Abstract
Patient: Male, 9-year-old
Final Diagnosis: Fulminant and diffuse cerebral toxoplasmosis
Symptoms: Decreased level of consciousness • fever • generalized tonic-clonic seizures • hemiplegia
Medication: —
Clinical Procedure: Decompressive hemicraniectomy
Specialty: Neurosurgery
Objective:
Unusual clinical course
Background:
One of the most common causes of central nervous system (CNS) opportunistic infections in immunocompromised patients is toxoplasmosis. It can cause focal or disseminated brain lesions leading to neurological deficit, coma, and death. Prompt management with optimal antibiotics is vital. However, the diagnosis of cerebral toxoplasmosis is challenging in infected individuals with human immunodeficiency virus (HIV). The possible diagnosis is based on clinical presentation, imaging, and specific serologic investigations. The diagnosis can be confirmed by histopathological examination and/or by finding nucleic material in the spinal cerebrospinal fluid (CSF) examination.
Case Report:
We present a review of the literature with a rare illustrative case of diffuse CNS toxoplasmosis as the first manifestation of HIV infection in a young patient. Brain MRI showed diffuse, ring-enhancing lesions, and significant midline shift. Decompressive hemicraniectomy for control of intracranial pressure and anti-infectious therapy were performed.
Conclusions:
This should raise awareness that cerebral toxoplasmosis can occur in pediatric patients with HIV infection, and, more importantly, as the first manifestation of AIDS. Although the prognosis is often poor, early diagnosis and immediate treatment of this life-threatening opportunistic infection can improve outcomes.
MeSH Keywords: HIV infections; Neurosurgery; Toxoplasmosis, Cerebral
Background
Toxoplasmosis is known as one of the most prevalent infections worldwide, and it is estimated that more than one-third of the human population is infected. The causative microorganism is Toxoplasma gondii, an obligate intracellular parasite that causes zoonotic infection [1].
Transfer occurs via several routes, including ingestion of contaminated water or food (the main route), contact with cat litter containing parasitic cysts, blood transfusion, organ/tissue transplantation, and via the placenta following maternal infection [2].
Although most infections are subclinical in immunocompetent individuals, the parasite remains dormant in tissues of an infected host, including the central nervous system (CNS) [3]. Significant clinical disease often occurs secondary to reactivation of the inactivated parasite, which occurs when the immune system is suppressed or compromised. This condition is most often seen in pregnancy, acquired immunodeficiency, or transplantation [4–9]. However, primary disease does occur and is associated with more severe and disseminated disease [10,11].
Toxoplasmosis is the leading cause of opportunistic infection and cerebral lesions in individuals with acquired immune deficiency syndrome (AIDS), accounting for 50% to 70% of all lesions in the brain [12]. Toxoplasma encephalitis usually appears in late stages of AIDS, when CD4 counts are below 200 cells/mm3, and patients with CD4 counts below 50 cells/mm3 are at higher risk [11].
Clinical manifestations of CNS involvement in HIV/AIDS patients are diverse and range from fever, headache, altered sensorium or motor function, and focal neurological deficit to disorientation, confusion, decreased level of consciousness, and seizure, related to a focal lesion or disseminated encephalitis [13,14]. In some patients with CD4 counts over 200 cells/mm3, CNS lesions mimic brain tumors [15,16].
Infrequently, cerebral toxoplasmosis present as the first manifestation of HIV/AIDS, which is life-threatening if left untreated [17–19]. Here, we describe a very rare case of a child who presented with diffuse cerebral toxoplasmosis as the first manifestation of pediatric HIV/AIDS.
Case Report
A 9-year-old boy was admitted to the Pediatric Emergency Department (ED) with a decreased level of consciousness, recent frequent episodes of generalized tonic-clonic seizures, and fever. The onset of fever was 3 weeks earlier, with oral ulcer, dyspnea, and coryza. He was treated on an outpatient basis, but the fever did not resolve. He also had a history of recent urinary incontinence and weight loss, but no history of night sweats or gastrointestinal symptoms (except oral ulcer).
Initial examination at the Pediatric ED revealed left hemiplegia, in addition to fever, seizure, and loss of consciousness (LOC), suggestive of meningitis. A hematologic workup showed significant leukopenia (WBC=2400/mm3) and anemia (hemoglobin=9.5 gr/dl). Results of chest radiography and abdominal ultrasonography were normal.
