Abstract
Aim.
To examine the incidence of asthma in adult patients with major depressive disorder (MDD).
Methods.
From the National Health Insurance database of Taiwan, we identified 30 169 adult patients who were newly diagnosed with MDD between 2000 and 2010. Individuals without depression were randomly selected four times and frequency matched for sex, age and year of diagnosis. Both cohorts were followed-up for the occurrence of asthma up to the end of 2011. Adjusted hazard ratios (aHRs) of asthma were estimated using the Cox proportional hazards method.
Results.
The overall incidence of asthma was 1.91-fold higher in the MDD cohort than in the non-depression cohort (7.55 v. 3.96 per 1000 person-years), with an aHR of 1.66 (95% confidence interval (CI) 1.55–1.78). In both cohorts, the incidence of asthma was higher in patients and controls who were female, aged, with comorbidities and users of aspirin or beta-adrenergic receptor blockers. No significant difference was observed in the occurrence of asthma between patients with MDD treated with selective serotonin reuptake inhibitors (SSRIs) and those treated with non-SSRIs (SSRIs to non-SSRIs aHR = 1.03, 95% CI 0.91–1.17).
Conclusion.
Adult patients with MDD are at a higher risk of asthma than those without depression are.
Key words: Asthma, cohort study, major depressive disorder (MDD), selective serotonin reuptake inhibitors (SSRIs)
Introduction
With low mood and aversion to activity, patients with depression encounter both physical and psychological difficulties (American Psychiatric Association, 2013; Jiang et al. 2014). Depression is associated with altered self-awareness, and it affects the patients’ emotions, thoughts, interpersonal relationships and work performance. The patients experience a diminished ability to cope with daily life. The diagnosis is typically made on the basis of criteria from the Diagnostic and Statistical Manual of Mental Disorders (DSM). The World Health Organization estimates that by 2020, depression will become the leading cause of lost disability-adjusted life years, which is a global public health and social problem (Reddy, 2010). In a recent epidemiologic study, Fu et al. (2013) reported that the prevalence of depression has significantly increased in Taiwan over the last 20 years. Females and populations with lower socioeconomic status and poor physical health are at an increased risk for depression.
Asthma is also a serious global health problem. It is a heterogeneous disease characterised by chronic airway inflammation. The definition and diagnosis of asthma are based on a history of characteristic symptoms and evidence of variable limitations in airflow (GINA Report, 2015). Certain comorbidities are common in patients with asthma, particularly in those with difficult-to-treat asthma. The most common comorbidities include gastroesophageal reflux disease (GERD), rhinitis, sinusitis, anxiety and depression (Goodwin et al. 2003; Boulet, 2009).
Poor mental health may lead to chronic health disorders (Mannino, 2008). Depression frequently occurs in patients with asthma and vice versa (Mannino, 2008; Jiang et al. 2014). The US CARDIA study recently completed a 20-year longitudinal study to evaluate the bidirectional relationship between asthma and depression in young and middle-aged adults (Brunner et al. 2014). The results showed that depression is a risk factor for developing asthma and that asthma is not associated with incident depression. However, the temporal linkage between depression and incident asthma requires more evidence and further clarification.
The National Health Insurance (NHI) database of Taiwan is a reliable longitudinal population dataset, which has been used for various studies, including those on both asthma and depression (Lin et al. 2014; Shen et al. 2014, 2015a; Lee et al. 2015). The present study investigated whether major depressive disorder (MDD) is associated with incident asthma. To the best of our knowledge, this is the first population-based cohort study of this type in an Asian population.
Materials and methods
Data source
The NHI programme in Taiwan was implemented in 1995 and has covered more than 99% of the estimated 23.74 million Taiwanese residents since 1996 (http://www.nhi.gov.tw/english/index.aspx). This study was performed using the Longitudinal Health Insurance Database (LHID) established for researchers by the Taiwan National Health Research Institutes (NHRI). LHID consists of original medical claims of 1 000 000 enrolees, randomly selected from the entire insured population in the year 2000. This database included information on medical services, such as prescriptions of medications and treatment procedure for inpatient and outpatient care. The identities of all the patients were converted to surrogate numbers by the NHRI. This study was exempted from a complete ethical review by the China Medical University and Hospital Research Ethics Committee (IRB permit number: CMUH104-REC2-115).
