Abstract
Background
Structured antenatal education programs for childbirth or parenthood, or both, are commonly recommended for pregnant women and their partners by healthcare professionals in many parts of the world. Such programs are usually offered to groups but may be offered to individuals.
Objectives
To assess the effects of this education on knowledge acquisition, anxiety, sense of control, pain, labour and birth support, breastfeeding, infant‐care abilities, and psychological and social adjustment.
Search methods
We searched the Cochrane Pregnancy and Childbirth Group's Trials Register (April 2006), CINAHL (1982 to April 2006), ERIC (1984 to April 2006), EMBASE (1980 to April 2006) and PsycINFO (1988 to April 2006). We handsearched the Journal of Psychosomatic Research from 1956 to April 2006 and reviewed the reference lists of retrieved studies. We updated the search of the Cochrane Pregnancy and Childbirth Group's Trials Register on 7 July 2011 and added the results to the awaiting classification section of the review.
Selection criteria
Randomized controlled trials of any structured educational program provided during pregnancy by an educator to either parent that included information related to pregnancy, birth or parenthood. The educational interventions could have been provided on an individual or group basis. Educational interventions directed exclusively to either increasing breastfeeding success, knowledge of and coping skills concerning postpartum depression, improving maternal psycho‐social health including anxiety, depression and self‐esteem or reducing smoking were excluded.
Data collection and analysis
Both authors assessed trial quality and extracted data from published reports.
Main results
Nine trials, involving 2284 women, were included. Thirty‐seven studies were excluded. Educational interventions were the focus of eight of the studies (combined n = 1009). Details of the randomization procedure, allocation concealment, and/or participant accrual or loss for these trials were not reported. No consistent results were found. Sample sizes were very small to moderate, ranging from 10 to 318. No data were reported concerning anxiety, breastfeeding success, or general social support. Knowledge acquisition, sense of control, factors related to infant‐care competencies, and some labour and birth outcomes were measured. The largest of the included studies (n = 1275) examined an educational and social support intervention to increase vaginal birth after caesarean section. This high‐quality study showed similar rates of vaginal birth after caesarean section in 'verbal' and 'document' groups (relative risk 1.08, 95% confidence interval 0.97 to 1.21).
Authors' conclusions
The effects of general antenatal education for childbirth or parenthood, or both, remain largely unknown. Individualized prenatal education directed toward avoidance of a repeat caesarean birth does not increase the rate of vaginal birth after caesarean section.
[Note: the 58 citations in the awaiting classification section may alter the conclusions of the review once assessed.]
Plain language summary
Individual or group antenatal education for childbirth or parenthood, or both
Benefits of antenatal education for childbirth, and the best educational approaches to use, remain unclear.
Antenatal education aims to help prospective parents prepare for childbirth and parenthood. Prospective parents often look to antenatal education to provide important information on issues such as decision making about and during labour, skills for labour, pain relief, infant and postnatal care, breastfeeding and parenting skills. There are many varied ways of providing this antenatal education and some may be more effective than others. The review found nine trials involving 2284 women. Interventions varied greatly and no consistent outcomes were measured. The review of trials found a lack of high‐quality evidence from trials and so the effects of antenatal education remain largely unknown. Further research is required to ensure that effective ways of helping health professionals support pregnant women and their partners in preparing for birth and parenting are investigated so that the resources used meet the needs of parents and their newborn infants.
Background
Extent of implementation of antenatal education
Antenatal education classes, including 'childbirth education programs', 'prenatal classes', and antenatal groups are attended by an important percentage of pregnant women worldwide. Reports can be found of programs based in the US, the UK, Canada, Mexico, Brazil, Finland, Germany, Australia, Japan, and China, to name a few. Many maternity providers, including public health departments, hospitals, private agencies and charities, and some obstetricians' and midwives' practices, are reported to provide antenatal education. In other parts of the world, antenatal preparation is still less of a formality and knowledge of the birth experience and care of children is passed from mothers to daughters or from traditional birth attendants to those in their care. Living arrangements in which several generations share common space also lend themselves to active participation in the experience of birth and consequently there may be no defined need for structured antenatal education. The existence of structured education in preparation for childbirth and parenthood has come about as traditional methods of information sharing have declined. Typically these programs have not been based on the expressed needs of attendees, but rather on the messages that the educators themselves believed they should impart.
Goals and content of antenatal education
Antenatal education programs often have a range of aims, such as to: influence health behaviour; build women's confidence in their ability to give birth; prepare women and their partners for childbirth; prepare for parenthood; develop social support networks; promote confident parents; and contribute to reducing perinatal morbidity and mortality. Antenatal education thus comprises a range of educational and supportive measures that help parents and prospective parents to understand their own social, emotional, psychological, and physical needs during pregnancy, labour, and parenthood.
Theoretical approaches to antenatal education
Common approaches which were identified in the early literature on this topic were 'natural childbirth' (Dick‐Read 1933) and psychoprophylaxis (Lamaze 1958) methods. The similarity of these two techniques is their emphasis on a healthy pregnancy, physical fitness, education on the physiology of normal birth, elimination of fear during labour, use of relaxation and breathing techniques, and continuous support by a familiar person. These two approaches have experienced relative degrees of popularity in North America and Europe since their inception. Tenets from these approaches still form the basis of many childbirth education programs today (Lothian 2005). Within the last two decades, an approach called 'Active Birth' has enjoyed and continues to enjoy some popularity (Balaskas 1992), and latterly 'hypnobirth', which teaches self‐hypnosis, relaxation, and breathing techniques (Mongan 2005). The essence of these approaches lies in helping mothers to identify and develop their own bodily resources for birth. It is meant to empower women through the birth experience. The choice of these and other approaches have largely been thought to be reflective of the nature of the agency sponsoring the educational program.
Reasons for participating in antenatal education
Regardless of the theoretical perspective, the question arises as to whether what is taught in classes meets the needs of attendees (Nolan 1997a; Nolan 1997b). In a survey of those planning to attend independent (private) childbirth education classes in Montreal, women reported that their main reason for attending childbirth classes was to reduce their anxiety about labour and birth (Gagnon 1995). In that same survey, men stated their primary reasons for attending antenatal classes as being to satisfy the wishes of their partners and to learn about infant care. A UK‐based survey found that women would like information on physical and psychological changes during pregnancy, fetal development, what will happen during labour and childbirth, their options during labour and childbirth and how to care for themselves during this time, possible complications, and how to care for the baby after birth (Sullivan 1993).
Delivery of antenatal education
In addition to differences in theoretical approaches, there is huge variation in the provision of antenatal education, with variation in the underlying aims and the way classes are delivered. Programs range from intensive one‐day classes, 'bench' classes (offered while waiting to be seen by a healthcare provider), to several classes over several weeks. There is variation in whether programs are offered individually or in groups; venues include teachers' homes, community centres, hospitals and clinics; and classes or groups may be for pregnant women only or for women and their partners or birth partners.
Teaching‐learning methods include self‐learning programs, didactic presentations, videos, group discussions, and programs based solely on adult learning principles in which mothers identify their own learning needs and develop an individualized learning program from there. The content of classes varies considerably and is likely to be affected by the underlying aims and the way classes are delivered, as well as the skills, experience, and motivation of the teacher. These factors may impact on the effectiveness of antenatal education programs. Because of these wide‐ranging goals, the effectiveness of antenatal education has been broken down by looking at specific goals: either looking at the effects on the experience of childbirth, or on adjustment to parenthood. Few studies have observed how women use preparation methods, but women reported difficulty in using them in a hospital setting (Spiby 1999).
Lay‐ versus professionally‐offered antenatal education
The majority of studies did not explore women's (and partners') expectations and views in depth. There are surprisingly few in‐depth explorations of antenatal preparation and of lay‐run groups, and the majority of research is of professionally‐run classes that may be directed at explaining and justifying polices, resulting in increased compliance. Lay‐run classes that are structured to include the lay perspective and the interests of women have had less attention.
Social capital in antenatal education
Very few studies have investigated the impact of building support networks for women. Yet there is a substantial body of evidence that the development of what is termed 'social capital' has a major influence on health and wellbeing. Social capital refers to features of social organisation, such as civic participation, norms of reciprocity, and trust in others, which facilitate co‐operation for mutual benefit. Thus, social capital is the advantage gained by an individual or group/community of individuals, a result of being part of a social network (Aldridge 2002).
High‐risk participants of antenatal education
The vast majority of literature on antenatal preparation describes courses offered to typical attendees, well‐educated women in the middle‐to‐upper socio‐economic strata. Many care providers feel that this advantaged group will do well regardless of which, if any, antenatal education program they attend. Consequently, evaluating educational program effects in this population may not be of interest. Rather, evaluating the effects of educational programs for medically or socially high‐risk mothers or fathers may be of greater interest to clinicians and important in terms of public health. Descriptions of educational programs from the fathers' perspectives and for special populations are fewer in number and show differences in the educational needs of these parents‐to‐be. Studies in the UK and Australia have examined the views and experiences of a group of new fathers concerning the role classes played in their transition to fatherhood, and fathers' sense of exclusion from such processes (Barclay 1996; Smith 1999).
Birth experience attenuation of antenatal education
The notion that the effects of antenatal education might be attenuated by what occurs at the time of birth is a common theme mentioned by childbirth educators and mothers. Encouraging a woman's assertiveness to express her birth wishes and concerns might lead to disappointment at birth. This notion points to the need to determine the independent effects of childbirth education. If their effects are attenuated, should the resources currently directed towards antenatal education be re‐directed toward programs of education for caregivers at the time of birth, or elsewhere?
Summary
In summary, evidence for the best method to deliver antenatal education is lacking. There is a great deal of variation in antenatal education programs, which must be considered in conducting a systematic review. This review will therefore include reports of programs developed from various theoretical perspectives, with a variety of objectives, content, and teaching‐learning methods employed, offered to a variety of populations. Due to the nature of antenatal education, the review must be broad rather than specific in trying to determine if there is any effect of any educator‐provided antenatal educational intervention in any population.
Objectives
The objectives of this review are based on stated women's and men's reports of their reasons for attending classes. The primary objective is to assess the effects of structured antenatal education delivered by an educator to an individual or group on:
(a) knowledge acquisition; (b) anxiety; (c) maternal sense of control/active decision‐making during labour and birth; (d) labour pain; (e) use of medications to reduce pain; (f) partner involvement at birth; (g) breastfeeding success; (h) infant care abilities; (i) social support (defined as general emotional and homemaking/parenting support); and (j) psychological and social adjustment to parenthood.
A secondary objective is to assess the effects of structured antenatal education on obstetrical interventions.
Methods
Criteria for considering studies for this review
Types of studies
We considered studies if they met the following inclusion criteria: controlled trial evaluating structured forms of antenatal education classes provided to individual parent(s)‐to‐be or groups of future parents; random allocation to treatment and control groups; violations of allocated management insufficient to materially affect outcomes; loss to follow up insufficient to materially affect the comparison; and data available in a form suitable for analysis.
Types of participants
One or both expectant parents.
Types of interventions
Any structured (organized) educational program, offered to individuals or groups by an educator, related to the birth of an infant including preparation for childbirth, child care, and adjustment of the parents associated with parenthood.
Types of outcome measures
Factors that could be affected by antenatal education for either childbirth or parenthood including:
knowledge acquisition;
anxiety;
maternal sense of control/active decision‐making, self‐confidence;
labour pain;
use of medications to reduce pain;
partner involvement at birth;
breastfeeding success;
infant care abilities;
general social support;
psychological and social adjustment to parenthood;
obstetrical interventions.
Search methods for identification of studies
Electronic searches
We searched the Cochrane Pregnancy and Childbirth Group's Trials Register by contacting the Trials Search Co‐ordinator (April 2006). We updated this search on 7 July 2011 and added the results to Studies awaiting classification.
The Cochrane Pregnancy and Childbirth Group’s Trials Register is maintained by the Trials Search Co‐ordinator and contains trials identified from:
quarterly searches of the Cochrane Central Register of Controlled Trials (CENTRAL);
weekly searches of MEDLINE;
weekly searches of EMBASE;
handsearches of 30 journals and the proceedings of major conferences;
weekly current awareness alerts for a further 44 journals plus monthly BioMed Central email alerts.
Details of the search strategies for CENTRAL, MEDLINE and EMBASE, the list of handsearched journals and conference proceedings, and the list of journals reviewed via the current awareness service can be found in the ‘Specialized Register’ section within the editorial information about the Cochrane Pregnancy and Childbirth Group.
Trials identified through the searching activities described above are each assigned to a review topic (or topics). The Trials Search Co‐ordinator searches the register for each review using the topic list rather than keywords.
In addition, we searched CINAHL (1982 to April 2006) (Appendix 1), EMBASE (1980 to April 2006) (Appendix 2), ERIC (1984 to April 2006) (Appendix 3 and PsycINFO (1988 to April 2006) (Appendix 4).
Searching other resources
We also handsearched the Journal of Psychosomatic Research beginning in 1956 up to April 2006 and reviewed the reference lists of retrieved studies.
We did not apply any language restrictions.
Data collection and analysis
The full text of all studies identified from all sources were obtained. Inclusion criteria were applied to the texts and their methodological quality was assessed.
Methodological quality was determined through assessment of the likely presence or absence of biases which might have affected the internal validity of the trials. These included: selection bias through assessment of allocation concealment, attrition bias through assessment of loss of study participants to analysis and protocol deviations, and performance bias through assessment of blinding of participants, caregivers, and outcome assessors.
Statistical analyses were based on intention‐to‐treat and were calculated using the Cochrane statistical package, Review Manager (RevMan 2003). Results are reported as weighted mean differences and 95% confidence interval (CI), and relative risk and 95% CI.
Because an insufficient number of acceptable trials was identified, the intended subgroup analyses could not be performed to examine the effects of: (a) specific class content (eg, childbirth, childcare), (b) specific childbirth education approaches (eg, natural, psychoprophylaxis, active birth), (c) specific teaching approaches (eg, didactic, experiential), or effects in (d) specific population groups (eg, low income, multiethnic).