The patient received intravenous steroids and empirical vancomycin plus ceftazidime plus metronidazole as broad-spectrum antibiotics, with clinical suspicion of meningitis. Brain magnetic resonance imaging (MRI) with and without intravenous contrast showed diffuse, ring-enhancing lesions with perifocal edema and significant midline shift (Figures 1, 2), suggestive of tuberculoma or cerebral toxoplasmosis. Therefore, serologic tests for toxoplasmosis and HIV antibodies were requested.
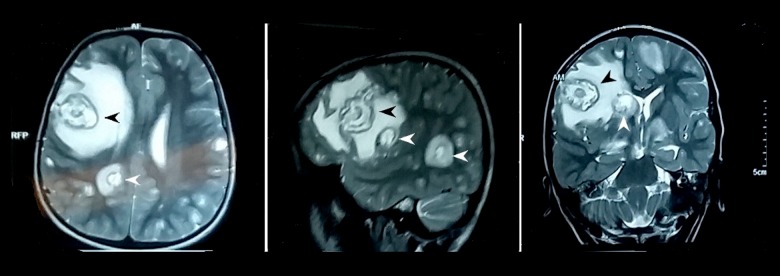
Figure 1.
T2-weighted axial, sagittal, and coronal images are showing diffuse intra-axial brain lesions with the characteristic concentric target sign (arrows).
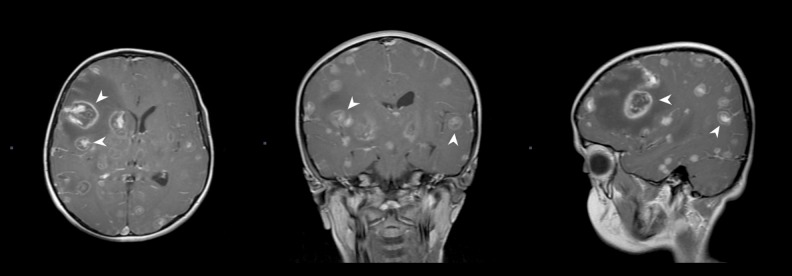
Figure 2.
Post-gadolinium T1-weighted axial, sagittal, and coronal scans are showing diffuse intra-axial brain lesions with the characteristic eccentric target sign (arrows).
A rapid decline in the patient’s mental status and corresponding midline shift warranted an urgent decompressive hemicraniectomy and resection of the largest lesion to prevent herniation syndrome and to control the intracranial pressure, and thus provided the specimen for diagnosis of cerebral toxoplasmosis (Figure 3). A pathological examination confirmed the diagnosis of cerebral toxoplasmosis.
Figure 3.
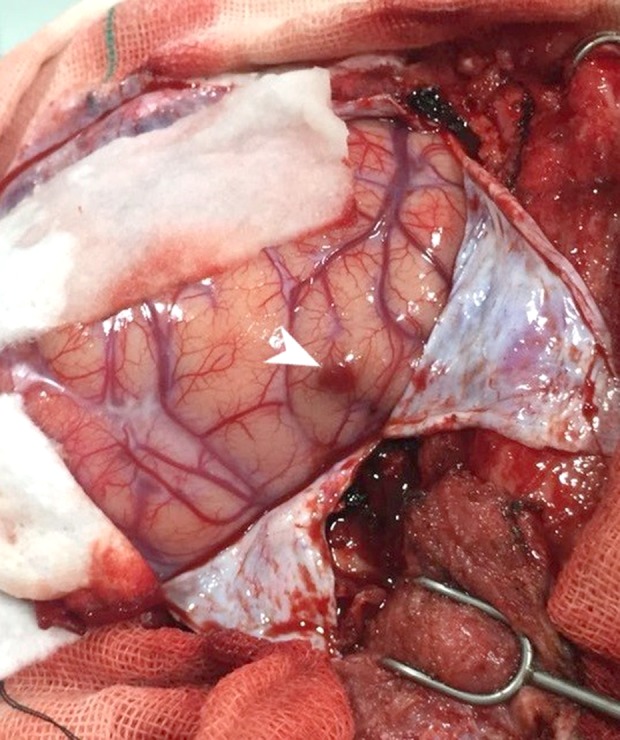
Intra-operative image of decompressive hemicraniectomy. Note the red, enlarged cortical nodule in the frontal lobe (arrow).