Selection of patients and controls for study
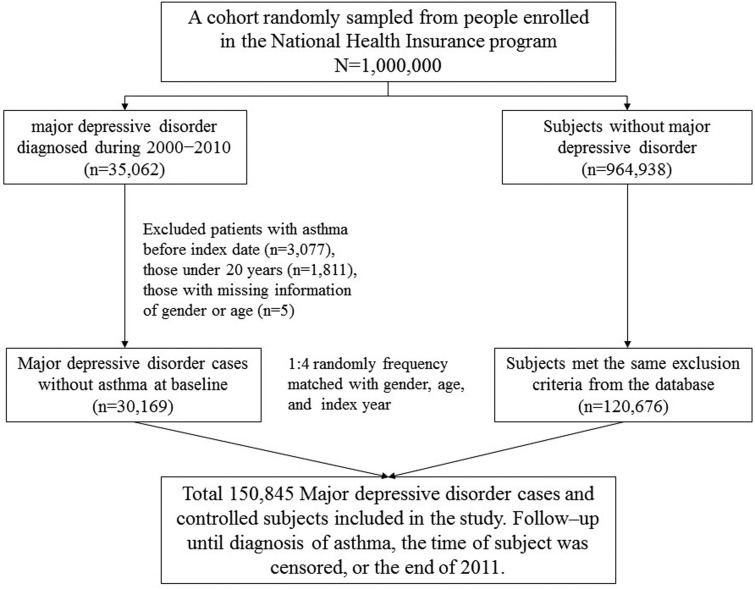
Diseases were coded using International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM). We identified patients aged ≥20 years with newly diagnosed MDD (ICD-9 code 296.2–296.3) in 2000–2010 (Fig. 1). To ensure the accuracy of diagnosis, we selected only those patients who had, at some point, received pharmacological therapy with selective serotonin reuptake inhibitors (SSRIs) or non-SSRIs (including tricyclic antidepressants, monoamine oxidase inhibitors, heterocyclic antidepressants and others (bupropion, venlafaxine and mirtazapine)). The date of diagnosis was defined as the index date. For each MDD case, four controls without depression were randomly selected from the LHID and frequency matched for sex, age group (every 5-year span) and the index year. In both the depression and the non-depression groups, individuals with a history of asthma (ICD-9 codes 493) and those with incomplete demographic information at baseline were excluded.
Fig. 1.
Flow chart depicting the study design and selection of patients and controls.
Outcome and relevant variables
All study patients and controls were followed up from the index date up to asthma diagnosis, the date of death or withdrawal from the insurance system, or up to the end of 2011. Patients with a discharge code of asthma in the admission dataset or patients with at least two visits for asthma in a year in the outpatient dataset were defined as asthma cases. We included several comorbidities and medications, which were considered risk factors of asthma (Covar et al. 2005; Boulet, 2009; Sanfiorenzo & Pipet, 2011; Mohanan et al. 2014; Henriksen et al. 2015; Postma & Rabe, 2015). The comorbidities included GERD (ICD-9 codes 530.11 and 530.81), chronic sinusitis (ICD-9 code 473), allergic rhinitis (ICD-9 code 477), atopic dermatitis (ICD-9 code 691.8), obesity (ICD-9 code 278.0) and chronic obstructive pulmonary disease (COPD) (ICD-9-CM code 496). The medication included aspirin and beta-adrenergic receptor blockers. Comorbidity was defined as any of the aforementioned diagnosis codes in the admission records or diagnoses coded at least two times within a year in the outpatient records. All comorbidities were identified before the index date.
Statistical analysis
The distributions according to sex, age group, comorbidities and medication (categorical variables) in the depression and the non-depression groups were compared and examined using the chi-square (χ2) test. The means and standard deviations (s.d.) of continuous variables were determined. The differences in the variables between the two cohorts were examined using the Student's t-test. The incidence for asthma (per 1000 person-years) was calculated in the two groups. We used Cox proportional hazards regression models to estimate the hazard ratios (HR) and 95% confidence intervals (CI) to assess the strength of the relationship between depression and incident asthma. The multivariable model estimated adjusted hazard ratio (aHR) after controlling for sex, age, comorbidities and medication, which were found to differ significantly in the univariate analysis. In the multivariable Cox model, only allergic rhinitis, obesity, and COPD exhibited a significant relationship with asthma. For further data analysis, we assessed the incident asthma associated with depression associated with allergic rhinitis, obesity or COPD. Moreover, we evaluated the role of medication in relation to asthma. Antidepressants were divided into the following two groups: SSRIs and non-SSRIs. We applied the Kaplan–Meier method to estimate the cumulative incidence of asthma in the depression and the non-depression groups and used the log-rank test to determine the significance level of the difference between the two curves. All analyses were performed using the statistical package SAS for Windows (Version 9.3, SAS Institute Inc., Cary, NC, USA). A two-tailed p < 0.05 was considered statistically significant.
