Abstract
Aims.
People with a mental illness have a shorter lifespan and higher rates of somatic illnesses than the general population. They also face multiple barriers which interfere with access to healthcare. Our objective was to assess the effect of mental illness on the timeliness and optimality of access to healthcare for somatic reasons by comparing indicators reflecting the quality of prior somatic care in hospitalised patients.
Methods.
An observational nation-wide study was carried out using exhaustive national hospital discharge databases for the years 2009–2013. All adult inpatient stays for somatic reasons in acute care hospitals were included with the exception of obstetrics and day admissions. Admissions with coding errors were excluded. Patients with a mental illness were identified by their admissions for a psychiatric reason and/or contacts with psychiatric hospitals. The quality of prior somatic care was assessed using the number of admissions, admissions through the emergency room (ER), avoidable hospitalisations, high-severity hospitalisations, mean length of stay (LOS) and in-hospital death. Generalised linear models studied the factors associated with poor quality of primary care.
Results.
A total of 17 620 770 patients were included, and 6.58% had been admitted at least once for a mental illness, corresponding to 8.96% of hospital admissions. Mentally ill patients were more often hospitalised (+41% compared with non-mentally patients) and for a longer LOS (+16%). They also had more high-severity hospitalisations (+77%), were more often admitted to the ER (+113%) and had more avoidable hospitalisations (+50%). After adjusting for other covariates, regression models found that suffering from a mental illness was significantly associated with a worse state for each indicator of the quality of care except in-hospital death.
Conclusion.
Inadequate primary care of mentally ill patients leads to more serious conditions upon admission to hospital and avoidable hospitalisations. It is, therefore, necessary to improve primary care and prevention for those patients.
Key words: Epidemiology, health economics, health service research, research design and methods
Introduction
Worldwide, mental disorders affect at least one in three adults during their lifetime (Narrow et al. 2002). Those affected are generally in less good health than the general population (Sokal et al. 2004), with a much shorter lifespan (Laursen et al. 2007; Tidemalm et al. 2008; Viron & Stern, 2010) and higher rates of somatic illnesses (Sokal et al. 2004; Druss, 2007; Viron & Stern, 2010; Stubbs et al. 2016). The prevalence of diabetes, for example, was found to be significantly higher in mentally ill patients than in other patients, and they also present an increased risk of hospitalisation for diabetes complications, diabetes-related mortality and all-cause mortality (Mai et al. 2011b). Mentally ill patients have also been shown as having a much higher rate of avoidable hospitalisations, which may be indicative of the poor quality of the primary care they receive (Mai et al. 2011a). The reasons for this are many and varied as mentally ill patients face barriers which interfere with timely and optimal access to healthcare. These barriers are dependent on different factors relative to the organisation of healthcare systems, providers and patients (Druss, 2007; Lawrence & Kisely, 2010; Viron & Stern, 2010). At a healthcare system level, this includes systematic separation of mental and somatic healthcare and lack of clarity and consensus about who should be responsible for detecting and managing physical problems in patients with a mental illness (Druss, 2007; van Hasselt et al. 2013; Small et al. 2017). At the provider level, time and resource constraints, stigma and regarding physical complaints as psychosomatic symptoms can also lead to a suboptimal quality of care offered by clinicians to patients with a mental illness (Lawrence & Kisely, 2010; De Hert et al. 2011), while patient-related factors include health risk factors and lifestyle (e.g. substance abuse, poor diet, smoking and lack of exercise), side effects of medications, cognitive impairment, suspiciousness, difficulties communicating physical needs and more often than not disadvantaged social circumstances (Lawrence & Kisely, 2010; De Hert et al. 2011; van Hasselt et al. 2013).
Previous research on the association between mental illness and quality of care has often been limited by their cross-sectional study design (Frayne et al. 2005; Brown et al. 2010), their focus on the consequences of a single mental illness (Daumit et al. 2006; Bradford et al. 2008; Schoepf et al. 2014) or physical disease (Rathore et al. 2008; Mai et al. 2011b; Druss et al. 2012; Lee et al. 2016), or their use of only one indicator to assess access to healthcare (Miller et al. 2006; Mai et al. 2011a). In addition, few studies have applied rigorous methods to define the mentally ill population using linked data.
Our objective is to compare acute somatic hospitalisations in patients admitted at least once for a mental illness to other patients’ and to assess the effect of mental illness on the timeliness and optimality of access to healthcare for somatic reasons with a wide range of indicators.
Methods
Study design and data sources
We carried out an observational study comparing indicators of quality of care in hospitalised patients with and without a diagnosed mental illness over a 5-year period.
Two linkable exhaustive hospital discharge databases were used. First, the acute in-hospital care database (Programme de Médicalisation des Systèmes d'Information: Médecine, Chirurgie, Obstétrique, Programme of medicalisation of information systems: medicine, surgery and obstetrics) for the years 2009–2013 provided information on all acute hospitalisations using diagnosis-related groups (DRG). It records variables on the characteristics of patients (age, sex, national anonymous identification number) and their admissions (principal and secondary diagnoses, using the 10th edition of the international classification of diseases (ICD-10), length of stay (LOS), year and month of discharge, etc.). Second, the psychiatric care database for the years 2007–2013 (Recueil d'Information Médicalisée en Psychiatrie, Summary of medical information for psychiatry) provided information on inpatient (full-time and part-time) psychiatric care by all hospitals and institutions providing psychiatric care, with similar information on patients and their admissions. Patients have a single national anonymous identification number present in both databases.
As there is no individual socioeconomic indicator in the discharge databases, we used an ecological proxy, the FDep (Rey et al. 2009), to account for patients’ deprivation. Similarly to the Carstairs and Townsend indices (Townsend et al. 1988; Carstairs & Morris, 1989), the FDep is based on patients’ zip code of residence but it has been developed specifically for the French context and has been validated against the Carstairs and Townsend indices (Rey et al. 2009). It contains four variables: the percentage of blue-collar workers in the labour force, the percentage of high school graduates in the population aged 15 and over, the unemployment rate in the labour force and the median income per household, all derived from data from the National Institute of Statistics and Economic Studies.
Study population
The study population included all adult inpatient stays for somatic reasons in acute care hospitals between 2009 and 2013 with the exception of obstetric and day admissions. Patients with a mental illness were identified as any patient who had at least one episode of inpatient care between 2007 and 2013 in the psychiatric care database, who had at least one hospitalisation for a psychiatric reason (with an ICD-10 psychiatric diagnosis coded as the principal diagnosis, i.e. as the reason for the admission) recorded in the acute care database, or who had a transfer to or from a psychiatric hospital between 2009 and 2013. As such, only patients who had been admitted at least once for a mental illness in the past were considered to be mentally ill in this study. Patients’ national anonymous identification number was used to identify those patients in the study population.