Results
Description of studies
See the tables of 'Characteristics of included studies' and 'Characteristics of excluded studies'. Nine trials, involving 2284 women, met the study inclusion criteria. Studies were conducted in the United States, Canada, and Iran. Trials directed toward women or couples included two focused on increasing fetal attachment, one on labour, baby care, counseling, and neuromuscular exercises, one on age‐appropriate development, one on early parenthood, one on a combination of 16 interventions including education about pregnancy, peer support, and health behavior, and one on the predisposing, enabling, and reinforcing factors for attempting a vaginal birth after caesarean. Two trials were directed towards men including one focusing on sexuality, pregnancy and prenatal care, labour and delivery, and infant and child care, while the other focused only on newborn care and related paternal behavior. (Fifty‐eight reports from an updated search on 7 July 2011 have been added to Studies awaiting classification.)
Risk of bias in included studies
The largest of the included studies (n = 1275), examining an individualized prenatal education and support program to increase vaginal birth after caesarean section, was of high quality. The remaining trials were of uncertain quality, since details of the randomization procedure, allocation concealment, and/or participant accrual/loss were not always reported.
Effects of interventions
We included nine trials, involving 2284 women. We excluded 37 studies. Eight of the included studies (combined n = 1009) tested more general educational interventions. Specific interventions, populations, and outcomes measured were different in each study. No data from these trials were reported on anxiety, breastfeeding success, or general social support. Knowledge acquisition, sense of control, factors related to infant‐care competencies, and some labour and birth outcomes were measured.
Three of the studies showed beneficial effects on knowledge gained. In one, weighted mean group differences (WMD) of 1.62 (95% confidence interval (CI) 0.49 to 2.75) on a scale of 20 were found (n = 48; Corwin 1999); a second, focusing on fathers‐to‐be, showed a WMD of 9.55 (95% CI 1.25 to 17.85) on a 75‐item scale (n = 28; Westney 1988); and a third study showed a range of being of 20% (relative risk (RR) 1.20, 95% CI 1.07 to 1.35) to over twice as likely (RR 2.22, 95% CI 1.27 to 3.90) of knowing about specific issues (Klerman 2001). Those receiving prenatal education in conjunction with several other interventions were found to be nearly 50% more likely to perceive mastery for behaviour change (RR, 1.48, 95% CI 1.05 to 2.09). Length of labour was found to be shorter in those receiving prenatal education in one study (Mehdizadeh 2005); in active labour: WMD ‐1.10 hours, 95% CI ‐1.64 to ‐0.56; in the second stage of labour: WMD ‐8.70, 95% CI ‐12.60 to ‐4.80. Benefits to attachment were found in very small studies (WMD 52.6 attachment behaviors, 95% CI 21.82 to 83.38, n = 10, Carter‐Jessop 1981; and WMD 9.70 attachment behaviors, 95% 0.15 to 19.25, n = 22, Davis 1987). Similar results were found for satisfaction with maternal role preparation (WMD 21.59 of a possible score ranging from 24 to 120, 95% CI 11.23 to 31.95, n = 16, Hamilton‐Dodd 1989). The results of all these smaller studies are likely to be subject to significant bias since reports of baseline characteristics by group are largely absent and when group differences were reported, were not addressed in terms of their potential effect on outcome assessment. No differences were found in any other outcomes measured. The ninth and largest of the included studies (n = 1275; Fraser 1997), examining an educational and social support intervention to increase vaginal birth after caesarean section, showed similar rates of vaginal birth after caesarean section in 'verbal' and 'document' groups (RR 1.08, 95% CI 0.97 to 1.21).
Discussion
Although women and their partners in many countries are commonly referred to structured antenatal education programs, the benefits of these programs to participants and their newborn infants remain unclear.
With the exception of one large trial aimed at increasing the rate of vaginal birth after caesarean delivery, the trials were small to moderate and of uncertain methodological quality. The usual benefit of meta‐analyses of increasing statistical power by combining small studies was not achieved, since each study was testing the effect of a different intervention on one or more different outcomes. Further, this variation did not permit proposed subgroup analyses to be conducted to examine the effects of specific class content, theoretical underpinnings, teaching approaches, or effects in specific population groups.
Authors' conclusions
Implications for practice.
No recommendations for practice changes can be made at this time since there exists insufficient evidence to determine the effects of person‐to‐person antenatal education for childbirth or parenthood, or both. The widespread popularity of antenatal classes, particularly in some northern countries, testifies to the desire of many (particularly first‐time) expectant parents or their caregivers for antenatal education.
Implications for research.
The extensive amount of resources placed in attendance and provision of structured antenatal education programs suggest the need for a large, well‐designed clinical trial to answer the question of effectiveness. Conducting such a trial in this field will be very challenging due to their popularity, particularly in some northern countries. In previous work, we found only 10% of women initially inquiring about classes to state their willingness to be randomized to either classes or a placebo arm (Gagnon 1995). Further, compliance to the assigned intervention may be difficult. Women not already planning to attend classes are unlikely to attend even if they are randomized to do so.
Difficulties in conducting a randomized controlled trial in this field can also be expected to arise when deciding just what and in whom to test antenatal education given the great variation in content, in approach, and in the populations to whom it is currently provided.
In conducting such a trial, one should ensure that outcomes to be measured include those defined as important by both the consumers of this education and those referring parents‐to‐be for education.
[Note: the 58 citations in the awaiting classification section may alter the conclusions of the review once assessed.]
What's new
| Date | Event | Description |
|---|---|---|
| 7 July 2011 | Amended | Search updated. Fifty‐eight reports added to Studies awaiting classification. |
History
Protocol first published: Issue 1, 1999 Review first published: Issue 4, 2000
| Date | Event | Description |
|---|---|---|
| 29 January 2009 | Amended | The contact person for this review is now Jane Sandall. |
| 3 September 2008 | Amended | Converted to new review format. |
| 17 May 2007 | New citation required but conclusions have not changed | New author helped to prepare the update. |
| 1 April 2006 | New search has been performed | Search updated. Three new trials (Davis 1987; Klerman 2001; Mehdizadeh 2005) included and 15 new trials excluded (Astbury 1980; D'Andrea 1994; De Nuncio 2000; Escott 2005; Ford 2002; Leitch 1999; Linares 2006; Manandhar 2004; O'Cathain 2002; Polley 2002; Schachman 2004; Schonberger 2004; Spence‐Cagle 1984; Springer 1996; Turan 2001). The conclusions concerning the effects of antenatal education remain largely the same and are generally unknown. |
Acknowledgements
We would like to acknowledge Hilary Elkins, Research Assistant with Anita J Gagnon at McGill University and McGill University Health Centre for administering the original search strategies and locating additional materials that were included in this update. We would also like to thank Tamara Rader, previously Information Officer at the Centre for Nursing Research of the SMBD Jewish General Hospital in Montreal, for developing the original search strategies and locating the initial material that made up this review; Kathy Waghorn, previously Research Co‐ordinator at the Centre for Nursing Research of the SMBD Jewish General Hospital in Montreal, for handsearching one year of the Journal of Psychosomatic Research and for stimulating interest in this topic; and Agnes Cho of the Maternal, Infant and Reproductive Health research Unit at The Centre for Research in Women's Health in Toronto for her translation of the Zhang 1996 article from Chinese.
Appendices
Appendix 1. Search terms for CINAHL
1982 to April 2006 (authors wrote and ran the search)
exp pregnancy/ or pregnancy.ti, ab, sh.
prenatal. ti, ab, sh.
antenatal. ti, ab, sh.
birth. ti, ab, sh. OR childbirth. ti, ab, sh.
early intervention (education)/ OR education/ OR education. ti, ab, sh.
preparation. ti, ab, sh.
5 OR 6
(mothers/ or motherhood. ti, ab, sh.) OR (father/ or fatherhood. ti, ab, sh.) OR (parent/ or parenthood)
1 OR 2 OR 3 OR 4 OR 8
7 AND 9
MeSH terms were consulted and the appropriate terms were used in conjunction with natural language to create a broad search. Natural language was also used to describe concepts which may be termed differently in each database.
Appendix 2. Search terms for EMBASE
1980 to April 2006 (authors wrote and ran the search)
birth/ OR childbirth/ OR pregnancy.exp
prenatal/ OR antenatal.exp
1 AND 2
3 AND Education.exp
randomized controlled trial.exp AND 4
pain.exp/ OR knowledge acquisition.exp/ OR self‐confidence.exp/ OR anxiety.exp/ OR decision‐making.exp/ OR obstetrical intervention.exp/ OR partner involvement.exp/ OR breast‐feeding.exp/ OR infant care.exp/ OR social support.exp
6 AND randomized controlled trial.exp
5 AND 7
Appropriate EMBASE keywords were selected to formulate a search strategy. Natural language was also employed to ensure a broad search. Terms were 'exploded' (exp) to access all related articles.
Appendix 3. Search terms for ERIC database
1984 to April 2006 (authors wrote and ran the search)
birth/ OR childbirth.ab, ti, hw, id OR pregnancy
(adult learning/ or didactic.ab, ti, hw, id) OR (class or course).ab, ti, hw, id. OR exp teaching methods/ OR exp educational research/
1 AND 2
parenthood education/ OR preparation.ab, ti, hw, id OR childbirth.ab, ti, hw ADJ education.ab, ti, hw, id.
3 OR 4
5 NOT school ADJ curriculum
The thesaurus for the ERIC database was consulted and the appropriate terms were selected to formulate a search strategy. Terms that are followed by a forward slash are the controlled vocabulary for the ERIC thesaurus. Natural language was also employed to ensure a broad search. Childbirth education or preparation; teaching methods; and stress or anxiety reduction were the three concepts covered by this search.
Appendix 4. Search strategy for PsycINFO
1988 to April 2006 (authors wrote and ran the search)
exp birth/ OR childbirth.ti, ab, hw, id. OR pregnancy/ OR prenatal.ti, ab, hw, id OR antenatal.ti, ab, hw, id.
exp education/ or preparation.ti, ab, hw, id.
1 and 2
Appropriate terms were selected from the PsycINFO thesaurus and the forward slash denotes this usage. Natural language was employed to help broaden the search. Terms were 'exploded' (exp) to access all related articles.
Data and analyses
Comparison 1. Individual maternal education versus routine care.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Observed maternal competence | 1 | 16 | Mean Difference (IV, Fixed, 95% CI) | 1.87 [‐16.04, 19.78] |
| 2 Adaptation to the maternal role (Lederman tool) | 1 | 16 | Mean Difference (IV, Fixed, 95% CI) | 12.0 [‐4.83, 28.83] |
| 3 Adaptation to the maternal role (Sheehan tool) | 1 | 16 | Mean Difference (IV, Fixed, 95% CI) | 2.12 [‐1.82, 6.06] |
| 4 Satisfaction with maternal role preparation | 1 | 16 | Mean Difference (IV, Fixed, 95% CI) | 21.59 [11.23, 31.95] |
1.1. Analysis.
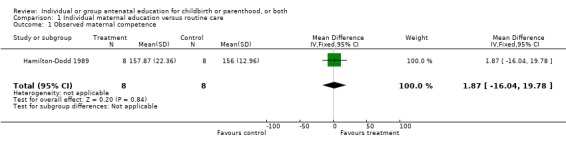
Comparison 1 Individual maternal education versus routine care, Outcome 1 Observed maternal competence.
1.2. Analysis.
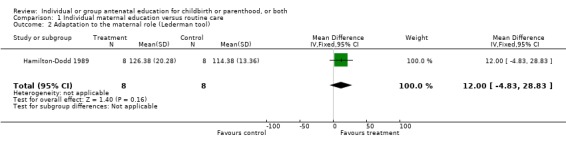
Comparison 1 Individual maternal education versus routine care, Outcome 2 Adaptation to the maternal role (Lederman tool).
1.3. Analysis.
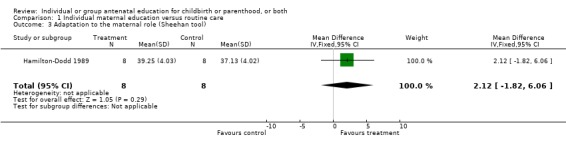
Comparison 1 Individual maternal education versus routine care, Outcome 3 Adaptation to the maternal role (Sheehan tool).
1.4. Analysis.
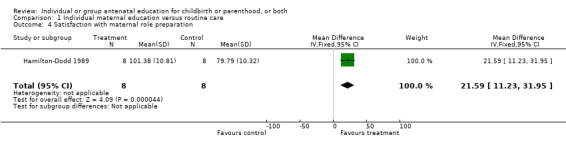
Comparison 1 Individual maternal education versus routine care, Outcome 4 Satisfaction with maternal role preparation.
Comparison 2. Paternal education classes versus routine care.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Paternal sensitivity | 1 | 66 | Mean Difference (IV, Fixed, 95% CI) | 0.38 [‐0.04, 0.80] |
| 2 Paternal plus infant sensitivity | 1 | 66 | Mean Difference (IV, Fixed, 95% CI) | 0.65 [0.04, 1.26] |
| 3 Paternal knowledge | 1 | 28 | Mean Difference (IV, Fixed, 95% CI) | 9.55 [1.25, 17.85] |
2.1. Analysis.
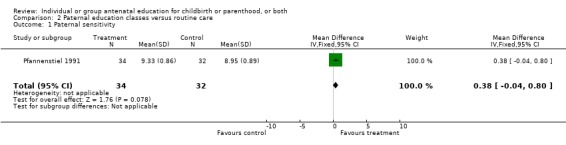
Comparison 2 Paternal education classes versus routine care, Outcome 1 Paternal sensitivity.
2.2. Analysis.
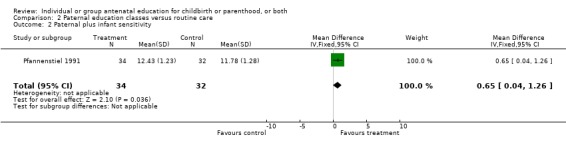
Comparison 2 Paternal education classes versus routine care, Outcome 2 Paternal plus infant sensitivity.
2.3. Analysis.
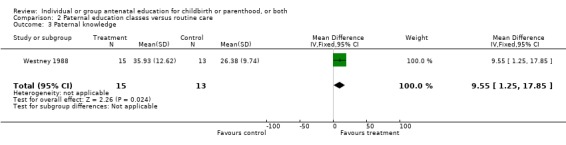
Comparison 2 Paternal education classes versus routine care, Outcome 3 Paternal knowledge.
