Abstract
Aims.
The study aimed to examine variations in the use of International Classification of Diseases, Tenth Edition (ICD-10) diagnostic categories for mental and behavioural disorders across countries, regions and income levels using data from the online World Psychiatric Association (WPA)-World Health Organization (WHO) Global Survey that examined the attitudes of psychiatrists towards the classification of mental disorders.
Methods.
A survey was sent to 46 psychiatric societies which are members of WPA. A total of 4887 psychiatrists participated in the survey, which asked about their use of classification, their preferred system and the categories that were used most frequently.
Results.
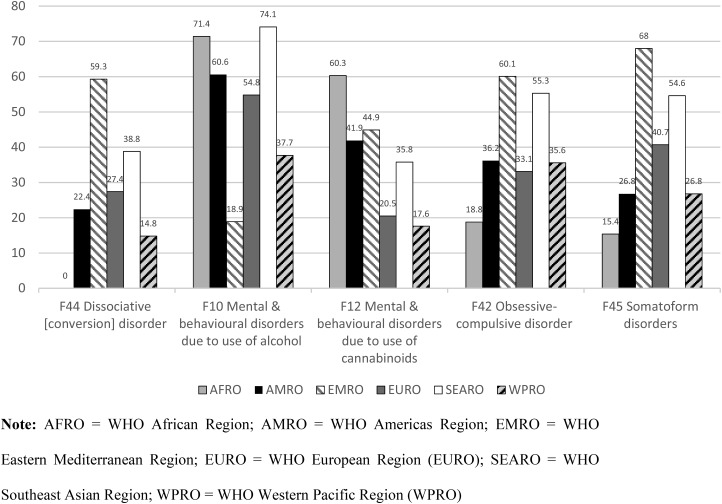
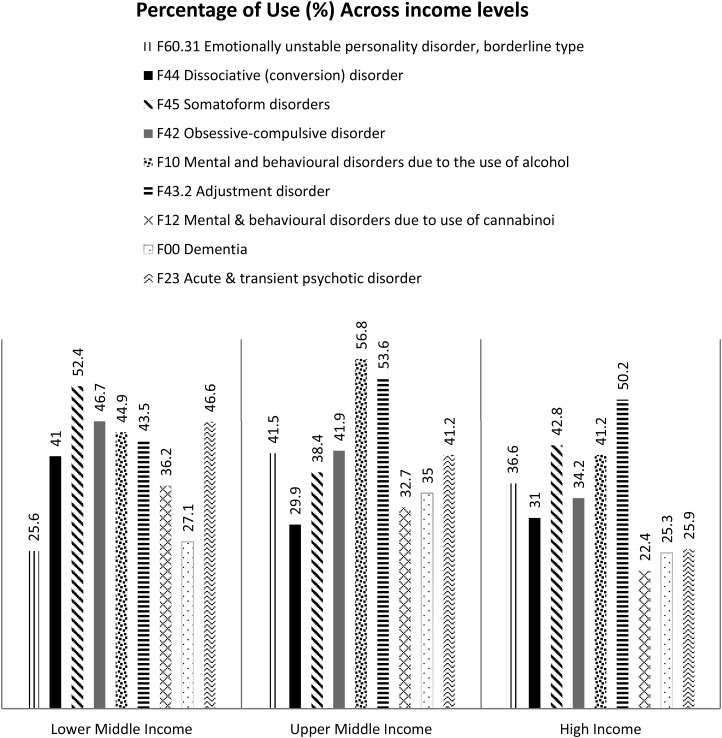
The majority (70.1%) of participating psychiatrists (out of 4887 psychiatrists) reported using the ICD-10 the most and using at least one diagnostic category once a week. Nine out of 44 diagnostic categories were considerably variable in terms of frequency of use across countries. These were: emotionally unstable personality disorder, borderline type; dissociative (conversion) disorder; somatoform disorders; obsessive–compulsive disorder (OCD); mental and behavioural disorders due to the use of alcohol; adjustment disorder; mental and behavioural disorders due to the use of cannabinoids; dementia in Alzheimer's disease; and acute and transient psychotic disorder. The frequency of use for these nine categories was examined across WHO regions and income levels. The most striking differences across WHO regions were found for five out of these nine categories. For dissociative (conversion) disorder, use was highest for the WHO Eastern Mediterranean Region (EMRO) and non-existent for the WHO African Region. For mental and behavioural disorders due to the use of alcohol, use was lowest for EMRO. For mental and behavioural disorders due to the use of cannabinoids, use was lowest for the WHO European Region and the WHO Western Pacific Region. For OCD and somatoform disorders, use was lowest for EMRO and the WHO Southeast Asian Region. Differences in the frequency of use across income levels were statistically significant for all categories except for mental and behavioural disorders due to the use of alcohol. The most striking variations were found for acute and transient psychotic disorder, which was reported to be more commonly used among psychiatrists from countries with lower income levels.