Blood analysis for the HIV antibody was positive postoperatively and was confirmed with ELISA. CD4 counts were below 100 cells/mm3. Three days later, the toxoplasma IgG titer was reported to be positive with significant levels. Accordingly, we confirmed the diagnosis of CNS toxoplasmosis based on serology and pathologic evidence, and trimethoprim-sulfamethoxazole was added to his antibiotic regimen. Also, the tuberculin sensitivity test was negative. The patient’s vaccination history was unclear. Unfortunately, the patient died on the 6th hospital day, probably because of disease dissemination. A postmortem pathological examination was not done.
Discussion
Central nervous system involvement in patients with HIV/AIDS often occurs secondary to opportunistic infections, most commonly due to toxoplasma, mycobacteria tuberculosis, and fungi, and less commonly due to primary lymphoma [12].
Toxoplasma gondii, considered as one of the most prevalent parasites, causes clinical infection in an immunocompromised individual, usually by reactivation of the dormant form of the microorganism. The most common sites for latent infection are the CNS, eye, and muscles (skeletal, smooth, and heart muscles) [20].
Cerebral toxoplasmosis is among the most common CNS infections in untreated immunocompromised patients [21]. Toxoplasma encephalitis almost always occurs secondary to reactivation of the inactivated parasite in the brain of HIV-infected patients, especially when the CD4 count is below 200 cell/mm3 [11,14].
CNS toxoplasmosis causes a wide range of symptoms corresponding to the location and distribution of involvement. Patients usually present with headache, confusion, or changes in the level of consciousness, fever, focal neurological signs, and seizure [22,23]. Presentation with meningeal signs and diffuse encephalitis is less common [24]. These lesions usually are seen as unifocal or multifocal abscess-like lesions or, rarely, as diffuse lesions. However, the first manifestation of AIDS in a child with fulminant encephalitic illness and diffuse involvement of the brain is quite rare. This situation warrants prompt diagnosis and treatment because of its high morbidity and mortality [25].
AIDS-related neurological signs/symptoms of brain involvement are not specific; thus, brain imaging with computed tomography (CT) or magnetic resonance (MR) is essential for the diagnosis of toxoplasma lesions. However, MRI should be used as the initial choice if there is a high clinical suspicion, due to its greater sensitivity than CT [26].
In CT, lesions usually show as ring enhancement with intravenous contrast, and cerebral edema may be found, which could be responsible for the mass effect in these patients. The most common locations of the lesion are in frontal, basal ganglia, and parietal regions [27]. The lesion(s) of cerebral toxoplasmosis is usually round, and is iso/hyperdense in gray-white matter junction, basal ganglia, and deep white matter. The lesion is usually ring-enhancing with intravenous contrast, but can also have a homogenous enhancing pattern [26].
The characteristic “target sign” in CT findings in patients with cerebral toxoplasmosis is defined as low-density mass lesions that enhance with intravenous contrast and are surrounded by edema [26,28]. This pattern also is seen in cerebral tuberculoma [29]. Additionally, diffuse toxoplasma encephalitis can occur without abscess formation and CT findings [26].
MRI shows “target sign” enhancement, which is commonly seen in cerebral toxoplasmosis and described as an isointense “eccentric” (or concentric) core surrounded by a hypointense zone and a peripheral hyperintense enhancing rim on post-contrast T1-weighted images and inverse appearance in T2-weighted/FLAIR images, with a hypointense core, an intermediate hyperintense region, and a peripheral hypointense rim [30,31]. Different features for cerebral toxoplasmosis on MRI have been described, which are probably due to the different stages of infection, including the degree of necrosis and cyst stages [29,32]. Furthermore, the peripheral rim of hyper-intensity and central hypointensity in T2-weighted images are seen in CNS tuberculoma [33].
After treatment with pyrimethamine and sulfadiazine, the resolution of lesions is indicated in CT scans, related to the degree of involvement and latency [26].
The MRI study in our illustrative case shows both of these diagnostic radiological signs. Some authors have described a T2-weighted symmetric, concentric target sign with a hypointense core, an intermediate hyperintense core, and a peripheral hypointense zone as a more specific diagnostic pattern (Figure 1) [34–37]. A ring-shaped zone of peripheral enhancement with a small eccentric nodule alone, the wall of the lesion on the post-gadolinium T1-weighted sequence is considered to be an eccentric target sign (Figure 2).
