Abstract
Aims
To determine the association between the sleep duration and the risk of all-cause mortality in adults.
Methods
A search strategy was conducted in the MEDLINE, CENTRAL, EMBASE and LILACS databases. Searches were also conducted in other databases and unpublished literature. Cohort studies were included without language, time or setting restrictions. The risk of bias was evaluated with a modified Cochrane Collaboration's tool. An analysis of random effects was conducted. The primary outcome was all-cause mortality. The measure of the effect was the risk difference (RD) with a 95% confidence interval (CI). The planned comparisons were 7–9 h of sleep v. <7 h and the same reference v. >9 h.
Results
Thirty-nine studies were included in our qualitative analysis, regarding the quantitative analysis, 19 studies were included in <7 v. 7–9 h analysis, and 18 studies in the >9 v. 7–9 h. A low risk of bias was shown for most of the study items. The overall RD for all-cause mortality was 0.09 (95% CI 0.07–0.11) favouring the >9 h group compared with our reference. In contrast, no differences were found between the <7 h and the reference sleep duration groups (RD 0.00, 95% CI 0.00–0.01).
Conclusion
We found a probable association of long sleep duration and higher mortality; however, it could reflect an underlying systemic or neurological disease that cause sleep fragmentation, deterioration in quality and micro-awakenings.
Key words: Meta-analysis, mortality, sleep, systematic review
Introduction
Although sleep and circadian rhythm are inherent to human body, in recent history, sleep problems have increased and it will keep this trend. The globalisation process and technological advances have led to a 24/7 society and the increasing night-time use of TV, internet and mobile phones prone to inadequate and interrupted sleep (Ferrie et al., 2011). Historically, evidence have shown an association between sleep deprivation and/or fragmentation and bad learning capacity and academic performance (Curcio et al., 2006), and also with public health issues like motor vehicle crashes with high economic impact (Durmer and Dinges, 2005; Pandi-Perumal et al., 2006). All these findings have led medical society to try to establish the association between short sleep duration and medical entities, suggesting that it is associated with increased risk of stroke (Leng et al., 2015), coronary heart disease (Cappuccio et al., 2011), metabolic syndrome (Xi et al., 2014), hypertension (Wang et al., 2012), central adiposity (Sperry et al., 2015), obesity (Wu et al., 2014), type 2 diabetes mellitus (Shan et al., 2015) and a rapid decline in renal function (McMullan et al., 2016). However, short sleep duration is not the only factor related with them. Actually, recent evidence suggests that long sleep duration plays an important role as well, relating it with increased risk of stroke (Leng et al., 2015), coronary heart disease (Cappuccio et al., 2011), colorectal cancer (Lu et al., 2013), type 2 diabetes mellitus (Gottlieb et al., 2005; Shan et al., 2015), impaired glucose tolerance (Gottlieb et al., 2005) and even a cross-sectional observational study suggest that the altered (above or below the median of 7–8 h) usual sleep duration is associated with an increased prevalence of hypertension (Gottlieb et al., 2006).
Additionally, sleep duration has been associated with mortality (Youngstedt and Kripke, 2004; Cappuccio et al., 2010; Shen et al., 2016). Youngstedt and Kripke warned about the U-shaped relationship between the sleep duration and the risk of death and furthermore exposed alternative explanations for this kind of association (Youngstedt and Kripke, 2004). Later this hypothesis was supported by a systematic review (SR) that indicated that both short sleep duration and long sleep duration are predictors of all-cause mortality among adults (Cappuccio et al., 2010). More recently, in a meta-analysis (MA) from prospective cohort studies about this issue, the authors found a U-shaped relationship; therefore, they commented that 7 h/day of sleep duration should be recommended to prevent premature death among adults (Shen et al., 2016).
Although there are multiple published studies, there is still a lack of high-quality evidence to establish this association as a real one. Furthermore, there are new studies that have not been included in previous SR; therefore, we developed this study which aims to determine the association between the sleep duration and the risk of all-cause mortality in adults.
Methods
We performed this review according to the recommendations of the Cochrane Collaboration and following the PRISMA Statement. The PROSPERO registration number is CRD42017076461.
Eligibility criteria
We included both retrospective and prospective cohort studies, which included adults – no pregnant women. The primary outcome was all-cause mortality determined by each study. For all outcomes, studies should have at least 12 months duration for follow-up and the outcome. There were no setting or language restrictions.
Information sources
Literature search was conducted in accordance to recommended (Robinson, 2002). We used medical subject headings (MeSH), Emtree language, Decs and text words related to sleep duration and mortality. We searched MEDLINE (OVID), EMBASE, LILACS and the Cochrane Central Register of Controlled Trials (CENTRAL). To ensure literature saturation, we scanned references from relevant articles identified through the search, conferences, thesis databases, opengray, Google scholar and clinicaltrials.gov, among others. We contacted authors by e-mail in case of missing information.
Data collection
We reviewed each reference by title and abstract. Then we scanned full texts of relevant studies, applied pre-specified inclusion and exclusion criteria and extracted the data. Disagreements were resolved by consensus.
We independently extracted the following information from each article using a standardised form: study design, geographic location, authors names, title, objectives, inclusion and exclusion criteria, number of patients included, losses to follow-up, timing, definition of short, regular and long sleep duration, method to measure sleep duration, definitions of outcomes, outcomes and association measures, sleep duration and funding source.
Risk of bias
The assessment of the risk of bias for each study was made using a modified Cochrane Collaboration tool for assessing the risk of bias, which covers: selection of participants (selection bias), comparability between groups (selection bias), conflict of interest, confounding control, statistical methods, selective reporting (detection and information bias), assessment of the outcome, follow-up long enough and lost to follow-up. Two independent researchers judged about the possible risk of bias from extracted information, rated as ‘high risk’, ‘low risk’ or ‘unclear risk’.
Data analysis/synthesis of results
The statistical analysis was performed using Review Manager 5.3 (RevMan® 5.3). For categorical outcomes, we reported information about risk differences (RD) with 95% confidence intervals (CI), and we pooled the information with a random-effect MA according to the heterogeneity expected. The results were reported in forest plots of the estimated effects of the included studies with a 95% CI. Heterogeneity was evaluated using the I2 test. For the interpretation, it was determined that the values of 25, 50 and 75% in the I2 test correspond to low, medium and high levels of heterogeneity, respectively.
Publication bias
An evaluation was conducted to identify reporting or publication bias using the funnel plot.
Sensitivity analysis
We performed sensitivity analysis extracting weighted studies and running the estimated effect to find differences.
