Abstract
Aim.
In low-income African countries, ensuring food security for all segments of the population is a high priority. Mental illness is associated consistently with poverty, but there is little evidence regarding the association with food insecurity. The aim of this study was to compare the levels of food insecurity in people with severe mental disorders (SMD) with the general population in a rural African setting with a high burden of food insecurity.
Method.
Households of 292 community-ascertained people with a specialist-confirmed diagnosis of SMD (including schizophrenia and bipolar disorder) were compared with 284 households without a person with SMD in a rural district in south Ethiopia. At the time of the study, no mental health services were available within the district. Food insecurity was measured using a validated version of the Household Food Insecurity Access Scale. Disability was measured using the World Health Organisation Disability Assessment Schedule 2.0.
Result.
Severe household food insecurity was reported by 32.5% of people with SMD and 15.9% of respondents from comparison households: adjusted odds ratio 2.82 (95% confidence interval 1.62 to 4.91). Higher annual income was associated independently with lower odds of severe food insecurity. When total disability scores were added into the model, the association between SMD and food insecurity became non-significant, indicating a possible mediating role of disability.
Conclusion.
Efforts to alleviate food insecurity need to target people with SMD as a vulnerable group. Addressing the disabling effects of SMD would also be expected to reduce food insecurity. Access to mental health care integrated into primary care is being expanded in this district as part of the Programme for Improving Mental health carE (PRIME). The impact of treatment on disability and food insecurity will be evaluated.
Key words: Disability, food insecurity, psychosis, severe mental disorder, sub-Saharan Africa
Introduction
Secure access to adequate amounts of healthy and nutritious food is considered to be a foundational determinant of health (Muldoon et al. 2013). Food insecurity is conceptualised as limited or uncertain access to adequate food, and encompasses food availability, access and utilisation (Mengistu et al. 2009; United States Department of Agriculture, 2016). Ending hunger and achieving food security is one of the United Nation's Sustainable Developmental Goals (SDG) to be achieved by 2030 (United Nations, 2015). In Ethiopia, both chronic and transitory (seasonal) food insecurity are persistent problems for a large segment of the population (Mengistu et al. 2009). In 2012, there was an 82.3% prevalence of household-level food insecurity in a zone in southern Ethiopia (Regassa & Stoecker, 2011).
The associations between food insecurity and physical health problems are well documented, but the links between food insecurity and mental illness have been less well characterised (Collins, 2005). Ethnographic work has linked the experience of food insecurity with mood disorders, symptoms of anxiety and depression (Kempson et al. 2002), poor mental health in general (Xiong et al. 1994) and higher levels of stress, anxiety, irritability, social isolation and depression (Collins, 2005). In cross-sectional studies, a consistent association has also been found between depression and anxiety and food insecurity (Hadley & Patil, 2006; Sorsdahl et al. 2009; Cole & Tembo, 2011), including within Ethiopia (Hadley et al. 2008; Maes et al. 2010; Jebena et al. 2015). There have been few longitudinal studies to examine the direction of association, but it is hypothesised that depression or anxiety are more likely to be a consequence than a cause of poverty and associated food insecurity (Lund et al. 2010).
The risk of food insecurity has been much less well studied in people with severe mental disorders (SMD; including schizophrenia, schizoaffective disorder, bipolar disorder or severe depression/depression with psychotic features). In a study from the USA, 45.8% of people with SMD were classified as food insecure, of which 29.2% experienced very low food security (Goetz, 2008). Such studies are unlikely to be generalisable to low- and middle-income countries (LMICs), where the background burden of food insecurity is higher and the consequences of food security more dire.
In this study, we evaluated food insecurity in a population sample of people with SMD identified before introduction of integrated primary care-based mental health care in a rural Ethiopian district. The study aimed to compare food insecurity in households with a person with SMD compared with households from the general population.
Methods
Study design
A community-based, comparative cross-sectional study was conducted between December 2014 and August 2015.
Setting
The study was carried out in Sodo District, Gurage Zone, of the Southern Nations, Nationalities and Peoples’ Region (SNNPR) of Ethiopia, which is located 100 km from the capital city, Addis Ababa. Sodo comprises 58 sub-districts (kebeles), with a total estimated population of around 165 000 (Lund et al. 2012). The district is mostly rural, with the majority of the population relying on subsistence farming. At the time of this study, there were no mental health services within the district. As part of the Programme for Improving Mental health carE (PRIME) (Lund et al. 2012), primary care workers were trained to detect and treat people with SMD, epilepsy, depression and alcohol use disorders. This study was nested within the PRIME project activities with people with SMD.
