Abstract
Aims.
Public controversy regarding the potential overdiagnosis and overmedication of children with attention-deficit/hyperactivity disorder (ADHD) has continued for decades. This study used the National Health Insurance Research Database of Taiwan (NHIRD-TW) to explore trends in ADHD diagnosis in youths and the proportion of those receiving medication, with the aim of determining whether ADHD is overdiagnosed and overmedicated in Taiwan.
Method.
Youths (age ≤18 years) who had at least two NHIRD-TW claims records with ADHD diagnosis between January 2000 and December 2011 were selected as the subject cohort. In total, the study sample comprised 145 018 patients with ADHD (mean age at a diagnosis of ADHD: 7.7 ± 3.1 years; 21.4% females). The number of cases of ADHD were calculated annually for each year (from 2000 to 2011), and the number of cases per year who received medication was determined as those with at least one record of pharmacotherapy (immediate-release methylphenidate, osmotic controlled-release formulation of methylphenidate, and atomoxetine) in each year.
Results.
The prevalence rates of a diagnosis of ADHD in the youths ranged from 0.11% in 2000 to 1.24% in 2011. Compared with children under 6 years of age, the ADHD diagnosis rates in children aged between 7 and 12 years (ratio of prevalence rates = 4.36) and in those aged between 13 and 18 years (ratio of prevalence rates = 1.42) were significantly higher during the study period. The prevalence in males was higher than that in females (ratio of prevalence rates = 4.09). Among the youths with ADHD, 50.2% received medications in 2000 compared with 61.0% in 2011. The probability of receiving ADHD medication increased with age. More male ADHD patients received medications that females patients (ratio of prevalence rates = 1.16).
Conclusions.
The rate of ADHD diagnosis was far lower than the prevalence rate (7.5%) identified in a previous community study using face-to-face interviews. Approximately 40–50% of the youths with ADHD did not receive any medications. These findings are not consistent with a systematic public opinion about overdiagnosis or overmedication of ADHD in Taiwan.
Key words: ADHD, diagnosis, epidemiology, pharmacotherapy, prevalence
Introduction
Attention-deficit/hyperactivity disorder (ADHD) encompasses symptoms, including inattention, hyperactivity and impulsivity, and is a common neurodevelopmental disorder in childhood (Feldman & Reiff, 2014; Thapar & Cooper, 2016). Previous systematic reviews and metaregression analyses have revealed that the prevalence of ADHD worldwide ranges from 5.3 to 7.2% (Polanczyk et al. 2007; Thomas et al. 2015), and that these rates were not affected by geographical location or year of the study (Polanczyk et al. 2014). A community study in Taiwan reported that ADHD affects approximately 7.5% of school-aged children (Gau et al. 2005). Various psychosocial interventions, such as behavioural, cognitive behavioural and parenting skills training strategies, represent evidence-based approaches for managing ADHD (Evans et al. 2014; Chan et al. 2016). Nevertheless, pharmacotherapy has been consistently used as the primary and most effective therapeutic option for ADHD (Findling, 2008; Vaughan et al. 2012). Although various studies have provided robust evidence with regards to the epidemiology and effectiveness of ADHD pharmacotherapy, public controversy related to the potential overdiagnosis and overmedication of children with ADHD remains (Sciutto & Eisenberg, 2007; Partridge et al. 2012; Rapoport, 2013).
The conception of overdiagnosis of ADHD typically refers to that too many children are diagnosed with ADHD when they do not really have it (false positives) (Sciutto & Eisenberg, 2007). In a survey of public attitude towards the diagnosis and treatment of ADHD, 78.3% of respondents thought that ADHD has been overdiagnosed (Partridge et al. 2014). A recent article questioned whether immaturity leads to a misdiagnosis of ADHD, and whether overdiagnosis may be harmful for the children (Coon et al. 2014). Another study suggested that clinicians do not adhere strictly to diagnostic manuals, and that ADHD is routinely overdiagnosed (Bruchmuller et al. 2012). In epidemiological studies, the rates of being diagnosed with ADHD increased across different geographical areas, such as the United States (USA) (Garfield et al. 2012; Getahun et al. 2013; Visser et al. 2014), the United Kingdom (UK) (Holden et al. 2013), Denmark (Mohr Jensen & Steinhausen, 2015), Western Australia (Atladottir et al. 2015), Korea (Hong et al. 2014) and also in Taiwan (Chien et al. 2012; Huang et al. 2014). However, previous studies in Taiwan have used claims data before 2005, and it is unclear how the rate of a diagnosis of ADHD has changed in recent years. Investigating the current rates of ADHD diagnosis among the general population is essential for determining whether identification of ADHD is consistent with the prevalence rate of ADHD estimated using a standardised interview (Gau et al. 2005).
The empirical definition of overmedication is either when medications are prescribed unnecessarily, when they are continued although not measurably respond, or when they are more of risk than a benefit (Safer, 2000). Public concern that youths with ADHD have been overmedicated has continued for decades (Rapoport, 2013). Criticisms with regards the overmedication of ADHD are generally based on two perspectives: drastic increases in prescriptions of ADHD medications, and the high proportion of ADHD patients receiving drug therapy (Safer, 2000). Rapid increases have been reported in the prescription of ADHD medications in a number of countries (Safer et al. 1996; Hodgkins et al. 2011; Treceno et al. 2012; Oner et al. 2014; Ponizovsky et al. 2014; Stuhec et al. 2015) including Taiwan, where the prevalence rates of ADHD and the use of medications in children diagnosed with ADHD have increased from 1997 to 2005 (Chien et al. 2012). Two studies conducted in the USA reported that 8–10% of school-aged students receive ADHD medications, and that this exceeded the expected rate of ADHD (LeFever et al. 1999; Rowland et al. 2002). In addition, a national survey in the USA indicated that the pharmacotherapy was used as treatment for ADHD in 93–96% of medical visits (Garfield et al. 2012). These studies suggest that ADHD is potentially overmedicated in children in the USA. However, little is known about the trends in prescriptions of ADHD medications in Taiwan after 2005, and whether ADHD is overmedicated in Taiwan warrants investigation.
