Abstract
Aims.
The primary objective of this systematic review was to identify and synthesise analytic studies examining the association between exposure to parental psychopathology in childhood and the nature of subsequent suicide-related thoughts (SRT) and suicide-related behaviour (SRB) (severity of ideation, planned/unplanned attempts/lethality) and to describe the direction, and magnitude of associations. The secondary objective was to determine if the associations from the primary objective differ by the type(s) and timing of parental psychopathology, sex/gender of the parent and child and is mediated by child psychiatric symptoms and family functioning.
Methods.
A systematic review was conducted using guidelines from the PRISMA statement. MEDLINE, CINAHL, EMBASE, psycINFO, Web of Science and grey literature sources were searched by two reviewers to March, 2017. Studies were included if they examined any parental psychopathology (Diagnostic and Statistical Manual of Mental Disorders criteria or equivalent) or SRT or SRB and offspring SRT or SRB occurring from birth <25 years of age.
Results.
Out of 10 231 studies identified, 54 were included for review. Studies were clinically and methodologically heterogeneous with none at low risk of bias (ROB). Nine studies with moderate ROB indicated a significantly increased risk of offspring SRT, suicide attempts (SA) and suicide among those exposed to maternal SA and suicide in childhood or adolescence. In the remaining 45 studies with higher ROB this association persisted. Several studies (67%) did not confirm that the exposure occurred in the offspring's childhood or adolescence. Findings were suggestive of a mediating effect of offspring psychiatric symptoms, however, few studies examined mediation and effect modification of contextual variables.
Conclusions.
Offspring exposed to maternal SA are at an increased risk of these same behaviours early in life. Prospective attention to the types and timing of maternal and paternal psychopathology and the intermediate pathways to offspring SRT and SRB onset is needed and could have implications for informing modifiable targets for early intervention and prevention.
Key words: Adolescence, gender differences, mental health, suicide, systematic reviews
Introduction
Suicide is among the leading causes of death in young people, globally (World Health Organization, 2014). Three quarters of suicides are in males, while suicide attempts (SA) are higher in females (Rhodes et al. 2014). Suicide-related behaviour (SRB) tends to onset in youth (Fergusson et al. 2000; Bridge et al. 2006), therefore it is imperative to study younger populations prior to the high-risk period for these behaviours. While psychopathology is strongly associated with a SA and suicide (Cavanagh et al. 2003), the nature of this relationship is not well understood. Additionally, there is evidence that the association between childhood risk factors and risk of SA and suicide can be explained by offspring psychiatric symptoms (Fergusson et al. 2000; Wanner et al. 2012; Geoffroy et al. 2014).
There is convergent evidence that SRB clusters in families, independent of familial history of other psychopathology, suggesting a specific genetic susceptibility (Brent & Mann, 2005; Gureje et al. 2011). Still, authors report a significant role of early childhood risk factors in the development of suicide-related thoughts (SRT) and SRB independent of genetic risk (Statham et al. 1998; Brent & Mann, 2005). Family histories of suicide and psychopathology are associated with SRT and SRB in offspring (Brent & Mann, 2005; Gureje et al. 2011; Brent et al. 2015). These associations could be explained by: a specific genetic transmission of risk; exposure to parental psychopathology during childhood while children are neuro-developmentally vulnerable; or both. In turn, these early exposures shape early childhood risk factors.
Studies reporting associations between parental psychopathology and/or SRB with the risk of adolescent and adult offspring SRT and SRB (Evans et al. 2004; Fotti et al. 2006; Peter et al. 2008; Cox et al. 2012; Geoffroy et al. 2014; Soole et al. 2014) differ by populations studied, magnitude of associations and levels of statistical adjustment. Factors related to the timing and nature of parental exposures could, in part, explain these inconsistencies. Moreover, the risk profiles of individuals who exhibit SRT (with or without a plan) compared with SRB differ and there is evidence that parental psychopathology is differentially associated with SRT and SRB in adults (Gureje et al. 2011). Variation in family functioning may also modify or mediate these associations. There is no single agreed upon definition of family functioning, but common themes include a family's ability to cope with stress as a unit, and promote emotional and physical health within the family unit (Hawley & DeHaan, 1996). One meta-analysis synthesising 28 studies up until April, 2011 (Geulayov et al. 2012a) reported a significant association between parental suicide and offspring suicide, and between parental SRB and offspring SRB. Associations were stronger when the mother (v. father) had a history of SRB or died by suicide. This review did not examine SRT or the effects of other types of parental psychopathology alone or in combination with SRB such as parental mood or substance use disorder. While the review included adult offspring, it did not quantify the temporal sequence of the effects in relation to the age of the offspring. For example, it is unclear whether parental SRB was present before birth and persisting prior to offspring SRB or whether it first onset shortly before their SRB in adulthood or afterwards (misclassified exposure window).
The primary objective of this systematic review was to identify and synthesise analytic studies examining the association between exposure to parental psychopathology in childhood and the nature of subsequent SRT and SRB (severity of ideation, planned/unplanned attempts/lethality) and to describe the direction, and magnitude of associations. The secondary objective was to determine if the associations from the primary objective differ by the type(s) and timing of parental psychopathology, sex/gender of the parent and child and is mediated by child psychiatric symptoms and family functioning.
Methods
This systematic review was conducted using principles from the PRISMA statement (Moher et al. 2009). The following resources were searched: MEDLINE, CINAHL, EMBASE, psycINFO, Web of Science and grey and fugitive literature sources (e.g., Dissertations and Theses, Child Welfare Information Gateway, Google Scholar). A comprehensive search strategy made up of search terms reflecting the exposure and outcomes was conducted using a combination of title, abstract and major subject heading terms such as ‘parents’ and ‘mental illness’ or ‘psychopathology’ and ‘suicide’ or ‘self-injurious behaviour’ or ‘self-harm’ (online Supplementary (S) Text 1). The search was conducted in March, 2017. A prior protocol was externally peer reviewed for this review (online Supplementary S Text 2).