Conclusions.
The differences in frequency of use reported in the current study show that cross-cultural variations in psychiatric practice exist. However, whether these differences are due to the variations in prevalence, treatment-seeking behaviour and other factors, such as psychiatrist and patient characteristics as a result of culture, cannot be determined based on the findings of the study. Further research is needed to examine whether these variations are culturally determined and how that would affect the cross-cultural applicability of ICD-10 diagnostic categories.
Key words: Cross-cultural applicability, diagnosis, International Classification of Diseases (ICD), mental disorders, classification
Introduction
The World Health Organization (WHO) is developing the 11th Revision of the International Classification of Diseases and Related Health Problems (ICD-11). The current version of the classification, the International Classification of Diseases, Tenth Edition (ICD-10), was approved in 1990 (World Health Organization, 1992). The Department of Mental Health and Substance Abuse is responsible for coordinating the development of the ICD-11 chapter on mental and behavioural disorders with the guidance of an International Advisory Group including representatives of several international professional societies such as the World Psychiatric Association (WPA). One of the main aims of the development of the ICD-11 classification of mental disorders is to improve the clinical utility of the classification system across health settings and cultural contexts (Reed, 2010; International Advisory Group for the Revision of ICD-10 Mental and Behavioral Disorders, 2011).
To provide context for this revision, it has been important to obtain the views of global mental health professionals regarding key issues relevant to the classification of mental disorders. This current study represents a secondary analysis of data collected by the WHO in collaboration with WPA and 46 WPA Member Societies (national psychiatric societies) regarding psychiatrists’ experiences and attitudes towards mental disorders classification (Reed et al. 2011). The sample of participants in the survey included 4887 psychiatrists in 44 countries. This was the largest and most broad international survey of psychiatrists’ views of mental disorders classification ever conducted, and produced several important recommendations that have informed the ICD-11 development process. A subsequent analysis provided additional information regarding categories the psychiatrists considered particularly problematic or stigmatising, as well as categories that should be added to the classification (Robles et al. 2014), which also provided a part of the basis for specific ICD-11 proposals.
Objective
The aim of the current study was to examine regional variations in the use of ICD-10 diagnostic categories for mental and behavioural disorders using data from the WPA-WHO Global Survey (Reed et al. 2011). Regional variations were considered likely given the cross-national differences in the prevalence of specific mental disorders (Demyttenaere et al. 2004; Baxter et al. 2014), as well as differences in health care delivery systems that affect patterns of service provision by psychiatrists (World Health Organization, 2014; Robles et al. 2015). It is important to consider such differences as part of the development of the ICD-11 classification of mental disorders, as patterns of use will likely have an influence on clinical utility and global applicability.
Method
The methodology for this study was described in detail elsewhere (Reed et al. 2011). Briefly, WPA Member Societies were invited by the WPA and the WHO to participate in an online international survey examining the attitudes of psychiatrists towards the classification of mental disorders. A total of 46 WPA Member Societies in 44 countries completed the survey. The survey was translated into 19 languages, following an explicit translation protocol using forward and back-translation methodology. Participating WPA Member Societies sent a standard initial solicitation message (provided by the WHO) by e-mail or regular mail to selected members, followed by reminder messages at 2 and 6 weeks. Societies with fewer than 1000 members were asked to solicit all eligible members for participation, and societies with more than 1000 members were asked to select a random sample of 500 eligible members for solicitation. Eligible members were defined as those who had completed their training as psychiatrists and were legally authorised in their countries to provide psychiatric services to patients.
