Abstract
Aims.
Suicide rates are increased among unemployed individuals and mental illness stigma can contribute to both unemployment and suicidality. Persons with mental illness perceive negative attitudes among the general public and experience discrimination in their everyday life (=public stigma components) potentially leading to self-stigma and anticipated discrimination (=individual stigma components). Previous research found evidence for an association between aspects of mental illness stigma and suicidality, but has not yet clarified the underlying pathways explaining how different stigma components interact and contribute to suicidal ideation.
Method.
Public and individual stigma components and their association with suicidal ideation were examined among 227 unemployed persons with mental illness. A path model linking public stigma components (experienced discrimination, perceived stigma) with suicidal ideation, mediated by individual stigma components (anticipated discrimination, self-stigma), was examined using structural equation modelling within Mplus.
Results.
Our sample was equally split in terms of gender, on average 43 years old and about half reported no suicidal ideation during the past 30 days. In bivariate analyses all stigma components were significantly associated with suicidal ideation. In the path model and controlling for symptoms, the association between experienced discrimination and suicidal ideation was fully mediated by anticipated discrimination and self-stigma. Perceived stigma's contribution to suicidal ideation was fully mediated by anticipated discrimination, but not by self-stigma.
Conclusions.
In general, programmes addressing multiple stigma components seem to be most effective in improving suicide prevention. Besides interventions targeting negative attitudes and discriminating behaviours of the general public, programmes to support persons with mental illness in coping with perceived and experienced stigma could improve suicide prevention. Future studies should test the short- and long-term effects of such interventions on suicidality and further investigate the role of stigma coping (e.g. secrecy) and emotional consequences (e.g. hopelessness and loneliness) for the association between stigma components and suicidality.
Key words: Individual stigma, mental illness stigma, public stigma, suicidality, unemployment
Introduction
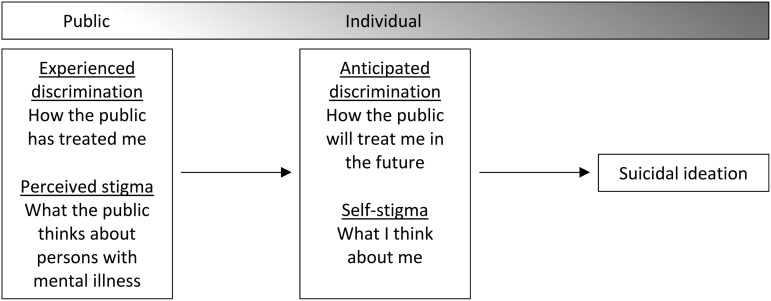
Persons with mental illness are additionally distressed by negative attitudes and discriminating behaviour of the general public (Rüsch et al. 2005). Past efforts to decrease public stigma were only partly successful, improving mental health literacy levels among the general population but not changing the social rejection of persons with mental disorders (Schomerus et al. 2012). Therefore, persons with mental illness still face negative stereotypes (e.g. people with mental illness are incompetent), prejudice (e.g. ‘Yes, applicants with mental illness are incompetent and I don't like them’) and discrimination (e.g. ‘I will not hire a person with a mental illness’), which are the central elements of mental illness stigma (Rüsch et al. 2005). Besides perceiving negative attitudes (‘What the public thinks about persons with mental illness like me’), persons with mental illness also experience discrimination in their everyday lives (‘How members of the general public have treated me’). As those two aspects reflect attitudes and behaviours of the general public, for the purpose of this paper we will refer to perceived stigma and experienced discrimination as public stigma components. In our model (Fig. 1) public stigma components affect the way individuals with mental illness think about themselves (self-stigma) and whether they anticipate future discrimination (anticipated discrimination). Self-stigma occurs if and when negative stereotypes are internalised (‘Because I have a mental illness, I am incompetent’), leading to poor self-esteem and behavioural futility (Corrigan et al. 2016). Based on personal experience and stigma perception, persons with mental illness may anticipate future discrimination (‘The public will treat me unfairly in the future’), often motivating them to keep their illness secret and avoid social situations for fear of being rejected (Link et al. 1989). We refer to self-stigma and anticipated discrimination as individual aspects of stigma since they reflect individual views and reactions to stigma. Among persons with mental illness public and individual stigma components were found to contribute to low help-seeking rates, poor clinical outcomes, social isolation, emotional distress and reduced access to housing and employment (Rüsch et al. 2005).