Inclusion criteria
Studies were included if they reported on any type of parental psychopathology (according to Diagnostic and Statistical Manual of Mental Disorders (DSM) criteria or equivalent) or SRT/SRB (exposure) and offspring SRT/SRB (outcome) occurring some time in childhood to early adulthood (>0–25 years). If studies included a wide age range including the time of interest (>0–25 years) and if the mean age of the sample was <25 years (or the range was collapsible into earlier age groups <25 years), the studies were included in the review. Any analytic study (excluding single case studies, case-series, qualitative studies and reviews) using a population from any Country was included. No restrictions were made by year of study or language.
Procedure
All abstracts of identified studies were screened by one screener (SG) and a 10% random sample of all identified studies by a second screener (JS). Inter-rater reliability for this selection was high (kappa >95%). Both screeners examined full texts of studies identified as potentially relevant and systematically abstracted data from included studies. When studies did not report a measure of association, efforts were made to calculate one using reported proportions and/or by contacting authors for additional information. Reference lists of included studies were reviewed for additional studies meeting criteria. It was anticipated that studies included in this review would be heterogeneous by several factors, and therefore the decision to not conduct a meta-analysis was made a priori.
Risk of bias (ROB) was systematically assessed by both screeners using criteria from the Cochrane Risk of Bias Assessment Tool: for Non-Randomised Studies of Interventions (ACROBAT-NRSI) (Sterne et al. 2014). Each study was assigned a summary rating using criteria from the GRADE assessment incorporating six domains of bias: confounding, selection, exposure measurement, outcome measurement, attrition and reporting. A study met criteria for low ROB if all domains were judged to be low ROB; moderate ROB included studies that were judged to have no serious/critical ROB domains; serious ROB included studies that were judged to meet criteria for serious ROB in at least one domain; and critical ROB included studies judged to have at least one critical ROB domain. Studies were not excluded from this review based on a ROB rating, but were discussed in the context of the specific bias. Qualitative syntheses of findings are presented in forest plots that were created in Microsoft Excel.
Definitions
In this paper, SRT are defined as follows: any thoughts/ideas pertaining to ending one's life, suicide threats and plans SA are defined as any self-inflicted, potentially injurious behaviour with some intent to end one's life. Measures that were irrespective of suicidal intent were labelled as SRB (Silverman et al. 2007). Exposure measures were defined as parental psychopathology: defined as any DSM Axis one and two disorders and SRT/SRB. An estimate refers to a specific association between one exposure and outcome. As several studies reported more than one exposure or outcome, estimates outnumber studies, with some studies presented more than once in figures.
Results
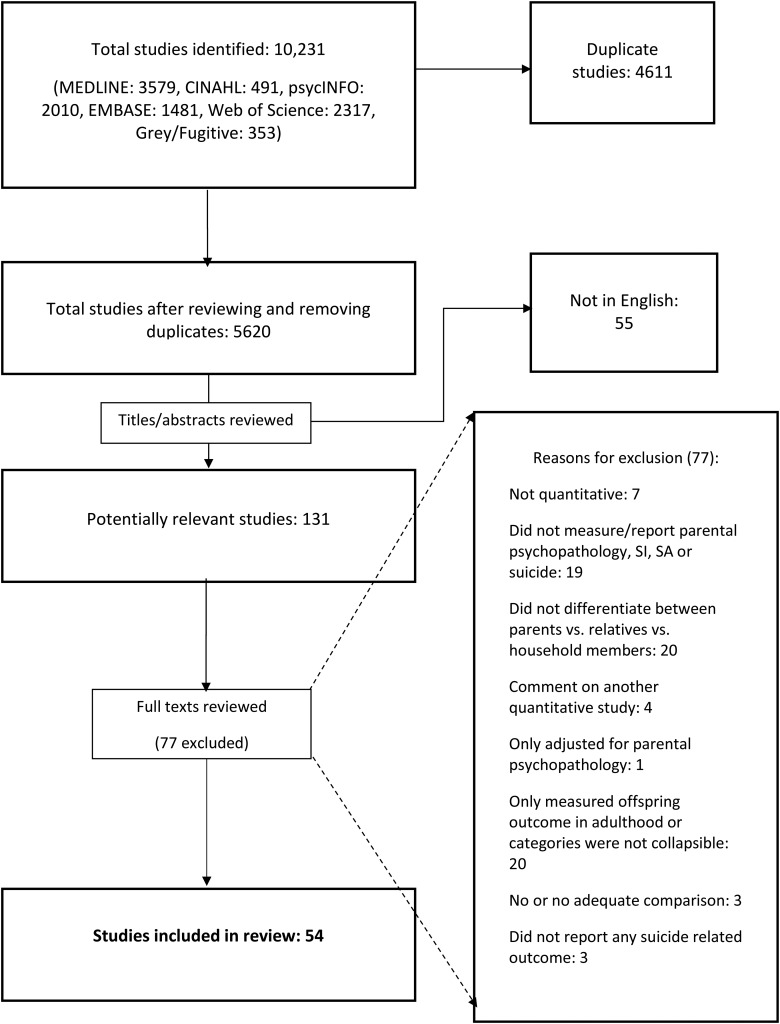
A total of 10 231 studies were identified from all combined data sources and after reviewing and removing duplicate studies (4611), the total was reduced to 5620 studies. In total 55 studies were excluded as they did not include an English abstract. A total of 131 studies were identified as potentially relevant and 54 of these studies met inclusion criteria (Fig. 1). Seventeen studies (32%) did not report a measure of association, and a measure of association could not be calculated. These studies are not in the primary synthesis but are discussed in text where appropriate. Study publication dates of eligible studies ranged from August, 1986 to March, 2017.
Fig. 1.
Flow chart of included studies and reasons for exclusion.
Characteristics of eligible studies (online Table S1)
Twenty-four studies (44%) were cohort studies, 19 were cross-sectional (35%) and 11 were some form of case-control study (20%). Most were conducted in, and included samples from the USA (n = 26, 48%) or Europe (n = 18, 33%). Fourteen studies (26%) included age ranges with the upper limit >25 years, but with a mean age <25 years. All studies reporting adjusted results (n = 33, 61%) accounted for at least age and sex/gender. In 26 of these studies that presented adjusted estimates (84%), some indicator of socio-economic status (SES) in one or both parents was reported. In the following sections, eligible studies are examined by ROB according to the overall associations, exposure and outcome specificity, and effect modifying and mediating variables.