Comparison 3. Childbirth education classes + maternal attachment preparation versus childbirth education classes alone.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Frequency of maternal attachment behaviors | 1 | 10 | Mean Difference (IV, Fixed, 95% CI) | 52.60 [21.82, 83.38] |
3.1. Analysis.
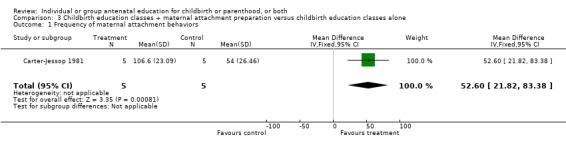
Comparison 3 Childbirth education classes + maternal attachment preparation versus childbirth education classes alone, Outcome 1 Frequency of maternal attachment behaviors.
Comparison 4. Expanded childbirth education classes versus traditional childbirth education classes.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Parenting knowledge | 1 | 48 | Mean Difference (IV, Fixed, 95% CI) | 1.62 [0.49, 2.75] |
4.1. Analysis.
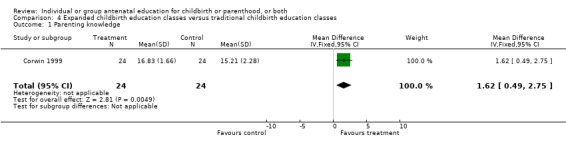
Comparison 4 Expanded childbirth education classes versus traditional childbirth education classes, Outcome 1 Parenting knowledge.
Comparison 5. Individual vaginal birth after caesarean education/support versus routine care.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Vaginal birth after caesarean | 1 | 1275 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.08 [0.97, 1.21] |
| 2 Attempted vaginal delivery | 1 | 1275 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.05 [0.97, 1.12] |
| 3 Scheduled caesarean | 1 | 1275 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.90 [0.74, 1.11] |
| 4 Unsuccessful attempt at vaginal birth after caesarean | 1 | 1275 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.96 [0.77, 1.19] |
| 5 Urgent caesarean | 1 | 1275 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.58, 1.33] |
| 6 Uterine rupture or dehiscence | 1 | 1275 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.32 [0.46, 3.78] |
| 7 Hysterectomy | 1 | 1275 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.20 [0.01, 4.11] |
| 8 Maternal blood transfusion | 1 | 1275 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.66 [0.11, 3.93] |
| 9 Perinatal death | 1 | 1280 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.50 [0.09, 2.69] |
| 10 Apgar score < 7 at 5 minutes | 1 | 1280 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.66 [0.24, 1.84] |
| 11 Neonatal intensive care unit admission | 1 | 1280 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.75, 1.34] |
| 12 Instrumental delivery | 1 | 1275 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.80, 1.31] |
5.1. Analysis.
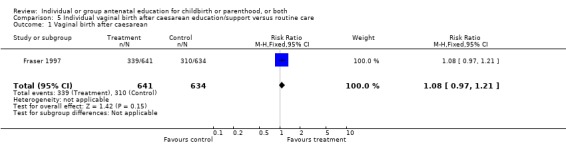
Comparison 5 Individual vaginal birth after caesarean education/support versus routine care, Outcome 1 Vaginal birth after caesarean.
5.2. Analysis.
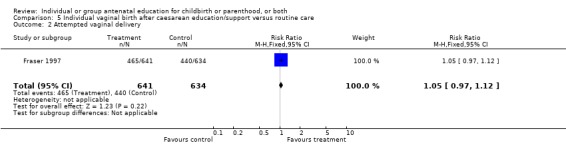
Comparison 5 Individual vaginal birth after caesarean education/support versus routine care, Outcome 2 Attempted vaginal delivery.
5.3. Analysis.
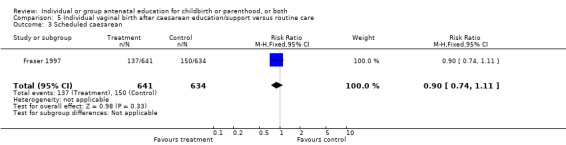
Comparison 5 Individual vaginal birth after caesarean education/support versus routine care, Outcome 3 Scheduled caesarean.
5.4. Analysis.
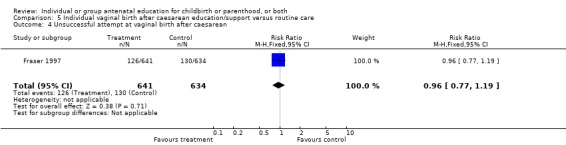
Comparison 5 Individual vaginal birth after caesarean education/support versus routine care, Outcome 4 Unsuccessful attempt at vaginal birth after caesarean.
5.5. Analysis.
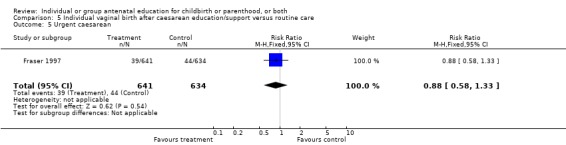
Comparison 5 Individual vaginal birth after caesarean education/support versus routine care, Outcome 5 Urgent caesarean.
5.6. Analysis.
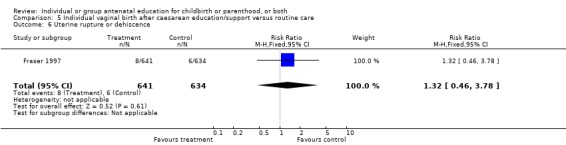
Comparison 5 Individual vaginal birth after caesarean education/support versus routine care, Outcome 6 Uterine rupture or dehiscence.
5.7. Analysis.
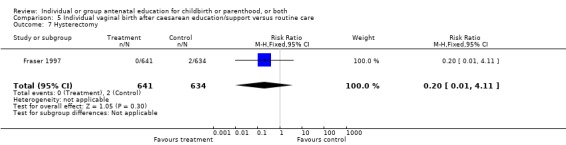
Comparison 5 Individual vaginal birth after caesarean education/support versus routine care, Outcome 7 Hysterectomy.
5.8. Analysis.
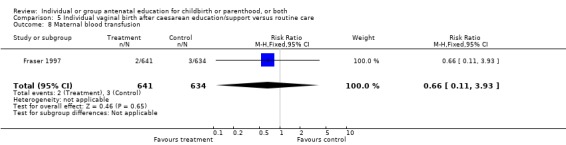
Comparison 5 Individual vaginal birth after caesarean education/support versus routine care, Outcome 8 Maternal blood transfusion.
5.9. Analysis.
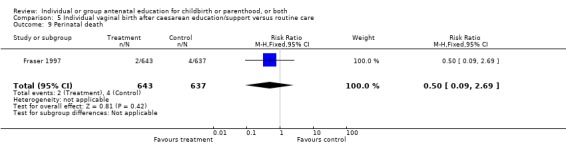
Comparison 5 Individual vaginal birth after caesarean education/support versus routine care, Outcome 9 Perinatal death.
5.10. Analysis.
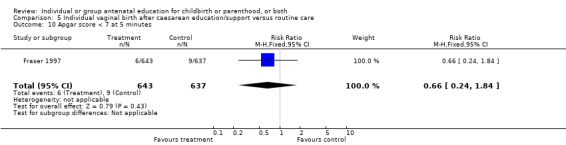
Comparison 5 Individual vaginal birth after caesarean education/support versus routine care, Outcome 10 Apgar score < 7 at 5 minutes.
5.11. Analysis.
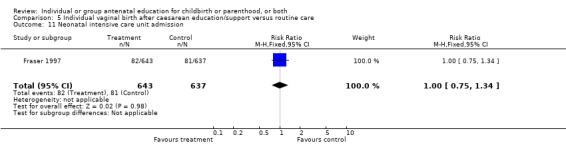
Comparison 5 Individual vaginal birth after caesarean education/support versus routine care, Outcome 11 Neonatal intensive care unit admission.
5.12. Analysis.
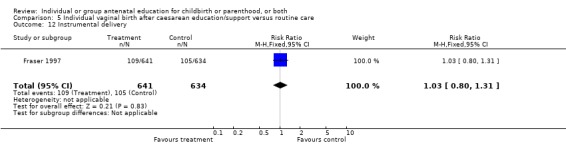
Comparison 5 Individual vaginal birth after caesarean education/support versus routine care, Outcome 12 Instrumental delivery.
Comparison 6. Promotion of intrauterine attachment versus routine care.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Affectionate behavior (maternal attachment subscale) | 1 | 22 | Mean Difference (IV, Fixed, 95% CI) | 9.70 [0.15, 19.25] |
| 2 Proximity maintaining (maternal attachment subscale) | 1 | 22 | Mean Difference (IV, Fixed, 95% CI) | 2.87 [‐1.04, 6.78] |
| 3 Mother's attachment (maternal attachment subscale) | 1 | 22 | Mean Difference (IV, Fixed, 95% CI) | ‐1.90 [‐8.52, 4.72] |
6.1. Analysis.
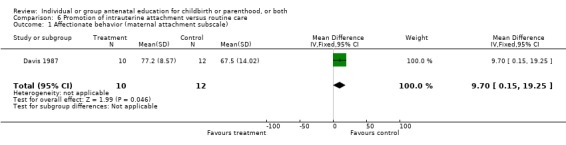
Comparison 6 Promotion of intrauterine attachment versus routine care, Outcome 1 Affectionate behavior (maternal attachment subscale).
6.2. Analysis.
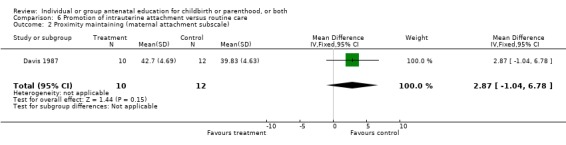
Comparison 6 Promotion of intrauterine attachment versus routine care, Outcome 2 Proximity maintaining (maternal attachment subscale).
6.3. Analysis.
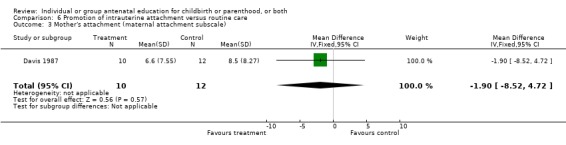
Comparison 6 Promotion of intrauterine attachment versus routine care, Outcome 3 Mother's attachment (maternal attachment subscale).
Comparison 7. Augmented prenatal care versus routine care.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Prenatal care ‐ very helpful | 1 | 223 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.17 [1.05, 1.30] |
| 2 Prenatal care ‐ somewhat or not too helpful | 1 | 223 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.27 [0.11, 0.64] |
| 3 Compared with last time, prenatal care rated ‐ better | 1 | 223 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.17 [1.05, 1.30] |
| 4 Compared with last time, prenatal care rated ‐ same | 1 | 223 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.43 [0.25, 0.74] |
| 5 Compared with last time, prenatal care rated ‐ worse | 1 | 223 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.10 [0.01, 0.77] |
| 6 Average time reported with nurse per visit ‐ less than 15 minutes | 1 | 223 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.39 [0.24, 0.64] |
| 7 Average reported time with nurse per visit ‐ about 30 minutes | 1 | 223 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.30 [1.02, 1.66] |
| 8 Average time reported with nurse per visit ‐ about 45 minutes | 1 | 223 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.37 [0.96, 5.84] |
| 9 Average time reported with nurse per visit ‐ about 60 minutes | 1 | 223 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.42 [0.48, 4.22] |
| 10 Average reported time from entering to leaving clinic ‐ about 1 hour | 1 | 223 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.05 [0.58, 1.89] |
| 11 Average reported time from entering to leaving clinic ‐ about 1.5‐2.5 hours | 1 | 223 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.48 [1.17, 1.86] |
| 12 Average reported time from entering to leaving clinic ‐ about 3 hours or more | 1 | 223 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.37 [0.21, 0.67] |
| 13 Same nurse reported as providing care each visit | 1 | 223 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.13 [1.03, 1.24] |
| 14 Nurse rated as "very helpful" | 1 | 223 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.16 [1.03, 1.30] |
| 15 Knowledge of risk factors ‐ told she or her baby might be "at risk" or "have problems" | 1 | 223 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.48 [1.03, 2.14] |
| 16 Knowledge of risk factors ‐ changed behavior during pregnancy in response to information about risks/problems | 1 | 223 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.22 [1.27, 3.90] |
| 17 Knowledge of risk factors ‐ told how much weight to gain | 1 | 223 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.20 [1.07, 1.35] |
| 18 Self‐report of behavioral change/status ‐ regular vitamin‐mineral supplementation | 1 | 223 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.88, 1.16] |
| 19 Self‐report of behavioral change/status ‐ smoking cessation (for smokers only) | 1 | 223 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.40 [0.56, 3.48] |
| 20 Self‐report of behavioral change/status ‐ perceived mastery | 1 | 223 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.48 [1.05, 2.09] |
| 21 Mean birthweight | 1 | 607 | Mean Difference (IV, Fixed, 95% CI) | 44.0 [‐50.51, 138.51] |
| 22 Low birthweight (less than 2500 g) | 1 | 607 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.48 [0.92, 2.39] |
| 23 Mean gestational weight age, week | 1 | 607 | Mean Difference (IV, Fixed, 95% CI) | 0.30 [‐0.13, 0.73] |
| 24 Preterm birth | 1 | 607 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.77 [0.50, 1.18] |
| 25 Intrauterine growth restriction | 1 | 607 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.30 [0.82, 2.09] |
| 26 Low Apgar score ‐ at 1 minute | 1 | 607 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.81 [0.53, 1.24] |
| 27 Low Apgar score ‐ at 5 minutes | 1 | 607 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.59 [0.38, 6.58] |
| 28 Neonatal intensive care unit stay | 1 | 607 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.71 [0.47, 1.09] |
| 29 Congenital anomalies | 1 | 607 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.68 [0.22, 2.12] |
| 30 Mean maternal weight gain during pregnancy, kg ‐ if BMI less than 19.8 (at risk) | 1 | 607 | Mean Difference (IV, Fixed, 95% CI) | 1.0 [‐0.01, 2.01] |
| 31 Mean maternal weight gain during pregnancy, kg ‐ if BMI is greater than or equal to 19.8 (not at risk) | 1 | 607 | Mean Difference (IV, Fixed, 95% CI) | 0.10 [‐1.16, 1.36] |
| 32 Caesarean deliveries | 1 | 607 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.80 [0.55, 1.17] |
7.1. Analysis.
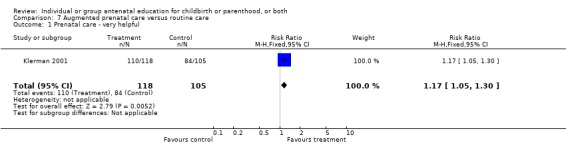
Comparison 7 Augmented prenatal care versus routine care, Outcome 1 Prenatal care ‐ very helpful.