Sampling and recruitment
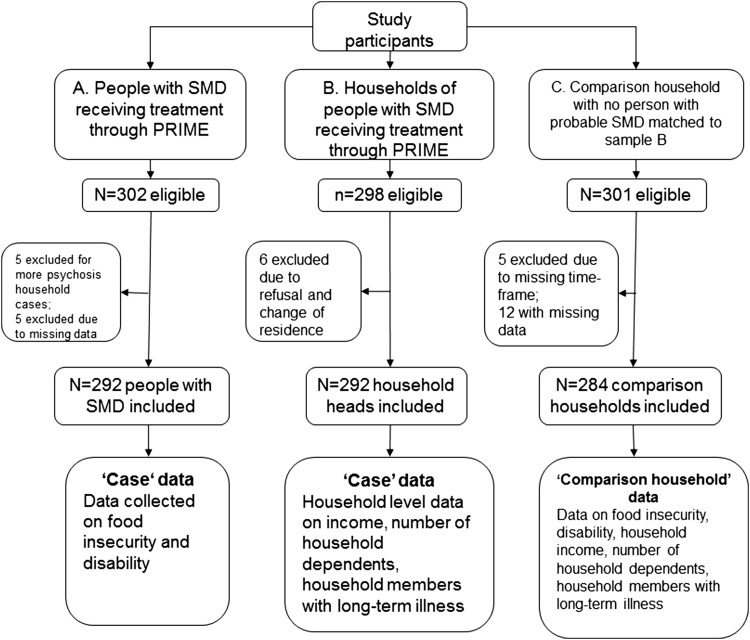
A summary of the study sampling and recruitment is found in Fig. 1. There were three sources of data: (1) person with probable SMD or their caregiver (PRIME project), (2) household of a person with SMD and (3) control household without a person with SMD. Data sources (2) and (3) were obtained from a household economic survey conducted by a linked project, Emerald (Emerging mental health systems in LMICs) (Semrau et al. 2015).
Fig. 1.
Flow chart of participant recruitment.
People with probable SMD were identified by community-based health extension workers, community leaders and project outreach workers who had received half a day of training on common presentations of SMD for the setting (Fekadu et al. 2016). This key informant method has been shown to be an effective means of community ascertainment of SMD for this setting (Shibre et al. 2002). People with suspected SMD were then referred to the nearest primary health care (PHC) centre and evaluated by primary care workers who had been trained in the World Health Organisation's mental health Gap Action Programme (mhGAP) base course (World Health Organisation, 2008; Dua et al. 2011). For those who received a PHC worker diagnosis of ‘psychosis’ or ‘bipolar disorder’, a confirmatory clinical interview was conducted by a psychiatric nurse using the semi-structured Operational Criteria for Research (OPCRIT) interview guide (McGuffin et al. 1991). Eligible people were then recruited into the study on the basis of the following criteria:
Eligibility criteria for people with SMD:
-
•
Aged 18 years or older,
-
•
Planning to stay resident in the district for the next 12 months,
-
•
Provided informed consent (evaluated by trained psychiatric nurses) or, if lacked capacity to consent, did not refuse and guardian permission was obtained,
-
•
Psychiatric nurse confirmed diagnosis using the OPCRIT, and
-
•
Able to understand Amharic, the official language of Ethiopia and the working language of the study site.
Eligibility criteria for respondent from household of person with SMD:
-
•
Having a person with SMD in a household; aged 18 years or above; provided informed consent; resided in the household for a minimum of 4 months; household head or the older person if two household members contributed equally to household decision-making;
Eligibility criteria for control households:
-
•
No person/family member with suspected or confirmed SMD within the household; aged 18 years or above; providing informed consent.
-
•
Matched to a household in which a person with SMD resided [on the basis of age (±5 years), sex, village (gott), household position (head v. not head) and household size, using a complete census of the district as a sampling frame (Fekadu et al. 2014)]. If more than one match was identified, the household was selected by lottery. If no respondent was identified for the first matched household after three home visits, or if they declined to participate, the next reserve was selected.
Sample size and power calculation
The sample size for this study was determined by the sample sizes for the PRIME and Emerald studies which were powered to detect change in symptoms and economic status in people with SMD and their households after introduction of mental health care. The PRIME study recruited 300 people with SMD. The Emerald study recruited 300 households of people with SMD and 300 households of controls. Details of the power that this sample size afforded us to detect differences in the prevalence of food insecurity are provided in Supplementary File 1.
Measures
Primary outcome: food insecurity
Food insecurity was measured using the Household Food Insecurity Access Scale (HFIAS) (Coates et al. 2007). The HFIAS was administered to people with SMD and the respondent for the control households. The HFIAS was developed to reflect three domains of the experience of inadequate household-level food access: (1) anxiety or uncertainty about food supply/access (item 1); (2) insufficient quality, which includes variety and preferences (items 2–4); and (3) insufficient quantity of food supply, the amount consumed and the physical consequences of insufficiency (items 5–9) (Swindale & Bilinsky, 2006). An Amharic version of the HFIAS-9 has been used in Ethiopia (Hadley et al. 2008; Maes et al. 2010; Jebena et al. 2015) and is reported to be valid in this setting (Gebreyesus et al. 2015). During piloting, there were acceptability concerns about items asking about missing meals. A contextualising lead-in statement was added, which led to improved acceptability. The HFIAS was administered by trained lay interviewers.
Primary exposure: SMD
The OPCRIT semi-structured interview was used to diagnose the presence of SMD (McGuffin et al. 1991). OPCRIT comprises a 90-item checklist of psychiatric symptoms, which is administered by a mental health professional and was used to generate psychiatric diagnoses according to the Diagnostic and Statistical Manual for mental disorders, version IV (McGuffin et al. 1991; Azevedo et al. 1999). OPCRIT allows the rater to make use of all available information sources, including clinical interviews with the person and their caregiver and case records and applies operational diagnostic criteria through a computer algorithm (Operational Criteria for Research, 2004). OPCRIT has been shown to have good inter-rater reliability, including among raters from different geographical and theoretical backgrounds (McGuffin et al. 1991; Williams et al. 1996). OPCRIT was administered by psychiatric nurses and only administered to people with suspected SMD.