For members of each society, solicitation messages contained a link to a survey webpage specific for that society, which provided information about the purpose of the survey, the confidential and voluntary nature of participation, its exempt status from WHO's Research Ethics Review Committee, the time required to participate and relevant contacts in case the potential respondent had questions or any comments. Two Societies – the Cuban Society of Psychiatry and the Pakistan Psychiatric Society – participated using a paper-and-pencil version of the survey because of the difficulties with Internet-based participation. Data were collected during a period of 11 months beginning in May 2010.
In the current study, the statistical analyses focused on the ICD-10 categories that varied most across countries in the percentage of clinicians who used them. For each disorder, countries’ percentages of usage were ordered from highest to lowest and the moment-to-moment slopes were calculated. An average of those slopes for each category, which indicated the degree of variability in disorder usage across countries, was created. The nine most variable diagnostic categories were selected for further analysis (with an average slope >2).
A series of hierarchical logistic regressions were conducted for those diagnoses to predict individual clinicians’ propensity to endorse using the category at least once a week or not. In all analyses, the total number of diagnostic categories used by the individual was entered in the first step to control for individual differences in the propensity to endorse using any given category. In the second step, the WHO regional classification for the individual's current country of residence was entered. This step accounted for regional differences in the usage of these categories beyond those already accounted for by individual differences. In a third step, the country income level as classified by the World Bank was added as a predictor beyond the previous two variables. Country income level consisted of three levels: lower middle income; upper middle income and high income (the two categories ‘low income’ and ‘lower middle income’ were combined into one category and labelled ‘lower middle income’).
Results
A total of 4887 psychiatrists participated in the study. By WHO region, the sample included 83 psychiatrists from the WHO African Region (AFRO), essentially comprising sub-Saharan Africa; 540 from the WHO Americas Region, including North, Central and South America and the Caribbean; 315 from the WHO Eastern Mediterranean Region (EMRO); 2774 from the WHO European Region (EURO); 463 from the WHO Southeast Asian Region (SEARO) and 712 from the WHO Western Pacific Region (WPRO).
Participants who saw patients were asked to indicate which classification system for mental disorders they used the most in their day-to-day clinical practice. Overall, 70.1% of participating psychiatrists reported that the ICD-10 was the classification system they used the most. Psychiatrists who indicated that they saw patients and used the ICD-10 the most in day-to-day clinical practice were asked to indicate which of a list of 44 ICD-10 diagnostic categories (Reed et al. 2011) they used at least once a week in their day-to-day clinical practice. The analyses presented in this article included a subsample of 3010 psychiatrists (61.6% of the total sample) from 42 countries who indicated that they used at least one ICD-10 diagnostic category once a week or more. Participants from Kenya (n = 14) and from the USA (n = 91) indicated that they used the Diagnostic and Statistical Manual of Mental Disorders (DSM) most often in clinical practice and, thus, were not included in the analyses presented in this article. Patterns of use of specific ICD-10 diagnostic categories were examined across countries, WHO regions and country income levels.
The nine most variable diagnostic categories across countries were selected for further analysis. These were: F60.31 emotionally unstable personality disorder, borderline type; F44 dissociative (conversion) disorder; F45 somatoform disorders; F42 obsessive–compulsive disorder (OCD); F10 mental and behavioural disorders due to the use of alcohol; F43.2 adjustment disorder; F12 mental and behavioural disorders due to the use of cannabinoids; F00 dementia in Alzheimer's disease; and F23 acute and transient psychotic disorder. Patterns of use across countries for all of these categories had an average slope >2. However, selecting these nine disorders does not mean that variations in use for all of these categories were dramatic; most were used at relatively consistent rates across countries.
