Abstract
Aims.
Little is known about outcomes of drug abuse related to attainment of stable housing. This study examined outcomes of cocaine use and service provision in an urban homeless sample.
Methods.
Two-year longitudinal study of systematically selected homeless individuals (N = 255) in St. Louis, Missouri from 1999 to 2001. The sample was interviewed three times annually using a structured diagnostic interview. Urine drug testing was conducted at every interview, and service utilisation data were obtained from the structured interviews and the agency-provided service use data.
Results.
Cocaine use disorder and cocaine use proved to be distinct concepts because they predicted different outcomes across time. Cocaine use predicted subsequent poor housing outcomes, but stable housing had no apparent effect on subsequent use of cocaine. Service use predicted neither subsequent reduced cocaine use nor attainment of stable housing. Services used were appropriate to type of mental health need, but cocaine use may have reduced successful utilisation of appropriate psychiatric services.
Conclusion.
These findings reinforce the concept that homelessness represents a complex phenomenon and consequently, service systems need to address multiple problems. Service approaches are needed that simultaneously address the complex needs of homeless individuals.
Key words: Cocaine use, homelessness, Housing First, psychiatric disorders, service utilisation, substance use disorder
Introduction
The association between homelessness and substance abuse has been a longstanding area of interest in the study of homeless populations. Studies using self-report or drug testing have indicated that the current prevalence of drug and alcohol abuse in the homeless populations are between 33 and 64% (Lambert & Caces, 1995; Appel et al. 2001; Stringfellow et al. 2016). The most prevalent current drugs of abuse in this population are marijuana and cocaine (O'Toole et al. 2004; Stringfellow et al. 2016). Studies published after the year 2000 have reported cocaine to be the most commonly used drug among the homeless, far above cannabis prevalence (Appel et al. 2001; North et al. 2010), in as many as 49–64% (Appel et al. 2001; O'Toole et al. 2004; North et al. 2010). Cocaine use has been linked to a failure to obtain and maintain stable housing (North et al. 2010). However, the role of service use in the relationship between cocaine use and housing outcomes was not explored, which is unique to this study.
Research prior to 1980 did not identify cocaine as a frequent drug of abuse among homeless populations. An epidemiologic study of homeless populations assessed at three different points in time a decade apart found no lifetime cocaine use disorders in 1980 but a decade later, cocaine surpassed marijuana in prevalence and rose even higher in the next decade (North et al. 2004b). At the last assessment, 93% of cocaine users were using the crack form of the drug (North et al. 2010). The advent of the crack form of cocaine produced a drug that was inexpensive and more widely available to homeless populations (Jencks, 1994; O'Toole et al. 2004; North et al. 2010), particularly minorities and women, and is thought to have been an important contributor to homelessness and especially to the influx of minorities, women and families into the homeless populations beginning in the 1980s (O'Toole et al. 2004; Stahler et al. 2005; North et al. 2010). Not surprisingly, the focus on drugs, specifically cocaine, was associated with a linear approach to services, in which achieving rehabilitation goals, particularly abstinence, was required as a precondition for receiving housing (Kertesz et al. 2009).
A model developed by Pathways to Housing for addressing substance use in the homeless population is Housing First. This model is based on housing as a basic right as well as the value of consumer choice. The program provides an apartment immediately without any prerequisites for sobriety. In addition to housing, opportunities are offered for treatment, support and other services. The goal is for people to be able to maintain stable housing without consideration of treatment for substance use (Tsemberis et al. 2004). In essence, Housing First is also a linear model with housing as the starting point. Housing First models have been studied predominantly for relatively mild alcohol use and suggest efficacy in maintaining stable housing (Tsemberis et al. 2004; Kertesz et al. 2009); however, there are limited data for this model in homeless participants with primarily cocaine use disorder (Kertesz et al. 2009). The lack of knowledge about outcomes of drug abuse with Housing First, precludes assumptions that Housing First will be as effective for drugs as for alcohol addiction. The increase of cocaine in homeless populations in recent decades emphasises the need for research that compares the starting points in the linearity of the order of services provision. The current study examines the order of service provision with respect to cocaine use and outcomes in a single representative urban homeless sample followed longitudinally for 2 years in a naturalistic study.