Subgroup analysis
-
•
Gender
-
•
Intervals of sleep duration
-
•
Short or long sleep duration
Results
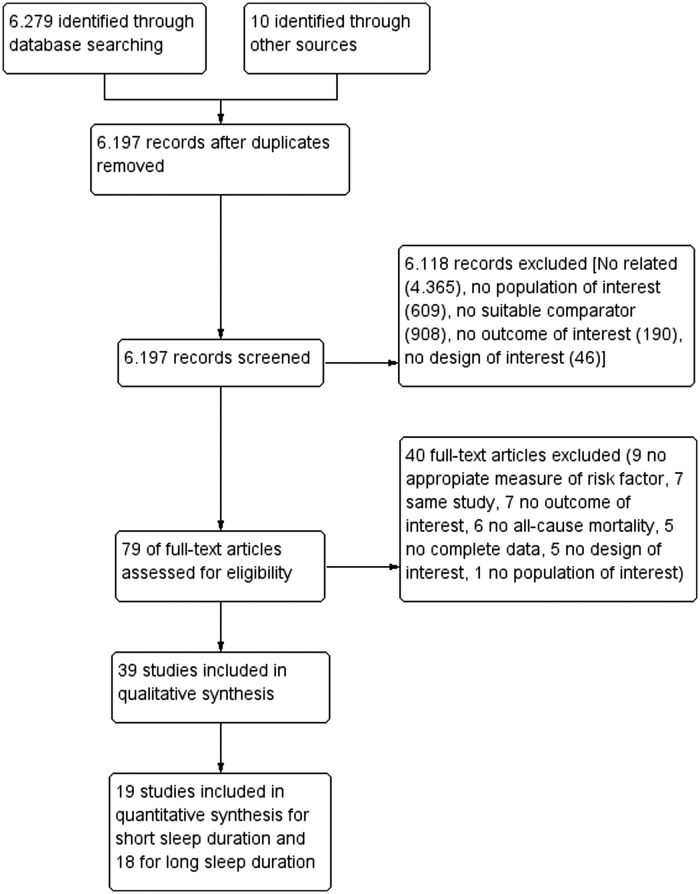
A total of 6289 studies were found with the designed search strategies, with a total of 6197 after duplicates were removed. Finally, 39 studies were included in our SR; however, to perform an MA, we grouped data into three different groups – <7 h, 7–9 h (reference) and more than 9 h – due to the heterogeneity between studies. We excluded the studies that overlapped these intervals from the MA; thus, 19 studies were included in <7 v. 7–9 h MA, and 18 studies in the >9 v. 7–9 h MA (Fig. 1).
Fig. 1.
Flow chart of included studies.
Included studies
Although our starting inclusion criterion was to include clinical trials additionally to cohort studies, none of them was found (Fig. 1). Thirty-nine studies were included in our SR; the reference for normal sleep duration was heterogeneous and the definition for short and long sleep duration varies between studies. Other characteristics were also heterogeneous, for instance included patients that vary from 567 to 135.685, follow-up durations going from 2.8 to 30 years and Africa was the only continent without representation in our study (Table 1). Furthermore, three studies excluded the deaths within 2 years after baseline (Tamakoshi and Ohno, 2004; Lan et al., 2007; Castro-Costa et al., 2011), and in these cases, these data were included; other study (Heslop et al., 2002) made two measurements and reported the results for who did not change the sleep duration, and in this case, these data were included.
Table 1.
Characteristics of included studies
| Author | Cohort name | Country | Age | Gender | Follow-up | N |
|---|---|---|---|---|---|---|
| Pollak et al. (1990) | USA | 65–98 y | M-F | 3.5 y | 1855 | |
| Rumble and Morgan (1992) | Nottingham Longitudinal Study of Activity and Ageing (NLSAA) | England | ⩾65 y | M-F | 5 y | 567 |
| Tsubono et al. (1993) | Japan Collaborative Cohort Study (JACC) | Japan | ⩾40 | M-F | 4 y | 4318 (1717M-2601F) |
| Ruigomez et al. (1995) | Health Interview Survey of Barcelona (HISB) | Spain | ⩾65 y | M-F | 5 y | 989 (395M-594F) |
| Kojima et al. (2000) | Shirakawa Town | Japan | 20–67 y | M-F | 12 y | 5322 (2438M-2884F) |
| Heslop et al. (2002) | Scotland | ⩽65 y | M-F | 25 y | 3030 (2588M-442F) | |
| Mallon et al. (2002) | Sweden | 45–65 y | M-F | 12 y | 1870 (906M-964F) | |
| Burazeri et al. (2003) | Kiryat Yovel Community Health Study (3rd round) | Israel | ⩾50 y | M-F | 9–11 y | 1842 (841M-1001F) |
| Tamakoshi and Ohno (2004) | Japan Collaborative Cohort Study (JACC) | Japan | 40–79 y | M-F | 9.9 y | 102 021 (42 784M-59 237 F) |
| Amagai (2004) | Jichi Medical School Cohort Study | Japan | 19–93 y | M-F | 9 y | 11 325 (4419M-6906F) |
| Patel et al. (2004) | Nurses’ Health Study | USA | 30–55 y | F | 16 y | 82 969 |
| Hublin et al. (2007) | Finnish Twin Cohort | Finland | ⩾24 y | M-F | 21 y | 19 794 (9529M-10 265F) |
| Ferrie et al. (2007) | White Hall II | England | 35–55 | M-F | 17.1 y | 9781 |
| Lan et al. (2007) | Survey of Health and Living Status of the Elderly in Taiwan | Taiwan | ⩾64 y | M-F | 8.4 y | 2834 (1602M-1232F) |
| Gangwisch et al. (2008) | NHANES I | USA | 32–86 y | M-F | 8–10 y | 9789 |
| Suzuki et al. (2009) | Shizuoka Study | Japan | 65–85 | M-F | 7 y | 12 601(6423M-6178 F) |
| Vgontzas et al. (2010) | Penn State Cohort | USA | >20 y | M-F | 14 y M and 10 y F | 1741 (741M-1000 F) |
| Castro-Costa et al. (2011) | Bambui Health and Ageing Study (BHAS) | Brazil | >60 y | M-F | 7.5 y | 1512 |
| Chien et al. (2010) | Chin-Shan Community Cardiovascular Cohort study | Taiwan | ⩾35 y | M-F | 15.9 y | 3430 |
| Mesas et al. (2010) | Spain | ⩾60 y | M-F | 8 y | 3820 | |
| Kutner et al. (2013) | Comprehensive Dialysis Study | US | >18 y | M-F | 5 y | 1440 |
| Rhee et al. (2012) | Seoul Male Cohort Study | South Korea | 40–59 y | M | 16 y | 14 095 |
| Kakizaki et al. (2013) | Ohsaki Cohort Study | Japan | 40–79 y | M-F | 10.8 y | 49 256 (23 749M-25 507F) |
| Cohen-mansfield and Perach (2012) | Cross-Sectional and Longitudinal Aging Study (CALAS) | Israel | 75–94 y | M-F | 20 y | 933 |
| Chen et al. (2013) | Shih-Pai Sleep Study | Taiwan | >65 | M-F | 9 y | 4064 |
| Yeo et al. (2013) | Korean Multi-center Cancer Cohort (KMCC) | South Korea | >20 | M-F | 9.44 y | 13 164 (5447M-7717F) |
| Kim et al. (2014) | Multiethnic Cohort Study | USA | 45–75 y | M-F | 12.9 y | 135 685 (61 936M-73 749) |
| Li et al. (2013) | The SAKUCESS (Saku Cancer Etiology Surveillance) study | Japan | 20–79 y | M-F | 7 y | 9455 |
| Garde et al. (2014) | Copenhagen Male Study | Denmark | 40–59 y | M | 30 y | 4941 |
| Bellavia et al. (2014) | Cohort of Swedish Men and the Swedish Mammography Cohort. | Sweden | 45–83 y | M-F | 15 y | 70 973 |
| Magee et al. (2013) | The 45 and Up Study | Australia | ⩾45 y | M-F | 2.8 y | 227 810 |
| Jung et al. (2013) | Rancho Bernardo Study | USA | >60 y | M-F | 19 y | 2001 (889M-1112F) |
| Xiao et al. (2014) | NIH-AARP Diet and Health Study | USA | 51–72 | M-F | 14 y | 239 896 |
| Rod et al. (2014) | The White Hall II | England | 35–55 y | M-F | 22 y | 9098 (6114M-2984F) |
| Zuurbier et al. (2014) | Rotterdam Study | The Netherlands | ⩾45 y | M-F | 7.3 y | 1734 |
| Kubota et al. (2015) | Japan Collaborative Cohort Study (JACC) | Japan | 40–79 y | M-F | 21 y | 2914 (1674M-1240 F) |
| Hall et al. (2015) | Health, Aging, and Body Composition (Health ABC) study | USA | 70–79 y | M-F | 8.2 y | 3013 |
| Cai et al. (2015) | Shanghai Women's and Men's Health Studies | China | 44–79 y M and 40–75 y F | M-F | 14 y F and 8 y M | 113 138(44 590M-68 548F) |
| Wang et al. (2016) | The Kailuan Study | China | M-F | 3.98 y | 95 903 |
y, years; M, male; F, female.
We excluded Gale and Martyn's study because the risk to measure was time in bed, and no sleep duration was reported (Gale and Martyn, 1998). Other studies were excluded because they did not report the sleep duration adequately (scales or short and long sleep duration pooled together) (Wingard, 1982; Wingard et al., 1982; Martínez-Gómez et al., 2013; Ding et al., 2015; Stamatakis et al., 2015).