The logistic regression analyses generated significant results (see Table 1). First, across all nine disorders, the total number of diagnostic categories used by the individual was a significant predictor of usage (all p < 0.001). In the second step, the WHO regional classification for the individual's current country of residence accounted for regional differences in the usage of these categories beyond those already accounted for by individual differences in the total number of categories used. In a third step, in all cases except for mental and behavioural disorders due to alcohol (F10), the country income level was a significant predictor in addition to the variability already accounted for by the individual use of categories and WHO region. For F10, country income approached significance (p = 0.061).
Table 1.
Logistic regression results for the nine diagnostic categories
| F00 | F10 | F12 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| −2 Log likelihood | Nagelkerke R2 | Wald | −2 Log likelihood | Nagelkerke R2 | Wald | −2 Log likelihood | Nagelkerke R2 | Wald | |
| Block 1 | 3309.22 | 0.216 | 3537.25 | 0.245 | 2797.83 | 0.225 | |||
| Number of categories used | 404.60** | 444.56** | 391.62** | ||||||
| Block 2 | 3142.44 | 0.279 | 3289.58 | 0.331 | 2604.57 | 0.304 | |||
| Number of categories used | 379.75** | 425.36** | 383.14** | ||||||
| WHO region | 160.02** | 179.43** | 117.10** | ||||||
| Block 3 | 3088.09 | 0.299 | 3283.98 | 0.333 | 2509.87 | 0.341 | |||
| Number of categories used | 378.63** | 425.47** | 388.56** | ||||||
| WHO region | 194.19** | 183.60** | 172.24** | ||||||
| Income level | 47.19** | 5.59 | 78.03** | ||||||
| F23 | F42 | F43.2 | |||||||
| −2 Log likelihood | Nagelkerke R2 | Wald | −2 Log likelihood | Nagelkerke R2 | Wald | −2 Log likelihood | Nagelkerke R2 | Wald | |
| Block 1 | 2970.48 | 0.330 | 2958.29 | 0.410 | 3540.16 | 0.250 | |||
| Number of categories used | 558.12** | 657.88** | 455.21** | ||||||
| Block 2 | 2863.18 | 0.368 | 2846.68 | 0.444 | 3461.01 | 0.278 | |||
| Number of categories used | 510.58** | 607.60** | 440.65** | ||||||
| WHO region | 99.01** | 107.19** | 64.04** | ||||||
| Block 3 | 2735.71 | 0.411 | 2839.54 | 0.446 | 3412.58 | 0.295 | |||
| Number of categories used | 517.12** | 608.31** | 436.66** | ||||||
| WHO region | 80.57** | 72.78** | 52.38** | ||||||
| Income level | 125.24** | 7.25* | 44.83** | ||||||
| F44 | F45 | F60.31 | |||||||
| −2 Log likelihood | Nagelkerke R2 | Wald | −2 Log likelihood | Nagelkerke R2 | Wald | −2 Log likelihood | Nagelkerke R2 | Wald | |
| Block 1 | 3025.85 | 0.294 | 3360.67 | 0.309 | 3435.65 | 0.281 | |||
| Number of categories used | 509.84** | 544.15** | 506.83** | ||||||
| Block 2 | 2638.64 | 0.428 | 3117.57 | 0.388 | 3209.67 | 0.357 | |||
| Number of categories used | 491.38** | 536.38** | 566.73** | ||||||
| WHO region | 308.35** | 197.32** | 190.64** | ||||||
| Block 3 | 2584.91 | 0.445 | 3103.79 | 0.393 | 3024.27 | 0.416 | |||
| Number of categories used | 491.84** | 535.54** | 575.30** | ||||||
| WHO region | 130.21** | 122.85** | 52.75** | ||||||
| Income level | 54.12** | 13.79** | 162.30** | ||||||
Note: *p < 0.05; **p < 0.001.
Discussion
Although variations in use across WHO regions were statistically significant for all nine diagnostic categories, the most striking differences across WHO regions were found for F44 dissociative (conversion) disorder, F10 mental and behavioural disorders due to the use of alcohol, F12 mental and behavioural disorders due to the use of cannabinoids, F42 OCD and F45 somatoform disorders (see Fig. 1).