Reimbursement data are ideal to explore the nationwide utilisation of medical services. Therefore, we used national population-based data from 2000 to 2011 to analyse trends in the diagnosis rate of ADHD and the proportion of patients receiving medications. We looked into the possibility of overdiagnosis and overmedication for ADHD by comparing the results of the present study with those of the epidemiological study on the prevalence rate of ADHD in Taiwan and the previous studies in other countries.
Methods
Data source
The Institutional Review Board of Chang Gung Memorial Hospital approved this study. Data were obtained from the National Health Insurance Research Database of Taiwan (NHIRD-TW), an ambulatory claims database. Initiated in Taiwan in 1995, the National Health Insurance (NHI) programme is a compulsory universal health insurance programme, with the Bureau of NHI as the sole payer of healthcare services. The Bureau of NHI has contracted 93% of all healthcare providers in Taiwan, and at least 96% of insured people have benefitted from healthcare services provided by one of the contracted hospitals or clinics at least once since 1995. These medical care institutions are required to electronically submit monthly medical expense-related claims documents, including the patients’ demographic data, the medical institution visited, diagnostic codes, dates of any prescriptions, drugs prescribed and all claimed medical expenses. The database of this programme contains registration files and original claim data for reimbursement. Large computerised databases derived from this system are maintained by the National Health Research Institutes, Taiwan, and are provided as NHIRD-TW to scientists in Taiwan for research purposes. The NHIRD-TW has previously been validated to be an effective resource for population-based research (Wu et al. 2014).
Definition of ADHD and ADHD diagnosis rates
We recruited all youths (age ≤18 years) from the NHIRD-TW who were diagnosed with ADHD from January 2000 to December 2011. In order to minimise possible cases of misdiagnosis, ADHD was defined as at least two NHIRD-TW claims records with the International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) code 314.X. Our study sample included 145 018 patients with ADHD (mean age at a diagnosis of ADHD: 7.7 ± 3.1 years; 21.4% females).
Cases of ADHD were determined annually as those with at least one NHIRD-TW claims record with a diagnosis of ADHD within the specific year (from 2000 to 2011). The annual ADHD diagnosis (prevalence) rates (per 100 000) were then determined by dividing the annual number of ADHD cases by the total population during each year. Data on the general population in Taiwan was obtained from the Executive Yuan, Taiwan (Directorate-General of Budget Accounting and Statistics, 2015). The distribution of the total population in each age group is listed in the Supplementary Table.
Definition of ADHD medication
ADHD medications were defined according to the Anatomical Therapeutic Chemical classification system. According to the Food and Drug Administration of Taiwan, only three drugs were licensed to treat ADHD prior to 2011: immediate-release methylphenidate (IR-MPH), osmotic controlled-release formulation of methylphenidate (OROS-MPH) and atomoxetine (ATX). All prescriptions for these three medications were recorded in an ambulatory care claim, pharmacy claim or hospital care claim.
The annual number of cases who received ADHD medication was defined as the number of youths with ADHD with at least one record of pharmacotherapy (IR-MPH, OROS-MPH or ATX) in each year. The proportion of ADHD youths receiving medications was determined by dividing the annual number of cases who received ADHD medications by the total number of ADHD patients in the entire study sample each year. We also calculated the annual prevalence rates of the use of ADHD medications among the whole population (per 100 000) by dividing the annual number of cases who used ADHD medications by the total population each year.
Statistical analysis
The Statistical Package for Social Sciences (SPSS) version 20.0 (SPSS Inc., Chicago, IL, USA) was used for all statistical analyses. A two-tailed p value of <0.05 was taken to indicate statistical significance.
In order to investigate the potential effect of age on the rates of a diagnosis of ADHD and the use of medication, we categorised the age of the patients into the following three groups: (1) preschoolers (≤6 years); (2) school-aged children (7–12 years); and (3) adolescents (13–18 years). A general linear model was used to evaluate trends with regard to the annual number of cases of ADHD, annual ADHD diagnosis rates, those receiving pharmacotherapy, annual proportion of those treated with medications and annual prevalence rates of using ADHD medications.
To assess the rates of a diagnosis of ADHD and the use of medications between years, age groups and gender, the ratios of prevalence rates and 95% confidence intervals (CI) were also calculated. A generalised estimating equations (GEE) model with the maximum-likelihood estimation method and auto-regression covariance matrix was used to examine differences in the prevalence of ADHD and medication use between years, age groups and gender. Autoregressive covariance matrix of GEE model is usually applied for longitudinal data analysis (Liang & Zeger, 1986).
Results
ADHD diagnosis rates
The annual ADHD diagnosis rate among the study cohort increased from 0.11% in 2000 to 1.24% in 2011 (10.8-fold increase, t = 20.98, p < 0.001) (Table 1). For the preschool children (age ≤6 years), the annual ADHD diagnosis rate increased from 0.07% in 2000 to 0.38% in 2011 (5.7-fold increase, t = 18.57, p < 0.001), compared with 0.24% in 2000 to 2.23% in 2011 (9.4-fold increase, t = 19.88, p < 0.001) in the school-aged children (7–12 years) and 0.04% in 2000 to 0.98% in 2011 (24.3-fold increase, t = 15.60, p < 0.001) in the adolescents (13–18 years).
Table 1.