Risk of bias
The risk of bias was assessed with a modified Cochrane Collaboration tool (explained above). Although the item for comparability between groups was warning, we have to remark the control they offered for confounding; besides a multivariate analysis in almost all the studies. The assessment of the outcome was graded as low risk in almost all the studies, since they used a good strategy to identify mortality within each population; furthermore, low risk was predominant in remaining items (Table 2).
Table 2.
Risk of bias assessment of included studies
| Author | Selection of participants (selection bias) | Comparability between groups (selection bias) | Conflict of interest | Confounding control | Statistical methods | Selective reporting (information and detection bias) | Assessment of the outcome | Follow-up long enough (5 years) | Lost to follow-up (20%) |
|---|---|---|---|---|---|---|---|---|---|
| Pollak et al. (1990) | Low risk | Unclear risk | Low risk | High risk | Low risk | Low risk | Low risk | High risk | Low risk |
| Rumbleand Morgan (1992) | Low risk | Unclear risk | Low risk | Low risk | High risk (intervals very wide) | Low risk | Unclear risk | Low risk | Low risk |
| Tsubono et al. (1993) | Low risk | Unclear risk | Low risk | Low risk | Low risk | Low risk | Low risk | High risk | Low risk |
| Ruigomez et al. (1995) | Low risk | Unclear risk | Low risk | High risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Kojima et al. (2000) | Low risk | High risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Heslop et al. (2002) | Low risk | Unclear risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Mallon et al. (2002) | Low risk | Unclear risk | Low risk | High risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Burazeri et al. (2003) | Low risk | High risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Tamakoshi and Ohno (2004) | Low risk | Unclear risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Amagai (2004) | Low risk | Unclear risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Patel et al. (2004) | Low risk | High risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Hublin et al. (2007) | Low risk | Unclear risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Ferrie et al. (2007) | Low risk | High risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Unclear risk |
| Lan et al. (2007) | Low risk | Unclear risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Unclear risk |
| Gangwisch et al. (2008) | Low risk | High risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Suzuki et al. (2009) | Low risk | Unclear risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | High Risk |
| Vgontzas et al. (2010) | Low risk | Unclear risk | Low risk | Low risk | High risk | Low risk | Low risk | Low risk | Low risk |
| Castro-Costa et al. (2011) | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Chien et al. (2010) | Low risk | High risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Mesas et al. (2010) | Low risk | High risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Unclear risk |
| Kutner et al. (2013) | Low risk | Unclear risk | Low risk | Low risk | Low risk | Low risk | Low risk | High risk | Low risk |
| Rhee et al. (2012) | Low risk | Unclear risk | Low risk | High risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Kakizaki et al. (2013) | Low risk | High risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Cohen-mansfield and Perach (2012) | Low risk | High risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Chen et al. (2013) | Low risk | Unclear risk | Low risk | High risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Yeo et al. (2013) | Low risk | High risk | Low risk | High risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Kim et al. (2014) | Low risk | High risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Li et al. (2013) | Low risk | Unclear risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Unclear risk |
| Garde et al. (2014) | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Bellavia et al. (2014) | Low risk | Unclear risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Magee et al. (2013) | Low risk | High risk | Low risk | Low risk | Low risk | Low risk | Low risk | High risk | Low risk |
| Jung et al. (2013) | Low risk | High risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Xiao et al. (2014) | Low risk | High risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Rod et al. (2014) | Low risk | Unclear risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Zuurbier et al. (2014) | Low risk | Unclear risk | Low risk | Unclear risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Kubota et al. (2015) | Low risk | Unclear risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Unclear risk |
| Hall et al. (2015) | Low risk | High risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Cai et al. (2015) | Low risk | High risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Wang et al. (2016) | Low risk | High risk | Low risk | Low risk | Low risk | Low risk | Low risk | High risk | Low risk |
Sleep duration and all-cause mortality
The results varied among studies, but most of them reported a higher mortality in long sleep duration groups, while short sleep duration was more controverted (Table 3). Tsubono et al. (1993) and Kubota et al. (2015) had the same cohort (Japan Collaborative Cohort Study), both showed the basic data; however, Kubota et al. (2015) had more participants and longer follow-up period; therefore, we excluded Tsubono et al.’s (1993) data from our MA. Additionally Ferrie et al. (2007) and Rod et al. (2014) also had the same cohort (The White Hall II), but in this case, Ferrie et al. (2007) did not show the basic data, thus this (Ferrie et al., 2007) was the excluded study.
