Abstract
Aims.
School-based psychological interventions encompass: universal interventions targeting youth in the general population; and indicated interventions targeting youth with subthreshold depression. This study aimed to: (1) examine the population cost-effectiveness of delivering universal and indicated prevention interventions to youth in the population aged 11–17 years via primary and secondary schools in Australia; and (2) compare the comparative cost-effectiveness of delivering these interventions using face-to-face and internet-based delivery mechanisms.
Methods.
We reviewed literature on the prevention of depression to identify all interventions targeting youth that would be suitable for implementation in Australia and had evidence of efficacy to support analysis. From this, we found evidence of effectiveness for the following intervention types: universal prevention involving group-based psychological interventions delivered to all participating school students; and indicated prevention involving group-based psychological interventions delivered to students with subthreshold depression. We constructed a Markov model to assess the cost-effectiveness of delivering universal and indicated interventions in the population relative to a ‘no intervention’ comparator over a 10-year time horizon. A disease model was used to simulate epidemiological transitions between three health states (i.e., healthy, diseased and dead). Intervention effect sizes were based on meta-analyses of randomised control trial data identified in the aforementioned review; while health benefits were measured as Disability-adjusted Life Years (DALYs) averted attributable to reductions in depression incidence. Net costs of delivering interventions were calculated using relevant Australian data. Uncertainty and sensitivity analyses were conducted to test model assumptions. Incremental cost-effectiveness ratios (ICERs) were measured in 2013 Australian dollars per DALY averted; with costs and benefits discounted at 3%.
Results.
Universal and indicated psychological interventions delivered through face-to-face modalities had ICERs below a threshold of $50 000 per DALY averted. That is, $7350 per DALY averted (95% uncertainty interval (UI): dominates – 23 070) for universal prevention, and $19 550 per DALY averted (95% UI: 3081–56 713) for indicated prevention. Baseline ICERs were generally robust to changes in model assumptions. We conducted a sensitivity analysis which found that internet-delivered prevention interventions were highly cost-effective when assuming intervention effect sizes of 100 and 50% relative to effect sizes observed for face-to-face delivered interventions. These results should, however, be interpreted with caution due to the paucity of data.
Conclusions.
School-based psychological interventions appear to be cost-effective. However, realising efficiency gains in the population is ultimately dependent on ensuring successful system-level implementation.
Key words: Adolescent, child, cost-effectiveness analysis, depressive disorder, economic evaluation, major depression, primary prevention
Introduction
Major depression (a.k.a., major depressive disorder) is the second leading cause of years lived with disability (YLDs) and mental health burden both in Australia and across the globe (Murray et al. 2012; Ferrari et al. 2013). Implementing strategies to reduce the burden of major depression has, in turn, become a top mental health priority (Pirkis et al. 2005; WHO, 2012). Conventional treatments for major depression (e.g., antidepressant drugs and psychological therapy) are efficacious and cost-effective (Whiteford et al. 2013), but are constrained in their capacity to reduce the population burden of major depression (Andrews et al. 2004; Jorm, 2014). For example, Andrews et al. (2004) found that around 66% of the overall burden of major depression would remain unaverted by evidence-based treatments despite an optimal effective coverage of 100%. This highlights the importance of disease prevention as an alternate strategy for reducing the burden of major depression.
Most depressive disorders have their initial onset during the formative years of childhood and adolescence (Thapar et al. 2012; Patton et al. 2014). In turn, schools are increasingly being recognised as an important platform for the widespread delivery of preventive mental health interventions (Fazel et al. 2014a, b). School-based prevention interventions for depression typically involve delivering a series of modules that have been adapted from conventional psychotherapeutic interventions (usually cognitive-behavioural therapy or CBT) and are categorised according to the target population (Stockings et al. 2016). These include: (1) ‘universal prevention’ which targets everyone in the population regardless of underlying risk; (2) ‘selective prevention’ which targets population subgroups with an elevated risk profile (e.g., children of parents with a mental illness or pregnant women at risk of perinatal depression); and (3) ‘indicated prevention’ which targets high-risk individuals with subthreshold symptoms that fall just below the diagnostic threshold for a mental disorder (Mrazek & Haggerty, 1994).
A recent review demonstrated that school-based psychological interventions are cost-effective in preventing the onset of depressive disorders in youth (Mihalopoulos & Chatterton, 2015). Likewise, an Australian study by Mihalopoulos et al. (2012) found that delivering a school-based indicated prevention intervention to youth aged 11–17 years was cost-effective. Since the publication of these studies, however, there have been several advances in the literature with regards to: (1) the epidemiology of depression (Slade et al. 2009; Vos et al. 2015); (2) the efficacy of universal school-based prevention (Merry et al. 2011); and (3) internet-based delivery of psychological interventions as an alternative to face-to-face delivery (Andrews & Titov, 2010; Calear & Christensen, 2010). To date, no study has concurrently analysed the population cost-effectiveness of universal and indicated prevention interventions among youth, delivered via the internet or face-to-face. Our study will build upon previous work undertaken by Mihalopoulos et al. (2012) which examined the cost-effectiveness of indicated prevention for depression in Australian school students. It aims to: (1) examine the population cost-effectiveness (i.e., value for money) of delivering indicated and universal prevention services to youth in the population aged 11–17 years via primary and secondary schools in Australia; and (2) compare the comparative cost-effectiveness of delivering these interventions using face-to-face and internet-based delivery mechanisms.
Methods
Analytic approach
This economic evaluation used a standardised approach for assessing cost-effectiveness (ACE) previously developed for evaluating health care interventions in the Australian context (Carter et al. 2008; Mihalopoulos et al. 2013). We reviewed literature on the prevention of depression to identify all interventions targeting youth aged 5–17 years that: (1) would be suitable for implementation in Australia; and (2) had evidence of efficacy to support analysis. Multiple studies of the same type of intervention were combined in a meta-analysis. We excluded studies that were too heterogeneous to: enable a precise definition of the intervention and comparator; or accurate measurement of resources used. Interventions were selected based on the strength of evidence of effectiveness (internal validity) and generalisability of the setting/population to the Australian context (external validity).
We developed a decision-analytic model to calculate the costs and benefits of implementing chosen interventions in the Australian context among youth aged 11–17 years (see Section 1.2 of the supplementary appendix for rationale). The baseline analysis modelled intervention pathways using best available information on costs and benefits from a range of data sources for demography, disease epidemiology and burden, health system costs and cost offsets that best describe services in the Australian context. In the absence of Australia-specific information, we used data from intervention trials to inform decision modelling. Assumptions were made to fill data gaps for several model parameters, which were tested in subsequent univariate sensitivity analyses. Detailed inclusion criteria for input model parameters are shown in Section 1 of the supplementary appendix. This study adopted a ‘health and education’ sector perspective, which encompassed the cost and health consequences accruing to: students and parents; school staff; health care providers; and third-party payers. Productivity costs (i.e., decreased labour productivity and/or absenteeism attributable to poor health) fall beyond the health/education sector and were thus excluded. Time and travel costs of intervention participants were excluded from the baseline analysis, but included in a sensitivity analysis.
We conducted a cost-utility analysis, which evaluated health outcomes using Disability-adjusted Life Years (DALYs), rather than the Quality-adjusted Life Year (QALY) measure. These were calculated using disability weights that employ a standardised set of weights across all diseases (Salomon et al. 2015). We developed a cost-effectiveness model using Microsoft Excel 2013 to calculate incremental cost-effectiveness ratios (ICERs), which were evaluated with respect to a willingness-to-pay threshold of $50 000 per DALY averted commonly used in Australia (Harris et al. 2008; Vos et al. 2010). The costs and benefits of the intervention were both discounted at a rate of 3% per annum with respect to a 2013 reference year. Health price deflators from the Australian Institute of Health and Welfare (AIHW) were used to convert costs into 2013 Australian dollars (AIHW, 2014). This study conforms to Consolidated Health Economic Evaluation Reporting Standards (CHEERS) (Husereau et al. 2013).
Intervention effect sizes for face-to-face delivery
A meta-review by Stockings et al. (2016) collected data from randomised control trials (RCTs) comparing the efficacy of interventions preventing the onset of major depression in youth aged 5–18 years relative to no intervention, placebo or usual care. The inclusion criteria for our model encompassed RCT studies evaluating changes to the number of incident cases of major depression regardless of whether they are measured using structured clinical interviews or cut-offs on a depression symptom rating scale. We excluded RCT studies evaluating outcomes with respect to changes in the mean score on a depression symptom rating scale. This was due to methodological difficulties in determining how changes to a mean score on a depression scale translate into corresponding changes to the number of incident cases.
We found sufficient evidence to meta-analyse three face-to-face intervention types: (1) universal prevention involving group-based psychological interventions delivered to all participating school students; (2) indicated prevention involving group-based psychological interventions delivered to students with subthreshold depression; and (3) indicated prevention involving self-help bibliotherapy delivered to students with subthreshold depression. Group-based psychological interventions typically involve: a teacher or external facilitator; delivering a series of intervention modules based on psychotherapeutic approaches such as CBT; to a group of students in the classroom setting. By contrast, self-help bibliotherapy involves students reading a book containing adapted psychotherapeutic modules.
We calculated pooled intervention effect sizes (expressed as a risk ratio) for each intervention type at: post-intervention, 6-month follow-up, 1-year follow-up and 2-year follow-up. Intervention outcomes were meta-analysed using the ‘quality effects’ (QE) model – which gives greater weight to studies that have a lower risk of bias, as measured using the Cochrane Collaboration's Risk of Bias tool (Doi et al. 2015). All meta-analyses were conducted using MetaXL 3.0, an Excel add-in developed by EpiGear International Pty Ltd (EpiGear, 2015).
Intervention effect sizes for internet-based delivery
The policy relevance of internet-delivered prevention interventions (Calear & Christensen, 2010; Reyes-Portillo et al. 2014; O'Dea et al. 2015) provided a clear rationale for modelling online prevention interventions. However, two relevant RCTs identified in the meta-review, which examine the efficacy of internet-delivered prevention interventions (Calear et al. 2009; Wong et al. 2014), were excluded as they reported changes to mean scores on a depression scale. A way of modelling online prevention interventions would involve assuming that their effect sizes would be equal to some proportion of the pooled intervention effect sizes calculated for face-to-face prevention interventions. This assumption is somewhat reasonable as treatment interventions for adult mental disorders have comparable efficacy when delivered through either face-to-face or internet-delivered modalities (Calear & Christensen, 2010; Cuijpers et al. 2010; Andersson et al. 2014). However, we deemed this assumption too heroic and excluded internet-based prevention interventions from the baseline model; choosing instead to model them in a sensitivity analysis.
Modelling intervention pathways
In the baseline analysis, we chose to model intervention pathways for which we derived pooled intervention effect sizes that reached the 5% level of significance. Universal and indicated psychological interventions were included in the baseline model, while indicated bibliotherapy was excluded (see Section 2 of the supplementary appendix). The structure of the model was based on intervention pathways adapted from the intervention literature. The steps for modelling universal and indicated psychological prevention broadly involved: (1) identifying the population eligible to receive the intervention; (2) estimating health benefits occurring in hypothetical ‘intervention’ and ‘comparator’ scenarios; and (3) calculating the costs associated with each scenario. A comparative analysis was conducted whereby we evaluated the total health impacts and costs that accrue under an intervention scenario with reference to a ‘no intervention’ counterfactual scenario. The intervention scenario simulated how the widespread delivery of universal and indicated prevention would impact on the incidence of depression in the eligible population.