Distribution of patients with a diagnosis of ADHD and annual prevalence rates from 2000 to 2011 in Taiwan
| Total (≤18 years) | ≤6 years | 7–12 years | 13–18 years | |||||
|---|---|---|---|---|---|---|---|---|
| Year | Case | Prev. | Case | Prev. | Case | Prev. | Case | Prev. |
| 2000 | 6637 | 114.8 | 1215 | 67.0 | 4604 | 237.7 | 818 | 40.3 |
| 2001 | 8920 | 157.5 | 1495 | 85.4 | 6198 | 317.8 | 1227 | 62.5 |
| 2002 | 12 167 | 219.4 | 1992 | 119.0 | 8362 | 431.6 | 1813 | 93.8 |
| 2003 | 14 609 | 269.0 | 2114 | 134.0 | 9976 | 514.1 | 2519 | 131.7 |
| 2004 | 20 031 | 374.8 | 3050 | 199.8 | 13 157 | 697.2 | 3824 | 198.0 |
| 2005 | 25 988 | 495.7 | 3471 | 239.3 | 16 880 | 915.7 | 5637 | 289.3 |
| 2006 | 31 682 | 633.4 | 3463 | 256.5 | 20 688 | 1132.5 | 7531 | 390.2 |
| 2007 | 40 042 | 784.0 | 4019 | 309.4 | 25 919 | 1473.5 | 10 104 | 519.7 |
| 2008 | 46 924 | 963.9 | 4379 | 349.2 | 29 674 | 1763.4 | 12 871 | 666.3 |
| 2009 | 51 137 | 1077.7 | 4705 | 385.4 | 31 436 | 1980.3 | 14 996 | 774.3 |
| 2010 | 53 460 | 1163.2 | 4871 | 415.4 | 32 422 | 2106.9 | 16 167 | 858.0 |
| 2011 | 55 212 | 1235.3 | 4453 | 382.5 | 32 718 | 2234.1 | 18 041 | 980.1 |
| Statistic value |
t = 21.47 p < 0.001 |
t = 20.98 p < 0.001 |
t = 12.67 p < 0.001 |
t = 18.57 p < 0.001 |
t = 18.85 p < 0.001 |
t = 19.88 p < 0.001 |
t = 16.10 p < 0.001 |
t = 15.60 p < 0.001 |
Note: Prev. (per 100 000): The annual prevalence rates of ADHD, in which the denominator is the total nationwide population and the numerator is the annual number of cases with a diagnosis of ADHD.
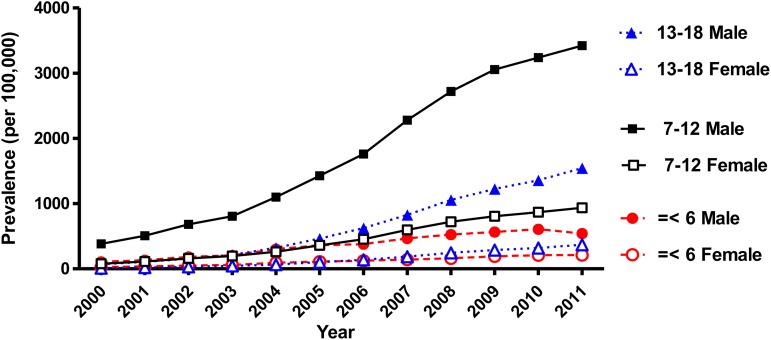
Figure 1 shows the annual ADHD diagnosis rates among the general population (per 100 000) stratified by age and gender from 2000 to 2011. The rates significantly increased in all age groups and in both genders during the study period. Compared with the ADHD diagnosis rates in the preschoolers (Table 3), the diagnosis rates in the school-aged children (ratio of prevalence rates = 4.36, Wald χ2 = 39.35, p < 0.001) and adolescents (ratio of prevalence rates = 1.42, Wald χ2 = 3.97, p = 0.046) were significantly higher during the study period. The prevalence in males was significantly higher than in females (ratio of prevalence rates = 4.09, Wald χ2 = 49.16, p < 0.001).
Fig. 1.
Annual prevalence of ADHD stratified by age and gender in Taiwan between 2000 and 2011. The Y-axis represents the prevalence of ADHD (per 100 000) in each year between 2000 and 2011. The ADHD prevalence rates significantly increased in all age groups and in both genders during the study period.
Table 3.
Generalised estimating equation models for the effects of age, gender and time on prevalence of ADHD and proportion of ADHD medication use from 2000 to 2011 in Taiwan
| ADHD prevalence | Proportion of ADHD drug therapy | |||||
|---|---|---|---|---|---|---|
| Characteristics | B (95% CI) | Wald χ2 | p-value | B (95% CI) | Wald χ2 | p-value |
| Age group | ||||||
| ≤6 years | Reference | Reference | ||||
| 7–12 years | 882.22 (606.57–1157.87) | 39.35 | <0.001 | 46.63 (44.66–48.60) | 2151.04 | <0.001 |
| 13–18 years | 166.84 (2.64–331.04) | 3.97 | 0.046 | 67.72 (65.47–69.96) | 3504.36 | <0.001 |
| Gender (male v. female) | 692.45 (498.88–886.02) | 49.16 | <0.001 | 4.77 (3.09–6.45) | 31.04 | <0.001 |
| Year | 106.27 (72.61–139.92) | 38.29 | <0.001 | 0.26 (−0.02 to 0.54) | 3.41 | 0.065 |
Note: Year was set as a continuous variable (range from 2000 to 2011).
Patients treated with ADHD medication
Among all patients with ADHD (Table 2), the proportion of those receiving ADHD medication increased from 50.2% in 2000 to 61.0% in 2011 (t = 16.02, p < 0.001). Among the preschoolers with ADHD, the proportion receiving ADHD medication significantly decreased from 14.3% in 2000 to 3.5% in 2011 (t = −25.43, p < 0.001), compared with an increase from 55.7% in 2000 to 57.8% in 2011 (t = 2.83, p = 0.018) in the school-aged children, and an increase from 72.4% in 2000 to 81.1% in 2011 (t = 6.76, p < 0.001) in the adolescents.
Table 2.
