Abstract
Background
While many different types of patient education are widely used, the effect of individual patient education for low‐back pain (LBP) has not yet been systematically reviewed.
Objectives
To determine whether individual patient education is effective in the treatment of non‐specific low‐back pain and which type is most effective.
Search methods
A computerized literature search of MEDLINE (1966 to July 2006), EMBASE (1988 to July 2006), CINAHL (1982 to July 2006), PsycINFO (1984 to July 2006), and the Cochrane Central Register of Controlled Trials (The Cochrane Library 2006, Issue 2) was performed. References cited in the identified articles were screened.
Selection criteria
Studies were selected if the design was a randomised controlled trial; if patients experienced LBP; if the type of intervention concerned individual patient education, and if the publication was written in English, German, or Dutch.
Data collection and analysis
The methodological quality was independently assessed by two review authors. Articles that met at least 50% of the quality criteria were considered high quality. Main outcome measures were pain intensity, global measure of improvement, back pain‐specific functional status, return‐to‐work, and generic functional status. Analysis comprised a qualitative analysis. Evidence was classified as strong, moderate, limited, conflicting or no evidence.
Main results
Of the 24 studies included in this review, 14 (58%) were of high quality. Individual patient education was compared with no intervention in 12 studies; with non‐educational interventions in 11 studies; and with other individual educational interventions in eight studies. Results showed that for patients with subacute LBP, there is strong evidence that an individual 2.5 hour oral educational session is more effective on short‐term and long‐term return‐to‐work than no intervention. Educational interventions that were less intensive were not more effective than no intervention. Furthermore, there is strong evidence that individual education for patients with (sub)acute LBP is as effective as non‐educational interventions on long‐term pain and global improvement and that for chronic patients, individual education is less effective for back pain‐specific function when compared to more intensive interventions. Comparison of different types of individual education did not show significant differences.
Authors' conclusions
For patients with acute or subacute LBP, intensive patient education seems to be effective. For patients with chronic LBP, the effectiveness of individual education is still unclear.
Plain language summary
Individual Patient Education for low‐back pain
Low‐back pain is a very common condition, particularly in developed countries. It can cause a great deal of pain and lost activity.
Health professionals use patient education to help people learn about low‐back pain and what to do about it, including:
‐ Staying active and returning to normal activities as soon as possible ‐ Avoiding worry ‐ Coping with having a sore back ‐ Ways to avoid strain and avoid future back injuries.
Patient education can mean a discussion with a health professional, a special class, written information such as a booklet to take home, or other formats such as a video.
This review found 24 trials testing different types of patient education for people with low‐back pain. The outcomes measured included pain, function and return‐to‐work.
People with low‐back pain who received an in‐person patient education session lasting at least two hours in addition to their usual care had better outcomes than people who only received usual care. Shorter education sessions, or providing written information by itself without an in‐person education session, did not seem to be effective.
People with chronic (long‐term) low‐back pain were less likely to benefit from patient education than people with acute (short‐term) pain.
Patient education was no more effective than other interventions such as cognitive behavioural group therapy, work‐site visits, x‐rays, acupuncture, chiropractic, physiotherapy, massage, manual therapy, heat‐wrap therapy, interferential therapy, spinal stabilisation, yoga, or Swedish back school. One study found that patient education was more effective than exercises alone for some measures of function.
Studies that compared different types of patient education did not find clear results on which type was most effective. Some studies found that written information was just as effective as in‐person education.
There appeared to be no harmful effects of patient education. Although there were 24 studies included in the review, most treatments were only tested by one or two studies. More research is needed to confirm these results, and to find out which types of patient education are the most effective.
Background
Low‐back pain (LBP) is a common disorder and a major health problem in industrialized countries. It is associated with substantial health care utilization and absenteeism from work (Maniadakis 2000; Van Tulder 1995). However, the natural course of LBP is favourable; LBP is considered a benign and self‐limiting 'disease' (Waddell 1987). Treatment options for LBP in primary care are diverse. Patient education has a long history as an integral part of clinical practice and is increasingly seen as an important intervention (Burton 1996; Waddell 1987).
Patient education has been defined as 'a systematic experience in which a combination of methods is generally used, such as the provision of information and advice and behaviour modification techniques, which influence the way the patient experiences his illness and/or his knowledge and health behaviour, aimed at improving or maintaining or learning to cope with a condition, usually a chronic one' (Van den Borne 1998).
Providing information is the central focus in educational activities. The information given by a health‐care provider is of utmost importance since it can prevent unnecessary use of health care and enhances self‐care and the use of active coping strategies (Burton 1996; Nordin 1995). Cherkin stated that 'the aim of patient education with regard to non‐specific low‐back pain is to improve patients' understanding of their back problems and what they should do about them; to reduce unwarranted concern about serious outcomes; and to empower patients to take actions that should expedite a return to normal activities, reduce the risk of subsequent back problems, and minimize dependency on health care providers' (Cherkin 1996).
So, patient education aims to change behaviour, which is difficult, requires time, considerable effort and motivation. Ambivalence about behaviour change is a common problem in health care consultations. There are two dominant models of health behaviour change: the theory of planned behaviour (Ajzen 1991) and the trans‐theoretical or stages of change model (Prochaska 1984). The theory of planned behaviour helps one to understand how the behaviour of people can be changed. According to this theory, the person's intentions are the deciding factors of whether the behaviour is performed. There are three determinants of behavioural intention: attitude, subjective norm and perceived control (Ajzen 1991).
The stages of change model is based on the individual's self‐reported motivation to change a specific behaviour. This model has five stages: (i) pre‐contemplation, with no perceived need or intention to change; (ii) contemplation, with awareness of a problem but no commitment to take action; (iii) preparation for action, which covers intention and initial behaviour change; (iv) action ‐changing behaviour and (v) maintenance ‐ maintaining the behaviour change.
Many different types of patient education are commonly used in clinical practice. Patient education may include oral or written information, may be provided as a separate intervention or as part of an intervention program, and it may be provided to an individual patient or to groups of patients.
Objectives
To determine whether individual patient education is effective for pain, global improvement, functioning and return‐to‐work in the treatment of non‐specific low‐back pain, and to determine which type of education is most effective.
The following comparisons were investigated:
individual patient education versus no intervention
individual patient education versus non‐educational interventions
individual patient education versus another type of individual patient education.
Methods
Criteria for considering studies for this review
Types of studies
Only randomised controlled trials (RCTs) were included.
Types of participants
The study population included adult subjects (16 years of age or older) suffering from acute, subacute or chronic non‐specific LBP. Low‐back pain was defined as pain localized below the lower ribs and above the inferior gluteal folds. Trials with participants suffering from LBP with a specific cause (e.g. infection, neoplasm, metastasis, osteoporosis, rheumatoid arthritis, fractures or lumbosacral radicular syndrome) were excluded.
Types of interventions
Individual patient education was defined as 'a systematic experience, in a one‐to one situation, that consists of one or more methods, such as the provision of information and advice and behaviour modification techniques, which influence the way the patient experiences his illness and/or his knowledge and health behaviour, aimed at improving or maintaining or learning to cope with a condition'.
Patient education for patients with low‐back pain was operationalised as any advise or information (verbal, written or audiovisual) given by a health care professional in order to improve patients' understanding of their back problems and what they should do about them. Studies on advise to stay active were included, studies on instructions on how to perform exercises were not included. Studies that evaluated group education were also excluded. Studies that compared an educational intervention as part of an intervention program with another non‐educational intervention were also excluded, as these studies lack a contrast for patient education. For example, trials on multidisciplinary treatment or a back school that included individual patient education compared to manual therapy were excluded. However, trials in which individual patient education as part of an intervention program were compared with the same intervention program without the patient education component were included.
Types of outcome measures
Trials using one or more of the following outcome measures were included:
Pain intensity (e.g. visual analogue scale (VAS); symptom bothersomeness scale (Patrick 1995))
Global measure (e.g. overall improvement assessed by the patient, proportion of patients recovered)
Back pain specific functional status (e.g. Roland Disability Questionnaire (Roland 1983), Oswestry Disability Index (Fairbank 2000), number of days in bed because of LBP)
Return‐to‐work (e.g. return to work, number of days off work)
Generic functional status (e.g. SF‐36 (Ware 1992), EuroQol (Van Agt 1994), Sickness Impact Profile (Bergner 1981); activities of daily living; self‐reported reduced activity)
Outcomes were separated into short‐term (less than six months after randomisation) and long‐term outcomes (six months or more).
Search methods for identification of studies
We searched these databases: MEDLINE (from 1966 to July 2006), EMBASE (1988 to July 2006), CINAHL (from 1982 to July 2006) and PsycINFO (from 1984 to July 2006) and the Cochrane Central Register of Controlled Trials (CENTRAL, The Cochrane Library 2006, Issue 2) using the search strategy recommended by the Cochrane Back Review Group (CBRG). References of relevant randomised controlled trials (RCTs) were checked to identify additional studies. Thirteen additional keywords used to identify the patient education interventions were: education, patient centred care, information booklet, book, video, pamphlet, leaflet, poster, psycho‐education, education and information. The search strategies are presented in Appendix 1; Appendix 2; Appendix 3; Appendix 4. A language restriction was used, excluding studies not published in English, Dutch or German, because the authors were not able to read and understand any other languages. Studies published in other languages might be included in a future update of this review.
Data collection and analysis
Study selection
One review author generated the electronic search strategies in MEDLINE, EMBASE, PsycLIT, CINAHL and CENTRAL. Two review authors then independently reviewed the information to identify trials that could potentially meet the inclusion criteria and selected trials based on title, abstract and keywords. Articles for which disagreement existed and articles for which title, abstract and keywords provided insufficient information for a decision were retrieved in full. Two review authors independently applied the selection criteria to the studies. Consensus was used to solve disagreements concerning the final inclusion of RCTs and a third review author was consulted if disagreements persisted. One of the review authors (Petra Jellema) is first author of one of the included trials. She was not involved in the decisions regarding inclusion of her trial.
Methodological quality assessment
The methodological quality of the RCTs was independently assessed by two review authors (PJ and AE). The quality assessment of Jellema 2005 was done by MvT and AE. Petra Jellema was not involved in the quality assessment of her trial. Quality assessment was not blinded with regard to the authors, institution and journal, because the review authors were familiar with the literature. A consensus method was used to solve disagreements and a third review author (MvT) was consulted if disagreement persisted. A pilot test was conducted using a trial on group patient education for back pain that is not included in the present systematic review (Bendix 1998). The criteria recommended by the CBRG were used in this review (Table 1, van Tulder 2003).
1. Criteria for the Risk of Bias Assessment.
| Criteria for a judgment of yes for the sources of risk of bias |
|
Was the method of randomisation adequate? A random (unpredictable) assignment sequence. Examples of adequate methods are computer‐generated random numbers table and use of sealed opaque envelopes. Methods of allocation using date of birth, date of admission, hospital numbers, or alternation should not be regarded as appropriate.
Was the treatment allocation concealed? Assignment generated by an independent person not responsible for determining the eligibility of the patients. This person has no information about the persons included in the trial and has no influence on the assignment sequence or on the decision about eligibility of the patient. Was the patient blinded to the intervention? The review author determines if the treatments were considered equally credible and acceptable to patients in order to score a "yes." Was the care provider blinded to the intervention? The review author determines if enough information about the blinding is given in order to score a "yes." Was the outcome assessor blinded to the intervention? The review author determines if enough information about the blinding is given in order to score a "yes." Was the drop‐out rate described and acceptable during the intervention? The number of participants who were included in the study but did not complete the intervention or were not included in the analysis must be described and reasons given. If the percentage of withdrawals and drop‐outs does not exceed 20% and does not lead to substantial bias a "yes" is scored. Was the drop‐out rate described and acceptable during the follow‐up period? The number of participants who were included in the study but did not complete the observation period or were not included in the analysis must be described and reasons given. If the percentage of withdrawals and drop‐outs does not exceed 20% for immediate and short‐term follow‐ups, 30% for intermediate and long‐term follow‐ups and does not lead to substantial bias a "yes" is scored. Did the analysis include an intention‐to‐treat analysis? All randomized patients are reported/analyzed in the group to which they were allocated by randomization for the most important moments of effect measurement (minus missing values), irrespective of noncompliance and co‐interventions. Were the groups similar at baseline regarding the most important prognostic indicators? In order to receive a "yes," groups have to be similar at baseline regarding demographic factors, duration and severity of complaints, percentage of patients with neurological symptoms, and value of main outcome measure(s). Were co‐interventions avoided or similar? Co‐interventions should either be avoided in the trial design or be similar between the index and control groups. Was the compliance acceptable in all groups? The review author determines if the compliance to the interventions is acceptable, based on the reported intensity, duration, number and frequency of sessions for both the index intervention and control intervention(s). |
As it is difficult to blind patients for patient education, we redefined the criterion regarding the blinding of patients. This item was scored positive if the credibility of the treatments were considered equally credible and acceptable to patients (Turk 1993). We also redefined the criterion about drop‐outs and withdrawals by dividing this into two criteria, one about drop‐outs during the intervention period, and the other about withdrawals during follow‐up. The timing of outcome assessment was not used as a criterion, because all trials scored positive on this item.
Each criterion was scored as "positive", "negative" or "unclear". A total score was computed by counting the number of positive scores, and high quality was defined as fulfilling six or more (more than 50%) of the internal validity criteria (range 0 to 11). We contacted the authors for additional information on methodological aspects of their studies. The additional information was weighted in a consensus meeting.
A sensitivity analysis was conducted in which the effect of variations in the cut‐off point distinguishing studies of high and low methodological quality was examined.
Clinical relevance
The clinical relevance of the RCTs was also independently assessed by the two review authors. Clinical relevance was scored using the five questions recommended by the Cochrane Back Review Group (Table 2).
2. Operationalization of clinical relevance criteria & internal validity criteria.
| Clinical Relevance |
| 1. Sufficient clinical information on patients: age, sex, duration of the back pain period and the proportion of patients with sciatica 2. Sufficient clinical information on the intervention: type of patient education, content of patient education, when exercises are involved information about the exercises themselves, frequency, intensity and availability 3 Use of (at least one) clinically relevant outcome measure: pain intensity, back specific functional status (e.g. Roland‐Morris Disability Questionnaire, Quebec LBP rating scale), generic functional status (e.g. SF‐36) and return‐to‐work or days absent from work.(Inclusion criterion, so positively scored for all studies in this review) 4. The effect size was considered relevant when 1) a group difference of more than 10 mm on a VAS scale for pain (100 mm) and/or 2) a group difference of more than 2 points on the Roland Disability Scale or and/or 3) a group difference of more 10% on any of the other primary outcomes was found. 5. Are treatment benefits worth the potential harms? (positively scored for all studies based on the assumption that it is not very likely that patient information will cause any harm) |
The effect size was considered relevant when at least one of these criteria were met: 1) there was a group difference of more than 10 mm on a VAS scale for pain (100 mm); 2) there was a group difference of more than two points on the Roland Disability Scale; or 3) there was a group difference of more 10% on any of the other primary outcomes.