Eligible population
The population eligible for intervention differed between universal and indicated prevention interventions. Both intervention pathways start with youth aged 11–17 years in the 2013 Australian population. In the case of universal prevention, the eligible population involved youth: (1) who attend a participating school; and (2) whose parent's/guardian's provide consent for their children to participate in the intervention. Ambiguity around the true likelihood of school participation in the population led us to assume a 100% participation rate (an assumption we tested in a sensitivity analysis); while the proportion of students who obtain parental consent was based on available data extracted from intervention studies. The eligible population for indicated prevention encompassed students with subthreshold depression. Identifying these students involved: (1) screening students at participating schools for elevated depressive symptoms; and (2) conducting further diagnostic testing to identify students without a depression diagnosis. Like universal prevention, we assumed a 100% school participation rate (the impact of which was tested in a sensitivity analysis). The intervention pathway next involved screening for subthreshold depression by assuming in-class dissemination of the Center for Epidemiologic Studies Depression Scale (CES-D). Students who scored above a CES-D cut-off of 16 would be invited to undergo a diagnostic clinical interview with a psychologist. Those subsequently failing to meet diagnostic criteria for major depression were identified as having subthreshold depression. The student participation rate was, once again, calculated using available data from intervention studies. Detailed methods describing the calculation of the eligible population (partitioned by age and sex) are presented in Section 3 of the supplementary appendix.
Health benefit modelling
We developed a multiple cohort Markov model to simulate disease dynamics that would occur with/without the delivery of universal and indicated prevention interventions (Habbema et al. 2010; Lee et al. 2013). An adapted DisMod 2 model was used to simulate how a population cohort moves between three health states over time – i.e., healthy, diseased and dead (Barendregt et al. 2003). In the universal prevention scenario, the ‘healthy’ and ‘diseased’ health states respectively correspond with those in the at-risk population and those with major depression. For indicated prevention, the ‘healthy’ state was substituted by a ‘subthreshold depression’ state encompassing the eligible population with subthreshold depression. Transitions between health states correspond with known epidemiological parameters (i.e., incidence, remission, case fatality and other mortality). Diagrams of these models are presented in Section 4.1 of the appendix. Our model calculated annual transitions between health states for each age-sex cohort over a 10-year time horizon – which is sufficient to evaluate the health impacts of preventive interventions (Tan-Torres Edejer et al. 2003). The model assumed that all interventions are fully implemented and operate under ‘steady state’ conditions – i.e., trained staff and necessary infrastructure are available to deliver all interventions, which operate in accordance with their effectiveness potential (Carter et al. 2009; Vos et al. 2010).
In the baseline analysis, we modelled intervention effect sizes for follow-up points that reached a 5% level of significance; assuming a null intervention effect size (i.e., no effect) for follow-up points that did not reach statistical significance. The impact of modelling non-significant intervention effect sizes and extrapolating intervention effects using an exponential decay function over the longer term was tested in a sensitivity analysis. Previous meta-analyses included RCTs that measure the number of incident cases using cut-offs on a depression rating scale (Merry et al. 2011). There are, however, criticisms regarding the diagnostic validity of depression rating scales (Stockings et al. 2015). As such, we conducted a sensitivity analysis to test the impact of modelling pooled intervention effect sizes that only include RCTs using a structured clinical interview. In the baseline model, we also meta-analysed RCTs regardless of whether they used an intention-to-treat (ITT) approach or not. A subsequent assumption in the model was that pooled effect sizes account for imperfect adherence (i.e., non-compliance and loss to follow-up) based on an ITT approach. A sensitivity analysis was conducted to test the validity of this assumption by modelling pooled intervention effect sizes based solely on RCTs using an ITT approach.
Our model calculated the total life years lived under the intervention and comparator scenarios, whereby the impact of prevention involved reductions in the current incidence of major depression – i.e., multiplying the incidence rate with the risk ratio of intervention efficacy at applicable time points over the 10-year time horizon. Mitigating the number of healthy (or subthreshold) people who transition to the depressed health state leads to: fewer prevalent YLDs; and a greater number of life years lived via a reduction in excess deaths attributable to major depression. The joint impacts on morbidity and mortality, in turn, lead to a greater number of DALYs averted in the intervention population relative to the comparator. The approach used by this model to simulate the transition from being at-risk to becoming depressed differs from that used by Mihalopoulos et al. (2012) – which used transition probability data derived from RCT studies, rather than population incidence rates.
Prevalent YLDs were calculated by multiplying the prevalence rate calculated by the model with an appropriate disability weight. In the baseline analysis, we derived a composite disability weight for major depression by calculating the weighted average of GBD 2013 disability weights for mild, moderate and severe depression (Salomon et al. 2015). This weighted average was based on a severity distribution derived from the GBD study (Ferrari et al. 2013); which calculated the comorbidity-adjusted proportion of mild, moderate and severe depression using validated SF-12 cut-offs from the 1997 National Survey of Mental Health and Wellbeing (NSMHWB) (Burstein et al. 2015). We conducted a sensitivity analysis to test the impact of using an alternative severity distribution based on DSM-IV diagnostic algorithms for mild, moderate and severe depression in the 1997 NSMHWB – as used in the previous study by Mihalopoulos et al. (2012). In addition, we conducted a sensitivity analysis to test the impact of using utility weights, in the place of disability weights, to calculate QALYs. We sourced data from a meta-analysis by Mohiuddin & Payne (2014) which calculated pooled utility weights for the most common direct and indirect valuation methods used to elicit utilities for major depression – i.e., standard gamble (direct) and EuroQol-5-dimension (EQ-5D) (indirect). Input epidemiologic parameters are briefly outlined in Table 1, with detailed methods presented in Section 4 of the supplementary appendix.
Table 1.
Input parameters and uncertainty ranges for health benefit modelling
| Parameter | Value and uncertainty range | Uncertainty distribution | Source |
|---|---|---|---|
| Effect size (risk ratio) for universal psychological prevention, by follow-up period | Post-intervention: 0.81 (95% CI 0.48–1.38) 6-month follow-up: 0.59 (95% CI 0.43–0.80)** 1-year follow-up: 0.99 (95% CI 0.77–1.27) 2-year follow-up: 1.03 (95% CI 0.81–1.31) |
Lognormal | Own meta-analysis of nine studies |
| Effect size (risk ratio) for indicated psychological prevention, by follow-up period | Post-intervention: 0.32 (95% CI 0.14–0.73)** 6-month follow-up: 0.34 (95% CI 0.20–0.59)** 1-year follow-up: 0.71 (95% CI 0.35–1.43) 2-year follow-up: 0.74 (95% CI 0.41–1.36) |
Lognormal | Own meta-analysis of eight studies |
| Effect size (risk ratio) for indicated bibliotherapy, by follow-up period | 6-month follow-up: 0.54 (95% CI 0.09–3.12) | Lognormal | Own meta-analysis of two studies |
| % of schools participating in screening | 100% | No uncertainty modelled | Own assumption |
| % scoring above CES-D cut-off (indicated only) | Average over 13–17 year age range: 20.6%a See online Supplementary Appendix for age- and sex-specific estimates |
Beta | Sawyer et al. (2000) |
| % of students agreeing to further diagnostic testing (indicated only) | 45.2% (s.e.: 1.8%) | Beta | Own meta-analysis of three indicated studies |
| % with no diagnosis of depression given a CES-D score above cut-off (indicated only) | Average over 13–17 year age range: 95.5%a See online Supplementary Appendix for age- and sex-specific estimates |
Beta | Sawyer et al. (2000) |
| % agreeing to participate in the intervention | Universal: 78.6% (s.e.: 7.2%) Indicated: 92.4% (s.e.: 2.7%) |
Beta | Own meta-analysis of: six universal studies; and five indicated studies |
| Average duration of a depressive episode | 29.9 weeks (or 0.57 years) Based on fitted lognormal distribution (μ = 2.049, σ = 1.599) and 2 weeks minimum duration |
Lognormal | Vos et al. (2004) |
| Incidence of depressionb | Average over 11–27 year age range: 0.10 See online Supplementary Appendix for age- and sex-specific estimates |
No uncertainty modelled | Vos et al. (2015) |
| Incidence rate ratio (IRR) of depression in people with subthreshold depression (indicated only) | 2.6 (95% CI 1.0–6.4) | Lognormal | Own meta-analysis of five studies identified in external meta-review |
| Other-cause mortality rate | Average over 11–17 year age range: 0.00032 See online Supplementary Appendix for age- and sex-specific estimates |
No uncertainty modelled | ABS (2014a) |
| Relative risk (RR) of mortality | 1.9 (95% CI 1.6–2.2) | Lognormal | Baxter et al. (2011) |
| Prevalence of depression (universal only) | Average over 11–27 year age range: 0.05 See online Supplementary Appendix for age- and sex-specific estimates |
No uncertainty modelled | Vos et al. (2015) |
| Disability weight for depressionc | 0.26 (95% CI 0.19–0.32) | Beta | Vos et al. (2015) |
95% CI, Confidence Interval; CES-D, Center for Epidemiologic Studies Depression Scale; GBD, Global Burden of Disease study; NSMHWB, National Survey of Mental Health and Wellbeing; s.e., standard error.
**Effect size p-value < 0.05.
Values for the 13-year-olds used for the 11- and 12-year-olds.
Incidence reflects average depressive episode duration of 29.9 weeks. See Online Supplementary Appendix for detailed methods on how GBD 2013 incidence estimates were adjusted to reflect an average episode duration of 29.9 weeks.
This is the weighted average of disability weights for mild, moderate and severe depression which were combined using a severity distribution (i.e., proportion of mild, moderate and severe cases) derived from the GBD study.
Costing analysis
The baseline model assumed that intervention delivery would occur via the public sector. The costs for face-to-face universal prevention involved intervention delivery through secondary school teachers who are trained by a salaried psychologist to teach intervention material during class hours. By contrast, the costs for face-to-face indicated prevention included: (1) using trained secondary school teachers to disseminate CES-D questionnaires to screen for elevated symptoms of depression; (2) having salaried psychologists offer further diagnostic testing to identify cases of subthreshold depression in students with depressive symptoms; and (3) intervention delivery through a psychologist who offers group-based sessions.
In the sensitivity analysis, internet-based delivery of universal psychological prevention was modelled on the assumption that eligible participants completed online modules during class hours under minimal teacher supervision (i.e., the teacher supervises the students but does not actively facilitate the completion of modules); while internet-based delivery of indicated psychological prevention involved eligible participants completing internet modules (potentially outside of the classroom setting). Both forms of internet-delivery are considered unmoderated (i.e., do not involve active therapeutic supervision from a clinician or trained facilitator). For completeness, we also modelled the cost-effectiveness of internet-delivered prevention when it is clinician-moderated (i.e., self-directed completion of modules by students with periodic monitoring by a health professional or clinician).