Risk of bias
Eleven studies (20%) met criteria for moderate ROB, no studies were low ROB and all other studies were serious (n = 36) or critical (n = 7) ROB (online Table S2). The most common potential bias among the included studies was recall bias leading to potential differential misclassification of the exposure. Most studies (n = 47, 87%) measured exposure to parental psychopathology retrospectively, often using one time clinical interviews to identify either lifetime DSM diagnoses, or self-reported past SRB and 69% (n = 37) did not confirm if the exposure to parental psychopathology occurred in the offspring's childhood or adolescence.
Main findings among lowest ROB studies
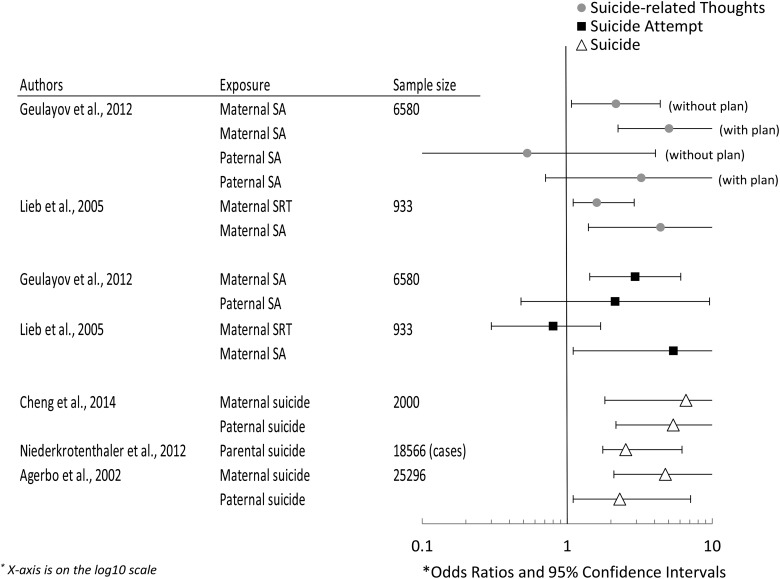
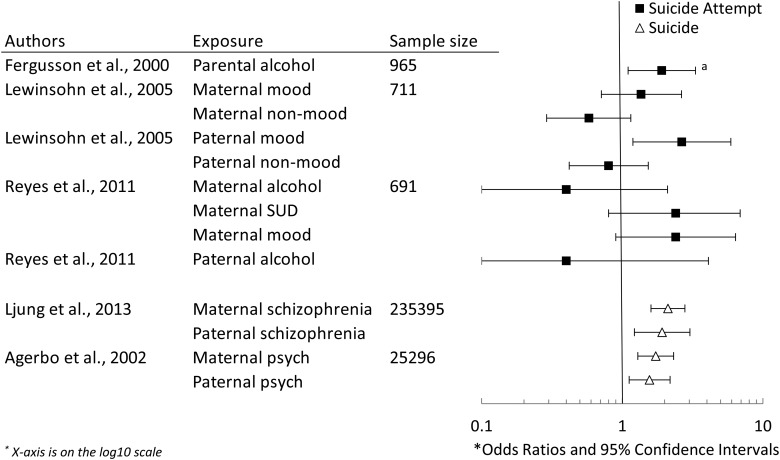
Figures 2 and 3 presents ORs and 95% CIs of associations among studies that met criteria for moderate ROB and reported adjusted measures of association. This consisted of nine studies as one of the moderate ROB studies (Klimes-Dougan et al. 1999) did not report an adjusted measure of association and another (Hammerton et al. 2015, 2016) did not report an OR (or a comparable estimate). All studies reported that exposure to maternal SA was significantly associated with offspring SRT and SA. The only estimates that were not significant were when the SA were in the father, or when the parental exposure was SRT. Three studies (Fergusson et al. 2000; Lewinsohn et al. 2005; Reyes et al. 2011) examined different types of psychopathology (e.g., mood disorders or SUD) and their association with offspring SA and reported mixed findings (Fig. 3). Irrespective of exposure type, all studies reporting on offspring suicide reported significant and positive associations that were high in magnitude (Figs 2 and 3).
Fig. 2.
Adjusted associations between parental suicide attempts and suicide and offspring suicide-related thoughts, suicide attempts and suicide among moderate risk of bias studies. SA, suicide attempt; SRT, suicide-related thoughts.
Fig. 3.
Adjusted associations between parental psychopathology and offspring suicide attempt and suicide among moderate risk of bias studies. Alcohol: alcohol use disorders; Mood, mood disorders; Non-mood psych, any non-mood psychopathology; Psych; any psychopathology; SUD, substance use disorders. aHazard ratio.
All studies included in Figs 2 and 3, established temporality between exposure and outcome and confirmed that the exposure was present during childhood or adolescence. The studies reporting offspring SRT and SA as an outcome (n = 5) were prospective cohort studies and adjusted for several socio-demographic variables. Regarding offspring suicide, studies in Figs 2 and 3 were case-control studies using mortality registries and adjusted for several socio-demographic variables (Agerbo et al. 2002; Niederkrotenthaler et al. 2012; Ljung et al. 2013; Cheng et al. 2014).
Studies reporting adjusted measures of association between parental psychopathology and offspring SRT, SA and suicide, irrespective of ROB are in online Figs S1–S3; studies measuring offspring SRB (irrespective of intent) are in online Fig. S4. The pattern of findings was similar among all eligible studies, irrespective of ROB.
