Abstract
Aims
To examine the quality of life (QOL) of parents of children with a specific mental disorder (any age).
Methods
Relevant articles were searched using different databases. Articles were included that compared the QOL of parents with mentally-ill children to parents of healthy controls or norm values or provided the required data for this comparison. A meta-analysis was conducted to obtain an overall mean effect size estimate. Additional analyses were performed to assess publication bias and moderation.
Results
Twenty-six out of 10 548 articles met the pre-defined inclusion criteria. Most of these studies focused on attention-deficit/hyperactivity disorder or autism spectrum disorder, used clinical samples that mainly included males and young children and studied the QOL of mothers. The meta-analysis revealed that parents of mentally-ill children are experiencing a clinically relevant reduction in their QOL relative to parents of healthy children and norm values (g = −0.66).
Conclusions
The compromised QOL of parents of mentally-ill children needs to be considered and addressed by health professionals who are in contact with them. The paper provides insights into existing research gaps and suggests improvements for subsequent work.
Key words: Adolescence, attention deficit hyperactivity disorder, autism, systematic reviews
Introduction
Mental disorders (including all conditions listed in Chapter V of the ICD (World Health Organization, 1992) or DSM (American Psychological Association, 2000, 2013) often have an early onset (Kessler et al., 2007; De Girolamo et al., 2012), with some conditions typically emerging in childhood (e.g., behavioural disorders or specific anxiety disorders) and others during adolescence and early adulthood (mood, anxiety, substance use, and psychotic disorders) (De Girolamo et al., 2012). These disorders account for a large proportion of the burden of disease in youth (Costello et al., 2005; Patel et al., 2007; Gore et al., 2011).
Parents occupy an important role in caring for a mentally-ill child and in fulfilling tasks that parents of children without such conditions are not confronted with, such as initiating and supporting the child's professional help-seeking (Logan and King, 2001; Sayal, 2006) or providing elevated and continuous levels of informal care (Chan, 2011). Furthermore, parents might experience negative emotions, such as worries and anxiety about whether someone else will assume the caregiving role for their child if they were no longer capable or around to do so (Corcoran et al., 2015; Klages et al., 2016).
Quality of life (QOL) is defined as ‘individuals’ perception of their position in life in the context of the culture and value systems in which they live and in relation to their goals, expectations, standards and concerns.’ (WHOQOL Group, 1995) and can be used to assess the situation of parents of mentally-ill children. This is particularly important, since a compromised parental QOL does not only concern caregivers, but can also negatively impact the child (Lange et al., 2005). So far, the impact of a care receiver's mental disorder on a caregiver has often been captured via concepts such as caregiver burden, parenting/psychological (di)stress or as frequencies of mental health problems (Steele et al., 2007; van der Voort et al., 2007; Zabala et al., 2009; Theule et al., 2010). The advantages of using the QOL instead of the above-mentioned concepts are in large due to QOL's broadness and multidimensionality.
To the best of our knowledge, only one systematic review specifically focused on the QOL of parents of mentally-ill children (Vasilopoulou and Nisbet, 2016). Among other things, these authors aimed to describe the QOL of parents of children (<18 years) with autism spectrum disorder (ASD) relative to the QOL of parents of typically developing children or norms. The present systematic review (first part of this paper) pursues similar aims. However, we do not focus on a specific mental disorder but include all conditions listed in Chapter V of the ICD (World Health Organization, 1992) or DSM (American Psychological Association, 2000, 2013). In doing so, we aim to outline the landscape of this field of research (e.g., illustrate which mental disorders have been considered or neglected so far). Furthermore, the current review differs from the one described above in so far as parents of children of any age are considered. This is important as the current paper does not only focus on mental disorders with an early onset (such as ASD), but also on conditions that might develop later in life (e.g., schizophrenia). In the second part, a meta-analysis regarding the comparison of parents of mentally-ill children v. parents of healthy controls or norms (including norm values reported in manuals of QOL-measures as well as QOL-data from the general population) is carried out. Based on existing publications in this and related fields, it is hypothesized that parents of children with a mental disorder report lower QOL relative to parents of healthy children/norms.
Methods of systematic review
Data sources and search strategy
A literature search was conducted (up to March 2017) to identify studies that (1) compare the QOL of parents of children with a mental disorder (any age) v. the QOL of healthy controls/norm values or (2) would allow such a comparison. The following databases were searched: the Cochrane database of systematic reviews, CINAHL, Embase, PsycInfo, and Pubmed. Searches were conducted in English, using the following keywords and Boolean operators: (‘quality of life’ OR QOL OR ‘health-related quality of life’ OR HRQOL) AND (parent* OR mother* OR maternal OR father* OR paternal) AND (child* OR daughter* OR son(s) OR offspring OR adolescent* OR ‘youth’) AND ((mental* OR psychiatric OR psychological OR behavio(u)ral OR emotional OR developmental) AND (diagnosis OR diagnoses OR disorder* OR difficult* OR disabilit* OR disease* OR disturb* OR health OR ‘health problem*’ OR problem* OR illness* OR ill OR morbidit*)). Additionally, keywords were used to search for specific mental disorders listed in the ICD/DSM.
Study selection
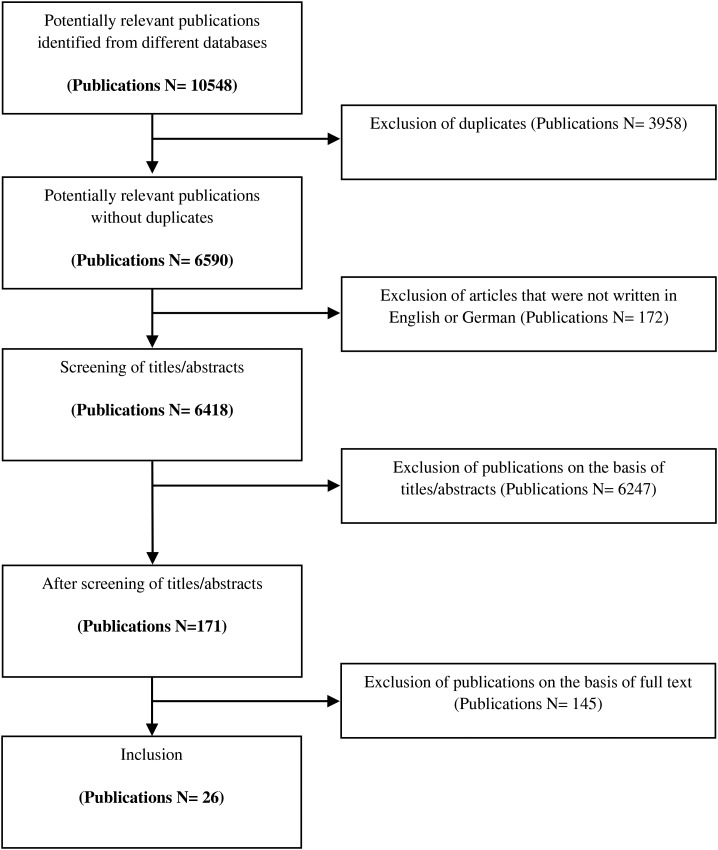
The process of study selection is outlined in Fig. 1. The search revealed 10 548 articles. After eliminating all duplicates (3958) and those articles not written in English or German (172), 6418 articles remained. Titles and abstracts of these entities were screened for eligibility by M.D. Altogether, 6247 articles were excluded during this stage. The remaining 171 articles were reviewed by two authors (M.D.; M.P.S.). Studies were excluded if at least one of the following pre-defined criteria was met:
-
(1)
Only published as an abstract (of an oral presentation), poster or thesis
-
(2)
No empirical data
-
(3)
Studies with no quantitative data/single-case studies
-
(4)
Intervention studies with no baseline data
-
(5)
Data already published in another included article
-
(6)
No mental disorder from Chapter V of the ICD or DSM
-
(7)
Mental disorder diagnosis not confirmed (not verified by a health professional or not assessed through a diagnostic instrument that has been designing to obtain a DSM- or ICD-diagnosis)
-
(8)
Very heterogeneous mental disorders (e.g., ‘any mental disorder’)
-
(9)
Mental disorder with an underlying physical disorder
-
(10)
No generic/multidimensional QOL-measure targeting parents
-
(11)
No standardised QOL-measure
-
(12)
Less than 80% of participants are parents (criteria does not apply if results are presented separately for parents)
-
(13)
No comparison between parents of children with mental disorders v. parents of healthy children/norm values are presented/provided
-
(14)
No basic descriptive data (means, s.d., group sizes) available or provided regarding the QOL of parents of mentally-ill children and for parents of healthy controls/norm values
Fig. 1.