Primary CNS lymphoma is another differential diagnosis of cerebral toxoplasmosis in neuroimaging with CT scan. Primary CNS lymphoma can mimic toxoplasma in CT scans with ring-enhancing lesions [28]. Primary CNS lymphoma and toxoplasmosis are indistinguishable in CT [26]. AIDS-associated lymphoma in T2-weighted MR images, often shown by areas of central hyperintense and surrounding hypointense area, present as a ring or “target sign” [28]. These similarities make biopsy necessary to differentiate lymphoma from toxoplasma lesions in people with AIDS [28].
The other mimicking brain lesions are pyogenic abscess (a thin hypointense rim on T2-weighted MRI) and metastasis (ring-enhancing lesions at the gray-white matter junction with vasogenic edema for the relative size of the lesion) [34].
MRI is more sensitive than CT and reveals multiple lesions [28]. Various neuroimaging patterns have been proposed for the diagnosis of toxoplasma lesions to differentiate from primary CNS lymphoma based on MR or other brain imaging modalities. Decreased or poor uptake in toxoplasmosis using single-photon emission computed tomography (SPECT) and positron emission tomography (PET) has been reported [17,38,39], but cost and availability of these modalities limit their use in the clinical setting, especially in countries with a high prevalence of HIV/AIDS and toxoplasma infections.
Other diagnostic tool includes polymerase chain reaction (PCR) detection of Toxoplasma gondii in cerebrospinal fluid (CSF) [40], but clinical use of this tool can be time-consuming and is less sensitive in toxoplasma encephalitis.
Definite diagnosis of toxoplasma encephalitis is only possible with histopathology. Some authors suggest a trial of treatment for toxoplasma, which could be helpful in presumptive diagnosis, particularly in patients with low CD4, multiple cerebral lesions suspicious of toxoplasmosis, reactive anti-toxoplasma IgG, and lack of proper prophylaxis [41].
A presumptive diagnosis of cerebral toxoplasmosis can be made based on a combination of the clinical syndrome, a positive toxoplasma IgG antibody, and brain imaging, especially if the CD4 count is below 200 cells/mm3. If a patient meets all the diagnostic criteria, the positive predictive value of toxoplasmosis is nearly 90% [37,42,43]. Biopsy confirms the clinical diagnosis of cerebral toxoplasmosis through detection of the organism, and differentiates it from primary CNS lymphoma and tuberculoma, but may delay start of treatment.
The cornerstone of treatment is a combination of pyrimethamine or trimethoprim-sulfamethoxazole, sulfadiazine or clindamycin, in addition to treatment for HIV infection by combination antiretroviral therapy (cART) [44–48]. Timely initiation of proper antibiotics to treat toxoplasma encephalitis is critical and should be started promptly when there is a high clinical suspicion of toxoplasmosis [11,41]. However, patients may need other interventions, including decompressive surgery, to reduce the mass effect of the lesion.
Empirical treatment with pyrimethamine and sulfadiazine for a patient with neurological symptoms and intracranial mass should be kept in mind, especially in patients with a history of immunodeficiency [49]. However, it is more challenging when the initial manifestation of immunodeficiency status is encephalitis due to toxoplasmosis or tuberculosis, in which clinical presentation of encephalitis and mass effect due to edema indicates the use of corticosteroids.
In this illustrative case, given the patient’s clinical presentation and brain MRI, the diagnosis was confirmed by pathology and high titers of anti-toxoplasma antibody, and treatment with TMP-SMX started shortly after serologic test results were received.
Conclusions
CNS toxoplasmosis should be considered in patients living in regions endemic for HIV and toxoplasma. Toxoplasmosis in immunocompromised patients should be considered when a combination of clinical presentation and neuroimaging evidence is suggestive, and promptly investigated as a life-threatening differential diagnosis, particularly in the pediatric population. Finally, toxoplasma encephalitis could be the first presentation of HIV infection in a child.
Footnotes
Conflict of Interests
None.