7.2. Analysis.
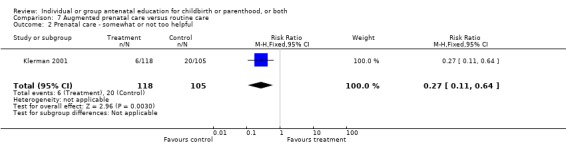
Comparison 7 Augmented prenatal care versus routine care, Outcome 2 Prenatal care ‐ somewhat or not too helpful.
7.3. Analysis.
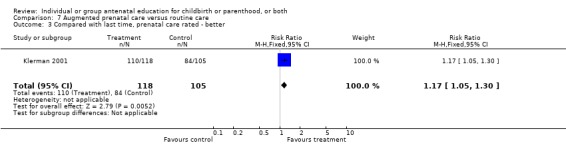
Comparison 7 Augmented prenatal care versus routine care, Outcome 3 Compared with last time, prenatal care rated ‐ better.
7.4. Analysis.
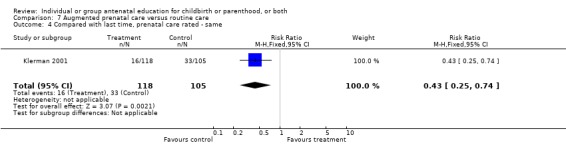
Comparison 7 Augmented prenatal care versus routine care, Outcome 4 Compared with last time, prenatal care rated ‐ same.
7.5. Analysis.
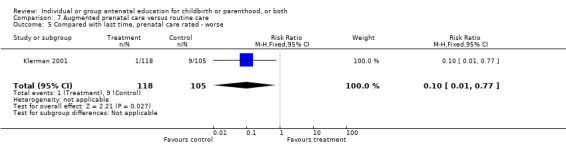
Comparison 7 Augmented prenatal care versus routine care, Outcome 5 Compared with last time, prenatal care rated ‐ worse.
7.6. Analysis.
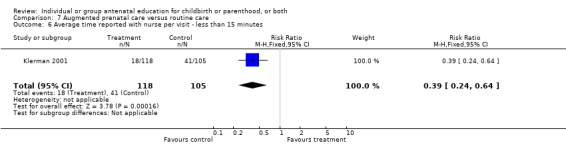
Comparison 7 Augmented prenatal care versus routine care, Outcome 6 Average time reported with nurse per visit ‐ less than 15 minutes.
7.7. Analysis.
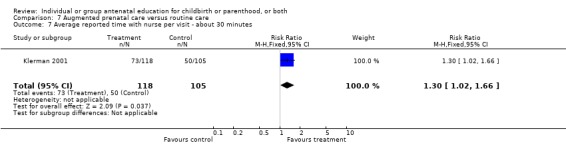
Comparison 7 Augmented prenatal care versus routine care, Outcome 7 Average reported time with nurse per visit ‐ about 30 minutes.
7.8. Analysis.
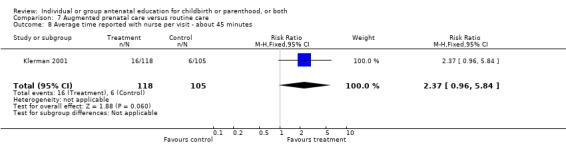
Comparison 7 Augmented prenatal care versus routine care, Outcome 8 Average time reported with nurse per visit ‐ about 45 minutes.
7.9. Analysis.
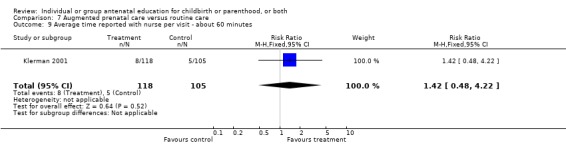
Comparison 7 Augmented prenatal care versus routine care, Outcome 9 Average time reported with nurse per visit ‐ about 60 minutes.
7.10. Analysis.
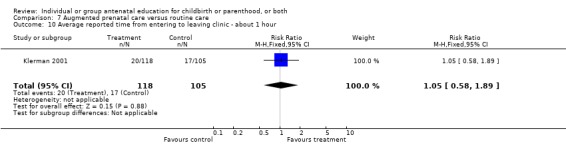
Comparison 7 Augmented prenatal care versus routine care, Outcome 10 Average reported time from entering to leaving clinic ‐ about 1 hour.
7.11. Analysis.
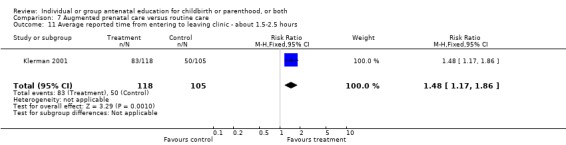
Comparison 7 Augmented prenatal care versus routine care, Outcome 11 Average reported time from entering to leaving clinic ‐ about 1.5‐2.5 hours.
7.12. Analysis.
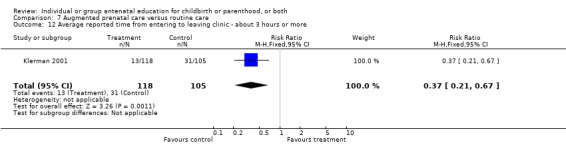
Comparison 7 Augmented prenatal care versus routine care, Outcome 12 Average reported time from entering to leaving clinic ‐ about 3 hours or more.
7.13. Analysis.
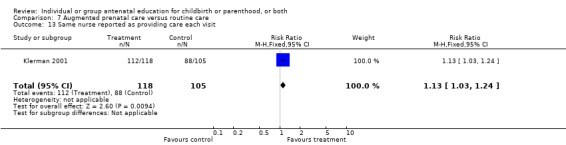
Comparison 7 Augmented prenatal care versus routine care, Outcome 13 Same nurse reported as providing care each visit.
7.14. Analysis.
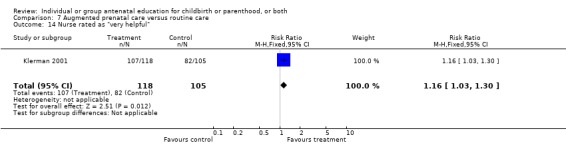
Comparison 7 Augmented prenatal care versus routine care, Outcome 14 Nurse rated as "very helpful".
7.15. Analysis.
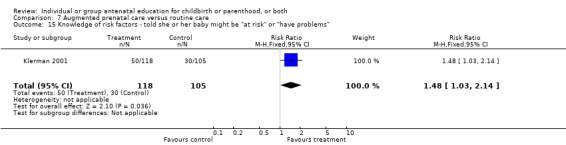
Comparison 7 Augmented prenatal care versus routine care, Outcome 15 Knowledge of risk factors ‐ told she or her baby might be "at risk" or "have problems".
7.16. Analysis.
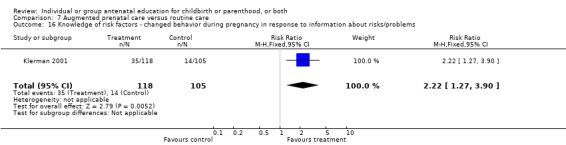
Comparison 7 Augmented prenatal care versus routine care, Outcome 16 Knowledge of risk factors ‐ changed behavior during pregnancy in response to information about risks/problems.
7.17. Analysis.
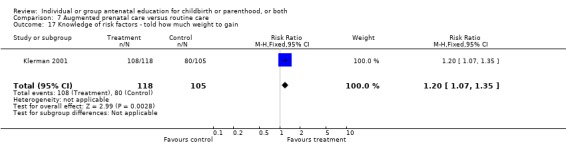
Comparison 7 Augmented prenatal care versus routine care, Outcome 17 Knowledge of risk factors ‐ told how much weight to gain.
7.18. Analysis.
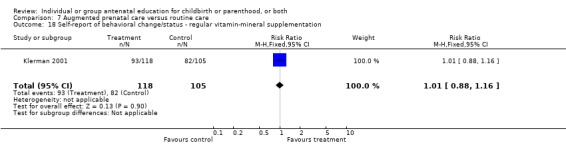
Comparison 7 Augmented prenatal care versus routine care, Outcome 18 Self‐report of behavioral change/status ‐ regular vitamin‐mineral supplementation.
7.19. Analysis.
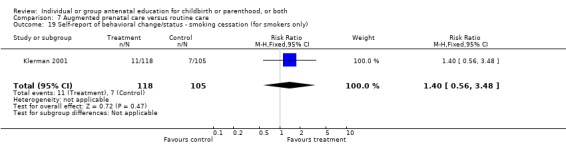
Comparison 7 Augmented prenatal care versus routine care, Outcome 19 Self‐report of behavioral change/status ‐ smoking cessation (for smokers only).
7.20. Analysis.
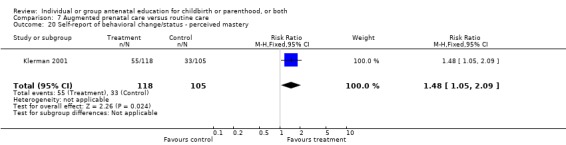
Comparison 7 Augmented prenatal care versus routine care, Outcome 20 Self‐report of behavioral change/status ‐ perceived mastery.
7.21. Analysis.
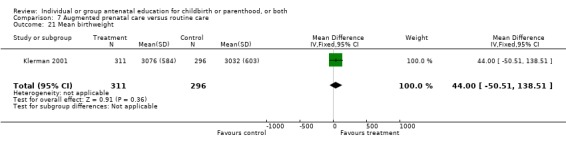
Comparison 7 Augmented prenatal care versus routine care, Outcome 21 Mean birthweight.
7.22. Analysis.
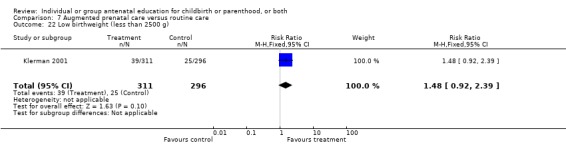
Comparison 7 Augmented prenatal care versus routine care, Outcome 22 Low birthweight (less than 2500 g).
7.23. Analysis.
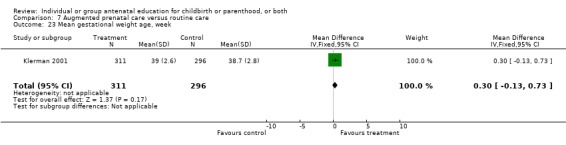
Comparison 7 Augmented prenatal care versus routine care, Outcome 23 Mean gestational weight age, week.
7.24. Analysis.
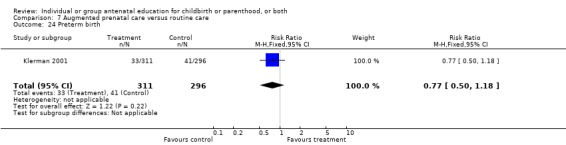
Comparison 7 Augmented prenatal care versus routine care, Outcome 24 Preterm birth.
7.25. Analysis.
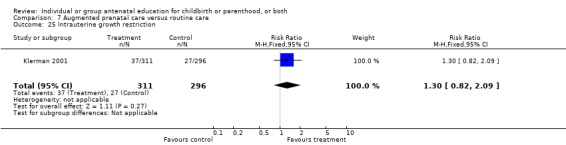
Comparison 7 Augmented prenatal care versus routine care, Outcome 25 Intrauterine growth restriction.
7.26. Analysis.
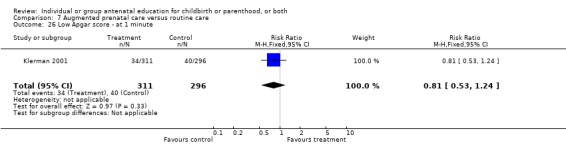
Comparison 7 Augmented prenatal care versus routine care, Outcome 26 Low Apgar score ‐ at 1 minute.
7.27. Analysis.
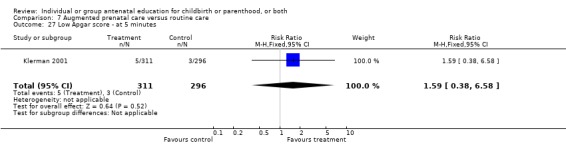
Comparison 7 Augmented prenatal care versus routine care, Outcome 27 Low Apgar score ‐ at 5 minutes.
7.28. Analysis.
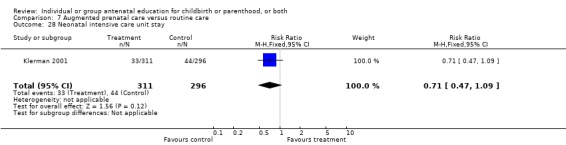
Comparison 7 Augmented prenatal care versus routine care, Outcome 28 Neonatal intensive care unit stay.
7.29. Analysis.
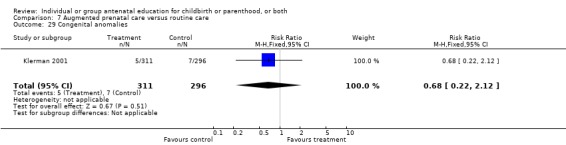
Comparison 7 Augmented prenatal care versus routine care, Outcome 29 Congenital anomalies.
7.30. Analysis.
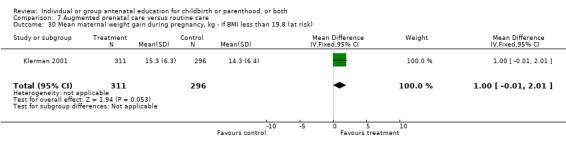
Comparison 7 Augmented prenatal care versus routine care, Outcome 30 Mean maternal weight gain during pregnancy, kg ‐ if BMI less than 19.8 (at risk).
7.31. Analysis.
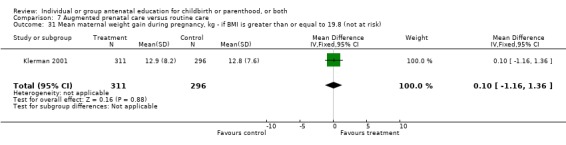
Comparison 7 Augmented prenatal care versus routine care, Outcome 31 Mean maternal weight gain during pregnancy, kg ‐ if BMI is greater than or equal to 19.8 (not at risk).
