ABSTRACT
Homonymous hemianopia is frequently associated with retrochiasmal lesions. Vascular etiology is the most common and usually evident on magnetic resonance imaging. When the results of neuroimaging are normal, there are other etiologies that we should consider, like nonketotic hyperglycemia (NKH). We report a 62-year-old female diabetic patient with headache, colour vision and sudden homonymous inferior quadrantanopia and elevated blood sugar levels with normal pH. The neuroimaging was normal and the visual lost improved after the correction of the hyperglycemia. NKH should be considered in patients with sudden and transient hemianopia and normal neuroimaging.
KEYWORDS: Homonymous hemianopia, quadrantanopia, visual field defects, nonketotic hyperglycemia, Todd’s phenomenon
Introduction
Homonymous hemianopia (HH) is frequently associated with retrochiasmal lesions that can affect the right optic tract, lateral geniculate nucleus, optic radiations, or visual cortex. The onset of symptoms guides us between different causes. When there is an acute onset, we should suspect first vascular etiologies, including ischemic or haemorrhagic stroke, venous sinus thrombosis with infarct, or reversible posterior leukoencephalopathy syndrome. The most common etiology can be objectified by abnormalities in magnetic resonance imaging (MRI) of the brain or on other neuroimaging studies. However, there are other etiologies that cause functional HH with normal neuroimaging and we must take in account. Temporary HH with spontaneous recovery may occur due to anaemia, migraine, MELAS (mitochondrial myopathy, encephalopathy, lactic acidosis, and strokelike episodes), occipital, parietal or temporal lobe seizures or transient ischemic attack. Nonketotic hyperglycemia (NKH) can cause HH that resolves with normalization of the blood sugar.1
We report a case of a reversible left inferior homonymous quadrantanopia, positive visual phenomena, and normal neuroimaging in a patient with NKH.
Case report
A 62 year-old woman with a history of diabetes mellitus type 2 with poor glycaemic control (last glycated haemoglobin 13,3%), arterial hypertension, apnea-hypopnea syndrome, atrial fibrillation, hypothyroidism, and rheumatoid arthritis, comes to the emergency room complaining of headache, colour lights and flashes over several days, followed from a sudden deficit of the left visual field. She started taking prednisone 20 mg 3 weeks before for eczema. The blood test shows elevated blood sugar (623 mg/dL) with a normal pH. The confrontation visual field reveals a left HH, the rest of the neurological examination is normal. The ophthalmological examination shows a normal intraocular pressure and a posterior vitreous detachment on the left eye. The Humphrey visual field analysis confirms the left inferior homonymous quadrantanopia with macular sparing (Figure 1). Cranial MRI is unremarkable, and the 18F-fluorodeoxyglucose positron emission tomography/computed tomography shows general hypometabolism in cortex, probably related with hyperglycaemia, without perfusion defects (Figure 2). When the blood sugar is in normal value ranges, the patient progressively initiates a clear clinical improvement with the practical resolution of the visual deficit (Figure 3).
Figure 1.
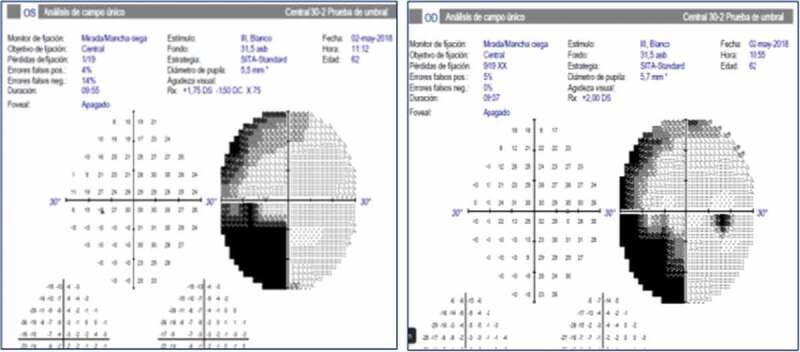
Humphrey visual field analysis shows left inferior homonymous quadrantanopia with macular sparing. The first image starting from the left eye and the second to the right eye.
Figure 2.
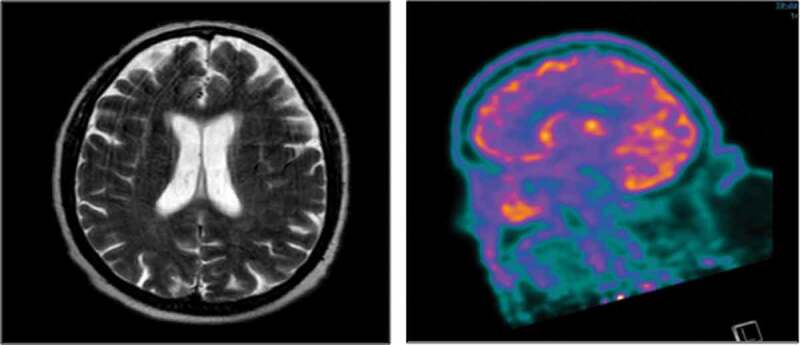
A Normal axial magnetic resonance image of the brain, T2-weighted. B. Coronal image of postron- emission tomography with general hypometabolism, without perfusion defects.