Methods
This study was approved by the Institutional Review Board of Washington University School of Medicine in St. Louis. All participants provided written informed consent. Previous publications have provided full details of the sampling procedures (Smith et al. 1992, 1993; North et al. 2012; Fuehrlein et al. 2014). In brief, participants were considered homeless if they did not have a stable address and stayed in a public shelter or an unsheltered location such as the street, a car, an abandoned building or a bus station. Participants who stayed in inexpensive motels or flophouses for <30 days or those who stayed with relatives or friends or in temporary single-room occupancy facilities for less than one half of the past 14 days were included. Systematic recruitment of 400 study participants from shelters and street locations proceeded from October 1999 through May 2001, and the sample was tracked for 2 years. 80% of the sample was randomly recruited from 12 homeless shelters proportionate to shelter size and the remainder of the sample was recruited through computer randomisation of 16 street routes covered systematically to screen all individuals encountered for current homelessness. The participation rate was 92%. Race/ethnicity was assessed as a standard part of the demographics section of the National Institute of Mental Health Diagnostic Interview Schedule (Robins et al. 1995), and for statistical parsimony, the variable used for this construct was simplified as a dichotomous minority/non-minority variable.
Of the 400 baseline participants, 255 (69%) of 371 of those eligible for follow-up (alive, not incarcerated, or not incapacitated) were reassessed in both follow-up years. No statistically significant differences were found between those followed up and not followed up for the entire 2 years of the study or between those with all three study assessments in baseline demographics, chronicity of homelessness, income, legal problems, substance use or any lifetime or current psychiatric disorders (North et al. 2012). Only the 255 participants with complete follow up data are included in the sample for the analyses in this paper.
All participants were assessed at baseline and one and two years later. All assessments included the socio-demographic sections of the National Comorbidity Study (Kessler et al. 1994), substance abuse sections of the Composite International Diagnostic Interview-Substance Abuse Module for DSM-III-R (Cottler & Compton, 1993), the Diagnostic Interview Schedule for DSM-IV (Robins et al., 1995), and the Homeless Supplement to the Diagnostic Interview Schedule (North et al. 2004a). These structured interviews provided full diagnostic assessment of lifetime and current psychiatric disorders including schizophrenia, bipolar disorder, major depression, panic disorder, generalised anxiety disorder, posttraumatic stress disorder, antisocial personality disorder and substance use disorders, as well as current housing status and details of all health and mental health services used during the previous year. Participants were considered stably housed at the end of the year if they had been housed in their own places for most of the past year. At each assessment, participants provided a urine sample, which was tested for alcohol, cannabis, cocaine, amphetamine and opiates using the Roche OnTRAK test kit.
Medical, mental health and substance abuse treatment agencies that delivered services to members of this sample provided data on services used by each individual. Service use data obtained from the structured interviews were combined with agency-provided service use data through procedures described in detail in a previous publication (Fuehrlein et al. 2014).
Missing data among the variables in the sample of 255 participants were managed for agency data by cross reference with self-report of service utilisation and then with multiple-imputation analysis as described in further detail in a previous publication (Fuehrlein et al. 2014). In summary, multiple imputation applied with 5000 iterations was used to replace missing values with plausible values specified based on known associations with the variables to be imputed for age, sex, ethnic minority, housing status and cocaine use.
Variables were created to represent lifetime diagnosis of alcohol and cocaine use disorder identified at any assessment in the study. A convention in the literature for defining ‘serious mental illness’ includes schizophrenia, bipolar disorder and major depression (Drake et al. 2007). Therefore, a variable representing serious mental illness was created for this study consisting of the same three psychiatric disorders. Self-report and urine substance testing data were combined to create a variable for cocaine use in the last year.
The health service use categories explored in this study were medical services, psychiatric services and substance abuse services. Medical services included medical emergency care visits, medical inpatient and outpatient care, use of medical supplies and pharmacy services. Psychiatric services included inpatient, outpatient, emergency, day treatment programs and pharmacy services. Types of psychiatric services included psychiatric case management, psychotropic medication management and individual and group psychotherapy. Substance use services included inpatient, residential and outpatient treatment. Types of substance abuse services were individual and group psychotherapy for substance abuse, psychotropic medication management for substance abuse and self-help groups such as Alcoholics Anonymous and Narcotics Anonymous.