Indicators of quality of primary care
The quality of care received prior to an admission for somatic reasons was assessed using six indicators reflecting patient severity at admission and health outcome during the hospitalisation. As there are no direct measures of quality of care – especially of quality of primary care – in French databases, we used as proxy patients’ health status upon admission under the assumption that poor or absent care in primary care settings would lead to poor health, which in turn would lead to more admissions, more avoidable admissions and more admissions through the emergency room (ER), and that those admissions would have poorer outcomes, i.e. longer LOS, more severe admissions and more in-hospital mortality. These six indicators have been used as proxies of quality of prior care trajectories in the literature in the past. They were measured over the 5-year period of the study and were as follows: number of overnight admissions (Azevedo Da Silva et al. 2015), under the assumption that poor primary care would increase the number of admissions due to a lack of management of chronic illnesses, poor prevention etc.; number and proportion of admissions through the ER (Cowling et al. 2013; O'Malley, 2013), under the assumption that poor primary care would lead to more ER visits which would, in turn, increase the likelihood to be admitted through the ER; number and proportion of avoidable hospitalisations (Weissman et al. 1992; IMS Health, 2006; Rosano et al. 2013), hospitalisations that could have been avoided if primary care had been timely and adequate (through immunisation, management of a disease episode, etc.), under the assumption that poor primary care would lead to an increase in avoidable admissions; mean LOS, under the assumption that due to a poorer health state at admission, patients’ LOS would be longer; number and proportion of high-severity hospitalisations, under the assumption that patients with poor primary care would arrive at a later stage of the disease at the hospital and would, therefore, be more severe; and in-hospital death (Jerant et al. 2012), under the assumption that mortality would be increased due to the poorer health state at admission. The severity of a hospitalisation was based on patients’ DRG whose last character reflects patient severity on a one-to-four scale (with increasing severity). Severity levels one and two were grouped together as non-severe hospitalisations, and severity levels three and four corresponded to severe hospitalisations. Avoidable hospitalisations were identified with their principal diagnosis (i.e. the reason for the hospitalisation), when they corresponded to one of the 12 conditions described as avoidable by Weissman et al.: pneumonia, congestive heart failure, asthma, cellulite, perforated or bleeding ulcer, pyelonephritis, diabetes with ketoacidosis or coma, perforated appendix, malignant hypertension, hypokalaemia, immunising conditions and gangrene (Weissman et al. 1992). While common, those inpatient admissions could potentially be prevented by appropriate and timely outpatient care in the majority of cases – for example, urinary tract infections if diagnosed and treated early should not lead to pyelonephritis.
Statistical analysis
A descriptive analysis was first carried out. Means were computed for continuous indicators, proportions were calculated for categorical indicators and both were computed for count variables for patients identified as having a mental illness and for other patients. In order to ensure comparability between the two groups, proportions and means were standardised in the mentally ill group according to the age and sex structure of the other group. No statistical test was performed as the study used exhaustive data. Subgroup analyses were also carried out in three subgroups of patients: patients suffering from cancer (CR group), from diabetes (DB group) and from a cardiovascular disease (CV group). Patients were classified in one of the subgroups if they had at least one hospitalisation with a principal diagnosis associated with one of those diseases between 2009 and 2013.
Generalised linear models were then carried out for each indicator to assess the effect of mental illness on the quality of care after adjusting for other potential explanatory variables like sex, age and the three main types of chronic diseases making up our subgroups. Additional explanatory variables included severity level (for the in-hospital death model), in-hospital death (models for the number of hospitalisations, number of avoidable hospitalisations, number of high-severity hospitalisations, number of admissions through the ER and mean LOS), number of hospitalisations (models for the number of avoidable hospitalisations, number of high-severity hospitalisations and number of admissions through the ER) and patients’ length of follow-up in the database (for the number of hospitalisation model). The type of generalised linear model was determined according to the distribution of the outcome variables. For in-hospital death (binary variable), a logistic regression was carried out. For count variables, negative binomial regressions were used to account for overdispersion that was observed in the data. For the LOS, a model with gamma log distribution was developed.
Results
Patients’ characteristics
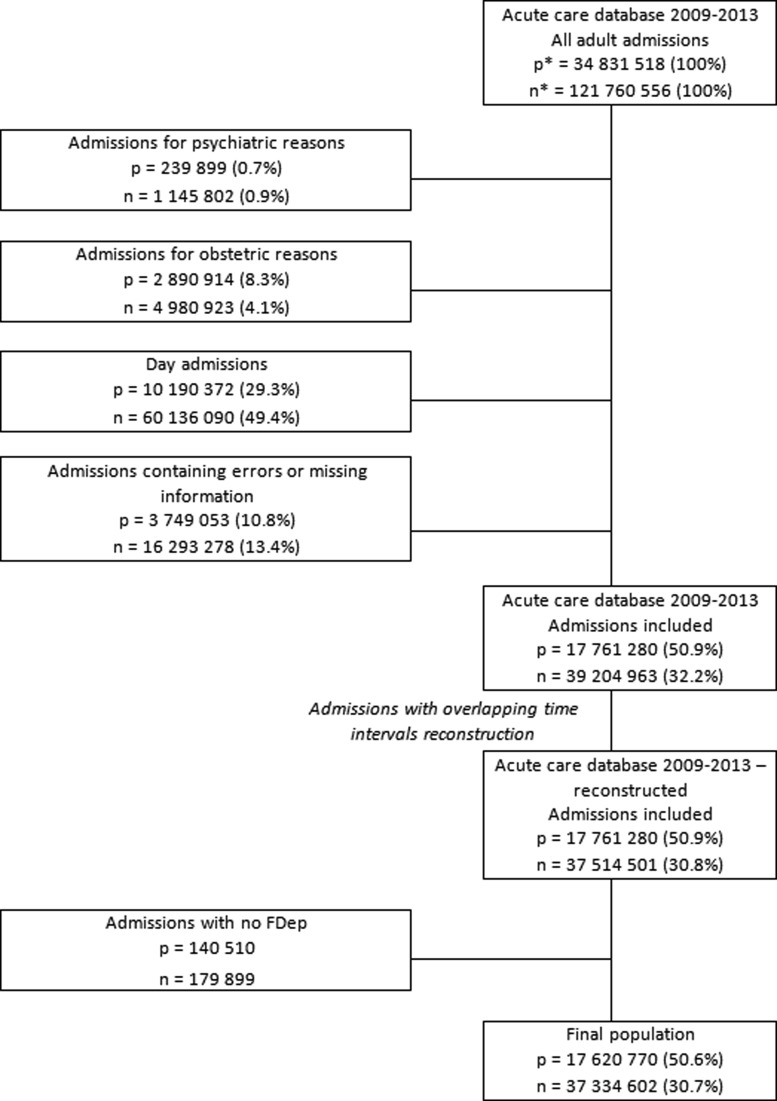
Out of 34 831 518 adult patients hospitalised at least once in acute care between 2009 and 2013 (for a total of 121 760 556 hospitalisations), 17 620 770 were included in the study population for a total of 37 334 602 hospitalisations (Fig. 1). A total of 1 159 672 patients (6.58%) were identified as being diagnosed with a mental illness, corresponding to 3 343 464 (8.96%) hospitalisations, and 16 461 098 patients (93.42%) were not (33 991 138 hospitalisations, 91.04%).