Cost offsets (i.e., treatment costs averted through prevention) were included in the baseline analysis. Time and travel costs were excluded at baseline, but considered in a sensitivity analysis. A full description of intervention pathways and associated costs is provided in Section 5 of the supplementary appendix. Resource use parameters and unit costs are shown in Table 2.
Table 2.
Input parameters and uncertainty ranges for costing analysis
| Parameter | Values | Uncertainty distribution | Source |
|---|---|---|---|
| Cost parameters relating to both face-to-face and internet-delivered intervention pathways | |||
| Average number of teachers per school | 32.8 | No uncertainty modelled | ABS (2014b) |
| Average number of students per class | 23.1 | No uncertainty modelled | OECD (2014) |
| Average hourly wage rate for salaried staff (including 30% on-costs)a | Teacher: $45.26 (s.e.: 1.05) Psychologist: $42.33 (s.e.: 3.10) |
Lognormal | ABS (2015) |
| Average time spent by a salaried psychologist per school training teachers to deliver universal prevention (universal prevention only) | 17.2 h (s.e.: 13.5) | Lognormal | Own meta-analysis of five universal studies |
| Average time spent by a salaried psychologist per school training teachers to conduct CES-D screening (indicated prevention only) | 1.0 h (range: ±20%) | Pert | Own assumption |
| Average time per student for a salaried school psychologist to administer DISC-IV modules(indicated prevention only)b | 0.53 h (range: 0.39–0.67) | Pert | Kamphaus & Mays (2011) |
| Annual cost of a prevalent case of depression (for the calculation of cost offsets) | $1182 (s.e.: 104) | Lognormal | AIHW (2010) |
| Cost parameters relating only to face-to-face intervention pathways | |||
| Unit cost of MBS-funded psychologist (indicated prevention only) | Single visit: $120.40c Group session: $30.13 |
No uncertainty modelled | Relevant MBS items from the Australian Government Department of Health and Ageing (2012) |
| Total no. of face-to-face intervention sessions offered to studentsd | Universal: 10.1 (s.e.: 1.5) Indicated: 9.9 (s.e.: 3.6) |
Lognormal | Own meta-analysis of: nine universal studies; and eight indicated studies |
| Average duration for each face-to-face intervention sessiond | Universal: 1.2 h (s.e.: 0.4) Indicated: 1.2 h (s.e.: 0.4) |
Lognormal | Own meta-analysis of: nine universal studies; and eight indicated studies |
| Cost parameters relating only to internet-delivered intervention pathways | |||
| Average annual cost of internet-delivered preventione | Unmoderated: $10.87 (range: ± 20%) Clinician-moderated: $223 (range: 55–392) |
Pert | Clinical Research Unit for Anxiety and Depression (2015); and MindSpot Clinic (2015). |
| Total no. of internet-delivered intervention sessions offered to studentsf | Universal: 5.5 (s.e.: 0.7) Indicated: 5.5 (s.e.: 0.7) |
Lognormal | Own meta-analysis of two universal prevention studies |
| Average duration for each internet-delivered intervention sessionf | Universal: 0.8 h (s.e.: 0.4) Indicated: 0.8 h (s.e.: 0.4) |
Lognormal | Own meta-analysis of two universal prevention studies |
| Cost parameters used in univariate sensitivity analyses | |||
| Unit cost of bibliotherapy manual (when modelling the cost-effectiveness of indicated bibliotherapy) | $24.14 (range: ±20%) | Pert | RRP of ‘The Feeling Good Book’ by David Byrne |
| Time cost (per hour) | $9.96 | No uncertainty modelled | Vos et al. (2010) |
| Average total number of hours used in the valuation of parental time (indicated prevention only)g | Diagnostic testing with school psychologist (following CES-D screening): 97 308 h Intervention delivery – initial consult: 161 835 h Intervention delivery – group-based sessions: 1 921 794 hh |
N/A | Own calculations (see Section 6.3 of the supplementary appendix for details) |
| Travel cost (per trip) | $24.67 | No uncertainty modelled | Vos et al. (2010) |
| Average total number of trips used in the valuation of parental travel (indicated prevention only)g | Diagnostic testing with school psychologist (following CES-D screening): 368 745 trips Intervention delivery – initial consult: 323 671 trips Intervention delivery – group-based sessions: 3 236 705 tripsh |
N/A | Own calculations (see Section 6.3 of the supplementary appendix for details) |
ABS, Australian Bureau of Statistics; AIHW, Australian Institute of Health and Welfare; DISC-IV, Diagnostic Interview Schedule for Children; MBS, Medicare Benefits Schedule; N/A, Not applicable; RRP, Recommended Retail Price; s.e., Standard Error.
Assumed 30% on-costs for all salaries/wages to account for additional employee overheads (e.g., superannuation and leave entitlements). On-costs were not applied to MBS-items.
Estimate of time spent administering the DISC-IV modules for depression and anxiety only.
Here we assume that an initial one-on-one visit to a psychologist (costed using the relevant MBS items) is required for orientation prior to the student participating in group-based indicated prevention sessions.
Here we assume that universal prevention is delivered to a group in-class by a trained teacher, while indicated prevention is delivered in a group setting by a psychologist costed using relevant MBS items.
The average cost for unmoderated internet-based prevention was used in the baseline analysis, while the average cost of clinician-moderated internet-based prevention was used in the sensitivity analysis.
Only two universal prevention studies contained data on the total number and duration of internet-delivered sessions. As such, we assumed that this was similar across both indicated and universal prevention delivered via the internet.
Time and travel costs were not applicable to the universal prevention intervention as the intervention was conducted in schools (i.e., no additional travel required by parents apart from usual travel to transport children to and from school).
This parameter was calculated by multiplying the total number of group sessions offered by the average duration for each group session. The precise number of group-based sessions is dependent on the input parameter entitled, ‘Total no. of face-to-face intervention sessions offered to students’, where the total reported here is based on an approximate average of 10 group sessions (i.e., 9.9 rounded to the nearest whole number).
Uncertainty and sensitivity analysis
We conducted uncertainty analyses alongside baseline cost-effectiveness models to evaluate the impact of parameter uncertainty on the final results. We used Ersatz (version 1.31, Sunrise Beach, Australia; available at: http://www.epigear.com/) to perform Monte Carlo simulation with 3000 iterations and produce 95% UI for DALY's averted, net costs and ICERs. Uncertainty parameters are presented in Tables 1 and 2.
We also conducted a series of univariate sensitivity analyses to evaluate the impact of: (1) excluding cost offsets; (2) including time and travel costs; (3) assuming a school participation rate of 50%; (4) modelling non-significant intervention effect sizes and extrapolating an exponential decay rate over time; (5) modelling effect sizes based on RCTs using structured clinical interviews; (6) modelling effect sizes based on RCTs using an ITT analysis; (7) using a weighted average disability weight based on a severity distribution derived from DSM-IV algorithms for mild, moderate and severe depression; (8) using pooled standard gamble and EQ-5D utility weights; (9) modelling internet-delivered intervention pathways when assuming 100/50% efficacy relative to face-to-face interventions and unmoderated/clinician-moderated cost profiles; and (10) applying different discount rates to costs and benefits. In the sensitivity analysis of internet-delivered intervention pathways, we conducted a threshold analysis to test the impact of: (1) varying the relative efficacy of universal and indicated prevention, when assuming unmoderated and clinician-moderated internet-delivery pathways; and (2) varying the average intervention cost of indicated and universal internet prevention, when adopting an effect size of 100 and 50% relative to face-to-face intervention.
Results
Baseline cost-effectiveness results are shown in Table 3. We found that universal and indicated prevention interventions delivered to students via face-to-face intervention pathways were both cost-effective relative to a $50 000 per DALY threshold. Baseline sensitivity analysis results are shown in Table 4. Across the majority of scenarios, we observed that cost-effectiveness results were either consistent or more favourable relative to baseline. For instance, cost-effectiveness results differed little from baseline when: assuming a 50% school participation rate; and using different permutations of discount rates. The cost-effectiveness of universal and indicated prevention improved greatly when modelling non-significant effect sizes and long-term health impacts. Lower ICERs were also observed when: using an alternative severity distribution to calculate a composite disability weight for depression; and using utility weights based on either standard gamble (direct) or EQ-5D (indirect) valuation methods. The exclusion of cost offsets led to marginally higher ICERs compared with baseline; while the addition of time and travel costs led to indicated prevention having a lower probability of being cost-effective.
Table 3.
Results of the baseline model examining the cost-effectiveness of indicated and universal psychological interventions delivered via face-to-face intervention pathways
| Model output | Universal psychological | Indicated psychological |
|---|---|---|
| Intervention costs (95% UI) AU$ thousands |
37 178 (16 404–72 107) | 77 592 (48 096–118 754) |
| Cost offsets (95% UI) AU$ thousands |
−15 376 (−22 968 to −7585) | −18 749 (−41 988 to −5 853) |
| Net costs (95% UI) AU$ thousands |
21 802 (−75 to 55 743) | 58 843 (23 460–102 573) |
| DALYs averted (95% UI) | 3367 (1618–5184) | 4083 (1295–9361) |
| Mean ICER (95% UI) AU$ per DALY averted |
7350 (dominates – 23 070) | 19 550 (3081–56 713) |
95% UI, 95% uncertainty interval; AU$, Australian dollars; DALYs, disability-adjusted life years; ICER, incremental cost-effectiveness ratio.
Table 4.