Study selection.
The criteria were applied hierarchically. If necessary information was not reported in the publications (e.g., means and s.d. of the QOL-domains; no comparison with a control/norm group), authors were contacted and asked to provide the required data (if available). Furthermore, authors were contacted to clarify any ambiguities. Inclusion criteria were defined as complementary to the exclusion criteria. Disagreements in the appraisal of the articles between M.D. and M.P.S. were resolved through discussion. Ultimately, 26 publications were included while 145 were excluded.
Data extraction
Two independent reviewers (M.D.; S.H.) extracted data from the 26 included studies. Norms were defined as norm values reported in manuals of QOL-measures and QOL-data from the general population (i.e. not only parents) that has been collected and published by other authors or by the authors of the included studies.
Results of systematic review
Excluding entities
Reasons for excluding entities based on full-text analyses are listed in Table 1. Since the exclusion criteria were applied hierarchically, one exclusion criterion per entity is reported.
Table 1.
Reasons for exclusion of entities with full-text analyses (organised according to the hierarchy that was applied during the exclusion process)
| Reason for exclusion | Frequency |
|---|---|
| Only published as an abstract (of an oral presentation), poster or thesis | 37 |
| Intervention studies with no baseline data | 1 |
| Data already published in another included article | 3 |
| Mental disorder diagnosis not confirmed (not verified by a health professional/diagnostic instrument) | 23 |
| Included mental disorders are very heterogeneous (e.g., any mental disorder) | 20 |
| Mental disorder with an underlying physical disorder | 1 |
| No generic/multidimensional QOL-measure targeting parents (including QOL-measures for children that include a family impact scale) | 17 |
| Parents represent less than 80% of participants (criteria does not apply if results are presented separately for parents) | 1 |
| No comparison between parents of children with mental disorders v. parents of healthy children/norm values | 32 |
| No basic descriptive data (means, s.d., group sizes) available regarding the QOL of parents of mentally-ill children and for parents of healthy controls/norm values | 6 |
| Others | 4 |
Table 2 lists the conditions that the excluded articles targeted. The numbers do not add up to 145 since some articles targeted several groups of children with mental disorders. Furthermore, it must be considered that some authors published several articles that were based on the same data set. ASD was most frequently studied (n = 56). Furthermore, ADHD was studied in a considerable number of articles (n = 23).
Table 2.
Mental disorders targeted in the excluded articles (organised according to the DSM)
| Mental disorder | Frequency |
|---|---|
| Any mental disorders, (possibly) including heterogeneous conditions (specified or unspecified) | 8 |
| Developmental disorders (or delays/disabilities)a | 21 |
| Intellectual disabilitiesa | 24 |
| Communication disorders (specific language impairments, speech impairments) | 3 |
| Autism Spectrum Disorder | 56 |
| Attention-Deficit/Hyperactivity Disorder | 23 |
| Specific learning disorders | 2 |
| Motor Disorders | 1 |
| Schizophrenia | 2 |
| Bipolar disorder | 3 |
| Obsessive-Compulsive Disorder | 1 |
| Eating disorders | 1 |
| Enuresis | 3 |
| Oppositional Defiant Disorder | 2 |
This term was not applied uniformly in the different studies and did often not correspond to particular ICD/DSM categories (i.e., some studies included a variety of very heterogeneous conditions).
Included studies
Considered mental disorders
As shown in Table 3, the largest proportion of included studies focused on ASD and related disorders (n = 12; Allik et al., 2006; Mugno et al., 2007; Lee et al., 2009; Benjak et al., 2011; Yamada et al., 2012; Eapen et al., 2014; Ji et al., 2014; Kuhlthau et al., 2014; Suzumura 2015; Chan and Lai 2016; Killian et al., 2016; Niinomi et al., 2016), followed by ADHD (n = 7; Lange et al., 2005; Schreyer and Hampel 2009; Xiang et al., 2009; Hadi et al., 2013; Kandemir et al., 2014; Avrech Bar et al., 2015; Zare et al., 2017).
Table 3.
Quality of life in parents of (adult) children with mental disorders v. parents of healthy controls/norm values (in 26 studies that met final inclusion criteria)
| Study; year of publication/data collection | Country | Comparison | Sampling of caregivers (1) of mentally-ill children and of (2) control childrena | Age in years of (1) mentally-ill and (2) control childrena | % males of (1) mentally-ill and (2) control childrenb | Age in years of parents of (1) mentally-ill and (2) control childrenb | Measure |
|---|---|---|---|---|---|---|---|
| Autism spectrum disorder (ASD)c and related disorders (with comorbidities) | |||||||
| Eapen et al. (Eapen et al., 2014) 2014/not reported |
Australia | 23 mothers of children with ASD v. norm values from Australia (396)d | (1) The ASD group consisted of mothers of children on the waitlist for, or having recently commenced at, an Autism Specific Early Learning and Care Centre. No information is provided about response/refusal rate. | (1) mean = 4.1; s.d. = 1.4 | (1) 73.9 | (1) mean = 35.1; s.d. = 4.5 | WHOQOL-BREF |
| Ji et al. (Ji et al. 2014) 2014/March 2011 to July 2012 |
China | 273 caregivers (72.9% mothers, 11% fathers, 16.1% aunts or grandparents) of children with ASD v. norm values (207) | (1) Caregivers of children with ASD were recruited in 15 autism centres by simple cluster sampling. The response rate was 97.5% (2.5% refused to participate because of privacy considerations). | (1) mean = 4.8; s.d. = 2.0 | (1) 81.0 | (1) mean = 35.2; s.d. = 9.6 | SF-36 |
| Niinomi et al. (Niinomi et al. 2016) 2016/2007–2009 |
Japan | 24 mothers of children with ASD v. general female population in Japan (n = 123) | (1) Mothers of children with ASD were recruited via flyers at public facilities (e.g., an autism society and a developmental support center). No information is provided about response/refusal rate. | (1) mean = 7.0; s.d. = 2.8; range = 3.5–12.5 | (1) 84.6 | (1) mean = 39.5, s.d. = 4.5 | WHOQOL-BREF |
| Kuhlthau et al. (Kuhlthau et al. 2014) 2014/not reported |
USA | 224 parents (95% parents; 89.5% of the parents were mothers) of children with ASD v. general population scores from the literature (642) | (1) Parents were sampled from two sites – a developmental center and an outpatient psychiatric clinic. Parents of children with confirmed ASD who agreed to be contacted for future research projects at an earlier date (90% and 95% at the above-mentioned sites) were considered for the study. The final response rates at the two sites were 53.2% and 60.9%, respectively. | (1) mean = 8.4, s.d. = 3.5, range = 4–18 | (1) 86.5 | (1) mean = 39.4, s.d. = 8.3, range = 22–61 | SF-6D EQ-5D |
| Benjak et al. (Benjak et al. 2011) 2011/not reported |
Croatia | 178 parents of children with ASD (59% mothers) v. 172 parents of non-disabled children (58.7% mothers; matched by sex and age of children, parents' age group and educational background, and municipality of residence) | (1) Parents of children with ASD were contacted through the Croatian Autism Center and its branch offices as well as through educational centers for children with disability. Questionnaires were distributed to 250 parents who agreed to participate (no information is provided about how many parents refused to participate). Thereof, 178 correctly filled in the questionnaires within the given deadline (response rate = 71.2% among those who agreed to participate). (2) Family doctors and school administrators were provided with lists about participants of the ASD-group and their key characteristics according to which they had to select matching parents from their client database. No information is provided about response/refusal rate in the control group. |
(1/2)* | (1) 83.7 (2)* |
(1) median = 43, range = 27–83 (2) median = 42, range = 24–82 |
SF-36 PWI |
| Allik et al. (Allik et al. 2006) 2006/not reported |
Sweden | 31 mothers of children with AS/HFA v. 30 mothers of age- and gender-matched children with typical development 30 fathers of children with AS/HFA v. 29 fathers of age- and gender-matched children with typical development |