Statistical analysis
Generalised estimating equation (GEE) models were used (PROC GENMOD in SAS) to predict outcomes related to cocaine use, type of service use and stable housing (dependent variables, one model for each) in the first and second years. Independent variables simultaneously included in these models were lifetime diagnosis at any time in the study of cocaine use disorder, alcohol use disorder, or serious mental illness and current cocaine use disorder, stable housing, and medical, psychiatric and substance service use; additional independent covariates also included simultaneously in these models controlled for age, sex and minority group membership status. For these models, only the variables for the first year were included in models with a first year dependent variable, and both first and second year variables were included in models with a second year dependent variable.
Results
Baseline demographic characteristics of the study sample (N = 255) were previously described (North et al. 2010; Fuehrlein et al. 2014). The sample was predominantly male (73%), African American (77%), relatively young (median = 43 years) and 60% high school graduates or educational equivalency. Nearly two thirds (64%) had ever experienced legal problems and 22% in the last month.
Over the course of the 2-year study, 50% (N = 127) were identified as having a lifetime cocaine use disorder, including 113 diagnosed at baseline and 14 others at subsequent assessments. During the study, 61% (N = 156) were diagnosed with a lifetime alcohol use disorder, including 151 at baseline and five others at subsequent assessments. Of the 127 diagnosed with a lifetime cocaine use disorder at any time in the study, 75% (N = 95) had used cocaine in the year prior to baseline. In the first study year, cocaine use in this group declined significantly (S = 10.37, p = 0.001) to 57% (N = 72) and in the second study year further declined significantly (S = 5.23, p = 0.022) to 45% (N = 57).
More than half of the sample (56%, N = 142) was diagnosed with lifetime serious mental illness at any time in the study, 11% (N = 16) had lifetime schizophrenia, 37% (N = 52) had lifetime bipolar disorder and 76% (N = 108) had lifetime major depressive disorder.
Table 1 presents a series of multivariate GEE models (one per row) predicting outcomes (dependent variables) of cocaine use, service use and stable housing in the first year. Cocaine use in the first year had a strong positive relationship with both lifetime cocaine and alcohol use disorders and a significant association with minority group membership. Cocaine use in the first year was negatively associated with medical service use in the same year. Both lifetime cocaine and alcohol use disorders had a strong positive relationship with substance service use in the first year. Cocaine use in the first year was not associated with substance service use in that year. Substance service use in the first year was positively associated with both medical and psychiatric service use in the same year. Psychiatric service use in the first year had a strong positive relationship with lifetime serious mental illness. Women were more likely to obtain stable housing in the first year, but obtaining housing was unrelated to cocaine use, cocaine use disorder, serious mental illness, or any service use in that year.
Table 1.
Multivariate GEE models (one per row) predicting year 1 outcomes related to cocaine use, service use and stable housing in year 1 in a prospective longitudinal 2 year study of a systematically selected homeless sample (N = 255) in St. Louis, Missouri completed in 2001
| Year 1 Dependent Variable | Lifetime cocaine use disorder | Lifetime alcohol use disorder | Lifetime serious mental illness | Cocaine use | Medical service use | Psychiatric service use | Substance service use | Stable housing | Male sex | Age | Minority group membership |
|---|---|---|---|---|---|---|---|---|---|---|---|
| (Significant p values only) | |||||||||||
| Cocaine use | <0.001a | 0.006b | 0.025c | 0.031d | |||||||
| Medical service use | 0.018e | 0.004f | |||||||||
| Psychiatric service use | <0.001g | 0.001h | |||||||||
| Substance service use | 0.001i | 0.037j | 0.004k | 0.001l | |||||||
| Stable housing | 0.007m | ||||||||||
Relationships in cells with gray shading are negative. All other listed associations are positive.
Y1 = year 1, Y2 = year 2.
E = 2.00; SE = 0.36; 95% CI = 1.29, 2.71; Z = 5.54.
E = 1.03; SE = 0.37; 95% CI = 0.30, 1.76; Z = 2.78.
E = −0.80; SE = 0.36; 95% CI = −1.50, −0.10; Z = −2.24.
E = 1.13; SE = 0.52; 95% CI = 0.10, 2.16; Z = 2.15.
E = −0.83; SE = 0.35; 95% CI = −1.52, −0.14; Z = −2.37.
E = 1.01; SE = 0.35; 95% CI = 0.32, 1.70; Z = 2.88.
E = 1.42; SE = 0.31; 95% CI = 0.81, 2.02; Z = 4.59.
E = 1.07; SE = 0.32; 95% CI = 0.44, 1.69; Z = 3.35.
E = 1.08; SE = 0.34; 95% CI = 0.42, 1.74; Z = 3.21.