Results of univariate sensitivity analyses
| Sensitivity analysis | Universal psychological ICER (95% UI) AU$ per DALY averted |
Indicated psychological ICER (95% UI) AU$ per DALY averted |
Indicated bibliotherapy ICER (95% UI) AU$ per DALY averted |
|---|---|---|---|
| Baseline model | 7350 (dominates – 23 070) | 19 550 (3081–56 713) | N/A |
| (1) No cost offsets | 11 993 (4483–28 137) | 24 220 (7608–61 106) | N/A |
| (2) Time and travel costs | N/A | 48 694 (11 154–146 530) | N/A |
| (3) Assume a 50% school participation rate | 7537 (dominates – 24 561) | 18 345 (2993–56 837) | N/A |
| (4) Model non-significant intervention effect sizes & extrapolate health benefits using an exponential decay rate | 1118 (dominates – 32 801) | 6671 (dominates – 29 980) | Dominates* (dominates* – 3594) |
| (5) Model effect sizes based on RCTs using structured clinical interviews only | Dominates (dominates – 4000) | 17 889 (2214–58 953) | N/A |
| (6) Model intervention effect sizes based on RCTs using an ITT analysis only | 15 521 (dominates – 41 658) | 20 783 (3012–64 316) | N/A |
| (7) Calculate the weighted average disability weight by using an alternative severity distribution based on DSM-IV algorithms for mild, moderate and severe depression | 4723 (dominates – 15 509) | 11 951 (1805–34 862) | N/A |
| (8a) Using the standard gamble utility weight (direct valuation) | 5403 (dominates – 19 513) | 11 294 (1791–48 375) | N/A |
| (8b) Using the EQ-5D utility weight (indirect valuation) | 3983 (dominates – 13 465) | 10 721 (1476–32 133) | N/A |
| (9a) Internet-delivered intervention pathway, assuming it is unmoderated and has 100% efficacy relative to face-to-face prevention interventions | 4890 (553–14 398) | Dominates (dominates – 3076) | N/A |
| (9b) Internet-delivered intervention pathway, assuming it is unmoderated and has 50% efficacy relative to face-to-face prevention interventions | 14 657 (5779–34 273) | 1698 (dominates – 10 186) | N/A |
| (9c) Internet-delivered intervention pathway, assuming it is clinician-moderated and has 100% efficacy relative to face-to-face prevention interventions | 113 960 (42 370–243 209) | 8711 (dominates – 30 536) | N/A |
| (9d) Internet-delivered intervention pathway, assuming it is clinician-moderated and has 50% efficacy relative to face-to-face prevention interventions | 227 922 (93 124–467 802) | 23 153 (4060–63 650) | N/A |
| (10a) Discount rate of 0% for health benefits and 3% for intervention costs | 7154 (3–24 070) | 18 751 (2799–54 418) | N/A |
| (10b) Discount rate of 6% for health benefits and 3% for intervention costs | 8503 (dominates – 25 277) | 20 187 (2720–59 167) | N/A |
| (10c) Discount rate of 3% for health benefits and 0% for intervention costs | 7430 (dominates – 24 641) | 19 081 (dominates – 58 970) | N/A |
| (10d) Discount rate of 3% for health benefits and 6% for intervention costs | 7771 (185–24 225) | 19 888 (2969–59 960) | N/A |
95% UI, 95% uncertainty interval; EQ-5D, EuroQol-5-dimension; ICER, incremental cost-effectiveness ratio; ITT, intention-to-treat; N/A, not applicable; RCT, randomised control trial.
A sizeable proportion of uncertainty iterations for indicated bibliotherapy lie in both the northwest and southeast quadrants of the cost-effectiveness plane – signifying that there is a dual likelihood of indicated bibliotherapy being either a dominating or dominated intervention.
Modelling intervention effect sizes based on RCTs using structured clinical interviews led to lower ICERs for universal and indicated prevention relative to baseline. The ICER for indicated prevention remained stable when modelling intervention effect sizes based on RCTs using ITT analysis; though a higher ICER was observed for universal prevention. Internet-delivered indicated prevention had a high probability of being cost-effective, even when assuming clinician-moderated pathways and 50% efficacy relative to face-to-face. Alternatively, internet-delivered universal prevention was only cost-effective when modelling it as an unmoderated intervention.
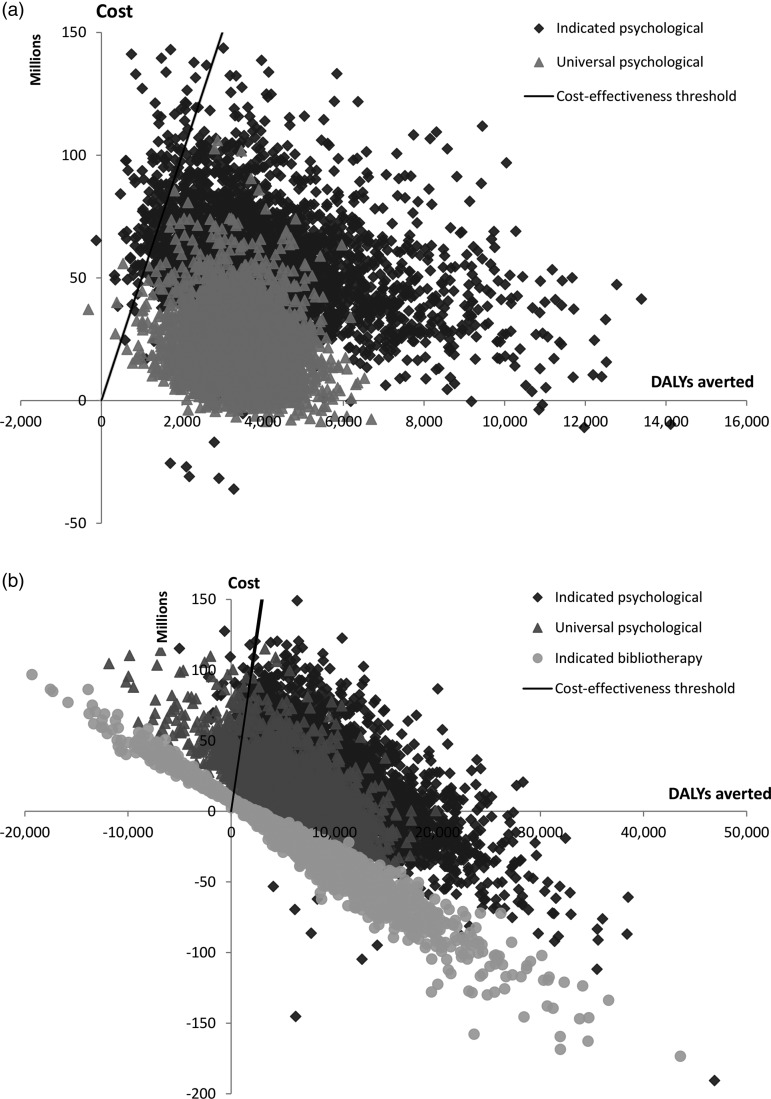
Figure 1 presents the results of the baseline model on a cost-effectiveness plane, alongside the sensitivity analysis modelling non-significant effect sizes over the long-term. In the baseline model, we observed that most uncertainty iterations for universal and indicated prevention interventions lie below the $50 000 per DALY threshold (i.e., high probability of cost-effectiveness). When modelling non-significant effect sizes we observed improvements in cost-effectiveness for universal and indicated prevention interventions (i.e., the uncertainty cloud moves downwards), alongside an increase in uncertainty around health benefits along the x-axis. Indicated bibliotherapy was cost-effective; however, we observed wide UI that intersected both the southeast and northwest quadrants of the cost-effectiveness plane – i.e., bibliotherapy can be either cost-saving or uneconomical.
Fig. 1.
Cost-effectiveness plane of: (a) the baseline analysis and (b) the sensitivity analysis modelling non-significant effect sizes over the long-term.
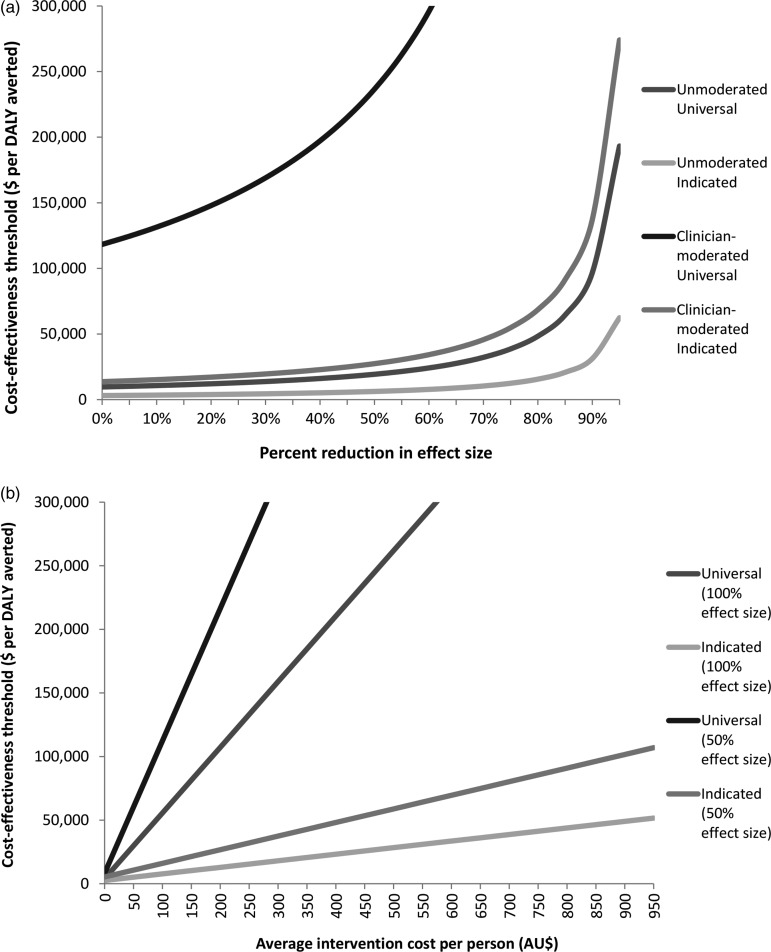
Figure 2 presents results of threshold analyses conducted to test the impact of varying the relative efficacy and average intervention cost of internet-delivered prevention. Internet-delivered indicated prevention (both unmoderated and clinician-moderated) remained cost-effective relative to the $50 000 per DALY threshold despite substantial variations in imputed efficacy and the average intervention cost. For instance, the ICER for clinician-moderated indicated prevention remained below the threshold despite assuming an effect size that is 70% lower than that of face-to-face delivery. Likewise, increasing the average intervention cost of indicated prevention up to $400 per person still resulted in an ICER below the threshold. By contrast, the cost-effectiveness of internet-delivered universal prevention was highly sensitive to variations in cost, where small changes to the average cost per person can lead to large changes in the resulting ICER. For instance, internet-delivered universal prevention (assuming 100% efficacy) was no longer cost-effective when the average intervention cost became greater than $90 per person.
Fig. 2.
Threshold analysis of internet-delivered prevention interventions conducted to examine the impact of varying: (a) the effect size and (b) the average intervention cost per person.
Discussion
Summary of findings and comparison with previous studies
The results of our study represent a scenario where prevention interventions are assumed to be properly implemented with high fidelity. We found that universal and indicated prevention interventions for youth are cost-effective when delivered through face-to-face intervention pathways. Despite available RCT studies only demonstrating significant intervention effects up to 6 months of follow-up (and not beyond), our baseline model provides support for the cost-effectiveness of universal and indicated prevention interventions delivered in schools. While this study is Australia-specific, the model can act as a template for cost-effectiveness studies on the prevention of mental disorders in other countries.
We conducted univariate sensitivity analyses to test the impact of several model assumptions. Overall, we found that ICERs were similar to or more favourable (i.e., lower) than ICERs calculated in the baseline model. For instance, using a 50% school participation rate did not affect resulting ICERs as net costs in the numerator and total benefits in the denominator are both reduced proportionally – i.e., costs and benefits both halve, while the ratio between the two remains constant. The true school participation rate is an implementation issue and, while 100% participation may be unlikely, these results represent the maximal distribution of costs and benefits in the Australian population; which can be adjusted to reflect a more appropriate coverage rate. Baseline assumptions regarding the meta-analysis of intervention effect sizes were found to be robust to changes in the scope of pooled RCT studies (i.e., whether they involved ITT analysis or used structured clinical interviews). Assuming different permutations of discount rates also had a minimal impact on resulting ICERs as intervention effect sizes are limited to the first year post-intervention.