Table 3.
Results within studies
| Author | Reference group (h) | Duration used (h) | Outcome |
|---|---|---|---|
| Pollak et al. (1990) | 0–4, 5, 6, 7, 8, ⩾9 | No association in adjusted analysis | |
| Rumble and Morgan (1992) | 4–9.9 | <4, 4–9.9, ⩾10 | No association |
| Tsubono et al. (1993) | 7–8 | ⩽6, 7–8, ⩾9 | ⩾9 h was associated with higher mortality |
| Ruigomez et al. (1995) | 7–9 | <7, 7–9, >9 | No association in adjusted analysis |
| Kojima et al. (2000) | 7–8.9 | <7, 7–8.9, 9–9.9, ⩾10 | Short sleep duration was associated with higher mortality in males |
| Heslop et al. (2002) | 7–8 | <7, 7–8, >8 | No association in fully adjusted analysis |
| Mallon et al. (2002) | 6–8 | <6, 6–8, >8 | >8 h was associated with higher mortality |
| Burazeri et al. (2003) | <6 | <6, 6–8, >8 | >8 h was associated with higher mortality in males |
| Tamakoshi and Ohno (2004) | 7 | ⩽4, 5, 6, 7, 8, 9, ⩾10 | ⩾8 h was associated with higher mortality in males and females; ⩽4 h in females |
| Amagai (2004) | 7–7.9 | <6, 6–6.9, 7–7.9, 8–8.9, ⩾9 | <6 h was associated with higher mortality in males |
| Patel et al. (2004) | 7 | ⩽5, 6, 7, 8, ⩾9 | ⩾8 h was associated with higher mortality |
| Hublin et al. (2007) | 7–8 | <7, 7–8, >8 | Short and long sleep duration was associated with higher mortality |
| Ferrie et al. (2007) | 7 | ⩽5, 6, 7, 8, ⩾9 | No association in the phase 1; in phase 3 ⩾9 h was associated with higher mortality |
| Lan et al. (2007) | 7–7.9 | <7, 7–7.9, 8–8.9, 9–9.9 ⩾10 | ⩾10 h was associated with higher mortality in males; ⩾8 h in females |
| Gangwisch et al. (2008) | 7 | ⩽5, 6, 7, 8, ⩾9 | ⩾8 h was associated with higher mortality |
| Suzuki et al. (2009) | 7 | ⩽5, 6, 7, 8, 9, ⩾10 | ⩾8 h was associated with higher mortality in general population and males; ⩾10 h in females |
| Vgontzas et al. (2010) | ⩾6. No insomnia | <6 and ⩾6. Insomnia and no insomnia | <6 h with insomnia is associated with higher mortality |
| Castro-Costa et al. (2011) | 7–7.9 | <6, 6–6.9, 7–7.9, 8–8.9, ⩾9 | ⩾8 h was associated with higher mortality |
| Chien et al. (2010) | 7 | ⩽5, 6, 7, 8, ⩾9 | ⩾9 h was associated with higher mortality |
| Mesas et al. (2010) | 7 | ⩽5, 6, 7, 8, 9, 10, ⩾11 | ⩽5 and ⩾8 h were associated with higher mortality |
| Kutner et al. (2013) | 6–7 | <6, 6–7, 7–9, >9 | >9 h was associated with higher mortality |
| Rhee et al. (2012) | ⩾8 | ⩽5, 6–7, ⩾8 | ⩽5 h was associated with higher mortality |
| Kakizaki et al. (2013) | 7 | ⩽6, 7, 8, 9, ⩾10 | ⩾8 h was associated with higher mortality |
| Cohen-mansfield and Perach (2012) | 7–9 | <7, 7–9, >9 | >9 h was associated with higher mortality |
| Chen et al. (2013) | 7 | ⩽4, 5, 6, 7, 8, ⩾9 | ⩾8 h was associated with higher mortality |
| Yeo et al. (2013) | 7 | ⩽5, 6, 7, 8, 9, ⩾10 | ⩽5 and ⩾9 h were associated with higher mortality |
| Kim et al. (2014) | 7 | ⩽5, 6, 7, 8, ⩾9 | ⩽5 and ⩾8 h were associated with higher mortality in males; ⩽5 and ⩾9 h in females |
| Li et al. (2013) | 7 | ⩽5, 6, 7, 8, ⩾9 | ⩾9 h was associated with higher mortality in males and females |
| Garde et al. (2014) | 6–7 | <6, 6–7, ⩾8 | No association in fully adjusted analysis |
| Bellavia et al. (2014) | 6.6–7.4 | <6, 6–6.5, 6.6–7.4, 7.5–8, >8 | ⩽6.5 and >8 h were associated with higher mortality |
| Magee et al. (2013) | 7 | <6, 6, 7, 8, 9, ⩾10 | <6 h and ⩾10 h were associated with higher mortality |
| Jung et al. (2013) | 7–7.9 | <6, 6–6.9, 7–7.9, 8–8.9, ⩾9 | ⩾9 h was associated with higher mortality in females |
| Xiao et al. (2014) | 7–8 | <5, 5–6, 7–8, ⩾9 | Short and long sleep duration was associated with higher mortality |
| Rod et al. (2014) | 7 | ⩽5, 6, 7, 8, ⩾9 | 6 h was associated with higher mortality, but ⩽5 h was not |
| Zuurbier et al. (2014) | 6–7.5 | <6, 6–7.5, >7.5 | No association in fully adjusted analysis |
| Kubota et al. (2015) | 7 | ⩽5, 6, 7, 8, ⩾9 | ⩽5 and ⩾9 h were associated with higher mortality in males; in females just ⩾9 h |
| Hall et al. (2015) | 7 | <6, 6, 7, 8, >8 | No association in fully adjusted analysis |
| Cai et al. (2015) | 7 | 4–5, 6, 7, 8, 9, ⩾10 | ⩽5 and ⩾8 h were associated with higher mortality in females; in males ⩾9 h |
| Wang et al. (2016) | 7 | ⩽5, 6, 7, 8, ⩾9 | ⩽5 and ⩾9 h were associated with higher mortality |
h, hours.