Fig. 1.
Multi-component model of the association between mental illness stigma and suicidal ideation from the perspective of persons with mental illness.
One aspect which only recently attracted scientific attention is stigma's contribution to suicidality. Perceived stigma was associated with increased suicidal ideation among persons labelled as mentally ill or with deficits in emotional clarity (Oexle et al. 2016a; Wang et al. 2016). Stigma stress (occurring when perceived stigma-related harm exceeds personal coping resources) was associated with suicidal ideation, mediated by social isolation (Xu et al. 2016a). In longitudinal studies self-stigma or an increase in stigma stress predicted suicidal ideation after 1 year (Oexle et al. 2016b; Xu et al. 2016b). Some studies already analysed pathways between public and individual stigma components on suicidal ideation: Oexle et al. (2016a) found that secrecy and hopelessness mediated the association between perceived stigma and suicidal ideation. One other study found discrimination experiences to contribute to suicidal ideation by leading to self-stigma, social isolation and hopelessness (Farrelly et al. 2015). Based on these findings, addressing public and individual stigma could contribute to suicide prevention (Rüsch et al. 2014). However, previous studies mostly focused on single stigma components. More research on different roles of multiple stigma components is needed in order to inform suicide prevention programmes. The link between stigma and suicidality among unemployed individuals is particularly relevant since mental illness stigma contributes to high unemployment rates among persons with mental illness and suicide rates are increased among unemployed persons (Stuart 2006; Milner et al. 2013).
Therefore, the present study examined a multi-component model of the association between public and individual stigma components and suicidal ideation from the perspective of persons with mental illness. Building on previous findings we developed a path model linking public stigma components as perceived and experienced by individuals with mental illness (experienced discrimination, perceived stigma) with suicidal ideation, mediated by individual stigma components (anticipated discrimination, self-stigma) (Fig. 1). We expected: (i) all included stigma components to be positively associated with suicidal ideation; and (ii) the associations between public stigma components and suicidal ideation to be at least partly mediated by individual stigma components.
Methods
Study design and participants
Data were derived from the AloHA project (AloHa: Arbeitslosigkeit und Hilfe-Aufsuchen), a study on unemployed persons with mental health problems. The study was advertised at unemployment agencies in southern Germany. Interested individuals completed a short telephone screening interview to determine eligibility. Inclusion criteria were being aged between 18 and 64 years and current unemployment (persons receiving full disability pension were excluded). Furthermore, individuals had to show psychological distress as indicated by a score ≥13 on the K6 Psychological Distress Scale (Kessler et al. 2003) OR have current alcohol- or substance abuse with a score ≥1 on items 2–4 of the CAGE-AID screening tool for current alcohol- and substance-use disorders (Brown & Rounds 1995). Conservatively and for the sake of specificity, we omitted item 1 (cut down) from the CAGE-AID score because in previous studies nearly half of normal controls endorsed that item (see Hinkin et al. 2001). In addition to fulfilling either the K6 or CAGE-AID criterion, participants needed to reach a score of ≥17 (range of possible scores: 12–60) on the WHO-Disability Assessment Schedule 2.0 (Üstün et al. 2010), corresponding approximately to the 85th general population percentile and to the average disability level of persons with one mental disorder (Andrews et al. 2009). We thus only included participants with significant illness-related disability.
In total, 590 persons participated in the screening of whom 331 fulfilled eligibility criteria and were invited to participate in a questionnaire survey. Three hundred and one persons completed the baseline assessment. Participants with increased suicidality scores were offered to discuss treatment options with a psychiatrist and received information leaflets about nearby mental health services and emergency help-lines.
Measures
The 5-item Suicidal Ideation Attributes Scale (SIDAS) was used to assess current suicidal ideation (van Spijker et al. 2014). On the first item, participants rated suicidal thoughts during the past 30 days on a 11-point scale (0/never – 10/always). Persons who scored 1 or more were then asked to which extent these thoughts were controllable (0/no control at all – 10/full control), distressing (0/not at all – 10/extremely), interfering with their daily life (0/not at all – 10/extremely), and how close they were to a suicide attempt (0/not at all close – 10/have made an attempt). Item two (controllability) was reverse coded and a sum score from 0 to 50 indicated current suicidal ideation (Cronbach's alpha in this sample α = 0.94).