Distribution of youths with ADHD who received medications from 2000 to 2011 in Taiwan
| Total (≤18 years) | ≤6 years | 7–12 years | 13–18 years | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Year | Case | Prop. | Prev. | Case | Prop. | Prev. | Case | Prop. | Prev. | Case | Prop. | Prev. |
| 2000 | 3329 | 50.2 | 57.6 | 174 | 14.3 | 9.6 | 2563 | 55.7 | 132.3 | 592 | 72.4 | 29.2 |
| 2001 | 4473 | 50.1 | 79.0 | 199 | 13.3 | 11.4 | 3397 | 54.8 | 174.2 | 877 | 71.5 | 44.7 |
| 2002 | 6017 | 49.5 | 108.5 | 236 | 11.8 | 14.1 | 4512 | 54.0 | 232.9 | 1269 | 70.0 | 65.7 |
| 2003 | 7385 | 50.6 | 136.0 | 221 | 10.5 | 14.0 | 5351 | 53.6 | 275.8 | 1813 | 72.0 | 94.8 |
| 2004 | 10 196 | 50.9 | 190.8 | 324 | 10.6 | 21.2 | 7029 | 53.4 | 372.5 | 2843 | 74.3 | 147.2 |
| 2005 | 14 102 | 54.3 | 269.0 | 325 | 9.4 | 22.4 | 9455 | 56.0 | 512.9 | 4322 | 76.7 | 221.8 |
| 2006 | 18 361 | 58.0 | 367.1 | 314 | 9.1 | 23.3 | 12 020 | 58.1 | 658.0 | 6027 | 80.0 | 312.3 |
| 2007 | 24 187 | 60.4 | 473.6 | 287 | 7.1 | 22.1 | 15 731 | 60.7 | 894.3 | 8169 | 80.8 | 420.2 |
| 2008 | 29 445 | 62.8 | 604.8 | 294 | 6.7 | 23.4 | 18 462 | 62.2 | 1097.1 | 10 689 | 83.0 | 553.4 |
| 2009 | 31 858 | 62.3 | 671.4 | 289 | 6.1 | 23.7 | 19 208 | 61.1 | 1210.0 | 12 361 | 82.4 | 638.2 |
| 2010 | 31 801 | 59.5 | 692.0 | 247 | 5.1 | 21.1 | 18 482 | 57.0 | 1201.0 | 13 072 | 80.9 | 693.7 |
| 2011 | 33 698 | 61.0 | 754.0 | 157 | 3.5 | 13.5 | 18 903 | 57.8 | 1290.8 | 14 638 | 81.1 | 795.2 |
| Statistic value |
t = 16.02 p < 0.001 |
t = 6.97 p < 0.001 |
t = 16.32 p < 0.001 |
t = 0.60 p = 0.565 |
t = −25.43 p < 0.001 |
t = 2.30 p = 0.044 |
t = 18.85 p < 0.001 |
t = 2.83 p = 0.018 |
t = 15.40 p < 0.001 |
t = 14.90 p < 0.001 |
t = 6.76 p < 0.001 |
t = 14.66 p < 0.001 |
Note: Prop.: The proportion of youths with ADHD who received medication, in which the denominator is the annual number of ADHD patients and the numerator is the annual number of ADHD case who used ADHD medications. Prev. (per 100 000): The annual prevalence rates of ADHD medication use among the national population, in which the denominator is the total population and the numerator is the annual number of cases who used ADHD medications.
Among the total population under 18 years of age in Taiwan (Table 2), the prevalence of ADHD medication use increased from 0.06% in 2000 to 0.75% in 2011 (13.1-fold increase, t = 16.32, p < 0.001). For preschool children, the annual prevalence of ADHD medication use increased from 0.009% in 2000 to 0.013% in 2011 (1.4-fold increase, t = 2.30, p = 0.044), compared with an increase from 0.13% in 2000 to 1.29% in 2011 (9.8-fold increase, t = 15.40, p < 0.001) in school-aged children and an increase from 0.03% in 2000 to 0.80% in 2011 (27.2-fold increase, t = 14.66, p < 0.001) in adolescents.
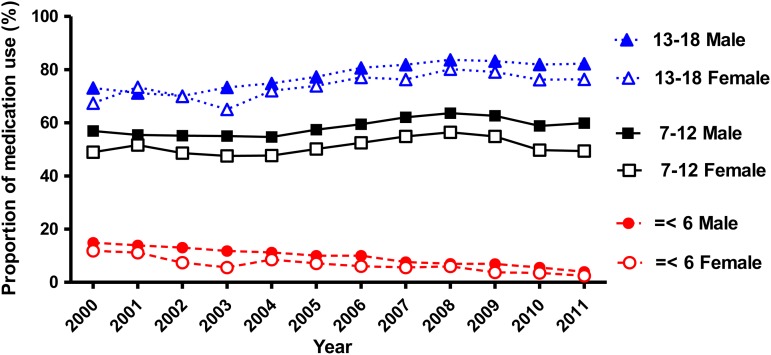
Figure 2 shows the proportions of medication use among the patients with ADHD in each age group and gender from 2000 to 2011. The proportion of ADHD medication use significantly increased in the school-aged children and adolescents, however it significantly decreased in the preschool children in both genders. Compared with the preschool patients (Table 3), the medication use in the school-aged children (ratio of prevalence rates = 7.54, Wald χ2 = 2151.04, p < 0.001) and adolescents (ratio of prevalence rates = 10.28, Wald χ2 = 3504.36, p < 0.001) was significantly higher during the study period. In addition, significantly more male ADHD patients received ADHD medications the female ADHD patients (ratio of prevalence rates = 1.16, Wald χ2 = 31.43, p < 0.001).
Fig. 2.
Proportion of medication use among the patients with ADHD in each age group and gender in Taiwan between 2000 and 2011. The Y-axis represents the proportion (%) of those receiving drug therapy among the patients with ADHD in each year between 2000 and 2011. The proportion of ADHD drugs use significantly increased in the patients aged 7–12 years and in those aged 13–18 years. The proportion of ADHD medication use significantly decreased in the patients under 6 years of age in both genders.
Discussion
The results of this study indicate that the number of youths being diagnosed with ADHD has increased over tenfold from 2000 to 2011. However, the prevalence rate of a diagnosis of ADHD was only 1.24% in 2011, which is still far lower than the prevalence rate reported in a previous community study using face-to-face interviews. Among the youths with ADHD, the proportion of those receiving ADHD medication increased from 50.2 to 61.0% during the study period. The likelihood of receiving ADHD medication was positively correlated with the patients’ age and gender. These findings do not support the overdiagnosis or overmedication of ADHD in youths in Taiwan.