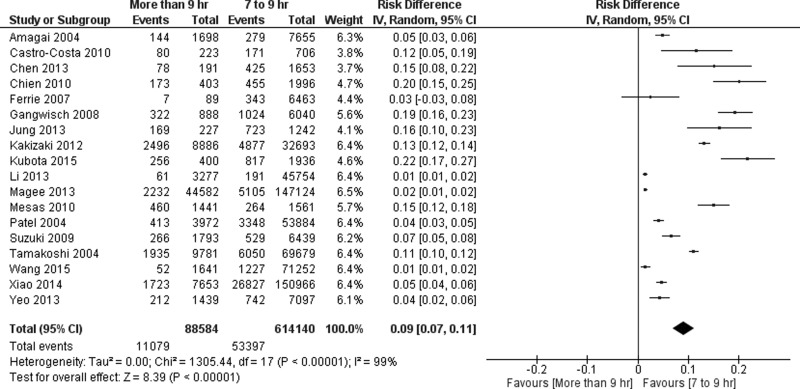
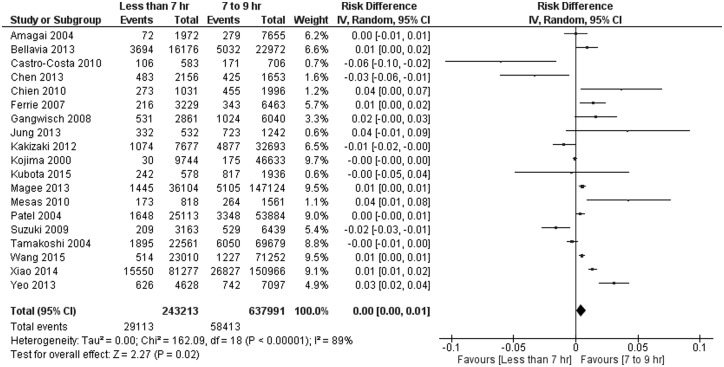
We found an overall RD of 0.09 (95% CI 0.07–0.11) (Table 4) (Fig. 2) favouring mortality in the >9 h group. In contrast, no differences were found between the <7 h and the reference sleep duration groups (RD 0.00, 95% CI 0.00–0.01) (Fig. 3). Similar outcomes were found in the subgroup gender analysis (Table 4).
Table 4.
Subgroup analysis
| Group | Sleep duration | |||||
|---|---|---|---|---|---|---|
| <4 h | <5 h | <6 h | <7 h | 7–9 h | >9 h | |
| General mortality | 0.05 (−0.04, 0.13) | 0.04 (0.02, 0.05)* | 0.01 (0.00, 0.01) | 0.00 (0.00, 0.01) | Ref | 0.09 (0.07, 0.11)* |
| Male | 0.00 (−0.09, 0.09) | −0.01 (−0.06, 0.05) | −0.01 (−0.04, 0.02) | Ref | 0.07 (0.01, 0.12)* | |
| Female | −0.01 (−0.06, 0.04) | −0.01 (−0.03, 0.02) | −0.01 (−0.02, 0.00) | Ref | 0.08 (0.03, 0.12)* | |
h, hours; Ref, reference.
*Statistically significant.
Fig. 2.
Meta-analysis of included studies for long sleep duration. Outcome: mortality.
Fig. 3.
Meta-analysis of included studies for short sleep duration. Outcome: mortality.
Discussion
Summary of the main results
All-cause mortality
Previous SR and MA showed a U-shaped association between sleep duration and mortality (Cappuccio et al., 2010; Shen et al., 2016); however, in our study, we did not find a real association with short sleep duration. We might say that it was an unexpected finding but a really interesting one. Regarding previous SR, Cappuccio et al. in their MA (Cappuccio et al., 2010) did not establish a well-defined parameter for short or normal sleep duration; thus, the comparison was made with many different definitions depending on each study; on the other hand, long sleep duration results were reproducible in our study. Shen et al. in a recent MA (Shen et al., 2016) found an association with both short and long sleep duration, but for longer duration, the association is clearly stronger, and for short duration, the association might be questioned, since it may have occurred for overlapping hours. Therefore, we grouped the studies according to definitions, by exact hours of sleep to prevent overlapping.
Long sleep duration
It is notable that in spite of long sleep duration seems a predictor of mortality, causality is unlikely. We cannot establish if there is any condition that predisposes to greater sleep duration. Magee et al. (2013) found a higher mortality in the <6 and ⩾10 h durations in the entire cohort, but additionally they performed a healthy and unhealthy groups analysis. In the healthy group, no association was found, meaning that sleep duration would be influenced by other conditions, which are the real reasons of higher mortality; however, other studies found association regardless of health status (Patel et al., 2004; Mesas et al., 2010). It is also possible that in this study, long sleep duration group has a greater number of old people; however, most of included studies in our analysis had adjusted analysis with a large number of variables – including age – and association was more consistent with this group. Therefore, these results suggested that long sleep duration should be an independent predictor of all-cause mortality.
The explanations to this association are still in theoretical field. Proposed mechanisms for mortality associated with long sleep include (Grandner and Drummond, 2007; Shen et al., 2016): (1) long sleep is linked to increased sleep fragmentation that is associated with a number of negative health outcomes; (2) long sleep is associated with feelings of fatigue and lethargy that may decrease resistance to stress and disease; (3) changes in cytokine levels associated with long sleep increase mortality risk; (4) long sleepers experience a shorter photoperiod that could increase the risk of death in mammalian species; (5) a lack of physiological challenge with long sleep decrease longevity; (6) underlying disease processes mediate the relationship between long sleep and mortality.
Some patients with neurologic and/or systemic alterations, which modify the quality of dream, could compensate with an increase in total sleep duration, being a marker of disease and, indirectly at least from a theoretical point of view, of mortality.
Short sleep duration
Alterations in the circadian cycle including sleep restriction have been documented in various mammalian and non-mammalian animal models as a risk factor for mortality (Snyder et al., 2013).