Specificity of parental psychopathology
Across all studies, irrespective of ROB, parental and maternal (but not paternal) SA and suicide were significantly associated with offspring SRT, SA, SRB and suicide. However, the association between mood disorders and SUD and offspring outcomes varied greatly. In particular, about 80% of all adjusted measures of association between parental mood disorders and offspring SRT and SA were significant with evidence of an increased risk (online Table S3). High-risk offspring studies where the parental mood disorder was measured using gold standard interviews with clinicians (Weissman et al. 1986; Klimes-Dougan et al. 1999), reported that adolescent offspring of mothers with major depressive disorder (MDD) or bipolar disorder reported significantly more SRT and SA compared with offspring of well mothers. Fifty-five per cent of studies examining the association between parental alcohol or SUD with offspring SRT or SA were significant and positive (online Table S3). Only one study examined the frequency of exposure to parental AUD (Rossow & Moan, 2012) and reported a significant dose response relationship between increasing frequency of exposure to parental intoxication and increasing risk of SA in offspring. However, in this study, the exposure was self-reported by offspring.
Specificity of offspring outcome
Among the moderate ROB studies, only two studies examined SRT as an outcome (Lieb et al. 2005; Geulayov et al. 2012b) both reporting significant and positive associations between maternal (but not paternal) SA and offspring SRT, and the effect estimates were stronger when SRT included a plan. One other cross-sectional study of high ROB (Glowinski & Heath, 2001) reported a significant and positive association between maternal mood disorder, AUD and SA and offspring SRT with a plan, while, the same associations were not significant when the outcome was SRT without a plan (online Fig. S2). Specificity of offspring SA, such as lethality of attempt or method was not reported by included studies. Almost all studies examining offspring SRB (Mittendorfer-Rutz et al. 2008; Kuramoto et al. 2010; Jakobsen & Christiansen, 2011; Christiansen & Larsen, 2012; Niederkrotenthaler et al. 2012) reported significant and positive associations with all forms of parental psychopathology (90% of estimates) (online Fig. S4; Table S3). All studies examining offspring suicide as an outcome (and reported an adjusted measure of association) (Agerbo et al. 2002; Niederkrotenthaler et al. 2012; Ljung et al. 2013; Cheng et al. 2014) were moderate ROB and reported significant and positive associations with parental psychopathology (irrespective of type) (Figs 2 and 3).
Timing of exposure to parental psychopathology
Seventeen studies (33%) confirmed that offspring were exposed to parental psychopathology sometime during childhood or adolescence (including studies measuring SRB). Most of these studies did not specifically quantify the timing of exposure and most measured the exposure retrospectively; for example, only seven (Klimes-Dougan et al. 1999, 2008; Fergusson et al. 2000; Kerr et al. 2008; Geulayov et al. 2012b; Niederkrotenthaler et al. 2012; Hammerton et al. 2015) parental exposures studies were based on prospective assessment. Among the moderate ROB studies: Geulayov et al. (2012b) reported a significant and positive association between prospectively measured maternal SA (but not paternal SA) occurring before age 11 years and offspring SRT and SA at age 16/17 years. Fergusson et al. (2000) reported that parental AUD during their child's first 15 years of life was significantly associated with offspring SA before the age of 21 years.
Two studies examined effect modification by timing of exposure in childhood: Niederkrotenthaler et al. (2012) (moderate ROB) reported a significant trend (p < 0.001), where parental psychiatric inpatient stay earlier in offspring childhood (birth to 3 years) was more strongly associated with offspring suicide compared with exposure later in childhood (3–10 and over 10 years); Rossow & Moan (2012) reported a significant interaction between offspring age and parental intoxication predicting SRT but not SA. The risk of SRT was higher in Junior High students compared with high-school students (Table 1). However, this study was cross-sectional and the exposure was self-reported by the offspring.
Table 1.
Effect modification and interaction of timing of exposure
| Authors | Exposure | Outcome | EM/INT | Result |
|---|---|---|---|---|
| Friedman et al. (1984) | Parental psychiatric disorder (primarily MDD and alcohol) | SA | EM: Exposed before and after 14 years | 50% of offspring with SA had mothers with a chronic psychiatric illness before age 14 years v. 5% of offspring without SA (Fishers exact test p < 0.01) |
| Niederkrotenthaler et al. (2012) | Parental psychiatric inpatient care | SRB/suicide | EM: Exposure age categories: <3 years, 3–10 years, >10 years | Predicting offspring SRB (p-trend < 0.001) <3 years (OR 2.6, 95% CI 2.5–2.8) 3–10 years (OR 2.3, 95% CI 2.2–2.5) >10 years (OR 2.2, 95% CI 2.0–2.3) Predicting offspring suicide (p-trend = 0.027) <3 years (OR 2.5, 95% CI 2.0–3.1) 3–10 years (OR 1.9, 95% CI 1.5–2.4) >10 years (OR 2.1, 95% CI 1.8–2.6) |
| Rossow & Moan (2012) | Parent alcohol | SRT/SA | Interaction: offspring age × parental intoxication EM: Jr. High v. high-school |
Significant interaction for offspring SRT (p < 0.05) Non-significant interaction for offspring SA (NR) Offspring SRT: Jr. High (OR 6.3, 95% CI 3.9–10.1) High-school (OR 2.6, 95% CI 1.4–4.8) |
Alcohol, alcohol use/dependence; CI, confidence interval; EM, effect modifier; HR, hazard ratio; INT, interaction; MDD, major depressive disorder; NR, not reported; OR, odds ratio; psych: SA, suicide attempt; SRB, suicide-related behaviour; SRT, suicide-related thoughts.
Effect of parental and offspring sex/gender
Within studies that looked at maternal and paternal exposures separately (irrespective of ROB), about half (14/27) demonstrated that maternal psychopathology was significantly associated with an increased risk of SRT, SA and suicide (online Fig. S2) and about a third (8/24) reported that paternal psychopathology was significantly associated with an increased risk of SRT, SA and suicide (online Fig. S3). 7/9 studies reported either stronger estimates, or the estimates were significant compared with not significant when the exposure was in the mother compared with the father. All studies that tested for interaction or effect modification of parental sex reported evidence of stronger associations when the exposure was in the mother compared with the father (Lewinsohn et al. 2005; King et al. 2010; Kuramoto et al. 2010) (Table 2).
Table 2.