Potential mediator: functional impairment
The World Health Organisation Disability Assessment Schedule 2.0 (WHODAS) was used to measure functional impairment (World Health Organisation, 1985). The WHODAS has been validated for use in people with SMD in rural Ethiopia (Habtamu et al. 2017). The WHODAS has both 36- and 12-item versions, with the 12-item version found to have equivalent psychometric properties to the longer version (Ustün et al. 2010). In the control households, the 12-item version of WHODAS was used. In the sample of people with SMD, the 12-item WHODAS was extracted from the longer 36-item version.
Potential confounders
Household measures
Structured lay interviewer-administered questions were used to assess household income, the number of household members with a long-term illness and the number of dependents (age 17 years or less) living in the household, employing items used in the WHO study on global ageing and adult health (World Health Organisation, 2013). Other potential confounders were age, sex, residence (urban or rural), household position (being a household head v. not being a household head) and educational level of the respondent. Month of assessment was also a potential confounder due to seasonal variation in food security.
Training of data collectors
The lay data collectors had completed at least tenth grade education and were recruited from the local area. The training was conducted for 12 days by project psychologists, public health and social work professionals and covered the following topics: basic interviewing skills, particular skills for interviewing people with SMD and their caregivers, ethical considerations and detailed training on the study instruments. The training included role play and observation of practice interviews.
Training of clinician assessors
The project psychiatric nurses were given intensive training by senior Ethiopian psychiatrists in the clinician-administered measures over a period of seven days. The training included observed interviews and feedback, although formal inter-rater reliability was not assessed formally.
Data management
Double data entry was carried out using EpiData software (Lauritsen & Bruus, 2003–2008). To maintain data quality, the field supervisor and principal investigator (PI) made unannounced visits to attend interviews at the site, with frequent and close supervision and cross-checks. Random quality checks of questionnaires were also made by the field supervisor and PI. Confidentiality was ensured. Hard copies of data were stored in a secure place, while the soft copies of data were saved on password-protected computers which could only be accessed by authorised members of the research team.
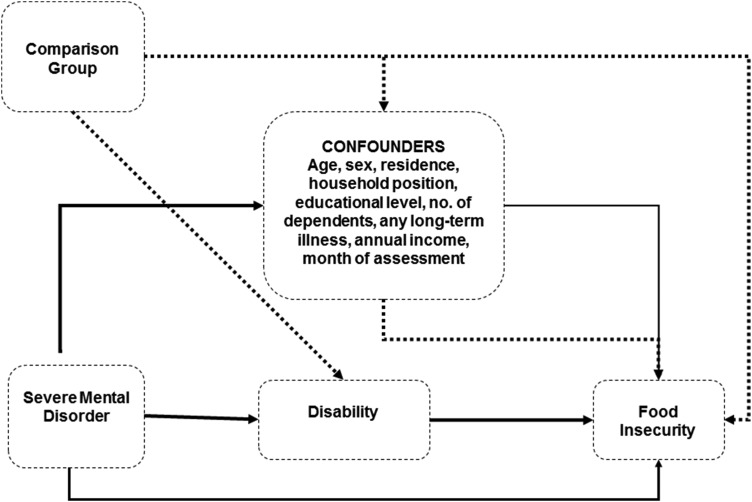
Statistical analysis
Data analysis was carried out using STATA software version 13.1 (StataCorp, 1985–2013). A conceptual model depicting hypothesised associations among the variables is presented in Fig. 2. The descriptive characteristics of cases (individual-level data from person with SMD combined with household reports) and controls were compared using Pearson χ2 test for categorical variables, Kruskal–Wallis (P < 0.001) for continuous non-normally distributed variables and two-sample t-test for continuous normally distributed variables.
Fig. 2.
Conceptual model for hypothesised associations between severe mental disorder, disability and food insecurity.
Multiple logistic regression was conducted to test the hypothesis that the presence of a household member with SMD was associated with food insecurity in that household. The HFIAS total score was dichotomised into severely food insecure v. combined categories of mild or moderate food insecurity or food secure (Swindale & Bilinsky, 2006). The rationale for this categorisation was that severe food insecurity was expected to be relatively common in the study setting and to represent a threshold which was likely to motivate intervention. We also repeated the analyses using a dichotomisation of no/mild food insecurity v. moderate/severe food insecurity as an exploratory secondary analysis. The potential confounders identified a priori (see above) were included into the model. In order to explore whether disability mediated the association between SMD and food insecurity, the total WHODAS score was added into the fully adjusted model with food insecurity as the dependent variable.
A further multivariable analysis was then conducted to examine factors associated with disability (total score on the WHODAS12-item version). On inspection, a histogram of WHODAS scores indicated excess zeroes. Variance in WHODAS scores was greater than the mean score (177.48 > 13.89), indicating overdispersion. The Vuong test z-value was significant, indicating that a zero-inflated negative binomial model was more appropriate than the standard negative binomial model. Coefficients are on a log scale and for ease of interpretation were exponentiated.
Results
Participant and household characteristics
Participant recruitment is summarised in Fig. 1. The characteristics of participants are summarised in Table 1. Respondents who had SMD were less likely to be the household head and to have dependents and more likely to be female, younger and have higher disability scores, formal education and lower annual income. The timing of assessments for case and comparison households differed significantly (see Supplementary File 2 for distribution). The assessment was conducted during the rainy season (June to August), a time of relative food insecurity, for 14.7% of case households and 43.3% of the comparison group. There was no significant difference in the location of the household (rural or urban) or presence of a household member with a long-term illness (excluding the person with SMD).