Experienced discrimination was assessed by the respective subscale of the Internalized Stigma of Mental Illness Inventory (ISMI; Ritsher et al. 2003). The subscale consists of five statements reflecting typical discrimination and participants rated the extent to which those statements reflected their personal experience on 4-point Likert scales (1/strongly disagree – 4/strongly agree; e.g. ‘People ignore me or take me less seriously just because I have a mental illness’). A total experienced discrimination mean score was calculated across all items (Cronbach's alpha in this sample α = 0.89). Perceived stigma was assessed by the Perceived Devaluation-Discrimination Questionnaire (PDDQ; Link et al. 1989). Participants indicated whether 12 statements reflected their perception of public attitudes towards persons with mental illness on 6-point Likert scales (1/not true at all – 6/very true; e.g., ‘Most people think less of a person who has been in a mental hospital’), with higher mean scores reflecting more perceived stigma (Cronbach's alpha in this sample α = 0.89). The anticipation of being discriminated was assessed by the Questionnaire on Anticipated Discrimination (QUAD; Gabbidon et al. 2013). Participants rated their agreement with 14 statements about discrimination expectations on 4-point Likert scales (1/strongly disagree – 4/strongly agree; e.g. ‘If the police know I have a mental health problem they will treat me unfairly’). A total anticipated discrimination score was calculated as the mean across all items (Cronbach's alpha in this sample α = 0.91). Self-stigma was measured using the self-apply subscale of the Self-stigma of Mental Illness Scale Short Form (SSMIS-SF; Corrigan et al. 2012a). Participants rated their agreement with five statements reflecting self-stigmatising attitudes on 9-point scales (1/strongly disagree – 9/strongly agree; e.g., ‘Because I have a mental illness, I am dangerous’). A self-stigma sum score from 5 to 45 was calculated across all items (Cronbach's alpha in this sample α = 0.64). Psychopathology was measured using a 9-item version of the revised Symptom Checklist 90 (Klaghofer & Brähler 2000), yielding a total mean symptom score.
Statistical analyses
Only participants who identified themselves as having a mental illness in response to a filter question (‘I have a mental illness/see myself as having a mental illness or am impaired due to mental illness’) were asked to provide information on experienced discrimination, anticipated discrimination and self-stigma associated with mental illness. Therefore, 227 individuals were included in the statistical analyses. Using SPSS Version 21, we compared those 227 individuals v. the 74 excluded participants who did not self-identify as mentally ill regarding suicidal ideation, perceived stigma, and socio-demographic variables (t-tests for continuous variables and chi-square (χ2) tests for categorical variables) to rule out potential bias introduced by the exclusion. Variable distributions were checked visually, characteristics of the sample were described and correlations between the independent and dependent variables were calculated (Pearson correlations for continuous independent variables and point-biserial correlations for categorical independent variables). Finally, the hypothesised model (Fig. 2) was tested as a structural equation model (SEM) using maximum-likelihood estimation within MPlus Version 7.4 (Muthén & Muthén 1998). In line with previous recommendations (Kenny 2015) acceptable model fit is indicated by a non-significant χ2-statistic, CFI > 0.90, TLI > 0.90, RMSEA < 0.08 and SRMR < 0.08. Bootstrapping was used to ensure robust standard errors and confidence intervals (bootstrap replications: 5000). Estimated paths were controlled for potential confounding effects.
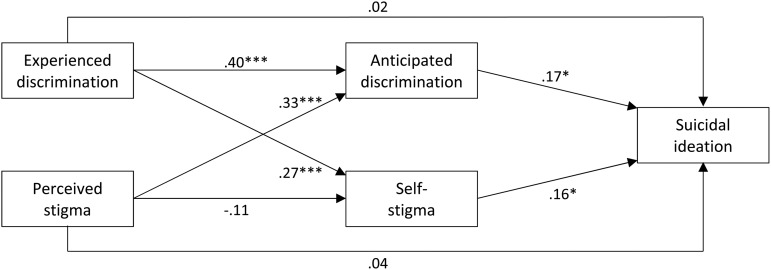
Fig. 2.
Path model linking public and individual stigma components with suicidal ideation. All paths were controlled for symptoms. *p < 0.05, ***p < 0.001.