Fig. 1.
Percentage of psychiatrists who reported using specific diagnostic categories at least once per week, by region. Note: AFRO, WHO African Region; AMRO, WHO Americas Region; EMRO, WHO Eastern Mediterranean Region; EURO, WHO European Region (EURO); SEARO, WHO Southeast Asian Region; WPRO, WHO Western Pacific Region (WPRO).
The most discrepant rates of use for F44 dissociative (conversion) disorder among participating psychiatrists were observed for AFRO (0%) and EMRO (59.3%). The lack of use of F44 among psychiatrists in AFRO may be related to socio-cultural factors that may affect help-seeking behaviour, such as the use of traditional healers for particular types of symptoms (Van Duijl et al. 2005). Higher rates of dissociative and conversion disorders in the EMRO region have been noted in previous literature (Okasha & Dawla, 1992; Chand et al. 2000). Some authors have speculated that this could be partly due to the stress to which people are subjected as they attempt to adjust to accelerated development and the rapid socio-cultural changes in the region (Chand et al. 2000), but these are also characteristics of developing countries in other parts of the world.
The use of F10 mental and behavioural disorders due to the use of alcohol by participating psychiatrists was much lower in the EMRO region (18.9%) as compared with other WHO regions (37.7–74.1%). These findings are consistent with available epidemiological data from the Arab region showing lower rates of disorders due to the use of alcohol (Abou-Saleh et al. 2001; Karam et al. 2006; Kadri et al. 2010). The infrequent use of F10 reported in this study could be due to the lower rates of alcohol consumption among Muslims and lower rates of help seeking among those who do drink given that alcohol is considered a religious sin in Islam (AlMarri & Oei, 2009; Adudabbeh & Hamid, 2012).
The use of F12 mental and behavioural disorders due to the use of cannabinoids was relatively less common among psychiatrists from EURO (20.5%) and WPRO (17.6%) compared with other WHO regions. Available epidemiological data suggest that in recent years, the prevalence of cannabis use has been increasing in developing countries, while it has decreased relative to historical peaks and stabilised in developed countries (Copeland & Swift, 2009). Moreover, although the prevalence of cannabis use has been reported to be quite high in Australia and New Zealand, it has been found to be very low and almost non-existent in Asian WPRO countries such as Japan and China (Smart & Ogborne, 2000; Degenhardt et al. 2008), consistent with the data presented in Fig. 1. Surprisingly, the use of F12 was found to be much more common among EMRO psychiatrists compared with F10 mental and behavioural disorders due to the use of alcohol. This unexpected discrepancy may relate to the differing legal statuses of alcohol and cannabis across EMRO. Cannabis use may be considered much more problematic and may be related with greater help-seeking behaviour given that it is considered illegal everywhere in the Arab world, while alcohol use is allowed in some Arab countries.
The use of F42 OCD and F45 somatoform disorders was much more common in EMRO (60.1 and 68.0%, respectively) and SEARO (55.3 and 54.6%) compared with other WHO regions. Large-scale international research, to date, does not show significant variations in the prevalence of OCD cross-culturally (Fontenelle et al. 2004; de Silva & Bhugra, 2007). The only features of OCD that were found to be influenced by socio-cultural factors are the content and intensity of OCD symptoms (obsessions and compulsions) (Staley & Wand, 1995; Kiejna et al. 2002; Fontenelle et al. 2004). Religion may affect the content and frequency of OCD symptoms in some of the countries in these regions (Mahgoub & Abdel-Hafeiz, 1991; Al-Sabaie et al. 1992; Okasha et al. 1994; de Silva & Bhugra, 2007; Kadri et al. 2007), given that religious practice in these areas may occupy a major portion of a pious person's daily life. The greater use of F42 in EMRO and SEARO may not necessarily reflect greater prevalence rates but rather greater help-seeking behaviour due to greater symptom severity.
