 (68) | 114 113 (68) | 1526 (71) | <0.001 |
| Aboriginals | 25 132 (15) | 24 649 (15) | 483 (22) | |
| Other | 28 137 (17) | 27 988 (17) | 149 (7) | |
| Education level* | ||||
| Grade 9 or less | 19 499 (13) | 19 150 (12) | 349 (17) | <0.001 |
| Grade 10/11 | 46 589 (30) | 45 839 (30) | 750 (36) | |
| Grade 12 | 61 288 (39) | 60 571 (40) | 717 (34) | |
| Vocational/University | 28 209 (18) | 27 945 (18) | 264 (13) | |
| Specific mental disorders*c | ||||
| Schizophrenia | 8047 (4) | 7153 (4) | 894 (41) | <0.001 |
| Bipolar disorder | 15 276 (8) | 14 036 (7) | 1240 (56) | <0.001 |
| Personality disorder | 5745 (3) | 5090 (3) | 655 (30) | <0.001 |
| Anxiety disorder | 38 422 (20) | 36 800 (20) | 1622 (74) | <0.001 |
| Drug dependence | 28 510 (15) | 26 262 (14) | 1888 (86) | <0.001 |
| Alcohol dependence | 17 577 (9) | 16 283 (9) | 1274 (58) | <0.001 |
| Any sentence in past 5 years | ||||
| Mean (s.d.) | 1.2 (3.6) | 1.1 (3.4) | 8.6 (8.8) | <0.001 |
| Median (Min, Max) | 0 (0, 95) | 0 (0, 71) | 5 (2, 95) | |
| Jail sentence in past 5 years | ||||
| Mean (s.d.) | 0.5 (1.7) | 0.5 (2.2) | 4.2 (6.1) | <0.001 |
| Median (Min, Max) | 0 (0, 66) | 0 (0, 48) | 5 (2, 95) | |
| Probation sentence in past 5 years | ||||
| Mean (s.d.) | 0.7 (1.7) | 0.6 (1.6) | 4.4 (3.9) | <0.001 |
| Median (Min, Max) | 0 (0, 48) | 0 (0, 48) | 3 (0, 37) | |
| Any offence in past 5 years | ||||
| Mean (s.d.) | 0.9 (2.7) | 0.9 (2.5) | 6.6 (6.7) | <0.001 |
| Median (Min, Max) | 0 (0, 70) | 0 (0, 54) | 4 (0, 70) | |
| Property offence in past 5 years | ||||
| Mean (s.d.) | 0.3 (1.3) | 0.3 (1.3) | 2.4 (3.7) | <0.001 |
| Median (Min, Max) | 0 (0, 48) | 0 (0, 48) | 1 (0, 41) | |
| Violent offence in past 5 years | ||||
| Mean (s.d.) | 0.2 (0.7) | 0.2 (0.7) | 1.2 (1.7) | <0.001 |
| Median (Min, Max) | 0 (0, 22) | 0 (0, 22) | 1 (0, 18) | |
| Acute hospital admission in past 5 years | ||||
| Mean (s.d.) | 0.6 (1.7) | 0.5 (1.6) | 3.2 (4.0) | <0.001 |
| Median (Min, Max) | 0 (0, 64) | 0 (0, 64) | 3 (1, 58) | |
| Psychiatricd hospital admission in past 5 years | ||||
| Mean (s.d.) | 0.2 (1.0) | 0.1 (0.7) | 4.9 (5.3) | <0.001 |
| Median (Min, Max) | 0 (0, 61) | 0 (0, 61) | 2 (1, 44) | |
| Hospital days in past 5 years | ||||
| Mean (s.d.) | 4.2 (20.9) | 3.9 (20.0) | 32.7 (53.3) | <0.001 |
| Median (Min, Max) | 0 (0, 970) | 0 (0, 970) | 13 (1, 755) | |
| MSP costs in past 5 years ($CAD) | ||||
| Mean (s.d.) | 2798 (4522) | 2709 (4381) | 10 357 (8331) | <0.001 |
| Social assistance in past 5 years ($CAD) | ||||
| Mean (s.d.) | 9119 (18 603) | 8798 (18 365) | 36 258 (18 652) | <0.001 |
| Shelter payments in past 5 years ($CAD) | ||||
| Mean (s.d.) | 5135 (10 034) | 4968 (9930) | 19 155 (8724) | <0.001 |
Variables with * was presented in terms of counts (N) and proportions (%). All other variables were presented in terms of mean with standard deviation (s.d.) and median with minimum (Min) and maximum (Max).