Results
Distributions based on age groups and sex were similar in both the depression group (N = 30 169) and the non-depression group (N = 120 676). 58.7% of the patients and controls were in the age range 20–49 years (Table 1) and females comprised 61.8% of both groups. Although the mean age was only slightly higher in the depression group than in the non-depression group, the difference was significant. The depression group showed a higher prevalence of GERD, chronic sinusitis, allergic rhinitis, atopic dermatitis, obesity, COPD and aspirin use than the non-depression group did.
Table 1.
Comparisons of demographic characteristics, comorbidities and medication between the depression and non-depression groups
| MDD | |||
|---|---|---|---|
| No | Yes | p-valuea | |
| N = 120 676 | N = 30 169 | ||
| Gender | 0.99 | ||
| Women | 74 592 (61.8) | 18 648 (61.8) | |
| Men | 46 084 (38.2) | 11 521 (38.2) | |
| Age | 0.99 | ||
| 20–49 | 70 824 (58.7) | 17 706 (58.7) | |
| 50–64 | 27 948 (23.2) | 6987 (23.2) | |
| ≥65 | 21 904 (18.2) | 5476 (18.2) | |
| Age, mean ± s.d.b | 47.2 ± 16.8 | 47.6 ± 16.7 | <0.001 |
| Comorbidity | |||
| GERD | 1098 (0.91) | 1082 (3.59) | <0.001 |
| Chronic sinusitis | 2444 (2.03) | 1188 (3.94) | <0.001 |
| Allergic rhinitis | 10 619 (8.80) | 4886 (16.2) | <0.001 |
| Atopic dermatitis | 1345 (1.11) | 643 (2.13) | <0.001 |
| Obesity | 1048 (0.87) | 488 (1.62) | <0.001 |
| COPD | 5545 (4.59) | 2908 (9.64) | <0.001 |
| Medication | |||
| Aspirin | 20 849 (17.3) | 8882 (29.4) | <0.001 |
| Beta blockers | 3804 (3.15) | 785 (2.60) | <0.001 |
MDD, major depressive disorder, s.d., standard deviation, GERD, gastroesophageal reflux disease, COPD, chronic obstructive pulmonary disease.
χ2 test for the distribution of sex, age group, comorbidities and medication.
t-test for the age, mean (s.d.).
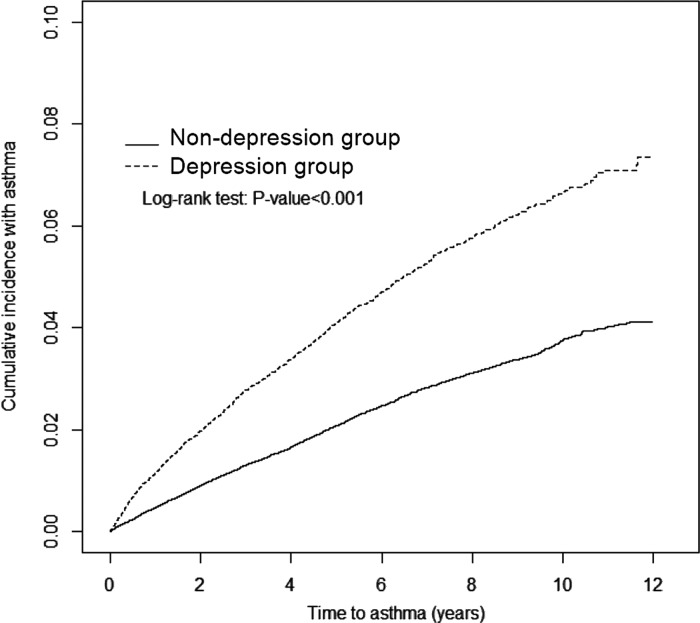
The average follow-up duration was 6.25 ± 3.21 years for the depression group and 6.36 ± 3.17 years for the non-depression group. The patients in the depression group had an approximately 3.2% higher rate of asthma than the controls in the non-depression group after a 12-year follow-up (log-rank test p < 0.001, Fig. 2).
Fig. 2.
Cumulative incidence of asthma in the depression (dashed line) and non-depression (solid line) groups.