7.32. Analysis.
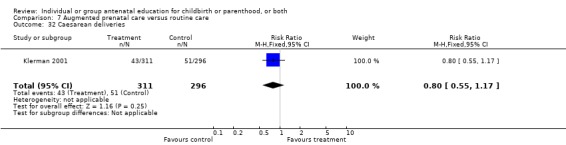
Comparison 7 Augmented prenatal care versus routine care, Outcome 32 Caesarean deliveries.
Comparison 8. Group maternal education versus routine care.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Back or pelvic pain (during labour) | 1 | 200 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.70 [0.54, 0.90] |
| 2 Length of labour (hours) ‐ active phase | 1 | 200 | Mean Difference (IV, Fixed, 95% CI) | ‐1.10 [‐1.64, ‐0.56] |
| 3 Length of labour (minutes) ‐ second stage | 1 | 200 | Mean Difference (IV, Fixed, 95% CI) | ‐8.7 [‐12.60, ‐4.80] |
| 4 Vaginal delivery | 1 | 200 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.08 [1.00, 1.16] |
| 5 Oxytocin | 1 | 200 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.12 [0.93, 1.35] |
| 6 Episiotomy | 1 | 200 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.13 [0.85, 1.50] |
| 7 Birthweight | 1 | 200 | Mean Difference (IV, Fixed, 95% CI) | 14.0 [‐55.11, 83.11] |
| 8 Increased daily activity | 1 | 200 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.28 [0.88, 1.85] |
| 9 Headache | 1 | 200 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.0 [1.16, 13.75] |
| 10 Sleep disturbance | 1 | 200 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.81 [0.64, 1.03] |
8.1. Analysis.
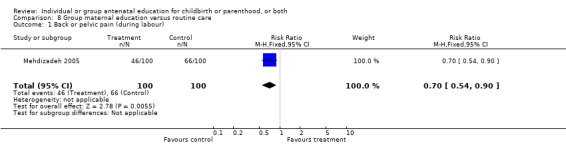
Comparison 8 Group maternal education versus routine care, Outcome 1 Back or pelvic pain (during labour).
8.2. Analysis.
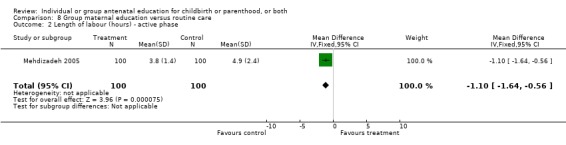
Comparison 8 Group maternal education versus routine care, Outcome 2 Length of labour (hours) ‐ active phase.
8.3. Analysis.
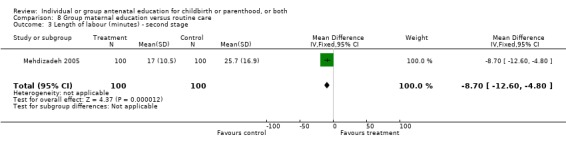
Comparison 8 Group maternal education versus routine care, Outcome 3 Length of labour (minutes) ‐ second stage.
8.4. Analysis.
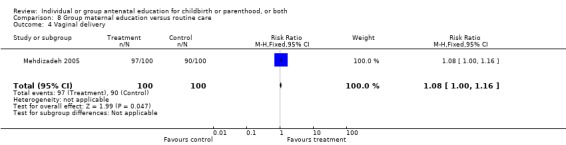
Comparison 8 Group maternal education versus routine care, Outcome 4 Vaginal delivery.
8.5. Analysis.
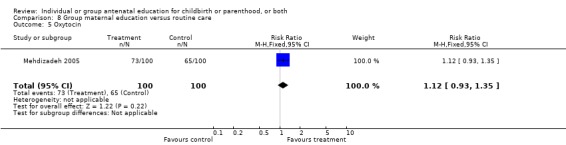
Comparison 8 Group maternal education versus routine care, Outcome 5 Oxytocin.
8.6. Analysis.
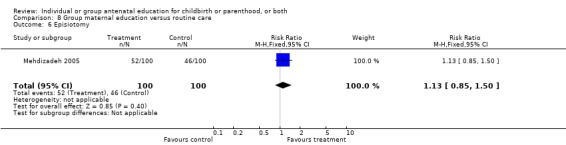
Comparison 8 Group maternal education versus routine care, Outcome 6 Episiotomy.
8.7. Analysis.
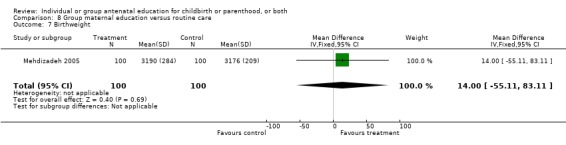
Comparison 8 Group maternal education versus routine care, Outcome 7 Birthweight.
8.8. Analysis.
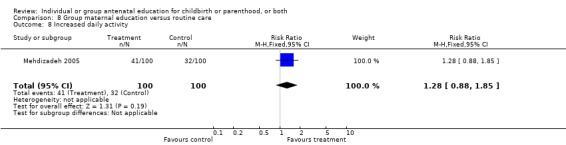
Comparison 8 Group maternal education versus routine care, Outcome 8 Increased daily activity.
8.9. Analysis.
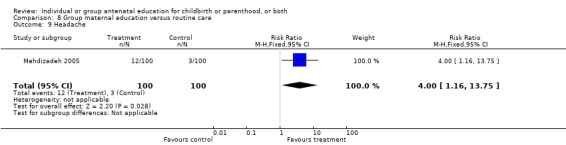
Comparison 8 Group maternal education versus routine care, Outcome 9 Headache.
8.10. Analysis.
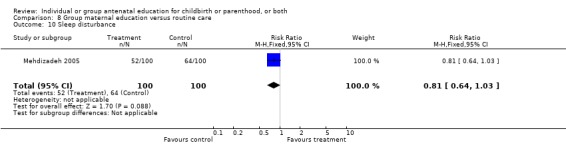
Comparison 8 Group maternal education versus routine care, Outcome 10 Sleep disturbance.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Carter‐Jessop 1981.
| Methods | Randomization to experimental and placebo/usual care groups, procedure not described. Outcome assessor was masked to group allocation. | |
| Participants | 10 healthy, married, "white", nulliparous women, 21‐34 years old, attended by private obstetricians in the US, 32‐37 weeks' gestation who were attending childbirth education classes. Reportedly an equivalent number of breastfeeders and equivalent attachment in both groups (no data provided). No other baseline comparisons reported. | |
| Interventions | All participants attended childbirth education classes. Group A: attachment intervention (n = 5). Consisted of 2‐3 weekly encounters with women (apparently not in groups) by the same nurse. During these encounters the women were encouraged to: (1) feel for the fetus' parts and to check for the fetal position daily, (2) increase their awareness of fetal activity and notice how they can affect that activity, and (3) rub, stroke, and gently massage their abdomens over the fetus. Group B: usual prenatal care (n = 5). | |
| Outcomes | Maternal attachment measured by observing the frequency of attachment behaviors for 1 second every 10 seconds during a 10‐minute period at day 2‐4 postpartum using the 'postnatal attachment test' developed by the author using the results of Marshall Klaus' work. No reliability or validity testing was done on this 'test'. There were 9 attachment behaviors which could be observed; no range of possible frequencies for these behaviors was given. Site of postpartum data collections was not stated. No SDs were reported. Means: attachment group, 106.6, control group, 54. Estimates of the SD from the crude data as reported: 23.09 (attachment group) and 26.46 (usual care group). | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
Corwin 1999.
| Methods | Randomization to experimental and placebo/usual care groups, procedure not described. In one section, authors state that those in classes were randomized, elsewhere it states that those who registered for classes by telephone were randomized. Masking to group allocation by provider or outcome assessor, or both, was not described. | |
| Participants | 48 adults (stated as 48 couples in the abstract) in expectant parent classes in the US. These were mothers with or without a partner/support person. Inclusion criteria were not described. Criteria to exclude from the analysis were: non‐English speaking, bedrest due to preterm labour, delivery prior to the intervention, missing 'significant' (not defined) portions of the class, attending refresher or VBAC classes. Baseline data were presented including gender, making it unclear as to whether the data presented refer to the women or women and partners. Their average ages were 32‐33 years old, 83.3% (control (C) group) to 91.7% (experimental (E) group) were Caucasian, 67‐71% held bachelors' degrees. The groups were not equivalent on female gender (E = 66.7%, C = 54.2%), income over $60,000 USD (E = 41.7%, C = 20.8%), and multiparity (E = 8.3%, C = 20.8%). | |
| Interventions | The number of classes, their duration, and rate of attendance were not reported for either group. Group A: 'expanded' or integrated childbirth education (n = 24 plus those subsequently excluded for not completing 'significant portions of the class'). Participants were taught information about age‐appropriate development in the first year of life through demonstrating parallels between labour challenges and early parenting challenges. The goal was to give parents the ability to generalize their labour coping skills to postpartum coping. Group B: 'traditional' or usual prenatal education (n = 24 plus those subsequently excluded for not completing 'significant portions of the class'). Usual education was not described. | |
| Outcomes | Parenting knowledge as measured by the Prenatal Parenting Scale, a 20‐item true/false questionnaire developed by the author. No reliability or validity data were provided. No scoring information was provided. | |
| Notes | Selection bias may have occurred given that at least some of the exclusion criteria appear to have been applied postrandomization. Analyses of effects, parent knowledge score means, did not address the issue of clinically important baseline differences in gender, income, and parity. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
Davis 1987.
| Methods | Randomization to experimental and control groups. The participant and provider were not masked to group allocation; the outcome assessor was masked. Allocation concealment was not described. | |
| Participants | 22 17‐32 year old, low‐risk, predominantly "white" English‐speaking pregnant women (32‐37 weeks' gestational age) in a US clinic. Baseline characteristics by group did not differ. | |
| Interventions | The "intrauterine attachment" intervention consisted of individual instruction given to women in a "clinical setting at scheduled visits". It was based on the theoretical framework of Barnard and Rubin and included: (1) demonstrating fetal position assessment through abdomen palpation and drawing pictures of what was found 3 times per week; (2) exploring any maternal behavior that the woman felt as an effect on fetal activity; (3) rubbing, stroking, massaging the abdomen for fetal response and taking note. 3 classes were scheduled; duration of these classes was not reported. Placebo/usual care was not described. | |
| Outcomes | Selected maternal attachment subscales: affectionate behavior, proximity maintaining, caretaking behavior, and mother's attention were reported based on observations at 2‐4 days postpartum. Overall score obtained by totalling the frequency of occurrence of each behavior in each subscale for 20 seconds of each minute for 15 minutes of observation. No ranges were provided. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | D ‐ Not used |
Fraser 1997.
| Methods | Eligible consenting women from one of 12 hospitals (1 US and 11 Canadian) were randomized through a central telephone answering service within strata defined by hospital and women's motivation to attempt vaginal delivery. Masking of outcome assessor was not described. | |
| Participants | Inclusion criteria: previous low transverse caesarean, gestational age < 28 weeks, planning to give birth in a participating hospital, receiving prenatal care from a physician in a participating hospital, knowledge of English or French sufficient to permit completion of a self‐administered questionnaire. Exclusion criteria: previous vaginal birth after caesarean, classic caesarean section or myomectomy scar, known multiple gestation. 1301 women were randomized, 1275 completed the study. No group differences were seen on characteristics measured at baseline. | |
| Interventions | Experimental: 'verbal' group (n = 641): offered an individualized prenatal education and support program that was provided by a research nurse with expertise in prenatal instruction and a resource person with strong communication skills and personal experience of a VBAC. The approach taken in providing the intervention was to consider the predisposing, enabling, and reinforcing factors for deciding to attempt a VBAC. Pain relief options for labour and methods for permanent contraception (for those considering tubal ligation at the time of the caesarean section) were discussed. Each of 2 contacts lasted approximately 1 hour. They usually occurred at 21 and 27 weeks' gestation. The first contact was provided to 98% of the group, the second was provided to 72% of those in the low motivation for VBAC stratum and 79% of those in the high motivation stratum. Control: 'document' group (n = 634): received a pamphlet highlighting the benefits of VBAC rather than an elective repeat caesarean section. | |
| Outcomes | Primary outcome: proportion of women achieving vaginal delivery. Other outcomes included: proportion attempting vaginal delivery, and maternal and neonatal morbidity. These data were obtained through medical record review. Women's sense of control over the birth experience was obtained as measured by the Birth Experience Rating Scale (shortened version of the Labour Agentry Scale, no reliability or validity data reported). This scale included 18 Likert‐type items, each with 7 steps resulting in a maximum total score of 126. | |
| Notes | Sample sizes by group were not presented for the Birth Experience Rating Scale thus prohibiting its inclusion in a meta‐analysis. Additional exploratory results were presented on sub‐groups defined by maternal motivation for VBAC. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
Hamilton‐Dodd 1989.
| Methods | Women were randomized to either the maternal preparation program or routine care. Randomization procedures were not described. Unclear whether outcome assessors were masked to group allocation. | |
| Participants | 22 women from a medical center in Coving, California, USA, were initially randomized. 6 women withdrew although no information is provided regarding when and from which group. Data were reported on 16 women who were successfully recruited and completed the study. Inclusion criteria were: participation approved by the physician, 18‐35 years old (inclusive), absence of major complications during pregnancy, women planning to be the primary caretakers of their infants for the first 2 months postbirth, predominantly anglophone. Exclusion criteria: major complications during birth, < 38 weeks' or > 41 weeks' gestation, 5‐minute Apgar < 7, birthweight < 2500 g, mental or physical anomalies identified at birth or during the project. Maternal age and caesarean birth rate (25%) were similar in both groups. Group differences were found in parity and infant gender. | |
| Interventions | Attendance (or lack thereof) at general childbirth education classes was not reported for any participants. Group A: maternal preparation program (n = 8). 4 individual sessions of 1 1/2 to 2 hours length were provided by 1 of 3 occupational therapists over a 3 to 7 week period beginning within 1 month prior to birth and finishing when the infant reached 2‐3 weeks of age. Content included activities of daily living incorporating the maternal role, infant development, physiological changes in the new mother, and mother‐infant relationship. In general, broad concepts were discussed rather than specific information. The occupational therapists were available for telephone inquiries. Group B: routine care (n = 8), not described. | |
| Outcomes | Maternal competence (measured by Ainsworth's 'System for Rating Maternal Care Behaviors'), adaptation to the maternal role (measured by Lederman's 'Postpartum Self Evaluation Questionnaire' and by Sheehan's 'Prenatal and Postnatal Questionnaire'), and satisfaction with the maternal role preparation provided with obstetrical care (measured by the Satisfaction with a Maternal Preparation Program Received in Conjunction with Obstetric Care Questionnaire). The System for Rating Maternal Care Behaviors consists of 7 general maternal care sub‐scales divided into a total of 22 behaviors rated on a scale of 1 to 9 with higher scores indicating greater competence. The Postpartum Self‐Evaluation Questionnaire is made up of 8 subscales containing 81 questions rated from 'very much so' (1) to 'not at all' (4). A ninth subscale was created by combining the last two. The Prenatal and Postnatal Questionnaire is a 10‐item Likert‐type Scale. The Satisfaction with a Maternal Preparation Program Received is a 24‐item Likert Scale . Total scores ranged from 24 to 120 with higher scores indicating greater satisfaction. | |
| Notes | Analyses of effects did not address the issue of clinically important baseline differences in parity and infant gender. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
Klerman 2001.