Age was calculated at April 1st of 2007.
Specific mental disorders were not mutually exclusive.
Related to non substance-related or substance-related mental disorders.
Geographic distribution
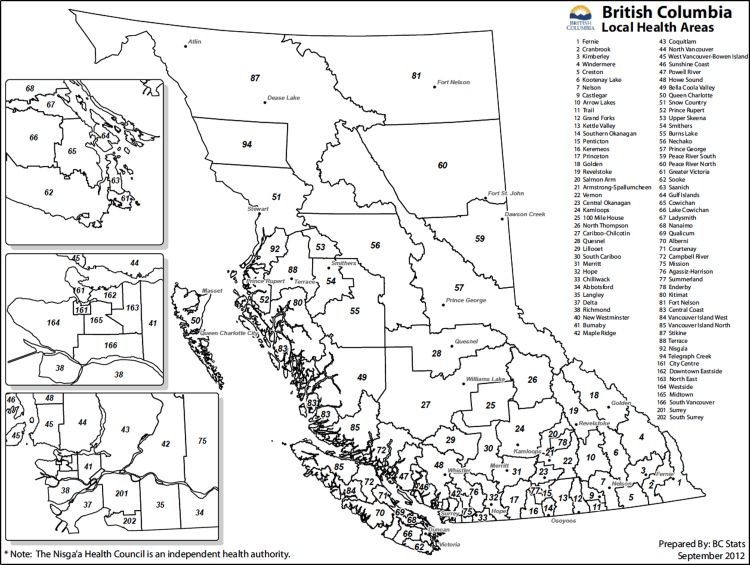
We examined the geographic distribution of those who met all of the CCD criteria (i.e., mental disorders, substance use disorders, criminal convictions, psychiatric hospitalisations and shelter support). Results are tabulated beginning with LHA (see map, Appendix 1), which represent the smallest available geographic units used to organise data by the BC Ministry of Health, BC Stats, Statistics Canada and the Canadian Institute for Health Information. LHAs are also used to examine and compare the health of communities in different parts of BC. There are 89 LHAs representing adult populations ranging from 420 to over 300 000 people over 19 years of age. Results were then aggregated into 16 HSDAs (see map, Appendix 2) and then the five geographic HAs (see map, Appendix 3). In each table, we included the size of the adult (20 years and older) population as of 2012 and reported the prevalence of CCD per 100 000 adults. At the provincial level (adult population 3 660 314) the prevalence of CCD was 60 per 100 000 adults.
LHA
The number of people in each LHA meeting the CCD criteria is listed in Table 2. LHAs are arranged in rows from those with the highest number of CCD individuals to those with the fewest. No results are shown for LHAs in which fewer than 15 people met the inclusion criteria. As expected, the highest rate was observed in the most urbanised region of the Province – the Downtown Eastside of Vancouver (330/100 000). The designation ‘Vancouver Unknown Place’ includes people with no fixed address, encompassing those who are homeless. The results indicate that the prevalence of CCD varied considerably between LHAs, and was not reliably related to geographic location in the province or population size. For example, regions of Greater Vancouver had relatively high rates in some instances (Downtown Eastside: 330/100 000) and relatively low rates in others (Burnaby 25/100 000). As a further reflection of geographic diversity, the threshold of at least 100 cases per 100 000 was exceeded in LHAs with relatively small populations (roughly 10 000 adults) as well as those with adult populations five times as large.
Table 2.