Data extraction
Data extraction was carried out by the same two review authors who performed the quality assessment, using a standardized data extraction sheet. Petra Jellema was not involved in the data extraction of her trial; this was done by MvT and AE. Again, the studies were not blinded for authors, institutions or journals.
The following data were extracted from the studies:
Characteristics of study population: number of participants, gender, age and setting. The diagnosis of the patients was noted and whether patients with sciatica were included. A distinction was made between acute/sub‐acute LBP (duration of symptoms less than 12 weeks) and chronic LBP (duration of symptoms 12 weeks or more).
Characteristics of interventions: the type, duration and frequency of the patient education and control interventions.
Characteristics of outcomes: the outcome measures, instruments, and scores (e.g. mean, median, confidence interval, and standard deviation).
Data analysis All analyses were conducted separately for 1) acute or sub‐acute low‐back pain versus chronic low‐back pain and 2) for short‐term (less than six moths after randomisation) versus long‐term outcomes (six months or more). Data on outcomes (mean and standard deviation (SD) or confidence interval (CI) or proportion improved) are presented in the Characteristics of included studies table. Clinical homogeneity was evaluated by exploring the differences between the RCTs with regard to study population, types of interventions, and types of outcomes and measurement instruments. Several trials did not provide sufficient data for inclusion in a meta‐analysis, and there was a wide variation in types of patient education. Therefore, we decided not to perform a meta‐analysis but to summarize the results using a rating system that consisted of five levels of scientific evidence (van Tulder 2003).
Strong evidence ‐ consistent findings among multiple high quality RCTs.
Moderate evidence ‐ consistent findings among multiple low quality RCTs and/or one high quality RCT
Limited evidence ‐ one low quality RCT.
Conflicting evidence ‐ inconsistent findings among multiple trials.
No evidence from trials ‐ No RCTs
Findings were judged as 'consistent' when 75% or more of the RCTs reported similar results.
The educational intervention was considered effective when the difference between this intervention and the reference treatment was statistically and clinically significant on at least one of the primary outcome measures and in favour of the educational intervention.
Results
Description of studies
Literature search and study selection
The computer‐assisted literature search produced a yield of 587 references in PubMed, 466 in EMBASE 128 in CINAHL 83 in PsycINFO and 247 in CENTRAL. Further assessment of the articles and application of the in‐ and exclusion criteria resulted in 24 included studies (Burton 1999; Cherkin 1996; Cherkin 1998; Cherkin 2001; Deyo 1987; Frost 2004; Goldby 2006; Hagen 2003; Hazard 2000; Hurley 2001; Hurri 1989; Indahl 1995; Jackson 1994; Jellema 2005; Karjalainen 2004; Linton 2000; Little 2001; Roberts 2002; Roland 1989; Mayer 2005; Moseley 2004; Sherman 2005; Storheim 2003; Wand 2004).
Data on sample size, age and gender, type and duration of symptoms, and setting are summarized in the Characteristics of included studies table. Fourteen studies included patients with acute or sub‐acute low‐back pain (Burton 1999; Cherkin 1998; Deyo 1987; Hagen 2003; Hazard 2000; Hurley 2001; Indahl 1995; Jellema 2005; Karjalainen 2004; Linton 2000; Mayer 2005; Roberts 2002; Storheim 2003; Wand 2004); four included patients with chronic low‐back pain (Goldby 2006; Hurri 1989; Moseley 2004; Sherman 2005) and six a mixed population of patients with acute, sub‐acute or chronic low‐back pain (Cherkin 1996; Cherkin 2001; Frost 2004; Jackson 1994; Little 2001; Roland 1989).
Eleven studies compared individual patient education with no intervention (Cherkin 1996; Hagen 2003; Hazard 2000; Indahl 1995; Jackson 1994; Jellema 2005; Karjalainen 2004; Little 2001; Roberts 2002; Roland 1989; Storheim 2003); eleven studies compared individual patient education with other non‐educational interventions (Cherkin 1998; Cherkin 2001; Deyo 1987; Frost 2004; Goldby 2006; Hurley 2001; Hurri 1989; Linton 2000; Karjalainen 2004; Mayer 2005; Storheim 2003); and eight studies compared individual patient education with other educational interventions (Burton 1999; Cherkin 1996; Jackson 1994; Linton 2000; Little 2001; Moseley 2004; Sherman 2005; Wand 2004). As some studies included more than one comparison, the total is more than 24.
In seventeen studies, written educational materials were used (Burton 1999; Cherkin 1996; Cherkin 1998; Cherkin 2001; Frost 2004; Goldby 2006; Hazard 2000; Hurley 2001; Hurri 1989; Jackson 1994; Karjalainen 2004; Linton 2000; Little 2001; Mayer 2005; Roberts 2002; Roland 1989; Sherman 2005; ; ). Three studies used pamphlets containing biopsychosocial information (Hazard 2000; Karjalainen 2004; Linton 2000). Linton 2000 used a pamphlet entitled 'Back pain ‐ don't suffer needlessly', that was developed in Symonds 1995. Hazard 2000 developed a pamphlet 'Good news about back pain' that was based on 1) the pamphlet 'Back pain ‐ don't suffer needlessly' 2) a booklet by Cherkin 1996 called 'Back in Action', and 3) a booklet developed by the Agency for Health Care Policy and Research called 'Understanding Acute Low Back Problems' (AHCPR 1994). Karjalainen used the Finnish leaflet 'Selkäkipuisen Käsikirja' (Malmivaara 1996).
Twelve trials made use of a variety of booklets: 'Back Book (Back Book 1997)' (Burton 1999; Hurley 2001), 'Back Book (1989)' (Roland 1989) ;'Back in Action' (Cherkin 1996; Cherkin 1998; Cherkin 2001; Goldby 2006); 'Fighting pain: Helping yourself fight neck and back pain' (Jackson 1994); 'Back Home' (Little 2001; Roberts 2002); 'Handy Hints' (Burton 1999), 'Acute low back pain problems in adults, patient guide' (Mayer 2005); 'The back guide helpbook (Sherman 2005). One study (Cherkin 2001) included a book and videotapes. Fourteen studies used oral individual education (Cherkin 1996; Deyo 1987; Frost 2004; Hagen 2003; Hurley 2001; Indahl 1995; Jellema 2005; Karjalainen 2004; Little 2001; Mayer 2005; Moseley 2004; Roberts 2002; Storheim 2003; Wand 2004).
Risk of bias in included studies
Using a cut‐off point of six out of 11 criteria, 14 of the 24 studies (58%) were of high quality (Figure 1 ‐ Burton 1999; Cherkin 1996; Cherkin 1998; Cherkin 2001; Deyo 1987; Frost 2004; Goldby 2006; Hagen 2003; Hazard 2000; Indahl 1995; Jellema 2005; Karjalainen 2004; Linton 2000; Sherman 2005).
1.
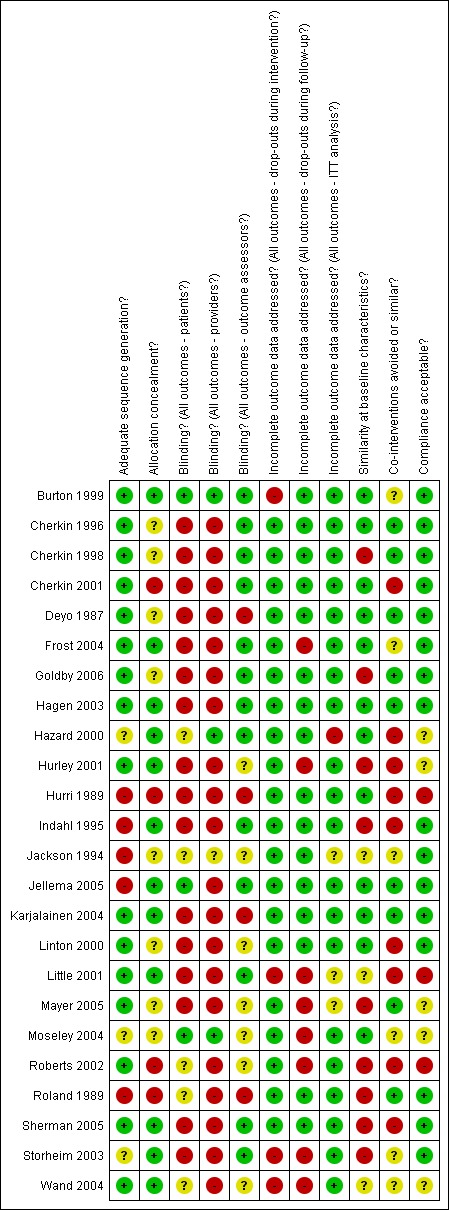
Summary of risks of bias
The most common methodological shortcomings were: 1) care providers not blinded (88%); 2) patients not blinded (88%); 3) co‐interventions not equal (63%). Comparison of the scores by the review authors for each study demonstrated an author concurrence rate of 84%. The disagreement in 16% of the scores could be attributed to subtle differences in interpretation of the criteria. Random errors in reading of the articles and ambiguities in the presentation of information in the articles also played a role. All disagreements were resolved in a consensus meeting.
Clinical relevance of included studies
The scores for clinical relevance are presented in Table 3, Table 4 and Table 5. All studies scored positive on 'at least one clinically relevant outcome measure', because this was one of the inclusion criteria. Also, all studies scored positive on 'are treatment benefits worth the potential harms', which seems obvious because patient education is not expected to be associated with any harm. In 18 studies (75%), the effect size was considered to be clinically relevant, in 17 studies (71%) the intervention was described in sufficient detail (e.g. content, frequency, duration, intensity, availability) for clinical use, and in 14 studies (58%) all clinical relevant patient details were described (e.g. sex, age, length of pain period and the proportion of patients with sciatica).
3. Clinical relevance assessment of the trials I.
| Characteristics | Burton 1999 | Cherkin 2001 | Cherkin 1998 | Cherkin 1996 | Deyo 1987 | Frost 2004 | Goldby 2006 | Hagen 2003 | Hazard 2000 |
| patients sufficiently described | + | + | + | + | + | + | + | ‐ | ‐ |
| intervention sufficiently described | + | + | ‐ | + | + | + | + | ? | + |
| use of clinical relevant outcome measures | + | + | + | + | + | + | + | + | + |
| clinically relevant effect size | ‐ | + | + | + | + | ‐ | + | + | ‐ |
| benefit worth the harms | + | + | + | + | + | + | + | + | + |
4. Clinical relevance assessment of the trials II.
| Criteria | Hurley 2001 | Hurri 1989 | Indahl 1995 | Jackson 1994 | Jellema | Karjalainen 2004 | Linton2000 | Little 2001 | Mayer 2005 |
| patients sufficiently described | ? | ? | ‐ | ‐ | + | + | ? | ? | + |
| interventions sufficiently described | ‐ | ‐ | + | + | + | + | ‐ | + | + |
| use of clinical relevant outcome measures | + | + | + | + | + | + | + | + | + |
| clinically relevant effect size | + | + | + | ‐ | ‐ | + | + | ‐ | + |
| benefit worth the harms | + | + | + | + | + | + | + | + | + |
5. Clinical relevance assessment of the trials III.
| Characteristics | Moseley 2004 | Roberts 2002 | Roland 1989 | Sherman 2005 | Storheim 2003 | Wand 2004 |
| patients sufficiently described | + | ‐ | ‐ | + | + | + |
| interventions sufficiently described | + | ? | ? | + | + | + |
| use of clinical relevant outcome measures | + | + | + | + | + | + |
| clinically relevant effect size | + | ‐ | ‐ | + | + | + |
| benefit worth the harms | + | + | + | + | + | + |
Effects of interventions
Effectiveness of individual patient education versus no intervention or of individual patient education added to usual care versus usual care only
Acute/subacute LBP
Four high quality studies (Hagen 2003; Hazard 2000; Indahl 1995; Jellema 2005) and two low quality studies (Roberts 2002; Storheim 2003) were identified (Figure 2). Two high quality studies (Hagen 2003; Indahl 1995) provide strong evidence that an individual 2.5‐hour oral educational session was more effective than no intervention on short‐term and long‐term return‐to‐work for patients with acute or subacute LBP. Two high quality studies provide strong evidence that there are no differences between giving a pamphlet (Hazard 2000) or a 20‐minute educational session (Jellema 2005) and no intervention for short‐term or long‐term pain relief . One high quality study provides moderate evidence that there are no differences in functional status (Jellema 2005). There is limited evidence from one low quality study (Storheim 2003) that a two‐hour individual educational session was more effective than usual care in improving short‐term back pain specific functional status and generic functional status for patients with acute or subacute low‐back pain.
2.
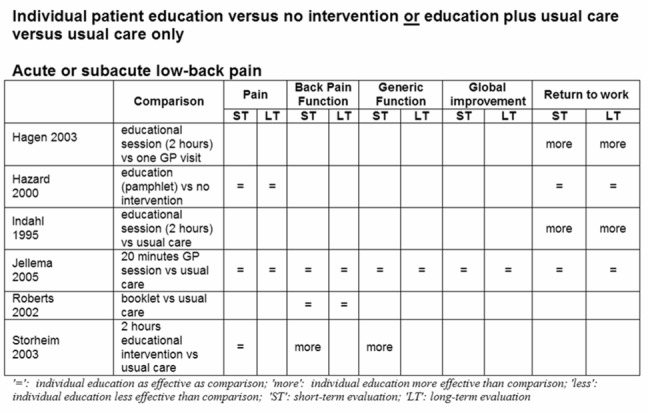
Chronic LBP
No RCTs were identified.
Mixed LBP
One high quality study (Cherkin 1996) and three low quality studies (Jackson 1994; Little 2001; Roland 1989) (Figure 3) provide moderate evidence (Cherkin 1996; Jackson 1994; Roland 1989) that there was no difference in back pain‐specific functional status, global improvement and return‐to‐work in the short and long‐term between those who received written patient education and those who received no intervention. One of the low‐quality studies (Jackson 1994) provides limited evidence that there was also no difference in short‐term pain relief.
3.