E = 0.73; SE = 0.35; 95% CI = 0.05, 1.41; Z = 2.09.
E = 1.03; SE = 0.35; 95% CI = 0.34, 1.73; Z = 2.92.
E = 1.07; SE = 0.31; 95% CI = 0.46, 1.68; Z = 3.43.
E = −0.98; SE = 0.36; 95% CI = −1.69, −0.27; Z = −2.69.
E, estimate; SE, standard error; CI, confidence interval.
Table 2 presents a series of multivariate GEE models (one per row) predicting outcomes (dependent variables) of cocaine use, service use and stable housing in the second year. All variables in the first year were strongly associated with themselves in the second year. In the second year, cocaine use was strongly associated with lifetime cocaine use disorder, but cocaine use was no longer associated with lifetime alcohol use disorder. Cocaine use in the second year was positively associated with substance service use and negatively associated with psychiatric service use in the same year. Lifetime cocaine use disorder in the second year was positively associated with substance service use in the same year. Medical and substance use services were no longer associated in the second year. Psychiatric service use in the second year was positively associated with medical and substance service use in the same year. Psychiatric service use in the second year was predicted by both lifetime serious mental illness and cocaine use disorder. Lack of stable housing in the first year predicted psychiatric service use in the second year. Stable housing in the second year was negatively predicted by cocaine use in the first year and positively associated with lifetime cocaine disorder. Women were still more likely to be stably housed than men in the second year. Stable housing in the second year was not associated with any type of service use in either year.
Table 2.
Multivariate GEE models (one per row) predicting year 2 outcomes related to cocaine use, service use, and stable housing in year 1 and 2 in a prospective longitudinal 2 year study of a systematically selected homeless sample (N = 255) in St. Louis, Missouri completed in 2001
| Year 2 Dependent Variable | Lifetime cocaine use disorder | Lifetime alcohol use disorder | Lifetime serious mental illness | Cocaine use | Medical service use | Psychiatric service use | Substance service use | Stable housing | Male sex | Age | Minority group membership |
|---|---|---|---|---|---|---|---|---|---|---|---|
| (Significant p values only) | |||||||||||
| Cocaine use | <0.001a | Y1 <0.001b | |||||||||
| Y2 0.012c | |||||||||||
| Medical service use | Y1 <0.001d | ||||||||||
| Y2 <0.001e | |||||||||||
| Psychiatric service use | 0.040f | 0.002g | Y1 <0.001j | Y1 0.013l | 0.039m | ||||||
| Y2 0.013h | Y2 <0.001i | Y2 0.010k | |||||||||
| Substance service use | 0.004n | Y1 <0.001q | |||||||||
| Y2 0.040o | Y2 0.013p | ||||||||||
| Stable housing | 0.028r | Y1 0.018s | Y1 <0.001t | 0.014u | |||||||
Relationships in cells with gray shading are negative. All other listed associations are positive.
Y1 = year 1, Y2 = year 2. In rows with significant findings in more than 1 year, Y1 results are placed on the first line and Y2 results are placed on the second line.
E = 2.24; SE = 0.55; 95% CI = 1.16, 3.33; Z = 4.06.
E = 1.69; SE = 0.44; 95% CI = 0.83, 2.55; Z = 3.87.
E = −1.44; SE = 0.58; 95% CI = −2.57, −0.32; Z = −2.51.
E = 2.06; SE = 0.36; 95% CI = 1.35, 2.76; Z = 5.71.
E = 1.79; SE = 0.47; 95% CI = 0.87, 2.72; Z = 3.79.
E = 0.98; SE = 0.48; 95% CI = 0.04, 1.91; Z = 2.05.
E = 1.38; SE = 0.44; 95% CI = 0.51, 2.25; Z = 3.11.
E = −1.48; SE = 0.59; 95% CI = −2.65, −0.32; Z = −2.50.
E = 2.06; SE = 0.53; 95% CI = 1.03, 3.09; Z = 3.91.
E = 2.32; SE = 0.46; 95% CI = 1.42, 3.21; Z = 5.07.
E = 1.45; SE = 0.56; 95% CI = 0.34, 2.55; Z = 2.57.
E = −1.48; SE = 0.59; 95% CI = −2.65, −0.32; Z = −2.50.
E = −0.94; SE = 0.46; 95% CI = −1.84, −0.05; Z = −2.07.