Fig. 1.
Flow diagram p = number of patients; n = number of hospitalisations in acute care.
Patients identified as having a mental illness had the same age (58 years old) as patients without a mental illness at their first hospitalisation (Table 1) and there was roughly the same percentage of men in both groups (46.28 and 47.39%, respectively). Among mentally ill patients, 9.30% had cancer diagnosis, 12.03% suffered from diabetes and 44.83% had cardiovascular disease. The distribution of diabetes and cardiovascular diseases was similar in non-mentally ill patients (11.48 and 43.52%, respectively) but cancer was more frequent (13.25%). In addition, patients with a mental illness were more likely to live in deprived areas than not (Table 1).
Table 1.
Patients’ characteristics at first admission in an acute care hospital for a somatic problem
| Patients with a mental illness | Patients without a mental illness | Total | |
|---|---|---|---|
| All patients | |||
| n (%) | 1 159 672 (6.58) | 1 6461 098 (93.42) | 1 7620 770 |
| Age, mean (s.d.) | 58.07 (20.23) | 58.04 (19.86) | 58.04 (19.89) |
| Men, n (%) | 5 36 745 (46.28) | 78 00 910 (47.39) | 8 337 655 (47.32) |
| FDep quintile 1, n (%) | 2 66 015 (22.94) | 42 38 784 (25.75) | 45 04 799 (25.57) |
| FDep quintile 2, n (%) | 2 47 122 (21.31) | 34 15 231 (20.75) | 36 62 353 (20.78) |
| FDep quintile 3, n (%) | 2 13 539 (18.41) | 28 35 691 (17.23) | 30 49 230 (17.30) |
| FDep quintile 4, n (%) | 2 19 511 (18.93) | 29 92 186 (18.18) | 32 11 697 (18.23) |
| FDep quintile 5, n (%) | 2 13 485 (18.41) | 29 79 206 (18.10) | 31 92 691 (18.12) |
| Patients with cancer | |||
| n (%) | 1 07 883 (9.30) | 21 80 371 (13.25) | 2 288 254 (12.99) |
| Age, mean (s.d.) | 67.44 (14.92) | 67.18 (14.12) | 67.20 (14.16) |
| Men, n (%) | 56 806 (52.66) | 11 70 739 (53.69) | 12 27 545 (53.65) |
| FDep quintile 1, n (%) | 25 405 (23.55) | 5 66 246 (25.97) | 5 91 651 (25.86) |
| FDep quintile 2, n (%) | 23 081 (21.39) | 4 54 572 (20.85) | 4 77 653 (20.87) |
| FDep quintile 3, n (%) | 20 262 (18.78) | 3 81 104 (17.48) | 4 01 366 (17.54) |
| FDep quintile 4, n (%) | 20 281 (18.80) | 3 97 432 (18.23) | 4 17 713 (18.25) |
| FDep quintile 5, n (%) | 18 854 (17.48) | 3 81 017 (17.47) | 3 99 871 (17.47) |
| Patients with diabetes | |||
| n (%) | 1 39 505 (12.03) | 1 890 235 (11.48) | 2 029 740 (11.52) |
| Age, mean (s.d.) | 67.45 (15.48) | 67.94 (14.11) | 67.90 (14.21) |
| Men, n (%) | 68 269 (48.94) | 10 32 824 (54.64) | 11 01 093 (54.25) |
| FDep quintile 1, n (%) | 29 615 (21.23) | 4 36 747 (23.11) | 4 66 362 (22.98) |
| FDep quintile 2, n (%) | 28 133 (20.17) | 3 68 724 (19.51) | 3 96 857 (19.55) |
| FDep quintile 3, n (%) | 25 741 (18.45) | 3 28 323 (17.37) | 3 54 064 (17.44) |
| FDep quintile 4, n (%) | 27 920 (20.01) | 3 62 488 (19.18) | 3 90 408 (19.23) |
| FDep quintile 5, n (%) | 28 096 (20.14) | 3 93 953 (20.84) | 4 22 049 (20.79) |
| Patients with a cardiovascular disease | |||
| n (%) | 5 19 938 (44.83) | 7 163 927 (43.52) | 7 683 865 (43.61) |
| Age, mean (s.d.) | 69.07 (16.45) | 69.12 (15.19) | 69.11 (15.28) |
| Men, n (%) | 2 39 214 (46.01) | 36 13 161 (50.44) | 38 52 375 (50.14) |
| FDep quintile 1, n (%) | 1 14 801 (22.08) | 16 96 636 (23.68) | 18 11 437 (23.57) |
| FDep quintile 2, n (%) | 1 06 786 (20.54) | 14 48 706 (20.22) | 15 55 492 (20.24) |
| FDep quintile 3, n (%) | 97 706 (18.79) | 12 81 050 (17.88) | 13 78 756 (17.94) |
| FDep quintile 4, n (%) | 1 02 521 (19.72) | 13 71 727 (19.15) | 14 74 248 (19.19) |
| FDep quintile 5, n (%) | 98 124 (18.87) | 13 65 808 (19.07) | 14 63 932 (19.05) |
Descriptive analysis of the indicators of quality of primary care
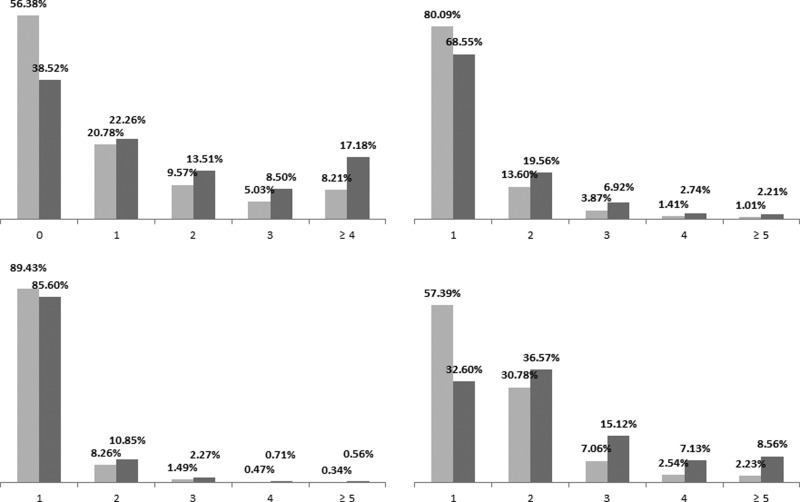
Patients identified as being mentally ill had worse outcomes than other patients for all indicators except in-hospital death, although the magnitude of the difference between the two groups varied depending on the indicator (Table 2). On average, mentally ill patients were more often hospitalised (+41% compared with non-mentally patients) and for a longer LOS (+16%). They also had more high-severity hospitalisations (+77%), were more often admitted through the ER (+113%) and had more avoidable hospitalisations (+50%). Moreover, mentally ill patients had a higher chance of being admitted through the ER, and for high-severity admissions (Table 2, Fig. 2). However in-hospital mortality was similar in both populations. The analysis by chronic disease subgroups showed very similar trends, with one notable exception: patients with a mental illness who also had cancer had a higher chance of having an avoidable hospitalisation (Table 2).