| Methods | Placebo/usual care controlled. It is unclear whether the participant, provider, and outcome assessor were masked. | |
| Participants | Included were: pregnant, African‐American women eligible for medicaid and seeking prenatal care from Jefferson County, AL, USA from 1994‐1996, scoring greater than 10 on a risk assessment scale, less than 26 weeks' gestational age, 16 years old, having had no major medical complications. Women having experienced alcoholism, high blood pressure, substance abuse, asthma, cancer, diabetes, epilepsy, sickle cell disease, or HIV/AIDS were excluded. Most participants were single. Groups were similar on baseline characteristics. 656 women enrolled in the trial, outcome data at birth were available for 619, postpartum interview data (year 2) were available for 118. | |
| Interventions | The experimental group (n = 318) received augmented care, including 16 interventions of which group education was only one. 40‐minute discussion groups and individual instruction were provided in a clinical setting. Written materials were distributed. Content focus was on pregnancy, peer social support, and health behavior education to minimize risk. Other supports for the experimental group (n = 318) included educationally‐oriented peer groups, additional appointments and extended time with clinicians. The control group (n = 301) received "usual care" including prenatal classes that were at different times and locations than clinic appointments. | |
| Outcomes | Perceived quality of prenatal care, average time with nurse, average time at clinic, same nurse reported as providing care each visit, nurse reported as "very helpful", knowledge of risk factors, self‐report of behavioral change, mean birthweight/age, low birthweight, mean gestational age, preterm birth, IUGR, low APGAR score, NICU, congenital anomalies, mean maternal weight gain, and caesarean deliveries. No measurement details were provided for questions posed to women. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | D ‐ Not used |
Mehdizadeh 2005.
| Methods | Women were randomized (no details given). | |
| Participants | 200 participants were recruited from Hedayat Hospital in Tehran, were under 35 years olds, and at 20 weeks' gestational age. The report states no statistically significant differences in demographic information by group (no data provided). | |
| Interventions | Women attended a total of 7 90‐minute classes which included 30 minutes of instruction on baby care, stages of labour, and diet, 30 minutes of counseling, and 30 minutes of neuromuscular exercises. | |
| Outcomes | Back or pelvic pain, length of labour, vaginal delivery, oxytocin, episiotomy, birthweight, increased daily activity, headache, and sleep disturbance. No measurement details were provided for questions posed to women. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | D ‐ Not used |
Pfannenstiel 1991.
| Methods | Randomized to 6 groups, 3 experimental and 3 placebo/usual care comparison groups. Randomization procedures were not described. Outcome assessors were masked to allocation. | |
| Participants | 67 men were recruited. Inclusion criterion: the mother had to agree to explain the study to the father. Of the 67 participating fathers, 22 of their partners were considered to be high medical risk. Their average age was 22.5 years, they had an average of 11 years of education, held unskilled and semi‐skilled positions, 70% were Caucasian, 88% were acquainted with their partners for over 1 year; 46% were married. There were reported to be no group differences at baseline on maternal or paternal age, maternal or paternal education, socioeconomic status (Hollingshead), or race. | |
| Interventions | 3 experimental groups: high‐risk pregnancy intervention with pre‐ and postmeasures (n = 11), low‐risk pregnancy intervention with pre‐ and postmeasures (n = 11), low‐risk pregnancy intervention with postmeasures only (n = 12). All 3 experimental groups received the same intervention: 2 1‐1/2 hour classes were presented to fathers through the hospital clinic, 57% attended the group sessions, 43% attended tutorials. The content included newborn care, normal newborn behaviour, paternal self‐image, attitude towards the infant, pregnancy, parent‐infant interactions, normal child development. The educational approach used was didactic and modeling. The background of the educators is not described. 3 control groups (n = 11 in each subgroup): content not described. | |
| Outcomes | Paternal sensitivity and empathetic behaviour (as measured by the Assessment of Father‐Infant Sensitivity scale) scored from 10 minute videotapes of infant feeding. The Assessment of Father‐Infant Sensitivity Scale incorporates 12 items, each item is rated on a 5‐point scale behaviorally defined from failure in behavioral empathy (scores 1,2) to relative failure alternating with sensitive responses (score 3) to sensitive/empathic behaviors (score 4,5). In addition, it includes ratings for 6 father‐plus‐infant items rated on a 5‐point scale with higher scores indicative of more sensitive and empathic behavior. Interrater reliability ranged from .72 to .85. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
Westney 1988.
| Methods | Randomization to experimental and placebo/usual care group, procedure not described. Masking to group allocation by provider or outcome assessor, or both, not described. | |
| Participants | 28 black, unmarried, 15‐18 year old prospective fathers recruited from public schools, adolescent prenatal clinics, recreation centers, other expectant fathers. Mean age did not differ by group. Reported not to differ on baseline knowledge. | |
| Interventions | Experimental: 4 2‐hour weekly prenatal classes addressing: human sexuality, pregnancy and prenatal care, labour and delivery, infant and child care. All were presented by a female registered nurse‐specialist in maternal‐child care. Teaching approaches included lectures, audiovisual aids, and group discussions of concerns. Control: no pregnancy‐related education program. | |
| Outcomes | Knowledge of human sexuality, pregnancy and prenatal care, labour and delivery, and infant and child care, measured using a 75‐item questionnaire developed for this study. One form of this questionnaire was administered at baseline, another at completion of the classes for the experimental group and at 4 weeks postbaseline for the control group. No reliability or validity data were provided for this questionnaire. The range of possible scores was not given. It appears that the higher the score, the greater the knowledge. | |
| Notes | The knowledge score means and standards deviations used in this review were taken from Table 2 of the article. Unfortunately, the labelling of that table (4 rows of data, each only partially labelled) prohibits the reader from being fully certain that the scores used in this review are correct. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
IUGR: intrauterine growth retardation NICU: neonatal intensive care unit VBAC: vaginal birth after caesarean section
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Astbury 1980 | 90 primigravidae women, half attending childbirth education classes, half not, were randomly assigned once in hospital in labour to either standard care, music, or information groups. Effects on anxiety were assessed; no standard deviations were reported thereby prohibiting inclusion of these data in the current review. No other outcomes were reported. |
| Beck 1980 | Participants were randomized to standard Lamaze preparation (n = 37) or Lamaze plus group desensitization to a hierarchy of labour and delivery‐related scenes (n = 30). These groups were compared to each other and to self‐selected controls. Only those participants who attended at least 4 of the 8 sessions were included in the data analyses, prohibiting an intention‐to‐treat analysis. Outcome data are not usable as presented, in that only correlations and F statistics are provided, and means and standard deviations cannot be calculated. |
| Bjornson 1997 | The aim of this study was to determine whether a video about infant immunization could inform parents as well as an oral presentation. There was no control condition permitting an assessment of the effects of education, the focus of the current review. |
| Calabro 1996 | The aim of this study was to determine whether health education materials in both English and Spanish were more effective when written at a lower rather than a higher reading level. The focus of the education material was to discourage alcohol use during pregnancy. There was no control condition permitting an assessment of the effects of education, the focus of the current review. |
| Carson 1984 | 69 women were randomized to one of three groups: relaxation (in which relaxation techniques for labour were taught); abdominal palpation (in which identification of the fetal position and massage were taught); and control. The objective of the study was to determine if abdominal palpation of the fetus would increase maternal attachment behavior. Published data include the mean number of attachment behaviors observed (relaxation, 159, palpation, 156, control 142); no standard deviations are reported thereby prohibiting inclusion of these data in the current review. Caesarean birth rate and breastfeeding data are only reported for the 3 groups combined. |
| Chang 1987 | Not a randomized controlled trial. This was a controlled experiment in which 1 of 4 childbirth classes was provided with a pamphlet on seatbelt use, another received the pamphlet and 15‐minute instruction, and the remaining 2 served as controls. There was no random assignment of individuals or groups to an intervention. |
| Cogan 1982 | Childbirth education teachers, rather than parents, were randomly assigned to an experimental group which received communication skills training. |
| D'Andrea 1994 | Inner city African‐American pregnant adolescents were randomized to receive either individual counseling and educational and community outreach‐referral services (n = 32) or usual care (n = 32). Program effects on social networks and self‐concept were assessed; no standard deviations were reported thereby prohibiting inclusion of these data in the current review. No other effects were assessed. |
| Dalzell 1965 | Not a randomized controlled trial. Each new participant was successively assigned to either prenatal classes, home visits, individual counseling, or a control group. |
| De Nuncio 2000 | 352 Latinas from two clinics in San Diego County were recruited and randomized to experimental and placebo/control care groups at the 34‐36 week prenatal visit. The experimental intervention included immunization education; the control intervention was education to prevent SIDS. Group sizes were not reported, thereby prohibiting inclusion of these data in the current review. |
| Durham 1986 | Unit of analysis error and outcome data are not usable as presented. Published data are presented as the number of times medication was used to reduce pain summed for the entire group rather than for the individuals within the group (i.e., not analyzed based on the unit of randomization). Group means and standard deviations cannot be calculated. |
| Escott 2005 | The aim of this study was "to compare the use and effects of enhanced pre‐existing coping strategies with the use and effects of coping strategies usually taught in National Health Service (NHS) antenatal education on women's experience of pain and emotions during labour". There was no control condition permitting an assessment of the effects of education, the focus of the current review. |
| Ferland 1981 | There was not random assignment to groups; "2 of the classes constituted the experimental group (n = 19); the 2 remaining classes, the control group (n = 22)". |
| Fischer 1972 | Not a randomized controlled trial. Primiparous women were assigned to classes or a control condition based on their expected dates of delivery. |
| Ford 2002 | 282 14‐20 year old primarily single women were recruited from 5 different urban clinics in the US. The intervention was mastery modeling and peer support. A group of 6‐8 pregnant girls were paired with other pregnant teens with similar due dates. The intervention took place in a clinic setting. Social cognition theory provided the theoretical basis for the classes, which introduced modeling and rehearsing skills to achieve the following: 1) increased knowledge about pregnancy, 2) preparation for childbirth, 3) working with the healthcare system, 4) assessing adolescent and infant health, and 5) preventing unplanned pregnancy. Normal first labour, birth, and exercise were included. Intervention and control groups received written material. The control group received individual instruction. The distribution of age and "race" differed by group, bringing into question the randomization procedure. Group sizes were not reported, thereby prohibiting inclusion of these data in the current review. |
| Glazier 1997 | The interventions compared were written ones: a pamphlet on triple marker screening versus one on activities of daily living during pregnancy. No information sharing by persons (as in a class or one‐to‐one teaching) was tested. |
| Goodson 1985 | Not a randomized controlled trial. Alternate prenatal classes were assigned a 30‐minute lecture on child passenger safety. There was no random assignment of individuals or groups to an intervention. |
| Leitch 1999 | Data presented is incompatible with Review Manager analysis methods. |
| Linares 2006 | 255 women were randomized to the standard arm (a standard educational sheet about a particular pregnancy‐related topic) and 370 to the intervention arm (an educational sheet with gestational age‐specific information, an explanation of the importance of next appointment, and a section of the woman's individual medical or pregnancy complications). Effects on missed appointments were assessed; no data by group were presented thereby prohibiting inclusion of these data in the current review. |
| Manandhar 2004 | This is a study of a community‐based participatory intervention meant to reduce neonatal mortality and is outside the realm of this review. |
| McEnery 1986 | Strong likelihood of selection bias and absence of an intention‐to‐treat analysis. 105 women initially volunteered for the study. 69 appear to have been randomized (35 to the 'educated' group and 34 to the 'not educated' group) although the point in the process at which this was done is unclear since reasons for exclusion include 'infant not examined at 1 year'. 19 women from the experimental group who did not attend more than 3 classes were moved to the control group for analyses leaving 16 in the 'educated' and 53 in the 'not educated' groups. |
| Midmer 1995 | Possible selection bias. Couples were reportedly randomized to receive either two classes on parenting communication in addition to usual childbirth education (experimental group) or usual childbirth education (control group). The authors state that "each couple had an equal probability of being randomized to the experimental group or the control group...". However, later in the text, the authors state "...more [were] assigned to the experimental group to ensure adequate class size..." (experimental group n = 41 couples, 58‐62 individuals were analyzed; control group n = 29 couples, 42‐45 individuals analyzed). The method of assignment to assure equal class size was not specified. Outcome data are not usable as presented. Published data include means without standard deviations. |
| Nichols 1987 | No outcome data are provided. |
| O'Cathain 2002 | This was a cluster‐randomized controlled trial with a written intervention. Leaflets on promoting informed choice in women using maternity services were used. Information sharing by persons (as in a class or one‐to‐one relationship) was not tested. The intervention is beyond the scope of this review. |
| Petrowski 1981 | Strong likelihood of selection bias and attrition bias. 56 women were initially randomized, 20 were subsequently lost, leaving 36 across 4 treatment conditions. 4 were subsequently non‐randomly added to obtain 4 groups of 10 each. Outcome data are not usable as presented. Published data include F statistics only; means and standard deviations can not be calculated. |
| Polley 2002 | This study focuses on limiting weight gain during pregnancy. The objective of it was to determine whether a stepped care behavioral intervention would decrease the percentage of women who gain more than the Institute of Medicine recommendation. The intervention is beyond the scope of the current review. |
| Schachman 2004 | US military wives were randomized to traditional childbirth education or "baby boot camp" (a childbirth‐parenting preparation program based on a resilience paradigm), thereby prohibiting an assessment of effects, the focus of this review. |
| Schonberger 2004 | Study intervention is focused on reducing newborn exposure to allergens and smoke, not a focus of this review. |
| Spence‐Cagle 1984 | All couples received regular Lamaze classes and were subsequently randomized to receive "added interpersonal needs content" to determine if the later might increase "love scores". No data were provided in the report. |
| Springer 1996 | Uses women attending childbirth classes as the population from which they drew their sample. Individuals were not randomized. This article does not evaluate antenatal education. |
| St. James‐Roberts | Women attendees of childbirth education classes were "randomly assigned to EMG and SCL biofeedback groups and to two equivalently sized control groups such that age, social class, and [anxiety] scores were counterbalanced across groups... group sizes were 13 SCL, 13 SCL‐control, 11 EMG, and 11 EMG‐control". The effects of childbirth education itself, the focus of this review, were not assessed. |
| Sullivan 1984 | 99 pregnant women were randomly assigned to receive either four self‐directed programmed instruction booklets with slides (experimental intervention) or no intervention (control). Since the intervention was not provided by an individual, the focus of the current review, it was excluded. Outcome data were also not presented in a format suitable for this review. Published data include mean group knowledge scores (experimental, 47.75; control, 27.57) without standard deviations. Degrees of freedom, mean square, f statistic and P values of an analysis of variance of a 3 x 2 factorial design were also reported. |
| Timm 1979 | Outcome data are not usable as presented and attrition bias may be present. Published data includes mean birthweight adjusted for gestational age without standard deviations. No other means or standard deviations are provided or can be calculated. Of 146 women agreeing to participate, 118 completed the study; numbers were unevenly distributed by group (Group A n = 40, Group B n = 31, Group C n = 47), suggesting attrition bias. |
| Turan 2001 | Couples in Istanbul, Turkey were randomized to an antenatal education program in a couple's group, a women‐only group, or a men‐only group. They received group educational sessions, a booklet, and a telephone counseling service. Outcomes included men's knowledge regarding breastfeeding, preventative healthcare, and family planning as well as contraceptive use. The number of subjects analyzed at follow up was not reported. |
| Washington 1983 | Outcome data are not usable as presented and attrition bias may be present. Published data include mean knowledge acquisition (experimental group, 13.2; control group, 10.3) without standard deviations and standard deviations can not be calculated. Of 68 women randomized, data are presented on 40, 20 having attended classes and 20 not. The 28 lost were unaccounted. The author reports the mean difference as being statistically significant. |
| Zhang 1996 | The experimental intervention is unclear; attempts to contact the trial author for further information have been unsuccessful. |
| Zimmermann‐Tansella | The aim of this study was to determine the effects of Respiratory Autogenic Training versus traditional psychoprophylaxis on relaxation and anxiety during the course, and pain and behaviour during birth. There was no control condition permitting an assessment of the effects of education, the focus of the current review. |
EMG: electromyographic SCL: skin conductance level SIDS: sudden infant death syndrome
Contributions of authors
For the update, Jane Sandall and Anita J Gagnon (AJG) collaborated on assessing the quality of and extracting the data for included studies. AJG conducted the quantitative analyses. AJG previously prepared the protocol and undertook the initial review, applying the inclusion criteria and extracting data for the included studies for the first version of this review.