Figure 3.
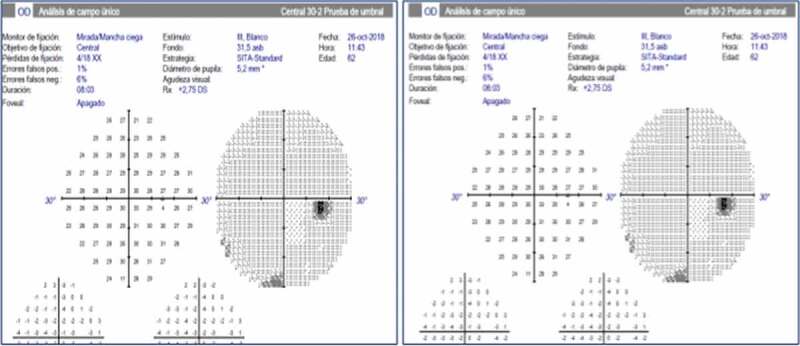
Humphrey visual field analysis shows the complete resolution of the visual deficit.
Discussion
Several neurological manifestations have been described due to NKH, like hemiparesis (stroke mimic), hemichorea - hemiballismus, hemianopia, coma and visual positive, and negative phenomena.1 The physiopathology of these symptoms is multifactorial. High blood sugar levels cause hyperosmolarity and intracellular dehydration, an increase in free radicals production and changes in neurotransmitter function, especially a decrease in the inhibition of gamma-aminobutyric acid. Moreover, there are focal changes in either the arterial or venous circulation induced by sludging or thrombosis during the acute illness, which explains why most symptoms are partial. In patients with DM, sympathetic dysautonomia also plays a role. The function of sympathetic nerve innervation is increasing cerebral vascular tone in response to acute changes in cerebral hemodynamics. The less sympathetic innervation of the posterior circulation results in clinical posterior predominance.1
HH can associate abnormalities in brain MRI or not.2 When they are present, the most common findings were decreased T2 signal of the white matter (due to hyperosmolarity moves fluids outside the cell), subtle gyral swelling, enhancement of the overlying meninges and restricted diffusion, predominantly in the posterior hemisphere opposite the hemianopia. These findings were reversible and not typical of those seen with partial seizures by other cause, where the typical findings include hyperintensity in grey and subcortical white matter on T2 and fluid-attenuated inversion recovery sequences attributed to oedema or gliosis.3 Functional imaging techniques, such as SPECT or PET, or diffusion/perfusion MRI should therefore be considered in patients with suspected cortical visual loss and normal results on CT or MR studies.2 The FDG PET findings in patients with NKH have been described in the past. 18F-FDG PET/CT study was subsequently performed in our patient and showed diffuse general hypometabolism in cortex.4,5 The hypometabolism observed on 18F-FDG PET/CT suggests that hypofunction is a possible common pathogenetic pathway in the development of quadrantanopia.
The prevalence of seizures is different in the literature; it goes from 25%6 to 40% of people with NKH.7 Motor seizures, like hemichorea - hemiballismus, are often recognized. The opposite occurs with nonmotor seizures, like apnea, aphasia, somatosensory symptoms and visual disturbance.7 Positive visual phenomena include reports of polyopia, flashing and flickering lights, hallucinations, and a persistence and transposition of objects in the visual fields.8 But the persistent hemianopia in these patients with normal neuroimaging may represent a postictal negative Todd’s visual phenomenon3, like patient we reported here. Seizure-induced blindness or hemianopia may be ictal or postictal (Todd’s phenomenon) visual occipital phenomenon or a permanent consequence following status epilepticus. There does not seem to be a clinical difference between patients with and those without occipital lesions.9,10
There are few reports in the literature with similar clinical characteristics to ours. Taban et al., report eight cases with visual hallucinations as the main symptom. These, can appear in patients with known DM or as disease’s debut. The imaging of the brain is normal in all of them. The mechanism is not completely understood but may represent ictal or postictal inhibition. The electroencephalogram (EEG) is not always made, however, when it is realized it shows ictal irregular waves in occipital lobe. In our patient we did not make an EEG, which could have provided useful information about the mechanism of her visual phenomena. All the symptoms resolved within days of controlling the blood glucose level.6 Damage to the occipital lobe usually does not produce other neurologic manifestations, although some patients may experience photopsias or other hallucinations in the blind hemifield. Our report is similar to the few cases described in the literature, with the singularity that the visual defect is a homonymous quadrantanopia instead of hemianopia. That presupposes a dysfunction of the occipital or parietal lobe; nevertheless, the macular sparing is concordant with occipital dysfunction. Involving of vascularity and posterior predominance, may contribute to observe hemianopia with sparing macula, which is congruent with other case report in the literature. 1,11 This can be explain by bilateral representation of the macula in the occipital cortex, incomplete damage to the striate cortex on the affected side, and, more commonly, dual blood supply of the occipital pole by middle and posterior cerebral arteries.12
In conclusion, NKH should be considered in patients with HH, positive visual phenomena, and negative neuroimaging studies. Although the mechanism of HH is not completely understood may represent ictal or postictal inhibition negative Todd’s visual phenomenon.