The only scenario in which ICERs increased substantially involved the inclusion of time and travel costs when calculating the ICER for indicated prevention. A higher ICER was also observed for universal prevention when modelling intervention effect sizes based on ITT analysis only; though this remained well below the $50 000 per DALY threshold. In the scenario modelling non-significant effect sizes, indicated bibliotherapy was found to be cost-effective. However, caution should be applied when interpreting this result given the wide UI (i.e., there is a high probability that this intervention is inefficacious and, in turn, uneconomical).
The sensitivity analysis involving internet-based intervention pathways provides preliminary support for the implementation of internet-delivered prevention interventions in schools. The threshold analysis demonstrated that unmoderated, internet-delivered prevention interventions (both universal and indicated) were cost-effective relative to a $50 000 per DALY threshold despite an 80% reduction in the effect size relative to face-to-face intervention. Furthermore, internet-delivered indicated prevention moderated by a clinician remained cost-effective even after a 70% reduction in the relative effect size. While clinician-moderated universal prevention was not deemed cost-effective, it is likely that the unmoderated intervention pathway would be implemented in practice. These results suggest a high probability of internet-based prevention interventions being cost-effective, even despite lower effect sizes relative to face-to-face modalities.
Our baseline model generated higher ICERs for face-to-face indicated prevention than that observed in the prior study by Mihalopoulos et al. (2012); which calculated an ICER of $5400 per DALY averted (95% uncertainty interval (UI): 1400–32 000). This divergence is attributable to major changes in model assumptions, parameters and the overall modelling structure. The sensitivity analysis modelling non-significant effect sizes into the long-term calculated an ICER of $6671 per DALY averted (95% UI: dominates – 29 980). It follows that the results of this sensitivity analysis best represent the model developed by Mihalopoulos et al. (2012); which also modelled intervention effectiveness up to 12 months (based on the literature available at the time) followed by a linear decay rate over 5 years. From this, it appears that the choice of model assumptions – rather than changes to the overall model structure – explains observed differences in study findings.
The baseline ICER for indicated prevention was larger than a previous study by Lynch et al. (2005) which found an ICER of $9275 (95% CI dominates – $45 641) when evaluating the cost-effectiveness of a group-based psychological intervention delivered to adolescent offspring of depressed parents in the U.S. Interestingly, our findings for universal prevention contradict a recent economic evaluation conducted alongside a large-scale RCT of universal prevention among schools in the UK (Anderson et al. 2014). Despite high levels of fidelity and adherence, this study found that classroom-based CBT did not lead to clinically significant reductions in depressive symptoms (measured using the Short Mood and Feelings Questionnaire or SMFQ) and led to a negligible mean difference in QALYs (measured using the EQ-5D) when compared with usual school provision. It is unclear why the universal intervention did not work in this study, or if there were particular contextual or study design factors that adversely impacted on the findings. The results in this solitary study are contrary to our meta-analysis of eight universal RCT studies, which measured changes in the onset of diagnosed depression later in life and included studies involving structured clinical interviews. It could be that the EQ-5D is less sensitive in picking up changes to depression status (Mihalopoulos et al. 2014), though this does not explain the null effect observed in relation to outcomes on the SMFQ.
System-level implementation of school-based prevention interventions can democratise access to mental health interventions in countries with compulsory education (Fazel et al. 2014a). Internet-based delivery of these interventions is particularly advantageous due to its relative ease of implementation compared with face-to-face delivery. There are, however, several implementation issues that can adversely impact on the cost-effectiveness of school-based prevention. For instance, we were agnostic as to whether indicated prevention was delivered during or after school hours. This distinction is, however, important from an implementation perspective given the risk of stigma due to labelling students with subthreshold depression. Nonetheless, preliminary empirical evidence suggests that a low risk of stigma is possible in a well-implemented programme delivered during school hours (Rapee et al. 2006). Our study found little evidence on the precise cost of internet-based prevention in schools. For example, while economies of scale may arise when using a common IT infrastructure to deliver internet-based prevention (e-Mental Health Alliance, 2014), it is unclear what the true costs will be when accounting for the large-scale expansion of existing IT infrastructure. In addition, there are issues around intervention adherence, uptake and the suitability of internet-based intervention modalities to consumers (Christensen et al. 2009; e-Mental Health Alliance, 2014).
There are arguments both for and against the involvement of teachers in the face-to-face delivery of school-based prevention. Delivering intervention material through teachers can facilitate the promotion of mental health literacy in the broader school setting as teachers are better educated to deal with mental health issues. Conversely, teachers may be too overworked and undermotivated to properly engage with intervention material (Han & Weiss, 2005). In a sensitivity analysis, we assumed that the fidelity of internet-based prevention was comparable with face-to-face intervention delivery. It is possible that internet-based delivery leads to better fidelity as the intervention is highly structured and less susceptible to facilitators departing from the intervention material (i.e., intervention drift) (Calear & Christensen, 2010). There are, however, concerns that self-directed completion of internet-based modules may lead to poorer rates of adherence (Christensen et al. 2009) – though this may be less relevant in the context of compulsory education. Evaluating the cost-effectiveness of treating students diagnosed with major depression following indicated prevention screening was beyond our study scope. Though Mihalopoulos et al. (2012) note that cases of major depression are unlikely to be ignored after being identified through screening, suggesting that screening and treatment can be effective for both prevention and treatment.
Strengths and limitations
Strengths of our study include: utilising the latest data on intervention efficacy and depression epidemiology; employing similar methods to concurrently evaluate face-to-face and internet-based delivery of universal and indicated prevention interventions; applying conservative assumptions, where possible; and conducting extensive testing of model parameters and assumptions. There are, however, several limitations. First, our study narrowly focussed on health benefits linked to the prevention of incident depression only. Current evidence suggests that school-based prevention programmes can have benefits across the continuum of internalising disorders (Stockings et al. 2016) and lead to potential improvements in: education outcomes among students (Dix et al. 2012); and mental health outcomes in teachers (Tyson et al. 2009). Second, our study excluded evidence from RCT studies assessing continuous changes on depression symptom rating scales. It is unlikely that this would have biased our study results as: we conducted a separate meta-analysis of RCTs measuring changes in depressive symptoms which also found universal and indicated prevention interventions to be efficacious (Stockings et al. 2016); and there was comparable risk of bias between studies measuring depression outcomes and those measuring depressive symptoms. Third, our model assumed that preventive interventions for depression led to a reduction in depression incidence based on the outcomes of meta-analysed RCT studies. However, short study timeframes (up to 2-years follow-up) mean that it is unclear whether such interventions actually prevent the incidence of depression or merely delay its onset (van Zoonen et al. 2014). These short study timeframes should not, however, adversely affect our baseline results given that we only modelled statistically significant intervention effect sizes occurring between post-intervention and 1-year follow-up (extrapolation of intervention effect sizes was constrained to the sensitivity analysis).
We sought to obtain the best available evidence to inform model parameters (see Section 1.3 of the supplementary appendix). Nevertheless, there were several data limitations, which we will briefly outline below. First, we modelled intervention pathways for indicated prevention using estimates from the 1997–1998 National Survey for Mental Health and Wellbeing – Child and Adolescent component (Sawyer et al. 2000); as the latest 2013–2014 population survey of mental disorders among youth in Australia (Lawrence et al. 2015) did not contain usable data to determine subthreshold depression cases via screening for elevated depression symptoms. According to Lawrence et al. (2015), the prevalence of major depression increased from 2.1% in 1998 to 3.2% in 2013–2014. It is, however, unlikely that this increase would alter the final ICER for indicated prevention as it would only impact the coverage of eligible students (cf. school participation rate). Second, we used data from intervention studies to impute intervention participation rates, which may differ in the Australian population. Third, we modelled the cost-effectiveness of interventions by assuming that interventions are fully implemented and their effectiveness corresponded with pooled intervention efficacy. Implementation factors can, however, adversely impact on the actual cost-effectiveness of these interventions. Fourth, universal prevention studies generally had a higher risk of bias than indicated prevention studies; and were less likely to conduct an ITT analysis or use structured clinical interviews to measure depression outcomes. Fifth, the results of the sensitivity analysis modelling the cost-effectiveness of internet-delivered prevention interventions should be interpreted with caution given the paucity of information on the efficacy and cost of these intervention pathways. Further evidence is needed to better understand the costs and efficacy of internet-delivered prevention interventions in schools.
Conclusion
Our study found that system-level implementation of indicated and universal school-based prevention interventions represents value for money. Nonetheless, the cost-effectiveness of these interventions is ultimately dependent on overcoming several implementation issues beyond the scope of this study. Further evaluation of the cost-effectiveness of school-based prevention will be required as evidence regarding system-level implementation of these programmes is refined.
Acknowledgements
The authors would like to acknowledge the conceptual contributions of Ron Rapee, Sally Merry, Helen Christensen, Aliza Werner-Seidler and Yael Perry.
Financial Support
This project was funded through the Australian Government National Health and Medical Research Council (NHMRC) Centre of Research Excellence in Mental Health Systems Improvement (CREMSI) (grant no. APP1041131). The views expressed in this manuscript are solely those of the authors and do not reflect the views of the NHMRC. Furthermore, the funding source had no involvement in: the study design; the collection, analysis or interpretation of data; in the writing of the report; or in the decision to submit the paper for publication. C. M. is supported by an NHMRC Early Career Fellowship (grant no. APP1035887). G. A. P. is supported by an NHMRC Senior Principal Research Fellowship (grant no. APP 1019887). Y. Y. L., A. J. F. and H. A. W. are affiliated with the Queensland Centre for Mental Health Research which receives its core funding from Queensland Health. E. A. S. is affiliated with the National Drug and Alcohol Research Centre at the University of New South Wales which is supported by funding from the Australian Government under the Substance Misuse Prevention and Service Improvements Grants Fund. The funders had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript.
Conflicts of Interest
J. J. B. owns Epigear International, which sells the Ersatz software used in the analysis. The other authors declare no conflicts of interest.
Ethical Standard
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
Availability of data and methods
Data supporting the findings of our study can be found in Tables 1 and 2 of the main manuscript and the online supplementary appendix. These data are also available upon request from the study authors.