Results
Regarding psychological distress and substance use criteria the analysed sample consisted of 154 persons fulfilling criteria based on the K6, 16 persons fulfilling criteria based on the CAGE-AID and 57 persons fulfilling criteria of both K6 and CAGE-AID. Compared with the 227 individuals included in the analyses, persons excluded due to the lack of self-identification as mentally ill were less distressed by suicidality (M = 8.0, s.d. = 10.9; M = 3.0, s.d. = 7.0; t = −4.5, p < 0.001) and symptoms (M = 3.2, s.d. = 0.7; M = 2.4, s.d. = 0.7; t = −8.1, p < 0.001). No significant differences between the two groups were found regarding perceived stigma, age, length of lifetime unemployment and gender (all p > 0.15).
As expected the distribution of suicidal ideation was skewed, with nearly half of participants (47%) reporting no suicidal thoughts during the past 30 days (Table 1). Compared to the midpoint of the scales, on average medium experienced discrimination, medium perceived stigma, medium anticipated discrimination, low to medium self-stigma and medium symptom levels were observed. Participants were on average 43 years old and about half female. The average length of lifetime unemployment was about 5 years, ranging from 3 days up to 30 years.
Table 1.
Sample characteristics, N = 227
| Variables (and range of possible scores, where appropriate) | Mean (SD), or n, % | Percentiles | ||
|---|---|---|---|---|
| 25 | 50 | 75 | ||
| Suicidal ideation (SIDAS), 0–50 | 8.0 (10.8) | 0.0 | 2.0 | 14.0 |
| Experienced discrimination (ISMI), 1–4 | 2.3 (0.8) | 1.6 | 2.2 | 2.8 |
| Perceived stigma (PDDQ), 1–6 | 4.3 (0.9) | 3.7 | 4.3 | 5.0 |
| Anticipated discrimination (QUAD), 1–4 | 2.2 (0.6) | 1.8 | 2.2 | 2.6 |
| Self-stigma (SSMIS-SF), 5–45 | 14.4 (6.7) | 9.0 | 13.0 | 19.0 |
| Symptoms (SCL9), 1–5 | 3.2 (0.7) | 2.7 | 3.2 | 3.8 |
| Age (years) | 43.1 (11.0) | 34.0 | 45.0 | 52.0 |
| Gender | ||||
| Male (0) | 113, 50% | – | ||
| Female (1) | 114, 50% | |||
| Lifetime unemployment (months) | 65.0 (59.6) | 24.0 | 48.0 | 96.0 |
Suicidal ideation was significantly and positively associated with experienced discrimination, perceived stigma, anticipated discrimination, self-stigma and symptoms (all p < 0.01). No significant associations with suicidal ideation were found for age, gender and length of lifetime unemployment. Therefore, only symptoms were included as a confounder in the subsequent SEM analysis (Table 2).
Table 2.
Pearson or point-biserial correlations between independent and outcome variables, N = 227
| Independent variables | Suicidal ideation (SIDAS) (past 30 days) |
|---|---|
| Experienced discrimination (ISMI) | 0.30** |
| Perceived stigma (PDDQ) | 0.20* |
| Anticipated discrimination (QUAD) | 0.35** |
| Self-stigma (SSMIS-SF) | 0.26** |
| Symptoms (SCL-9) | 0.40** |
| Age (years) | −0.06 |
| Gender (0 = male, 1 = female) | −0.05 |
| Lifetime unemployment (months) | 0.00 |
**p < 0.001; *p < 0.01.
Fit indices of the final model suggest acceptable fit (Table 3). Path estimates are shown in Fig. 2. Previously observed direct effects of public stigma components (experienced discrimination, perceived stigma) on suicidal ideation lost significance, while individual stigma variables significantly contributed to the outcome. Total indirect effects were significant for experienced discrimination (β = 0.11, 95%CI 0.03–0.21), but not for perceived stigma (β = 0.04, 95%CI −0.03 to 0.11). Experienced discrimination indirectly contributed to suicidal ideation via both self-stigma (β = 0.01, 95%CI 0.01–0.11) and anticipated discrimination (β = 0.07, 95%CI 0.01–0.15). Perceived stigma increased suicidal ideation via anticipated discrimination (β = 0.06, 95%CI 0.01–0.13), but not via self-stigma (β = −0.02, 95%CI −0.06 to 0.01). The estimated model explained 22% of the total variance in suicidal ideation (R2 = 0.22). We also tested an alternative model, including covariance between experienced discrimination and perceived stigma as well as between anticipated discrimination and self-stigma. As the fit was bad, the model was rejected.