Effect modification and interaction of offspring/parental sex
| Authors | Exposure | Outcome | EM/INT | Result |
|---|---|---|---|---|
| Tsypes & Gibb (2015) | Maternal MDD | SRT | Interaction: offspring sex × maternal MDD | Significant interaction: OR 5.99, p < 0.01 Girls (OR 5.18, p < 0.01) Boys (OR 0.89, p = 0.78) |
| Geulayov et al. (2012b) | Maternal SA | SRT/SA | Interaction: offspring sex × maternal SA | Non-significant interactions predicting offspring SA: p = 0.69 or SRT: p = 0.74 |
| Lieb et al. (2005) | Maternal SRT/SA | SRT/SA | Interaction: offspring sex × maternal SRT and SA | Non-significant interactions p > 0.05 |
| Kuramoto et al. (2010) | Maternal/paternal suicide compared to death from accidents | SA | Interaction: parent sex × parent suicide | Significant interaction: p = 0.05 Maternal suicide (HR 1.8, 95% CI 1.2–2.7) Paternal suicide (HR 1.1, 95% CI 0.96–1.3) |
| King et al. (2010) | History of mental health problems | SA | EM: parent sex | Both parents: (OR 2.6, 95% CI 1.25–5.5) Mother only: (OR 2.4, 95% CI 1.2–4.6) Fathers only (OR 1.6, 95% CI 0.67–3.8) |
| Lewinsohn et al. (2005) | Maternal/paternal MDD | SA | Interaction: parental sex × MDD | Parental sex × MDD: p > 0.05 |
CI, confidence interval; EM, effect modifier; HR, hazard ratio; INT, interaction; MDD, major depressive disorder; NR, not reported; OR, odds ratio; psych: any psychopathology; SA, suicide attempt; SRT, suicide-related thoughts.
Few studies stratified by offspring sex/gender and among these studies, the findings were heterogeneous. One study (Tsypes & Gibb, 2015) reported a significant unadjusted difference in SA risk in girls but not boys (8–14 years), while other studies of samples of adolescents (Geulayov et al. 2012b; Isohookana et al. 2013) or young adults (Lieb et al. 2005) (moderate ROB study) reported no difference in male/female estimates. Three studies tested for interaction or effect modification of offspring sex (Lieb et al. 2005; Geulayov et al. 2012b; Tsypes & Gibb, 2015) and reported mixed findings (Table 2).
Effect of offspring psychiatric symptoms and family functioning
Four studies (Fergusson et al. 2000; Kerr et al. 2008; Rossow & Moan, 2012; Hammerton et al. 2015), two of which met criteria for moderate ROB (Fergusson et al. 2000; Hammerton et al. 2015), reported the attenuation of effect estimates after adjusting for offspring psychiatric symptoms. All provided some evidence that child psychiatric symptoms partially mediate the association between parental SA, MDD and SUD and offspring's risk of SRT and SA in adolescence and young adulthood. Two studies found that family functioning partially mediated the association between maternal MDD and offspring SRT/SA (Garber et al. 1998; Hammerton et al. 2016) and another reported significant interaction and effect modification of family intactness. The odds of exposed (parental psychopathology) offspring SRB were higher among those living with parents who were unmarried, divorced, widowed, or non-cohabitating compared with those living with married and cohabitating parents (Niederkrotenthaler et al. 2012). None of the studies testing for mediating effects accounted for exposure – mediator, mediator – outcome confounding (Table 3).
Table 3.
Mediating effect of offspring psychiatric symptoms and family functioning
| Authors | Exposure | Outcome | Mediator | Results |
|---|---|---|---|---|
| Fergusson et al. (2000) | Parental SA | Parental SA | Offspring life stress/mental health | Adjusting for life stress/mental health attenuated the association between parent alcohol/substance to non-significance (NR) |
| Kerr et al. (2008) | Parental depression and SUD when boys were 9–11 years | SRT | Offspring depressive symptoms (11–29 years) | HRs were attenuated slightly after adjusting for offspring depressive symptoms: Parent depression HR changed from 1.18 to 1.13 Parent SUD HR changed from 1.23 to 1.18 |
| Rossow & Moan (2012) | Parental alcohol | SRT/SA | Offspring past year intoxication | Offspring intoxication significantly mediated the association between parent alcohol and offspring SRT and SA (sobel test z-values ranging from 5.8 to 8.2) |
| Hammerton et al. (2015) | Chronic severe maternal MDD | SRT | Offspring psychopathology | Adjusted indirect effects: MDD (0.07, 95% CI 0.04–0.11, p < 0.001) GAD (0.04, 95% CI 0.01–0.07, p = 0.002) DBD (0.08, 95% CI 0.04–0.12, p < 0.002) ADHD (−0.01, 95% CI −0.04–0.03, p = 0.74) Alcohol (0.01, 95% CI −0.00–0.02, p = 0.16) |
| Niederkrotenthaler et al. (2012) | Parental SRB/Psychiatric inpatient care | SRB | Interaction: Intact family × (parent SRB, inpatient care) EM: Intact v. non-intact familiesa |
Parental SRB × marital status: p < 0.001 Parental inpatient care × marital status: p = 0.002 Exposed to parental SRB: offspring SRB among intact families: (OR 1.87, 95% CI 1.6–2.2) non-intact families (OR 2.51, 95% CI 2.1–3.0) Exposed to parental inpatient care: offspring SRB among intact families: (OR 2.2, 95% CI 2.1–2.4) non-intact families (OR 3.2, 95% CI 3.0–3.3) |
| Hammerton et al. (2016) | Chronic severe maternal MDD | SRT | Parent-child relationship | Adjusted indirect effects: 0.04(95% CI 0.02–0.07, p < 0.05) |
| Garber et al. (1998) | Maternal MDD | SRT/SA | Mediator: family functioning | t = changed to 1.07, p > 0.05 from 2.19, p < 0.05 after including family functioning score into model with maternal MDD predicting offspring SRT/SA |
ADHD, attention deficit hyperactivity disorder; Alcohol: alcohol use/dependence; CI, confidence interval; DBD, disruptive behaviour disorder; GAD, generalised anxiety disorder; NR: not reported; HR: hazard ratio; MDD, major depressive disorder; OR, odds ratio; psych: psychiatric; SA, suicide attempt; SRT, suicide-related thoughts; SUD, substance use disorder.