Sleep restriction has been associated with different metabolic alterations. The reduction of total sleep duration increases blood pressure, induces insulin resistance and is associated with weight gain and obesity (Grandner et al., 2014). Consequently, sleep restriction is a recognised risk factor for cerebrovascular disease, an important cause of mortality (Eguchi et al., 2008). Sleep restriction has also been associated with dysfunction of the immune system, negative nitrogen balance and protein catabolism (Friese, 2008). In addition, chronic sleep deprivation is fatal in humans, as is the case in patients suffering from fatal familial insomnia, a degenerative brain disorder that results in death between 6 and 24 months from the onset (Manetto et al., 1992). In this study, no increased risk was identified in the group of <7 h of sleep, with boundary hours to 7 being unlikely to represent a risk and to be part of the variability of normal sleep time in the general healthy population. The observed effect of increased risk of mortality with sleep deprivation is best identified with lower total sleep time (<5 h). However, with <4 h of sleep, there are no differences, probably in association with the low number of studies.
Strengths and limitations
The main strength of our study was the well-defined comparison groups. Previous studies used the particular definition from each study to determine the association between sleep duration and mortality; however, we have noticed that many patients were lost to analysis since they were in groups that overlapped with our definition, or – in some studies – the data were shown with measures of association, and the number of patients was not provided. Although all the studies were cohorts, it is unlikely that clinical trials could be performed on this topic due to ethic and methodological issues. Additionally, we suggest that more studies must be performed to evaluate sleep quality, sleep disturbances and other dimensions because sleep duration is just one of sleep-related variables and perhaps molecular studies would be important trying to explain this outcome and the association with mortality.
Conclusion
According to the results, we found a probable association of long sleep duration and higher mortality; however, it could reflect an underlying systemic or neurological disease that causes sleep fragmentation, deterioration in quality and micro-awakenings. We recommend further high-quality studies to establish a well-defined association between sleep duration and mortality since we found many gaps in the literature.
Acknowledgement
We thank every men and women involved in cohorts included in our research.
Data
Data have not been published. The authors could share it if anybody requests it.
Ethical standards
This systematic review and meta-analysis accomplishes all the ethics requirements according to Helsinki declaration and all international statements.
Footnotes
Financial support
None.
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/S2045796018000379.
click here to view supplementary material
Conflict of interest
None.
References
- Amagai Y, Ishikawa S, Gotoh T, Doi Y, Kayaba K, Nakamura Y and Kajii E (2004) Sleep duration and mortality in Japan: the Jichi Medical School Cohort Study. Journal of epidemiology 14, 124–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bellavia A, Åkerstedt T, Bottai M, Wolk A and Orsini N (2014) Sleep duration and survival percentiles across categories of physical activity. American Journal Epidemiology 179, 484–491. [DOI] [PubMed] [Google Scholar]
- Burazeri G, Gofin J and Kark JD (2003) Over 8 hours of sleep – marker of increased mortality in mediterranean population: follow-up population study. Journal of Sleep Research 44, 193–198. [PubMed] [Google Scholar]
- Cai H, Shu X, Xiang Y, Yang G, Li H and Ji B (2015) Sleep duration and mortality: a prospective study of 113 , 138 middle-aged and elderly Chinese men and women. Sleep 38, 529–536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cappuccio FP, D'Elia L, Strazzullo P and Miller MA (2010) Sleep duration and all-cause mortality: a systematic review and meta-analysis of prospective studies. Sleep 33, 585–592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cappuccio FP, Cooper D, Delia L, Strazzullo P and Miller MA (2011) Sleep duration predicts cardiovascular outcomes: a systematic review and meta-analysis of prospective studies. European Heart Journal 32, 1484–1492. [DOI] [PubMed] [Google Scholar]
- Castro-Costa É, Dewey ME, Ferri CP, Uchôa E, Firmo JOA, Rocha FL, Prince M, Lima-Costa MF and Stewart R (2011) Association between sleep duration and all-cause mortality in old age: 9-year follow-up of the Bambuí Cohort Study, Brazil. Journal of Sleep Research 20, 303–310. [DOI] [PubMed] [Google Scholar]
- Chen H, Su T and Chou P (2013) A nine-year follow-up study of sleep patterns and mortality in community-dwelling older adults in Taiwan. Sleep 36, 1187–1198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chien K, Chen P, Hsu H, Su T, Sung F and Chen M (2010) Habitual sleep duration and insomnia and the risk of cardiovascular events and all-cause death: report from a community-based cohort. SLEEP 33, 177–184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen-mansfield J and Perach R (2012) Sleep duration, nap habits, and mortality in older persons. Sleep 35, 1003–1009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curcio G, Ferrara M and De Gennaro L (2006) Sleep loss, learning capacity and academic performance. Sleep Medicine Reviews 10, 323–337. [DOI] [PubMed] [Google Scholar]
- Ding D, Rogers K, van der Ploeg H, Stamatakis E and Bauman AE (2015) Traditional and emerging lifestyle risk behaviors and all-cause mortality in middle-aged and older adults: evidence from a large population-based Australian cohort. PLoS Medicine 12, 1–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Durmer JS and Dinges D (2005) Neurocognitive consequences of sleep deprivation. Seminars in Neurology 25, 117–129. [DOI] [PubMed] [Google Scholar]
- Eguchi K, Pickering TG, Schwartz JE, Hoshide S, Ishikawa J, Ishikawa S, Shimada K and Kario K (2008) Short sleep duration as an independent predictor of cardiovascular events in Japanese patients with hypertension. Archives of Internal Medicine 168, 2225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrie JE, Kumari M, Salo P, Singh-Manoux A and Kivimäki M (2011) Sleep epidemiology – a rapidly growing field. International Journal of Epidemiology 40, 1431–1437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrie JE, Shipley MJ, Cappuccio FP, Brunner E, Miller MA, Kumari M and Marmot MG (2007) A prospective study of change in sleep duration: associations with mortality in the Whitehall II cohort. Sleep 30, 1659–1666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friese RS (2008) Sleep and recovery from critical illness and injury: a review of theory, current practice, and future directions*. Critical Care Medicine 36, 697–705. [DOI] [PubMed] [Google Scholar]