The greater use of F45 is consistent with the popular belief that somatoform disorders are more common in non-western contexts where the indirect expression of distress through physical complaints is considered more culturally and socially acceptable (Okasha, 2004). However, so far, research has not reported meaningful differences in the prevalence of somatoform disorders cross-culturally except for the higher rates in Latin American settings (Janca et al. 1995; Isaac et al. 1996; Gureje et al. 1997; Gureje, 2004; Chandrashekar & Math, 2006). Nonetheless, the form and intensity of somatic symptoms may vary across cultures (Escobar & Gureje, 2007) and, thus, the greater use of F45 in EMRO and SEARO may possibly reflect higher rates of help seeking due to greater symptom severity.
The differences in frequency of use across income levels for the nine diagnoses were statistically significant for all categories except for F10 (see Fig. 2). The most striking variability across income levels was found for F23 acute and transient psychotic disorder. The use of F23 acute and transient psychotic disorder was more common among psychiatrists from lower middle income countries (46.60%) and upper middle income countries (41.20%) compared with high-income countries (25.90%). The greater use of F23 among psychiatrists from countries with the lower income levels is expected given that this diagnostic category was found to be more prevalent in developing rather than developed countries (Susser & Wanderling, 1994; Susser et al. 1995; Kulhara & Chakrabarti, 2001).
Fig. 2.
Percentage of psychiatrists using specific diagnostic categories at least once per week, by income levels.
Limitations
Although the WPA-WHO Global Survey contributed significantly to the literature by examining psychiatrists’ views about the classification of mental disorders on a broader international scope, the current findings should be interpreted with caution considering the following limitations. First and foremost, convenience sampling was sometimes used which compromised the generalisability of the samples recruited from some countries. Second, the representativeness of the results is also questionable given that there were dramatic variations in response rates across member societies. Finally, although examining the frequency of use sheds light on the possible existence of variations in psychiatric practice, it does not explain or clarify the nature and cause of these variations and whether or not they are culturally determined.
Conclusion
In considering the data presented here, it is important to be clear that they suggest possible regional differences in psychiatric practice. The present study shows that variations in frequency of use may exist across world regions, which may, to some extent, be culturally determined. However, whether variations in the rates of use by psychiatrists of ICD-10 diagnostic categories reflect differences in prevalence, treatment-seeking behaviour, patient characteristics, psychiatrist characteristics or socio-cultural contexts cannot be determined based on the current findings. Nonetheless, the study results clearly highlight the importance of conducting further research to closely examine applicability of ICD-10 diagnostic categories in the context of different regions and cultures.
Acknowledgements
None.
Conflict of interest
None to declare.
Author Note:
B. Khoury, M. Maj, and O. Gureje are members of the WHO International Advisory Group for the Revision of ICD-10 Mental and Behavioral Disorders. G.M. Reed is a member of the WHO Secretariat, Department of Mental Health and Substance Abuse, WHO, and J. Keeley is a Consultant to the WHO Secretariat. Unless specifically stated, the views expressed in this article are those of the authors and do not represent the official policies or positions of the WHO or of the International Advisory Group.