Prevalence of CCD by LHA in BC
| Local health area (LHA) | n | Total adult population | Rate (n/100 000) |
|---|---|---|---|
| Downtown eastside | 210 | 63 597 | 330 |
| Vancouver unknown place | 170 | ||
| Surrey | 168 | 307 678 | 55 |
| Greater Victoria | 122 | 185 729 | 66 |
| Prince George | 105 | 74 621 | 141 |
| Central Okanagan | 92 | 149 766 | 61 |
| Abbotsford | 85 | 105 277 | 81 |
| Kamloops | 69 | 88 281 | 78 |
| City Centre (Vancouver) | 65 | 112 779 | 58 |
| Maple Ridge | 54 | 73 836 | 73 |
| Nanaimo | 53 | 85 625 | 62 |
| Burnaby | 47 | 188 690 | 25 |
| Chilliwack | 45 | 66 470 | 68 |
| Coquitlam | 45 | 174 459 | 26 |
| Vernon | 43 | 52 322 | 82 |
| Midtown (Vancouver) | 36 | 82 189 | 44 |
| South Vancouver | 36 | 109 577 | 33 |
| Cowichan | 33 | 45 291 | 73 |
| Mission | 32 | 32 359 | 99 |
| Alberni | 30 | 24 859 | 121 |
| Langley | 30 | 102 534 | 29 |
| North Vancouver | 30 | 113 325 | 26 |
| North East | 29 | 89 965 | 32 |
| Richmond | 29 | 158 713 | 18 |
| Penticton | 26 | 34 102 | 76 |
| Delta | 26 | 78 088 | 33 |
| New Westminster | 24 | 56 389 | 43 |
| Unknown LHA | 24 | ||
| Quesnel | 23 | 18 530 | 124 |
| Terrace | 21 | 15 412 | 136 |
| Nelson | 20 | 20 242 | 99 |
| Campbell River | 20 | 33 182 | 60 |
| Sunshine Coast | 17 | 25 186 | 67 |
| Peace River North | 17 | 26 262 | 65 |
| Vancouver Island North | 16 | 9157 | 175 |
| Prince Rupert | 16 | 10 559 | 152 |
| Nechako | 16 | 11 043 | 145 |
| Courtenay | 16 | 52 170 | 31 |
| Powell River | 15 | 16 405 | 91 |
| Peace River South | 15 | 21 699 | 69 |
| Sooke | 15 | 55 585 | 27 |
| South Surrey/White Rock | – | 72 398 | – |
| Trail | – | 15 464 | – |
| Saanich | – | 52 715 | – |
| West Side | – | 112 678 | – |
| Salmon Arm | – | 28 139 | – |
| Qualicum | – | 38 870 | – |
| Merritt | – | 9231 | – |
| Cranbrook | – | 20 120 | – |
| Howe Sound | – | 29 592 | – |
| Smithers | –- | 11 983 | – |
| Cariboo – Chilcotin | – | 20 592 | – |
| Gulf Islands | – | 13 833 | – |
| Upper Skeena | – | 3814 | – |
| Castlegar | – | 10 860 | – |
| Ladysmith | – | 15 647 | – |
| West Vancouver-Bowen Island | – | 42 495 | – |
| Burns Lake | – | 5906 | – |
| Agassiz – Harrison | – | 7053 | – |
| Kitimat | – | 7730 | – |
| Queen Charlotte | – | 3585 | – |
| Fort Nelson | – | 4772 | – |
| South Cariboo | – | 5952 | – |
| 100 Mile House | – | 12 276 | – |
| Southern Okanagan | – | 16 440 | – |
| Arrow Lakes | – | 4064 | – |
| Keremeos | – | 4334 | – |
| Lake Cowichan | – | 5217 | – |
| Enderby | – | 6053 | – |
| Hope | – | 6507 | – |
| Summerland | – | 9261 | – |
| Fernie | – | 11 786 | – |
| Kimberley | – | 6899 | – |
| Armstrong – Spallumcheen | – | 7560 | – |
| Snow Country | – | 420 | – |
| Central Coast | – | 1150 | – |
| Nisga'a | – | 1416 | – |