The overall incidence of asthma was greater in the depression group than in the non-depression group (7.55 and 3.96 per 1000 person-years, crude HR = 1.91, 95% CI 1.79–2.03), with an aHR of 1.66 (95% CI 1.55–1.78) after adjusting for sex, age, comorbidities and medications (Table 2). In both groups, the incidence of asthma increased with age, comorbidity and the use of aspirin or beta-adrenergic receptor blockers. The HR of asthma (depression group to the non-depression group) was significant for each stratum.
Table 2.
Comparison of incidence and hazard ratios of asthma between the depression and non-depression groups stratified by demographic characteristics, comorbidities and medication
| MDD | ||||||||
|---|---|---|---|---|---|---|---|---|
| No | Yes | |||||||
| Event | PY | Rate† | Event | PY | Rate† | Crude HR (95% CI) | Adjusted HR (95% CI)‡ | |
| All | 3041 | 767 519 | 3.96 | 1424 | 188 585 | 7.55 | 1.91 (1.79–2.03)*** | 1.66 (1.55–1.78)*** |
| Gender | ||||||||
| Women | 1931 | 480 807 | 4.02 | 936 | 118 889 | 7.87 | 1.96 (1.81–2.12)*** | 1.72 (1.58–1.87)*** |
| Men | 1110 | 286 712 | 3.87 | 488 | 69 696 | 7.00 | 1.81 (1.62–2.01)*** | 1.57 (1.40–1.76)*** |
| Stratify age | ||||||||
| 20–49 | 1107 | 467 932 | 2.37 | 623 | 115 967 | 5.37 | 2.27 (2.06–2.51)*** | 2.00 (1.79–2.22)*** |
| 50–64 | 889 | 177 340 | 5.01 | 376 | 42 941 | 8.76 | 1.74 (1.55–1.97)*** | 1.50 (1.31–1.71)*** |
| ≥65 | 1045 | 122 247 | 8.55 | 425 | 29 677 | 14.3 | 1.67 (1.49–1.87)*** | 1.44 (1.27–1.63)*** |
| Comorbidity§ | ||||||||
| No | 2187 | 669 408 | 3.27 | 814 | 141 994 | 5.73 | 1.76 (1.62–1.90)*** | 1.78 (1.64–1.93)*** |
| Yes | 854 | 98 112 | 8.70 | 610 | 46 590 | 13.1 | 1.52 (1.37–1.68)*** | 1.49 (1.34–1.65)*** |
| Medication | ||||||||
| Aspirin | ||||||||
| No | 2364 | 652 777 | 3.62 | 905 | 138 707 | 6.52 | 1.80 (1.67–1.95)*** | 1.72 (1.58–1.87)*** |
| Yes | 677 | 114 742 | 5.90 | 519 | 49 878 | 10.4 | 1.77 (1.58–1.99)*** | 1.55 (1.37–1.75)*** |
| Beta blockers | ||||||||
| No | 2907 | 749 136 | 3.88 | 1370 | 184 671 | 7.42 | 1.91 (1.79–2.04)*** | 1.64 (1.53–1.77)*** |
| Yes | 134 | 18 384 | 7.29 | 54 | 3913 | 13.8 | 1.90 (1.39–2.61)*** | 1.93 (1.38–2.70)*** |
MDD, major depressive disorder; PY, person-years; HR, hazard ratio; CI, confidence interval.
incidence rate per 1000 person-years.
Model was adjusted for sex, age, comorbidities of GERD, chronic sinusitis, allergic rhinitis, atopic dermatitis, obesity, COPD and medication with aspirin and beta blockers.
Patients or controls with any comorbidity from among GERD, chronic sinusitis, allergic rhinitis, atopic dermatitis, obesity and COPD were included in the comorbidity group.
***p < 0.001.
The multivariate models showed that asthma was independently associated with some comorbidities, including allergic rhinitis (aHR = 1.71, 95% CI 1.55–1.89), obesity (aHR = 1.28, 95% CI 1.00–1.80) and COPD (aHR = 2.65, 95% CI 2.38–2.94) (data not shown). Table 3 presents the incident asthma associated with interactions between MDD and the comorbidity of allergic rhinitis, obesity or COPD. The incident asthma and relative hazard was higher for those with both MDD and the selected comorbidities, particularly for patients with MDD and the comorbidity COPD. The asthmatic risk increased further and was 3.4-fold higher in patients with both MDD and COPD than in patients with MDD, but without COPD (21.3 v. 6.31 per 1000 person-years).
Table 3.