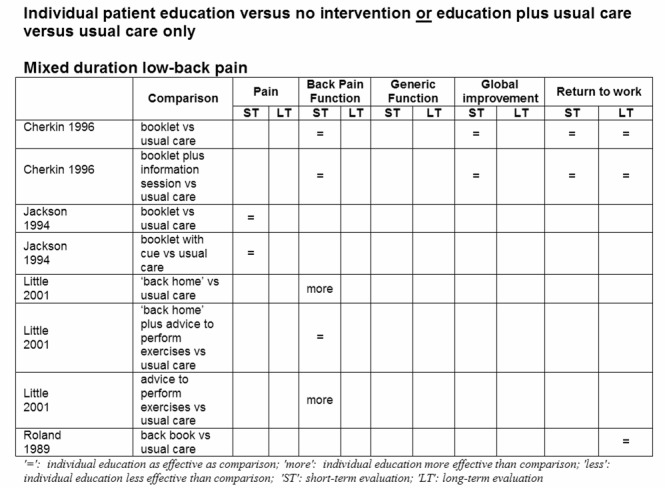
Effectiveness of Individual patient education versus non‐educational interventions
Acute/subacute LBP
Eight studies, four high quality (Cherkin 1998; Deyo 1987; Linton 2000; Karjalainen 2004) and four low quality (Hurley 2001; Mayer 2005; Storheim 2003; Wand 2004) were identified (Figure 4) that compared education with chiropractic manipulation and McKenzie therapy (Cherkin 1998), immediate x‐ray (Deyo 1987), cognitive behavioural group therapy (Linton 2000), work‐site visit (Karjalainen 2004), interferential therapy (Hurley 2001), heat‐wrap therapy (Mayer 2005), group exercise therapy (Storheim 2003), manual therapy and exercise (Wand 2004). There is strong evidence that there was no difference between educational and non‐educational interventions on short (Deyo 1987; Hurley 2001; Karjalainen 2004; Mayer 2005; Storheim 2003; Wand 2004) and long‐term pain (Deyo 1987; Hurley 2001; Karjalainen 2004; Linton 2000; Storheim 2003; Wand 2004), on short‐term back pain specific functional status (Cherkin 1998; Karjalainen 2004), and functional status (Deyo 1987; Karjalainen 2004; Linton 2000).
4.
There is conflicting evidence with regard to return‐to‐work for patients with (sub) acute LBP. While one high‐quality study (Linton 2000) found that an educational intervention was less effective than cognitive‐behavioural group therapy for long‐term return‐to‐work, another high‐quality study (Karjalainen 2004) found that a mini‐intervention (1.5 hours of education by a physiotherapist) was as effective for return‐to‐work as a work‐site visit. Another high quality study (Deyo 1987) found no difference between a brief educational session (five minutes) and an immediate x‐ray.
There is conflicting evidence with regard to global improvement since one high quality study (Cherkin 1998) concluded that a booklet was less effective for global improvement than six to nine chiropractic manipulations but found no difference between the booklet and four to six physiotherapy sessions (McKenzie approach).
There is limited evidence from one low quality study each that individual education was less effective than interferential therapy (Hurley 2001), heat‐wrap therapy plus exercises (Mayer 2005) and manual therapy plus exercises (Wand 2004) for back pain, but that individual education was more effective than exercises (Storheim 2003) for generic functional status.
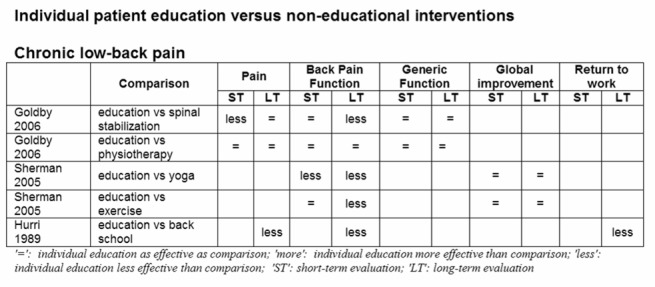
Chronic LBP
Two high quality studies (Goldby 2006; Sherman 2005) and one low quality study (Hurri 1989) were identified (Figure 5). There is strong evidence that written educational material was less effective than non‐educational interventions for low‐back pain (i.e. spinal stabilization (Goldby 2006), physiotherapy (Goldby 2006), yoga (Sherman 2005), exercises (Sherman 2005) or a modified Swedish back school (Hurri 1989) for long‐term back pain specific functional status. There is moderate evidence that there was no difference between individual education and non‐educational interventions for low‐back pain (i.e. spinal stabilization (Goldby 2006), physiotherapy (Goldby 2006), yoga (Sherman 2005) and exercises (Goldby 2006) for long‐term pain, short‐term back pain‐specific function (Goldby 2006; Sherman 2005) and short‐ and long‐term generic functional status (Goldby 2006; Hurri 1989) and global improvement (Sherman 2005). There is limited evidence from one low quality study that there was no difference in return‐to‐work between those who received written educational material and those who attended a modified Swedish back school (Hurri 1989).
5.
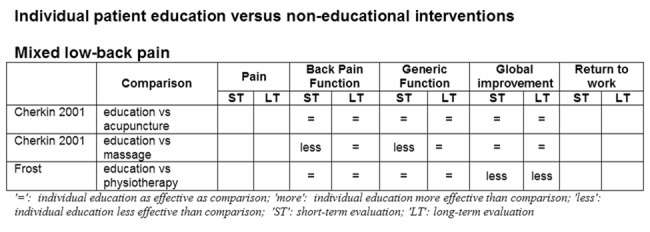
Mixed LBP
Two high quality studies (Cherkin 2001; Frost 2004) were identified (Figure 6). One high quality study (Cherkin 2001) provides moderate evidence that a book and videotapes were less effective than massage for short‐term functional status, but as effective as acupuncture. The other high quality study (Frost 2004) provides moderate evidence that there was no difference in functional status between those who received patient education and those who received routine physiotherapy.
6.
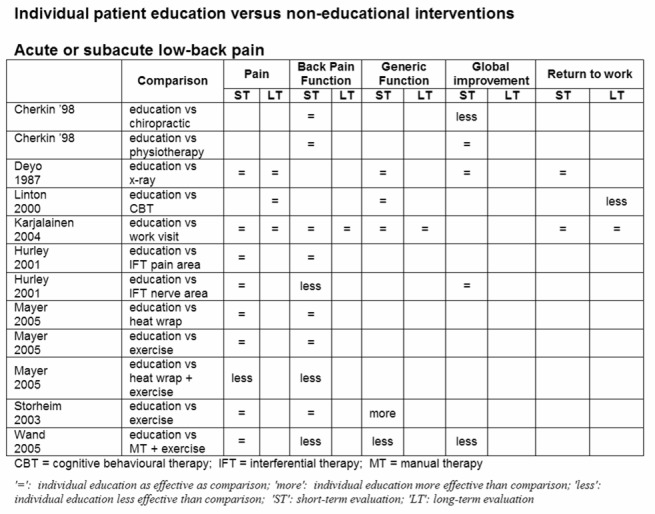
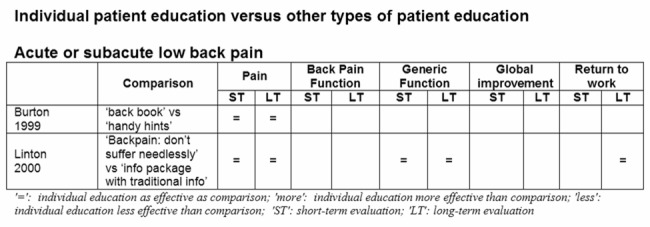
Individual patient education versus other types of patient education
Acute/subacute LBP
Two high quality studies (Burton 1999; Linton 2000) were identified (Figure 7) that provide strong evidence that there was no difference in short‐term and long‐term pain reduction between several types of individual patient education ('The Back Book' versus 'Handy Hints'; pamphlet versus information package). One of these high quality studies (Linton 2000) also evaluated the effects of a pamphlet and an information package on functional status and return‐to‐work, but found no differences in the short‐ and long‐term for patients with (sub)acute LBP.
7.
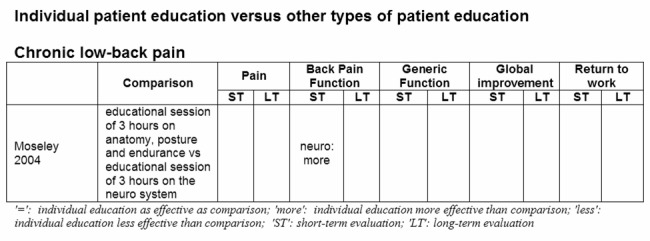
Chronic LBP
One low quality study (Moseley 2004) was identified (Figure 8) that provides limited evidence that an individual educational session of three hours was more effective for back pain‐specific functional status when the focus was on the nervous system then when the focus was on the lower back (anatomy, posture, endurance) at short‐term follow‐up (three days).
8.
Mixed LBP
Three studies, one high quality (Cherkin 1996) and two low quality (Jackson 1994; Little 2001) were identified (Figure 9) that provide moderate evidence that there was no difference in short‐ and long‐term return‐to‐work rates and global improvement between those who received a booklet and those who received a booklet plus oral information plus a telephone feedback session.
9.
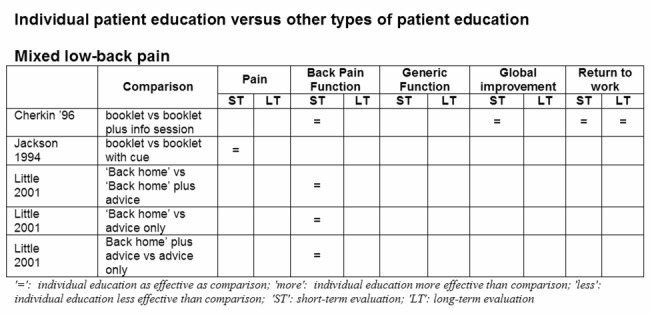
There is conflicting evidence with regard to back pain‐specific functioning. In one high quality study (Cherkin 1996), a booklet and a booklet plus oral information plus a telephone feedback session were equally effective, while a low quality study (Little 2001) found that the group who received the 'Back home' booklet plus advice to perform exercises improved less then the group that only received the 'Back Home' booklet. Only one low quality study (Jackson 1994) provides limited evidence that a booklet with a physician‐related cue was as effective as a booklet without this cue.
Sensitivity analysis
A best case analysis was carried out in which internal validity criteria that were scored as unclear ('?') were scored positive. This obviously increased the number of high quality studies. This procedure changed the results of two hours educational session versus usual care for acute/subacute LBP on back pain specific function and generic function from limited to moderate evidence, and changed the results of written information versus interferential therapy in the nerve area, heat‐wrap plus exercises and manual therapy plus exercises for back pain specific function from limited to moderate evidence.
Lowering the threshold for high quality studies from six out of 11 criteria to five out of 11 criteria changed two studies from low to high quality (Moseley 2004; Roland 1989). This changed the level of evidence from limited to moderate that a three‐hour educational session focusing on the neurological system was more effective than a three‐hour educational session focusing on anatomy, posture and endurance.
Discussion
Is individual patient education effective?
For patients with acute or subacute LBP a 2.5‐hour individual patient education session was more effective than no intervention, while less intensive patient education did not seem to be more effective than no intervention. Individual education appeared to be equally effective to interventions like chiropractic manipulation and physiotherapy for patients with acute or subacute LBP. However, for patients with chronic LBP, individual education was less effective than more intensive treatment.
In the majority of national and international guidelines on acute LBP, great store is set on stimulating the patient to remain active. A Cochrane review showed that advise to stay active as a single intervention is not effective (Hilde 2002). However, an earlier review concluded that intervention programs that included advice to stay active and to continue ordinary activities resulted in a faster return to work, less chronic disability, and fewer recurrent problems (Waddell 1997). In daily practice, patient education will often be part of a treatment program and seldom be used as single intervention.
The results of this review show that there is no difference between the effects of various types of individual patient education. What form of educational intervention is preferred and what content, intensity and frequency is best remains unclear. The extensive intervention as described by Indahl 1995 and later replicated by Hagen 2003 produced promising results in patients with subacute LBP. The effects were not only statistically significant but also had rather large clinically relevant effect sizes. Twice as many patients in the study by Indahl were still on sick leave at 200 and 400 days in the control group (60%, 39%) compared with the intervention group (30%, 15%) (Indahl 1995). However, both trials were conducted in Norway and it remains uncertain whether these findings can be replicated in other countries.
It is also very difficult to evaluate the effects of oral and written patient education. The way educational material has been developed and presented, and how much time patients spend reading the material may all influence its effectiveness. Besides, social and communication skills and clinical experience may be important in providing oral information, and these skills may differ significantly among health care providers.
None of the papers explicitly described the theoretical model on which the intervention was based. As patient education is complex and aims at behavioural changes, it is important that interventions are developed that are based on a theoretical model. This will have implications for the content of the intervention and will increase its effectiveness. Future trials should evaluate patient educational interventions that are properly developed.
Methodological considerations
The results of this review must be interpreted against several potential sources of bias involving the literature search and selection process. Studies not published in English, Dutch or German were not included in the review. It is not clear whether a language restriction is associated with bias. Some studies have indicated that the exclusion of languages other than English has little effect on summary treatment effect estimates (Moher 2000). However, we will attempt to include trials published in other languages in a future update of this review. In addition, no efforts were undertaken to track down and include the results of unpublished studies.
We defined patient education as 'any set of planned condition‐specific educational activities in a one‐to‐one situation, designed to improve patients' health behaviours and/or health status in regard to the low‐back pain problem' (Burton 1996; Tones 1991). Using this definition, we included a great diversity of interventions ranging from a five‐minute oral information 'session' (Deyo 1987) to 'examination and educational information in a spine clinic with three health care providers from three different disciplines' lasting up to three hours (Hagen 2003; Indahl 1995). We acknowledge that there is a thin line between individual patient education for several hours, psycho‐education and counselling. This makes it difficult to identify all RCTs that meet our selection criteria. We may have missed some RCTs that have labelled their intervention differently (e.g. as cognitive‐behavioural intervention), but would have fitted in our review. However, we also screened other related Cochrane reviews (advice to stay active (Hilde 2002), behavioural treatment (Ostelo 2005), back schools (Heymans 2004) for additional trials.
Authors' conclusions
Implications for practice.
An individual oral educational intervention of 2.5 hours is useful to speed up return‐to‐work in workers with acute or subacute LBP. Simple patient education sessions of shorter duration or written information do not seem to be effective as a single treatment. However, as they may be considered harmless if they are evidence‐based and up‐to‐date, there is no reason for not using oral and written education to support treatment.
Implications for research.
With regard to future research, we would like to highlight the lack of research on the effectiveness of individual patient education in patients with chronic LBP. Second, trials are needed in which the effect of patient education is evaluated for subgroups of patients (for instance high versus low level of fear of pain). Third, research is also needed to evaluate what type of education is most effective or most efficient with respect to intensity and duration, and which health care professional can best provide patient education.
What's new
| Date | Event | Description |
|---|---|---|
| 19 January 2011 | Amended | Contact details updated. |
History
Protocol first published: Issue 1, 2003 Review first published: Issue 1, 2008
| Date | Event | Description |
|---|---|---|
| 23 November 2009 | Amended | Contact details updated. |
| 21 May 2008 | Amended | Converted to new review format. |
| 25 September 2007 | New citation required and conclusions have changed | Substantive amendment |
Acknowledgements
Thank you to Rachel Couban, Trial Search Co‐ordinator for the Cochrane Back Review Group, for updating the literature search.