Conflict of interests
Regarding this presentation, there are no relationships that can be perceived as potential conflicts of interest. The intervention that I submit has NOT been financed, totally or partially, by any company with economic interests in the products, equipment or similar mentioned in it.
References
- 1.Strowd RE, Wabnitz A, Balakrishnan N, Craig J, Tegeler CH.. Clinical reasoning: acute-onset homonymous hemianopia with hyperglycemia: seeing is believing. Neurology. 2014;82(15):e129–33. doi: 10.1212/WNL.0000000000000308. [DOI] [PubMed] [Google Scholar]
- 2.Brazis PW, Lee AG, Graff-Radford N, Desai NP, Eggenberger ER. Homonymous visual field defects in patients without corresponding structural lesions on neuroimaging. J Neuroophthalmol. 2000;20(02):92–96. [DOI] [PubMed] [Google Scholar]
- 3.Lavin PJ. Hyperglycemic hemianopia: a reversible complication of non-ketotic hyperglycemia. Neurology. 2005;65(4):616–619. doi: 10.1212/01.wnl.0000173064.80826.b8. [DOI] [PubMed] [Google Scholar]
- 4.D’souza MM, Sharma R, Jaimini A, Mondal A, Tripathi RP. 18F-fluorodeoxyglucose positron emission tomography/computed tomography in a case of non-ketotic hyperglycemia. Indian J Nucl Med. 2014;29(4):254–256. doi: 10.4103/0972-3919.142633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nguyen BD. Brain and upper extremity PET/CT findings of hyperglycemia-induced hemiballism-hemichorea. Clin Nucl Med. 2007;32:643–645. doi: 10.1097/RLU.0b013e3180a1acb0. [DOI] [PubMed] [Google Scholar]
- 6.Taban M, Naugle RI, Lee MS. Transient homonymous hemianopia and positive visual phenomena in patients with nonketotic hyperglycemia. Arch Ophthalmol. 2007;125(6):845–847. doi: 10.1001/archopht.125.6.845. [DOI] [PubMed] [Google Scholar]
- 7.Mitchell JP, Yancy A, Saint Louis L, Rosberger DF. Reversible hyperglycemic homonymous hemianopia. J Natl Med Assoc. 2009;101(4):373–376. [DOI] [PubMed] [Google Scholar]
- 8.Freedman KA, Polepalle S. Transient homonymous hemianopia and positive visual phenomena in nonketotic hyperglycemic patients. Am J Ophthalmol. 2004;137(6):1122–1124. doi: 10.1016/j.ajo.2003.11.067. [DOI] [PubMed] [Google Scholar]
- 9.Joseph JM, Louis S. Transient ictal cortical blindness during middle age. A case report and review of the literature. J Neuroophthalmol. 1995;15(1):39–42. [PubMed] [Google Scholar]
- 10.Theodore WH. The postictal state: effects of age and underlying brain dysfunction. Epilepsy Behav. 2010;19(2):118–120. doi: 10.1016/j.yebeh.2010.06.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ghosh P, Motamedi G, Osborne B, Mora CA. Reversible blindness: simple partial seizures presenting as ictal and postictal hemianopsia. J Neuroophthalmol. 2010;30(3):272–275. doi: 10.1097/WNO.0b013e3181e05340. [DOI] [PubMed] [Google Scholar]
- 12.Liu GT, Volpe NJ, Galetta SL. Retrochiasmal disorders. In: Gt L, Volpe NJ, Galetta SL, eds. Neuro-Ophthalmology: Diagnosis and Management. Philadelphia: W.B. Saunders; 2001:296. [Google Scholar]