References
- Abou-Saleh MT, Ghubash R, Daradkeh TK (2001). Al Ain Community Psychiatric Survey. I. Prevalence and socio-demographic correlates. Social Psychiatry and Psychiatric Epidemiology l36, 20–28. [DOI] [PubMed] [Google Scholar]
- Adudabbeh N, Hamid A (2012). Substance use among Arabs and Arab Americans In Ethnocultural Factors in Substance Abuse Treatment (ed. Straussner SLA), pp. 275–290. The Guilford Press: New York. [Google Scholar]
- AlMarri TSK, Oei TPS (2009). Alcohol and substance use in the Arabian Gulf region: a review. International Journal of Psychology 44, 222–233. [DOI] [PubMed] [Google Scholar]
- Al-Sabaie AS, Abdul-Rahim F, Al-Hamad AR (1992). Obsessive compulsive disorder. Annals of Saudi Medicine 12, 558–561. [DOI] [PubMed] [Google Scholar]
- Baxter AJ, Vos T, Scott KM, Norman RE, Flaxman AD, Blore J, Whiteford HA (2014). The regional distribution of anxiety disorders: implications for the Global Burden of Disease Study, 2010. International Journal of Methods in Psychiatric Research 23, 422–438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chand SP, Al-Hussaini AA, Martin R, Mustapha S, Zaidan Z, Viernes N, Al-Adawi S (2000). Dissociative disorders in the Sultanate of Oman. Acta Psychiatrica Scandinavica 102, 185–187. [DOI] [PubMed] [Google Scholar]
- Chandrashekar CR, Math SB (2006). Psychosomatic disorders in developing countries: current issues and future challenges. Current Opinion in Psychiatry 19, 201–206. [DOI] [PubMed] [Google Scholar]
- Copeland J, Swift W (2009). Cannabis use disorder: epidemiology and management. International Review of Psychiatry 21, 96–103. [DOI] [PubMed] [Google Scholar]
- Degenhardt L, Chiu W-T, Sampson N, Kessler RC, Anthony JC, Angermeyer M, Bruffaerts R, De Girolamo G, Gureje O, Huang Y, Karam A (2008). Toward a global view of alcohol, tobacco, cannabis, and cocaine use: findings from the WHO World Mental Health Surveys. PLoS Medicine 5, e141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Demyttenaere K, Bruffaerts R, Posada-Villa J, Gasquet I, Kovess V, Lepine JP, Angermeyer MC, Bernert S, de Girolamo G, Morosini P, Polidori G (2004). Prevalence, severity, and unmet need for treatment of mental disorders in the World Health Organization World Mental Health Surveys. JAMA 29, 2581–2590. [DOI] [PubMed] [Google Scholar]
- de Silva P, Bhugra D. (2007). Culture and obsessive-compulsive disorder In Textbook of Cultural Psychiatry (eds. Bhugra D, Bhui K), pp. 282–291. Cambridge University Press: New York. [Google Scholar]
- Escobar JI, Gureje O (2007). Influence of cultural and social factors on the epidemiology of idiopathic somatic complaints and syndromes. Psychosomatic Medicine 69, 841–845. [DOI] [PubMed] [Google Scholar]
- Fontenelle LF, Mendlowicz MV, Marques C, Versiani M (2004). Trans-cultural aspects of obsessive–compulsive disorder: a description of a Brazilian sample and a systematic review of international clinical studies. Journal of Psychiatric Research 38, 403–411. [DOI] [PubMed] [Google Scholar]
- Gureje O (2004). What can we learn from a cross-national study of somatic distress? Journal of Psychosomatic Research 56, 409–412. [DOI] [PubMed] [Google Scholar]
- Gureje O, Simon GE, Ustun TB, Goldberg DP (1997). Somatization in a cross-cultural perspective: a World Health Organization study in primary care. American Journal of Psychiatry 154, 989–995. [DOI] [PubMed] [Google Scholar]
- International Advisory Group for the Revision of ICD-10 Mental and Behavioural Disorders (2011). A conceptual framework for the revision of the ICD-10 classification of mental and behavioural disorders. World Psychiatry 10, 86–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Isaac M, Janca A, Orley J (1996). Somatization-a culture bound or universal syndrome? Journal of Mental Health 5, 219–222. [Google Scholar]
- Janca A, Isaac M, Bennett LA, Tacchini G (1995). Somatoform disorders in different cultures – a mail questionnaire survey. Social Psychiatry and Psychiatric Epidemiology 30, 44–48. [DOI] [PubMed] [Google Scholar]