(1) The study sample was selected from a total of 122 children with a clinical diagnosis of AS who were registered at three PDD-habilitation centers. Thereof, 53 had to be excluded due to the defined exclusion criteria. Information was collected about 32 of the remaining 69 children (response rate = 46.4%). (2) The control group was recruited via school nurses. No information is provided about the response/refusal rate. |
(1) mean = 10.8, range = 8–12 (2) 10.9, range = 8–13 |
(1) 87.5 (2) 87.5 |
(1) mothers: mean = 42.4, range = 28–54; fathers: mean = 45.6, range = 35–64 (2) mothers: mean = 40.3, range = 31–51; fathers: mean age = 42.7, range = 35–53 |
SF-12 |
| Lee et al. (Lee et al. 2009) 2009/not reported |
USA | 89 parents of children with HFASD (70.7% mothers) v. 46 parents of children without disabilities (70.2% mothers) | (1) Parents were recruited from a social skills summer program serving children with HFASD. All parents who were invited agreed to participate (response rate = 100%). (2) Parents of the control group were recruited from the local community by word of mouth and flyers. All parents who initially agreed to participate completed and returned the measures. However, no information is provided about the number of parents who were initially asked to participate (no response rate can be calculated). |
(1) mean = 9.5, s.d. = 2.0, range = 7–13 (2) mean = 9.7, s.d. = 2.1, range = 7–13 |
(1) 91.9 (2) 90.0 |
(1) mean = 42.2, s.d. = 6.2 (2) mean = 38.5, s.d. = 5.4 |
SF-36 |
| Suzumura (Suzumura 2015) 2015/not reported |
Japan | 30 mothers of preschoolers with HFPDD v. 30 mothers of age- and gender-matched typically developing children | (1) The sample was recruited at a child psychiatric outpatient clinic. No information is provided about response/refusal rate. (2) The control group was recruited in kindergartens (via kindergarten nurses) located in the same region as the outpatient clinic where the clinical sample was recruited. No information is provided about response/refusal rate. |
(1) mean = 5.0, range = 3–6 (2) mean = 5.0, range = 3–6 |
(1) 83.3 (2) 83.3 |
(1) mean = 37.7, s.d. = 4.6, range = 28–47 (2) mean = 36.5, s.d. = 4.7, range = 28–46 |
SF-36 |
| Mugno et al. (Mugno et al. 2007) 2007/June 2005 to June 2006 |
Italy | 39 mothers of children with PDD v. 42 mothers of healthy children 30 fathers of children with PDD v. 35 fathers of healthy children |
(1) The questionnaire was distributed to the families of the study group during inpatient/outpatient visits, during home visits or by mail. Altogether, 39 out of 120 questionnaires were not sent back (refusal rate = 32.5%; response rate = 67.5%). Of the questionnaires that were sent back, 12 were excluded due to missing data. (2) The control group was recruited via school nurses of mainstream schools. Altogether, 19 out of 40 questionnaires were not returned (refusal rate = 47.5%; response rate = 52.5%). Additionally, seven questionnaires had to be excluded due to missing data. |
(1) mean = 7.5, s.d. = 5 (2) mean = 8, s.d. = 4 |
(1) 79.2 (2) 35.4 |
(1) mean = 37, s.d. = 12.7, range = 3–17 (2) mean = 41, s.d. = 14.3, range = 4–15 |
WHOQOL-BREF |
| Yamada et al. (Yamada et al. 2012) 2012/September to November 2006 |
Japan | 147 mothers of children with PDD v. norms (255) 122 fathers of children with PDD v. norms (241) |
(1) A consecutive sample of parents of children with PDD who visited an outpatient clinic was used. The study was explained to 198 families, whereof 147 families participated (response rate = 74.2%), including 147 mothers and 122 fathers (covering 158 children). | (1) mean = 9.1, s.d. = 2.5, range = 6–15 | (1) 81.65 | (1) mothers: mean = 38.3, s.d. = 4.6; fathers: mean = 41.0, s.d. = 5.7 |
SF-36 |
| Killian et al. (Killian et al. 2016) 2016/2006–2014 |
USA | Caregiver of children with Rett syndrome (727; approximately 95% were mothers; precise percentage unknown) v. norm values of the general female US-population, age group 35–44 (7069) | (1) Individuals with classic Rett syndrome were recruited as part of the multicenter Rett Natural History Study. No information is provided about response/refusal rates. | (1) mean = 9.2, s.d. = 8.3, range = 1–47 | (1) 0 | (1) mothers: mean = 38.3, s.d. = 9.0, range = 20–81; fathers: mean = 40.5, s.d. = 9.5, range = 19–83 | SF-36 |
| Chan & Lai (Chan and Lai 2016) 2016/2006–2014 |
China | 117b parents (72.6% mothers; 25.6% fathers; 1.7% other guardians) of children with ASD with comorbid learning disabilities v. local normative data from the general population of Hong Kong (155) | (1) Convenient sampling was used at a child and adolescent psychiatric clinic of a university teaching hospital (at follow-ups) and in special schools for children with learning disability in the same catchment area as the clinic (schools were first informed about the purpose of the study and the inclusion criteria and information sessions were then held for parents). No information is provided about the response/refusal rate. | (1) mean = 10.4, s.d. = 4.1, range = 4–21 | (1) 88 | (1) mothers: mean = 43.6, s.d. = 5.2, range = 34–57; fathers: mean = 46.4, s.d. = 5.6, range = 35–61 | WHOQOL-BREF |
| Attention-deficit/hyperactivity disorder (ADHD) and additional disorders | |||||||
| Hadi et al. (Hadi et al. 2013) 2013/not reported |
Iran | 100 mothers of children with ADHD v. 100 mothers of age- and gender-matched healthy 4th grade primary school students | (1) Mothers of children with ADHD who were referred to a psychiatric clinic were recruited. No information is provided about response/refusal rate. (2) The control group targeted mothers of healthy 4th grade students. No information is provided about response/refusal rate. |
(1/2)* | (1/2)* | (1) mean = 35.04, s.d. = 6.02, range = 23–50 (2) mean = 33.49, s.d. = 4.47, range = 25–48 |
SF-36 |
| Zare et al. (Zare et al. 2017) 2017/not reported |
Iran | 101 parents of children with ADHD (86% mothers) v. 243 parents (69% mothers) of school children (control group) | (1) The study sample was recruited at a child psychiatric clinic. No information is provided about response/refusal rate. (2) Parents belonging to the control group were selected in a two-stage cluster random sampling from the four educational districts of Shiraz. No information is provided about response/refusal rate. |
(1/2)* |
(1/2)* | (1) mean = 34.8, s.d. = 6.1 (2) mean = 37.3, s.d. = 7.1 |
SF-36 |
| Xiang et al. (Xiang et al. 2009) 2009/October 2007 to February 2008 |
China | 77 parents (83.1% mothers) of children with ADHD v. norms of the general population of Hong Kong (155) | (1) A consecutive sample was used. Subjects meeting the study criteria were invited to participate in the study when they attended the psychiatric clinic of a university-affiliated district general hospital for routine follow up. Altogether, 77 out of 98 parents who were approached participated (response rate = 78.6%). | (1) mean = 10.1, s.d. = 2.0 | (1) 79.2 | (1) mean = 41.7; s.d. = 5.3 | WHOQOL-BREF |
| Kandemir et al. (Kandemir et al. 2014) 2014/February to September 2008 |
Turkey | 76 mothers of children with ADHD v. 59 mothers of control children (matched by age, gender, family income level, family type) | (1) The sample was recruited via an outpatient clinic. No information is provided about response/refusal rate. (2) The control group included children who were attending a summer school. No information is provided about response/refusal rate. |
(1) mean = 10.5, s.d. = 2.4, range = 7–16 (2) mean = 10.4, s.d. = 2.2, range = 7–16 |
(1) 71.1 (2) 62.7 |
(1/2)* | SF-36 |
| Avrech Bar et al. (Avrech Bar et al. 2015) 2015/not reported |
Israel | 20 mothers of children with ADHD v. 20 mothers of typically developing children (matched by mothers’ age and number of children) | (1/2) No details are provided about the sampling and response/refusal rate. However, based on the inclusion criteria it can be assumed that the control sample was recruited via schools. | (1) mean = 7.2, s.d. = 2.6, range = 1–14 (2) mean = 7.7, s.d. = 2.8 |
(1) 85 (2)* |
(1) mean = 33.5, s.d. = 4.4, range = 26–42 (2) mean = 33.8, s.d. = 3.8, range = 28–40 |
SF-36 |
| Schreyer & Hampel (Schreyer and Hampel 2009) 2009/October 2006 to March 2007 |
Germany | 29 mothers of children with ADHD v. 29 mothers of healthy controls (matched by age, verbal intelligence, and education level) | (1) A consecutive sample was used. Children with ADHD and their mothers were recruited at a rehabilitation clinic, specialised in treating children with ADHD. The response rate was 100%. (2) Children of the control group and their mothers were recruited in several schools (children were asked to carry a letter about the study to their parents). No information is provided about response/refusal rate. |