Table 2.
Descriptive results for each indicator of quality of prior somatic care trajectories in the population with and without a mental illness as well as in patients with cancer, cardiovascular disease and diabetes
| Patients with a mental illnessa | Patients without a mental illness | Ratio | |
|---|---|---|---|
| All patients | n = 1 159 672 | n = 16 461 098 | |
| Number of hospitalisations, mean (s.d.) | 2.91 (2.80) | 2.06 (2.02) | 1.41 |
| Length of stay, mean (s.d.), d | 6.62 (7.29) | 5.70 (7.21) | 1.16 |
| Number of high-severity hospitalisations, mean (s.d.) | 0.53 (0.92) | 0.30 (0.76) | 1.77 |
| Proportion of high-severity hospitalisations (%) | 18.00% | 14.49% | 1.24 |
| Number of admissions through the ER, mean (s.d.) | 1.36 (1.79) | 0.64 (1.05) | 2.13 |
| Proportion of admissions through the ER (%) | 47.65% | 31.04% | 1.54 |
| Number of avoidable hospitalisations, mean (s.d.) | 0.21 (0.60) | 0.14 (0.52) | 1.50 |
| Proportion of avoidable hospitalisations (%) | 7.11% | 6.98% | 1.02 |
| In-hospital deaths, n (%) | NA (7.57) | 1 225 396 (7.44) | 1.02 |
| Patients with cancer | n = 1 07 883 | n = 21 80 371 | |
| Number of hospitalisations, mean (s.d.) | 4.86 (3.86) | 3.60 (3.22) | 1.35 |
| Length of stay, mean (s.d.), d | 9.46 (8.88) | 8.77 (9.31) | 1.08 |
| Number of high-severity hospitalisations, mean (s.d.) | 1.11 (1.40) | 0.74 (1.13) | 1.50 |
| Proportion of high-severity hospitalisations (%) | 23.17% | 20.09% | 1.15 |
| Number of admissions through the ER, mean (s.d.) | 1.67 (2.11) | 0.84 (1.33) | 1.99 |
| Proportion of admissions through the ER (%) | 35.05% | 23.42% | 1.50 |
| Number of avoidable hospitalisations, mean (s.d.) | 0.29 (0.73) | 0.17 (0.59) | 1.71 |
| Proportion of avoidable hospitalisations (%) | 6.06% | 4.81% | 1.26 |
| In-hospital deaths, n (%) | NA (23.08) | 5 61 543 (25.75) | 0.90 |
| Patients with diabetes | n = 1 39 505 | n = 18 90 235 | |
| Number of hospitalisations, mean (s.d.) | 4.39 (3.73) | 3.15 (2.91) | 1.39 |
| Length of stay, mean (s.d.), d | 8.77 (7.42) | 7.97 (8.27) | 1.10 |
| Number of high-severity hospitalisations, mean (s.d.) | 1.05 (140) | 0.68 (1.17) | 1.54 |
| Proportion of high-severity hospitalisations (%) | 23.81% | 21.18% | 1.12 |
| Number of admissions through the ER, mean (s.d.) | 1.96 (2.34) | 1.03 (1.50) | 1.90 |
| Proportion of admissions through the ER (%) | 45.28% | 32.81% | 1.38 |
| Number of avoidable hospitalisations, mean (s.d.) | 0.45 (0.99) | 0.34 (0.87) | 1.32 |
| Proportion of avoidable hospitalisations (%) | 10.32% | 10.81% | 0.95 |
| In-hospital deaths, n (%) | NA (12.45) | 2 47 894 (13.11) | 0.95 |
| Patients with a cardiovascular disease | n = 5 19 938 | n = 71 63 927 | |
| Number of hospitalisations, mean (s.d.) | 3.88 (3.27) | 2.76 (2.52) | 1.41 |
| Length of stay, mean (s.d.), d | 8.61 (7.91) | 7.55 (8.34) | 1.14 |
| Number of high-severity hospitalisations, mean (s.d.) | 0.93 (1.25) | 0.57 (1.02) | 1.63 |
| Proportion of high-severity hospitalisations (%) | 24.01% | 20.24% | 1.19 |
| Number of admissions through the ER, mean (s.d.) | 1.81 (2.12) | 0.94 (1.34) | 1.93 |
| Proportion of admissions through the ER (%) | 47.53% | 34.00% | 1.40 |
| Number of avoidable hospitalisations, mean (s.d.) | 0.36 (0.83) | 0.26 (0.71) | 1.38 |
| Proportion of avoidable hospitalisations (%) | 9.42% | 9.54% | 0.99 |
| In-hospital deaths, n (%) | NA (13.00) | 9 40 376 (13.13) | 0.99 |
Mean/proportion standardised on the sex and age at first hospitalisation of the non-mentally ill patient group.
Fig. 2.
Patients’ repartition per number of hospitalisations, high-severity hospitalisations, admissions through the ER and avoidable hospitalisations Y-axis: % of patients X-axis: (clockwise from top left to bottom left) number of hospitalisations, number of high-severity hospitalisations, number of admissions through the ER, number of avoidable hospitalisations Light grey bars: patients without a mental illness Dark grey bars: patients with a mental illness.
Multivariate modelling of the indicators of quality of primary care
After adjusting for other covariates, multivariate regression models found that, ‘all things being equal’, suffering from a mental illness was significantly associated with a worse state for each indicator of the quality of care except in-hospital death (Table 3). Indeed, patients showing a mental illness had 37% more hospitalisations, 45% more high-severity hospitalisations, 70% more admissions through the ER and 5% more avoidable hospitalisations. They also had a 19% higher LOS. Mental illness, however, appeared to decrease the risk of in-hospital death by 13% after adjusting on other variables, unlike cancer and cardiovascular diseases. We also found a clear gradient of deprivation on all indicators (Table 3).
Table 3.