Appendices
Appendix 1. PUBMED search strategy
((((randomized controlled trial [pt] OR controlled clinical trial [pt] OR randomized controlled trials [mh] OR random allocation [mh] OR double‐blind method [mh] OR single‐blind method [mh] OR clinical trial [pt] OR clinical trials [mh] OR ("clinical trial" [tw]) OR ((singl* [tw] OR doubl* [tw] OR trebl* [tw] OR tripl* [tw]) AND (mask* [tw] OR blind* [tw])) OR ("latin square" [tw]) OR placebos [mh] OR placebo* [tw] OR random* [tw] OR research design [mh:noexp]) NOT (animal [mh] NOT human [mh])) AND (back pain [mh] OR low back pain [mh] OR back pain [tw] OR backache [tw])) AND (education [mh] OR patient education [mh] OR patient centred care [mh] OR information booklet [tw] OR book* [tw] OR video* [tw] OR pamphlet* [tw] OR leaflet* [tw] OR poster* [tw] OR education* [tw] OR information* [tw] OR psycheducation [tw]))
Appendix 2. OVID/CINAHL search strategy
((((randomized controlled trial.pt OR controlled clinical trial.pt OR randomized controlled trials.sh OR random allocation.sh OR double‐blind method.sh OR single‐blind method.sh OR clinical trial.pt OR exp clinical trials/ OR (clin$adj25 trial$).ti,ab OR ((singl$ OR doubl$ OR trebl$ OR tripl$) adj25 (blind$ or mask$)).ti,ab OR placebos.sh OR placebo$.ti,ab OR random$.ti,ab OR research design.sh) NOT (animal.sh NOT human.sh)) AND (back pain.sh OR low back pain.sh OR back pain.ti,ab OR backache.ti,ab)) AND (education.sh OR patient education.sh OR patient centred care.sh OR information booklet.ti,ab OR book$.ti,ab OR video$.ti,ab OR pamphlet$.ti,ab OR leaflet$.ti,ab OR poster$.ti,ab OR psychoeducation.ti,ab OR education$.ti,ab OR information$ti,ab))
Appendix 3. PsycINFO search strategy
((((randomized controlled trial [pt] OR control* [tw] OR controlled clinical trial [pt] OR randomized controlled trials [mh] OR random allocation [mh] OR double‐blind method [mh] OR single‐blind method [mh] OR clinical trial [pt] OR clinical trials [mh] OR ("clinical trial" [tw]) OR ((singl* [tw] OR doubl* [tw] OR trebl* [tw] OR tripl* [tw]) AND (mask* [tw] OR blind* [tw])) OR ("latin square" [tw]) OR placebos [mh] OR placebo* [tw] OR random* [tw] OR research design [mh:noexp]) NOT (animal [mh] NOT human [mh])) AND (back pain [mh] OR low back pain [mh] OR back pain [tw] OR backache [tw])) AND (education [mh] OR patient education [mh] OR patient centred care [mh] OR information booklet [tw] OR book* [tw] OR video* [tw] OR pamphlet* [tw] OR leaflet* [tw] OR poster* [tw] OR education* [tw] OR information* [tw] OR psycheducation [tw]))
Appendix 4. EMBASE search strategy
(((randomized controlled trial or controlled clinical trial).pt. or randomized controlled trials.sh. or random allocation.sh. or double‐blind method.sh. or single‐blind method.sh. or clinical trial.pt. or exp clinical trials/ or clin$adj25 trial$.ti,ab. or ((singl$ or doubl$ or trebl$ or tripl$) adj25 (blind$ or mask$)).ti,ab. or placebos.sh. or placebo$.ti,ab. or random$.ti,ab. or research design.sh.) not (animal not human).sh.) and ((back pain or low back pain).sh. or back pain.ti,ab. or backache.ti,ab.) and ((education or patient education or patient centred care).sh. or information booklet.ti,ab. or book$.ti,ab. or video$.ti,ab. or pamphlet$.ti,ab. or leaflet$.ti,ab. or poster$.ti,ab. or psychoeducation.ti,ab. or education$.ti,ab. or information$ti,ab.mp.)
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Burton 1999.
| Methods | RCT | |
| Participants | N = 162; Mean age (yrs): 43.6; Gender (female): 55%; Diagnosis: Acute or recurrent LBP, with or without referred leg pain; sciatica excluded. Setting: Primary Care. | |
| Interventions | (E1) The 'Back Book': a booklet with biopsychosocial information ‐ plus usual care (N=79); (E2) 'Handy Hints': a booklet with biomedical information plus usual care (N=83). | |
| Outcomes | Pain
Pain intensity at worst (VAS 1‐10) at baseline, 2 wk, 3 mo and 1 yr: (E1) 71.5 (19.2); 53.9 (27.2); 49.2 (29.7); 50.9 (29.6); (E2) 68.7 (18.5); 53.9 (26.3); 50.1 (28.5); 50.8 (27.8).
Pain intensity at best (VAS 1‐10) at baseline, 2 wk, 3 mo and 1 yr: (E1) 15.8 (17.5); 9.7 (12.2); 8.7 (14.4); 10.1 (16.6); (E2) 15.6 (18.7); 12.9 (5.2); 8.8 (5.2); 10.6 (17.8). Secondary outcomes Fear avoidance: at 2 wk, 3 mo and 1 yr: E1 superior to E2 (P<0.05). |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | |
| Allocation concealment? | Low risk | A ‐ Adequate |
| Blinding? All outcomes ‐ patients? | Low risk | |
| Blinding? All outcomes ‐ providers? | Low risk | |
| Blinding? All outcomes ‐ outcome assessors? | Low risk | |
| Incomplete outcome data addressed? All outcomes ‐ drop‐outs during intervention? | High risk | |
| Incomplete outcome data addressed? All outcomes ‐ drop‐outs during follow‐up? | Low risk | |
| Incomplete outcome data addressed? All outcomes ‐ ITT analysis? | Low risk | |
| Similarity at baseline characteristics? | Low risk | |
| Co‐interventions avoided or similar? | Unclear risk | Unclear from text. |
| Compliance acceptable? | Low risk | |
Cherkin 1996.
| Methods | RCT | |
| Participants | N=294; Mean age: 42.6; Gender (female): 48%; Diagnosis: LBP (sciatica included) or hip pain. Setting: Primary Care. | |
| Interventions | (E1) A booklet with biopsycho‐social information plus usual care (N= 102); (E2) Nurse intervention: a booklet with biopsychosocial information, a 15‐min session with a clinic nurse, a follow‐up phone call plus usual care (N=95); (C) Usual care (N=97). | |
| Outcomes | Back pain‐specific functional status:
Roland Disability score (0 to 24, 0 = no disability) overall at baseline and change at 1 wk: (E1) 13.8, ‐5.4; (E2) 13.8, ‐5.2; (C) 13.8, ‐5.3
% Patients with any bed days in first 7 wks and in 6th to 12th mo: (E1) 23%, 8%; (E2) 28%, 6%; (C) 21%, 7% Global improvement: Bothersomeness (0 to 10), overall at baseline and change at 1 wk: (E1) 7.4, ‐3.3; (E2) 7.4, ‐3.5; (C) 7.4 ‐3.6 Return to work: % Patients with any work‐loss days in first 7 wks and in 6th to 12th mo: (E1) 24%, 7%; (E2) 36%, 6% ; (C) 29%, 9% Secondary outcomes: 'Perceived knowledge': at 1 wk, (E1) and (E2) superior to (C); at 3 and 7 wk, (E2) superior to (E1) and (C) (P<0.05) 'Satisfaction with care': at 1 wk, (E2) superior to (E1) and (C) (P<0.05) |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Blinding? All outcomes ‐ patients? | High risk | |
| Blinding? All outcomes ‐ providers? | High risk | |
| Blinding? All outcomes ‐ outcome assessors? | Low risk | |
| Incomplete outcome data addressed? All outcomes ‐ drop‐outs during intervention? | Low risk | |
| Incomplete outcome data addressed? All outcomes ‐ drop‐outs during follow‐up? | Low risk | |
| Incomplete outcome data addressed? All outcomes ‐ ITT analysis? | Low risk | |
| Similarity at baseline characteristics? | Low risk | |
| Co‐interventions avoided or similar? | Low risk | |
| Compliance acceptable? | Low risk | |
Cherkin 1998.
| Methods | RCT | |
| Participants | N= 321; Mean age (yrs): 40.7; Gender (female): 48%; Diagnosis: > 7 days LBP, sciatica excluded Setting: Primary Care. | |
| Interventions | (E) A booklet with biopsychosocial information (N=66); (C1) Chiropractic manipulation: 6 to 9 sessions, 145 minutes (N=122); (C2) Physiotherapy (McKenzie approach): 4 to 6 sessions, 145 minutes (N=133). | |
| Outcomes | Back pain specific functional status:
Roland Disability score at baseline, 4 wk and 12 wk: (E) 11.7 (10.4 to 13.0); 4.9 (3.8 to 6.0); 4.3 (3.1 to 5.5); (C1) 12.1 (11.2 to 13.1); 3.7 (2.9 to 4.5); 3.1 (2.4 to 3.9); (C2) 12.2 (11.2 to 13.1); 4.1 (3.3 to 4.9); 4.1 (3.2 to 5.0) Global improvement: Symptom bothersomeness score at baseline, 4 wk** and 12 wk: (E) 5.3 (4.9 to 5.7); 3.1 (2.4 to 3.9); 3.2 (2.4 to 4.0); (C1) 5.5 (5.1 to 5.8); 1.9 (1.5 to 2.2); 2.0 (1.6 to 2.4); (C2) 6.0 (5.6 to 6.5); 2.3 (1.9 to 2.8); 2.7 (2.2 to 3.2). Secondary outcomes: 'Satisfaction with care': at 1 and 4 wk, (E) inferior to (C1) and (C2) (p < 0.05) 'Costs of care': at 2 yr, (E) superior to (C1) and (C2) (p < 0.05) **(E) significantly less effective than (C1) (p < 0.05). |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Blinding? All outcomes ‐ patients? | High risk | |
| Blinding? All outcomes ‐ providers? | High risk | |
| Blinding? All outcomes ‐ outcome assessors? | Low risk | |
| Incomplete outcome data addressed? All outcomes ‐ drop‐outs during intervention? | Low risk | |
| Incomplete outcome data addressed? All outcomes ‐ drop‐outs during follow‐up? | Low risk | |
| Incomplete outcome data addressed? All outcomes ‐ ITT analysis? | Low risk | |
| Similarity at baseline characteristics? | High risk | |
| Co‐interventions avoided or similar? | Low risk | |
| Compliance acceptable? | Low risk | |
Cherkin 2001.
| Methods | RCT | |
| Participants | N = 262; Mean age (yrs): 44.9; Gender (female): 58%; Diagnosis: > 6 weeks of LBP, sciatica excluded. Setting: Primary Care. | |
| Interventions | (E) Self‐care biopsychosocial education material: book and 2 videotapes (N=90); (C1) Acupuncture: mean (SD) 8 (2.4) sessions (N=94); (C2) Massage: mean (SD) 8.3 (2.3) sessions (N=78). | |
| Outcomes | Back pain‐specific functional status:
Roland Disability score (0 to 24) at baseline, 4 wk, 10 wk** and 1 yr: (E) 12.0 (10.9 to 13.0); 9.3 (8.0 to 10.6); 8.8 (7.4 to 10.2); 6.4 (5.1 to 7.7); (C1) 12.8 (11.7 to 13.8); 9.1 (7.8 to 9.9); 7.9 (6.5 to 9.3); 8.0 (6.6 to 9.3); (C2) 11.8 (10.8 to 12.7); 7.9 (6.9 to 9.0); 6.3 (5.1 to 7.5); 6.8 (5.5 to 8.1) Global improvement: Symptom bothersomeness score at baseline, 4 wk, 10 wk and 1 yr: (E) 6.1 (5.7 to 6.5); 4.9 (4.3 to 5.5); 4.6 (3.9 to 5.3); 3.8 (3.1 to 4.5); (C1) 6.2 (5.8 to 6.5); 4.3 (3.7 to 4.9); 4.0 (3.4 to 4.9); 4.5 (3.8 to 5.2); (C2) 6.2 (5.8 to 6.6); 4.5 (4.0 to 5.1); 3.6 (3.0 to 4.2); 3.2 (2.5 to 3.9) Generic Functional Status (no data provided): Mental Health Scale (SF‐12): at 4 wk, (E) significantly less effective than (C2) Physical Health Scale (SF‐12): at 10 wk, (E) significantly less effective than (C2) Secondary outcomes: Satisfaction with care: at 10 wk, (E) inferior to (C1) and (C2) (p < 0.05) **(E) significantly less effective than (C2) (p < 0.05). |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | |
| Allocation concealment? | High risk | C ‐ Inadequate |
| Blinding? All outcomes ‐ patients? | High risk | |
| Blinding? All outcomes ‐ providers? | High risk | |
| Blinding? All outcomes ‐ outcome assessors? | Low risk | |
| Incomplete outcome data addressed? All outcomes ‐ drop‐outs during intervention? | Low risk | |
| Incomplete outcome data addressed? All outcomes ‐ drop‐outs during follow‐up? | Low risk | |
| Incomplete outcome data addressed? All outcomes ‐ ITT analysis? | Low risk | |
| Similarity at baseline characteristics? | Low risk | |
| Co‐interventions avoided or similar? | High risk | |
| Compliance acceptable? | Low risk | |
Deyo 1987.
| Methods | RCT | |
| Participants | N=101; Mean age (yrs): 33.4; Gender (female): 52%; Diagnosis: low risk LBP patients Setting: Walk‐in Clinic | |
| Interventions | (E) Brief (5 min) educational session (N=52); (C) Immediate roentgenogram (N=49). | |
| Outcomes | Pain:
Duration of pain (days) at 3 wk and 3 mo: (E) 10.8, 29.2; (C) 9.4, 22.7 Generic functional status: Sickness Impact Profile at baseline, 3 wk and 3 mo: (E) 17.5, 13.6, 10.3; (C) 20.1, 16.6, 12.3 Global improvement: Self‐rated improvement (1 to 6) at 3 wk and 3 mo: (E) 2.7, 2.6; (C) 2.7, 2.6 Return to work Work absenteeism (days) at 3 wk and 3 mo: (E) 4.4, 4.5; (C) 4.1, 4.4 Secondary outcomes: 'Agree that everyone with LBP should have roentgenogram': at 3 wk, (E) 44% vs. (C) 73% |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Blinding? All outcomes ‐ patients? | High risk | |
| Blinding? All outcomes ‐ providers? | High risk | |
| Blinding? All outcomes ‐ outcome assessors? | High risk | |
| Incomplete outcome data addressed? All outcomes ‐ drop‐outs during intervention? | Low risk | |
| Incomplete outcome data addressed? All outcomes ‐ drop‐outs during follow‐up? | Low risk | |
| Incomplete outcome data addressed? All outcomes ‐ ITT analysis? | Low risk | |
| Similarity at baseline characteristics? | Low risk | |
| Co‐interventions avoided or similar? | Low risk | |
| Compliance acceptable? | Low risk | |
Frost 2004.