| Vancouver Island West | – | 1852 | – |
| Lillooet | – | 3666 | – |
| Princeton | – | 4512 | – |
| Golden | – | 5779 | – |
| Revelstoke | – | 6370 | – |
| Grand Forks | – | 7213 | – |
| Windermere | – | 8625 | – |
| Telegraph Creek | – | 531 | – |
| Stikine | – | 784 | – |
| Bella Coola Valley | – | 2293 | – |
| Kettle Valley | – | 3103 | – |
| Kootenay Lake | – | 3252 | – |
| North Thompson | – | 3378 | – |
| Creston | – | 10 191 | – |
| Overall/total in BC | 2202 | 3 660 314 | 60 |
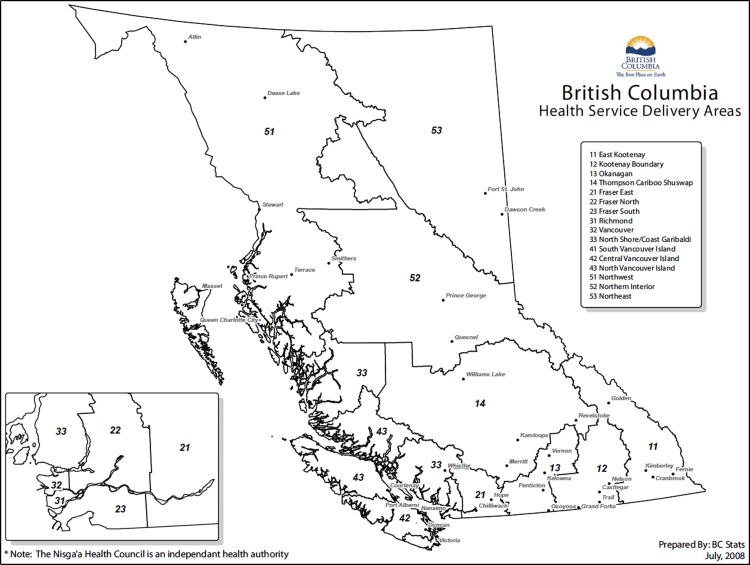
HSDA
HSDAs (see Appendix 2) are comprised between one and ten LHAs, based largely on relative remoteness and population density. Table 3 presents HSDAs alongside the number of individuals meeting inclusion criteria and the rate per 100 000 adults. The city of Vancouver had the highest absolute number of people who met the CCD criteria. Note that we present two samples corresponding to the City of Vancouver, one based on those individuals with a known LHA (n = 388) and a second that includes people whose address was unknown (n = 588). Individuals who are homeless (and thus lack a fixed address) are included in the second sample. Although higher absolute numbers of CCD individuals were identified in regions with higher overall populations, the highest rates per 100 000 were observed in the less urbanised Northern Interior and Northwest of the Province.
Table 3.
Prevalence of CCD by HSDA in BC
| Health service delivery area (HSDA) | n | Total adult population | Rate (n/100 000) |
|---|---|---|---|
| Vancouver | 388 | 570 785 | 68 |
| Fraser South | 237 | 560 698 | 42 |
| Okanagan | 177 | 284 350 | 62 |
| Fraser East | 170 | 217 666 | 78 |
| Fraser North | 170 | 493 374 | 34 |
| South Vancouver Island | 156 | 307 862 | 51 |
| Northern Interior | 149 | 110 100 | 135 |
| Central Vancouver Island | 136 | 215 509 | 63 |
| Thompson Cariboo Shuswap | 108 | 177 885 | 61 |
| North Shore/Coast Garibaldi | 78 | 230 446 | 34 |
| Northwest | 62 | 56 234 | 110 |
| North Vancouver Island | 53 | 96 361 | 55 |
| Kootenay Boundary | 42 | 64 198 | 65 |
| Northeast | 36 | 52 733 | 68 |
| Richmond | 29 | 158 713 | 18 |
| East Kootenay | 17 | 63 400 | 27 |
| Vancouver including Vancouver unknown place | 388 | 570 785 | 98 |
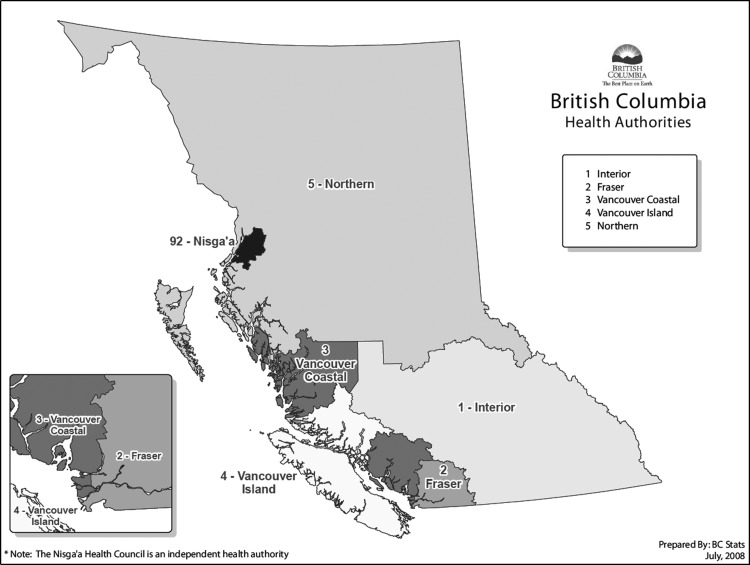
Regional HAs
BC is divided into five regional HAs (see Appendix 3). The total number and rate of people with CCD in each HA is shown in Table 4. As was seen with the results from HSDAs, the greatest numbers of individuals meeting CCD criteria were located in the most populous HAs. However, as in the preceding analyses the highest prevalence rate of CCD was observed in the comparatively rural Northern HA, which is the HA with the smallest and most dispersed total population.