E = 1.25; SE = 0.44; 95% CI = 0.39, 2.10; Z = 2.85.
E = 0.87; SE = 0.43; 95% CI = 0.04, 1.70; Z = 2.05.
E = 1.27; SE = 0.51; 95% CI = 0.27, 2.27; Z = 2.50.
E = 1.53; SE = 0.39; 95% CI = 0.77, 2.30; Z = 3.91.
E = 0.83; SE = 0.38; 95% CI = 0.09, 1.58; Z = 2.19.
E = −0.91; SE = 0.39; 95% CI = −1.67, −0.16; Z = −2.36.
E = 1.27; SE = 0.33; 95% CI = 0.62, 1.91; Z = 3.83.
E = −0.98; SE = 0.40; 95% CI = −1.76, −0.19; Z = −2.44.
E, estimate; SE, standard error; CI, confidence interval.
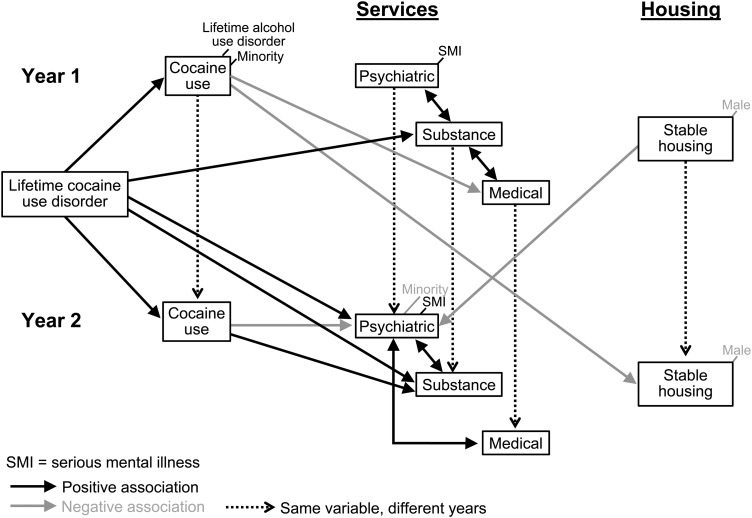
Figure 1 provides a visual model of these results, with black arrows and text referring to positive associations and gray arrows and text to negative associations. Conceptually the model was constructed with stable housing as the final outcome of interest in both years, with cocaine use and service utilisation representing intermediate variables predicting subsequent outcomes.
Fig. 1.
The visual model of the relationship between cocaine use, service utilisation, and stable housing.
Discussion
This 2-year prospective study of a systematically assessed homeless sample examined the temporal associations of cocaine use and abuse in the context of longitudinal housing status and health service utilisation over time. In this study, individuals who used cocaine in the first year were somewhat less likely to have stable housing in the second year, demonstrating a moderate lagged time effect of cocaine use on subsequent housing status. Conversely, no lagged effect was observed from stable housing in the first year to cocaine use in the second year. Thus, cocaine use appeared to affect later ability to obtain housing, but housing had no effect on use of cocaine. This suggests that abstinence from cocaine may be important for efforts to gain housing, but housing-focused models do not appear to have any long term effects on cocaine use. Another study concluded that once the effects of other variables are accounted for, homeless status does not affect general substance use (McVicar et al. 2015). Therefore, based on these findings, substance abuse treatment that successfully decreases cocaine use will be required in addition to provision of housing to successfully address the important role of cocaine use in perpetuation of homelessness. In support of this assumption, a recent study also suggested that additional assistance will be needed to address substance use once stable housing is obtained (Tsai et al. 2014). In this study, serious mental illness was not associated with stable housing. The findings of this study indicate that cocaine use but not serious mental illness is relevant to housing outcomes.
In both years, service use was appropriate for the identified psychiatric disorders (e.g., psychiatric services for serious mental illness and substance abuse services for alcohol and cocaine use disorders). In the first year, cocaine users were less likely than others to utilise medical services. In the second year, psychiatric services were negatively associated with cocaine use, suggesting the possibility that cocaine served as a barrier to or was used instead of seeking psychiatric services. Psychiatric and substance abuse services demonstrated no detectable benefits for cocaine abstinence or attainment of housing.