Results of the multivariate regression models for each indicator of quality of prior somatic care trajectories
| Rate ratios/odds ratiosa | 95% confidence interval | p-value | |
|---|---|---|---|
| Number of hospitalisationsb | |||
| Intercept | 0.86 | 0.86–0.87 | <0.0001 |
| Sex (men) | 1.02 | 1.02–1.02 | <0.0001 |
| Age | 1.00 | 1.00–1.00 | <0.0001 |
| Mental illness | 1.37 | 1.37–1.37 | <0.0001 |
| Cancer | 1.67 | 1.66–1.67 | <0.0001 |
| Diabetes | 1.27 | 1.27–1.27 | <0.0001 |
| Cardiovascular disease | 1.52 | 1.52–1.52 | <0.0001 |
| In-hospital death | 1.17 | 1.16–1.17 | <0.0001 |
| Follow-up, in months | 1.01 | 1.01–1.01 | <0.0001 |
| FDep quintile 2 | 1.04 | 1.04–1.05 | <0.0001 |
| FDep quintile 3 | 1.07 | 1.07–1.07 | <0.0001 |
| FDep quintile 4 | 1.06 | 1.05–1.06 | <0.0001 |
| FDep quintile 5 | 1.05 | 1.05–1.05 | <0.0001 |
| Number of avoidable hospitalisationsb | |||
| Intercept | 0.01 | 0.01–0.01 | <0.0001 |
| Sex (men) | 1.00 | 0.99–1.00 | 0.6359 |
| Age | 1.02 | 1.02–1.02 | <0.0001 |
| Mental illness | 1.05 | 1.04–1.05 | <0.0001 |
| Cancer | 0.51 | 0.50–0.51 | <0.0001 |
| Diabetes | 1.31 | 1.31–1.32 | <0.0001 |
| Cardiovascular disease | 2.07 | 2.06–2.08 | <0.0001 |
| Number of hospitalisations | 1.28 | 1.28–1.28 | <0.0001 |
| In-hospital death | 1.65 | 1.64–1.66 | <0.0001 |
| FDep quintile 2 | 1.01 | 1.00–1.01 | 0.0237 |
| FDep quintile 3 | 1.02 | 1.02–1.03 | <0.0001 |
| FDep quintile 4 | 1.05 | 1.04–1.05 | <0.0001 |
| FDep quintile 5 | 1.06 | 1.05–1.06 | <0.0001 |
| Number of high-severity hospitalisationsb | |||
| Intercept | 0.01 | 0.01–0.01 | <0.0001 |
| Sex (men) | 1.02 | 1.02–1.02 | <0.0001 |
| Age | 1.04 | 1.04–10.4 | <0.0001 |
| Mental illness | 1.45 | 1.45–1.46 | <0.0001 |
| Cancer | 1.32 | 1.32–1.33 | <0.0001 |
| Diabetes | 1.22 | 1.21–1.22 | <0.0001 |
| Cardiovascular disease | 1.83 | 1.83–1.84 | <0.0001 |
| Number of hospitalisations | 1.25 | 1.25–1.25 | <0.0001 |
| In-hospital death | 1.99 | 1.98–2.00 | <0.0001 |
| FDep quintile 2 | 1.01 | 1.00–1.01 | 0.0008 |
| FDep quintile 3 | 1.01 | 1.01–1.01 | <0.0001 |
| FDep quintile 4 | 1.03 | 1.03–1.03 | <0.0001 |
| FDep quintile 5 | 1.05 | 1.05–1.05 | <0.0001 |
| Number of admissions through the ERb | |||
| Intercept | 0.18 | 0.18–0.18 | <0.0001 |
| Sex (men) | 1.05 | 1.05–1.05 | <0.0001 |
| Age | 1.01 | 1.01–1.01 | <0.0001 |
| Mental illness | 1.70 | 1.70–1.71 | <0.0001 |
| Cancer | 0.70 | 0.69–0.70 | <0.0001 |
| Diabetes | 1.02 | 1.02–1.02 | <0.0001 |
| Cardiovascular disease | 1.27 | 1.27–1.27 | <0.0001 |
| Number of hospitalisations | 1.22 | 1.22–1.22 | <0.0001 |
| In-hospital death | 1.50 | 1.49–1.50 | <0.0001 |
| FDep quintile 2 | 1.08 | 1.08–1.08 | <0.0001 |
| FDep quintile 3 | 1.15 | 1.15–1.15 | <0.0001 |
| FDep quintile 4 | 1.12 | 1.12–1.13 | <0.0001 |
| FDep quintile 5 | 1.13 | 1.13–1.13 | <0.0001 |
| Mean length of stayc | |||
| Intercept | 2.12 | 2.12–2.12 | <0.0001 |
| Sex (men) | 1.04 | 1.04–1.04 | <0.0001 |
| Age | 1.01 | 1.01–1.01 | <0.0001 |
| Mental illness | 1.19 | 1.19–1.19 | <0.0001 |
| Cardiovascular disease | 1.31 | 1.31–1.31 | <0.0001 |
| Diabetes | 1.17 | 1.17–1.17 | <0.0001 |
| Cancer | 1.32 | 1.32–1.32 | <0.0001 |
| In-hospital death | 1.66 | 1.65–1.66 | <0.0001 |
| FDep quintile 2 | 0.99 | 0.99–0.99 | 0.0003 |
| FDep quintile 3 | 1.01 | 1.00–1.01 | <0.0001 |
| FDep quintile 4 | 1.02 | 1.02–1.02 | <0.0001 |
| FDep quintile 5 | 1.03 | 1.03–1.03 | <0.0001 |
| In-hospital deathd | |||
| Sex (men) | 1.43 | 1.42–1.43 | <0.0001 |
| Age | 1.04 | 1.04–1.04 | <0.0001 |
| Mental illness | 0.87 | 0.86–0.87 | <0.0001 |
| Cardiovascular disease | 1.50 | 1.49–1.50 | <0.0001 |
| Diabetes | 0.97 | 0.97–0.98 | <0.0001 |
| Cancer | 4.67 | 4.65–4.69 | <0.0001 |
| Number of hospitalisations | 1.13 | 1.13–1.13 | <0.0001 |
| Mean severity | 2.90 | 2.90–2.91 | <0.0001 |
| FDep quintile 2 | 1.04 | 1.04–1.05 | <0.0001 |
| FDep quintile 3 | 1.05 | 1.05–1.06 | <0.0001 |
| FDep quintile 4 | 1.08 | 1.07–1.09 | <0.0001 |
| FDep quintile 5 | 1.13 | 1.12–1.13 | <0.0001 |
For the negative binomial regression and generalised linear model (GLM), exponential transformation was used on the estimation to obtain the rate ratio.
A negative binomial regression was carried out.
A generalised linear model (GLM) with gamma log distribution was carried out.
A logistic regression was carried out.
Discussion
We found that patients identified as carrying a mental illness were more often hospitalised and for a longer LOS. They were also more admitted through the ER, for more severe hospitalisations and had more avoidable admissions than patients without a mental illness. As each of these indicators was chosen to reflect the quality of primary care, our findings suggest that access to healthcare for somatic reasons may be delayed, inadequate and/or non-optimal in patients with an identified mental illness.