Table 3.
Fit indices of the final path model
Acceptable fit is indicated by a non-significant χ2, CFI > 0.90, TLI > 0.90, RMSEA < 0.08, SRMR < 0.08 (Kenny 2015).
Discussion
Our findings provide initial evidence how public and individual aspects of stigma contribute to suicidal ideation among unemployed persons with mental health problems. As hypothesised and in line with previous findings, all included stigma components were positively associated with suicidal ideation. In the path analysis, we found that individual stigma components completely mediated the association between public stigma and suicidal ideation.
More experienced discrimination increased both self-stigma and anticipated discrimination, which then both contributed to suicidal ideation. While we expected the same pattern for perceived stigma, it was only associated with anticipated discrimination, not with self-stigma. This is in line with previous observations that the sole awareness of stigma does not always lead to self-stigma, as perception alone is not necessarily self-relevant (Link et al. 1989; Corrigan et al. 2009). A recent investigation based on a different sample than the one included in the current study found perceived stigma to be associated with suicidal ideation only among persons labelled as mentally ill for whom stigma was self-relevant (Oexle et al. 2016a). Although all included individuals in the current study identified themselves as having a mental illness, some participants might have judged perceived stigma as less self-relevant. Nevertheless, as it leads to increased anticipated discrimination, perceived stigma contributed to suicidal ideation. While no previous study examined the effect of anticipated discrimination on suicidal ideation, we found a robust association between the two. As the anticipation of being discriminated is common among persons with mental illness, even if discrimination is not experienced (Thornicroft et al. 2009; Lasalvia et al. 2013), this finding is noteworthy and deserves more scientific attention. While our model included public stigma as perceived and experienced by persons with mental illness as well as individual stigma components, we did not include stigma coping and emotional consequences as potential mediators. In line with previous findings (Farrelly et al. 2015; Oexle et al. 2016a; Xu et al. 2016a) loneliness and hopelessness could mediate the association between stigma components and suicidal ideation. In contrast to earlier studies (Milner et al. 2013) we did not find an association between the length of unemployment and suicidal ideation.
Findings on the association between mental illness stigma and suicidal ideation are rare and previous studies employed heterogeneous study designs mainly focused on single stigma components. Additionally, some previous findings were subject to bias as analyses were not controlled for confounding effects such as symptom levels or binary outcome measures were used. Our study addressed a meaningful gap by analysing data derived from unemployed individuals, a hard to reach population with increased suicide rates. A continuous outcome measure was used and our analyses accounted for the complexity of mental illness stigma as perceived and experienced by people with mental illness as well as controlled for symptoms. The generalisability of findings is limited due to self-selection of participants and the sampling criteria. As merely unemployed persons with mental health problems were included, associations might be different in other samples. However, our results are in line with previous findings among other samples and lifetime unemployment was considered as a potential confounding variable. Due to cross-sectional data no firm conclusions about causality can be drawn.
Nevertheless, the present study provides meaningful information for future programmes targeting mental illness stigma in order to improve suicide prevention. In general, multi-faceted approaches targeting both public and individual stigma components are likely to be most effective. Perceived stigma and experienced discrimination among persons with mental illness could be reduced by interventions targeting negative attitudes and discriminating behaviour of the general public, such as programmes including social contact with stigmatised persons and education (Corrigan et al. 2012b; Thornicroft et al. 2016). In line with our results, such interventions are likely to also reduce individual stigma components (Evans-Lacko et al. 2012). Additionally, persons with mental illness should be supported in coping with perceived stigma and experienced discrimination. While self-stigma can be reduced by interventions using psycho-education and peer support (Mittal et al. 2012), evidence for programmes reducing anticipated discrimination is lacking. Future research should examine short- and long-term effects of anti-stigma interventions on suicidality.
Acknowledgements
We are grateful to the German Federal Employment Agency and its Medical Service as well as to joint local agencies and approved local providers for their support with participant recruitment.
Financial Support
The AloHA study was funded by the German Research Foundation (DFG grant number, RU 1200/3-1).
Conflict of Interest
None.
Ethical Standards
All individuals gave their written informed consent prior to their participation. The study was approved by the Ethics Committee of Ulm University (reference number: 344/13).