Prevalence of ADHD and whether it is overdiagnosed
Similar to our findings, many time-trend surveys using diagnostic reports based on medical records have indicated that the prevalence of ADHD has increased worldwide (Chien et al. 2012; Garfield et al. 2012; Getahun et al. 2013; Holden et al. 2013; Hong et al. 2014; Huang et al. 2014; Visser et al. 2014; Atladottir et al. 2015; Mohr Jensen & Steinhausen, 2015). However, individuals with diagnostic records of ADHD only represent those who sought medical care, but not all patients with ADHD in the general population. Meta-analyses of epidemiological studies have reported that the prevalence of ADHD worldwide is between 5.3 and 7.2% (Polanczyk et al. 2007; Thomas et al. 2015), and these rates were not affected by the changes of diagnostic criteria from different versions of the Diagnostic and Statistical Manual of Mental Disorders, or geographical and chronological variations (Polanczyk et al. 2014). This implies that the prevalence rates of ADHD, determined by face-to-face assessments of community youths, had not changed significantly over time. Therefore, the ascending trend of numbers of patients being diagnosed with ADHD may only reflect the increase in patients seeking medical care, but should not be viewed as an increase of youths with ADHD (Safer, 2015).
The most reliable estimate of the prevalence of ADHD in Taiwan reported that ADHD affects 7.5% of school-aged children (Gau et al. 2005). Our results revealed that the proportion of patients with a diagnosis of ADHD increased from 0.11% in 2000 to 1.24% in 2011, which is far lower than the reported prevalence rate of 7.5%. We suggest this finding is not consistent with a public opinion about overdiagnosis of ADHD in Taiwan. Moreover, we speculate that a large number of patients who meet the criterions for ADHD do not seek medical care. In our survey, the number of individuals with a diagnosis of ADHD significantly increased over time and consistently across different age groups and in both genders. This implies that the increasing trend in the diagnosis of ADHD according to the medical records from the NHIRD-TW is due to increasing awareness about ADHD and increased access to psychiatric services.
We found that the prevalence of ADHD in males was approximately four times higher than in females. Gender differences in the prevalence of ADHD are well established (ratios of boys to girls range from 2 : 1 to 9 : 1) (Rucklidge, 2010; Nussbaum, 2012), and our national survey revealed compatible findings. With regards to the influence of age on the rates of a diagnosis of ADHD, we found that the rate was highest among school-aged children (7–12 years), followed by adolescents (13–18 years) and preschool children (age ≤6 years). These results are comparable with previous epidemiological studies, which revealed that the symptoms of ADHD are most prominent in school-aged children and that most require medical care (Holden et al. 2013; Huang et al. 2014). A possible explanation for this may be that the confirmation of a diagnosis of ADHD can be difficult in patients of a preschool age. The symptoms of ADHD decrease in around 50% of patients at puberty or in early adulthood (Cherkasova et al. 2013), and the likelihood of seeking medical care decreases with decreases in clinical manifestations.
Use of ADHD medication and whether youths are overmedicated in Taiwan
Significant increases in the number of patients receiving medications for ADHD have been reported in several countries in recent years (Safer et al. 1996; Hodgkins et al. 2011; Chien et al. 2012; Treceno et al. 2012; Oner et al. 2014; Ponizovsky et al. 2014; Visser et al. 2014; Stuhec et al. 2015), which is consistent with our findings. However, the higher number of patients receiving ADHD medication is naturally related to the higher number of patients diagnosed with ADHD. We found that the proportion of youths with a diagnosis of ADHD receiving medications (any prescription of IR-MPH, OROS-MPH or ATX for at least one dose) increased from 49.5 to 62.8% during the study period. This finding indicates that approximately 40–50% of patients were not prescribed with any medications during their medical visits in this study. Despite public controversy regarding the potential overmedication for ADHD has continued for decades, there are currently no guidelines to determine whether or not patients with ADHD are overmedicated. Empirically, the overuse or inappropriate use of ADHD medications is defined as when they are less effective than alternative interventions, when continued although not measurably useful, or when they are more of risk than a benefit (Safer, 2000). Because the clinical information about patients’ symptom severity and outcomes were unavailable in the NHIRD-TW, the appropriateness of the use of medications cannot be directly judged through the results of the current study.
Alternatively, we could compare the prevalence rates of ADHD medication use with those reported in other countries. Barbaresi et al. (2002) reported a prevalence rate of treatment with stimulants of 86.5% for children with a definite diagnosis of ADHD in the USA. Moreover, a national survey in the USA indicated that the proportion of visits in which pharmacotherapy was used as treatment ranged from 93 to 96% (Garfield et al. 2012). In a Danish cohort (Dalsgaard et al. 2013), 61% of ADHD patients were treated with ADHD medications, corresponding to a 0.82% prevalence rate of treatment in the total population. In a national survey in the UK (McCarthy et al. 2012), the prevalence of ADHD medication usage ranged from 0.48 to 0.92% among children aged 6–12 years. A study using the Medicaid database in the USA reported that the prevalence of ADHD drug use increased from 2.52% in 1995 to 4.63% in 2004 (Winterstein et al. 2008). Taken together, the prevalence of ADHD drug prescription seems to be higher in the USA than which in the European countries, and the prevalence of prescriptions for ADHD medications in Taiwan is not higher than that reported in other international studies. It is noteworthy that since pharmacotherapy has been suggested as the first-line treatment for ADHD (Barbaresi et al. 2007; Vaughan et al. 2012; Chan et al. 2016), the high rates of ADHD drug prescription (even as high as 100%) do not necessarily represent that ADHD youths are overmedicated. A future study which consists of comprehensive clinical information of a representative ADHD sample (e.g., severity of ADHD symptoms, treatment effects, adverse effects and patient outcomes) is warranted to determine the legitimate of the use of ADHD medications.