Supplementary material
For supplementary material accompanying this paper visit http://dx.doi.org/10.1017/S2045796016000469.
click here to view supplementary material
References
- ABS (2014a). 3302.0 – Deaths, Australia, 2013 [Online]. Australian Bureau of Statistics: Canberra. Retrieved 16 September 2015 from http://www.abs.gov.au/ausstats/abs@.nsf/mf/3302.0/
- ABS (2014b). 4221.0 – Schools, Australia, 2014 [Online]. Australian Bureau of Statistics: Canberra. Retrieved 16 September 2015 from http://www.abs.gov.au/ausstats/abs@.nsf/mf/4221.0
- ABS (2015). 6306.0 – Employee Earnings and Hours, Australia, May 2014 [Online]. Australian Bureau of Statistics: Canberra. Retrieved 16 September 2015 from http://www.abs.gov.au/ausstats/abs@.nsf/mf/6306.0/
- AIHW (2010). Health System Expenditure on Disease and Injury in Australia, 2004–05. Australian Institute of Health and Welfare: Canberra. [Google Scholar]
- AIHW (2014). Health Expenditure Australia 2012–13. Australian Institute of Health and Welfare: Canberra. [Google Scholar]
- Anderson R, Ukoumunne OC, Sayal K, Phillips R, Taylor JA, Spears M, Araya R, Lewis G, Millings A, Montgomery AA, Stallard P (2014). Cost-effectiveness of classroom-based cognitive behaviour therapy in reducing symptoms of depression in adolescents: a trial-based analysis. Journal of Child Psychology and Psychiatry 55, 1390–1397. [DOI] [PubMed] [Google Scholar]
- Andersson G, Cuijpers P, Carlbring P, Riper H, Hedman E (2014). Guided Internet-based vs. face-to-face cognitive behavior therapy for psychiatric and somatic disorders: a systematic review and meta-analysis. World Psychiatry 13, 288–295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andrews G, Titov N (2010). Treating people you never see: internet-based treatment of the internalising mental disorders. Australian Health Review 34, 144–147. [DOI] [PubMed] [Google Scholar]
- Andrews G, Issakidis C, Sanderson K, Corry J, Lapsley H (2004). Utilising survey data to inform public policy: comparison of the cost-effectiveness of treatment of ten mental disorders. British Journal of Psychiatry 184, 526–533. [DOI] [PubMed] [Google Scholar]
- Australian Government Department of Health and Ageing (2012). Medicare Benefits Schedule Book: Operating from 01 July 2013. Commonwealth of Australia: Canberra. [Google Scholar]
- Barendregt JJ, Van Oortmarssen GJ, Vos T, Murray CJ (2003). A generic model for the assessment of disease epidemiology: the computational basis of DisMod II. Population Health Metrics 1, 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baxter A, Page A, Whiteford H (2011). Factors influencing risk of premature mortality in community cases of depression: a meta-analyitc review. Epidemiology Research International, 1–12. [Google Scholar]
- Burstein R, Fleming T, Haagsma J, Salomon JA, Vos T, Murray CJ (2015). Estimating distributions of health state severity for the global burden of disease study. Population Health Metrics 13, 31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calear AL, Christensen H (2010). Review of internet-based prevention and treatment programs for anxiety and depression in children and adolescents. Medical Journal of Australia 192, S12–S14. [DOI] [PubMed] [Google Scholar]
- Calear AL, Christensen H, Mackinnon A, Griffiths KM, O'Kearney R (2009). The YouthMood Project: a cluster randomized controlled trial of an online cognitive behavioral program with adolescents. Journal of Consulting and Clinical Psychology 77, 1021–1032. [DOI] [PubMed] [Google Scholar]
- Carter R, Vos T, Moodie M, Haby M, Magnus A, Mihalopoulos C (2008). Priority setting in health: origins, description and application of the Australian Assessing Cost-Effectiveness initiative. Expert Review of Pharmacoeconomics and Outcomes Research 8, 593–617. [DOI] [PubMed] [Google Scholar]
- Carter R, Moodie M, Markwick A, Magnus A, Vos T, Swinburn B, Haby MM (2009). Assessing cost-effectiveness in obesity (ACE-obesity): an overview of the ACE approach, economic methods and cost results. BMC Public Health 9, 419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christensen H, Griffiths KM, Farrer L (2009). Adherence in internet interventions for anxiety and depression. Journal of Medical Internet Research 11, e13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clinical Research Unit for Anxiety and Depression (2015). THIS WAY UP: Online Treatment, Education and Research in Anxiety and Depression [Online]. St Vincent's Hospital Sydney: Sydney. Retrieved 10 September 2015 from https://thiswayup.org.au/.
- Cuijpers P, Donker T, van Straten A, Li J, Andersson G (2010). Is guided self-help as effective as face-to-face psychotherapy for depression and anxiety disorders? A systematic review and meta-analysis of comparative outcome studies. Psychological Medicine 40, 1943–1957. [DOI] [PubMed] [Google Scholar]
- Dix KL, Slee PT, Lawson MJ, Keeves JP (2012). Implementation quality of whole-school mental health promotion and students’ academic performance. Child and Adolescent Mental Health 17, 45–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doi SA, Barendregt JJ, Khan S, Thalib L, Williams GM (2015). Advances in the meta-analysis of heterogeneous clinical trials II: the quality effects model. Contemporary Clinical Trials 45, 23–29. [DOI] [PubMed] [Google Scholar]
- e-Mental Health Alliance (2014). e-Mental Health Services in Australia 2014: Current and Future [Online]. e-Mental Health Alliance: Australia. Retrieved 20 October 2015 from https://emhalliance.fedehealth.org.au/wp-content/uploads/sites/42/2014/10/e-Mental-Health-in-Australia-2014.pdf
- EpiGear (2015). MetaXL (Version 3.0) [Online]. EpiGear International: Sunrise Beach, QLD. Retrieved 15 September 2015 from http://www.epigear.com/index_files/metaxl.html
- Fazel M, Hoagwood K, Stephan S, Ford T (2014a). Mental health interventions in schools 1: mental health interventions in schools in high-income countries. Lancet Psychiatry 1, 377–387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fazel M, Patel V, Thomas S, Tol W (2014b). Mental health interventions in schools in low-income and middle-income countries. Lancet Psychiatry 1, 388–398. [DOI] [PubMed] [Google Scholar]
- Ferrari AJ, Charlson FJ, Norman RE, Patten SB, Freedman G, Murray CJ, Vos T, Whiteford HA (2013). Burden of depressive disorders by country, sex, age, and year: findings from the global burden of disease study 2010. PLoS Medicine 10, e1001547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Habbema J, Boer R, Barendregt JJ (2010). Chronic disease modeling In Epidemiology and Demography in Public Health (ed. Killewo J, Heggenhougen K and Quah SR), pp. 173–178. Academic Press/Elsevier: San Diego. [Google Scholar]
- Han SS, Weiss B (2005). Sustainability of teacher implementation of school-based mental health programs. Journal of Abnormal Child Psychology 33, 665–679. [DOI] [PubMed] [Google Scholar]
- Harris AH, Hill SR, Chin G, Li JJ, Walkom E (2008). The role of value for money in public insurance coverage decisions for drugs in Australia: a retrospective analysis 1994–2004. Medical Decision Making 28, 713–722. [DOI] [PubMed] [Google Scholar]
- Husereau D, Drummond M, Petrou S, Carswell C, Moher D, Greenberg D, Augustovski F, Briggs AH, Mauskopf J, Loder E, Force CT (2013). Consolidated health economic evaluation reporting standards (CHEERS) statement. Value Health 16, e1–e5. [DOI] [PubMed] [Google Scholar]
- Jorm AF (2014). Why hasn't the mental health of Australians improved? The need for a national prevention strategy. Australian New Zealand Journal of Psychiatry 48, 795–801. [DOI] [PubMed] [Google Scholar]
- Kamphaus R, Mays K (2011). Chapter 14: assessment of internalizing behavioral deficits In The Oxford Handbook of School Psychology (ed. Bray M and Kehle T), pp. 312–333. Oxford University Press: New York. [Google Scholar]
- Lawrence D, Johnson S, Hafekost J, Boterhoven de Haan K, Sawyer M, Ainley J, Zubrick S (2015). The Mental Health of Children and Adolescents: Report on the second Australian Child and Adolescent Survey of Mental Health and Wellbeing. Department of Health: Canberra. [Google Scholar]
- Lee YY, Veerman JL, Barendregt JJ (2013). The cost-effectiveness of laparoscopic adjustable gastric banding in the morbidly obese adult population of Australia. PLoS ONE 8, e64965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lynch FL, Hornbrook M, Clarke GN, Perrin N, Polen MR, O'Connor E, Dickerson J (2005). Cost-effectiveness of an intervention to prevent depression in at-risk teens. Archives of General Psychiatry 62, 1241–1248. [DOI] [PubMed] [Google Scholar]
- Merry SN, Hetrick SE, Cox GR, Brudevold-Iversen T, Bir JJ, McDowell H (2011). Psychological and educational interventions for preventing depression in children and adolescents. Cochrane Database of Systematic Reviews, CD003380. [DOI] [PubMed] [Google Scholar]
- Mihalopoulos C, Chatterton ML (2015). Economic evaluations of interventions designed to prevent mental disorders: a systematic review. Early Intervention in Psychiatry 9, 85–92. [DOI] [PubMed] [Google Scholar]
- Mihalopoulos C, Vos T, Pirkis J, Carter R (2012). The population cost-effectiveness of interventions designed to prevent childhood depression. Pediatrics 129, e723–e730. [DOI] [PubMed] [Google Scholar]
- Mihalopoulos C, Carter R, Pirkis J, Vos T (2013). Priority-setting for mental health services. Journal of Mental Health 22, 122–134. [DOI] [PubMed] [Google Scholar]
- Mihalopoulos C, Chen G, Iezzi A, Khan MA, Richardson J (2014). Assessing outcomes for cost-utility analysis in depression: comparison of five multi-attribute utility instruments with two depression-specific outcome measures. British Journal of Psychiatry 205, 390–397. [DOI] [PubMed] [Google Scholar]
- MindSpot Clinic (2015). MindSpot: Online Assessment and Treatment for Anxiety and Depression [Online]. Access Macquarie Ltd: Macquarie Park, NSW. Retrieved 10 September 2015 from https://mindspot.org.au/.