Availability of Data and Materials
Participants provided written informed consent under the condition of confidentiality of their data including restricted access of third parties. Therefore, data cannot be shared publicly.
References
- Andrews G, Kemp A, Sunderland M, Von Korff M, Ustun TB (2009). Normative data for the 12 item WHO disability assessment schedule 2.0. PLoS ONE 4, e8343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown RL, Rounds LA (1995). Conjoint screening questionnaires for alcohol and other drug abuse: criterion validity in a primary care practice. Wisconsin Medical Journal 94, 135–140. [PubMed] [Google Scholar]
- Corrigan PW, Larson JE, Rüsch N (2009). Self-stigma and the “why try” effect: impact on life goals and evidence-based practices. World Psychiatry 8, 75–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corrigan PW, Michaels PJ, Vega E, Gause M, Watson AC, Rüsch N (2012a). Self-stigma of mental illness scale-short form: reliability and validity. Psychiatry Research 199, 65–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corrigan PW, Morris SB, Michaels PJ, Rafacz JD, Rüsch N (2012b). Challenging the public stigma of mental illness: a meta-analysis of outcome studies. Psychiatric Services 63, 963–973. [DOI] [PubMed] [Google Scholar]
- Corrigan PW, Bink AB, Schmidt A, Jones N, Rüsch N (2016). What is the impact of self-stigma? Loss of self-respect and the “why try” effect. Journal of Mental Health 25, 10–15. [DOI] [PubMed] [Google Scholar]
- Evans-Lacko S, Brohan E, Mojtabai R, Thornicroft G (2012). Association between public views of mental illness and self-stigma among individuals with mental illness in 14 European countries. Psychological Medicine 42, 1741–1752. [DOI] [PubMed] [Google Scholar]
- Farrelly S, Jeffery D, Rüsch N, Williams P, Thornicroft G, Clement S (2015). The link between mental health-related discrimination and suicidality: service user perspectives. Psychological Medicine 45, 2013–2022. [DOI] [PubMed] [Google Scholar]
- Gabbidon J, Brohan E, Clement S, Henderson RC, Thornicroft G (2013). The development and validation of the Questionnaire on Anticipated Discrimination (QUAD). BMC Psychiatry 13, 297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hinkin CH, Castellon SA, Dickson-Fuhrman E, Daum G, Jaffe J, Jarvik L (2001). Screening for drug and alcohol abuse among older adults using a modified version of the CAGE. The American Journal on Addictions 10, 319–326. [PubMed] [Google Scholar]
- Kenny DA (2015). SEM: Measuring Model Fit Retrieved 25 July 2016 from http://davidakenny.net/cm/fit.htm
- Kessler RC, Barker PR, Colpe LJ, Epstein JF, Gfroerer JC, Hiripi E, Howes MJ, Normand S-LT, Manderscheid RW, Walters EE, Zaslavsky AM (2003). Screening for serious mental illness in the general population. Archives of General Psychiatry 60, 184–189. [DOI] [PubMed] [Google Scholar]
- Klaghofer R, Brähler E (2000). Konstruktion und teststatistische Prüfung einer Kurzform der SCL-90-R [construction and evaluation of the short version of SCL-90-R]. Zeitschrift für klinische Psychologie, Psychiatrie und Psychotherapie 49, 115–124. [Google Scholar]
- Lasalvia A, Zoppei S, Van Bortel T, Bonetto C, Cristofalo D, Wahlbeck K, Bacle SV, Van Audenhove C, van Weeghel J, Reneses B, Germanavicius A, Economou M, Lanfredi M, Ando S, Sartorius N, Lopez-Ibor JJ, Thornicroft G (2013). Global pattern of experienced and anticipated discrimination reported by people with major depressive disorder: a cross-sectional survey. The Lancet 381, 55–62. [DOI] [PubMed] [Google Scholar]
- Link BG, Cullen FT, Struening E, Shrout PE, Dohrenwend BP (1989). A Modified Labeling Theory approach to mental disorders: an empirical assessment. American Sociological Review 54, 400–423. [Google Scholar]