- Gale C and Martyn C (1998) Larks and owls and health, wealth, and wisdom. British Medical Journal (Clinical Research Ed.) 317, 1675–1677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gangwisch JE, Heymsfield SB, Boden-albala B, Buijs RM, Kreier F and Opler MG (2008) Sleep duration associated with mortality in elderly , but not middle-aged , adults in a large US sample. Sleep 31, 1087–1096. [PMC free article] [PubMed] [Google Scholar]
- Garde A, Hansen Å, Holtermann A, Gyntelberg F and Suadicani P (2014) Sleep duration and ischemic heart disease and all-cause mortality: prospective cohort study on effects of tranquilizers/hypnotics and perceived stress. Scandinavian Journal of Work and Environment health 39, 550–558. [DOI] [PubMed] [Google Scholar]
- Gottlieb DJ, Punjabi NM, Newman AB, Resnick HE, Redline S, Baldwin CM and Nieto FJ (2005) Association of sleep time with diabetes mellitus and impaired glucose tolerance. Archives of Internal Medicine 165, 863–867. [DOI] [PubMed] [Google Scholar]
- Gottlieb DJ, Redline S, Nieto FJ, Baldwin CM, Newman AB, Resnick HE and Punjabi NM (2006) Association of usual sleep duration with hypertension: the Sleep Heart Health Study. Sleep 29, 1009–1014. [DOI] [PubMed] [Google Scholar]
- Grandner MA and Drummond SPA (2007) Who are the long sleepers? Towards an understanding of the mortality relationship. Sleep Medicine Reviews 11, 341–360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grandner MA, Jackson N, Gerstner JR and Knutson KL (2014) Sleep symptoms associated with intake of specific dietary nutrients. Journal of Sleep Research 23, 22–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall MH, Smagula SF, Boudreau RM, Ayonayon HN, Goldman SE, Harris TB, Naydeck BL, Rubin SM, Samuelsson L, Satterfield S, Stone KL, Visser M and Newman AB (2015) Association between sleep duration and mortality is mediated by markers of inflammation and health in older adults: the health, aging and body composition study. Sleep 38, 189–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heslop P, Smith GD, Metcalfe C, Macleod J and Hart C (2002) Sleep duration and mortality: the effect of short or long sleep duration on cardiovascular and all-cause mortality in working men and women. Sleep Medicine 3, 305–314. [DOI] [PubMed] [Google Scholar]
- Hublin C, Partinen M, Koskenvuo M and Kaprio J (2007) Sleep and mortality: a population-based 22-year follow-up study. Sleep 30, 1245–1253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jung K, Song C, Ancoli-israel S and Barrett-connor E (2013) Gender differences in nighttime sleep and daytime napping as predictors of mortality in older adults: the Rancho Bernardo Study. Sleep Medicine 14, 12–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kakizaki M, Kuriyama S, Nakaya N, Sone T, Nagai M, Sugawara Y, Hozawa A, Fukudo S and Tsuji I (2013) Long sleep duration and cause-specific mortality according to physical function and self-rated health: the Ohsaki Cohort Study. Journal of sleep research 22, 209–216. [DOI] [PubMed] [Google Scholar]
- Kim Y, Wilkens LR, Schembre SM, Henderson BE, Kolonel LN and Goodman MT (2014) Insufficient and excessive amounts of sleep increase the risk of premature death from cardiovascular and other diseases: the Multiethnic Cohort Study. Preventive Medicine 57, 377–385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kojima M, Wakai K, Kawamura T, Tamakoshi A, Aoki R, Lin Y, Nakayama T, Horibe H, Aoki N and Ohno Y (2000) Sleep patterns and total mortality: a 12-year follow-up study in Japan. Journal of epidemiology / Japan Epidemiological Association 10, 87–93. [DOI] [PubMed] [Google Scholar]
- Kubota Y, Iso H, Ikehara S and Tamakoshi A (2015) Relationship between sleep duration and cause-specific mortality in diabetic men and women based on self-reports. Sleep and Biological Rhythms 13, 85–93. [Google Scholar]
- Kutner N, Zhang R, Johansen K and Bliwise D (2013) Associations among nocturnal sleep, daytime intradialytic sleep, and mortality risk in patients on daytime conventional hemodialysis: US Renal Data System special study data. Hemodialysis Internation 17, 223–229. [DOI] [PubMed] [Google Scholar]
- Lan T-Y, Lan T-H, Wen C-P, Lin Y-H and Chuang Y-L (2007) Nighttime sleep, Chinese afternoon nap, and mortality in the elderly. Sleep 30, 1105–1110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leng Y, Cappuccio FP, Wainwright NWJ, Surtees PG, Luben R, Brayne C and Khaw KT (2015) Sleep duration and risk of fatal and nonfatal stroke. A prospective study and meta-analysis. Neurology 84, 1072–1079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y, Sato Y and Yamaguchi N (2013) Potential biochemical pathways for the relationship between sleep duration and mortality. Elsevier B.V. Sleep Medicine 14, 98–104. [DOI] [PubMed] [Google Scholar]
- Lu Y, Tian N, Yin J, Shi Y and Huang Z (2013) Association between sleep duration and cancer risk: a meta-analysis of prospective cohort studies. PLoS ONE 8, e74723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magee CA, Holliday EG, Attia J, Kritharides L and Banks E (2013) Investigation of the relationship between sleep duration, all-cause mortality, and preexisting disease. Sleep Medicine 14, 591–596. [DOI] [PubMed] [Google Scholar]
- Manetto V, Medori R, Cortelli P, Montagna P, Tinuper P, Baruzzi A, Rancurel G, Hauw JJ, Vanderhaeghen JJ and Mailleux P (1992) Fatal familial insomnia: clinical and pathologic study of five new cases. Neurology 42, 312–319. [DOI] [PubMed] [Google Scholar]
- Martínez-Gómez D, Guallar-Castillón P, León-Muñoz LM, López-García E and Rodríguez-Altalejo F (2013) Combined impact of traditional and non-traditional health behaviors on mortality: a national prospective cohort study in Spanish older adults. BMC Medicine 11, 47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mallon L, Broman J and Hetta J (2002) Sleep complaints predict coronary artery disease mortality in males: a 12-year follow-up study of a middle-aged Swedish population. Journal of Internal Medicine 251, 207–216. [DOI] [PubMed] [Google Scholar]
- McMullan CJ, Curhan GC and Forman JP (2016) Association of short sleep duration and rapid decline in renal function. Kidney International 89, 1324–1330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mesas AE, López-García E, León-Muñoz LM, Guallar-Castillón P and Rodríguez-Artalejo F (2010) Sleep duration and mortality according to health status in older adults. Journal of the American Geriatrics Society 58, 1870–1877. [DOI] [PubMed] [Google Scholar]