(1) range = 8–11 (2) range = 8–11 |
(1) 100 (2) 100 |
(1/2)* | SF-8 |
| Lange et al. (Lange et al. 2005) 2005/November 2001 to March 2003 |
Ireland | 22 mothers/13 fathers of boys with ADHD v. 20 mothers/15 fathers of boys with an emotional disorder (mood or anxiety disorder) v. 26 mothers/16 fathers of normal controls (groups were matched by age and gender of children and family composition) | (1) Both clinical groups were recruited trough child psychiatric and community care psychology services (convenience samples). No information is provided about response/refusal rate. (2) The control group was recruited through urban and rural primary schools (convenience sample). No information is provided about response/refusal rate. |
(1) ADHD: mean = 8.43; s.d. = 2.88 (1) emotional disorder: mean = 8.89; s.d. = 3.09 (2) mean = 8.11; s.d. = 2.06 |
(1) ADHD: 100 (1) Emotional disorder: 100 (2) 100 |
(1) ADHD: mean = 34.5; s.d. = 7.5 (1) emotional disorder: mean = 42.3; s.d. = 5.9 (2) mean = 41.4; s.d. = 5.3 |
Quality of Life Inventory |
| Other neurodevelopmental disorders | |||||||
| Jalenques et al. (Jalenques et al. 2017) 2017/October 2010 to September 2013 |
France | 75 mothers of adolescents with GTS v. 75 mothers of gender- and age-matched healthy controls 63 fathers of adolescents with GTS v. 62 fathers of gender- and age-matched healthy controls |
(1) The sample was recruited from primary and secondary referral centers. Overall, 83 families of adolescents with GTS were considered. Excluding the 6 families that remained uncontactable (83–6 = 77), the response rate for mothers was 97.4% and those of fathers 81.8%. (2) A control family was recruited for each family with an adolescent with GTS. To be included, the control family had to live in the same region, be composed of the same number of children, and have no family relationship with the GTS-family. No information is provided about participation/refusal rate. |
(1) mean = 14.8, s.d. = 1.8, range = 12–18 (2) range = 12–18, range = 12–18 |
(1) 80 (2) 80 |
(1) mothers: mean = 44.1, s.d. = 4.7; fathers: mean = 47.1, s.d. = 6.2 (2) mothers: mean = 45.3, s.d. = 4.8; fathers: mean = 47.3, s.d. = 5.5 |
SF-36 WHOQOL-BREF |
| Ginieri-Coccossis et al. (Ginieri-Coccossis et al. 2012) 2012/not reported |
Greece | 70 parents (84.3% mothers) of children with SpLD v. 69 parents (69.6% mothers) of typically developing children | (1) The study sample was recruited at a centre specialised in diagnosing and treating SpLD. Children were recruited if they have not visited the centre previously. One case refused to participate (i.e. response rate = 98.6%). (2) A convenient sample recruited from a central public school of the same area as the clinical sample was used. No information is provided about response/refusal rate. |
(1) mean age = 10.1, s.d. = 2.24 (2) mean age = 10.6, s.d. = 2.77 |
(1) 54.3 (2) 58 |
(1) mean age = 38.1, s.d. = 3.84 (2) mean age = 37.9, s.d. = 5.84 |
WHOQOL-BREF |
| Schizophrenia | |||||||
| Foldemo et al. (Foldemo et al. 2005) 2005/2001 |
Sweden | 38 parents of outpatients with schizophrenia (68% mothers) v. reference group (consisting of parents and non-parents; 46% females; 698) | (1) Outpatients with schizophrenia were recruited at a psychiatric outpatient clinic. Parents of these outpatients were contacted if outpatients gave permission to do so. The response rate among contacted parents was 86%. (2) The population study consisted of a randomly selected group of 18–80-year olds who were drawn from the Swedish population register. Altogether, 1800 people of the total targeted sample (2980 people) participated, which corresponds to a response rate of 61%. Thereof, 698 people between 51 and 80 years of age (parents and non-parents) were selected as reference group. |
(1) mean age = 38, s.d. = 7 | (1) 81.3 (gender only reported for 32 people) | (1) mean age = 66, s.d. = 9, range = 51–80 (2) mean age = 63, s.d. = 8, range = 51–80 |
Quality of Life Index |
| Eating disorders/substance-related disorder | |||||||
| Anastasiadou et al. (Anastasiadou et al. 2016) 2016/October 2011 to July 2014 |
Spain | 48 mothers of adolescents with ED v. 47 mothers of adolescents with SRD v. 66 mothers of healthy controls 45 fathers of adolescents with ED v. 37 fathers of adolescents with SRD and 50 fathers of healthy controls |
(1a) The study sample was randomly recruited from consecutive admissions to inpatient or outpatient services at the Eating Disorders Unit of the Child and Adolescent Psychiatric Department of a university hospital. Altogether, 51 families were informed about the study, whereof 49 decided to participate (response rate = 96.1%; one patient had to be excluded later on due to exhibiting psychotic symptoms). (1b) The study sample was randomly recruited from an adolescent outpatient clinic for treatment for substance abuse or dependence. Altogether, 47 out of 55 families were willing to participate (response rate = 85.5%). (2) The control group consisted of families recruited from public secondary schools and were matched for age and gender with ED patients. A summary of the study was provided to students asking them to inform their parents about it. Eighty-seven of the families that expressed interest in participating were approached and 73 agreed to participate in the study (response rate cannot be calculated on the basis of the provided information). |
(1) ED: mean age = 14.8, s.d. = 1.7 , range = 12–18 (1) SRD: mean age = 18.2, s.d. = 2.1, range = 12–22 (2) mean age = 14.5, s.d. = 1.4, range = 12–18 |
(1) ED: 0 1) SRD: 85.1 (2) 0 |
(1) ED: mothers: mean = 44.9, s.d. = 4.5; fathers: mean = 47.5, s.d. = 4.1 (1) SRD: mothers: mean = 49.6, s.d. = 4.9; fathers: mean = 51.5, s.d. = 5.7 (2) mothers: mean = 47.5, s.d. = 4.0; fathers: mean = 50.0, s.d. = 4.1 |
SF-36 |
| Nocturnal enuresis | |||||||
| Naitoh et al. (Naitoh et al. 2012) 2012/2005–2009 |
Japan | 139 mothers of children with NE v. 109 mothers of age- and gender-matched children without NE | (1) Children who were presented with NE at an outpatient clinic and their mothers were recruited for the study. No information is provided about refusal/response rate. (2) The control group consisted of age- and gender-matched pairs of children without NE who volunteered to participate and their mothers. No information is provided about response/refusal rate. |
(1) mean = 9.7; s.d. = 2.6 (2) mean = 9.9; s.d. = 2.5 |
(1) 79.1 (2) 74.3 |
(1) mean = 39.8; s.d. = 4.3 (2) mean = 38.5; s.d. = 4.6 |
SF-36 |
| Kilicoglu et al. (Kilicoglu et al. 2014) 2014/January 2012 to June 2013 |
Turkey | 82 mothers of children with ED v. 93 mothers of healthy children (matched by age, gender, parents' education level and socioeconomic status) | (1) The sample was recruited via an outpatient clinic. No information is provided about response/refusal rate. (2) The control group was recruited via house visits. No response rate can be calculated, since the authors only provide an approximate number of houses that were contacted (200). It is unclear how many of them were actually eligible and were informed about the study. |
(1) mean = 9.6, s.d. = 1.3, range = 8–12 (2) mean = 9.5, s.d. = 1.2, range = 8–12 |
(1) 59.8 (2) 54.8 |
(1/2) * | WHOQOL-BREF |
| Egemen et al. (Egemen et al. 2008) 2008/May 2005 to August 2006 |
Turkey | 28 mothers of children with MNE v. 38 mothers of children without any health problems | (1) Mothers of children with NE were selected from those who applied for treatment at a university hospital. No information is provided about response/refusal rate. (2) Mothers who presented their child for outpatient service at the same hospital as the clinical sample were selected consecutively. No information is provided about response/refusal rate. |
(1) mean = 8.5, s.d. = 2.5 (2) mean = 8.3, s.d. = 2.5 |
(1) 50 (2) 47 |
(1) mean = 34.0, s.d. = 4.3 (2) mean = 36.2, s.d. = 6.8 |
SF-36 |
ADHD, attention-deficit hyperactivity disorder; AS, Asperger syndrome; ASD, autism spectrum disorder; ED, eating disorder; GTS, Gilles de la Tourette Syndrome; HFA, high-functioning autism; HFASD, high-functioning autism spectrum disorder; HFPDD, high functioning pervasive developmental disorders; MNE, monosymptomatic enuresis nocturna; NE, noctural enuresis; PDD, pervasive developmental disorders; SpLD, specific learning disabilities; SRD, substance-related disorders; QOL, quality of life; PWI, Personal Wellbeing Index; SF-8, −12, −36, −6D, 8-Item/12-Item/36-Item/ Short Form Survey or Short Form Six Dimension; WHOQOL-BREF, World Health Organization Quality of Life-BREF.