- Kadri N, Agoub M, El Gnaoui S, Berrada S, Moussaoui D (2007). Prevalence of anxiety disorders: a population-based epidemiological study in metropolitan area of Casablanca, Morocco. Annals of General Psychiatry 6, 1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kadri N, Agoub M, Assouab F, Tazi MA, Didouh A, Stewart R, Moussaoui D (2010). Moroccan national study on prevalence of mental disorders: a community-based epidemiological study. Acta Psychiatrica Scandinavica 121, 71–74. [DOI] [PubMed] [Google Scholar]
- Karam EG, Mneimneh Z, Karam AN, Fayyad J, Nasser S, Chatterji S, Kessler RC (2006). Prevalence and treatment of mental disorders in Lebanon: a national epidemiological survey. Lancet 367, 1000–1006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiejna A, Rymaszewska J, Kantorska-Janiec M, Tokarski W (2002). Epidemiology of obsessive-compulsive disorder. Psychiatria Polska l36, 539–548. [PubMed] [Google Scholar]
- Kulhara P, Chakrabarti S. (2001). Culture and schizophrenia and other psychotic disorders. Psychiatric Clinics of North America 24, 449–464. [DOI] [PubMed] [Google Scholar]
- Mahgoub OM, Abdel-Hafeiz HB (1991). Pattern of obsessive-compulsive disorder in Eastern Saudi Arabia. The British Journal of Psychiatry 158, 840–842. [DOI] [PubMed] [Google Scholar]
- Okasha A (2004). Focus on psychiatry in Egypt. The British Journal of Psychiatry 185, 266–272. [DOI] [PubMed] [Google Scholar]
- Okasha A, Dawla ASE (1992). Reliability of ICD-10 research criteria: an Arab perspective. Acta Psychiatrica Scandinavica 86, 484–488. [DOI] [PubMed] [Google Scholar]
- Okasha A, Saad A, Khalil A, Seif El Dawla A, Yehia N (1994). Phenomenology of obsessive-compulsive disorder: a transcultural study. Comprehensive Psychiatry 35, 191–197. [DOI] [PubMed] [Google Scholar]
- Reed GM (2010). Towards ICD-11: improving the clinical utility of WHO's international classification of mental disorders. Professional Psychology, Research and Practice 41, 457–464. [Google Scholar]
- Reed GM, Correia JM, Esparza P, Saxena S, Maj M (2011). The WPA-WHO Global Survey of psychiatrists’ attitudes towards mental disorders classification. World Psychiatry 10, 118–131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robles R, Fresán A, Evans SC, Lovell AM, Medina-Mora ME, Maj M, Reed GM (2014). Problematic, absent, and stigmatizing diagnoses in current mental disorders classifications: results from the WHO-WPA and WHO-IUPsyS Global Surveys. International Journal of Clinical and Health Psychology 14, 165–177. [Google Scholar]
- Robles R, Fresán A, Medina-Mora ME, Sharan P, Roberts MC, de Jesus Mari J Matsumoto C, Maruta T, Gureje O, Ayuso-Mateos JL, Xiao Z (2015). Categories that should be removed from mental disorders classifications: perspectives and rationales of clinicians from eight countries. Journal of Clinical Psychology 71, 267–281. [DOI] [PubMed] [Google Scholar]
- Smart RG, Ogborne AC (2000). Drug use and drinking among students in 36 countries. Addictive Behaviors 25, 455–460. [DOI] [PubMed] [Google Scholar]
- Staley D, Wand RR (1995). Obsessive-compulsive disorder: a review of the cross-cultural epidemiological literature. Transcultural Psychiatry 32, 103–136. [Google Scholar]
- Susser E, Wanderling J (1994). Epidemiology of nonaffective acute remitting psychosis vs schizophrenia. Sex and sociocultural setting. Archives of General Psychiatry 51, 294–301. [DOI] [PubMed] [Google Scholar]
- Susser E, Varma VK, Malhotra S, Conover S, Amador XF (1995). Delineation of acute and transient psychotic disorders in a developing-country setting. The British Journal of Psychiatry 167, 216–219. [DOI] [PubMed] [Google Scholar]
- Van Duijl M, Cardena E, De Jong JTVM (2005). The validity of DSM IV dissociative disorders categories in South-West Uganda. Transcultural Psychiatry 42, 219–241. [DOI] [PubMed] [Google Scholar]
- World Health Organization (1992). International Classification of Diseases and Related Health Problems, 10th Revision. World Health Organization: Geneva. [Google Scholar]
- World Health Organization (2014). Mental Health Atlas. World Health Organization: Geneva. [Google Scholar]