- Mohiuddin S, Payne K (2014). Utility values for adults with unipolar depression: systematic review and meta-analysis. Medical Decision Making 34, 666–685. [DOI] [PubMed] [Google Scholar]
- Mrazek P, Haggerty R (1994). Reducing Risks for Mental Disorders: Frontiers for Preventive Intervention Research. National Academy Press: Washington, DC. [PubMed] [Google Scholar]
- Murray CJ, Vos T, Lozano R, Naghavi M, Flaxman AD, Michaud C, Ezzati M, Shibuya K, Salomon JA, Abdalla S, Aboyans V, Abraham J, Ackerman I, Aggarwal R, Ahn SY, Ali MK, Alvarado M, Anderson HR, Anderson LM, Andrews KG, Atkinson C, Baddour LM, Bahalim AN, Barker-Collo S, Barrero LH, Bartels DH, Basanez MG, Baxter A, Bell ML, Benjamin EJ, Bennett D, Bernabe E, Bhalla K, Bhandari B, Bikbov B, Bin Abdulhak A, Birbeck G, Black JA, Blencowe H, Blore JD, Blyth F, Bolliger I, Bonaventure A, Boufous S, Bourne R, Boussinesq M, Braithwaite T, Brayne C, Bridgett L, Brooker S, Brooks P, Brugha TS, Bryan-Hancock C, Bucello C, Buchbinder R, Buckle G, Budke CM, Burch M, Burney P, Burstein R, Calabria B, Campbell B, Canter CE, Carabin H, Carapetis J, Carmona L, Cella C, Charlson F, Chen H, Cheng AT, Chou D, Chugh SS, Coffeng LE, Colan SD, Colquhoun S, Colson KE, Condon J, Connor MD, Cooper LT, Corriere M, Cortinovis M, de Vaccaro KC, Couser W, Cowie BC, Criqui MH, Cross M, Dabhadkar KC, Dahiya M, Dahodwala N, Damsere-Derry J, Danaei G, Davis A, De Leo D, Degenhardt L, Dellavalle R, Delossantos A, Denenberg J, Derrett S, Des Jarlais DC, Dharmaratne SD, Dherani M, Diaz-Torne C, Dolk H, Dorsey ER, Driscoll T, Duber H, Ebel B, Edmond K, Elbaz A, Ali SE, Erskine H, Erwin PJ, Espindola P, Ewoigbokhan SE, Farzadfar F, Feigin V, Felson DT, Ferrari A, Ferri CP, Fevre EM, Finucane MM, Flaxman S, Flood L, Foreman K, Forouzanfar MH, Fowkes FG, Fransen M, Freeman MK, Gabbe BJ, Gabriel SE, Gakidou E, Ganatra HA, Garcia B, Gaspari F, Gillum RF, Gmel G, Gonzalez-Medina D, Gosselin R, Grainger R, Grant B, Groeger J, Guillemin F, Gunnell D, Gupta R, Haagsma J, Hagan H, Halasa YA, Hall W, Haring D, Haro JM, Harrison JE, Havmoeller R, Hay RJ, Higashi H, Hill C, Hoen B, Hoffman H, Hotez PJ, Hoy D, Huang JJ, Ibeanusi SE, Jacobsen KH, James SL, Jarvis D, Jasrasaria R, Jayaraman S, Johns N, Jonas JB, Karthikeyan G, Kassebaum N, Kawakami N, Keren A, Khoo JP, King CH, Knowlton LM, Kobusingye O, Koranteng A, Krishnamurthi R, Laden F, Lalloo R, Laslett LL, Lathlean T, Leasher JL, Lee YY, Leigh J, Levinson D, Lim SS, Limb E, Lin JK, Lipnick M, Lipshultz SE, Liu W, Loane M, Ohno SL, Lyons R, Mabweijano J, MacIntyre MF, Malekzadeh R, Mallinger L, Manivannan S, Marcenes W, March L, Margolis DJ, Marks GB, Marks R, Matsumori A, Matzopoulos R, Mayosi BM, McAnulty JH, McDermott MM, McGill N, McGrath J, Medina-Mora ME, Meltzer M, Mensah GA, Merriman TR, Meyer AC, Miglioli V, Miller M, Miller TR, Mitchell PB, Mock C, Mocumbi AO, Moffitt TE, Mokdad AA, Monasta L, Montico M, Moradi-Lakeh M, Moran A, Morawska L, Mori R, Murdoch ME, Mwaniki MK, Naidoo K, Nair MN, Naldi L, Narayan KM, Nelson PK, Nelson RG, Nevitt MC, Newton CR, Nolte S, Norman P, Norman R, O'Donnell M, O'Hanlon S, Olives C, Omer SB, Ortblad K, Osborne R, Ozgediz D, Page A, Pahari B, Pandian JD, Rivero AP, Patten SB, Pearce N, Padilla RP, Perez-Ruiz F, Perico N, Pesudovs K, Phillips D, Phillips MR, Pierce K, Pion S, Polanczyk GV, Polinder S, Pope CA III, Popova S, Porrini E, Pourmalek F, Prince M, Pullan RL, Ramaiah KD, Ranganathan D, Razavi H, Regan M, Rehm JT, Rein DB, Remuzzi G, Richardson K, Rivara FP, Roberts T, Robinson C, De Leon FR, Ronfani L, Room R, Rosenfeld LC, Rushton L, Sacco RL, Saha S, Sampson U, Sanchez-Riera L, Sanman E, Schwebel DC, Scott JG, Segui-Gomez M, Shahraz S, Shepard DS, Shin H, Shivakoti R, Singh D, Singh GM, Singh JA, Singleton J, Sleet DA, Sliwa K, Smith E, Smith JL, Stapelberg NJ, Steer A, Steiner T, Stolk WA, Stovner LJ, Sudfeld C, Syed S, Tamburlini G, Tavakkoli M, Taylor HR, Taylor JA, Taylor WJ, Thomas B, Thomson WM, Thurston GD, Tleyjeh IM, Tonelli M, Towbin JA, Truelsen T, Tsilimbaris MK, Ubeda C, Undurraga EA, van der Werf MJ, van Os J, Vavilala MS, Venketasubramanian N, Wang M, Wang W, Watt K, Weatherall DJ, Weinstock MA, Weintraub R, Weisskopf MG, Weissman MM, White RA, Whiteford H, Wiebe N, Wiersma ST, Wilkinson JD, Williams HC, Williams SR, Witt E, Wolfe F, Woolf AD, Wulf S, Yeh PH, Zaidi AK, Zheng ZJ, Zonies D, Lopez AD, AlMazroa MA, Memish ZA (2012). Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 380, 2197–2223. [DOI] [PubMed] [Google Scholar]
- O'Dea B, Calear AL, Perry Y (2015). Is e-health the answer to gaps in adolescent mental health service provision? Current Opinion in Psychiatry 28, 336–342. [DOI] [PubMed] [Google Scholar]
- OECD (2014). Education at a Glance 2014: OECD Indicators. OECD Publishing: Paris. [Google Scholar]
- Patton GC, Coffey C, Romaniuk H, Mackinnon A, Carlin JB, Degenhardt L, Olsson CA, Moran P (2014). The prognosis of common mental disorders in adolescents: a 14-year prospective cohort study. Lancet 383, 1404–1411. [DOI] [PubMed] [Google Scholar]
- Pirkis J, Hickie I, Young L, Burns J, Highet N, Davenport T (2005). An evaluation of beyondblue, Australia's national depression initiative. International Journal of Mental Health Promotion 7, 35–53. [Google Scholar]
- Rapee RM, Wignall A, Sheffield J, Kowalenko N, Davis A, McLoone J, Spence SH (2006). Adolescents’ reactions to universal and indicated prevention programs for depression: perceived stigma and consumer satisfaction. Prevention Science 7, 167–177. [DOI] [PubMed] [Google Scholar]
- Reyes-Portillo JA, Mufson L, Greenhill LL, Gould MS, Fisher PW, Tarlow N, Rynn MA (2014). Web-based interventions for youth internalizing problems: a systematic review. Journal of the American Academy of Child and Adolescent Psychiatry 53, 1254–1270 e5. [DOI] [PubMed] [Google Scholar]
- Salomon JA, Haagsma JA, Davis A, de Noordhout CM, Polinder S, Havelaar AH, Cassini A, Devleesschauwer B, Kretzschmar M, Speybroeck N, Murray CJ, Vos T (2015). Disability weights for the global burden of disease 2013 study. Lancet Global Health 3, e712–e723. [DOI] [PubMed] [Google Scholar]
- Sawyer M, Arney F, Baghurst P, Clark J, Graetz B, Kosky R, Nurcombe B, Patton G, Prior M, Raphael B, Rej J, Whaites L, Zubrick S (2000). Child and Adolescent Component of the National Survey of Mental Health and Well-Being. Mental Health and Special Programs Branch, Commonwealth Department of Health and Aged Care: Canberra. [Google Scholar]
- Slade T, Johnston A, Oakley Browne MA, Andrews G, Whiteford H (2009). 2007 National Survey of Mental Health and Wellbeing: methods and key findings. Australian New Zealand Journal of Psychiatry 43, 594–605. [DOI] [PubMed] [Google Scholar]
- Stockings E, Degenhardt L, Lee YY, Mihalopoulos C, Liu A, Hobbs M, Patton G (2015). Symptom screening scales for detecting major depressive disorder in children and adolescents: a systematic review and meta-analysis of reliability, validity and diagnostic utility. Journal of Affective Disorders 174, 447–463. [DOI] [PubMed] [Google Scholar]
- Stockings EA, Degenhardt L, Dobbins T, Lee YY, Erskine HE, Whiteford HA, Patton G (2016). Preventing depression and anxiety in young people: a review of the joint efficacy of universal, selective and indicated prevention. Psychological Medicine 46, 11–26. [DOI] [PubMed] [Google Scholar]
- Tan-Torres Edejer T, Baltussen R, Adam T, Hutubessy R, Acharya A, Evans DB, Murray CJL (2003). Making Choices in Health: WHO Guide to Cost-effectiveness Analysis. World Health Organization: Geneva. [Google Scholar]
- Thapar A, Collishaw S, Pine DS, Thapar AK (2012). Depression in adolescence. Lancet 379, 1056–1067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tyson O, Roberts CM, Kane R (2009). Can implementation of a resilience program for primary school children enhance the mental health of teachers? Australian Journal of Guidance and Counselling 19, 116–130. [Google Scholar]
- van Zoonen K, Buntrock C, Ebert DD, Smit F, Reynolds CF III, Beekman AT, Cuijpers P (2014). Preventing the onset of major depressive disorder: a meta-analytic review of psychological interventions. International Journal of Epidemiology 43, 318–329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vos T, Haby MM, Barendregt JJ, Kruijshaar M, Corry J, Andrews G (2004). The burden of major depression avoidable by longer-term treatment strategies. Archives of General Psychiatry 61, 1097–1103. [DOI] [PubMed] [Google Scholar]
- Vos T, Carter R, Barendregt JJ, Mihalopoulos C, Veerman JL, Magnus A, Cobiac L, Bertram MY, ACE-Prevention Team (2010). Assessing Cost-Effectiveness in Prevention (ACE–Prevention): Final Report. University of Queensland: Brisbane. [Google Scholar]