Sources of support
Internal sources
McGill University, Montreal, Canada.
McGill University Health Centre ‐ Montreal, Canada.
The SMBD Jewish General Hospital (for initial review), Montreal, Canada.
King's College, London, UK.
External sources
Le Fonds de la recherche en santé du Québec (FRSQ), Canada.
La Fondation de recherche en sciences infirmières du Québec (FRESIQ)(for initial review), Canada.
Groupe de recherche interuniversitaire en sciences infirmieres de Montreal (GRISIM), Canada.
Declarations of interest
None known.
Edited (no change to conclusions)
References
References to studies included in this review
Carter‐Jessop 1981 {published data only}
- Carter‐Jessop L. Promoting maternal attachment through prenatal intervention. MCN. The American Journal of Maternal Child Nursing 1981;6:107‐12. [DOI] [PubMed] [Google Scholar]
Corwin 1999 {published data only}
- Corwin A. Integrating preparation for early parenting into childbirth education: Part I ‐ A curriculum. Journal of Perinatal Education 1998;7(4):26‐33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corwin A. Integrating preparation for parenting into childbirth education: Part II ‐ A study. Journal of Perinatal Education 1999;8(1):22‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Davis 1987 {published data only}
- Davis MS, Akridge KM. The effect of promoting intrauterine attachment in primparas on postdelivery attachment. Journal of Obstetric, Gynecologic and Neonatal Nursing 1987;16(6):430‐7. [DOI] [PubMed] [Google Scholar]
Fraser 1997 {published data only}
- Fraser W, Maunsell E, Hodnett E, Moutquin JM, Childbirth Alternatives Post‐Cesarean Study Group. Randomized controlled trial of a prenatal vaginal birth after cesarean section education and support program. American Journal of Obstetrics and Gynecology 1997;176(2):419‐25. [DOI] [PubMed] [Google Scholar]
Hamilton‐Dodd 1989 {published data only}
- Hamilton‐Dodd C, Kawamoto T, Clark F, Burke JP, Fanchiang SP. The effects of a maternal preparation program on mother‐infant pairs: a pilot study. American Journal of Occupational Therapy 1989;43(8):513‐21. [DOI] [PubMed] [Google Scholar]
Klerman 2001 {published data only}
- Klerman LV, Ramey SL, Goldenberg RL, Marbury S, Hou J, Clirer SP. A randomized trial of augmented prenatal care for multiple‐risk, medicaid eligible African‐American women. American Journal of Public Health 2001;91(1):105‐11. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mehdizadeh 2005 {published data only}
- Mehdizadeh A, Roosta F, Chaichian S, Alaghehbandan R. Evaluation of the impact of birth preparation on the health of the mother and the newborn. American Journal of Perinatology 2005;22(1):7‐9. [DOI] [PubMed] [Google Scholar]
Pfannenstiel 1991 {published data only}
- Pfannenstiel AE, Honig AS. Prenatal intervention and support for low‐income fathers. Infant Mental Health Journal 1991;12(2):103‐15. [Google Scholar]
Westney 1988 {published data only}
- Westney OE, Cole OJ, Munford T. The effects of prenatal education intervention on unwed prospective adolescent fathers. Journal of Adolescent Health Care 1988;9(3):214‐8. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Astbury 1980 {published data only}
- Astbury, J. The crisis of childbirth: can information and childbirth education help?. Journal of Psychosomatic Research 1980;24(1):9‐13. [DOI] [PubMed] [Google Scholar]
Beck 1980 {published data only}
- Beck NC, Siegel LJ, Davidson NP, Kormeier S, Breitenstein A, Hall DG. The prediction of pregnancy outcome: maternal preparation, anxiety and attitudinal sets. Journal of Psychosomatic Research 1980;24:343‐51. [DOI] [PubMed] [Google Scholar]
Bjornson 1997 {published data only}
- Bjornson GL, Scheifele DW, Gold R. Assessment of parent education methods for infant immunization. Canadian Journal of Public Health 1997;88(6):405‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Calabro 1996 {published data only}
- Calabro K, Taylor WC, Kapadia A. Pregnancy, alcohol use and the effectiveness of written health education materials. Patient Education and Counseling 1996;29:301‐9. [DOI] [PubMed] [Google Scholar]
Carson 1984 {published data only}
- Carson K, Virden S. Can prenatal teaching promote maternal attachment? Practicing nurses test Carter‐Jessop's prenatal attachment intervention. Health Care for Women International 1984;5:355‐69. [DOI] [PubMed] [Google Scholar]
Chang 1987 {published data only}
- Chang A, Magwene K, Frand E. Increased safety belt use following education in childbirth classes. Birth 1987;14:148‐52. [DOI] [PubMed] [Google Scholar]
Cogan 1982 {published data only}
- Cogan R, Winer JL. Effect of childbirth educator communication skills training on postpartum reports of parents. Birth 1982;9(4):241‐4. [Google Scholar]
D'Andrea 1994 {published data only}
- D'Andrea M. The family development project: a comprehensive mental health counseling program for pregnant adolescents. Journal of Mental Health Counseling 1994;16:184‐95. [Google Scholar]
Dalzell 1965 {published data only}
- Dalzell I. Evaluation of a prenatal teaching program. Nursing Research 1965;14:160‐3. [DOI] [PubMed] [Google Scholar]
De Nuncio 2000 {published data only}
- Zuniga de Nuncio MZ. A prospective randomized study to determine the effects of a prenatal immunization intervention on timeliness of infant immunization schedule initiation in two San Diego County community clinics [dissertation]. University of California, San Diego and San Diego State University, 2000. [Google Scholar]
- Nuncio MZ, Nader P, Sawyer M, Guire M, Prislin R, Elder J. A prospective randomized study to determine the effects of a prenatal immunization intervention on timeliness of immunization initiation in Latino infants in two San Diego county community clinics. Pediatric Research 2000;47:237A. [Google Scholar]
- Nuncio MZ, Nader P, Sawyer M, Guire M, Prislin R, Elder J. A prospective randomized study to determine the effects of a prenatal immunization intervention on timeliness of immunization initiation in Latino infants in two San Diego county community clinics [abstract]. Pediatric Academic Society Annual Meeting; 2000 May 12‐16; Boston, MA, USA. 2000.
- Nuncio MZ, Nader PR, Sawyer MH, Guire M, Prislin R, Elder JP. A prenatal intervention study to improve timeliness of immunization initiation in Latino infants. Journal of Community Health 2003;28:151‐65. [DOI] [PubMed] [Google Scholar]
Durham 1986 {published data only}
- Durham L, Collins M. The effect of music as a conditioning aid in prepared childbirth education. Journal of Obstetric, Gynecologic and Neonatal Nursing 1986;15(3):268‐70. [DOI] [PubMed] [Google Scholar]
Escott 2005 {published data only}
- Escott D, Slade P, Spiby H, Fraser RB. Preliminary evaluation of a coping strategy enhancement method of preparation for labour. Midwifery 2005;21(3):278‐91. [DOI] [PubMed] [Google Scholar]
Ferland 1981 {published data only}
- Ferland F, Piper MC. Evaluation of a sensory‐motor education programme for 'parents‐to‐be'. Child Care, Health and Development 1981;7:245‐54. [DOI] [PubMed] [Google Scholar]
Fischer 1972 {published data only}
- Fischer WM, Huttel FA, Mitchell I, Meyer AE. The efficacy of the psychoprophylactic method of prepared childbirth. Proceedings of 3rd International Congress on Psychosomatic Medicine in Obstetrics and Gynaecology; 1972; London, UK. 1972:38‐44.