Our study is the first to look at the association between mental illness and somatic comorbidities at the national level using multiple indicators and exhaustive data over a 5-year period. However, some limits have to be acknowledged. The main one concerns the population identified as being mentally ill, who is only considered to be so if they have been hospitalised for a mental disorder at some point in their past. Patients not treated for their illness or treated only in an ambulatory care setting could not be identified in the databases because of their structure. Therefore there are patients with a mental illness in our ‘patients without a mental illness’ group, which could lead to an underestimation of the effect of mental health on quality of care. Another limit is that neither database records drug prescriptions and/or side effects, which makes it impossible to differentiate a hospitalisation for a side effect from one for an unrelated somatic illness. Additionally, the psychiatric care database provides very few clinical characteristics (for example, it does not record disease severity) and its ICD-10 diagnoses are unreliable due to the difficulty of making a diagnosis in psychiatry and the different schools of thoughts in France, which is why we did not carry out an analysis per diagnosis. Our study also used hospital proxies as indicators of quality of primary care as they were the only ones available to us in the French databases. It would be interesting to perform smaller, additional studies using true primary care indicators, similar to the study carried out using the Quality and Outcomes Framework in the NHS (Jacobs et al. 2015). In addition, the number of hospitalisations may not be a satisfactory indicator of late or poor access to healthcare. Indeed recent research (Zhao et al. 2013) has found a U-shaped association between primary healthcare visits and hospitalisations and therefore an increased number of hospitalisations may not be synonymous with poor primary care. That being said, given that all our other indicators are consistent with a poor quality of primary care, it seems unlikely that our patients with a mental illness would find themselves in the rising portion of the U. Finally, the large sample size of our study must lead us to question statistical significance v. clinical relevance, as other studies have pointed out in the past (Page, 2014; Slobogean et al. 2015; Lee & Yoon, 2017). Indeed while we found that the vast majority of our associations were significant, some may not be clinically relevant, in particular age and sex whose rate ratios – while significant – were very close to one. However, those variables were only used as adjustment variables. With regard to mental illness, all rate ratios were consistently far greater than one except for avoidable hospitalisations, which would imply clinical relevance as well.
Other studies have looked at the association between mental illness and individual indicators of quality of care in the past. Regarding mortality, one study found that the aggregated standardised mortality ratio from all causes of death was 3.2, corresponding to 417 excess deaths (p < 0.001) (Miller et al. 2006). However, there was no association with in-hospital death, similarly to our findings. Another study on patients with acute coronary syndrome found similar findings, with no significant differences in mortality (HR = 0.91; 95% CI 0.81–1.02) between patients with and without severe mental illness (Plomondon et al. 2007). Those studies seem to indicate that people with a mental illness die more often outside the hospital, and indeed one study found that leading causes of death were heart disease (21%) and suicides (18%) (Miller et al. 2006). Death by heart disease, in particular, could be due for example to a lack of patient education on the warning signs and symptoms that lead other patients to consult a doctor or call emergency services when an acute event occurs, on top of the underdiagnosis and undertreatment of heart diseases in that population. Additionally most studies – including our own – use existing data and therefore can only consider that a patient has a mental illness if said patient has sought treatment or been involuntarily committed in the past and is identified – by himself or the healthcare system – as being mentally ill.
Regarding other indicators, many studies have found that mental illness increases potentially preventable hospitalisations (Li et al. 2008; Mai et al. 2011a), as did we. Indeed people with a mental illness obtain fewer general preventive healthcare services (Crews et al. 1998; Haupt et al. 2009; Blane et al. 2017). For example, it has been found that patients with a coronary heart disease and two or more mental health comorbidities were more than twice as likely of being current smokers than those with no mental health conditions, and yet they were also less likely to receive smoking cessation advice (Blane et al. 2017). In general, people with a mental illness tend to receive medical care sporadically and at later stages of their illness (Salsberry et al. 2005; Li et al. 2008; Woodhead et al. 2016). This may explain why they also have more admissions through the ER: patients with a severe mental illness have high rates of ER use for medical illness, with one study reporting that in a randomly selected sample of 200 psychiatric outpatients, 37% had made one or more visits to the ER for medical concerns in the past year v. 20% for those in the general population (Hackman et al. 2006), which can then lead to more admissions to hospital. This is particularly important as one study found that over a 5-year period the number of ER visits by people with mental health comorbidities increased by 53.3% while decreasing for those without a mental illness (Capp et al. 2016). Regarding admission, a French study found that in a cohort of 15 811 employees, participants with a mental disorder had significantly higher rates of all-cause hospitalisation with an incidence rate ratio of 1.20 (Azevedo Da Silva et al. 2015), rather similar to our findings, although they did not find any association for cancer admissions. We also found that once admitted, patients with a mental illness had an increased LOS (+20%) compared with patients without a mental illness. This was also reported in other studies: for example, one study focusing on the burden of mental illness on hospital and patient outcomes among asthma hospitalisations found that any mental illness was associated with a 10% increase in the LOS (Becerra et al. 2016).
Interestingly, we found a lower prevalence of cancer in mentally ill patients compared with non-mentally ill patients (9.30 vs. 13.25%). This result joins the conflicting literature currently available on the subject, some studies reporting a lower incidence (Pinquart & Duberstein, 2010; Chou et al. 2011), others the same (Catts et al. 2008) and others still a higher incidence (Lichtermann et al. 2001; Gross et al. 2010) depending on the mental disorder under consideration and sometimes even within a given mental disorder. The lower prevalence could be due to less frequent screening associated with higher mortality rates (Howard et al. 2010). This population also had a higher chance of avoidable hospitalisations. There is little on the subject in the literature but patients with both a mental illness and cancer could be more likely to decompensate other somatic illnesses such as heart disease or diabetes due to their lack of previous care or be more prone to infections for other reasons, such as poor living conditions.
Finally, one must consider that quality of somatic care can also have an impact on psychiatric care. Indeed one study found that physical comorbidities were more common among readmitted patients than single admission patients in psychiatry (Šprah et al. 2017) and another found that while hospitalised in psychiatry, half of the patients needed one or more referrals for a somatic disorder, with a positive linear trend between LOS and number of referrals (Douzenis et al. 2012).
Conclusions
Our results show that mental illness has a major impact on acute care hospitalisation for somatic comorbidities and psychiatrists should, therefore, be aware of concomitant somatic conditions in their patients. There is a need for increased and better ambulatory care for patients with a mental illness in order to reduce inequalities in access to care. This should include improved interactions and coordination between mental and physical care, including preventive medicine, and may require developing somatic skills during psychiatric residency.
Acknowledgements
The authors would like to thank Céline Quelen and Dr Marie-Caroline Clément for their help with the databases.
Ethical standards
In accordance to French laws, this study was approved by the French Data Protection Authority (Commission nationale de l'informatique et des libertés) which granted access to the databases. As no patient was included in this study, no ethics committee approval was required.
Availability of data and materials
The database is available to researchers after they comply with French laws with regard to its access.
Footnotes
Financial support
This study was undertaken with the joint support of the French Ministry of Health, General Directorate of Health (Direction Générale de la Santé) and Directorate of Research, Studies, Evaluation and Statistics (Direction de la Recherche, des Etudes, de l'Evaluation et des Statistiques); the general scheme of the statutory health insurance system (Caisse Nationale d'Assurance Maladies des Travailleurs Salariés); the scheme for self-employed people (Régime Social des Indépendants); the National Solidarity Fund for Autonomy (Caisse Nationale de Solidarité pour l'Autonomie) and the National Institute for Prevention and Health Education (Insitut National de Prévention et d'Education pour la Santé) in the context of the French Institute for public health research's 2010 call for research projects. The funding sources had no role in the design and conduct of the study; collection, management, analysis and interpretation of the data; preparation, review or approval of the manuscript; and decision to submit the manuscript for publication.
Conflict of interest
The authors declare no conflict of interest.