| Methods | RCT | |
| Participants | N=975; Mean age (yrs): 42.5; Gender (female): 39%; Diagnosis: workers 8 to 12 wks sick‐listed because of LBP (sciatica not excluded) Setting: Spine Clinic vs Primary Care | |
| Interventions | (E) One session of one hour with a physiotherapist (physical examination, general advice to remain active, advice book) (N=142) (C) Physical examination and advice book, routine physiotherapy up to 5 sessions (N=144) | |
| Outcomes | Back pain specific‐functional status:
Oswestry Disability Index at 2, 6 and 12 mo: (E) ‐1.33 (9.29), ‐1.83 (10.61), ‐2.23 (11.47); (C) ‐2.65 (9.34), ‐2.89 (11.59), ‐3.27 (10.99)
Roland Morris at 2, 6 and 12 mo: (E) ‐0.56 (3.38), ‐0.79 (4.20), ‐0.99 (4.23); (C) ‐1.13 (3.98), ‐1.19 (4.74), ‐1.36 (4.66) Generic Functional Status: Physical function (SF‐36) at 2, 6 and 12 mo: (E) 1.70 (16.10), 2.77 (17.07), 3.22 (18.87); (C) 5.24 (19.99), 5.43 (18.80), 5.98 (20.98) Global improvement: Patient perceived benefit (0 to 10) at 2**, 6** and 12** mo: (E) 3.66 (2.78), 3.61(2.98), 4.13 (2.95); (C)5.42 (2.84), 4.74 (3.24), 5.02 (3.12) ** (C) significantly more effective than (E) (p < 0.05) |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | |
| Allocation concealment? | Low risk | A ‐ Adequate |
| Blinding? All outcomes ‐ patients? | High risk | |
| Blinding? All outcomes ‐ providers? | High risk | |
| Blinding? All outcomes ‐ outcome assessors? | Low risk | |
| Incomplete outcome data addressed? All outcomes ‐ drop‐outs during intervention? | Low risk | |
| Incomplete outcome data addressed? All outcomes ‐ drop‐outs during follow‐up? | High risk | |
| Incomplete outcome data addressed? All outcomes ‐ ITT analysis? | Low risk | |
| Similarity at baseline characteristics? | Low risk | |
| Co‐interventions avoided or similar? | Unclear risk | Unclear from text. |
| Compliance acceptable? | Low risk | |
Goldby 2006.
| Methods | RCT | |
| Participants | N=302; Mean age (yrs): 42; Gender (female): 69%; Diagnosis: > 12 weeks LBP (with or without leg pain or sciatica); mean LBP at baseline: 11.7 yrs Setting: Hospital physiotherapy department | |
| Interventions | (E) Booklet 'Back in Action' plus back school (= one three‐hour group session with questions and answers) (N=40) (C1) Spinal stabilization program (10 weeks course) plus back school (N=84) (C2) Physiotherapy (maximum of 10 interventions on exercises and/or manual therapy and/or massage) plus back school (N=89) | |
| Outcomes | Pain:
Pain intensity (0 to 100) NRS at 3, 6, 12 and 24 months: (E) 34.4 (36.43), 30.25 (31.68), 30 (34.05), 50.9 (33.7); (C1) 28.81 (28.14), 23.16 (27.43), 29.23 (28.1), 35.4 (29.0); (C2)35.38 (35.38), 37.16 (30.24), 35.17 (30.99), 37.8 (29.6)
Back pain last 2 days: %yes; at 3, 6##, 12 and 24 months: (E) 67.6, 56, 53.60, 80; (C1) 71.4, 47.9, 56.3, 27; (C2) 72.6, 72.4, 61.1, 0 43 Back pain‐specific functional status: Oswestry Disability at 3, 6, 12** and 24 months: (E) 28.1 (17.34), 23.9 (17.75), 26.9 (19.6), 27 (18); (C1) 31.00 (15.62), 25.81 (17.07), 24.76 (17.82), 27 (17.44); (C2) 31.36 (13.16), 30.45 (14.34), 29.56 (16.65), 31 (16.47) Generic Functional Status: Nottingham Health Profile at 3, 6, 12 and 24 months: (E) 94.32 (85.41), 77.50 (90.5), 87.47 (107.11), 83 (106.3); (C1) 94.97 (99.35), 76.30 (75.46), 70.06 (78.48), 82 (103.8); (C2) 107.18 (112.29), 115.85 (124.25), 103.58 (110.15); 121.60 (114.4) ## (C1) significantly more effective than (C2) or (E) (P < 0.05) ** (C1) significantly more effective than (E) (P < 0.05) |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Blinding? All outcomes ‐ patients? | High risk | |
| Blinding? All outcomes ‐ providers? | High risk | |
| Blinding? All outcomes ‐ outcome assessors? | Low risk | |
| Incomplete outcome data addressed? All outcomes ‐ drop‐outs during intervention? | Low risk | |
| Incomplete outcome data addressed? All outcomes ‐ drop‐outs during follow‐up? | Low risk | |
| Incomplete outcome data addressed? All outcomes ‐ ITT analysis? | Low risk | |
| Similarity at baseline characteristics? | High risk | |
| Co‐interventions avoided or similar? | Low risk | |
| Compliance acceptable? | Low risk | |
Hagen 2003.
| Methods | RCT | |
| Participants | N=457; Mean age (yrs): 40.9; Gender (female): 48%; Diagnosis: Workers with LBP (sciatica included) and sick‐listed for 8 to 12 weeks Setting: Spine Clinic and Primary Care | |
| Interventions | (E) Oral educational session and examination in Spine Clinic (±2 hrs) (N=237); (C) Primary health care: at least one visit with GP (N=220). | |
| Outcomes | Return to work
% Patients returned to full‐duty work at 12## , 24 and 36 mo: (E) 68.8%, 61.2%, 63.8%; (C) 57.3%, 66.1%, 61.8% ## (E) significantly more effective than (C) (p < 0.05) |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | |
| Allocation concealment? | Low risk | A ‐ Adequate |
| Blinding? All outcomes ‐ patients? | High risk | |
| Blinding? All outcomes ‐ providers? | High risk | |
| Blinding? All outcomes ‐ outcome assessors? | Low risk | |
| Incomplete outcome data addressed? All outcomes ‐ drop‐outs during intervention? | Low risk | |
| Incomplete outcome data addressed? All outcomes ‐ drop‐outs during follow‐up? | Low risk | |
| Incomplete outcome data addressed? All outcomes ‐ ITT analysis? | Low risk | |
| Similarity at baseline characteristics? | Low risk | |
| Co‐interventions avoided or similar? | Low risk | |
| Compliance acceptable? | Low risk | |
Hazard 2000.
| Methods | RCT | |
| Participants | N=489; Mean age (yrs): 37.7; Gender (female): 40%; Diagnosis: reported LBP within 11 days after an occupational injury, unclear whether sciatica was included. Setting: occupational | |
| Interventions | (E1) 'Back Home' booklet with biopsychosocial information and usual care (N=63); (E2) 'Back Home' booklet with biopsychosocial information plus advice to perform exercises and usual care (N=56); (E3) Advice to perform exercises and usual care (N=61); (C) Usual care: no booklet nor exercises (N=59). | |
| Outcomes | Back pain specific functional status:
Pain/function score (0 to 100), mean change and 95% CI at 1 and 3 wk:
(E1) vs. (C) ‐8.7 (‐17.4 to ‐0.03), # ‐6.3 (‐14.6 to 2.0)
(E2) vs. (C) ‐0.1 (‐9.0 to 8.9), ‐4.0 (‐12.6 to 4.6)
(E3) vs. (C) ‐7.9 (‐16.7 to 0.8), # ‐1.4 (‐9.9 to 7.1) Aberdeen Pain & Function scale (0 to 100), mean change and 95% CI at 1 wk: (E1) vs. (C) ‐3.8 (‐7.7 to 0.1) # (E2) vs. (C) ‐1.9 (‐5.8 to 2.1) (E3) vs. (C) ‐5.3 (‐9.3 to ‐1.4) # |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Unclear from text. |
| Allocation concealment? | Low risk | A ‐ Adequate |
| Blinding? All outcomes ‐ patients? | Unclear risk | Unclear from text. |
| Blinding? All outcomes ‐ providers? | Low risk | |
| Blinding? All outcomes ‐ outcome assessors? | Low risk | |
| Incomplete outcome data addressed? All outcomes ‐ drop‐outs during intervention? | Low risk | |
| Incomplete outcome data addressed? All outcomes ‐ drop‐outs during follow‐up? | Low risk | |
| Incomplete outcome data addressed? All outcomes ‐ ITT analysis? | High risk | |
| Similarity at baseline characteristics? | Low risk | |
| Co‐interventions avoided or similar? | High risk | |
| Compliance acceptable? | Unclear risk | Unclear from text. |
Hurley 2001.
| Methods | RCT | |
| Participants | N=59; Mean age (yrs): 34.6; Gender (female): 55%; Diagnosis: LBP for 1 to 3 months, with or without pain radiation (sciatica included). Setting: Physiotherapy | |
| Interventions | (E) The 'Back Book': a booklet with biopsychosocial information. Message reinforced by physiotherapist (3 sessions) (N=20); (C1) Interferential therapy (IFT) in painful area (3 sessions) and the 'Back Book' (N=18); (C2) IFT in spinal nerve area (4 sessions) and the 'Back Book' (N=21). | |
| Outcomes | Pain:
Median Pain rating index (MPQ) at baseline, discharge and 3 mo: (E)15.5 (IQR 14.7), 4.0 (IQR 5.0), 3.0 (IQR 5.0); (C1)11.5 (IQR 11.8), 1.0 (IQR 6.3), 5.0 (IQR 14.0); (C2)14.0 (IQR 12.5), 2.0 (IQR 5.0), 2.0 (IQR 10.0) Back pain‐specific functional status: Roland‐Morris Disability score: median at baseline, discharge and 3## mo: (E) 5.0 (IQR 4.5), 2.0 (IQR 2.0), 1.0 (IQR 1.0); (C1) 5.5 (IQR 6.3),1.5 (IQR 3.3), 2.0 (IQR 3.0); (C2)9.0 (IQR 8.0), 2.0 (IQR 4.5), 1.0 (IQR 5.5) Global improvement: EuroQol, median at baseline, discharge and 3 mo: (E) 0.69 (IQR 0.20), 0.93 (IQR 0.20), 1.0 (IQR 0.20); (C1) 0.69 (IQR 0.14), 0.80 (IQR 0.24), 0.8 (IQR 0.27); (C2) 0.76 (IQR 0.17), 0.79 (IQR 0.31), 0.8 (IQR 0.31) ## (E) significantly less effective than (C2) (P < 0.05). |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | |
| Allocation concealment? | Low risk | A ‐ Adequate |
| Blinding? All outcomes ‐ patients? | High risk | |
| Blinding? All outcomes ‐ providers? | High risk | |
| Blinding? All outcomes ‐ outcome assessors? | Unclear risk | Unclear from text. |
| Incomplete outcome data addressed? All outcomes ‐ drop‐outs during intervention? | Low risk | |
| Incomplete outcome data addressed? All outcomes ‐ drop‐outs during follow‐up? | High risk | |
| Incomplete outcome data addressed? All outcomes ‐ ITT analysis? | Low risk | |
| Similarity at baseline characteristics? | High risk | |
| Co‐interventions avoided or similar? | High risk | |
| Compliance acceptable? | Unclear risk | Unclear from text. |
Hurri 1989.
| Methods | RCT | |
| Participants | N=188; Mean age (yrs): 45.8; Gender (female): 100%; Diagnosis: patients with idiopathic LBP for at least 12 months. Setting: Occupational | |
| Interventions | (E) Instruction material of back school in written form (no actual treatment was administered) (N=93); (C) Modified Swedish back school: 6 x 60‐minutes education and exercise sessions in 3 weeks; 11 participants per group. Refresher course 2 x 60 min after 6 months (N=95); | |
| Outcomes | Pain (graph):
Pain VAS (0 to 100) at baseline, 6## and 12 mo (graph): (E) 86, 95, 89; (C) 91, 70, 78
Low Back Pain Index (0 to 20) at baseline, 6## and 12 mo (graph): (E) 18.2, 17.7, 17.5; (C) 17.8, 15.5, 16.2 Back pain‐specific functional status (graph): Oswestry LBP Disability Questionnaire (0 to 100) at baseline, 6## and 12## mo: (E) 20.5, 21.5, 21.3; (C) 19.9, 19.2, 19.4 Return to work (no data) Sick leave due to LBP: no significant differences ## (E) significantly less effective than (C) (p < 0.05). |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | High risk | |
| Allocation concealment? | High risk | C ‐ Inadequate |
| Blinding? All outcomes ‐ patients? | High risk | |
| Blinding? All outcomes ‐ providers? | High risk | |
| Blinding? All outcomes ‐ outcome assessors? | High risk | |
| Incomplete outcome data addressed? All outcomes ‐ drop‐outs during intervention? | Low risk | |
| Incomplete outcome data addressed? All outcomes ‐ drop‐outs during follow‐up? | Low risk | |
| Incomplete outcome data addressed? All outcomes ‐ ITT analysis? | Low risk | |
| Similarity at baseline characteristics? | Low risk | |
| Co‐interventions avoided or similar? | High risk | |
| Compliance acceptable? | High risk | |
Indahl 1995.
| Methods | RCT | |
| Participants | N=975; Mean age (yrs): 42.5; Gender (female): 39%; Diagnosis: workers 8 to 12 wks sick‐listed because of LBP (sciatica not excluded). Setting: Spine Clinic vs Primary Care | |
| Interventions | (E) Oral educational session and examination in Spine Clinic (±2 hrs) (N=463); (C) Usual care (N=512). | |
| Outcomes | Return to work (graph):
% Patients on sickness leave at 200## and 400## days: (E)30%, 15%; (C) 60%, 39%
Sickness leave: Proportional Hazard Model: (E) vs (C) RR = 2.2 (1.7 to 2.8)## ## (E) significantly more effective than (C) (p < 0.05) |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | High risk | |
| Allocation concealment? | Low risk | A ‐ Adequate |
| Blinding? All outcomes ‐ patients? | High risk | |
| Blinding? All outcomes ‐ providers? | High risk | |
| Blinding? All outcomes ‐ outcome assessors? | Low risk | |
| Incomplete outcome data addressed? All outcomes ‐ drop‐outs during intervention? | Low risk | |
| Incomplete outcome data addressed? All outcomes ‐ drop‐outs during follow‐up? | Low risk | |
| Incomplete outcome data addressed? All outcomes ‐ ITT analysis? | Low risk | |
| Similarity at baseline characteristics? | High risk | |
| Co‐interventions avoided or similar? | High risk | |
| Compliance acceptable? | Low risk | |
Jackson 1994.
| Methods | RCT | |
| Participants | N=68; Mean age (yrs): 43; Gender (female): 60%; Diagnosis: patients with neck and / or back pain, who were advised to exercise. Unclear whether sciatica was included. Setting: Primary Care | |
| Interventions | (E1) Booklet with biopsychosocial information (N=?)