Table 4.
Prevalence of CCD by HA in BC
| Health authority (HA) | N | Total adult population | Rate (n/100 000) |
|---|---|---|---|
| Interior HA | 344 | 589 833 | 58 |
| Fraser HA | 577 | 1 271 738 | 45 |
| Vancouver Coastal HA | 495 | 959 944 | 52 |
| Vancouver Island HA | 345 | 619 732 | 56 |
| Northern HA | 247 | 219 067 | 113 |
| Vancouver Coastal HA including Vancouver unknown place | 665 | 959 944 | 69 |
Discussion
This study is one of the first to investigate the prevalence and distribution of people with CCD defined on the basis of diagnosed substance dependence and non-substance-related mental disorders, and psychiatric hospitalisations, and multiple criminal convictions and financial need for housing. We found that the largest absolute numbers of people meeting all of these criteria were concentrated in densely populated regions where the high prevalence of CCD has been reported based on police encounters (Thompson, 2010) as well as academic research (Patterson et al. 2012). However, we also found that not all populous regions had commensurately high absolute numbers of CCD individuals. Moreover, we found that the highest per capita rates of CCD were observed in comparatively rural and remote regions. Taken together, these findings suggest the need for service planning and inter-agency collaboration in diverse regions, both urban and rural, and counter the hypothesis that the service requirements of CCD individuals are limited to inner-city settings.
The 5-year provincial rate of CCD was 60 per 100 000 (2202 individuals in an adult population of 3.7 million). Per capita, the rate of CCD in the rural and least populous HA was about two and a half times higher than the rate in the most heavily populated and urbanised HA. Large variations in rates were also observed within each HA when comparing the constituent LHAs. In LHAs serving at least 50 000 people the rate of CCD varied more than 20 times, from fewer than 15–330 cases per 100 000. This demonstration of variability is a strong indication that the allocation of specialised resources should be informed by empirical details concerning local populations.
These findings confirm the need for coordinated inter-agency resources involving health, justice and social services for the large numbers of individuals with CCD who are concentrated in urban settings. But they also demonstrate the need to implement similar collaborative approaches in less populated environments. Several empirically supported programmes for sub-populations with complex psychiatric needs have been adapted for both urban and rural contexts, including housing first (Stefancic et al. 2013), assertive community treatment (Aagard & Müller-Nielsen, 2011) and specialised courts (Hiday & Ray, 2010). However, the implementation of specialised services is more common in urban settings, due to a number of factors such as popular support, the availability of relevant experts and their proximity to institutional resources, champions for reform, including police and front-line service providers (e.g., Szkopek-Szkopowski et al. 2013) and the sheer visibility of problems related to CCD. Moreover, it is unclear whether the concentration of inter-agency resources in urban areas contributes to relocation of individuals with CCD from other locations (Lix et al. 2006).