We found that the patients’ age significantly influenced the prescription rate of ADHD medication. The preschool patients had the lowest rate (under 15%), compared with 70–80% of the adolescent patients. It has been reported that parents of preschoolers with ADHD usually seek options other than pharmacotherapy first (e.g., psychosocial or rehabilitation treatment) (Lien et al. 2015). In contrast, older patients may have greater functional impairments and therefore a higher likelihood of being prescribed with medication (Morrow et al. 2012). Patients who respond well to medication may maintain such therapy as they grow (Chen et al. 2011). With regards to differences in gender, significantly more males received medications than females. Boys with ADHD may exhibit more externalised behavioural problems and have a higher probability of being prescribed with medication and then to maintain this therapy (Visser et al. 2007; Garbe et al. 2012), which is consistent with the findings in the current study.
Limitations
This study has several limitations. First, the diagnoses of ADHD were identified on the basis of ICD codes only, and were not validated using face-to-face diagnostic instruments. Although ADHD was defined by at least two NHIRD-TW claims records with ADHD, the possibility of misdiagnosis still exists. Without standardised, multidimensional assessments for the national population, the actual false positive rate or false negative rate of a diagnosis of ADHD is unknown (Sciutto & Eisenberg, 2007). Second, the specific drug distribution, duration of drug treatment, gap in prescriptions (e.g., drug holiday) and drug adherence were not analysed in this study. In addition, ADHD medications prescribed for indications other than ADHD were not analysed. Third, some clinical data such as socioeconomic status, residential area, clinical manifestations and patient outcomes were not provided in the claims data. It is unclear how the prevalence rates of ADHD diagnosis or medication treatment were influenced by the aforementioned factors. Consequently, we could not determine whether or not the prescribed ADHD medications were appropriate. Last, data on therapy other than medication (i.e., behavioural or occupational therapy) were not available in this study. In addition, the reasons underlying the decision of whether or not to prescribe pharmacotherapy were not available from the claims data.
Conclusions
In conclusion, this population-based study shows that the number of youths being diagnosed with ADHD who attended medical services and who received medications increased from 2000 to 2011 in Taiwan. However, the proportion of youths with a diagnosis of ADHD among the total population was still lower than the prevalence rate of ADHD reported in previous community-based research in Taiwan. In addition, approximate 40–50% of youths with ADHD did not receive medications. These findings are not consistent with a systematic public opinion on overdiagnosis or overmedication of ADHD in Taiwan. We suggest that our findings may help to increase public awareness that a large number of children with ADHD in Taiwan are not currently identified or treated.
Acknowledgements
The authors thank Mr Keng-Hao Chang and Mr Yao-cheng Lyu for retrieving data from the NHIRD-TW. This study is based in part on data from the NHIRD-TW provided by the National Health Insurance Administration, Ministry of Health and Welfare and managed by the National Health Research Institutes (registration number: NHIRD-102-088). The interpretations and conclusions contained herein do not represent those of the National Health Insurance Administration, Ministry of Health and Welfare or National Health Research Institutes.
Financial Support
This study was sponsored by the Chang Gung Memorial Hospital Research Project (Grant numbers CMRPG8D0581, CMRPG2D0422, CRRPG2B0114 and CLRPG2C0024).
Conflict of Interest
None.
Availability of data and materials
Data are available from the NHIRD published by Taiwan National Health Insurance Bureau. Due to legal restrictions imposed by the Government of Taiwan in relation to the ‘Personal Information Protection Act’, data cannot be made publicly available. Requests for data can be sent as a formal proposal to the NHIRD (http://nhird.nhri.org.tw).
Supplementary material
For supplementary material accompanying this paper visit http://dx.doi.org/10.1017/S2045796016000500.
click here to view supplementary material
References
- Atladottir HO, Gyllenberg D, Langridge A, Sandin S, Hansen SN, Leonard H, Gissler M, Reichenberg A, Schendel DE, Bourke J, Hultman CM, Grice DE, Buxbaum JD, Parner ET (2015). The increasing prevalence of reported diagnoses of childhood psychiatric disorders: a descriptive multinational comparison. European Child and Adolescent Psychiatry 24, 173–183. [DOI] [PubMed] [Google Scholar]
- Barbaresi WJ, Katusic SK, Colligan RC, Pankratz VS, Weaver AL, Weber KJ, Mrazek DA, Jacobsen SJ (2002). How common is attention-deficit/hyperactivity disorder? Incidence in a population-based birth cohort in Rochester, Minn. Archives of Pediatrics and Adolescent Medicine 156, 217–224. [DOI] [PubMed] [Google Scholar]
- Barbaresi WJ, Katusic SK, Colligan RC, Weaver AL, Jacobsen SJ (2007). Modifiers of long-term school outcomes for children with attention-deficit/hyperactivity disorder: does treatment with stimulant medication make a difference? Results from a population-based study. Journal of Developmental and Behavioral Pediatrics 28, 274–287. [DOI] [PubMed] [Google Scholar]
- Bruchmuller K, Margraf J, Schneider S (2012). Is ADHD diagnosed in accord with diagnostic criteria? Overdiagnosis and influence of client gender on diagnosis. Journal of Consulting and Clinical Psychology 80, 128–138. [DOI] [PubMed] [Google Scholar]
- Chan E, Fogler JM, Hammerness PG (2016). Treatment of attention-deficit/hyperactivity disorder in adolescents: a systematic review. JAMA 315, 1997–2008. [DOI] [PubMed] [Google Scholar]
- Chen CY, Yeh HH, Chen KH, Chang IS, Wu EC, Lin KM (2011). Differential effects of predictors on methylphenidateinitiation and discontinuation among young people with newly diagnosed attention-deficit/hyperactivity disorder. Journal of Child and Adolescent Psychopharmacology 21, 265–273. [DOI] [PubMed] [Google Scholar]
- Cherkasova M, Sulla EM, Dalena KL, Ponde MP, Hechtman L (2013). Developmental course of attention deficit hyperactivity disorder and its predictors. Journal of the Canadian Academy of Child and Adolescent Psychiatry 22, 47–54. [PMC free article] [PubMed] [Google Scholar]
- Chien IC, Lin CH, Chou YJ, Chou P (2012). Prevalence, incidence, and stimulant use of attention-deficit hyperactivity disorder in Taiwan, 1996–2005: a national population-based study. Social Psychiatry and Psychiatric Epidemiology 47, 1885–1890. [DOI] [PubMed] [Google Scholar]
- Coon ER, Quinonez RA, Moyer VA, Schroeder AR (2014). Overdiagnosis: how our compulsion for diagnosis may be harming children. Pediatrics 134, 1013–1023. [DOI] [PubMed] [Google Scholar]
- Dalsgaard S, Nielsen HS, Simonsen M (2013). Five-fold increase in national prevalence rates of attention-deficit/hyperactivity disorder medications for children and adolescents with autism spectrum disorder, attention-deficit/hyperactivity disorder, and other psychiatric disorders: a Danish register-based study. Journal of Child and Adolescent Psychopharmacology 23, 432–439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Directorate-General of Budget Accounting and Statistics, Executive Yuan, Taiwan (2015). Resident Population by 5-Year, 10-Year Age Group.