Table 1.
Characteristics of households with a person with severe mental disorder (SMD) and comparison households
| Characteristics | Person with severe mental disorder (SMD) | Comparison households with no person with SMD | P-value** |
|---|---|---|---|
| N (%) | N (%) | ||
| Currently household head | |||
| No | 184 (63.0) | 6 (2.1) | <0.001 |
| Yes | 108 (37.0) | 277 (97.9) | |
| Educational level | |||
| Non-literate | 116 (39.7) | 99 (34.8) | <0.001 |
| Able to read and write | 37 (12.7) | 88 (31.0) | |
| Formal education | 139 (47.6) | 97 (34.1) | |
| Sex | |||
| Female | 126 (43.1) | 77 (27.1) | <0.001 |
| Male | 166 (56.9) | 207 (72.9) | |
| Residence | |||
| Urban | 60 (20.6) | 56 (19.7) | 0.788 |
| Rural | 231 (79.4) | 228 (80.3) | |
| HFIAS | |||
| Secure/mildly/moderately food insecure | 195 (67.5) | 239 (84.1) | <0.001 |
| Severely food insecure | 94 (32.5) | 45 (15.9) | |
| Mean (standard deviation) | Mean (standard deviation) | ||
| Age (years) | 35.6 (13.50) | 49.7 (13.86) | <0.001 |
| Month of assessment* | 4.3 (3.28) | 5.5 (1.84) | <0.001 |
| Median (25th, 75th centiles) | Median (25th, 75th centiles) | ||
| No. of members with any Long-term illness | 0 (0, 0) | 0 (0, 0) | 0.4701 |
| No. of dependents | 2 (1, 3) | 2 (1, 4) | 0.0001 |
| Number of children | 1 (0, 3) | 4 (2, 6) | <0.001 |
| Annual Income (ETB) | 6000 (3000, 11 000) | 9000 (5000, 15 000) | <0.001 |
| WHODAS 2.0 total score | 24 (14, 32) | 2 (0, 7) | <0.001 |
Months numbered starting from January. ETB: Ethiopian Birr; WHODAS: World Health Organisation Disability Assessment Schedule.
P-value of Pearson χ2 for categorical variables, Kruskal–Wallis for continuous non-normally distributed descriptive variables and two-sample t-test with equal variances for continuous normally distributed variables.
SMD and food insecurity
The percentage of respondents reporting severe household food insecurity was 32.5% for people with SMD and 15.9% for the control households. The median HFIAS score was higher for people with SMD (median 15, IQR 10) compared with control households (median 12, IQR 7) (P < 0.001).
In keeping with the hypothesis, SMD was associated with severe food insecurity (adjusted OR = 2.82; 95% CI 1.62, 4.91) after adjustment for potential confounders (Table 2). Higher annual income was found to be associated independently with lower odds of food insecurity. There was no difference in the findings when the food insecurity score was categorised as no/mild food insecurity v. moderate/severe food insecurity (see Supplementary File 3).
Table 2.
Crude and adjusted model for association between severe mental disorder and severe food insecurity
| Dependent variable: severe food insecurity | ||
|---|---|---|
| Characteristics | Crude odds ratio (95% confidence interval) | Adjusted odds ratio (95% confidence interval) (n = 556) |
| Person with SMD | 2.56 (1.71, 3.83) | 2.82 (1.62, 4.91) |
| Male Sex | 1.46 (0.98, 2.15) | 1.12 (0.71, 1.78) |
| Age (in years) | 0.99 (0.98, 1.01) | 1.01 (0.99, 1.03) |
| Urban residence | 0.88 (0.55, 1.42) | 0.73 (0.43, 1.25) |
| Able to read and write | 0.78 (0.47, 1.31) | 1.01 (0.56, 1.81) |
| Formal education | 0.69 (0.45, 1.07) | 0.84 (0.49, 1.43) |
| Current household head | 0.67 (0.45, 0.99) | 1.06 (0.61, 1.85) |
| Annual income | 0.99 (0.99, 0.99) | 0.99 (0.99, 0.99) |
| Number of dependents | 0.90 (0.81, 1.01) | 1.07 (0.93, 1.22) |
| Any long-term illness | 1.56 (0.98, 2.28) | 1.34 (0.85,2.12) |
| Month of assessment | 0.94 (0.87, 1.01) | 0.98 (0.91, 1.06) |
SMD: severe mental disorder.
Exploring mediation
After including total WHODAS 12.0 score in the multivariable model with food insecurity as the dependent variable, the association between SMD and food insecurity became non-significant, indicating the probable mediating role of disability in this relationship. Annual income remained associated significantly with food insecurity even after including disability within the model (Supplementary File 4).
Factors associated with disability
In the multivariable model, having SMD and increasing age were associated with increased disability, whereas formal education and current household head position were associated with lower disability (Table 3).
Table 3.