The characteristics of people who met our CCD criteria confirm the seriousness and severity of needs within the sample. During a 5-year period members of the sample had an average of nine convictions and five psychiatric hospital admissions per person. Personality disorders and Schizophrenia were ten times more common in the CCD sample than among other offenders, and they were six times more likely to have been diagnosed with alcohol dependence and drug dependence. The rate of violent offences was six times higher in the CCD sample compared with other convicted offenders. Payments for shelter, other social assistance and physician visits were also significantly higher in the CCD sample. Compared with other offenders, the CCD group was significantly younger, more likely to be female and of aboriginal ethnicity and less well educated. Appropriate therapeutic interventions are urgently needed to divert this relatively youthful cohort from a chaotic and costly revolving door of health and justice services (Baillargeon et al. 2009a). Females and aboriginal (or indigenous) people are increasingly prevalent in offender populations (Harrison et al. 2005; Kong & Au Coin, 2008; Landry & Sinha, 2008). The over-representation of both groups in the CCD subpopulation suggests the need for preventative as well as treatment programmes that are responsive to cultural and gender-based considerations.
The present analysis indicates that the raw number of CCD individuals varies regionally. Further work is required to establish whether the characteristics of CCD offenders in different regions might differ on factors such as diagnostic severity, propensity to violence, psychopathy, chronicity of homelessness, etc. Nevertheless, the present analysis provides an empirically based estimate of the prevalence and distribution of those with CCD. The delivery of services to this population requires a focus on contextual factors so that interventions are maximally responsive to individual risks and needs (Andrews & Dowden, 2007).
This research was made possible by the ability to link population-level data spanning several years for relevant services that are universally provided. Selection criteria for inclusion in this study were chosen in order to identify people who share similar profiles of need regardless of their specific location. Nevertheless our study is subject to a number of limitations associated with our methodology and approach. The use of administrative data to operationalise CCD inevitably fails to include people who do not come into contact with services. It is therefore likely that our results form an underestimate of the prevalence of CCD. We attempted to avoid criteria that may have biased the sample due to regional variation in access to services. For example, we did not include psychiatric consultations in our criteria due to the grossly uneven distribution of specialists. But despite our efforts, it remains possible that our inclusion criteria may have been biased by regional differences in the provision of services. Community mental health and addiction services are not evenly distributed throughout the large geography of BC. It is therefore possible that individuals in more rural setting may have a higher likelihood of hospitalisation (one of our CCD criteria) due to insufficient community-based care. We used physician diagnoses as the basis for identifying mental and substance use disorders, which may reflect errors of under-diagnosis and/or over-diagnosis. However, the fact that the sample had multiple psychiatric hospitalisations is an indication that if we erred at all, it was towards the inclusion of severe psychiatric cases, rather than people without mental illness who had been wrongly diagnosed. We interpret our results as indicative of regional clusters and nodes of CCD throughout a large and variably populated landscape. Further research is necessary to investigate the distribution of CCD in other settings in Canada and internationally. Our results demonstrate that administrative data may be a useful asset to help direct the implementation of specialised offender services to locations with relatively greater need. Finally, our analyses represent a step towards better understanding a sub-population with concurrent disorders and socio-legal needs. Further research will undoubtedly lead to refinements in the criteria that best identify relevant forms of ‘complexity’ among people with substance use and mental disorders.
The confluence of mental illness, substance use, crime and poverty has been identified as an extremely costly revolving door, measurable in financial terms (Gilmer et al. 2010) and in greatly premature mortality (Nielsen et al. 2011; Nusselder et al. 2013). The implementation of effective interventions can be defended on the basis of the best interests of individual offenders, fiscal prudence and community safety. Our findings suggest that it is important to provide those employed in health, justice and social services with the education and support to assist people with CCD, knowing that such individuals are likely to present in all regions, and understanding that the costs of inadequate care are unsustainable.
Acknowledgements
The authors gratefully acknowledge support of the British Columbia Inter-Ministry Research Initiative and members of the IMRI Steering Committee.
Appendix 1: British Columbia Local Health Areas
Appendix 2: British Columbia Health Service Delivery Areas
Appendix 3: British Columbia Health Authorities
Financial Support
Grant support was provided by the Forensic Psychiatric Services Commission of British Columbia.
Conflict of interest
The authors have no conflicts of interest or other disclosures.
Ethics standard
This study was approved by the Research Ethics Board of Simon Fraser University.