- Vos T, Barber RM, Bell B, Bertozzi-Villa A, Biryukov S, Bolliger I, Charlson F, Davis A, Degenhardt L, Dicker D, Duan L, Erskine H, Feigin VL, Ferrari AJ, Fitzmaurice C, Fleming T, Graetz N, Guinovart C, Haagsma J, Hansen GM, Hanson SW, Heuton KR, Higashi H, Kassebaum N, Kyu H, Laurie E, Liang X, Lofgren K, Lozano R, MacIntyre MF, Moradi-Lakeh M, Naghavi M, Nguyen G, Odell S, Ortblad K, Roberts DA, Roth GA, Sandar L, Serina PT, Stanaway JD, Steiner C, Thomas B, Vollset SE, Whiteford H, Wolock TM, Ye P, Zhou M, Ãvila MA, Aasvang GM, Abbafati C, Ozgoren AA, Abd-Allah F, Aziz MIA, Abera SF, Aboyans V, Abraham JP, Abraham B, Abubakar I, Abu-Raddad LJ, Abu-Rmeileh NME, Aburto TC, Achoki T, Ackerman IN, Adelekan A, Ademi Z, Adou AK, Adsuar JC, Arnlov J, Agardh EE, Al Khabouri MJ, Alam SS, Alasfoor D, Albittar MI, Alegretti MA, Aleman AV, Alemu ZA, Alfonso-Cristancho R, Alhabib S, Ali R, Alla F, Allebeck P, Allen PJ, AlMazroa MA, Alsharif U, Alvarez E, Alvis-Guzman N, Ameli O, Amini H, Ammar W, Anderson BO, Anderson HR, Antonio CAT, Anwari P, Apfel H, Arsenijevic VSA, Artaman A, Asghar RJ, Assadi R, Atkins LS, Atkinson C, Badawi A, Bahit MC, Bakfalouni T, Balakrishnan K, Balalla S, Banerjee A, Barker-Collo SL, Barquera S, Barregard L, Barrero LH, Basu S, Basu A, Baxter A, Beardsley J, Bedi N, Beghi E, Bekele T, Bell ML, Benjet C, Bennett DA, Bensenor IM, Benzian H, Bernabe E, Beyene TJ, Bhala N, Bhalla A, Bhutta Z, Bienhoff K, Bikbov B, Abdulhak AB, Blore JD, Blyth FM, Bohensky MA, Basara BB, Borges G, Bornstein NM, Bose D, Boufous S, Bourne RR, Boyers LN, Brainin M, Brauer M, Brayne CEG, Brazinova A, Breitborde NJK, Brenner H, Briggs ADM, Brooks PM, Brown J, Brugha TS, Buchbinder R, Buckle GC, Bukhman G, Bulloch AG, Burch M, Burnett R, Cardenas R, Cabral NL, Nonato IRC, Campuzano JC, Carapetis JR, Carpenter DO, Caso V, Castaneda-Orjuela CA, Catala-Lopez F, Chadha VK, Chang J-C, Chen H, Chen W, Chiang PP, Chimed-Ochir O, Chowdhury R, Christensen H, Christophi CA, Chugh SS, Cirillo M, Coggeshall M, Cohen A, Colistro V, Colquhoun SM, Contreras AG, Cooper LT, Cooper C, Cooperrider K, Coresh J, Cortinovis M, Criqui MH, Crump JA, Cuevas-Nasu L, Dandona R, Dandona L, Dansereau E, Dantes HG, Dargan PI, Davey G, Davitoiu DV, Dayama A, De la Cruz-Gongora V, de la Vega SF, De Leo D, del Pozo-Cruz B, Dellavalle RP, Deribe K, Derrett S, Des Jarlais DC, Dessalegn M, deVeber GA, Dharmaratne SD, Diaz-Torne C, Ding EL, Dokova K, Dorsey ER, Driscoll TR, Duber H, Durrani AM, Edmond KM, Ellenbogen RG, Endres M, Ermakov SP, Eshrati B, Esteghamati A, Estep K, Fahimi S, Farzadfar F, Fay DFJ, Felson DT, Fereshtehnejad S-M, Fernandes JG, Ferri CP, Flaxman A, Foigt N, Foreman KJ, Fowkes FGR, Franklin RC, Furst T, Futran ND, Gabbe BJ, Gankpe FG, Garcia-Guerra FA, Geleijnse JM, Gessner BD, Gibney KB, Gillum RF, Ginawi IA, Giroud M, Giussani G, Goenka S, Goginashvili K, Gona P, de Cosio TG, Gosselin RA, Gotay CC, Goto A, Gouda HN, Guerrant Rl, Gugnani HC, Gunnell D, Gupta R, Gupta R, Gutierrez RA, Hafezi-Nejad N, Hagan H, Halasa Y, Hamadeh RR, Hamavid H, Hammami M, Hankey GJ, Hao Y, Harb HL, Haro JM, Havmoeller R, Hay RJ, Hay S, Hedayati MT, Pi IBH, Heydarpour P, Hijar M, Hoek HW, Hoffman HJ, Hornberger JC, Hosgood HD, Hossain M, Hotez PJ, Hoy DG, Hsairi M, Hu H, Hu G, Huang JJ, Huang C, Huiart L, Husseini A, Iannarone M, Iburg KM, Innos K, Inoue M, Jacobsen KH, Jassal SK, Jeemon P, Jensen PN, Jha V, Jiang G, Jiang Y, Jonas JB, Joseph J, Juel K, Kan H, Karch A, Karimkhani C, Karthikeyan G, Katz R, Kaul A, Kawakami N, Kazi DS, Kemp AH, Kengne AP, Khader YS, Khalifa SEAH, Khan EA, Khan G, Khang Y-H, Khonelidze I, Kieling C, Kim D, Kim S, Kimokoti RW, Kinfu Y, Kinge JM, Kissela BM, Kivipelto M, Knibbs L, Knudsen AK, Kokubo Y, Kosen S, Kramer A, Kravchenko M, Krishnamurthi RV, Krishnaswami S, Defo BK, Bicer BK, Kuipers EJ, Kulkarni VS, Kumar K, Kumar GA, Kwan GF, Lai T, Lalloo R, Lam H, Lan Q, Lansingh VC, Larson H, Larsson A, Lawrynowicz AEB, Leasher JL, Lee J-T, Leigh J, Leung R, Levi M, Li B, Li Y, Li Y, Liang J, Lim S, Lin H-H, Lind M, Lindsay MP, Lipshultz SE, Liu S, Lloyd BK, Ohno SL, Logroscino G, Looker KJ, Lopez AD, Lopez-Olmedo N, Lortet-Tieulent J, Lotufo PA, Low N, Lucas RM, Lunevicius R, Lyons RA, Ma J, Ma S, Mackay MT, Majdan M, Malekzadeh R, Mapoma CC, Marcenes W, March LM, Margono C, Marks GB, Marzan MB, Masci JR, Mason-Jones AJ, Matzopoulos RG, Mayosi BM, Mazorodze TT, McGill NW, McGrath JJ, McKee M, McLain A, McMahon BJ, Meaney PA, Mehndiratta MM, Mejia-Rodriguez F, Mekonnen W, Melaku YA, Meltzer M, Memish ZA, Mensah G, Meretoja A, Mhimbira FA, Micha R, Miller TR, Mills EJ, Mitchell PB, Mock CN, Moffitt TE, Ibrahim NM, Mohammad KA, Mokdad AH, Mola GL, Monasta L, Montico M, Montine TJ, Moore AR, Moran AE, Morawska L, Mori R, Moschandreas J, Moturi WN, Moyer M, Mozaffarian D, Mueller UO, Mukaigawara M, Murdoch ME, Murray J, Murthy KS, Naghavi P, Nahas Z, Naheed A, Naidoo KS, Naldi L, Nand D, Nangia V, Narayan KMV, Nash D, Nejjari C, Neupane SP, Newman LM, Newton CR, Ng M, Ngalesoni FN, Nhung NT, Nisar MI, Nolte S, Norheim OF, Norman RE, Norrving B, Nyakarahuka L, Oh IH, Ohkubo T, Omer SB, Opio JN, Ortiz A, Pandian JD, Panelo CIA, Papachristou C, Park E-K, Parry CD, Caicedo AJP, Patten SB, Paul VK, Pavlin BI, Pearce N, Pedraza LS, Pellegrini CA, Pereira DM, Perez-Ruiz FP, Perico N, Pervaiz A, Pesudovs K, Peterson CB, Petzold M, Phillips MR, Phillips D, Phillips B, Piel FB, Plass D, Poenaru D, Polanczyk GV, Polinder S, Pope CA, Popova S, Poulton RG, Pourmalek F, Prabhakaran D, Prasad NM, Qato D, Quistberg DA, Rafay A, Rahimi K, Rahimi-Movaghar V, Rahman SU, Raju M, Rakovac I, Rana SM, Razavi H, Refaat A, Rehm J, Remuzzi G, Resnikoff S, Ribeiro AL, Riccio PM, Richardson L, Richardus JH, Riederer AM, Robinson M, Roca A, Rodriguez A, Rojas-Rueda D, Ronfani L, Rothenbacher D, Roy N, Ruhago GM, Sabin N, Sacco RL, Ksoreide K, Saha S, Sahathevan R, Sahraian MA, Sampson U, Sanabria JR, Sanchez-Riera L, Santos IS, Satpathy M, Saunders JE, Sawhney M, Saylan MI, Scarborough P, Schoettker B, Schneider IJC, Schwebel DC, Scott JG, Seedat S, Sepanlou SG, Serdar B, Servan-Mori EE, Shackelford K, Shaheen A, Shahraz S, Levy TS, Shangguan S, She J, Sheikhbahaei S, Shepard DS, Shi P, Shibuya K, Shinohara Y, Shiri R, Shishani K, Shiue I, Shrime MG, Sigfusdottir ID, Silberberg DH, Simard EP, Sindi S, Singh JA, Singh L, Skirbekk V, Sliwa K, Soljak M, Soneji S, Soshnikov SS, Speyer P, Sposato LA, Sreeramareddy CT, Stoeckl H, Stathopoulou VK, Steckling N, Stein MB, Stein DJ, Steiner TJ, Stewart A, Stork E, Stovner LJ, Stroumpoulis K, Sturua L, Sunguya BF, Swaroop M, Sykes BL, Tabb KM, Takahashi K, Tan F, Tandon N, Tanne D, Tanner M, Tavakkoli M, Taylor HR, Te Ao BJ, Temesgen AM, Have MT, Tenkorang EY, Terkawi AS, Theadom AM, Thomas E, Thorne-Lyman AL, Thrift AG, Tleyjeh IM, Tonelli M, Topouzis F, Towbin JA, Toyoshima H, Traebert J, Tran BX, Trasande L, Trillini M, Truelsen T, Trujillo U, Tsilimbaris M, Tuzcu EM, Ukwaja KN, Undurraga EA, Uzun SB, van Brakel WH, van de Vijver S, Dingenen RV, van Gool CH, Varakin YY, Vasankari TJ, Vavilala MS, Veerman LJ, Velasquez-Melendez G, Venketasubramanian N, Vijayakumar L, Villalpando S, Violante FS, Vlassov VV, Waller S, Wallin MT, Wan X, Wang L, Wang J, Wang Y, Warouw TS, Weichenthal S, Weiderpass E, Weintraub RG, Werdecker A, Wessells KRR, Westerman R, Wilkinson JD, Williams HC, Williams TN, Woldeyohannes SM, Wolfe CDA, Wong JQ, Wong H, Woolf AD, Wright JL, Wurtz B, Xu G, Yang G, Yano Y, Yenesew MA, Yentur GK, Yip P, Yonemoto N, Yoon S-J, Younis M, Yu C, Kim KY, Zaki MES, Zhang Y, Zhao Z, Zhao Y, Zhu J, Zonies D, Zunt JR, Salomon JA, Murray CJL (2015). Global, regional, and national incidence, prevalence, and YLDs for 301 acute and chronic diseases and injuries for 188 countries, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 386, 743–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whiteford H, Harris M, Diminic S (2013). Mental health service system improvement: translating evidence into policy. Australian New Zealand Journal of Psychiatry 47, 703–706. [DOI] [PubMed] [Google Scholar]
- WHO (2012). Depression: a Global Crisis [Online]. World Health Organization: Geneva. Retrieved 14 September 2015 from http://www.who.int/mental_health/management/depression/wfmh_paper_depression_wmhd_2012.pdf.
- Wong N, Kady L, Mewton L, Sunderland M, Andrews G (2014). Preventing anxiety and depression in adolescents: a randomised controlled trial of two school based Internet-delivered cognitive behavioural therapy programmes. Internet Interventions 1, 90–94. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
For supplementary material accompanying this paper visit http://dx.doi.org/10.1017/S2045796016000469.
click here to view supplementary material