No description/information is provided if norm values were used for the comparison. * not reported/not available.
The publication speaks about 116 caregivers. However, the authors provided additional data and confirmed that the correct number of participants is 117.
Disorders with the DSM-code 299.00 as well as those listed under F84 in the ICD are considered.
This study included a control group. However, the WHOQOL-BREF was only filled out in the clinical group. Hence, existing norm values of the WHOQOL-BREF were used for the current paper.
Preformed comparisons as well as recruitment and response/refusal rates of studied groups
Nine comparisons were based on norm values (Foldemo et al., 2005; Xiang et al., 2009; Yamada et al., 2012; Eapen et al., 2014; Ji et al., 2014; Kuhlthau et al., 2014; Chan and Lai, 2016; Killian et al., 2016; Niinomi et al., 2016). All other studies (n = 17) assessed a control group. Among the former, five (i.e. 55.6%) provide information about response/refusal rate in regard to caregivers of mentally-ill children (Foldemo et al., 2005; Xiang et al., 2009; Yamada et al., 2012; Ji et al., 2014; Kuhlthau et al., 2014). Among studies that assessed a control group, one provided information about response/refusal rate for both groups (Mugno et al., 2007), seven only for caregivers of mentally-ill children (Allik et al., 2006; Lee et al., 2009; Schreyer and Hampel, 2009; Benjak et al., 2011; Ginieri-Coccossis et al., 2012; Anastasiadou et al., 2016; Jalenques et al., 2017) and nine for neither group (Lange et al., 2005; Egemen et al., 2008; Naitoh et al., 2012; Hadi et al., 2013; Kandemir et al., 2014; Kilicoglu et al., 2014; Avrech Bar et al., 2015; Suzumura, 2015; Zare et al., 2017). Caregivers of mentally-ill children were mostly recruited via (psychiatric) outpatient clinics or other centers specialised on the child's diagnosis.
Caregivers of mentally-ill children
Altogether, ten studies only include mothers of mentally-ill children (Egemen et al., 2008; Schreyer and Hampel, 2009; Naitoh et al., 2012; Hadi et al., 2013; Eapen et al., 2014; Kandemir et al., 2014; Kilicoglu et al., 2014; Avrech Bar et al., 2015; Suzumura, 2015; Niinomi et al., 2016). Six studies included both mothers and fathers and examined these groups separately (Lange et al., 2005; Allik et al., 2006; Mugno et al., 2007; Yamada et al., 2012; Anastasiadou et al., 2016; Jalenques et al., 2017). The remaining ten studies also included both fathers and mothers, but did not differentiate between the groups (Foldemo et al., 2005; Lee et al., 2009; Xiang et al., 2009; Benjak et al., 2011; Ginieri-Coccossis et al., 2012; Ji et al., 2014; Kuhlthau et al., 2014; Chan and Lai, 2016; Killian et al., 2016; Zare et al., 2017). The percentage of mothers was larger than the percentage of fathers in all of these studies.
Socio-demographic characteristics of children
The mean age of children was mostly below 10 years (14 studies; Lange et al., 2005; Mugno et al., 2007; Egemen et al., 2008; Lee et al., 2009; Naitoh et al., 2012; Yamada et al., 2012; Eapen et al., 2014; Ji et al., 2014; Kilicoglu et al., 2014; Kuhlthau et al., 2014; Avrech Bar et al., 2015; Suzumura 2015; Killian et al., 2016; Niinomi et al., 2016). And the percentage of males was mostly over 70% (in 19 studies; Foldemo et al., 2005; Lange et al., 2005; Allik et al., 2006; Mugno et al., 2007; Lee et al., 2009; Schreyer and Hampel 2009; Xiang et al., 2009; Benjak et al., 2011; Naitoh et al., 2012; Yamada et al., 2012; Eapen et al., 2014; Ji et al., 2014; Kandemir et al., 2014; Kuhlthau et al., 2014; Avrech Bar et al., 2015; Suzumura 2015; Chan and Lai 2016; Niinomi et al., 2016; Jalenques et al., 2017).
Methods of meta-analysis
Effects were extracted for the QOL-measures mentioned in Table 3 (SF-6D/8/12/36, WHOQOL-BREF, EQ-5D, QOL Index, QOL Inventory, and PWI). The N of the studied groups was sometimes slightly lower in these analyses relative to the N reported in Table 3 (only cases without missing QOL-data were considered).
The following measures were taken to reduce interdependences of effects: Firstly, only effects for mothers were considered in studies that reported effects for mothers and fathers of the same child separately (Lange et al., 2005; Allik et al., 2006; Mugno et al., 2007; Yamada et al., 2012; Anastasiadou et al., 2016; Jalenques et al., 2017). Since most included studies targeted samples that (mainly) consisted of mothers, the described decision allowed to reduce possible heterogeneity. Secondly, only one comparison was considered from publications that compared the QOL of caregivers of two different groups of mentally-ill children to just one control group. In one study (Anastasiadou et al., 2016), caregivers of children with substance-related disorders (SRD) were included (excluded: caregivers of children with eating disorders, ED) as the proportion of boys was higher in this clinical group and thus more comparable with the other included studies. In another study (Lange et al., 2005), the ADHD sample was given preference over the ED sample, since ADHD was the second most commonly considered disorder in the included studies. Thirdly, only one QOL-measure was considered per study. In one study (Jalenques et al., 2017), the more prevalent measure (SF-36) was used for the meta-analysis (excluded: WHOQOL-BREF). Another study (Benjak et al., 2011) used two QOL-measures (PWI and SF-36), but the means and s.d. were only available for the PWI, which was subsequently considered for the meta-analysis. One study (Killian et al., 2016) could not be considered for the meta-analysis since the effects had a variance of zero. In the end, a total of k = 26 effects were included in the analysis.
Effect sizes (ES) according to Cohen were calculated in a first step to evaluate the magnitude of the differences between the QOL of parents of mentally-ill children and the QOL of parents of healthy controls or norm values. For studies reporting effects for QOL-subdomains and for a total QOL-score, only the effects for QOL-subdomains were used. ES from different QOL-subdomains were aggregated to a total QOL-score using the procedure described by Borenstein et al. (2009), which outperformed other common procedures in a large simulation study (Hoyt and Del Re 2015). For aggregating the ES, a correlation of r = 0.5 was assumed, as a conservative and common used value (Del Re and Flückiger, 2016). As a last step, Cohen's d was converted to Hedges’ g to correct for upwards biased ES in studies with small sample sizes (n < 50) (Del Re and Flückiger, 2016). Hedges’ g was interpreted identical to ES as small (0.2), medium (0.5), or large (0.8) (Cohen, 1988). Furthermore, ES ⩾ 0.5 were – based on a recommendation for QOL research (Norman et al., 2003) – considered clinically meaningful.
The ES were examined for possible outliers. An outlier was defined as an ES exceeding three standard deviations from the composite ES (Lipsey and Wilson, 2001). Based on this criteria, only one study was identified as an outlier (Anastasiadou et al., 2016). Given that the outlier effect was in the same direction as the mean effect and since no reasons for the variation were found, the effect was retained.
Separate meta-regressions were used to account for the two comparisons: (1) QOL of parents of mentally-ill children v. QOL of parents of healthy children and (2) QOL of parents of mentally-ill children v. QOL norm values. Random effect models were used for all meta-analyses, given the wide range of different disorders included in this study. In addition, homogeneity analyses were conducted using the Q statistic (Del Re and Flückiger, 2016). Given that the analyses indicated high heterogeneity, the following moderating variables were examined: publication year, QOL-measure, child's gender, age, and disorder. As recommended by Del Re and Flückiger (2016), publication bias was further examined visually by means of a funnel plot. Where possible, the Egger's test (Sterne et al., 2001) was applied to test for publication bias. The test requires a minimum of ten studies per comparison.