Cox proportional hazards regression analysis for the risk of asthma-associated major depressive disorder and the selected comorbidities
| Variables | Event | PY | Rate† | Adjusted HR (95% CI) | p-value‡ | |
|---|---|---|---|---|---|---|
| MDD | Allergic rhinitis | 0.009 | ||||
| No | No | 1773 | 711 577 | 3.67 | 1 (Reference)§ | |
| No | Yes | 321 | 55 942 | 7.61 | 1.91 (1.72–2.12)*** | |
| Yes | No | 756 | 161 828 | 6.91 | 1.75 (1.63–1.89)*** | |
| Yes | Yes | 212 | 26 756 | 11.4 | 2.49 (2.19–2.83)*** | |
| MDD | Obesity | 0.71 | ||||
| No | No | 2064 | 762 154 | 3.95 | 1 (Reference)‖ | |
| No | Yes | 30 | 5365 | 5.96 | 1.34 (0.95–1.90) | |
| Yes | No | 938 | 186 036 | 7.51 | 1.66 (1.55–1.78)*** | |
| Yes | Yes | 30 | 2549 | 10.2 | 2.24 (1.52–3.30)*** | |
| MDD | COPD | 0.001 | ||||
| No | No | 2593 | 738 465 | 3.51 | 1 (Reference)¶ | |
| No | Yes | 448 | 29 055 | 15.4 | 2.62 (2.36–2.92)*** | |
| Yes | No | 1090 | 172 867 | 6.31 | 1.74 (1.62–1.88)*** | |
| Yes | Yes | 334 | 15 718 | 21.3 | 3.57 (3.15–4.05)*** |
MDD, major depressive disorder; COPD, chronic obstructive pulmonary disease.
Incidence rate per 1000 person-years.
p-value for interaction.
Model was adjusted for sex, age, comorbidities of GERD, chronic sinusitis, atopic dermatitis, obesity, COPD and medication with aspirin and beta blockers by using Cox proportional hazards regression.
Model was adjusted for sex, age, comorbidities of GERD, chronic sinusitis, allergic rhinitis, atopic dermatitis, COPD and medication with aspirin and beta blockers by using Cox proportional hazards regression.
Model was adjusted for sex, age, comorbidities of GERD, chronic sinusitis, allergic rhinitis, atopic dermatitis, obesity and medication with aspirin and beta blockers by using Cox proportional hazards regression.
***p < 0.001.
The data analysis in Table 4 evaluates the incidence of asthma associated with medication in patients with MDD. Nearly 70% of patients with MDD had SSRI prescriptions. However, no significant difference was observed between patients taking SSRIs and non-SSRIs.
Table 4.
Incidence and hazard ratios of asthma in the depression and non-depression groups stratified by medication
| Variables | N | Event | PY | Rate† | Adjusted HR (95% CI)‡ | Adjusted HR (95% CI)‡ |
|---|---|---|---|---|---|---|
| Without depression | 120 676 | 3041 | 767 519 | 3.96 | 1 (Reference) | |
| MDD with medications | ||||||
| Non-SSRIs | 7196 | 363 | 44 366 | 8.18 | 1.62 (1.45–1.81)*** | 1 (Reference) |
| SSRIs | 22 973 | 1061 | 144 219 | 7.36 | 1.69 (1.56–1.82)*** | 1.03 (0.91–1.17) |
SSRI, selective serotonin reuptake inhibitor.
Incidence rate per 1000 person-years.
Model was adjusted for sex, age, comorbidities of GERD, chronic sinusitis, allergic rhinitis, atopic dermatitis, obesity, COPD and medication with aspirin and beta blockers by using Cox proportional hazards regression.
***p < 0.001.
Discussion
This population-based cohort study demonstrated that adult patients with MDD were at a higher risk of asthma than the matched controls. Patients and controls who were female sex, aged, with comorbidities and users of aspirin or beta-adrenergic receptor blockers showed a higher incidence of asthma. Furthermore, our study revealed no significant difference in the development of asthma between patients with MDD who treated with SSRIs and those treated with non-SSRIs.
Childhood-onset asthma is more atopic than adult-onset asthma. However, adult-onset asthma is more severe and involves a more rapid decline in lung function than childhood-onset asthma does (de Nijs et al. 2013). Adult-onset asthma is common among the aged population, affecting approximately 4–8% of this population (Kitch et al. 2000). In a systemic analysis, de Nijs et al. (2013) reported that the adult incidence of asthma in the general population is higher in females than in males (4.6 v. 3.6 per 1000 person-years), and the incidence increases with age. They concluded that the prevalence of asthma actually increases in adults. These findings are similar to the incidence of asthma observed in our non-depression group.