Intact families: married, cohabitating compared with unmarried, divorced, widowed and non-cohabitating.
Discussion
Studies examining the association between parental psychopathology and offspring SRT and SRB indicate that children, adolescents and young adults exposed to a mother who attempted suicide and died by suicide early in life are at an increased risk of thinking about suicide, attempting suicide and dying by suicide themselves. When the father was reported to exhibit the SRB, the risk of SA and suicide in offspring was less conclusive. These findings were confirmed after excluding higher ROB studies. All studies examining the association between exposure to any type of parental psychopathology and offspring suicide were significant with large magnitude. These results are consistent with a previous systematic review (Geulayov et al. 2012a) and further suggest that among studies with established temporality, and confirming that the exposure occurred during childhood or adolescence, that exposure to parental SA and suicide significantly increase risk of these same behaviours in offspring before the age of 25. Further, these parental exposures are additionally associated with offspring SRT (particularly with a plan).
Few studies examined specific types of parental psychopathology alone, or in combination with SRB and among the few conducted, the findings were heterogeneous. Parental psychopathology may be associated with offspring SRT or SRB depending on the type and quantity of exposure. Lifetime DSM diagnoses are highly heterogeneous, and depending on the nature and frequency of exposure, the risk imposed by these exposures may vary. For example, there is a greater SA risk among offspring with parents with chronic, non-remitting mood disorders with persistent exposure over childhood compared with parents with a less chronic, remitting illness (Friedman et al. 1984).
While it is established that SRB has a genetic component (Brent & Mann, 2005; Gureje et al. 2011), the environmental effect of growing up with a parent with psychopathology is highly understudied, despite it being a potentially modifiable target for early intervention. Thirty-three percent of studies included in this review confirmed that the exposure occurred sometime during childhood to young adulthood. Most studies did not measure any other details about the nature and timing of the parent's illness and very few adjusted for family history for psychopathology making the disentangling of genetic risk v. early exposure challenging. Only one study (Niederkrotenthaler et al. 2012) broke down exposure into potentially developmentally sensitive time periods reporting that exposure to parental psychiatric admission was more strongly associated with offspring suicide if exposed from birth to three years of age supporting the hypothesis that exposure to parental psychopathology early in childhood when children are undergoing rapid neuro-developmental change increases risk of suicide.
Findings were suggestive of a mediating effect of child and adolescent psychiatric symptoms on the association between parental psychopathology and offspring SA, however, only four studies tested this and the methodological approach was limited by lack of adjustment for confounding. Most studies examined offspring psychiatric symptoms as a potential confounder, which is inappropriate if this variable is in fact on the causal pathway, and this may help to explain some of the non-significant findings.
Methodological considerations
Approximately 80% of included studies were serious or critical ROB, emphasising the need for more rigorous research in this area. Studies that measured the exposure through offspring self-report are subject to differential recall biases related to the psychiatric status of the offspring when reporting, for example, if the offspring are acutely unwell when reporting. Cross-sectional studies cannot disentangle whether the exposure occurred before the outcome. Using a lifetime diagnosis as an exposure variable can be problematic as this can reflect very different exposure histories. For example, a lifetime diagnosis of a mood disorder could reflect the following two cases: (1) a mother who had one single lifetime episode of MDD in adolescence, and stayed in complete remission for the remainder of her life including during her offspring's childhood, and (2) a mother with bipolar disorder with a chronic, non-remitting illness, present during her child's early life. Outcomes in children coming from these two different exposure histories would plausibly look very different. Finally, the use of ICD codes to measure SRB can be advantageous, as in some countries offspring and parent data can be linked, making the measurement of timing of exposure feasible. However, limitations surrounding the lack of confirmed suicide intent, inability to measure SRT and the selection bias imposed by excluding individuals who were not admitted to the hospital are problematic.
Future research should focus on prospective cohort designs using validated self-report measures or semi-structured interviews in both parents and offspring. Careful measurement of timing of exposure and outcome from childhood to late adolescence is crucial to understand risk trajectories and onset times. More consideration of subgroups of offspring SRT/SA is needed as there may be differential effects by increasing severity of SRT and SA. Finally, there may be variation in SRT, SA and suicide by sex/gender of offspring and parent. Large sample sizes are needed to be able to effectively stratify by sex of offspring to determine sex-specific trajectories of risk.
Limitations
Several other factors might potentially modify the relationship between parental psychopathology and offspring SRT, SA or suicide, but were outside the scope of this review. For, example, low SES families with a parent with psychopathology may lack resources to seek treatment, have lower social support, or have differential access to care compared to offspring from high SES families, which could in turn increase exposure to acute illness in the parents. Moreover, ethnicity, religion and individual level variables such as temperament and coping may act as effect modifiers in the development of SRT and onset of SA and require future investigation.
Implications
It is important to clarify that this research does not elude that parents with psychopathology or those expressing SRB display poor parenting practices. The main goal of this research is to identify families at excess risk and pathways through which exposure to parental illness may impact offspring risk to inform early interventions in the form of increased support and awareness. A prior SA and presenting to the hospital for self-inflicted injuries and poisonings substantially increases the risk of youth suicide (Hawton & Harriss, 2007). Knowledge of antecedent risk factors before the progression of SRB is essential in reaching those at risk. High-risk families where a parent is affected with major psychopathology and/or has expressed SRB are potential target groups for intervention and the level of functioning within families and psychiatric problems in children and adolescents could serve to inform interventions for these target groups.
Financial Support
This research was supported by an Ontario Graduate Scholarship.
Conflicts of Interest
None.
Availability of Data and Materials
As unpublished data were provided by individual authors of included studies in this review, data will not be shared. Queries are welcome by contacting the corresponding author.