The alpha level in all analyses was set to p < 0.01 to reduce the probability of Type I error. All analyses were conducted with the packages MAd (Del Re and Hoyt, 2010), compute.es (Del Re 2010) and metafor (Viechtbauer, 2010) in R (version 3.3.0; R Core Team 2013).
Results of meta-analysis
QOL ES
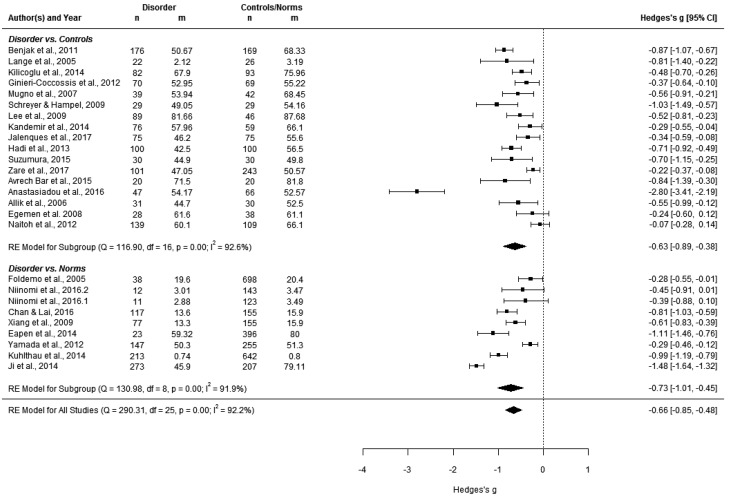
Parents of mentally-ill children reported significantly lower QOL compared with parents of healthy children (g = −0.63) and compared with norm values (g = −0.73; Fig. 2). The effect is larger for the comparison with norm values. Both effects are clinically meaningful (Norman et al., 2003). Heterogeneity between studies was significant in all meta-regressions, but most pronounced for the comparison of parents of mentally-ill children with norm values (Q(8) = 130.98, p < 0.001).
Fig. 2.
Forest plot of comparisons (1) parents of children with a disorder v. norm values and (2) parents of children with a disorder v. parents of healthy children (controls).
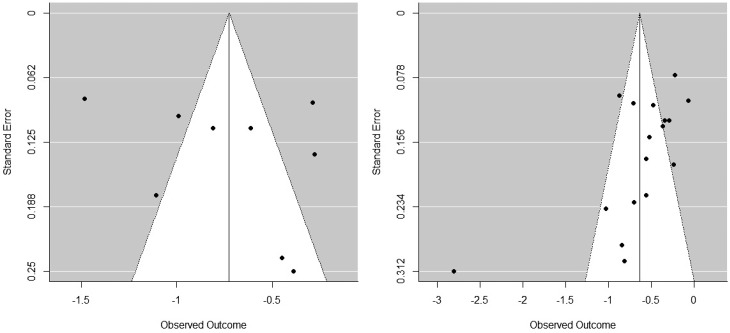
The two funnel plots suggest that publication bias existed (Fig. 3). For the comparison of parents of mentally-ill children with norm values, the funnel plot was symmetrical: smaller studies had a higher likelihood of being published if they yielded either large or small to almost no effects. For the comparison of parents of mentally-ill children with control parents, the funnel plot revealed asymmetrical publication bias: smaller studies had a higher likelihood of being published if they reported small to almost no effects. The Egger's test for the last comparison was applied (requirement: k > 10), and its result was significant (z = −3.39, p < 0.001).
Fig. 3.
Funnel plots of comparisons (1) parents of children with a disorder v. norm values (left) and (2) parents of children with a disorder v. healthy children (right).
Moderator analyses
Relevant moderators were tested to explain heterogeneous effects for the total sample and the two subsamples of comparisons. Neither publication year, publication type nor QOL-measurement were significant moderators.
Of the sample characteristics, child's disorder, and age significantly influenced the effects. Compared with parents of children with ASD, parents of children with the following disorders reported higher QOL than controls and norms: Enuresis nocturna (k = 3, β = 0.682, p = 0.002), pervasive developmental disorders (PDD) (k = 2, β = 0.534, p = 0.036), and schizophrenia (k = 1, β = 0.663, p = 0.049). Only parents of children with a SRD reported significant lower QOL than parents of children with ASD (k = 1, β = −1.857, p = 0.036) compared with controls and norms. These findings are based on few studies only and must be interpreted with caution.
Child's age was a significant moderator for the comparisons between parents of mentally-ill children and control parents. Parents of older mentally-ill children showed lower QOL than parents of younger mentally-ill children compared with control parents (k = 14, β = −0.102, p = 0.036).
Discussion
Confirming our hypothesis, the meta-analysis showed that parents of mentally-ill children are experiencing a compromised QOL relative to the norms and relative to parents of healthy children. This finding is in line with research showing heightened caregiver burden, parenting or psychological distress and rates of mental health problems in parents of mentally-ill children (Steele et al., 2007; van der Voort et al., 2007; Zabala et al., 2009; Theule et al., 2010). The ES were large for the comparison between parents of children with mental disorders and norm values, but lower for the comparison with a control group of parents of healthy children. The ES might have been underestimated in the latter comparison due to publication bias (smaller studies with a control group were more likely to be published if they reported small to almost no effects). However, the smaller ES for the comparison with controls might also be attributable to higher levels of stress and strains among parents of healthy children relative to the general population (e.g., lack of time to follow personal interests). Despite the different ES of the two comparisons, the identified QOL-reduction experienced by parents of children with a mental disorder was clinically relevant in both comparisons. Hence, it is important to address parental needs.
Moderation analyses yielded that parents of older mentally-ill children have a lower QOL than parents of younger mentally-ill children compared with controls. This is in contrast to the findings of the meta-analysis of Theule et al. (2010) that did not identify the child's age as a significant moderator of parenting stress. This discrepancy might not only be due to the different concepts assessed (QOL v. parenting stress), but also due to differences in the scopes of the analysis: Theule et al. focused on ADHD, whereas the present meta-analysis included different mental disorders. Hence, it is possible that age was confounded with the type of condition in the present analysis. Nevertheless, it is also possible that caregivers of older children become more distressed when symptoms of the child's condition persist and further problems develop.
The systematic review revealed several gaps in the here-studied field of research. The majority of both included and excluded studies focused on ADHD or ASD, whereas other mental disorders received less attention. One reason for this predominance might be attributable to the fact that ADHD and ASD emerge early in life (Baxter et al., 2015; Thapar and Cooper, 2016), i.e. at a stage when children are still strongly dependent on their parents. The relative high prevalence of ADHD might have also contributed to the interest in this condition. Furthermore, most included studies looked at the QOL of parents of young children (<10) and boys. Again, this might be explained by the early onset of the predominantly considered mental disorders (e.g., ADHD, ASD) as well as a higher prevalence of such disorders in males (Baxter et al., 2015; Thapar and Cooper, 2016). Additionally, it must be emphasised that research to date mainly included mothers, presumably because they are often more involved in the caregiving process than fathers (e.g. Niinomi et al., 2016). Non-response might have biased the results of some studies. However, the extent of this bias is often difficult to estimate because many publications did not report response/refusal rates for the clinical and/or control group(s). As well, most included studies recruited caregivers of mentally-ill children via (psychiatric) outpatient clinics or other clinical institutions. These samples might differ from parents of mentally-ill children that are not (yet) or no longer treated professionally. Lastly, it must be considered that a significant number of studies was excluded because no comparison was made between the parents of children with mental disorders and parents of healthy children/norms.
Future research should not only focus on ADHD and ASD, but also on other disorders. Furthermore, the QOL of male caregivers should be elaborated, as fathers and mothers have been shown to differ in (some domains of) their QOL (e.g. Allik et al., 2006; Mugno et al., 2007). Using population-based rather than clinical samples might further deepen our understanding in this field. However, it would still be important to verify the clinical diagnosis of the child's condition through a clinical evaluation of a health professional and/or a diagnostic test. The reporting might be improved in subsequent research by providing important details, such as information on refusal/response rates. Whenever possible, QOL of parents of mentally-ill children should be compared with the QOL of parents of healthy children, since they might also experience a slight reduction in their QOL relative to the general population. However, in case that no control group can be assessed, researchers should consider comparisons on the OOL-data of parents of mentally-ill children with norm values, keeping in mind that the effect for this comparison might be slightly overestimated. Lastly, the association between age of the child and QOL of parents should be studied in more detail to clarify the question whether the QOL depends on the age of onset of the child's condition and if it increases with the duration of the disorder.