In a study with a total of 2270 participants from Sweden, Iceland and Norway, Leander et al. (2014) reported a significant prevalence of respiratory symptoms in patients with depression and anxiety (adjusted odds ratio (OR) = 1.33–1.94). Patients with depression are more likely to have physician-diagnosed asthma, bronchial hyper-responsiveness, nocturnal dyspnoea and chest tightness. Depression is also associated with attacks of breathlessness after activity or at rest, wheezing and wheezing without a cold. Leander et al. therefore concluded that respiratory symptoms and psychological status are strongly associated.
The US CARDIA study found that young adults with depression had a relative risk of 1.26 (95% CI 1.02–1.56) of developing asthma (Brunner et al. 2014). In another population-based study in middle-aged adults, Loerbroks et al. (2010) found that the risk of adult-onset asthma increased in participants with depressive symptoms, but decreased in participants with favourable social support. Patten et al. (2008) reported that MDD was a risk factor for increased incidence of chronic diseases in general, which also included asthma. Our results are in agreement with those of all the aforementioned studies. Notably, our study reflects a realistic scenario, where the diagnoses of both MDD and asthma resulted from actual medical consultations.
The definitive mechanism of asthma development in patients with depression remains largely unknown. Some evidence of changes in airway responsiveness in different psychological states has been documented. For instance, depressing stimuli may induce airway instability and can lead to asthma exacerbations (Ritz et al. 2001; Lehrer et al. 2002). Brunner et al. (2014) hypothesised that the central nervous system, autonomic nerve system, shared comorbidities and substances exposure, inflammation, and neuroendocrine factors, all contribute to depression-induced asthma. Furthermore, socioeconomic status, lifestyle, diet, occupation, genetics and infections in patients with depression may also be linked to the occurrence of asthma (Shen et al. 2015a).
Previous studies have shown that treatment with SSRIs is associated with lower Hamilton Rating Scale for Depression scores, higher rates of sustained remission of depression, and lesser oral corticosteroid use than treatment with placebo is, in patients with both asthma and MDD (Brown et al. 2005, 2012). We expected the asthmatic risks to be different between patients with MDD taking SSRIs and those taking non-SSRIs. However, we found that the incidence of asthma was slightly lower in the SSRIs subgroup than in the non-SSRIs subgroup although the difference was not significant.
The major strength of this study is that it is a population-based longitudinal study evaluating the asthmatic risk in an adult Asian population with MDD. A retrospective cohort study performed using insurance data is a more convenient and cost-effective alternative than a prospective cohort study if the retrospective study meets the requirements of a longitudinal study. However, the limitations of such a study should be considered while interpreting our study findings. First, diagnostic variation may have occurred among physicians. Furthermore, the ICD-9-CM was used for diagnosis. Therefore, the Taiwan health insurance authority has established a mechanism to monitor the reimbursement claims to prevent violation of laws. Depression and asthma were diagnosed mainly by psychiatrists and pulmonologists, on the basis of the DSM and GINA criteria. The care regimens for depressive disorder and asthma used specific medications or treatments such as antidepressants and electroshock therapy and devices such as bronchodilators. In this study, we selected only diagnoses with repeated coding to increase the validity and accuracy of the diagnoses (MDD, asthma and all comorbidities) to prevent coding errors. Second, detailed information regarding socioeconomic status, lifestyle, body mass index, environmental exposure and family history was unavailable in the claims data. Therefore, we could not consider these potential confounders in our data analysis. Third, relevant clinical variables, such as scores on depression rating scales, pulmonary function tests, serum laboratory data and imaging results were not available in our database (Shen et al. 2015b). Therefore, we were unable to evaluate the severity of MDD and asthma. Fourth, individuals who met the diagnostic criteria for depression might not have sought treatment. Possibly, only people who experienced severe depression visited a psychiatrist. Patients selected for the MDD cohort constituted a group representing severely depressed, treatment seeking cases. Therefore, this cohort was an atypical sample of depression cases, findings regarding the risk of asthma may not apply to a more representative sample of patients with depression.
Conclusion
Adult patients with MDD may have a nearly 2-fold higher risk of asthma than those without MDD. Psychiatrists may need to monitor patients with MDD for the potential risk of asthma. No significant difference was observed in asthma risk between patients with MDD taking SSRIs and those taking non-SSRIs.