References
- Aagard J, Müller-Nielsen K (2011). Clinical outcome of assertive community treatment (ACT) in a rural area in Denmark: a case–control study with a 2-year follow-up. Nordic Journal of Psychiatry 65, 299–305. doi: 10.3109/08039488.2010.544405. [DOI] [PubMed] [Google Scholar]
- Andrews DA, Dowden C (2007). The risk-need-responsivity model of assessment and human service in prevention and corrections: crime-prevention jurisprudence. Canadian Journal of Criminology and Criminal Justice 49, 439–464. [Google Scholar]
- Baillargeon J, Binswanger IA, Penn JV, Williams BA, Murray OJ (2009a). Psychiatric disorders and repeat incarcerations: the revolving prison door. American Journal of Psychiatry 166, 103–9. [DOI] [PubMed] [Google Scholar]
- Baillargeon J, Penn JV, Thomas CR, Temple JR, Baillargeon G, Murray OJ (2009b). Psychiatric disorders and suicide in the nation's largest state prison system. Journal of the American Academy of Psychiatry Law 37, 188–93. [PubMed] [Google Scholar]
- BC Stats (2013). Retrieved 28 December 2014 from http://www.bcstats.gov.bc.ca/StatisticsBySubject/Demography/PopulationProjections.aspx
- Culhane D, Avery JM, Hadley T (1996). The treated prevalence of mental health and substance use disorders among adults admitted to the Philadelphia shelter system: Results from the integration of longitudinal data on shelter and mental health services utilization. The Selected Works of Dennis P. Culhane. Retrieved 12 December 2014 from http://works.bepress.com/dennis_culhane/55
- Cusack KJ, Morrisey JP, Cuddeback GS, Prins A, Williams DM (2010). Criminal justice involvement, behavioral health service use, and costs of forensic assertive community treatment: a randomized trial. Community Mental Health Journal 46, 356–363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fazel S, Geddes JR, Kushel M (2014). The health of homeless people in high-income countries: descriptive epidemiology, health consequences, and clinical policy recommendations. The Lancet 384, 1529–1540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilmer TP, Stefancic A, Ettner SL, Manning WG, Tsemberis S (2010). Effect of full-service partnerships on homelessness, use and costs of mental health services, and quality of life among adults with serious mental illness. Archives of General Psychiatry 67, 645–652. [DOI] [PubMed] [Google Scholar]
- Harrison P, Allen MJ, Beck J (2005). Prison and Jail Inmates at Midyear 2004 (Bureau of Justice Statistics). U.S. Department of Justice: Washington, DC. [Google Scholar]
- Hiday VA, Ray B (2010). Arrests two years after a well-established mental health court. Psychiatric Services 61, 263–268. [DOI] [PubMed] [Google Scholar]
- James DJ, Glaze LE (2006). Mental health problems of prison and jail inmates Bureau of Justice Statistics Special Report, U.S. Department of Justice, Office of Justice Programs, NCJ 213600, September 2006 (revised 12/14/06), pp. 1–11. Retrieved 20 December 2012 from http://bjs.ojp.usdoj.gov/content/pub/pdf/mhppji.pdf
- Kariminia A, Law MG, Butler TG, Corben SP, Levy MH, Kaldor JM, Grant L. (2007). Factors associated with mortality in a cohort of Australian prisoners. European Journal of Epidemiology 22, 417–28. [DOI] [PubMed] [Google Scholar]
- Kong R, Au Coin K (2008). Female offenders in Canada. Juristat 28, 1–28. [Google Scholar]
- Lamont A, Ukoumunne OC, Tyrer P, Thornicroft G, Patel R, Slaughter J (2000). The geographical mobility of severely mentally ill residents in London. Social Psychiatry and Psychiatric Epidemiology 35, 164–169. [DOI] [PubMed] [Google Scholar]
- Landry L, Sinha M (2008). Adult Correctional Services in Canada, 2005/2006 (Juristat Catalogue No. 85-002-XIE, Vol. 28, No. 6). Statistics Canada: Ottawa, ON. [Google Scholar]
- Lix LM, Hinds A, DeVerteuil G, Robinson JR, Walker J, Roos LL (2006). Residential mobility and severe mental illness: a population-based analysis. Administration and Policy in Mental Health 33, 160–171. [DOI] [PubMed] [Google Scholar]