The limitations of the systematic review include that only articles published in English or German were considered and that all included studies were based on cross-sectional data, which limits causal inferences. With regard to the meta-analysis, heterogeneity was considerably high due to the broad scope of the literature review. Therefore, the ES only have a guiding value. Secondly, the described publication biases, as well as the limited number of studies targeting particular mental disorders, must be considered when interpreting the results.
Despite these limitations, the results of the meta-analysis indicate that parents of mentally-ill children are experiencing a clinically relevant reduction in their QOL relative to the general population and relative to parents of healthy children. This compromised QOL needs to be addressed by health professionals who are in contact with the parents of mentally-ill children (see, for instance, literature from Da Paz and Wallander 2017 who conducted a narrative review on interventions aiming to improve the mental health of parents whose children have ASD). Furthermore, the impact that a child's mental disorder can have on parents should be further examined and elaborated. The results of the systematic review and meta-analysis can be used to plan subsequent studies that aim to fill the important research gaps.
Acknowledgements
We are grateful to all authors who provided additional data we needed to complete the evaluation of papers and the data extraction. Furthermore, we would like to thank Jenny Yi-Chen Lee for the English editing.
Ethical standards
Not applicable.
Availability of data and materials
Data used for the systematic review/meta-analysis will be provided on request.
Footnotes
Financial support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Conflicts of interest
None.
References
- Allik H, Larsson J-O and Smedje H (2006) Health-related quality of life in parents of school-age children with Asperger syndrome or high-functioning autism. Health and Quality of Life Outcomes 4, 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychological Association (2000) Diagnostic and Statistical Manual of Mental Disorders (4th Edition Text Revision), 4th Edn Washington, DC: APA. [Google Scholar]
- American Psychological Association (2013) Diagnostic and Statistical Manual of Mental Disorders, 5th Edn Washington, DC: APA. [Google Scholar]
- Anastasiadou D, Sepulveda AR, Sánchez JC, Parks M, Álvarez T and Graell M (2016) Family functioning and quality of life among families in eating disorders: a comparison with substance-related disorders and healthy controls. European Eating Disorders Review 24, 294–303. [DOI] [PubMed] [Google Scholar]
- Avrech Bar M, Jlole Majadla S and Bart O (2015) Managing everyday occupations as a predictor of health and life satisfaction among mothers of children with ADHD. Journal of Attention Disorders 22, 1008–1016. [DOI] [PubMed] [Google Scholar]
- Baxter AJ, Brugha TS, Erskine HE, Scheurer RW, Vos T and Scott JG (2015) The epidemiology and global burden of autism spectrum disorders. Psychological Medicine 45, 601–613. [DOI] [PubMed] [Google Scholar]
- Benjak T, Mavrinac G V, Šimetin IP and Kolarić B (2011) A comparative study on self-perceived health and quality of life of parents of children with autism spectrum disorders and parents of non disabled children in Croatia. Developmental Medicine and Child Neurology 53, 131–144.21039441 [Google Scholar]
- Borenstein M, Hedges LV, Higgins JPT and Rothstein HR (2009) Introduction to Meta-Analysis. Chichester, UK: Wiley, Ltd. [Google Scholar]
- Chan Sc (2011) Global perspective of burden of family caregivers for persons with schizophrenia. Archives of Psychiatric Nursing 25, 339–349. [DOI] [PubMed] [Google Scholar]
- Chan J and Lai K (2016) Psychological adjustment of siblings of children with autism spectrum disorder in Hong Kong. East Asian Archives of Psychiatry 26, 141–147. [PubMed] [Google Scholar]
- Cohen J (1988) Statistical Power Analysis for the Behavioral Sciences. Hillsdale, NJ. [Google Scholar]
- Corcoran J, Berry A and Hill S (2015) The lived experience of US parents of children with autism spectrum disorders: a systematic review and meta-synthesis. Journal of Intellectual Disabilities 19, 356–366. [DOI] [PubMed] [Google Scholar]
- Costello EJ, Egger H and Angold A (2005) 10-year research update review: the epidemiology of child and adolescent psychiatric disorders: I. Methods and public health burden. Journal of the American Academy of Child and Adolescent Psychiatry 44, 972–986. [DOI] [PubMed] [Google Scholar]
- Da Paz NS and Wallander JL (2017) Interventions that target improvements in mental health for parents of children with autism spectrum disorders: a narrative review. Clinical Psychology Review 51, 1–14. [DOI] [PubMed] [Google Scholar]
- De Girolamo G, Dagani J, Purcell R, Cocchi A and McGorry PD (2012) Age of onset of mental disorders and use of mental health services: needs, opportunities and obstacles. Epidemiology and Psychiatric Sciences 21, 47–57. [DOI] [PubMed] [Google Scholar]
- Del Re AC (2010) Compute.es: Compute Effect Sizes. Madison, WI. [Google Scholar]
- Del Re AC and Flückiger C (2016) Meta-Analysis. In APA Handbook of Clinical Psychology: Vol. 2. Theory and Research, pp. 479–491.
- Del Re AC and Hoyt WT (2010) MAD: Meta-Analysis with Mean Differences. Madison, WI. [Google Scholar]
- Eapen V, Črnčec R, Walter A and Tay KP (2014) Conceptualisation and development of a quality of life measure for parents of children with autism spectrum disorder. Autism Research and Treatment 2014, 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egemen A, Akil I, Canda E, Ozyurt BC and Eser E (2008) An evaluation of quality of life of mothers of children with enuresis nocturna. Pediatric Nephrology 23, 93–98. [DOI] [PubMed] [Google Scholar]
- Foldemo A, Gullberg M, Ek AC and Bogren L (2005) Quality of life and burden in parents of outpatients with schizophrenia. Social Psychiatry and Psychiatric Epidemiology 40, 133–138. [DOI] [PubMed] [Google Scholar]
- Ginieri-Coccossis M, Rotsika V, Skevington S, Papaevangelou S, Malliori M, Tomaras V and Kokkevi A (2012) Quality of life in newly diagnosed children with specific learning disabilities (SpLD) and differences from typically developing children: a study of child and parent reports. Child: Care, Health and Development 39, 581–591. [DOI] [PubMed] [Google Scholar]
- Gore FM, Bloem PJN, Patton GC, Ferguson J, Joseph V, Coffey C, Sawyer SM and Mathers CD (2011) Global burden of disease in young people aged 10-24 years: a systematic analysis. The Lancet 377, 2093–2102. [DOI] [PubMed] [Google Scholar]
- Hadi N, Saghebi A, Ghanizadeh A and Montazeri A (2013) Assessment of health-related quality of life in mothers of children with attention-deficit hyperactivity disorder (ADHD), Shiraz, 2008-2009. Shiraz E Medical 14, 91–101. [Google Scholar]
- Hoyt WT and Del Re AC (2015) Comparison of methods for aggregating dependent effect sizes in meta-analysis, Manuscript in preparation.