Financial Support
This study was supported in part by Taiwan Ministry of Health and Welfare Clinical Trial and Research Center of Excellence (MOHW105-TDU-B-212-133019); China Medical University Hospital, Academia Sinica Taiwan Biobank, Stroke Biosignature Project (BM10501010037); NRPB Stroke Clinical Trial Consortium (MOST 104-2325-B-039 -005); Tseng-Lien Lin Foundation, Taichung, Taiwan; Taiwan Brain Disease Foundation, Taipei, Taiwan; Katsuzo and Kiyo Aoshima Memorial Funds, Japan; and CMU under the Aim for Top University Plan of the Ministry of Education, Taiwan. The funding bodies had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript. No additional external funding was received for this study.
Conflict of Interest
None.
Author Contributions
T. C. S., C. H. L. and C. C. W. contributed to the conception and design; F. C. S. and C. H. K. provided administrative support; T. C. S., C. L. L., F. C. S. and C. H. K. contributed to data analysis and interpretation; T. C. S., C. L. L., F. C. S. and C. H. K. helped in manuscript writing and revision. All the authors helped in collection and assembly of data and approve the final version of manuscript.
Availability of Data and Materials
All data and related metadata were deposited in an appropriate public repository. The data on the study population were obtained from the NHIRD (http://nhird.nhri.org.tw/). The National Health Research Institutes (NHRI) is a non-profit foundation established by the government. Only citizens of the Republic of China who fulfil the requirements of conducting research projects are eligible to apply for the NHIRD. The use of NHIRD is limited to research purposes only. Applicants must follow the Computer-Processed Personal Data Protection Law (http://www.winklerpartners.com/?p=987) and related regulations of National Health Insurance Administration and NHRI, and an agreement must be signed by applicants and their supervisors upon application submission. All applications are reviewed for approval of data release.
There was an error of omission in the title that has now been corrected and a notice has been published providing details.
References
- American Psychiatric Association (2013). The Diagnostic and Statistical Manual of Mental Disorders, 5th edn (DSM-5). American Psychiatric Association: Arlington, VA. [Google Scholar]
- Boulet LP (2009). Influence of comorbid conditions on asthma. European Respiratory Journal 33, 897–906. [DOI] [PubMed] [Google Scholar]
- Brown ES, Vigil L, Khan DA, Liggin JD, Carmody TJ, Rush AJ (2005). A randomized trial of citalopram versus placebo in outpatients with asthma and major depressive disorder: a proof of concept study. Biological Psychiatry 58, 865–870. [DOI] [PubMed] [Google Scholar]
- Brown ES, Howard C, Khan DA, Carmody TJ (2012). Escitalopram for severe asthma and major depressive disorder: a randomized, double-blind, placebo-controlled proof-of-concept study. Psychosomatics 53, 75–80. [DOI] [PubMed] [Google Scholar]
- Brunner WM, Schreiner PJ, Sood A, Jacobs DR Jr. (2014). Depression and risk of incident asthma in adults. The CARDIA study. American Journal of Respiratory and Critical Care Medicine 189, 1044–1051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Covar RA, Macomber BA, Szefler SJ (2005). Medications as asthma triggers. Immunology and Allergy Clinics of North America 25, 169–190. [DOI] [PubMed] [Google Scholar]
- de Nijs SB, Venekamp LN, Bel EH (2013). Adult-onset asthma: is it really different? European Respiratory Review 22, 44–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fu TS, Lee CS, Gunnell D, Lee WC, Cheng AT (2013). Changing trends in the prevalence of common mental disorders in Taiwan: a 20-year repeated cross-sectional survey. Lancet 381, 235–241. [DOI] [PubMed] [Google Scholar]
- GINA Report. Global Strategy for Asthma Management and Prevention. Retrieved 11 August 2015 from http://www.ginasthma.org.