Strengths of this study include a large systematic selection of clearly defined homeless participants from street locations and shelters, utilisation of a structured diagnostic interview, annual reassessment of participants, 2 year length of follow up, successful retention rate and absence of attrition bias on important variables. In addition, combined data source of both self-report and objective data collected from the agencies and substance testing of urine sample provides for more comprehensive findings. In analysing the data, GEE models were used to control for repeated assessments on the same individuals within a particular model. In the case of missing agency data, multiple-imputation procedures were used to replace the missing values with plausible values based on other variables with known associations to the missing variables. Further descriptions of the study strengths have been described in detail in previous publications by the research team (North et al. 2010; Fuehrlein et al. 2014).
Although this study had clear strengths, it also had some noteworthy limitations. The data collection was limited to one city, St. Louis and as a result, may not generalise to other regions. For example, geographical variation has been demonstrated in social and medical variables associated with environmental deprivation (Carrà et al. 2016), but other studies have found more geographical consistency for other variables such as prevalence of psychiatric disorders (Koegel et al. 1988; Smith et al. 1992). The study spanned a time period of over a decade ago; therefore, the data may no longer represent the current situation of the homeless population. For example, it has been found that the prevalence of psychiatric disorders and especially cocaine use disorder changed substantially in the two decades between 1980 and 2000 (North et al. 2004b), and it is possible that further change in the prevalence rates followed in the subsequent two decades. Consequently, these changes could be reflected in different patterns of service utilisation and housing outcomes. Agency data were incomplete especially the year before individual baseline interviews and the study did not measure the utilisation of the criminal justice system. Measurement of the variables of interest was dichotomous with the exception of age, and therefore the analysis cannot establish dosage effects.
Overall, this study's findings appear to suggest three overarching conclusions: (1) obtaining stable housing did not reduce cocaine use, but cocaine use negatively affected housing outcomes, suggesting that housing-focused models may not be optimal for cocaine-using homeless subgroups; (2) use of services did not improve housing outcomes; and (3) cocaine use disorder is a separate concept from current cocaine use in its associations with service use and housing outcomes. Taken as a whole, these findings reinforce the concept that homelessness represents a complex phenomenon and consequently service use needs to address multiple needs. The concept that services addressing single needs represent a panacea for homeless needs is not supported by these data. Rather, the findings appear to support approaches tailored to the specific and varied needs of homeless individuals. For example, housing-focused services (such as Housing First) could be appropriate for homeless individuals without cocaine use. Conversely, multiple services would be required and additional outcomes would need to be examined for homeless individuals with various comorbidities. The conclusions suggest the need to move beyond linear approaches by including housing first and treatment first models in service systems, by combining service types based on the specific needs of individuals.
This study found that service use provided no positive benefits for promoting abstinence from cocaine or attainment of stable housing. The amount of services used with no drug use or housing favourable outcomes represents some investment without a specific cost return. A fruitful direction for future inquiry would be to characterise costs associated with service use and achievement of stable housing especially for persons using cocaine. Additionally, research will be needed to examine the specific effects of comorbidities involving substance use and other psychiatric disorders in association with service use.
Acknowledgements
None.
Financial Support
This study was funded by grant R01 DA10713 to Dr North from the National Institute on Drug Abuse and by the National Institute of Mental Health of the National Institute of Health under Award Number R25MH101078. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Health.
Conflict of Interest
None.
Ethical Standards
The authors assert that all procedures contributing to this work comply with ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
Availability of Data and Materials
Because the dataset includes identifiable patient information and relevant privacy regulations prohibit dissemination, data utilised in this study are not available for sharing.