- Evans SW, Owens JS, Bunford N (2014). Evidence-based psychosocial treatments for children and adolescents with attention-deficit/hyperactivity disorder. Journal of Clinical Child and Adolescent Psychology 43, 527–551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feldman HM, Reiff MI (2014). Clinical practice. Attention deficit-hyperactivity disorder in children and adolescents. New England Journal of Medicine 370, 838–846. [DOI] [PubMed] [Google Scholar]
- Findling RL (2008). Evolution of the treatment of attention-deficit/hyperactivity disorder in children: a review. Clinical Therapeutics 30, 942–957. [DOI] [PubMed] [Google Scholar]
- Garbe E, Mikolajczyk RT, Banaschewski T, Petermann U, Petermann F, Kraut AA, Langner I (2012). Drug treatment patterns of attention-deficit/hyperactivity disorder in children and adolescents in Germany: results from a large population-based cohort study. Journal of Child and Adolescent Psychopharmacology 22, 452–458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garfield CF, Dorsey ER, Zhu S, Huskamp HA, Conti R, Dusetzina SB, Higashi A, Perrin JM, Kornfield R, Alexander GC (2012). Trends in attention deficit hyperactivity disorder ambulatory diagnosis and medical treatment in the United States, 2000–2010. Academic Pediatrics 12, 110–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gau SS, Chong MY, Chen TH, Cheng AT (2005). A 3-year panel study of mental disorders among adolescents in Taiwan. American Journal of Psychiatry 162, 1344–1350. [DOI] [PubMed] [Google Scholar]
- Getahun D, Jacobsen SJ, Fassett MJ, Chen W, Demissie K, Rhoads GG (2013). Recent trends in childhood attention-deficit/hyperactivity disorder. JAMA Pediatrics 167, 282–288. [DOI] [PubMed] [Google Scholar]
- Hodgkins P, Sasane R, Meijer WM (2011). Pharmacologic treatment of attention-deficit/hyperactivity disorder in children: incidence, prevalence, and treatment patterns in the Netherlands. Clinical Therapeutics 33, 188–203. [DOI] [PubMed] [Google Scholar]
- Holden SE, Jenkins-Jones S, Poole CD, Morgan CL, Coghill D, Currie CJ (2013). The prevalence and incidence, resource use and financial costs of treating people with attention deficit/hyperactivity disorder (ADHD) in the United Kingdom (1998 to 2010). Child and Adolescent Psychiatry and Mental Health 7, 34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hong M, Kwack YS, Joung YS, Lee SI, Kim B, Sohn SH, Chung US, Yang J, Bhang SY, Hwang JW, Choi HY, Oh IH, Lee YJ, Bahn GH (2014). Nationwide rate of attention-deficit hyperactivity disorder diagnosis and pharmacotherapy in Korea in 2008–2011. Asia-Pacific Psychiatry 6, 379–385. [DOI] [PubMed] [Google Scholar]
- Huang CL, Chu CC, Cheng TJ, Weng SF (2014). Epidemiology of treated attention-deficit/hyperactivity disorder (ADHD) across the lifespan in Taiwan: a nationwide population-based longitudinal study. PLoS ONE 9, e95014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LeFever GB, Dawson KV, Morrow AL (1999). The extent of drug therapy for attention deficit-hyperactivity disorder among children in public schools. American Journal of Public Health 89, 1359–1364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang KY, Zeger SL (1986). Longitudinal data analysis using generalized linear models. Biometrika 73, 13–22. [Google Scholar]
- Lien YT, Yeh HH, Soong WT, Jeng SF, Huang N, Chen CY (2015). Factors associated with treatment mode and termination among preschoolers with ADHD in Taiwan. Psychiatric Services 66, 177–185. [DOI] [PubMed] [Google Scholar]
- McCarthy S, Wilton L, Murray ML, Hodgkins P, Asherson P, Wong IC (2012). The epidemiology of pharmacologically treated attention deficit hyperactivity disorder (ADHD) in children, adolescents and adults in UK primary care. BMC Pediatrics 12, 78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohr Jensen C, Steinhausen HC (2015). Time trends in incidence rates of diagnosed attention-deficit/hyperactivity disorder across 16 years in a nationwide Danish registry study. Journal of Clinical Psychiatry 76, e334–e341. [DOI] [PubMed] [Google Scholar]
- Morrow RL, Garland EJ, Wright JM, Maclure M, Taylor S, Dormuth CR (2012). Influence of relative age on diagnosis and treatment of attention-deficit/hyperactivity disorder in children. CMAJ 184, 755–762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nussbaum NL (2012). ADHD and female specific concerns: a review of the literature and clinical implications. Journal of Attention Disorders 16, 87–100. [DOI] [PubMed] [Google Scholar]
- Oner O, Yilmaz ES, Karada XFH, Vural M, Vural EH, Akbulat A, Gursoz HX, Turkcapar H, Kerman S (2014). ADHD Medication Trends in Turkey: 2009–2013. Journal of Attention Disorders. doi: 10.1177/1087054714523129. [DOI] [PubMed] [Google Scholar]
- Partridge B, Lucke J, Hall W (2012). Public attitudes towards the acceptability of using drugs to treat depression and ADHD. Australian and New Zealand Journal of Psychiatry 46, 958–965. [DOI] [PubMed] [Google Scholar]