- Goodwin RD, Jacobi F, Thefeld W (2003). Mental disorders and asthma in the community. Archives of General Psychiatry 60, 1125–1130. [DOI] [PubMed] [Google Scholar]
- Henriksen L, Simonsen J, Haerskjold A, Linder M, Kieler H, Thomsen SF, Stensballe LG (2015). Incidence rates of atopic dermatitis, asthma, and allergic rhinoconjunctivitis in Danish and Swedish children. Journal of Allergy and Clinical Immunology 136, 360–366. [DOI] [PubMed] [Google Scholar]
- Jiang M, Qin P, Yang X (2014). Comorbidity between depression and asthma via immune-inflammatory pathways: a meta-analysis. Journal of Affective Disorders 166, 22–29. [DOI] [PubMed] [Google Scholar]
- Kitch BT, Levy BD, Fanta CH (2000). Late onset asthma: epidemiology, diagnosis and treatment. Drugs and Aging 17, 385–397. [DOI] [PubMed] [Google Scholar]
- Leander M, Lampa E, Rask-Andersen A, Franklin K, Gislason T, Oudin A, Svanes C, Torén K, Janson C (2014). Impact of anxiety and depression on respiratory symptoms. Respiratory Medicine 108, 1594–1600. [DOI] [PubMed] [Google Scholar]
- Lee CW, Liao CH, Lin CL, Liang JA, Sung FC, Kao CH (2015). Increased risk of osteoporosis in patients with depression: a population-based retrospective cohort study. Mayo Clinic Proceedings 90, 63–70. [DOI] [PubMed] [Google Scholar]
- Lehrer P, Feldman J, Giardino N, Song HS, Schmaling K (2002). Psychological aspects of asthma. Journal of Consulting and Clinical Psychology 70, 691–711. [DOI] [PubMed] [Google Scholar]
- Lin YN, Lin CL, Chang YJ, Peng CL, Sung FC, Chang KC, Kao CH (2014). Increased subsequent risk of acute coronary syndrome for patients with depressive disorder: a nationwide population-based retrospective cohort study. Psychiatry and Clinical Neurosciences 68, 263–269. [DOI] [PubMed] [Google Scholar]
- Loerbroks A, Apfelbacher CJ, Bosch JA, Stürmer T (2010). Depressive symptoms, social support, and risk of adult asthma in a population-based cohort study. Psychosomatic Medicine 72, 309–315. [DOI] [PubMed] [Google Scholar]
- Mannino DM (2008). Doc, my asthma (depression) has gotten me down (wheezing). Chest 134, 1116–1117. [DOI] [PubMed] [Google Scholar]
- Mohanan S, Tapp H, McWilliams A, Dulin M (2014). Obesity and asthma: pathophysiology and implications for diagnosis and management in primary care. Experimental Biology and Medicine/Society for Experimental Biology and Medicine 239, 1531–1540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patten SB, Williams JV, Lavorato DH, Modgill G, Jetté N, Eliasziw M (2008). Major depression as a risk factor for chronic disease incidence: longitudinal analyses in a general population cohort. General Hospital Psychiatry 30, 407–413. [DOI] [PubMed] [Google Scholar]
- Postma DS, Rabe KF (2015). The asthma-COPD overlap syndrome. New England Journal of Medicine 373, 1241–1249. [DOI] [PubMed] [Google Scholar]
- Reddy MS (2010). Depression: the disorder and the burden. Indian Journal of Psychological Medicine 32, 1–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ritz T, Claussen C, Dahme B (2001). Experimentally induced emotions, facial muscle activity, and respiratory resistance in asthmatic and non-asthmatic individuals. British Journal of Medical Psychology 74, 167–182. [PubMed] [Google Scholar]
- Sanfiorenzo C, Pipet A (2011). Exacerbations of asthma–precipitating factors: drugs. Revue des Maladies Respiratoires 28, 1059–1070. [DOI] [PubMed] [Google Scholar]
- Shen TC, Tu CY, Lin CL, Wei CC, Li YF (2014). Increased risk of asthma in patients with systemic lupus erythematosus. American Journal of Respiratory and Critical Care Medicine 189, 496–499. [DOI] [PubMed] [Google Scholar]
- Shen TC, Lin CL, Wei CC, Chen CH, Tu CY, Hsia TC, Shih CM, Hsu WH, Sung FC (2015a). The risk of asthma in patients with ankylosing spondylitis: a population-based cohort study. PLoS ONE 10, e0116608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shen TC, Lin CL, Wei CC, Chen CH, Tu CY, Hsia TC, Shih CM, Hsu WH, Sung FC, Kao CH (2015b). Risk of obstructive sleep apnea in adult patients with asthma: a population-based cohort study in Taiwan. PLoS ONE 10, e0128461. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data and related metadata were deposited in an appropriate public repository. The data on the study population were obtained from the NHIRD (http://nhird.nhri.org.tw/). The National Health Research Institutes (NHRI) is a non-profit foundation established by the government. Only citizens of the Republic of China who fulfil the requirements of conducting research projects are eligible to apply for the NHIRD. The use of NHIRD is limited to research purposes only. Applicants must follow the Computer-Processed Personal Data Protection Law (http://www.winklerpartners.com/?p=987) and related regulations of National Health Insurance Administration and NHRI, and an agreement must be signed by applicants and their supervisors upon application submission. All applications are reviewed for approval of data release.