Crude and adjusted models for factors associated with disability score
| Characteristics | WHODAS 12.0 crude multiplier value (95% CI) | WHODAS 12.0 adjusted multiplier value (95% CI) (n = 559) |
|---|---|---|
| Age (years) | 0.99 (0.98, 0.99) | 1.01 (1.00, 1.01) |
| Sex (male) | 1.14 (0.96, 1.34) | 1.08 (0.95, 1.23) |
| Residence (urban) | 1.02 (0.83, 1.25) | 1.04 (0.89, 1.21) |
| Education (formal) | 0.93 (0.85, 1.02) | 0.91 (0.84, 0.98) |
| Currently household head | * | 0.71 (0.61, 0.83) |
| Number of dependents | 0.95 (0.91, 0.99) | 0.98 (0.94, 1.02) |
| Person with SMD | 3.30 (2.89, 3.77) | 3.36 (2.83, 3.99) |
| Annual income | 0.99 (0.99, 0.99) | 0.99 (0.99, 1.00) |
SMD: severe mental disorder; WHODAS: World Health Organisation Disability Assessment Schedule.
Fitting constant-only model; long iteration output.
Discussion
In this community-based study conducted in rural Ethiopia, severe food insecurity and disability were increased significantly among people with SMD compared with general population controls, in support of our hypothesis.
The prevalence of severe food insecurity was more than twice as high in households with a member living with SMD compared with households from the general population, which is in keeping with the findings from a small study from the USA (Goetz, 2008) and a facility-based case–control study from India (Trani et al. 2016). SMD was associated with household food insecurity independently of household annual income. In this subsistence farming community, food insecurity is related to the amount of food available due to household production and not just to income. In addition to the impact of disability of the person with SMD, the opportunity costs of other household members due to engagement in caregiving activities and direct reductions in productivity of caregivers are likely to contribute to an overall decrease in household productivity (Flyckt et al. 2011). In a qualitative study from the same area, respondents conceptualised disability in people with SMD as arising from a combination of direct effects of the illness, poverty and stigma (Habtamu et al. 2015). Stigma and discrimination extends beyond the individual person with SMD to affect the whole household (Shibre et al. 2001), which may lead to decreased co-operation with community members for key farming activities and resultant decrease in food production.
Ethiopia is reported to have well-established and strong programmes to address the food security needs of vulnerable groups (Combaz, 2013; Endalew et al. 2015). In the Productive Safety Net Programme, rural households facing chronic food insecurity are supported to resist financial shocks, create assets and become food self-sufficient by providing predictable transfers, as food, cash or a combination of both (Ministry of Agriculture & Rural Development, 2009; Endalew et al. 2015; World Food Program, 2016) conditional upon engagement in daily labouring activities. Households of people who are ‘chronically sick, disabled or mentally challenged in such a way as to prevent them from undertaking work’ are explicitly excluded from this scheme but considered eligible for permanent direct support and the possibility of linkages to appropriate social services, where capacity exists at the district level (Ministry of Agriculture, 2014); however, the extent to which households with a person with SMD are able to access this support is unknown and likely to be low. As well as the prevailing low levels of awareness about mental health and illness, the stigma and social exclusion associated with SMD (Shibre et al. 2001) are likely to act as barriers to participation in interventions to address food insecurity.
The consequences of exposure to food insecurity in people with SMD in this setting may be profound. A previous study found that people with SMD in a rural Ethiopian district were more likely to be undernourished compared with community controls (Lijalem, 2002). Excess mortality in people with SMD in Ethiopia has been linked to undernutrition (Fekadu et al. 2015). Food insecurity is likely to also affect access to, and engagement with, care. In a qualitative study of people with SMD and their caregivers in a food-insecure area, justification for ongoing use of khat (chewing leaves containing the amphetamine-like substance cathinone) against medical advice was in part to curb one's appetite even though there was awareness that it could worsen the person's mental health (Teferra, 2011). Formative work indicated the need for interventions to address basic needs, including food security, among people with SMD in Ethiopia to ensure equitable access to care (Hailemariam et al. 2016; Mall et al. 2017).
Our findings suggest that interventions to address food insecurity need to include both expanded access to mental health care (to reduce disability) and strategies to alleviate poverty, particularly for vulnerable individuals living with SMD. Through the PRIME project, and in keeping with the policy of the Federal Ministry of Health of Ethiopia, access to mental health care is being increased through integration into PHC in this district (Fekadu et al. 2016). Although there is an emphasis on community mobilisation in the PRIME Ethiopia plan, at the individual level the intervention is mostly centred on facility-based treatment and, specifically, on psychotropic medication combined with provision of information (‘psychoeducation’). An evaluation of the BasicNeeds model of providing development interventions (e.g. income-generating activities and interventions to promote sustainable livelihoods) alongside mental health care (BasicNeeds, 2008; Raja et al. 2012) found improved economic status in people with SMD (Lund et al. 2013); however, the study design could not distinguish the effects of mental health care alone from any added value of development interventions. Within PRIME, planned follow-up assessments after 12 months of the new integrated service will help to answer the question of whether treatment alone is sufficient to address indicators of poverty in general, and food insecurity in particular. A community-based rehabilitation (CBR) intervention trial for people with schizophrenia is also underway in Ethiopia (Asher et al. 2016). The CBR model includes facility-based treatment, home-based sessions from community workers and community mobilisation. The goal of CBR is to promote restoration of functioning and recovery which is expected to translate into improved social inclusion, economic status and food security. The findings will show whether such an intensive intervention yields dividends over and above the PRIME service.