- Pandi-Perumal SR, Verster JC, Kayumov L, Lowe AD, Santana MG, Pires MLN, Tufik S and Mello MT (2006) Sleep disorders, sleepiness and traffic safety: a public health menace. Brazilian Journal of Medical and Biological Research 39, 863–871. [DOI] [PubMed] [Google Scholar]
- Patel SR, Ayas NT, Malhotra MR, White DP, Schernhammer ES, Speizer FE, Stampfer MJ and Hu FB (2004) A prospective study of sleep duration and mortality risk in women. Sleep 27, 440–444. [DOI] [PubMed] [Google Scholar]
- Pollak CP, Perlick D, Linsner JP, Wenston J and Hsieh F (1990) Sleep problems in the community elderly as predictors of death and nursing home placement. Journal of Community Health 15, 123–135. [DOI] [PubMed] [Google Scholar]
- Rhee CW, Kim JY, Park BJ, Li ZM and Ahn Y (2012) Impact of individual and combined health behaviors on all causes of premature mortality among middle aged men in Korea: the Seoul Male Cohort Study. Journal of Preventive Medicine and Public Health 45, 14–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson KA (2002) Development of a highly sensitive search strategy for the retrieval of reports of controlled trials using PubMed. International Journal of Epidemiology 31, 150–153. [DOI] [PubMed] [Google Scholar]
- Rod NH, Kumari M, Lange T, Kivimäki M, Shipley M and Ferrie J (2014) The joint effect of sleep duration and disturbed sleep on cause-specific mortality: results from the Whitehall II cohort study. PLoS ONE 9, e91965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rumble R and Morgan K (1992) Hypnotics, sleep, and mortality in elderly people. Journal of the American Geriatrics Society 40, 787–791. [DOI] [PubMed] [Google Scholar]
- Ruigomez ANA, Alonso J and Anto JM (1995) Relationship of health behaviours to five-year mortality in an elderly cohort. Age and Ageing 24, 113–119. [DOI] [PubMed] [Google Scholar]
- Shan Z, Ma H, Xie M, Yan P, Guo Y, Bao W, Rong Y, Jackson CL, Hu FB and Liu L (2015) Sleep duration and risk of type 2 diabetes: a meta-analysis of prospective studies. Diabetes Care 38, 529–537. [DOI] [PubMed] [Google Scholar]
- Shen X, Wu Y and Zhang D (2016) Nighttime sleep duration, 24-hour sleep duration and risk of all-cause mortality among adults: a meta-analysis of prospective cohort studies. Nature Publishing Group Scientific Reports 6, 21480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snyder JM, Molk DM and Treuting PM (2013) Increased mortality in a colony of zebra finches exposed to continuous light. Journal of the American Association for Laboratory Animal Science: JAALAS 52, 301–307. [PMC free article] [PubMed] [Google Scholar]
- Sperry SD, Scully ID, Gramzow RH and Jorgensen RS (2015) Sleep duration and waist circumference in adults: a meta-analysis. Sleep 38, 1269–1276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stamatakis E, Rogers K, Ding D, Berrigan D, Chau J, Hamer M and Bauman A (2015) All-cause mortality effects of replacing sedentary time with physical activity and sleeping using an isotemporal substitution model: a prospective study of 201,129 mid-aged and older adults. The International Journal of Behavioral Nutrition and Physical Activity 12, 121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suzuki E, Yorifuji T, Ueshima K, Takao S, Sugiyama M and Ohta T (2009) Sleep duration, sleep quality and cardiovascular disease mortality among the elderly: a population-based cohort study. Preventive Medicine 49, 135–141. [DOI] [PubMed] [Google Scholar]
- Tamakoshi A and Ohno Y (2004) Self-reported sleep duration as a predictor of all-cause mortality: results from the JACC study, Japan. Sleep 27, 51–54. [PubMed] [Google Scholar]
- Tsubono Y, Fukao A and Hisamichi S (1993) Health practices and mortality in a rural Japanese population. Journal of Experimental Medicine 171, 339–348. [DOI] [PubMed] [Google Scholar]
- Vgontzas AN, Liao D, Pejovic S, Calhoun S, Karataraki M, Basta M, Fernández-mendoza J and Bixler EO (2010) Insomnia with short sleep duration and mortality: the Penn State cohort. Sleep 33, 1159–1164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang X, Liu X, Song Q and Wu S (2016) Sleep duration and risk of myocardial infarction and all-cause death in a Chinese population: the Kailuan study. Sleep Medicine 19, 13–16. [DOI] [PubMed] [Google Scholar]
- Wang Q, Xi B, Liu M, Zhang Y and Fu M (2012) Short sleep duration is associated with hypertension risk among adults: a systematic review and meta-analysis. Hypertension Research 35, 1012–1018. [DOI] [PubMed] [Google Scholar]
- Wingard DL (1982) The sex differential in mortality rates: demographic and behavioral factors. American Journal Epidemiology 115, 205–216. [DOI] [PubMed] [Google Scholar]
- Wingard DL, Berkman LF and Brand RJ (1982) A multivariate analysis of health-related practices: a nine-year mortality follow-up of The Alameda County. American Journal of Epidemiology 115, 205–216. [DOI] [PubMed] [Google Scholar]
- Wu Y, Zhai L and Zhang D (2014) Sleep duration and obesity among adults: a meta-analysis of prospective studies. Sleep Medicine 15, 1456–1462. [DOI] [PubMed] [Google Scholar]
- Xi B, He D, Zhang M, Xue J and Zhou D (2014) Short sleep duration predicts risk of metabolic syndrome: a systematic review and meta-analysis. Sleep Medicine Reviews 18, 293–297. [DOI] [PubMed] [Google Scholar]
- Xiao Q, Keadle SK, Hollenbeck AR and Matthews CE (2014) Sleep duration and total and cause-specific mortality in a large US cohort: interrelationships with physical activity, sedentary behavior, and body mass index. American Journal of Epidemiology 180, 997–1006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeo Y, Ma SH, Park SK, Chang S, Shin H, Kang D (2013) A prospective cohort study on the relationship of sleep duration with all-cause and disease-specific mortality in the Korean Multi-center Cancer Cohort Study. Journal of Preventive Medicine & Public Health 46, 271–281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Youngstedt SD and Kripke DF (2004) Long sleep and mortality: rationale for sleep restriction. Sleep Medicine Reviews 8, 159–174. [DOI] [PubMed] [Google Scholar]
- Zuurbier LA, Luik AI, Hofman A, Franco OH, Someren EJW Van and Tiemeier H (2014) Fragmentation and stability of circadian activity rhythms predict mortality: the Rotterdam study. American journal of Epidemiology, 1–10. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
For supplementary material accompanying this paper visit https://doi.org/10.1017/S2045796018000379.
click here to view supplementary material