(E2) Booklet with biopsycho‐social information with physician related cue (N=?)
(C) No booklet (N=?) Note: For the analysis we did the assumption of 23 patients per group |
|
| Outcomes | Pain (no data): Short‐Form McGill Pain Questionnaire: no significant differences | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | High risk | |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Blinding? All outcomes ‐ patients? | Unclear risk | Unclear from text |
| Blinding? All outcomes ‐ providers? | Unclear risk | Unclear from text |
| Blinding? All outcomes ‐ outcome assessors? | Unclear risk | Unclear from text |
| Incomplete outcome data addressed? All outcomes ‐ drop‐outs during intervention? | Low risk | |
| Incomplete outcome data addressed? All outcomes ‐ drop‐outs during follow‐up? | Low risk | |
| Incomplete outcome data addressed? All outcomes ‐ ITT analysis? | Unclear risk | Unclear from text |
| Similarity at baseline characteristics? | Unclear risk | Unclear from text |
| Co‐interventions avoided or similar? | Unclear risk | Unclear from text |
| Compliance acceptable? | Low risk | |
Jellema 2005.
| Methods | RCT | |
| Participants | N=314; Mean age (yrs): 42.5; Gender (female): 47.5%; Diagnosis: < 3 months LBP (75% < 3 weeks LBP) Setting: General practice | |
| Interventions | (E) GP consultation with emphasis on psychosocial prognostic factors (at least one consultation of 20 minutes) plus educational booklet (N=143) (C) Usual care by GP (N=171) | |
| Outcomes | Pain:
NRS Pain (0 to 10) at baseline, 6, 13, 26 and 52 wks: (E) 5 (3‐7), 2 (0‐4), 0 (0‐3), 0 (0‐3), 0 (0‐3); (C) 5 (3‐6), 2 (0‐4), 1 (0‐3), 0 (0‐2), 0 (0‐2) Back Pain specific functional status: Roland Morris (0 to 24) at baseline, 6, 13, 26 and 52 wks: (E)13 (7‐16), 4 (1‐9), 2 (0‐6), 1 (0‐4), 1 (0‐4); (C) 13 (8‐16), 4 (1‐10), 2 (0‐5), 1 (0‐3), 1 (0‐4) Return to Work: Sick leave due to LBP (%yes) at baseline, 6, 13, 26 and 52 wks: (E) 34.9%, 16.4%, 4.4%, 2.7%, 7.5%; (C) 41.0%, 19.7%, 12.7%, 8.2%, 7.0% Generic Functional status: Perceived general health (1 to 5) (SF‐36) at baseline, 13, 26 and 52 wks: (E) 2.7 (0.8), 2.6 (0.8), 2.6 (0.7), 2.7 (0.9); (C) 2.9 (0.8), 2.6 (0.8), 2.6 (0.8), 2.7 (0.8) Global Improvement: Perceived no recovery (%yes) at 13, 26 and 52 wks: (E) 39.4%, 33.3%, 32.4%, 31.8%; (C) 37.8%, 32.3%, 30.7%, 27.6% |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | High risk | |
| Allocation concealment? | Low risk | A ‐ Adequate |
| Blinding? All outcomes ‐ patients? | Low risk | |
| Blinding? All outcomes ‐ providers? | High risk | |
| Blinding? All outcomes ‐ outcome assessors? | Low risk | |
| Incomplete outcome data addressed? All outcomes ‐ drop‐outs during intervention? | Low risk | |
| Incomplete outcome data addressed? All outcomes ‐ drop‐outs during follow‐up? | Low risk | |
| Incomplete outcome data addressed? All outcomes ‐ ITT analysis? | Low risk | |
| Similarity at baseline characteristics? | Low risk | |
| Co‐interventions avoided or similar? | Low risk | |
| Compliance acceptable? | Low risk | |
Karjalainen 2004.
| Methods | RCT | |
| Participants | N=164; Mean age (yrs): 43.6; Gender (female): 58%; Diagnosis: workers with subacute LBP (69% had sciatica) which had made working difficult for > 4 wk and < 3 mo. Setting: Occupational | |
| Interventions | (E) Mini‐intervention group: one assessment with physician and physiotherapist plus 1‐1/2 hours instruction by physiotherapist and a pamphlet with biopsychosocial information (N=56). (C1) Work‐site visit group: one assessment with physician and physiotherapist plus a work visit and the same pamphlet (N=51) (C2) The same pamphlet and usual care (N=57) | |
| Outcomes | Pain:
Intensity of pain (0 to 10) at baseline, 24 mo: (E) 6.2 (2‐10), 3.5 (0‐9); (C1) 5.4 (1‐10), 3.2 (0‐9); (C2) 5.7 (1‐10), 3.4 (0‐9)
% Patients with daily symptoms at 24 mo: (E) 15%; (C1) 16%; (C2) 17% Back pain specific functional status: Oswestry disability index at baseline, 24 mo: (E) 36 (4‐69), 19 (0‐60); (C1) 33 (7‐71), 18 (0‐60); (C2) 34 (13‐67), 18 (0‐58) Return to work: Days on sick‐leave at 24 mo: (E) 30 (0‐615); (C1) 45 (0‐610); (C2) 62 (0‐630); Generic functional status: Health related quality of life (15D; 0 to 1) at baseline and 24 mo: (E) 0.85( 0.61 to 1.00), 0.90 (0.7 to 1.0); (C1) 0.86 (0.70 to 0.99), 0.89 (0.49 to 1.0); (C2) 0.86 (0.70 to 0.98), 0.89 (0.6 to 1.0) |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | |
| Allocation concealment? | Low risk | A ‐ Adequate |
| Blinding? All outcomes ‐ patients? | High risk | |
| Blinding? All outcomes ‐ providers? | High risk | |
| Blinding? All outcomes ‐ outcome assessors? | High risk | |
| Incomplete outcome data addressed? All outcomes ‐ drop‐outs during intervention? | Low risk | |
| Incomplete outcome data addressed? All outcomes ‐ drop‐outs during follow‐up? | Low risk | |
| Incomplete outcome data addressed? All outcomes ‐ ITT analysis? | Low risk | |
| Similarity at baseline characteristics? | Low risk | |
| Co‐interventions avoided or similar? | Low risk | |
| Compliance acceptable? | Low risk | |
Linton 2000.
| Methods | RCT | |
| Participants | N=243; Mean age (yrs): 44.3; Gender (female): 71%; Diagnosis: patients with (sub)acute spinal pain and a 'self‐perceived risk of a chronic problem developing' and < 3 months cumulative sick leave during past year. Unclear whether sciatica was included. Setting: Primary Care | |
| Interventions | (E1): A pamphlet with biopsychosocial information 'Backpain‐don't suffer needlessly' and usual care (N=70); (E2) An information package with traditional information and usual care (N=66); (C) A cognitive‐behavioral intervention (6 sessions of 2 hrs in groups with 6‐10 participants) and usual care (N=92). | |
| Outcomes | Pain:
Average pain (0 to 10) and 95% CI at baseline and 1 yr: (E1) 4.8 (4.4 to 5.3), 4.0 (3.5 to 4.6); (E2) 5.0 (4.3 to 5.6), 4.2 (3.4 to 5.0); (C) 4.8 (4.3 to 5.3), 3.9 (3.3 to 4.4)
Worst pain (0 to 10) and 95% CI at baseline and 1 yr: (E1) 7.1 (6.6 to 7.6), 6.1 (5.6 to 6.7); (E2) 7.3 (6.8 to 7.8), 6.5 (5.9 to 7.1); (C) 7.0 (6.5 to 7.4), 5.7 (5.3 to 6.3)
Pain‐free days (0 to 7) and 95% CI at baseline and 1 yr: (E1) 0.9 (0.5 to 1.3), 1.8 (1.3 to 2.4); (E2) 1.2 (0.6 to 1.8), 2.1 (1.4 to 2.8); (C) 1.4 (1.0 to 1.8), 2.1 (1.5 to 2.6) Generic functional status: Activities of Daily Living (0 to 60) and 95% CI at baseline and 1 yr: (E1) 42.0 (39 to 45), 41.8 (38 to 45); (E2) 42.7 (39 to 46), 43.5 (40 to 47); (C) 45.0 (42 to 48) 45.6 (43 to 48); Return to work Days of sick leave and 95% CI at baseline and between 6 to 12## mo: (E1) 3.0 (‐0.5 to 6.4), 13.0 (1.2 to 24.8); (E2) 5.0 (0 to 10.0), 19.4 (3.4 to 35.3); (C) 3.0 (0.5 to 5.5), 2.6 (‐1.6 to 6.7) |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Blinding? All outcomes ‐ patients? | High risk | |
| Blinding? All outcomes ‐ providers? | High risk | |
| Blinding? All outcomes ‐ outcome assessors? | Unclear risk | Unclear from text |
| Incomplete outcome data addressed? All outcomes ‐ drop‐outs during intervention? | Low risk | |
| Incomplete outcome data addressed? All outcomes ‐ drop‐outs during follow‐up? | Low risk | |
| Incomplete outcome data addressed? All outcomes ‐ ITT analysis? | Low risk | |
| Similarity at baseline characteristics? | Low risk | |
| Co‐interventions avoided or similar? | High risk | |
| Compliance acceptable? | Low risk | |
Little 2001.
| Methods | RCT | |
| Participants | N=311; Mean age (yrs): 46; Gender (female): 57%; Diagnosis: < 3 months or exacerbation of chronic LBP (30%). Unclear whether sciatica was included. Setting: Primary Care | |
| Interventions | (E1) 'Back Home' booklet with biopsychosocial information and usual care (N=63); (E2) 'Back Home' booklet with biopsychosocial information plus advice to perform exercises‐ and usual care (N=56); (E3) Advice to perform exercises ‐ and usual care (N=61); (C) Usual care: no booklet nor exercises (N=59). | |
| Outcomes | Back pain‐specific functional status:
Pain/function score (0 to 100), mean change and 95% CI at 1 and 3 wk:
(E1) vs. (C) ‐8.7 (‐17.4 to ‐0.03) ##, ‐6.3 (‐14.6 to 2.0)
(E2) vs. (C) ‐0.1 (‐9.0 to 8.9), ‐4.0 (‐12.6 to 4.6)
(E3) vs. (C) ‐7.9 (‐16.7 to 0.8) ##, ‐1.4 (‐9.9 to 7.1) Aberdeen Pain & Function scale (0 to 100), mean change and 95% CI at 1 wk: (E1) vs. (C) ‐3.8 (‐7.7 to 0.1) ## (E2) vs. (C) ‐1.9 (‐5.8 to 2.1) (E3) vs. (C) ‐5.3 (‐9.3 to ‐1.4) ## Secondary outcomes: 'Knowledge': at 1 wk, (E1) and (E2) superior to (E3) and C (p < 0.05) 'Satisfaction with care': at 1 wk, (E1), (E2) and (E3) superior to (C) (p < 0.05) ## Significant at p < 0.05 level |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | |
| Allocation concealment? | Low risk | A ‐ Adequate |
| Blinding? All outcomes ‐ patients? | High risk | |
| Blinding? All outcomes ‐ providers? | High risk | |
| Blinding? All outcomes ‐ outcome assessors? | Low risk | |
| Incomplete outcome data addressed? All outcomes ‐ drop‐outs during intervention? | High risk | |
| Incomplete outcome data addressed? All outcomes ‐ drop‐outs during follow‐up? | High risk | |
| Incomplete outcome data addressed? All outcomes ‐ ITT analysis? | Unclear risk | Unclear from text |
| Similarity at baseline characteristics? | Unclear risk | Unclear from text |
| Co‐interventions avoided or similar? | High risk | |
| Compliance acceptable? | High risk | |
Mayer 2005.
| Methods | RCT | |
| Participants | N=100; Mean age (yrs): 31; Gender (%female): no info; Diagnosis: < 3 months LBP, unclear whether sciatica was included. Setting: 3 outpatient medical facilities | |
| Interventions | (E) Educational booklet 'acute low back problems in adults, patient guide'. Review of booklet by therapist plus advice to read booklet at home (N=26) (C1) heat wrap (5 consecutive days, 8 hours per day) (N=25) (C2) exercise under supervision of therapist, standardized full range of motion exercise plus home exercises for 5 days (N=25) (C3) heat wrap plus exercise (N=24) | |
| Outcomes | Pain:
Relief (0 to 5 verbal rating scale) at end of intervention## (graph): (E) 1.4; (C1) 2.3; (C2) 2.0; (C3) 3.4 Back pain‐specific functional status: Roland Morris (0 to 24) at baseline and end of intervention## (graph): (E) 10.78.0; (C1) 9.16.3; (C2) 9.16.7; (C3) 7.43.6 multidimensional task ability profile questionnaire (0 to 200) at baseline and end of intervention## (graph); (E) 100.5, 120; (C1) 91.9, 132; (C2)100.0, 130; (C3) 85.7, 165 (comparison (E) vs (C1) or (C2) is not clear from text) ## (E) less effective than (C3) (p < 0.05) |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Blinding? All outcomes ‐ patients? | High risk | |
| Blinding? All outcomes ‐ providers? | High risk | |
| Blinding? All outcomes ‐ outcome assessors? | Unclear risk | Unclear from text |
| Incomplete outcome data addressed? All outcomes ‐ drop‐outs during intervention? | Low risk | |
| Incomplete outcome data addressed? All outcomes ‐ drop‐outs during follow‐up? | High risk | |
| Incomplete outcome data addressed? All outcomes ‐ ITT analysis? | Unclear risk | Unclear from text |
| Similarity at baseline characteristics? | High risk | |
| Co‐interventions avoided or similar? | Low risk | |
| Compliance acceptable? | Unclear risk | Unclear from text |
Moseley 2004.