There were limitations of our study. Although the HFIAS is a household measure, the information for the ‘case’ group was provided by the person with SMD. It is possible that they reported higher food insecurity levels than other household members due to less access to household resources than other household members or that they experienced greater hunger due to appetite-stimulating effects of antipsychotic medication (Teferra et al. 2013); however, only a third (35.0%) of people with SMD were taking psychotropic medication at the time of assessment so this is unlikely to be the full explanation. Furthermore, the HFIAS is designed to capture household-level information regardless of the respondent. Respondents may have given affirmative responses in the expectation that they would receive some kind of aid, although this would have applied to both case and comparison groups. Social desirability could also have led to minimisation of the true experience of food insecurity due to the sensitivity of the topic. There may have been inadequate adjustment for seasonal variation in food insecurity. Strengths of the study include the use of a culturally validated measure of food insecurity, use of standardised diagnostic assessment by mental health specialists to define SMD, the large sample size and the community-based ascertainment of cases which reduces the risk of selection bias.
Conclusions
People with SMD living in a rural Ethiopian district experienced higher levels of severe food insecurity than the general population. The inclusion and prioritisation of people with SMD in food security programmes and development opportunities, including income-generating opportunities and schemes should be ensured. This requires awareness-raising and tackling the stigma, which undermines inclusion of people with SMD. Increasing access to holistic mental health care is also expected to reduce food insecurity through a reduction in the disability associated with mental illness.
Acknowledgements
The authors sincerely thank their respondents, data collectors, field supervisors, psychiatric nurses and the Sodo district health centre staff.
Ethical Considerations
Ethical approval was obtained from the College of Health Sciences Institutional Review Board, Addis Ababa University (Ref. 026/15/Psy). Written informed consent was obtained from literate participants. For non-literate respondents, verbal consent was accompanied by a finger print in the presence of a literate witness. All participants with SMD were offered mental health care through the PRIME project. For people with SMD who lacked capacity to consent and were not refusing participation, caregiver permission was obtained.
Availability of Data and Materials
The data are being used for a PhD student (KT) for his thesis and are not, therefore, available at the present time to the general public. The data may be requested from the corresponding author for verification of the analyses in this paper.
Footnotes
Financial Support
This study is a direct output of the PRogramme for Improving Mental health carE (PRIME). This work was supported by the UK Department for International Development [201446]. The views expressed do not necessarily reflect the UK Government's official policies. Research leading to these results was also funded by the European Union's Seventh Framework Programme (FP7/2007-2013) under grant agreement no. 305968 as part of the Emerald project (Emerging mental health systems in low- and middle-income countries).
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/S2045796017000701.
click here to view supplementary material
Conflict of Interest
None.
References
- Asher L, De-Silva M, Hanlon C, Weiss HA, Birhane R, Medhin G, Ejigu DA, Patel V, Fekadu A (2016). Community-based Rehabilitation Intervention for people with Schizophrenia in Ethiopia (RISE): study protocol for a cluster randomised controlled trial. Trials 17, 299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Azevedo MH, Soares MJ, Coelho I, Dourado A, Valente J, Macedo A, Pato M, Pato C (1999). Using consensus OPCRIT diagnoses. An efficient procedure for best-estimate lifetime diagnoses. British Journal of Psychiatry 175, 154–157. [DOI] [PubMed] [Google Scholar]
- BasicNeeds (2008). Mental Health and Development: A Model in Practice. Leamington Spa: BasicNeeds. [Google Scholar]
- Coates J, Swindale A, Bilinsky P (2007). Household Food Insecurity Access Scale (HFIAS) for Measurement of Food Access: Indicator Guide. Food and Nutrition Technical Assistance (FANTA) project. United States Agency for International Development: Washington, DC. [Google Scholar]
- Cole S, Tembo G (2011). The effect of food insecurity on mental health: panel evidence from rural Zambia. Social Science and Medicine 73, 1071–1079. [DOI] [PubMed] [Google Scholar]
- Collins L (2005). The impact of food insecurity on women's mental health. Journal of the Association for Research on Mothering 11, 251–262. [Google Scholar]
- Combaz E (2013). Social inclusion in productive safety net programmes. Help Desk Research Report. GSDRC, Applied Knowledge Services.