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/S2045796017000397.
click here to view supplementary material
References
- Agerbo E, Nordentoft M, Mortensen PB (2002). Familial, psychiatric, and socioeconomic risk factors for suicide in young people: nested case-control study. British Medical Journal 325, 74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brent DA, Mann JJ (2005). Family genetic studies, suicide, and suicidal behavior. American Journal of Medical Genetics Part C: Seminars in Medical Genetics 133C, 13–24. [DOI] [PubMed] [Google Scholar]
- Brent DA, Melhem NM, Oquendo M, Burke A, Birmaher B, Stanley B, Biernesser C, Keilp J, Kolko D, Ellis S, Porta G, Zelazny J, Iyengar S, Mann J (2015). Familial pathways to early-onset suicide attempt: a 5.6-year prospective study. Journal of the American Medical Association Psychiatry 72, 160–168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bridge JA, Goldstein TR, Brent DA (2006). Adolescent suicide and suicidal behavior. Journal of Child Psychology and Psychiatry 47, 372–394. [DOI] [PubMed] [Google Scholar]
- Cavanagh JT, Carson AJ, Sharpe M, Lawrie SM (2003). Psychological autopsy studies of suicide: a systematic review. Psychological Medicine 33, 395–405. [DOI] [PubMed] [Google Scholar]
- Cheng CC, Yen WJ, Chang WT, Wu KC, Ko MC, Li CY (2014). Risk of adolescent offspring's completed suicide increases with prior history of their same-sex parents’ death by suicide. Psychological Medicine 44, 1845–1854. [DOI] [PubMed] [Google Scholar]
- Christiansen E, Larsen KJ (2012). Young people's risk of suicide attempts after contact with a psychiatric department – a nested case-control design using Danish register data. Journal of Child Psychology and Psychiatry 53, 16–25. [DOI] [PubMed] [Google Scholar]
- Cox LJ, Stanley BH, Melhem NM, Oquendo MA, Birmaher B, Burke A, Kolko DJ, Zelazny JM, Mann JJ, Porta G, Brent DA (2012). Familial and individual correlates of nonsuicidal self-injury in the offspring of mood-disordered parents. Journal of Clinical Psychiatry 73, 813–820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans E, Hawton K, Rodham K (2004). Factors associated with suicidal phenomena in adolescents: a systematic review of population-based studies. Clinical Psychological Review 24, 957–979. [DOI] [PubMed] [Google Scholar]
- Fergusson DM, Woodward LJ, Horwood LJ (2000). Risk factors and life processes associated with the onset of suicidal behaviour during adolescence and early adulthood. Psychological Medicine 30, 23–39. [DOI] [PubMed] [Google Scholar]
- Fotti SA, Katz LY, Afifi TO, Cox BJ (2006). The associations between peer and parental relationships and suicidal behaviours in early adolescents. Canadian Journal of Psychiatry 51, 698–703. [DOI] [PubMed] [Google Scholar]
- Friedman RC, Corn R, Hurt SW, Fibel B, Schulick J, Swirsky S (1984). Family history of illness in the seriously suicidal adolescent – A life cycle approach. American Journal of Orthopsychiatry 54, 390–397. [DOI] [PubMed] [Google Scholar]
- Garber J, Little S, Hilsman R, Weaver KR (1998). Family predictors of suicidal symptoms in young adolescents. Journal of Adolescence 21, 445–457. [DOI] [PubMed] [Google Scholar]
- Geoffroy MC, Gunnell D, Power C (2014). Prenatal and childhood antecedents of suicide: 50-year follow-up of the 1958 British Birth Cohort study. Psychological Medicine 44, 1245–1256. [DOI] [PubMed] [Google Scholar]
- Geulayov G, Gunnell D, Holmen TL, Metcalfe C (2012a). The association of parental fatal and non-fatal suicidal behaviour with offspring suicidal behaviour and depression: a systematic review and meta-analysis. Psychological Medicine 42, 1567–1580. [DOI] [PubMed] [Google Scholar]
- Geulayov G, Metcalfe C, Gunnell DJ (2012b). Parental suicide attempt and offspring self-harm and suicidal thoughts: results from the alspac birth cohort. Journal of Epidemiological Community Health 66, A25–A25. [Google Scholar]
- Glowinski AL, Heath AC (2001). Parental alcohol dependence and suicidal behavior in adolescent female twins. Behavior Genetics 31, 454–454. [Google Scholar]
- Gureje O, Oladeji B, Hwang I, Chiu WT, Kessler RC, Sampson NA, Alonso J, Andrade LH, Beautrais A, Borges G, Bromet E, Bruffaerts R, de Girolamo G, de Graaf R, Gal G, He Y, Hu C, Iwata N, Karam EG, Kovess-Masféty V, Matschinger H, Moldovan MV, Posada-Villa J, Sagar R, Scocco P, Seedat S, Tomov T, Nock MK (2011). Parental psychopathology and the risk of suicidal behavior in their offspring: results from the World Mental Health surveys. Molecular Psychiatry 16, 1221–1233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammerton G, Zammit S, Mahedy L, Pearson RM, Sellers R, Thapar A, Collishaw S (2015). Pathways to suicide-related behavior in offspring of mothers with depression: the role of offspring psychopathology. Journal of the American Academy of Child Adolescent Psychiatry 54, 385–393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammerton G, Zammit S, Thapar A, Collishaw S (2016). Explaining risk for suicidal ideation in adolescent offspring of mothers with depression. Psychological Medicine 46, 265–275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawley DR, DeHaan L (1996). Toward a definition of family resilience: integrating life-span and family perspectives. Family Process 35, 283–298. [DOI] [PubMed] [Google Scholar]
- Hawton K, Harriss L (2007). Deliberate self-harm in young people: characteristics and subsequent mortality in a 20-year cohort of patients presenting to hospital. Journal of Clinical Psychiatry 68, 1574–1583. [PubMed] [Google Scholar]
- Isohookana R, Riala K, Hakko H, Rasanen P (2013). Adverse childhood experiences and suicidal behavior of adolescent psychiatric inpatients. European Child Adolescent Psychiatry 22, 13–22. [DOI] [PubMed] [Google Scholar]
- Jakobsen IS, Christiansen E (2011). Young people's risk of suicide attempts in relation to parental death: a population-based register study. Journal of Child Psychology and Psychiatry 52, 176–183. [DOI] [PubMed] [Google Scholar]