| Methods | RCT | |
| Participants | N=58; Mean age: 43; Gender (female): 57%; Diagnosis: > 6 months LBP (mean 29 mo LBP) Setting: private rehabilitation clinics | |
| Interventions | (E1) 1:1 educational session of 3 hours by physical therapist with focus on anatomy of lower back, posture and endurance (N=27) (E2) 1:1 educational session of 3 hours by physical therapist with focus on the neurosystem (N=31) | |
| Outcomes | Back pain‐specific functional status
Roland Morris (0 to 24) baseline and at end of intervention (after 15 week days after first session)##: (E1)15 (±4), 16(±3); (E2)15 (±4), 14(±3) Secondary outcomes: 'Survey of pain attitudes' at baseline and at end of intervention (after 15 weekdays after first session)## Pain catastrophizing scale at baseline and at end of intervention (after 15 weekdays after first session)## ## (E2) more effective than (E1) (P < 0.05) |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Unclear from text |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Blinding? All outcomes ‐ patients? | Low risk | |
| Blinding? All outcomes ‐ providers? | Low risk | |
| Blinding? All outcomes ‐ outcome assessors? | Unclear risk | Unclear from text |
| Incomplete outcome data addressed? All outcomes ‐ drop‐outs during intervention? | Low risk | |
| Incomplete outcome data addressed? All outcomes ‐ drop‐outs during follow‐up? | High risk | |
| Incomplete outcome data addressed? All outcomes ‐ ITT analysis? | Low risk | |
| Similarity at baseline characteristics? | Low risk | |
| Co‐interventions avoided or similar? | Unclear risk | Unclear from text |
| Compliance acceptable? | Unclear risk | Unclear from text |
Roberts 2002.
| Methods | RCT | |
| Participants | N=64; Mean age (yrs): 39.2; Gender (female): 35%; Diagnosis: acute LBP, no LBP in previous 6 months, at least 3 days of work. Unclear whether sciatica was included. Setting: Primary Care | |
| Interventions | (E) 'Back Home' booklet with biopsychosocial information and empowering statement of GP (N=35); (C) Usual care (N=28) | |
| Outcomes | Back pain specific functional status: Aberdeen Low Back Pain Scale at 2 days, 2 wk, 3 mo, 6 mo, 1 yr: (E) 42.7 (11.9), 37.7 (14.8), 14.6 (17.6), 14.7 (16.1), 11.0 (14.2); (C) 42.6 (13.6), 35.6 (15.9), 14.4 (17.6), 8.6 (10.1), 8.1 (9.6) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | |
| Allocation concealment? | High risk | C ‐ Inadequate |
| Blinding? All outcomes ‐ patients? | Unclear risk | Unclear from text |
| Blinding? All outcomes ‐ providers? | High risk | |
| Blinding? All outcomes ‐ outcome assessors? | Unclear risk | Unclear from text |
| Incomplete outcome data addressed? All outcomes ‐ drop‐outs during intervention? | Low risk | |
| Incomplete outcome data addressed? All outcomes ‐ drop‐outs during follow‐up? | High risk | |
| Incomplete outcome data addressed? All outcomes ‐ ITT analysis? | Low risk | |
| Similarity at baseline characteristics? | High risk | |
| Co‐interventions avoided or similar? | High risk | |
| Compliance acceptable? | High risk | |
Roland 1989.
| Methods | RCT | |
| Participants | N=936; Mean age (yrs): 38; Gender (female): ?%; Diagnosis: acute and chronic LBP. Unclear whether sciatica was included. Setting: Primary Care | |
| Interventions | (E) The 'Back Book': a booklet with biomedical information (N=483); (C) Usual care (N=453) | |
| Outcomes | Return to work:
Mean number of days of sickness absence at 1 yr: (E) 10.3 (?); (C) 10.1 (?) Secondary outcomes Knowledge about back pain at 1 yr: (E) superior to (C) (p < 0.05) Health care consumption at 1 yr: (E) superior to (C) (p < 0.05) |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | High risk | |
| Allocation concealment? | High risk | C ‐ Inadequate |
| Blinding? All outcomes ‐ patients? | Unclear risk | Unclear from text |
| Blinding? All outcomes ‐ providers? | High risk | |
| Blinding? All outcomes ‐ outcome assessors? | High risk | |
| Incomplete outcome data addressed? All outcomes ‐ drop‐outs during intervention? | Low risk | |
| Incomplete outcome data addressed? All outcomes ‐ drop‐outs during follow‐up? | Low risk | |
| Incomplete outcome data addressed? All outcomes ‐ ITT analysis? | Low risk | |
| Similarity at baseline characteristics? | High risk | |
| Co‐interventions avoided or similar? | Low risk | |
| Compliance acceptable? | Low risk | |
Sherman 2005.
| Methods | RCT | |
| Participants | N=101; Mean age (yrs): 44; Gender (female): 66%; Diagnosis: >12 weeks LBP, unclear whether sciatica was included. Setting: non‐profit integrated health care system | |
| Interventions | (E) Self care book ' The back pain helpbook' that emphasizes self‐care strategies (N=30) (C1) Yoga: 12 weekly 75‐minute classes, handout with home practices, auditory compact disc (N=36) (C2) Exercise: 12 weekly 75‐minute classes, handout with home practices (N=35) | |
| Outcomes | Back pain‐specific functional status:
Roland‐Morris disability score (0 to 24) at baseline, 6#, 12# and 26§ weeks (mean score differences):
(C1) vs (E) ‐ 2.6 (‐4.6 to ‐0.6), ‐3.4 (‐5.1 to ‐1.6) ‐3.6 (‐5.4 to ‐1.8)
(C2) vs (E) ‐ 1.7 (‐3.7 to 0.4), ‐1.6 (‐3.5 to 0.4), ‐2.1 (‐4.1 to 0.1) Global improvement: bothersomeness scale at baseline, 6 and 26 weeks (mean score differences): (C1) vs (E) ‐ 1.6 (‐2.6 to ‐0.5), ‐2.2 (‐3.2 to ‐1.2) (C2) vs (E) ‐ 0.9 (‐1.9 to ‐0.1), ‐0.8 (‐2.1 to 0.5) (E) less effective than (C1) at wk and 26 wk General health (SF‐36): NS (no data) |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | |
| Allocation concealment? | Low risk | A ‐ Adequate |
| Blinding? All outcomes ‐ patients? | High risk | |
| Blinding? All outcomes ‐ providers? | High risk | |
| Blinding? All outcomes ‐ outcome assessors? | Low risk | |
| Incomplete outcome data addressed? All outcomes ‐ drop‐outs during intervention? | Low risk | |
| Incomplete outcome data addressed? All outcomes ‐ drop‐outs during follow‐up? | Low risk | |
| Incomplete outcome data addressed? All outcomes ‐ ITT analysis? | Low risk | |
| Similarity at baseline characteristics? | High risk | |
| Co‐interventions avoided or similar? | High risk | |
| Compliance acceptable? | Low risk | |
Storheim 2003.
| Methods | RCT | |
| Participants | N=93; Mean age (yrs): 41, Gender (female): 52%; Diagnosis: sick listed 8 to 12 weeks LBP (sciatica was excluded). Setting: local national insurance offices and from GPs | |
| Interventions | (E) 'cognitive intervention': 2 consultations of 30 to 60 min each) with a specialist in physical medicine and a physical therapist) (N=34) (C1) intensive group exercise training: 15 weeks 3 sessions per wk of 1 hour each (aerobic fitness) (N=30) (C2) usual care by GP (N=29) | |
| Outcomes | Pain:
Intensity of pain (0 to 100 mm VAS) pre‐post (15 weeks after first session) (mean score differences):
(C1) vs (E) 6.0 (‐5.8 to 17.9)
(E) vs (C2) ‐10.9 (‐22.3 to 0.4) Back pain‐specific functional status: Roland Morris scale pre‐post (15 weeks after first session) (mean score differences)#: (C1) vs (E1).3 (‐0.5 to 3.2) (E) vs (C2) ‐1.9 (‐3.8 to ‐0.06) Generic Functional status: General Health subscale (SF‐36) pre‐post (15 weeks after first session) (mean score differences)#: (C1) vs (E1) 2 (‐8.1 to 5.7) (E) vs (C) 25.0 (‐1.5 to 11.4) Physical functioning subscale (SF‐36) pre‐post (15 weeks after first session) (mean score differences) # § (C1) vs (E) ‐6.1 (‐15.1 to 2.8) (E) vs (C) 26.6 (‐2.6 to 15.9) |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Unclear from text |
| Allocation concealment? | Low risk | A ‐ Adequate |
| Blinding? All outcomes ‐ patients? | High risk | |
| Blinding? All outcomes ‐ providers? | High risk | |
| Blinding? All outcomes ‐ outcome assessors? | Low risk | |
| Incomplete outcome data addressed? All outcomes ‐ drop‐outs during intervention? | High risk | |
| Incomplete outcome data addressed? All outcomes ‐ drop‐outs during follow‐up? | High risk | |
| Incomplete outcome data addressed? All outcomes ‐ ITT analysis? | Low risk | |
| Similarity at baseline characteristics? | High risk | |
| Co‐interventions avoided or similar? | Unclear risk | Unclear from text |
| Compliance acceptable? | Low risk | |
Wand 2004.
| Methods | RCT | |
| Participants | N=102; Mean age (yrs): 35; Gender (female): 60%; Diagnosis: <6 wks LBP, Unclear whether sciatica was included; Setting: local national insurance offices and from GPs | |
| Interventions | (E) 'assess‐advise‐wait' ‐ advise to stay active (N=51) (C) 'assess‐advise‐treat' ‐ biopsychosocial education, manual therapy, exercise (no information on frequency and duration of sessions and on health care providers) (N=43) | |
| Outcomes | Pain:
Usual pain (0‐10 VAS) at baseline and 6 wks. (E) 5.2 (2.4), 3.3 (2.5); (C) 5.8 (2.1), 2.4 (2.0) Back pain‐specific functional status: Roland Morris scale at baseline and 6 wks. (E) 10.1 (6.2), 6.3 (5.9); (C) 12.7 (6.0), 4.5 (4.5) Generic Functional status: Generic Health Questionnaire (EuroQol) at baseline and 6 wks. (E) 1.1 (0.7), 0.7 (0.3); (C) 1.4 (0.7), 0.8 (0.1) General Health subscale (SF‐36) at baseline and 6 wks.(E) 81.5 (18.8), 77 (19); (C) 87.0 (12.1), 89 (13) Physical functioning subscale (SF‐36) at baseline and 6 wks.(E) 66 (25.5), 75 (19); (C) 59 (25.4), 78 (19) |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | |
| Allocation concealment? | Low risk | A ‐ Adequate |
| Blinding? All outcomes ‐ patients? | Unclear risk | Unclear from text |
| Blinding? All outcomes ‐ providers? | High risk | |
| Blinding? All outcomes ‐ outcome assessors? | Unclear risk | Unclear from text |
| Incomplete outcome data addressed? All outcomes ‐ drop‐outs during intervention? | High risk | |
| Incomplete outcome data addressed? All outcomes ‐ drop‐outs during follow‐up? | High risk | |
| Incomplete outcome data addressed? All outcomes ‐ ITT analysis? | Low risk | |
| Similarity at baseline characteristics? | Unclear risk | Unclear from text |
| Co‐interventions avoided or similar? | Unclear risk | Unclear from text |
| Compliance acceptable? | Unclear risk | Unclear from text |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Fleten 2006 | No backpain‐specific education. |
| Friedrich 1996 | No individual patient education, but instructions for exercises. |
| Harkäpää 1989 | Insufficient contrast for individual patient education |
| Hartvigsen 2005 | No individual patient education but group invention |
| Niemisto 2003 | Insufficient contrast for individual patient education |
Contributions of authors
P. Jellema and A. Engers: Writing the body of the review, literature search, screening trials for inclusion, methodological quality assessment, data extraction and data analysis.
M. van Tulder, M. Wensing and D. vander Windt : editing and contributing to the body of the protocol and review; final decision in inclusion of studies and consensus of quality assessment; commenting on final draft of the review.
R Grol: commenting on final draft of the review.
Sources of support
Internal sources
Centre for Quality of Care Research, University medical centre Nijmegen, Netherlands.
EMGO Institute, VU University Medical Centre, Amsterdam, Netherlands.
External sources
Ministry of Health, Netherlands.
Declarations of interest
A study of one of the authors (PJ) was included in this review. For this particular study the quality assessment was done by MvT and AE. She was not involved in any decision regarding selection, quality assessment and data extraction of this study. One author (Maurits van Tulder) is co‐ordinating editor of the Cochrane Back Review Group. Editors are required to conduct at least one Cochrane review. This requirement ensures that editors are aware of the processes and commitment needed to conduct reviews. None of the editors are first authors. This involvement does not seem to be a source of conflict of interest in the Cochrane Back Review Group. Any editor who is a review author is excluded from editorial decisions on the review in which they are contributors.