- Partridge B, Lucke J, Hall W (2014). Over-diagnosed and over-treated: a survey of Australian public attitudes towards the acceptability of drug treatment for depression and ADHD. BMC Psychiatry 14, 74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polanczyk G, de Lima MS, Horta BL, Biederman J, Rohde LA (2007). The worldwide prevalence of ADHD: a systematic review and metaregression analysis. American Journal of Psychiatry 164, 942–948. [DOI] [PubMed] [Google Scholar]
- Polanczyk GV, Willcutt EG, Salum GA, Kieling C, Rohde LA (2014). ADHD prevalence estimates across three decades: an updated systematic review and meta-regression analysis. International Journal of Epidemiology 43, 434–442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ponizovsky AM, Marom E, Fitoussi I (2014). Trends in attention deficit hyperactivity disorder drugs consumption, Israel, 2005–2012. Pharmacoepidemiology and Drug Safety 23, 534–538. [DOI] [PubMed] [Google Scholar]
- Rapoport JL (2013). Pediatric psychopharmacology: too much or too little? World Psychiatry 12, 118–123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rowland AS, Umbach DM, Stallone L, Naftel AJ, Bohlig EM, Sandler DP (2002). Prevalence of medication treatment for attention deficit-hyperactivity disorder among elementary school children in Johnston County, North Carolina. American Journal of Public Health 92, 231–234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rucklidge JJ (2010). Gender differences in attention-deficit/hyperactivity disorder. Psychiatric Clinics of North America 33, 357–373. [DOI] [PubMed] [Google Scholar]
- Safer DJ (2000). Are stimulants overprescribed for youths with ADHD? Annals of Clinical Psychiatry 12, 55–62. [DOI] [PubMed] [Google Scholar]
- Safer DJ (2015). Is ADHD really increasing in youth? Journal of Attention Disorders. doi: 10.1177/1087054715586571. [DOI] [PubMed] [Google Scholar]
- Safer DJ, Zito JM, Fine EM (1996). Increased methylphenidate usage for attention deficit disorder in the 1990s. Pediatrics 98, 1084–1088. [PubMed] [Google Scholar]
- Sciutto MJ, Eisenberg M (2007). Evaluating the evidence for and against the overdiagnosis of ADHD. Journal of Attention Disorders 11, 106–113. [DOI] [PubMed] [Google Scholar]
- Stuhec M, Locatelli I, Svab V (2015). Trends in attention-deficit/hyperactivity disorder drug consumption in children and adolescents in Slovenia from 2001 to 2012: a drug use study from a national perspective. Journal of Child and Adolescent Psychopharmacology 25, 254–259. [DOI] [PubMed] [Google Scholar]
- Thapar A, Cooper M (2016). Attention deficit hyperactivity disorder. Lancet 19, 1240–1250. [DOI] [PubMed] [Google Scholar]
- Thomas R, Sanders S, Doust J, Beller E, Glasziou P (2015). Prevalence of attention-deficit/hyperactivity disorder: a systematic review and meta-analysis. Pediatrics 135, e994–e1001. [DOI] [PubMed] [Google Scholar]
- Treceno C, Martin Arias LH, Sainz M, Salado I, Garcia Ortega P, Velasco V, Jimeno N, Escudero A, Velasco A, Carvajal A (2012). Trends in the consumption of attention deficit hyperactivity disorder medications in Castilla y Leon (Spain): changes in the consumption pattern following the introduction of extended release methylphenidate. Pharmacoepidemiology and Drug Safety 21, 435–441. [DOI] [PubMed] [Google Scholar]
- Vaughan BS, March JS, Kratochvil CJ (2012). The evidence-based pharmacological treatment of paediatric ADHD. International Journal of Neuropsychopharmacology 15, 27–39. [DOI] [PubMed] [Google Scholar]
- Visser SN, Lesesne CA, Perou R (2007). National estimates and factors associated with medication treatment for childhood attention-deficit/hyperactivity disorder. Pediatrics 119 (Suppl. 1), S99–S106. [DOI] [PubMed] [Google Scholar]
- Visser SN, Danielson ML, Bitsko RH, Holbrook JR, Kogan MD, Ghandour RM, Perou R, Blumberg SJ (2014). Trends in the parent-report of health care provider-diagnosed and medicated attention-deficit/hyperactivity disorder: United States, 2003–2011. Journal of the American Academy of Child & Adolescent Psychiatry 53, 34–46 e32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winterstein AG, Gerhard T, Shuster J, Zito J, Johnson M, Liu H, Saidi A (2008). Utilization of pharmacologic treatment in youths with attention deficit/hyperactivity disorder in Medicaid database. Annals of Pharmacotherapy 42, 24–31. [DOI] [PubMed] [Google Scholar]
- Wu CS, Lai MS, Gau SS, Wang SC, Tsai HJ (2014). Concordance between patient self-reports and claims data on clinical diagnoses, medication use, and health system utilization in Taiwan. PLoS ONE 9, e112257. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
For supplementary material accompanying this paper visit http://dx.doi.org/10.1017/S2045796016000500.
click here to view supplementary material
Data Availability Statement
Data are available from the NHIRD published by Taiwan National Health Insurance Bureau. Due to legal restrictions imposed by the Government of Taiwan in relation to the ‘Personal Information Protection Act’, data cannot be made publicly available. Requests for data can be sent as a formal proposal to the NHIRD (http://nhird.nhri.org.tw).