References:
- 1.Schlüter D, Barragan A. Advances and challenges in understanding cerebral toxoplasmosis. Front Immunol. 2019;10:242. doi: 10.3389/fimmu.2019.00242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Murray PR, Rosenthal KS, Pfaller MA. Medical microbiology : Elsevier Health Sciences. 2015 [Google Scholar]
- 3.Benson CA, Kaplan JE, Masur H, et al. Treating opportunistic infections among HIV-infected adults and adolescents : Recommendations from CDC, the National Institutes of Health, and the HIV Medicine Association/Infectious Diseases Society of America. Clin Infect Dis. 2005;40(Suppl. 3):S131–235. [Google Scholar]
- 4.Pistacchi M, Gioulis M, Zirillo M, et al. Cerebral toxoplasmosis in undifferentiated connective disease treated with mycophenolate mofetil : An unusual case report. Acta Neurol Belg. 2016;116(4):633–36. doi: 10.1007/s13760-015-0595-9. [DOI] [PubMed] [Google Scholar]
- 5.Bernardo DR, Chahin N. Toxoplasmic encephalitis during mycophenolate mofetil immunotherapy of neuromuscular disease. Neurol Neuroimmunol Neuroinflamm. 2015;2(1):e63. doi: 10.1212/NXI.0000000000000063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cren J, Bouvard B, Crochette N. Cerebral toxoplasmosis and anti-TNFα : A case report. IDCases. 2016;5:40–42. doi: 10.1016/j.idcr.2016.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Enriquez-Marulanda A, Valderrama-Chaparro J, Parrado L, et al. Cerebral toxoplasmosis in an MS patient receiving Fingolimod. Mult Scler Relat Disord. 2017;18:106–8. doi: 10.1016/j.msard.2017.05.004. [DOI] [PubMed] [Google Scholar]
- 8.Xu J, Nault RJ, Maldonado-Naranjo A, et al. Disseminated cerebral toxoplasmosis in a patient with chronic lymphocytic leukemia. J Clin Neurosci. 2018;50:127–28. doi: 10.1016/j.jocn.2018.01.057. [DOI] [PubMed] [Google Scholar]
- 9.Murro D, Novo J, Arvanitis L. Asymptomatic diffuse “encephalitic” cerebral toxoplasmosis in a woman with systemic lupus erythematosus. J Clin Neurosci. 2016;29:194–96. doi: 10.1016/j.jocn.2015.12.022. [DOI] [PubMed] [Google Scholar]
- 10.Kumral E, Kşkderelioğlu A, Atalay S, Gkengin D. Diffuse cerebral toxoplasmosis in an immunocompetent patient. Turkish Journal of Neurology/Turk Noroloji Dergisi. 2012;18(1):43–45. [Google Scholar]
- 11. AIDS info: Guidelines for the Prevention and Treatment of Opportunistic Infections in HIV-Infected Adults and Adolescents, 2018.
- 12.Smirniotopoulos JG, Koeller KK, Nelson AM, Murphy FM. Neuroimaging – autopsy correlations in AIDS. Neuroimaging Clin N Am. 1997;7(3):615–37. [PubMed] [Google Scholar]
- 13.Ibebuike K, Mantanga L, Emereole O, et al. Cerebellar toxoplasmosis in HIV/AIDS infant : Case report and review of the literature. Neurol Sci. 2012;33(6):1423–28. doi: 10.1007/s10072-012-0960-x. [DOI] [PubMed] [Google Scholar]
- 14.Basavaraju A. Toxoplasmosis in HIV infection : An overview. Trop Parasitol. 2016;6(2):129–35. doi: 10.4103/2229-5070.190817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.León Ruiz M. A novel case of solitary cerebral toxoplasmosis mimicking glioblastoma as the first presentation of HIV. J Clin Neurol. 2016;12(2):248–50. doi: 10.3988/jcn.2016.12.2.248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mentzer A, Perry M, Fitzgerald N, et al. Is it all cerebral toxoplasmosis? Lancet. 2012;379(9812):286. doi: 10.1016/S0140-6736(11)61579-1. [DOI] [PubMed] [Google Scholar]
- 17.Skiest D, Erdman W, Chang W, et al. SPECT thallium-201 combined with Toxoplasma serology for the presumptive diagnosis of focal central nervous system mass lesions in patients with AIDS. J Infect. 2000;40(3):274–81. doi: 10.1053/jinf.2000.0664. [DOI] [PubMed] [Google Scholar]