- Dua T, Barbui C, Clark N, Fleischmann A, Poznyak V, van-Ommeren M, Taghi Yasamy MT, Ayuso- Mateos JL, Birbeck GL, Drummond C, Freeman M, Giannakopoulos P, Levav I, Obot IS, Omigbodun O, Patel V, Phillips M, Prince M, Rahimi-Movaghar A, Rahman A, Sander JW, Saunders JB, Servili C, Rangaswamy T, Unützer J, Ventevogel P, Vijayakumar L, Thornicroft G, Saxena S (2011). Evidence-based guidelines for mental, neurological, and substance use disorders in low- and middle-income countries: summary of WHO recommendations. PLoS Medicine 8, e1001122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Endalew B, Muche M, Tadesse S (2015). Assessment of food security situation in Ethiopia. World Journal of Dairy and Food Sciences 10, 37–43. [Google Scholar]
- Fekadu A, Medhin G, Selamu M, Hailemariam M, Alem A, Breuer E, Lund C, Prince M, Hanlon C (2014). Population level mental distress in rural Ethiopia. BMC Psychiatry 14, 194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fekadu A, Medhin G, Kebede D, Alem A, Cleare AJ, Prince M, Hanlon C, Shibre T (2015). Excess mortality in severe mental illness: 10-year population-based cohort study in rural Ethiopia. British Journal of Psychiatry 206, 289–296. [DOI] [PubMed] [Google Scholar]
- Fekadu A, Hanlon C, Medhin G, Alem A, Selamu M, Welde-Giorgis T, Shibre T, Teferra S, Tegegn T, Breuer E, Patel V, Tomlinson M, Thornicroft G, Prince M, Lund C (2016). Development of a scalable mental healthcare plan for a rural district in Ethiopia. British Journal of Psychiatry 208, s4–s12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flyckt L, Lothman A, Jorgenson L, Rylander A, Koering T (2011). Burden of informal caregiving to patients with psychosis: a descriptive and methodological study. International Journal of Social Psychiatry 59, 137–146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gebreyesus SH, Lunde T, HaileMariam D, Woldehanna T, Lindtjørn B (2015). Is the adapted Household Food Insecurity Access Scale (HFIAS) developed internationally to measure food insecurity valid in urban and rural households of Ethiopia? BMC Nutrition 1, 2. [Google Scholar]
- Goetz JR (2008). Exploring food insecurity among individuals with serious mental illness: a qualitative study. Ph.D. Thesis, University of Kansas, Kansas, USA. [Google Scholar]
- Habtamu K, Alem A, Hanlon C (2015). Conceptualizing and contextualizing functioning in people with severe mental disorders in rural Ethiopia: a qualitative study. BMC Psychiatry 15, 34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Habtamu K, Alem A, Medhin G, Fekadu A, Dewey M, Prince M, Hanlon C (2017). Validation of the World Health Organization Disability Assessment Schedule in people with severe mental disorders in rural Ethiopia. Health and Quality of Life Outcomes 15, 64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hadley C, Patil C (2006). Food insecurity in rural Tanzania is associated with maternal anxiety and depression. American Journal of Human Biology 18, 359–368. [DOI] [PubMed] [Google Scholar]
- Hadley C, Tegegn A, Tessema F, Cowan JA, Asefa M, Galea S (2008). Food insecurity, stressful life events and symptoms of anxiety and depression in east Africa: evidence from the Gilgel Gibe growth and development study. Journal of Epidemiology and Community Health 62, 980–986. [DOI] [PubMed] [Google Scholar]
- Hailemariam M, Fekadu A, Selamu M, Medhin G, Prince M, Hanlon C (2016). Equitable access to integrated primary mental healthcare for people with severe mental disorders in Ethiopia: a formative study. International Journal for Equity in Health 15, 121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jebena M, Taha M, Nakajima M, Lemieux A, Lemessa F, Hoffman R, Tesfaye M, Tefera Belachew T, Workineh N, Kebede E, Tariku Y, Segni H, Kolsteren P, al'Absi M (2015). Household food insecurity and mental distress among pregnant women in southwestern Ethiopia: a cross-sectional study design. BMC Pregnancy and Childbirth 15, 250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kempson KM, Keenan DP, Sadani PS, Ridlen S, Rosato NS (2002). Food management practices used by people with limited resources to maintain food sufficiency as reported by nutrition educators. Journal of the American Dietetic Association 102, 1795–1799. [DOI] [PubMed] [Google Scholar]
- Lauritsen JM, Bruus M (2003. –2008). EpiData (version 3). A comprehensive tool for validated entry and documentation of data (ed. T. E. Association): Odense, Denmark.
- Lijalem M (2002). Assessment of nutritional status of people with major mental disorders and their controls in Meskan and Marako District (Butajira), Ethiopia. MSc Thesis, Addis Ababa University, Addis Ababa, Ethiopia. [Google Scholar]
- Lund C, Breen A, Flisher AJ, Kakuma R, Corrigall J, Joska JA, Swartz L, Patel V (2010). Poverty and common mental disorders in low and middle income countries: a systematic review. Social Science and Medicine 71, 517–528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lund C, Tomlinson M, De-Silva M, Fekadu A, Shidhaye R, Jordans M, Petersen I, Bhana A, Kigozi F, Prince M, Thornicroft G, Hanlon C, Kakuma R, McDaid D, Saxena S, Chisholm D, Raja S, Kippen-Wood S, Honikman S, Fairall L, Patel V (2012). PRIME: a programme to reduce the treatment gap for mental disorders in five low- and middle-income countries. PLoS Medicine 9, e1001359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lund C, Waruguru M, Kingori J, Kippen-Wood S, Breuer E, Mannarath S, Raja S (2013). Outcomes of the mental health and development model in rural Kenya: a 2-year prospective cohort intervention study. International Health 5, 43–50. [DOI] [PubMed] [Google Scholar]
- Maes K, Hadley C, Tesfaye F, Shifferaw S (2010). Food insecurity and mental health: surprising trends among community health volunteers in Addis Ababa, Ethiopia during the 2008 food crisis. Social Science and Medicine 70, 1450–1457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mall S, Hailemariam M, Selamu M, Fekadu A, Lund C, Patel V, Petersen I, Hanlon C (2017). ‘Restoring the person's life’: a qualitative study to inform development of care for people with severe mental disorders in rural Ethiopia. Epidemiology and Psychiatric Sciences 26, 43–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGuffin P, Farmer AE, Harvey I (1991). A polydiagnostic application of operational criteria in studies of psychotic illness: development and reliability of the OPCRIT system. Archives of General Psychiatry 48, 764–770. [DOI] [PubMed] [Google Scholar]
- Mengistu E, Regassa N, Yusufe A (2009). The Levels, Determinants and Coping Mechanisms of Food Insecure Households in Southern Ethiopia: Case Study of Sidama, Wolaita and Guraghe Zones. DCG Report No. 55.
- Ministry of Agriculture (2014). Productive Safety Net Programme, Phase IV Programme Implementation Manual. 1.0.