References
- Azevedo Da Silva M, Lemogne C, Melchior M, Zins M, Van Der Waerden J, Consoli SM, Goldberg M, Elbaz A, Singh-Manoux A, Nabi H (2015). Excess non-psychiatric hospitalizations among employees with mental disorders: a 10-year prospective study of the GAZEL cohort. Acta Psychiatrica Scandinavica 131, 307–317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becerra BJ, Banta JE, Ghamsary M, Martin LR, Safdar N (2016). Burden of mental illness on hospital and patient outcomes among asthma hospitalizations. The Journal of Asthma: Official Journal of the Association for the Care of Asthma 53, 392–397. [DOI] [PubMed] [Google Scholar]
- Blane DN, Mackay D, Guthrie B, Mercer SW (2017). Smoking cessation interventions for patients with coronary heart disease and comorbidities: an observational cross-sectional study in primary care. The British Journal of General Practice: The Journal of the Royal College of General Practitioners 67, e118–e129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradford DW, Kim MM, Braxton LE, Marx CE, Butterfield M, Elbogen EB (2008). Access to medical care among persons with psychotic and major affective disorders. Psychiatric Services (Washington, DC) 59, 847–852. [DOI] [PubMed] [Google Scholar]
- Brown C, Leith J, Dickerson F, Medoff D, Kreyenbuhl J, Fang L, Goldberg R, Potts W, Dixon L (2010). Predictors of mortality in patients with serious mental illness and co-occurring type 2 diabetes. Psychiatry Research 177, 250–254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Capp R, Hardy R, Lindrooth R, Wiler J (2016). National trends in emergency department visits by adults with mental health disorders. The Journal of Emergency Medicine 51, 131–135.e1. [DOI] [PubMed] [Google Scholar]
- Carstairs V, Morris R (1989). Deprivation: explaining differences in mortality between Scotland and England and Wales. BMJ 299, 886–889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Catts V, Catts S, O'Toole B, Frost A (2008). Cancer incidence in patients with schizophrenia and their first-degree relatives – a meta-analysis. Acta Psychiatrica Scandinavica 117, 323–336. [DOI] [PubMed] [Google Scholar]
- Chou F, Tsai K, Su C, Lee C (2011). The incidence and relative risk factors for developing cancer among patients with schizophrenia: a nine-year follow-up study. Schizophrenia Research 129, 97–103. [DOI] [PubMed] [Google Scholar]
- Cowling TE, Cecil EV, Soljak MA, Lee JT, Millett C, Majeed A, Wachter RM, Harris MJ (2013). Access to primary care and visits to emergency departments in England: a cross-sectional, population-based study. PLoS ONE 8, e66699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crews C, Batal H, Elasy T, Casper E, Mehler PS (1998). Primary care for those with severe and persistent mental illness. The Western Journal of Medicine 169, 245–250. [PMC free article] [PubMed] [Google Scholar]
- Daumit GL, Pronovost PJ, Anthony CB, Guallar E, Steinwachs DM, Ford DE (2006). Adverse events during medical and surgical hospitalizations for persons with schizophrenia. Archives of General Psychiatry 63, 267–272. [DOI] [PubMed] [Google Scholar]
- De Hert M, Cohen D, Bobes J, Cetkovich-Bakmas M, Leucht S, Ndetei DM, Newcomer JW, Uwakwe R, Asai I, Möller H-J, Gautam S, Detraux J, Correll CU (2011). Physical illness in patients with severe mental disorders. II. Barriers to care, monitoring and treatment guidelines, plus recommendations at the system and individual level. World Psychiatry: Official Journal of the World Psychiatric Association (WPA) 10, 138–151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Douzenis A, Seretis D, Nika S, Nikolaidou P, Papadopoulou A, Rizos EN, Christodoulou C, Tsopelas C, Mitchell D, Lykouras L (2012). Factors affecting hospital stay in psychiatric patients: the role of active comorbidity. BMC Health Services Research 12, 166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Druss BG (2007). Improving medical care for persons with serious mental illness: challenges and solutions. The Journal of Clinical Psychiatry 68 (Suppl 4), 40–44. [PubMed] [Google Scholar]
- Druss BG, Zhao L, Cummings JR, Shim RS, Rust GS, Marcus SC (2012). Mental comorbidity and quality of diabetes care under Medicaid: a 50-state analysis. Medical Care 50, 428–433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frayne SM, Halanych JH, Miller DR, Wang F, Lin H, Pogach L, Sharkansky EJ, Keane TM, Skinner KM, Rosen CS, Berlowitz DR (2005). Disparities in diabetes care: impact of mental illness. Archives of Internal Medicine 165, 2631–2638. [DOI] [PubMed] [Google Scholar]
- Gross AL, Gallo JJ, Eaton WW (2010). Depression and cancer risk: 24 years of follow-up of the Baltimore Epidemiologic Catchment Area sample. Cancer Causes Control 21, 191–199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hackman AL, Goldberg RW, Brown CH, Fang LJ, Dickerson FB, Wohlheiter K, Medoff DR, Kreyenbuhl JA, Dixon L (2006). Use of emergency department services for somatic reasons by people with serious mental illness. Psychiatric Services (Washington, D.C.) 57, 563–566. [DOI] [PubMed] [Google Scholar]
- Haupt DW, Rosenblatt LC, Kim E, Baker RA, Whitehead R, Newcomer JW (2009). Prevalence and predictors of lipid and glucose monitoring in commercially insured patients treated with second-generation antipsychotic agents. The American Journal of Psychiatry 166, 345–353. [DOI] [PubMed] [Google Scholar]
- Howard L, Barley E, Davies E, Rigg A, Lempp H, Rose D, Taylor D, Thornicroft G (2010). Cancer diagnosis in people with severe mental illness: practical and ethical issues. The Lancet Oncology 11, 797–804. [DOI] [PubMed] [Google Scholar]
- IMS Health (2006). Hospitalisations évitables et Soins primaires. Etude réalisée pour le LEEM. Publications du LEEM, Puteaux, France. [Google Scholar]
- Jacobs R, Gutacker N, Mason A, Goddard M, Gravelle H, Kendrick T, Gilbody S, Aylott L, Wainwright J (2015). Do Higher Primary Care Practice Performance Scores Predict Lower Rates of Emergency Admissions for Persons with Serious Mental Illness? An Analysis of Secondary Panel Data. Health Services and Delivery Research. NIHR Journals Library: Southampton, UK. [PubMed] [Google Scholar]
- Jerant A, Fenton JJ, Franks P (2012). Primary care attributes and mortality: a national person-level study. Annals of Family Medicine 10, 34–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laursen TM, Munk-Olsen T, Nordentoft M, Mortensen PB (2007). Increased mortality among patients admitted with major psychiatric disorders: a register-based study comparing mortality in unipolar depressive disorder, bipolar affective disorder, schizoaffective disorder, and schizophrenia. The Journal of Clinical Psychiatry 68, 899–907. [DOI] [PubMed] [Google Scholar]
- Lawrence D, Kisely S (2010). Inequalities in healthcare provision for people with severe mental illness. Journal of Psychopharmacology (Oxford, England) 24, 61–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee C, Yoon H (2017). Medical big data: promise and challenges. Kidney Research and Clinical Practice 36, 3–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee DS, Marsh L, Garcia-Altieri MA, Chiu LW, Awad SS (2016). Active mental illnesses adversely affect surgical outcomes. The American Surgeon 82, 1238–1243. [PubMed] [Google Scholar]