- 18.Barman B, Tiewsoh I, Lynrah KG, et al. Cerebral toxoplasmosis with fever and erythematous macular rash : An initial presentation in an advanced HIV infection. Trop Parasitol. 2018;8(1):41. doi: 10.4103/tp.TP_91_15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Al Zoubi M, Zulfiqar B, Kulkarni M. Cerebral toxoplasmosis requiring urgent brain biopsy. IDCases. 2017;9:59–61. doi: 10.1016/j.idcr.2017.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Montoya JG, Boothroyd JC, Kovacs JA. 280 – Toxoplasma gondii. In: Bennett JE, Dolin R, Blaser MJ, editors. Mandell, Douglas, and Bennett’s Principles and Practice of Infectious Diseases. Eighth Edition. Philadelphia: Content Repository Only!; 2015. pp. 3122–53.e7. [Google Scholar]
- 21.San-Andrés F-J, Rubio R, Castilla J, et al. Incidence of acquired immunodeficiency syndrome-associated opportunistic diseases and the effect of treatment on a cohort of 1115 patients infected with human immunodeficiency virus, 1989–1997. Clin Infect Dis. 2003;36(9):1177–85. doi: 10.1086/374358. [DOI] [PubMed] [Google Scholar]
- 22.Espinoza-Oliva M, Avila E, Artega M, et al. Case report : Cerebral toxoplasmosis infection by reactivation of T. gondii in pediatric patients with HIV. J Neuroinfect Dis. 2015;5(175):2. [Google Scholar]
- 23.Ramachandran R, Radhan P, Anand R, et al. CNS toxoplasmosis in an immunocompetent individual. Radiol Case Rep. 2014;9(1):e00031. doi: 10.2484/rcr.v9i1.908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gray F, Gherardi R, Wingate E, et al. Diffuse “encephalitic” cerebral toxoplasmosis in AIDS. J Neurol. 1989;236(5):273–77. doi: 10.1007/BF00314455. [DOI] [PubMed] [Google Scholar]
- 25.Basavaraju A. Toxoplasmosis in HIV infection : An overview. Trop Parasitol. 2016;6(2):129–35. doi: 10.4103/2229-5070.190817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Levy RM, Rosenbloom S, Perrett LV. Neuroradiologic findings in AIDS : A review of 200 cases. Am J Roentgenol. 1986;147(5):977–83. doi: 10.2214/ajr.147.5.977. [DOI] [PubMed] [Google Scholar]
- 27.Porter SB, Sande MA. Toxoplasmosis of the central nervous system in the acquired immunodeficiency syndrome. N Engl J Med. 1992;327(23):1643–48. doi: 10.1056/NEJM199212033272306. [DOI] [PubMed] [Google Scholar]
- 28.Ciricillo SF, Rosenblum ML. Use of CT and MR imaging to distinguish intracranial lesions and to define the need for biopsy in AIDS patients. J Neurosurg. 1990;73(5):720–24. doi: 10.3171/jns.1990.73.5.0720. [DOI] [PubMed] [Google Scholar]
- 29.Masamed R, Meleis A, Lee EW, Hathout GM. Cerebral toxoplasmosis : Case review and description of a new imaging sign. Clin Radiol. 2009;64(5):560–63. doi: 10.1016/j.crad.2008.09.016. [DOI] [PubMed] [Google Scholar]
- 30.Osborn A. Diagnostic neuroradiology. 1994. Infections of the brain and its linings. [Google Scholar]
- 31.Masamed R, Meleis A, Lee E, Hathout G. Cerebral toxoplasmosis : Case review and description of a new imaging sign. Clin Radiol. 2009;64(5):560–63. doi: 10.1016/j.crad.2008.09.016. [DOI] [PubMed] [Google Scholar]
- 32.Chang L, Cornford ME, Chiang FL, et al. Radiologic-pathologic correlation. Cerebral toxoplasmosis and lymphoma in AIDS. Am J Neuroradiol. 1995;16(8):1653–63. [PMC free article] [PubMed] [Google Scholar]
- 33.Wasay M, Kheleani BA, Moolani MK, et al. Brain CT and MRI findings in 100 consecutive patients with intracranial tuberculoma. J Neuroimaging. 2003;13(3):240–47. [PubMed] [Google Scholar]