- Ministry of Agriculture and Rural Development (2009). Food Security Programme 2010–2014: Productive Safety Net. Addis Ababa. [Google Scholar]
- Muldoon K, Duff P, Fielden SJ, Anema A (2013). Food insufficiency is associated with psychiatric morbidity in a nationally representative study of mental illness among food insecure Canadians. Social Psychiatry and Psychiatric Epidemiology 48, 795–803. [DOI] [PubMed] [Google Scholar]
- Operational Criteria for Research (2004). Opcrit for Windows (v4), Item Checklist. Retrieved 14th January 2014 from sgdp.iop.kcl.ac.uk/opcrit/checklist.pdf.
- Raja S, Underhill C, Shrestha P, Sunder U, Mannarath S, Kippen-Wood S, Patel V (2012). Integrating mental health and development: a case study of the basic needs model in Nepal. PLoS Medicine 9, e1001261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Regassa N, Stoecker BJ (2011). Household food insecurity and hunger among households in Sidama district, Southern Ethiopia. Public Health Nutrition 15, 1276–1283. [DOI] [PubMed] [Google Scholar]
- Semrau M, Evans-Lacko S, Alem A, Ayuso-Mateos JL, Chisholm D, Gureje O, Hanlon C, Jordans M, Thornicroft G (2015). Strengthening mental health systems in low- and middle-income countries: the Emerald programme. BMC Medicine 13, 79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shibre T, Negash A, Kullgren G, Kebede D, Alem A, Fekadu A, Fekadu D, Medhin G, Jacobsson L (2001). Perception of stigma among family members of individuals with schizophrenia and major affective disorders in rural Ethiopia. Social Psychiatry and Psychiatric Epidemiology 36, 299–303. [DOI] [PubMed] [Google Scholar]
- Shibre T, Kebede D, Alem A, Negash A, Kibreab S, Fekadu A, Fekadu D, Jacobsson J, Kullgren G (2002). An evaluation of two screening methods to identify cases with schizophrenia and affective disorders in a community survey in rural Ethiopia. International Journal of Social Psychiatry 48, 200–208. [DOI] [PubMed] [Google Scholar]
- Sorsdahl K, Slopen N, Siefert K, Seedat S, Stein DJ, Williams DR (2009). Household food insufficiency and mental health in South Africa. Journal of Epidemiology and Community Health 65, 426e–431e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- StataCorp (1985. –2013). STATA/SE 13.1. statacorp, college station, Texas USA.
- Swindale A, Bilinsky P (2006). Development of a universally applicable household food insecurity measurement tool: process, current status, and outstanding issues. Journal of Nutrition 136, 1449S-1452S. [DOI] [PubMed] [Google Scholar]
- Teferra S (2011). Studies on psychotic disorders in rural Ethiopia. Umeå University Medical Dissertations. New Series No 1427.
- Teferra S, Hanlon C, Beyero T, Jacobsson L, Shibre T (2013). Perspectives on reasons for non-adherence to medication in persons with schizophrenia in Ethiopia: a qualitative study of patients, caregivers and health workers. BMC Psychiatry 13, 168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trani J-S, Venkataraman H, Mishra N, Groce NE, Jadhav S, Deshpande S (2016). Mental illness, poverty and stigma in India: a case–control study. BMJ Open 5, e006355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United Nations (2015). Sustainable Development Goals: 17 Goals to transform the world. Retrieved 23 October 2016 from http://www.un.org/sustainabledevelopment/hunger/.
- United States Department of Agriculture Economic Research Service (2016). Definitions of Food Security. Retrieved 12 January 2017 from https://www.ers.usda.gov/topics/food-nutrition-assistance/food-security-in-the-us/definitions-of-food-security.aspx.
- Ustün TB, Chatterji S, Kostanjsek N, Rehm J, Kennedy C, Epping-Jordan J, Saxena S, von-Korff M, Pull C (2010). Developing the World Health Organization Disability Assessment Schedule 2.0. Bulletin of the World Health Organization 88, 815–823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams J, Farmer AE, Ackenheil M, Kaufmann CA, McGuffin P (1996). A multicentre inter-rater reliability study using the OPCRIT computerized diagnostic system. Psychological Medicine 26, 775–783. [DOI] [PubMed] [Google Scholar]
- World Food Program (2016). Productive safety net program (PSNP): Ethiopia. Retrieved 29 November 2016 from https://www.wfp.org/sites/default/files/PSNP%20Factsheet.pdf.
- World Health Organisation (1985). World Health Organisation Disability Assessment Schedule. WHO: Geneva. [Google Scholar]
- World Health Organisation (2008). WHO mhGAP: Mental Health Gap Action Programme: Scaling Up Care for Mental, Neurological and Substance use Disorders. WHO: Geneva. [PubMed] [Google Scholar]
- World Health Organisation (2013). WHO Study on Global Ageing and Adult Health (SAGE). WHO: Geneva. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiong W, Philips M, Hu X, Wang R, Dai Q, Kleinman J, Kleinman A (1994). Family-based intervention for schizophrenia patients in China: a randomized control trial. British Journal of Psychiatry 165, 239–247. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
For supplementary material accompanying this paper visit https://doi.org/10.1017/S2045796017000701.
click here to view supplementary material
Data Availability Statement
The data are being used for a PhD student (KT) for his thesis and are not, therefore, available at the present time to the general public. The data may be requested from the corresponding author for verification of the analyses in this paper.