- Milner A, Page A, LaMontagne AD (2013). Long-term unemployment and suicide: a systematic review and meta-analysis. PLoS ONE 8, e51333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mittal D, Sullivan G, Chekuri L, Allee E, Corrigan PW (2012). Empirical studies of self-stigma reduction strategies: a critical review of the literature. Psychiatric Services 63, 974–981. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO (1998). MPlus User's Guide, 7th edn., Muthén & Muthén: Los Angeles, CA. [Google Scholar]
- Oexle N, Ajdacic-Gross V, Kilian R, Müller M, Rodgers S, Xu Z, Rössler W, Rüsch N (2016a). Mental illness stigma, secrecy and suicidal ideation. Epidemiology and Psychiatric Sciences, published online. doi: 10.1017/S2045796015001018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oexle N, Rüsch N, Viering S, Wyss C, Seifritz E, Xu Z, Kawohl W (2016b). Self-stigma and suicidality: a longitudinal study. European Archives of Psychiatry and Clinical Neuroscience, published online. doi: 10.1007/s00406-016-0698-1 [DOI] [PubMed] [Google Scholar]
- Ritsher JB, Otilingam PG, Grajales M (2003). Internalized stigma of mental illness: psychometric properties of a new measure. Psychiatry Research 121, 31–49. [DOI] [PubMed] [Google Scholar]
- Rüsch N, Angermeyer MC, Corrigan PW (2005). Mental illness stigma: concepts, consequences, and initiatives to reduce stigma. European Psychiatry 20, 529–539. [DOI] [PubMed] [Google Scholar]
- Rüsch N, Zlati A, Black G, Thornicroft G (2014). Does the stigma of mental illness contribute to suicidality? The British Journal of Psychiatry 205, 257–259. [DOI] [PubMed] [Google Scholar]
- Schomerus G, Schwahn C, Holzinger A, Corrigan PW, Grabe HJ, Carta MG, Angermeyer MC (2012). Evolution of public attitudes about mental illness: a systematic review and meta-analysis. Acta Psychiatrica Scandinavica 125, 440–452. [DOI] [PubMed] [Google Scholar]
- van Spijker BAJ, Batterham PJ, Calear AL, Farrer L, Christensen H, Reynolds J, Kerkhof AJFM (2014). The Suicidal Ideation Attributes Scale (SIDAS): community-based validation study of a new scale for the measurement of suicidal ideation. Suicide & Life – Threatening Behavior 44, 408–419. [DOI] [PubMed] [Google Scholar]
- Stuart H (2006). Mental illness and employment discrimination. Current Opinion in Psychiatry 19, 522–526. [DOI] [PubMed] [Google Scholar]
- Thornicroft G, Brohan E, Rose D, Sartorius N, Leese M, the INDIGO Study Group (2009). Global pattern of experienced and anticipated discrimination against people with schizophrenia: a cross-sectional survey. The Lancet 373, 408–415. [DOI] [PubMed] [Google Scholar]
- Thornicroft G, Mehta N, Clement S, Evans-Lacko S, Doherty M, Rose D, Koschorke M, Shidhaye R, O'Reilly C, Henderson C (2016). Evidence for effective interventions to reduce mental-health-related stigma and discrimination. The Lancet 387, 1123–1132. [DOI] [PubMed] [Google Scholar]
- Üstün TB, Chatterji S, Kostanjsek N, Rehm J, Kennedy C, Epping-Jordan J, Saxena S, von Korff M, Pull C (2010). Developing the World Health Organization disability assessment schedule 2.0. Bulletin of the World Health Organization 88, 815–823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang K, Weiss NH, Pachankis JE, Link BG (2016). Emotional clarity as a buffer in the association between perceived mental illness stigma and suicide risk. Stigma and Health. doi: 10.1037/sah0000032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu Z, Müller M, Heekeren K, Theodoridou A, Metzler S, Dvorsky D, Oexle N, Walitza S, Rössler W, Rüsch N (2016a). Pathways between stigma and suicidal ideation among people at risk of psychosis. Schizophrenia Research 172, 184–188. [DOI] [PubMed] [Google Scholar]
- Xu Z, Mayer B, Müller M, Heekeren K, Theodoridou A, Dvorsky D, Metzler S, Oexle N, Walitza S, Rössler W, Rüsch N (2016b). Stigma and suicidal ideation among young people at risk of psychosis after one year. Psychiatry Research 243, 219–224. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Participants provided written informed consent under the condition of confidentiality of their data including restricted access of third parties. Therefore, data cannot be shared publicly.