- Luciano A, Belstock J, Malmberg P, McHugo GJ, Drake RE, Xie H, Essock SM, Covell NH (2014). Predictors of incarceration among urban adults with co-occurring severe mental illness and a substance use disorder. Psychiatric Services 65, 1325–1331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNiel DE, Binder RL (2007). Effectiveness of a mental health court in reducing criminal recidivism and violence. American Journal of Psychiatry 164, 395–1403. doi: 10.1176/appi.ajp.2007.06101664. [DOI] [PubMed] [Google Scholar]
- Nielsen SF, Hjorthoj CR, Erlangsen A, Nordentoft M (2011). Psychiatric disorders and mortality among people in homeless shelters in Denmark: a nationwide register-based cohort study. The Lancet 337, 2205–2214. [DOI] [PubMed] [Google Scholar]
- Nusselder WJ, Slockers MT, Krol L, Slockers CT, Looman CW, van Beeck EF (2013). Mortality and life expectancy in homeless men and women in Rotterdam: 2001–2010. PLoS ONE 8, e73979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patterson M, Markey M, Somers JM (2012). Multiple paths to just ends: using narrative interviews and timelines to explore health equity and homelessness. International Journal of Qualitative Methods 11, 132–151. [Google Scholar]
- Rezansoff SN, Moniruzzaman A, Gress C, Somers JM (2013). Psychiatric diagnoses and multiyear criminal recidivism in a Canadian provincial offender population. Psychology, Public Policy, and Law 19, 443–453. [Google Scholar]
- Ruiz MA, Douglas KS, Edens JF, Nikolova NL, Lilienfeld SO (2012). Co-occurring mental health and substance use problems in offenders: implications for risk assessment. Psychological Assessment 24, 77–87. doi: 10.1037/a0024623. [DOI] [PubMed] [Google Scholar]
- SAMHSA (2007). Results from the 2006 National Survey on Drug Use and Health: National Findings Office of Applied Studies, NSDUH Series H-32, DHHS Publication No. SMA 07-4293, Rockville, MD. Retrieved 20 December 2012 from http://www.oas.samhsa.gov/nsduh/2k6nsduh/2k6Results.pdf
- Somers JM, Currie L, Moniruzzaman A, Eiboff F, Patterson M (2012). Drug treatment court of Vancouver: An empirical evaluation of recidivism. International Journal of Drug Policy 23, 393–400. [DOI] [PubMed] [Google Scholar]
- Somers JM, Patterson ML, Moniruzzaman A, Currie L, Rezansoff SN, Palepu A, Fryer K (2013a). Vancouver at home: pragmatic randomized trials investigating housing first for homeless and mentally ill adults. Trials 14, 365–385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Somers JM, Rezansoff SN, Moniruzzaman A (2013b). Comparative analysis of recidivism outcomes following drug treatment court in Vancouver, Canada. International Journal of Offender Therapy and Comparative Criminology doi: 10.1177/0306624X13479770. [DOI] [PubMed]
- Steadman HJ, Osher FC, Robbins PC, Case B, Samuels S (2009). Prevalence of serious mental illness among jail inmates. Psychiatric Services 60, 761–765. [DOI] [PubMed] [Google Scholar]
- Stefancic A, Henwood BF, Melton H, Shin SM, Lawrence-Gomez R, Tsemberis S (2013) Implementing housing first in rural areas: pathways Vermont. American Journal of Public Health 103(S2), S206–S209. doi: 10.2105/AJPH.2013.301606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szkopek-Szkopowski T, Palmer A, LePard D, Robinson D, Pauw R, Tran H (2013). Vancouver's mental health crisis: an update report. Vancouver Police Department. Retrieved 12 December 2014 from http://vancouver.ca/police/assets/pdf/reports-policies/mental-health-crisis.pdf
- Thompson S (2010). Policing Vancouver's mentally ill: The disturbing truth. Vancouver Police Department. Retrieved 12 December 2014 from https://vancouver.ca/police/assets/pdf/reports-policies/vpd-lost-in-transition-part-2-draft.pdf
- Tsemberis S, Kent D, Respress C (2012). Housing stability and recovery among chronically homeless persons with co-occurring disorders in Washington, DC. American Journal of Public Health 102, 13–16. doi: 10.2105/AJPH.2011.300320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Visher CA, Winterfield L, Coggeshall MB (2005). Ex-offender employment programs and recidivism: a meta-analysis. Journal of Experimental Criminology 1, 295–316. [Google Scholar]