- Kerr DC, Owen LD, Capaldi DM (2008). Suicidal ideation and its recurrence in boys and men from early adolescence to early adulthood: an event history analysis. Journal of Abnormal Psychology 117, 625–636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King CA, Kerr DC, Passarelli MN, Foster CE, Merchant CR (2010). One-year follow-up of suicidal adolescents: parental history of mental health problems and time to post-hospitalization attempt. Journal of Youth Adolescence 39, 219–232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klimes-Dougan B, Free K, Ronsaville D, Stilwell J, Welsh CJ, Radke-Yarrow M (1999). Suicidal ideation and attempts: a longitudinal investigation of children of depressed and well mothers. Journal of the American Academy of Child and Adolescent Psychiatry 38, 651–659. [DOI] [PubMed] [Google Scholar]
- Klimes-Dougan B, Lee CY, Ronsaville D, Martinez P (2008). Suicidal risk in young adult offspring of mothers with bipolar or major depressive disorder: a longitudinal family risk study. Journal of Clinical Psychology 64, 531–540. [DOI] [PubMed] [Google Scholar]
- Kuramoto SJ, Stuart EA, Runeson B, Lichtenstein P, Långström N, Wilcox HC (2010). Maternal or paternal suicide and offspring's psychiatric and suicide-attempt hospitalization risk. Pediatrics 126, e1026–e1032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewinsohn PM, Olino TM, Klein DN (2005). Psychosocial impairment in offspring of depressed parents. Psychological Medicine 35, 1493–1503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lieb R, Bronisch T, Höfler M, Schreier A, Wittchen H-U (2005). Maternal suicidality and risk of suicidality in offspring: findings from a community study. American Journal of Psychiatry 162, 1665–1671. [DOI] [PubMed] [Google Scholar]
- Ljung T, Lichtenstein P, Sandin S, D'Onofrio B, Runeson B, Långström N, Larsson H (2013). Parental schizophrenia and increased offspring suicide risk: exploring the causal hypothesis using cousin comparisons. Psychological Medicine 43, 581–590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mittendorfer-Rutz E, Rasmussen F, Wasserman D (2008). Familial clustering of suicidal behaviour and psychopathology in young suicide attempters. Social Psychiatry and Psychiatric Epidemiology 43, 28–36. [DOI] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG, Group P (2009). Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. British Medical Journal 339, b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niederkrotenthaler T, Floderus B, Alexanderson K, Rasmussen F, Mittendorfer-Rutz E (2012). Exposure to parental mortality and markers of morbidity, and the risks of attempted and completed suicide in offspring: an analysis of sensitive life periods. Journal of Epidemiology and Community Health 66, 233–239. [DOI] [PubMed] [Google Scholar]
- Peter T, Roberts LW, Buzdugan R (2008). Suicidal ideation among Canadian youth: a multivariate analysis. Archives of Suicide Research 12, 263–275. [DOI] [PubMed] [Google Scholar]
- Reyes JC, Robles RR, Colón HM, Negrón JL, Matos TD, Calderón JM (2011). Polydrug use and attempted suicide among Hispanic adolescents in Puerto Rico. Archives of Suicide Research 15, 151–159. [DOI] [PubMed] [Google Scholar]
- Rhodes A, Boyle MH, Bridge JA, Sinyor M, Links PS, Tonmyr L, Skinner R, Bethell J, Carlisle C, Goodday S, Salway Hottes T, Newton A, Bennett K, Sundar P, Cheung AH, Szatmari P (2014). Antecedents and sex/gender differences in youth suicidal behavior. World Journal of Psychiatry 4, 120–132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rossow I, Moan I (2012). Parental intoxication and adolescent suicidal behavior. Archives of Suicide Research 16, 73–84. [DOI] [PubMed] [Google Scholar]
- Silverman MM, Berman AL, Sanddal ND, O'Carroll PW, Joiner TE (2007). Rebuilding the tower of Babel: a revised nomenclature for the study of suicide and suicidal behaviors. Part 2: suicide-related ideations, communications, and behaviors. Suicide and Life Threatening Behavior 37, 264–277. [DOI] [PubMed] [Google Scholar]
- Soole R, Kolves K, De Leo D (2014). Suicide in children: a systematic review. Archives of Suicide Research 19, 285–304. [DOI] [PubMed] [Google Scholar]
- Statham DJ, Heath AC, Madden PA, Bucholz KK, Bierut L, Dinwiddie SH, Slutske WS, Dunne MP, Martin NG (1998). Suicidal behaviour: an epidemiological and genetic study. Psychological Medicine 28, 839–855. [DOI] [PubMed] [Google Scholar]
- Sterne J, Higgins P, Reeves B (2014). On behalf of the development group for ACROBAT-NRSI. A cochrane risk of bias assessment tool: for non-randomized studies of interventions (ACROBAT-NRSI), version 1.0. 0, 24.
- Tsypes A, Gibb BE (2015). Peer victimization mediates the impact of maternal depression on risk for suicidal ideation in girls but not boys: a prospective study. Journal of Abnormal Child Psychology 43, 1439–1445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wanner B, Vitaro F, Tremblay RE, Turecki G (2012). Childhood trajectories of anxiousness and disruptiveness explain the association between early-life adversity and attempted suicide. Psychological Medicine 42, 2373–2382. [DOI] [PubMed] [Google Scholar]
- Weissman MM, John K, Merikangas KR, Prusoff BA, Wickramaratne P, Gammon GD, Angold A, Warner V (1986). Depressed parents and their children. General health, social, and psychiatric problems. American Journal of Diseases of Children 140, 801–805. [DOI] [PubMed] [Google Scholar]
- World Health Organization (2014). Preventing Suicide. A Global Imperative, pp. 1–89. World Health Organization: Geneva, Switzerland. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
For supplementary material accompanying this paper visit https://doi.org/10.1017/S2045796017000397.
click here to view supplementary material
Data Availability Statement
As unpublished data were provided by individual authors of included studies in this review, data will not be shared. Queries are welcome by contacting the corresponding author.