- Li Y, Glance LG, Cai X, Mukamel DB (2008). Mental illness and hospitalization for ambulatory care sensitive medical conditions. Medical Care 46, 1249–1256. [DOI] [PubMed] [Google Scholar]
- Lichtermann D, Ekelund J, Pukkala E, Tanskanen A, Lönnqvist J (2001). Incidence of cancer among persons with schizophrenia and their relatives. Arch Gen Psychiatry 58, 573–578. [DOI] [PubMed] [Google Scholar]
- Mai Q, Holman CDJ, Sanfilippo FM, Emery JD (2011a). The impact of mental illness on potentially preventable hospitalisations: a population-based cohort study. BMC Psychiatry 11, 163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mai Q, Holman CDJ, Sanfilippo FM, Emery JD, Preen DB (2011b). Mental illness related disparities in diabetes prevalence, quality of care and outcomes: a population-based longitudinal study. BMC Medicine 9, 118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller BJ, Paschall CB, Svendsen DP (2006). Mortality and medical comorbidity among patients with serious mental illness. Psychiatric Services (Washington, D.C.) 57, 1482–1487. [DOI] [PubMed] [Google Scholar]
- Narrow WE, Rae DS, Robins LN, Regier DA (2002). Revised prevalence estimates of mental disorders in the United States: using a clinical significance criterion to reconcile 2 surveys’ estimates. Archives of General Psychiatry 59, 115–123. [DOI] [PubMed] [Google Scholar]
- O'Malley AS (2013). After-hours access to primary care practices linked with lower emergency department use and less unmet medical need. Health Affairs (Project Hope) 32, 175–183. [DOI] [PubMed] [Google Scholar]
- Page P (2014). Beyond statistical significance: clinical interpretation of rehabilitation research literature. International Journal of Sports Physical Therapy 9, 726–736. [PMC free article] [PubMed] [Google Scholar]
- Pinquart M, Duberstein P (2010). Depression and cancer mortality: a meta-analysis. Psychological Medicine 40, 1797–1810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plomondon ME, Ho PM, Wang L, Greiner GT, Shore JH, Sakai JT, Fihn SD, Rumsfeld JS (2007). Severe mental illness and mortality of hospitalized ACS patients in the VHA. BMC Health Services Research 7, 146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rathore SS, Wang Y, Druss BG, Masoudi FA, Krumholz HM (2008). Mental disorders, quality of care, and outcomes among older patients hospitalized with heart failure: an analysis of the national heart failure project. Archives of General Psychiatry 65, 1402–1408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rey G, Jougla E, Fouillet A, Hémon D (2009). Ecological association between a deprivation index and mortality in France over the period 1997–2001: variations with spatial scale, degree of urbanicity, age, gender and cause of death. BMC Public Health 9, 33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosano A, Loha CA, Falvo R, van der Zee J, Ricciardi W, Guasticchi G, de Belvis AG (2013). The relationship between avoidable hospitalization and accessibility to primary care: a systematic review. European Journal of Public Health 23, 356–360. [DOI] [PubMed] [Google Scholar]
- Salsberry PJ, Chipps E, Kennedy C (2005). Use of general medical services among Medicaid patients with severe and persistent mental illness. Psychiatric Services (Washington, D.C.) 56, 458–462. [DOI] [PubMed] [Google Scholar]
- Schoepf D, Uppal H, Potluri R, Heun R (2014). Physical comorbidity and its relevance on mortality in schizophrenia: a naturalistic 12-year follow-up in general hospital admissions. European Archives of Psychiatry and Clinical Neuroscience 264, 3–28. [DOI] [PubMed] [Google Scholar]
- Slobogean GP, Giannoudis PV, Frihagen F, Forte ML, Morshed S, Bhandari M (2015). Bigger data, bigger problems. Journal of Orthopaedic Trauma. 29(Suppl 12), S43–S46. [DOI] [PubMed] [Google Scholar]
- Small N, Brooks H, Grundy A, Pedley R, Gibbons C, Lovell K, Bee P (2017). Understanding experiences of and preferences for service user and carer involvement in physical health care discussions within mental health care planning. BMC Psychiatry 17, 138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sokal J, Messias E, Dickerson FB, Kreyenbuhl J, Brown CH, Goldberg RW, Dixon LB (2004). Comorbidity of medical illnesses among adults with serious mental illness who are receiving community psychiatric services. Journal of Nervous and Mental Disease 192, 421–427. [DOI] [PubMed] [Google Scholar]
- Šprah L, Dernovšek MZ, Wahlbeck K, Haaramo P (2017). Psychiatric readmissions and their association with physical comorbidity: a systematic literature review. BMC Psychiatry 17, 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stubbs B, Koyanagi A, Veronese N, Vancampfort D, Solmi M, Gaughran F, Carvalho AF, Lally J, Mitchell AJ, Mugisha J, Correll CU (2016). Physical multimorbidity and psychosis: comprehensive cross sectional analysis including 242,952 people across 48 low- and middle-income countries. BMC Medicine 14, 189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tidemalm D, Waern M, Stefansson C-G, Elofsson S, Runeson B (2008). Excess mortality in persons with severe mental disorder in Sweden: a cohort study of 12 103 individuals with and without contact with psychiatric services. Clinical Practice and Epidemiology in Mental Health: CP & EMH 4, 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Townsend P, Phillimore P, Beattie A (1988). Deprivation: Inequality and the North. Routledge: London. [Google Scholar]
- van Hasselt FM, Oud MJT, Loonen AJM (2013). Improvement of care for the physical health of patients with severe mental illness: a qualitative study assessing the view of patients and families. BMC Health Services Research 13, 426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Viron MJ, Stern TA (2010). The impact of serious mental illness on health and healthcare. Psychosomatics 51, 458–465. [DOI] [PubMed] [Google Scholar]
- Weissman JS, Gatsonis C, Epstein AM (1992). Rates of avoidable hospitalization by insurance status in Massachusetts and Maryland. JAMA 268, 2388–2394. [PubMed] [Google Scholar]
- Woodhead C, Ashworth M, Broadbent M, Callard F, Hotopf M, Schofield P, Soncul M, Stewart RJ, Henderson MJ (2016). Cardiovascular disease treatment among patients with severe mental illness: a data linkage study between primary and secondary care. The British Journal of General Practice: The Journal of the Royal College of General Practitioners 66, e374–e381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao Y, Wright J, Guthridge S, Lawton P (2013). The relationship between number of primary health care visits and hospitalisations: evidence from linked clinic and hospital data for remote Indigenous Australians. BMC Health Services Research 13, 466. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The database is available to researchers after they comply with French laws with regard to its access.