- Jalenques I, Auclair C, Morand D, Legrand G, Marcheix M, Ramanoel C, Hartmann A, The Syndrome de Gilles de la Tourette Study Group, Derost P (2017) Health-related quality of life, anxiety and depression in parents of adolescents with Gilles de la Tourette syndrome: a controlled study. European Child and Adolescent Psychiatry 26, 603–617. [DOI] [PubMed] [Google Scholar]
- Ji B, Zhao I, Turner C, Sun M, Yi R and Tang S (2014) Predictors of health-related quality of life in Chinese caregivers of children with autism spectrum disorders: a cross-sectional study. Archives of Psychiatric Nursing 28, 327–332. [DOI] [PubMed] [Google Scholar]
- Kandemir H, Kiliç BG, Ekinci S and Yüce M (2014) An evaluation of the quality of life of children with ADHD and their families. Anadolu Psikiyatri Dergisi 15, 265–271. [Google Scholar]
- Kessler RC, Amminger GP, Aguilar-Gaxiola S, Alonso J, Lee S and Ustün TB (2007) Age of onset of mental disorders: a review of recent literature. Current Opinion in Psychiatry 20, 359–364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kilicoglu AG, Mutlu C, Bahali MK, Adaletli H, Gunes H, Metin Duman H, Toz HI and Uneri OS (2014) Impact of enuresis nocturna on health-related quality of life in children and their mothers. Journal of Pediatric Urology 10, 1261–1266. [DOI] [PubMed] [Google Scholar]
- Killian JT, Lane JB, Lee HS, Pelham JH, Skinner SA, Kaufmann WE, Glaze DG, Neul JL and Percy AK (2016) Caretaker quality of life in Rett Syndrome: disorder features and psychological predictors. Pediatric Neurology 58, 67–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klages D, Usher K and Jackson D (2016) ‘Canaries in the mine’. Parents of adult children with schizophrenia: an integrative review of the literature. International Journal of Mental Health Nursing 26, 5–19. [DOI] [PubMed] [Google Scholar]
- Kuhlthau K, Payakachat N, Delahaye J, Hurson J, Pyne JM, Kovacs E and Tilford JM (2014) Quality of life for parents of children with autism spectrum disorders. Research in Autism Spectrum Disorders 8, 1339–1350. [Google Scholar]
- Lange G, Sheerin D, Carr A, Dooley B, Barton V, Marshall D, Mulligan A, Lawlor M, Belton M and Doyle M (2005) Family factors associated with attention deficit hyperactivity disorder and emotional disorders in children. Journal of Family Therapy 27, 76–96. [Google Scholar]
- Lee GK, Lopata C, Volker MA, Thomeer ML, Nida RE, Toomey JA, Chow SY and Smerbeck AM (2009) Health-related quality of life of parents of children with high-functioning autism spectrum disorders. Focus on Autism and Other Developmental Disabilities 24, 227–239. [Google Scholar]
- Lipsey MW and Wilson DB (2001) Practical Meta-Analysis. Thousand Oaks, CA: Sage Publications. [Google Scholar]
- Logan DE and King Ca (2001) Parental facilitation of adolescent mental health services utilization: a conceptual and empirical review. Clinical Psychology: Science and Practice 8, 319–333. [Google Scholar]
- Mugno D, Ruta L, D'Arrigo VG and Mazzone L (2007) Impairment of quality of life in parents of children and adolescents with pervasive developmental disorder. Health and Quality of Life Outcomes 5, 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naitoh Y, Kawauchi A, Soh J, Kamoi K and Miki T (2012) Health related quality of life for monosymptomatic enuretic children and their mothers. Journal of Urology 188, 1910–1914. [DOI] [PubMed] [Google Scholar]
- Niinomi K, Asano M, Kadoma A, Yoshida K, Ohashi Y, Furuzawa A, Yamamoto M, Yamakita N and Mori A (2016) Developing the “Skippu-Mama” program for mothers of children with autism spectrum disorder. Nursing & Health Sciences 18, 283–291. [DOI] [PubMed] [Google Scholar]
- Norman GR, Sloan JA and Wyrwich KW (2003) Interpretation of changes in health-related quality of life: the remarkable universality of half a standard deviation. Medical Care 41, 582–592. [DOI] [PubMed] [Google Scholar]
- Patel V, Flisher AJ, Hetrick S and McGorry P (2007) Mental health of young people: a global public-health challenge. Lancet 369, 1302–1313. [DOI] [PubMed] [Google Scholar]
- R Core Team (2013) R: a Language and Environment for Statistical Computing. 2013. Vienna, Austria: R Foundation for Statistical Computing. [Google Scholar]
- Sayal K (2006) Annotation: pathways to care for children with mental health problems. Journal of Child Psychology and Psychiatry and Allied Disciplines 47, 649–659. [DOI] [PubMed] [Google Scholar]
- Schreyer I and Hampel P (2009) ADHS bei Jungen im Kindesalter - Lebensqualität und Erziehungsverhalten. Zeitschrift fur Kinder- und Jugendpsychiatrie und Psychotherapie 37, 69–75. [DOI] [PubMed] [Google Scholar]
- Steele L, Dewa C and Lee K (2007) Socioeconomic status and self-reported barriers to mental health service use. Canadian Journal of Psychiatry. Revue canadienne de psychiatrie 52, 201–206. [DOI] [PubMed] [Google Scholar]
- Sterne J, Egger M and Smith G (2001) Investigating and dealing with publication and other biases in meta-analysis. BMJ 323, 101–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suzumura S (2015) Quality of life in mothers of preschoolers with high-functioning pervasive developmental disorders. Pediatrics International 57, 149–154. [DOI] [PubMed] [Google Scholar]
- Thapar A and Cooper M (2016) Attention deficit hyperactivity disorder. The Lancet 387, 1240–1250. [DOI] [PubMed] [Google Scholar]
- Theule J, Wiener J, Tannock R and Jenkins JMJ (2010) Parenting stress in families of children with ADHD: a meta-analysis. Journal of Emotional and Behavioral Disorders 21, 3–17. [Google Scholar]
- van der Voort TY, Goossens PJ and van der Bijl JJ (2007) Burden, coping and needs for support of caregivers for patients with a bipolar disorder: a systematic review. Journal of Psychiatric and Mental Health Nursing 14, 679–687. [DOI] [PubMed] [Google Scholar]
- Vasilopoulou E and Nisbet J (2016) The quality of life of parents of children with autism spectrum disorder: a systematic review. Research in Autism Spectrum Disorders 23, 36–49. [Google Scholar]
- Viechtbauer W (2010) Conducting meta-analyses in R with the metafor package. Journal of Statistical Software 36, 1–48. [Google Scholar]
- WHOQOL Group (1995) The World Health Organization Quality of Life assessment (WHOQOL): position paper from the World Health Organization. Social Science & Medicine 41, 1403–1409. [DOI] [PubMed] [Google Scholar]
- World Health Organization (1992) The ICD-10 classification of mental and behavioural disorders. International Classification 10, 1–267. [Google Scholar]
- Xiang Y-T, Luk ESL and Lai KYC (2009) Quality of life in parents of children with attention-deficit-hyperactivity disorder in Hong Kong. The Australian and New Zealand Journal of Psychiatry 43, 731–738. [DOI] [PubMed] [Google Scholar]
- Yamada A, Kato M, Suzuki M, Suzuki M, Watanabe N, Akechi T, Furukawa TA, Wingate M, Mulvihill B, Kirby R, Pettygrove S, Cunniff C, Meaney F, Schulz E, Miller L, Robinson C, Quintana G, Konstantareas M, Homatidis S, Konstantareas MM, Homatidis S, Moes D, Koegel RL, Schreibman L, Loos LM, Dumas J, Wolf LC, Fisman SN, Culligan A, Freeman NL, Perry A, Factor DC, Holroyd J, Wolf LC, Noh S, Fisman SN, Speechley M, Hastings RP, Hastings RP, Kovshoff H, Ward NJ, Espinosa FD, Brown T, Remington B, Bristol MM, Gallagher JJ, Schopler E, Olsson MB, Hwang CP, Gray DE, Yamada A, Suzuki M, Kato M, Suzuki M, Tanaka S, Shindo T, Taketani K, Akechi T, Furukawa TA, Mugno D, Ruta L, D'Arrigo VG, Mazzone L, Allik H, Larsson JO, Smedje H, Benjak T, Mavrinac GV, Simetin IP, Koegel RL, Schreibman L, Loos LM, Dirlich-Wilhelm H, Dunlap G, Robbins FR, Plienis AJ, Doo S, Wing YK, Montes G, Halterman JS, Weiss SJ, Siman-Tov A, Kaniel S, Dunn ME, Burbine T, Bowers CA, Tantleff-Dunn S, Gill MJ, Harris SL, Factor DC, Perry A, Freeman N, Pakenham KI, Samios C, Sofronoff K, Ekas NV, Lickenbrock DM, Whitman TL, Weiss MJ, Cappe E, Wolff M, Bobet R (2012) Quality of life of parents raising children with pervasive developmental disorders. BMC Psychiatry 12, 119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zabala MJ, Macdonald P and Treasure J (2009) Appraisal of caregiving burden, expressed emotion and psychological distress in families of people with eating disorders: a systematic review. European Eating Disorders Review 17, 338–349. [DOI] [PubMed] [Google Scholar]
- Zare R, Jafari P and Ghanizadeh A (2017) Do Adult Attention Deficit Hyperactivity Disorder Quality-Of-Life (AAQoL) scale and the SF-36 scale measure the same construct of health-related quality of life? ADHD Attention Deficit and Hyperactivity Disorders 9, 39–45. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data used for the systematic review/meta-analysis will be provided on request.