References
- Appel PW, Hoffman JH, Blane HT, Frank B, Oldak R, Burke M (2001). Comparison of self-report and hair analysis in detecting cocaine use in a homeless/transient sample. Journal of Psychoactive Drugs 33, 47–55. [DOI] [PubMed] [Google Scholar]
- Carrà G, Crocamo C, Borrelli P, Tabacchi T, Bartoli F, Popa I, Montomoli C, Clerici M (2016). Area-level deprivation and adverse consequences in people with substance use disorders: findings from the Psychiatric and Addictive Dual Disorder in Italy (PADDI) Study. Substance Use & Misuse 52, 1–8. [DOI] [PubMed] [Google Scholar]
- Cottler LB, Compton WM (1993). Advantages of the CIDI family of instruments in epidemiological research of substance use disorders. International Journal of Methods in Psychiatric Research 3, 109–119. [Google Scholar]
- Drake RE, Mueser KT, Brunette MF (2007). Management of persons with co-occurring severe mental illness and substance use disorder: program implications. World Psychiatry 6, 131–136. [PMC free article] [PubMed] [Google Scholar]
- Fuehrlein BS, Cowell AJ, Pollio DE, Cupps LY, Balfour ME, North CS (2014). Deriving costs of service use among an urban homeless population. Journal of Substance Abuse Treatment 46, 491–497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jencks C (1994). The Homeless. Harvard University Press: Cambridge, Massachusetts. [Google Scholar]
- Kertesz SG, Crouch K, Milby JB, Cusimano RE, Schumacher JE (2009). Housing first for homeless persons with active addiction: are we overreaching? Milbank Q 87, 495–534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, Wittchen H-U, Kendler KS (1994). Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: results from the National Comorbidity Survey. Archives of General Psychiatry 51, 8–19. [DOI] [PubMed] [Google Scholar]
- Koegel P, Burnam MA, Farr RK (1988). The prevalence of specific psychiatric disorders among homeless individuals in the inner city of Los Angeles. Archives of General Psychiatry 45, 1085–1092. [DOI] [PubMed] [Google Scholar]
- Lambert EY, Caces MF (1995). Correlates of drug abuse among homeless and transient people in the Washington, DC, metropolitan area in 1991. Public Health Reports 110, 455–461. [PMC free article] [PubMed] [Google Scholar]
- McVicar D, Moschion J, van Ours JC (2015). From substance use to homelessness or vice versa? Social Science & Medicine 136, 89–98. [DOI] [PubMed] [Google Scholar]
- North CS, Eyrich KM, Pollio DE, Foster DA, Cottler LB, Spitznagel EL (2004a). The homeless supplement to the diagnostic interview schedule: test-retest analyses. International Journal of Methods in Psychiatric Research 13, 184–191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- North CS, Eyrich KM, Pollio DE, Spitznagel EL (2004b). Are rates of psychiatric disorders in the homeless population changing? American Journal of Public Health 94, 103–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- North CS, Eyrich-Garg KM, Pollio DE, Thirthalli J (2010). A prospective study of substance use and housing stability in a homeless population. Social Psychiatry and Psychiatric Epidemiology 45, 1055–1062. [DOI] [PubMed] [Google Scholar]
- North CS, Black M, Pollio DE (2012). Predictors of successful tracking over time in a homeless population. Social Work Research 36, 153–159. [Google Scholar]
- O'Toole TP, Conde-Martel A, Gibbon JL, Hanusa BH, Freyder PJ, Fine MJ (2004). Substance-abusing urban homeless in the late 1990s: how do they differ from non-substance-abusing homeless persons? Journal of Urban Health 81, 606–617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robins L, Cottler L, Bucholz K, Compton W (1995). Diagnostic Interview Schedule for the DSM-IV (DIS-IV). Washington University: St Louis, MO. [Google Scholar]
- Smith EM, North CS, Spitznagel EL (1992). A systematic study of mental illness, substance abuse, and treatment in 600 homeless men. Annals of Clinical Psychiatry 4, 111–120. [Google Scholar]
- Smith EM, North CS, Spitznagel EL (1993). Alcohol, drugs, and psychiatric comorbidity among homeless women: an epidemiologic study. Journal of Clinical Psychiatry 54, 82–87. [PubMed] [Google Scholar]
- Stahler GJ, Shipley TE Jr.,, Kirby KC, Godboldte C, Kerwin ME, Shandler I, Simons L (2005). Development and initial demonstration of a community-based intervention for homeless, cocaine-using, African-American Women. Journal of Substance Abuse Treatment 28, 171–179. [DOI] [PubMed] [Google Scholar]
- Stringfellow EJ, Kim TW, Gordon AJ, Pollio DE, Grucza RA, Austin EL, Johnson NK, Kertesz SG (2016). Substance use among persons with homeless experience in primary care. Substance Abuse 37, 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai J, Kasprow WJ, Rosenheck RA (2014). Alcohol and drug use disorders among homeless veterans: prevalence and association with supported housing outcomes. Addictive Behaviors 39, 455–460. [DOI] [PubMed] [Google Scholar]
- Tsemberis S, Gulcur L, Nakae M (2004). Housing First, consumer choice, and harm reduction for homeless individuals with a dual diagnosis. American Journal of Public Health 94, 651–656. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Because the dataset includes identifiable patient information and relevant privacy regulations prohibit dissemination, data utilised in this study are not available for sharing.