- 34.Mahadevan A, Ramalingaiah AH, Parthasarathy S, et al. Neuropathological correlate of the “concentric target sign” in MRI of HIV-associated cerebral toxoplasmosis. J Magn Reson Imaging. 2013;38(2):488–95. doi: 10.1002/jmri.24036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Roche AD, Rowley D, Brett FM, Looby S. Concentric and eccentric target MRI signs in a case of HIV-associated cerebral toxoplasmosis. Case Rep Neurol Med. 2018;2018:9876514. doi: 10.1155/2018/9876514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kumar GS, Mahadevan A, Guruprasad A, et al. Eccentric target sign in cerebral toxoplasmosis : Neuropathological correlate to the imaging feature. J Magn Reson Imaging. 2010;31(6):1469–72. doi: 10.1002/jmri.22192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Luft BJ, Remington JS. Toxoplasmic encephalitis in AIDS. Clin Infect Dis. 1992;15(2):211–22. doi: 10.1093/clinids/15.2.211. [DOI] [PubMed] [Google Scholar]
- 38.Love C, Tomas MB, Tronco GG, Palestro CJ. FDG PET of infection and inflammation. Radiographics. 2005;25(5):1357–68. doi: 10.1148/rg.255045122. [DOI] [PubMed] [Google Scholar]
- 39.Yang M, Sun J, Bai HX, et al. Diagnostic accuracy of SPECT, PET, and MRS for primary central nervous system lymphoma in HIV patients : A systematic review and meta-analysis. Medicine (Baltimore) 2017;96(19):e6676. doi: 10.1097/MD.0000000000006676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Anselmo LMP, Vilar FC, Lima JE, et al. Usefulness and limitations of polymerase chain reaction in the etiologic diagnosis of neurotoxoplasmosis in immunocompromised patients. J Neurol Sci. 2014;346(1):231–34. doi: 10.1016/j.jns.2014.08.034. [DOI] [PubMed] [Google Scholar]
- 41.Marra CM. Handbook of clinical neurology. Vol. 152. Elsevier; 2018. Central nervous system infection with Toxoplasma gondii; pp. 117–22. [DOI] [PubMed] [Google Scholar]
- 42.Luft BJ, Hafner R, Korzun AH, et al. Toxoplasmic encephalitis in patients with the acquired immunodeficiency syndrome. N Engl J Med. 1993;329(14):995–1000. doi: 10.1056/NEJM199309303291403. [DOI] [PubMed] [Google Scholar]
- 43.Cohn JA, McMeeking A, Cohen W, et al. Evaluation of the policy of empiric treatment of suspected Toxoplasma encephalitis in patients with the acquired immunodeficiency syndrome. Am J Med. 1989;86(5):521–27. doi: 10.1016/0002-9343(89)90378-1. [DOI] [PubMed] [Google Scholar]
- 44.Leport C, Meulemans A, Robine D, et al. Levels of pyrimethamine in serum and penetration into brain tissue in humans. AIDS. 1992;6(9):1040–41. doi: 10.1097/00002030-199209000-00021. [DOI] [PubMed] [Google Scholar]
- 45.Dannemann B, McCutchan JA, Israelski D, et al. Treatment of toxoplasmic encephalitis in patients with AIDS : A randomized trial comparing pyrimethamine plus clindamycin to pyrimethamine plus sulfadiazine. Ann Intern Med. 1992;116(1):33–43. doi: 10.7326/0003-4819-116-1-33. [DOI] [PubMed] [Google Scholar]
- 46.Katlama C, De Wit S, O’doherty E, et al. Pyrimethamine-clindamycin vs. pyrimethamine-sulfadiazine as acute and long-term therapy for toxoplasmic encephalitis in patients with AIDS. Clin Infect Dis. 1996;22(2):268–75. doi: 10.1093/clinids/22.2.268. [DOI] [PubMed] [Google Scholar]
- 47.Hodgson HA, Sim T, Gonzalez H, et al., editors. Open forum infectious diseases. Oxford University Press US; 2018. Successful treatment of cerebral toxoplasmosis using pyrimethamine oral solution compounded from inexpensive bulk powder. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hernandez AV, Thota P, Pellegrino D, et al. A systematic review and meta-analysis of the relative efficacy and safety of treatment regimens for HIV-associated cerebral toxoplasmosis : Is trimethoprim-sulfamethoxazole a real option? HIV Med. 2017;18(2):115–24. doi: 10.1111/hiv.12402. [DOI] [PubMed] [Google Scholar]
- 49.Levy RM, Bredesen DE, Rosenblum ML. Neurological manifestations of the acquired immunodeficiency syndrome (AIDS) : Experience at UCSF and review of the literature. J Neurosurg. 1985;62(4):475–95. doi: 10.3171/jns.1985.62.4.0475. [DOI] [PubMed] [Google Scholar]