Edited (no change to conclusions)
References
References to studies included in this review
Burton 1999 {published data only}
- Burton AK, Waddell G, Burtt R, Blair S. Patient education material in the management of low back pain in primary care. Bulletin of Hospital Jt Dis 1996;55:138‐41. [PubMed] [Google Scholar]
Cherkin 1996 {published data only}
- Cherkin DC, Deyo RA, Street JH, Hunt M, Barlow W. Pitfalls of patient education. Limited success of a program for back pain in primary care. Spine 1996;21:345‐55. [DOI] [PubMed] [Google Scholar]
Cherkin 1998 {published data only}
- Cherkin DC, Deyo RA, Battie M, Street J, Barlow W. A comparison of physical therapy, chiropractic manipulation, and provision of an educational booklet for the treatment of patients with low back pain. N Engl J Med 1998;339:1021‐9. [DOI] [PubMed] [Google Scholar]
Cherkin 2001 {published data only}
- Cherkin DC, Eisenberg D, Sherman KJ, Barlow W, Kaptchuk TJ, Street J, et al. Randomized trial comparing traditional Chinese medical acupuncture, therapeutic massage, and self‐care education for chronic low back pain. Arch Intern Med 2001;161:1081‐8. [DOI] [PubMed] [Google Scholar]
Deyo 1987 {published data only}
- Deyo RA, Diehl AK, Rosenthal M. Reducing roentgenography use: can patient expectations be altered?. Arch Int Med 1987;147:141‐5. [DOI] [PubMed] [Google Scholar]
Frost 2004 {published data only}
- Frost H, Lamb SE, Doll HA, Carver PT, Stewart‐Brown S. Randomised controlled trial of physiotherapy compared with advice for low back pain. BMJ 2004;329(7468):708. [DOI] [PMC free article] [PubMed] [Google Scholar]
Goldby 2006 {published data only}
- Goldby LJ, Moore AP, Doust J, Trew ME. A randomised controlled trial investigating the efficiency of musculoskeletal fysiotherapie on chronic low back disorder. Spine 2006;31:1083‐93. [DOI] [PubMed] [Google Scholar]
Hagen 2003 {published data only}
- Hagen EM, Eriksen HR, Ursin H. Does early intervention with a light mobilization program reduce long‐term sick leave for low back pain?. Spine 2000;25:1973‐6. [DOI] [PubMed] [Google Scholar]
- Hagen EM, Grasdal A, Eriksen HR. Does early intervention with a light mobilization program reduce long‐term sick leave for low back pain? A 3‐year follow‐up study. Spine 2003;28:2309‐16. [DOI] [PubMed] [Google Scholar]
Hazard 2000 {published data only}
- Hazard RG, Reid S, Haugh LD, McFarlane G. A controlled trial of an educational pamphlet to prevent disability after occupational low back injury. Spine 2000;25:1419‐23. [DOI] [PubMed] [Google Scholar]
Hurley 2001 {published data only}
- Hurley DA, Minder PM, McDonough S, Walsh DM, Moore AP, Baxter D. Interferential therapy electrode placement technique in acute low back pain: a prelimary investigation. Arch Phys Med Rehab 2001;82:485‐93. [DOI] [PubMed] [Google Scholar]
Hurri 1989 {published data only}
- Hurri H. The Swedish back school in chronic low back pain, Part I: benefits. Scand J Rehab Med 1989;21:33‐40. [PubMed] [Google Scholar]
Indahl 1995 {published data only}
- Indahl A, Velund L, Reikeraas O. Good prognosis for low back pain when left untampered: a randomised clinical trial. Spine 1995;20:473‐7. [DOI] [PubMed] [Google Scholar]
Jackson 1994 {published data only}
- Jackson LD. Maximizing treatment adherence among back‐pain patients: an experimental study of the effects of physician‐related cues in written medical messages. Health communication 1994;6:173‐91. [Google Scholar]
Jellema 2005 {published data only}
- Jellema P, Windt DAWM, Horst HE, Twisk JWR, Stalman WAB, Bouter LM. Should treatment of (sub)acute low back pain be aimed at psychosocial prognostic factors? Cluster randomised clinical trial in general practice. BMJ 2005;331(7508):84. [DOI] [PMC free article] [PubMed] [Google Scholar]
Karjalainen 2004 {published data only}
- Karjalainen K, Malmivaara A, Mutanen P, Roine R, Hurri H, Pohjolainen T. Mini‐intervention for subacute low back pain: two‐year follow‐up and modifiers of effectiveness. Spine 2004;29:1069‐76. [DOI] [PubMed] [Google Scholar]
- Karjalainen K, Malmivaara A, Pohjolainen T, Hurri H, Mutanen P, Rissanen P, Pahkajarvi H, Levon H, Karpoff H, Roine R. Mini‐intervention for subacute low back pain: a randomized controlled trial. Spine 2003;28:533‐40. [DOI] [PubMed] [Google Scholar]
Linton 2000 {published data only}
- Linton SJ, Andersson T. Can chronic disability be prevented? A randomized trial of a cognitive‐ behavior intervention and two forms of information for patients with spinal pain. Spine 2000;25:2825‐31. [DOI] [PubMed] [Google Scholar]
Little 2001 {published data only}
- Little P, Roberts L, Blowers H, et al. Should we give detailed advice and information booklets to patients with back pain? A randomized controlled factorial trial of a self‐management booklet and doctor advice to take exercise for back pain. Spine 2001;26:2065‐72. [DOI] [PubMed] [Google Scholar]
Mayer 2005 {published data only}
- Mayer JM, Ralph L, Look M, Erasala GN, Verna JL, Matheson LN, et al. Treating acute low back pain with continuous low‐level heat wrap therapy and/or exercise: a randomized controlled trial. The Spine Journal 2005;5:395‐403. [DOI] [PubMed] [Google Scholar]
Moseley 2004 {published data only}
- Moseley GL, Nicholas MK, Hodges PW. A controlled trial of intensive neurophysiology education in chronic low back pain. Clin J Pain 2004;20:324‐30. [DOI] [PubMed] [Google Scholar]
Roberts 2002 {published data only}
- Roberts L, Little P, Chapman J, Cantrell T, Pickering R, Langridge J. The Back home trial; General practitioner‐supported leaflets may change back pain behavior. Spine 2002;27:1821‐8. [DOI] [PubMed] [Google Scholar]
Roland 1989 {published data only}
- Roland M, Dixon M. Randomized controlled trial of an educational booklet for patients presenting with back pain in general practice. Journal of the Royal College of General Practitioners 1989;39:244‐6. [PMC free article] [PubMed] [Google Scholar]
Sherman 2005 {published data only}
- Sherman KJ, Cherkin DC, Erro J, Miglioretti DL, Deyo R. Comparing yoga, exercise and a self‐care book for low back pain: a randomized cltrolled trial. Ann Intern Med 2005;143:849‐56. [DOI] [PubMed] [Google Scholar]
Storheim 2003 {published data only}
- Storheim K, Brox JI, Holm I, Koller AK, Bø K. Intensive group training versus cognitive intervention in sub‐acute low back pain: short‐term results of a single‐blind randomised controlled trial. J Rehabil Med 2003;35:132‐40. [DOI] [PubMed] [Google Scholar]
Wand 2004 {published data only}
- Wand BM, Bird C, McAuley JH, Doré CJ, MacDowell M, Souza LH. Early intervention for the management of acute low back pain: a single‐blind randomised controlled trial of biopsychosocial education, manual therapie and exercise. Spine 2004;29:2350‐6. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Fleten 2006 {published data only}
- Fleten N, Johnsen R. Reducing sick leave by minimal postal intervention: a randomised, controlledintervention study. Occup Environ Med 2006;63:676‐82. [DOI] [PMC free article] [PubMed] [Google Scholar]
Friedrich 1996 {published data only}
- Friedrich M, Cermak T, Maderbacher P. The effect of brochure use versus therapist teaching on patients performing therapeutic exercise and on changes in impairment status. Physical Ther 1996;76:1082‐8. [DOI] [PubMed] [Google Scholar]
Harkäpää 1989 {published data only}
- Härkäpää K, Järvikoski A, Mellin G, Hurri H. A controlled study of the outcome of inpatient and outpatient treatment of low back pain. Scand J Rehab Med 1989;21(2):81‐9. [PubMed] [Google Scholar]
Hartvigsen 2005 {published data only}
- Hartvigsen J, Lauritzen S, Lings S, Lauritzen T. Intensive education combined with low tech ergonomic intervention does not preventlow back pain in nurses. Occup Environ Med 2005;62:13‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Niemisto 2003 {published data only}
- Niemisto L, Lahtinen‐Suopanki T, Rissanen P, Lindgren KA, Sarna S, Hurri H. A randomized trial of combined manipulation, stabilizing exercises, and physsician consultation compared to physician consultation alone for chronic low back pain. Spine 2003;28:285‐91. [DOI] [PubMed] [Google Scholar]
References to studies awaiting assessment
Donzelli 2006 {published data only}
- Donzelli S, Domenica F, Cova AM, Giunta N. Two different rechniques in the rehabilitation treatment of low back pain: a randomized controlled trial. Europa medicophysica 2006;42:205‐10. [PubMed] [Google Scholar]
Frost 2007 {published data only}
- Frost H, Haahr P, Andersen JH. Reduction of pain‐related disability in working populations: a randomized intervention study of the effects of an educational booklet addressing psychosocial risk factors and screening workplaces for physical health hazards. Spine 2007;32:1949‐54. [DOI] [PubMed] [Google Scholar]
Gohner 2006 {published data only}
- Göhner W, Schlicht W. Preventing chronic back pain: evaluation of a theory‐based cognitive behavioural training programme for patients with subacute back pain. Patient education and counseling 2006;64:87‐95. [DOI] [PubMed] [Google Scholar]
Linton 2006 {published data only}
- Linon SJ, Nodin E. A 5‐year follow‐up evaluation of the health and economic consequences of an early cognitive behavioral intervention for back pain: a randomized controlled trial. Spine 2006;31:853‐8. [DOI] [PubMed] [Google Scholar]
Oleske 2007 {published data only}
- Oleske DM, Lavender SA, Andersson GB, Kwasny MM. Ae back supports plus education more effective than education alone in promoting recovery from low back pain?. Spine 2007;32:2050‐7. [DOI] [PubMed] [Google Scholar]
Pengel 2007 {published data only}
- Pengel LHM, Refshauge KM, Maher CG, Nicholas MK, Hebet D, McNair P. Physiotherapist‐directed exercise, advice, or both for subacute low back pain: a randomized rial. Annals of Internal medicine 2007;146:787‐96. [DOI] [PubMed] [Google Scholar]
Additional references
AHCPR 1994
- Agency for Health Care Policy and Research. Understanding low back problems: Consumer version; Clinical practice guideline Number 14. Publication no. 95‐0644: Agency for Health Care Policy and Research, Public Health Service, U.S. Department of Health and Human Services 1994; Vol. December.
Ajzen 1991
- Ajzen I. The theory of planned behavior. Organizational behavrior and human dicision processes 1991;50:179‐211. [Google Scholar]
Back Book 1997
- Roland M, Waddell G, Klaber Moffett J, Burton K, Main C, Cantrell T. The Back Book. Clinical Guidelines for the management of acute low back pain, Royal College of General Practitioners. London: Stationery Office, 1997.
Bendix 1998
- Bendix T, Bendix AF, Labriola M, Boekgaard P. Functional restoration for chronic low back pain: rwo year follow‐up of two randomized clinical trials. Spine 1998;19:787‐805. [DOI] [PubMed] [Google Scholar]
Bergner 1981
- Bergner M, Bobbitt RA, Carter WB, Gilson BS. The Sickness Impact Profile: development and final revision of a health status measure. Med Care 1981;19:787‐805. [DOI] [PubMed] [Google Scholar]
Burton 1996
- Burton Ak, Wadell G, Burtt R, Blair S. Patient education material in the management of low back pain in primary care. Bulletin of Hospital Jt Dis 1996;55:138‐41. [PubMed] [Google Scholar]
Fairbank 2000
- Fairbank JC, Pynsent PB. The Oswestry Disability Index. Spine 2000;25:2940‐53. [DOI] [PubMed] [Google Scholar]
Heymans 2004
- Heymans MW, Tulder MW, Esmail R, Bombardier C, Koes BW. Back schools for non‐specific low‐back pain. Cochrane Database of Systematic Reviews 2004, Issue 4. [Art. No.: CD000261. DOI: 10.1002/14651858.CD000261.pub2] [DOI] [PubMed] [Google Scholar]
Hilde 2002
- Hilde G, Hagen KB, Jamtvedt G, Winnem M. Advice to stay active as a single treatment for low‐back pain and sciatica. Cochrane Database of Systematic Reviews 2002, Issue 2. [Art. No.: CD003632. DOI: 10.1002/14651858.CD003632] [DOI] [PubMed] [Google Scholar]
Malmivaara 1996
- Malmivaara A, Pohjolainen T. Selkakipuisen Kasikirja [in Finnish]. Suomen Selkalitto, 1996. [Google Scholar]
Maniadakis 2000
- Maniadakis N, Gray A. The economic burden of back pain in the UK. Pain 2000;84:95‐103. [DOI] [PubMed] [Google Scholar]
Moher 2000
- Moher D, Pham B, Klassen TP, et al. What contributions do languages other the English make on the results of meta‐analysis?. J Clin Elidemiol 2000;53:964‐72. [DOI] [PubMed] [Google Scholar]
Nordin 1995
- Nordin M. Back pain: lessons from patient education. Patient education and counseling 1995;26(1‐3):67‐70. [DOI] [PubMed] [Google Scholar]
Ostelo 2005
- Ostelo RWJG, Tulder MW, Vlaeyen JWS, Linton SJ, Morley SJ, Assendelft WJJ. Behavioural treatment for chronic low‐back pain. Cochrane Database of Systematic Reviews 2005, Issue 1. [Art. No.: CD002014. DOI: 10.1002/14651858.CD002014.pub2] [DOI] [PubMed] [Google Scholar]
Patrick 1995
- Patrick DL, Deyo RA, Atlas SJ, Singer DE, Chapin A, Keller RB. Assessing health‐related quality of life in patients with sciatica. Spine 1995;20:1899‐1909. [DOI] [PubMed] [Google Scholar]
Prochaska 1984
- Prochaska JO, DiClemente CC. The transtheoretical approach: crossing traditional boundaries of therapy. Homewood IL: Dow Jones‐Irwin, 1984. [Google Scholar]
Roland 1983
- Roland M, Morris R. A study of the natural history of back pain. Part I: development of a reliable and sensitive measure of disability in low‐back pain. Spine 1983;8:141‐4. [DOI] [PubMed] [Google Scholar]
Symonds 1995
- Symonds TL, Burton AK, Tillotson KM, Main CJ. Absence resulting from low back trouble can be reduced by psychosocial intervention at the work place. Spine 1995;20:2738‐45. [DOI] [PubMed] [Google Scholar]
Tones 1991
- Tones K, Tilford S, Robinson T. Health education: effectiveness and efficiency. London: Chapman and Hall, 1991. [Google Scholar]
Turk 1993
- Turk DC, Zaki HS, Rudy TE. Effects of intra‐oral appliance and biofeedback/stress management alone and in combination in reating pain and depression in patients with temporomandibular disorders. J Prosthet Dent 1993;70:158‐64. [DOI] [PubMed] [Google Scholar]
Van Agt 1994
- Agt HME, Essinck‐Bot ML, Krabbe PFM, Bonsel GJ. Test‐retest reliability of the health state valuations collected with the EuroQol questionnaire. Soc Sci Med 1994;39:1537‐44. [DOI] [PubMed] [Google Scholar]
Van den Borne 1998
- Borne HW. The patient from receiver of information to informed decision‐maker. Patient Education and Counseling 1998;34(2):89‐102. [DOI] [PubMed] [Google Scholar]
Van Tulder 1995
- Tulder MW van, Koes BW, Bouter LM. A cost‐of‐illness study of back pain in the Netherlands. Pain 1995;62:233‐40. [DOI] [PubMed] [Google Scholar]
van Tulder 2003
- Tulder MW, Furlan A, Bombadier C, Bouter LM, Editorial Board of the Cochrane Collaboration Back Review Group. Updated method guidelines for systematic reviews in the Cochrane Collaboration Back Review Group. Spine 2003;28:1290‐9. [DOI] [PubMed] [Google Scholar]
Waddell 1987
- Waddell G. A new clinical model for the treatment of low‐back pain. Spine 1987;12:632‐44. [DOI] [PubMed] [Google Scholar]
Waddell 1997
- Waddell G, Feder G, Lewis M. Systematic reviews of bed rest and advice to stay active for acute low back pain. Br J Gen Pract 1997;47:647‐52. [PMC free article] [PubMed] [Google Scholar]
Ware 1992
- Ware JE, Sherbourne CD. The MOS 36‐item short form health survey (SF‐36). Med Care 1992;30:473‐83. [PubMed] [Google Scholar]