Ford 2002 {published data only}
- Ford K, Weglicki L, Kershaw T, Schram C, Hoyer PJ, Jacobsen ML. Effects of prenatal care intervention for adolescent mothers on birth weight, repeat pregnancy, and educational outcomes at one year postpartum. Journal of Perinatal Education 2002;11(1):35‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Glazier 1997 {published data only}
- Glazier R, Goel V, Holzapfel S, Summers A, Pugh P, Yeung M. Written patient information about triple‐marker screening: a randomized controlled trial. Obstetrics & Gynecology 1997;90(5):769‐74. [DOI] [PubMed] [Google Scholar]
Goodson 1985 {published data only}
- Goodson JG, Buller C, Goodson WH. Prenatal child safety education. Obstetrics & Gynecology 1985;65:312‐5. [PubMed] [Google Scholar]
Leitch 1999 {published data only}
- Leitch, D. Mother‐infant interaction: achieving synchrony. Nursing Research 1999;48(1):55‐8. [DOI] [PubMed] [Google Scholar]
Linares 2006 {published data only}
- Linares ST, Pierce TJ, Phatak DG, Riggs JW, Hollier LM. A randomized trial of personalized prenatal education [abstract]. Obstetrics & Gynecology 2006;107(4 Suppl):71S. [Google Scholar]
Manandhar 2004 {published data only}
- Borghi J, Thapa B, Osrin D, Jan S, Morrison J, Tamang S, et al. Economic assessment of a women's group intervention to improve birth outcomes in rural Nepal. Lancet 2005;366(9500):1882‐4. [DOI] [PubMed] [Google Scholar]
- Manandhar D, Osrin D, Shrestha BP, Mesko N, Morrison J, Tumbahangphe KM, et al. Effect of participatory intervention with women's groups on birth outcomes in nepal: cluster randomised controlled trial. Lancet 2004;364:970‐9. [DOI] [PubMed] [Google Scholar]
- Osrin D, Mesko N, Shrestha BP, Shrestha D, Tamang S, Thapa S, et al. Reducing childhood mortality in poor countries. Transactions of the Royal Society of Tropical Hygiene and Medicine 2003;97:18‐21. [DOI] [PubMed] [Google Scholar]
McEnery 1986 {published data only}
- McEnery G, Rao KPS. The effectiveness of antenatal education of Pakistani and Indian women living in this country. Child Care, Health and Development 1986;12:385‐99. [DOI] [PubMed] [Google Scholar]
Midmer 1995 {published data only}
- Midmer D, Wilson L, Cummings S. A randomized, controlled trial of the influence of prenatal parenting education on postpartum anxiety and marital adjustment. Family Medicine 1995;27(3):200‐5. [PubMed] [Google Scholar]
Nichols 1987 {published data only}
- Nichols FH. The psychological effects of prepared childbirth on self‐esteem, active participation during childbirth, and childbirth satisfaction of single adolescent mothers. Journal of Obstetric, Gynecologic and Neonatal Nursing 1987;1(1):207‐8. [Google Scholar]
O'Cathain 2002 {published data only}
- O'Cathain A, Walters SJ, Nicholl JP, Thomas KJ, Kirkham M. Use of evidence‐based leaflets to promote informed choice in maternity care: randomised controlled trial in everyday practice. BMJ 2002;324:1‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Petrowski 1981 {published data only}
- Petrowski DD. Effectiveness of prenatal and postnatal instruction in postpartum care. Journal of Obstetric, Gynecologic and Neonatal Nursing 1981;10(5):386‐9. [DOI] [PubMed] [Google Scholar]
Polley 2002 {published data only}
- Polley BA, Wing RR, Sims CJ. Randomised controlled trial to prevent excessive weight gain in pregnant women. International Journal of Obesity 2002;26:1494‐502. [DOI] [PubMed] [Google Scholar]
Schachman 2004 {published data only}
- Schachman KA, Lee RK, Lederman RP. Baby boot camp: facilitating maternal role adaptation among military wives. Nursing Research 2004;53(2):107‐15. [DOI] [PubMed] [Google Scholar]
Schonberger 2004 {published data only}
- Schonberger HJ, Maas T, Dompeling E, Knottnerus JA, Weel C, Schayck CP. Compliance of asthmatic families with a primary prevention programme of asthma and effectiveness of measures to reduce inhalant allergens ‐ a randomized trial. Clinical and Experimental Allergy 2004;34:1024‐31. [DOI] [PubMed] [Google Scholar]
Spence‐Cagle 1984 {published data only}
- Spence‐Cagle C. Changed interpersonal needs of the pregnant couple: nursing roles. Journal of Obstetric, Gynecologic and Neonatal Nursing 1984;13:56. [Google Scholar]
Springer 1996 {published data only}
- Springer, D. Birth plans: the effect on anxiety in pregnant women. International Journal of Childbirth Education 1996;11(3):20‐5. [Google Scholar]
St. James‐Roberts {published data only}
- James‐Roberts I, Chamberlain G, Haran FJ, Hutchinson CMPA. Use of electromyographic and skin‐conductance biofeedback relaxation training to facilitate childbirth in primiparae. Journal of Psychosomatic Research 1982;26(4):455‐62. [DOI] [PubMed] [Google Scholar]
Sullivan 1984 {published data only}
- Sullivan PL. Designed instruction for pregnant women: its effect on their learning. Health Care for Women International 1984;5:1‐27. [DOI] [PubMed] [Google Scholar]
Timm 1979 {published data only}
- Timm MM. Prenatal education evaluation. Nursing Research 1979;28(6):338‐42. [DOI] [PubMed] [Google Scholar]
Turan 2001 {published data only}
- Turan JM, Nalbant H, Bulut A, Sahip Y. Including expectant fathers in antenatal education programmes in Istanbul, Turkey. Reproductive Health Matters 2001;9(18):114‐25. [DOI] [PubMed] [Google Scholar]
Washington 1983 {published data only}
- Washington WN, Stafford VM, Stomsvik J, Giannini C. Prenatal education for the Spanish speaking: an evaluation. Patient Education and Counseling 1983;5(1):30‐4. [DOI] [PubMed] [Google Scholar]
Zhang 1996 {published data only}
- Zhang CL, Yu ZJ, Feng AH. Study of psychological nursing to ease pain during labor. Chinese Journal of Nursing 1996;31(6):311‐3. [PubMed] [Google Scholar]
Zimmermann‐Tansella {published data only}
- Zimmermann‐Tansella C, Dolcetta G, Azzini V, Zacche G, Bertagni P, Siani R, et al. Preparation courses for childbirth in primipara. A comparison. Journal of Psychosomatic Research 1979;23:227‐33. [DOI] [PubMed] [Google Scholar]
References to studies awaiting assessment
Ahmadian 2009 {published data only}
- Ahmadian heris S, Taghavi S, Hoseininasab D. The effect of antenatal education interventions on state‐trait anxiety in the parturition process. International Journal of Gynecology & Obstetrics 2009;107(Suppl 2):S548. [Google Scholar]
Aracena 2009 {published data only}
- Aracena M, Krause M, Perez C, Mendez MJ, Salvatierra L, Soto M, et al. A cost‐effectiveness evaluation of a home visit program for adolescent mothers. Journal of Health Psychology 2009;14(7):878‐87. [DOI] [PubMed] [Google Scholar]
Barlow 2006 {published data only}
- Barlow A, Varipatis‐Baker E, Speakman K, Ginsburg G, Friberg I, Goklish N, et al. Home‐visiting intervention to improve child care among American Indian adolescent mothers: a randomized trial. Archives of Pediatrics and Adolescent Medicine 2006;160(11):1101‐7. [DOI] [PubMed] [Google Scholar]
Bergstrom 2009 {published data only}
- Bergstrom M, Kieler H, Waldenstrom U. Effects of natural childbirth preparation versus standard antenatal education on epidural rates, experience of childbirth and parental stress in mothers and fathers: a randomised controlled multicentre trial. BJOG: an international journal of obstetrics and gynaecology 2009;116(9):1167‐76. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bergstrom 2009a {published data only}
- Bergstrom M, Kieler H, Waldenstrom U. Effects of natural childbirth preparation versus standard antenatal education on epidural rates, experience of childbirth and parental stress in mothers and fathers: a randomised controlled multicentre trial. International Journal of Gynecology & Obstetrics 2009;107(Suppl 2):S546. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bergstrom 2010 {published data only}
- Bergstrom M, Kieler H, Waldenstrom U. Psychoprophylaxis during labor: associations with labor‐related outcomes and experience of childbirth. Acta Obstetricia et Gynecologica Scandinavica 2010;89(6):794‐800. [DOI] [PubMed] [Google Scholar]
Delaram 2009 {published data only}
- Delaram M. The effects of consultation with mother in third trimester of pregnancy on pregnancy outcomes. Iranian Registry of Clinical Trials (http://www.irct.ir/) (accessed 6 December 2010) 2009.
Doan 2007 {published data only}
- Doan T, Gardiner A, Gay CL, Lee KA. Breast‐feeding increases sleep duration of new parents. Journal of Perinatal & Neonatal Nursing 2007;21(3):200‐6. [DOI] [PubMed] [Google Scholar]
Doherty 2006 {published data only}
- Doherty WJ, Erickson MF, LaRossa R. An intervention to increase father involvement and skills with infants during the transition to parenthood. Journal of Family Psychology 2006;20(3):438‐47. [DOI] [PubMed] [Google Scholar]
Fagan 2008 {published data only}
- Fagan J. Randomized study of a prebirth coparenting intervention with adolescent and young fathers. Family Relations 2008;57:308‐23. [Google Scholar]
Feinberg 2008 {published data only}
- Feinberg ME, Kan ML. Establishing family foundations: intervention effects on coparenting, parent/infant well‐being, and parent‐child relations. Journal of Family Psychology 2008;22(2):253‐63. [DOI] [PMC free article] [PubMed] [Google Scholar]
Fisher 2009 {published data only}
- Fisher B, Esplin S, Stoddard G, Silver R. Randomized controlled trial of hypnobirthing versus standard childbirth classes: patient satisfaction and attitudes towards labor. American Journal of Obstetrics and Gynecology 2009;201(6 Suppl 1):S61‐2. [Google Scholar]
Gao 2010 {published data only}
- Gao LL, Chan SW, Li X, Chen S, Hao Y. Evaluation of an interpersonal‐psychotherapy‐oriented childbirth education programme for Chinese first‐time childbearing women: a randomised controlled trial. International Journal of Nursing Studies 2010;47(10):1208‐16. [DOI] [PubMed] [Google Scholar]
Gjerdingen 2002 {published data only}
- Gjerdingen DK, Center B. A randomized controlled trial testing the impact of a support/work‐planning intervention on first‐time parents' health, partner relationship, and work responsibilities. Behavioral Medicine 2002;28(3):84‐91. [DOI] [PubMed] [Google Scholar]
Halford 2010 {published data only}
- Halford WK, Petch J, Creedy DK. Promoting a positive transition to parenthood: a randomized clinical trial of couple relationship education. Prevention Science 2010;11(1):89‐100. [DOI] [PubMed] [Google Scholar]
Hawkins 2006 {published data only}
- Hawkins AJ, Fawcett EB, Carroll JS, Gilliland TT. The marriage moments program for couples transitioning to parenthood: divergent conclusions from formative and outcome evaluation data. Journal of Family Psychology 2006;20(4):561‐70. [DOI] [PubMed] [Google Scholar]
Hemminki 2007 {published data only}
- Hemminki E. A randomised trial of childbirth classes to reduce caesarean rates (ongoing trial) [Synnytysvalmennus keisarinleikkausten vahentajana ‐ uuden valmennussisallon arviointi kokeellisessa tutkimuksessa]. Current Controlled Trials (www.controlled‐trials.com) (accessed 15 February 2007) 2007.
Hoseininasab 2009 {published data only}
- Hoseininasab D, Ahmadian heris S, Taghavi S. The effect of antenatal education on postpartum depression. International Journal of Gynecology & Obstetrics 2009;107(Suppl 2):S607‐8. [Google Scholar]
Hoyer 1994 {published data only}
- Hoyer PJ, Jacobson M, Ford K, Walsh E. Pregnancy care for the adolescent. Nurse Practitioner 1994;19(4):27‐8, 31‐2. [DOI] [PubMed] [Google Scholar]
Ickovics 2007 {published data only}
- Ickovics JR, Kershaw TS, Westdahl C, Magriples U, Massey Z, Reynolds H, et al. Group prenatal care and perinatal outcomes: a randomized controlled trial. Obstetrics & Gynecology 2007;110(2 Pt 1):330‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ip 2009 {published data only}
- Ip WY, Tang CS, Goggins WB. An educational intervention to improve women's ability to cope with childbirth. Journal of Clinical Nursing 2009;18(15):2125‐35. [DOI] [PubMed] [Google Scholar]
Jennings 2010 {published data only}
- Jennings L, Yebadokpo AS, Affo J, Agbogbe M. Antenatal counseling in maternal and newborn care: use of job aids to improve health worker performance and maternal understanding in Benin. BMC Pregnancy and Childbirth 2010;10:75. [DOI] [PMC free article] [PubMed] [Google Scholar]
Johnston 2001 {published data only}
- Johnston BD, Thompson RS, Huebner CE, Barlow WE, Tyll L. Expanded well‐child care with a pre‐natal component: early results from the group health evaluation of "healthy steps" [abstract]. Pediatric Research 2001;49(4):132A. [Google Scholar]
Jungmann 2010 {published data only}
- Jungmann T, Kurtz V, Brand T, Sierau S, Klitzing K. Child health as a prevention objective in the context of the pilot project "Pro Kind". Preliminary results of a randomized controlled trial [Praventionasziel Kindergesundheit im Rahmen des Modellprojektes ,,Pro Kind'' Vorlaufige Befunde einer langsschnittlichen, randomisierten Kontrollgruppenstudie]. Bundesgesundheitsblatt, Gesundheitsforschung, Gesundheitsschutz 2010;53(11):1180‐7. [DOI] [PubMed] [Google Scholar]
Kershaw 2009 {published data only}
- Kershaw TS, Magriples U, Westdahl C, Schindler Rising S, Ickovics J. Pregnancy as a window of opportunity for HIV prevention: effects of an HIV intervention delivered within prenatal care. American Journal of Public Health 2009;99(11):2079‐86. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kuo 2009 {published data only}
- Kuo SC, Chen YS, Lin KC, Lee TY, Hsu CH. Evaluating the effects of an Internet education programme on newborn care in Taiwan. Journal of Clinical Nursing 2009;18(11):1592‐601. [DOI] [PubMed] [Google Scholar]
Kuo 2010 {published data only}
- Kuo SC, Lin KC, Hsu CH, Yang CC, Chang MY, Tsao CM, et al. Evaluation of the effects of a birth plan on Taiwanese women's childbirth experiences, control and expectations fulfilment: a randomised controlled trial. International Journal of Nursing Studies 2010;47(7):806‐14. [DOI] [PubMed] [Google Scholar]
Lasater 2006 {published data only}
- Lasater T. Reducing ETS exposure of pregnant women and newborns (ongoing trial). ClinicalTrials.gov (http://clinicaltrials.gov/) (accessed 21 March 2006) 2006.
Lee 2006 {published data only}
- Lee KO, Kim KR, Ahn SH. Effects of a Qigong prenatal education program on anxiety, depression and physical symptoms in pregnant women. Korean Journal of Women Health Nursing 2006;12(3):240‐8. [Google Scholar]
Li 2009 {published data only}
- Li HT, Lin KC, Chang SC, Kao CH, Liu CY, Kuo SC. A birth education program for expectant fathers in Taiwan: effects on their anxiety. Birth 2009;36(4):289‐96. [DOI] [PubMed] [Google Scholar]
Liu 2009 {published data only}
- Liu N, Mao L, Sun X, Liu L, Yao P, Chen B. The effect of health and nutrition education intervention on women's postpartum beliefs and practices: a randomized controlled trial. BMC Public Health 2009;9:45. [DOI] [PMC free article] [PubMed] [Google Scholar]
Maimburg 2010 {published data only}
- Maimburg RD, Vaeth M, Durr J, Hvidman L, Olsen J. Randomised trial of structured antenatal training sessions to improve the birth process. BJOG: an international journal of obstetrics and gynaecology 2010;117(8):921‐8. [DOI] [PubMed] [Google Scholar]
Marsiglia 2010 {published data only}
- Marsiglia FF, Bermudez‐Parsai M, Coonrod D. Familias Sanas: an intervention designed to increase rates of postpartum visits among Latinas. Journal of Health Care for the Poor and Underserved 2010;21(3 Suppl):119‐31. [DOI] [PMC free article] [PubMed] [Google Scholar]
McEnery 1986a {published data only}
- McEnery G, Rao KP. The effectiveness of antenatal education of Pakistani and Indian women living in this country. Child Care, Health and Development 1986;12:385‐99. [DOI] [PubMed] [Google Scholar]
Mirmolaei 2010 {published data only}
- Mirmolaei ST, Moshrefi M, Kazemnejad A, Morteza H. Effect of antenatal preparation courses on the health behaviors of pregnant women. Journal of Maternal‐Fetal and Neonatal Medicine 2010;23(S1):138. [Google Scholar]
Mullany 2007 {published data only}
- Mullany BC, Becker S, Hindin MJ. The impact of including husbands in antenatal health education services on maternal health practices in urban Nepal: results from a randomized controlled trial. Health Education Research 2007;22(2):166‐76. [DOI] [PubMed] [Google Scholar]
Mullany 2009 {published data only}
- Mullany BC, Lakhey B, Shrestha D, Hindin MJ, Becker S, Mullany BC, et al. Impact of husbands' participation in antenatal health education services on maternal health knowledge: Impact of husbands' participation in antenatal health education services on maternal health knowledge. Journal of the Nepal Medical Association 2009;48(173):28‐34. [PubMed] [Google Scholar]
Ngai 2009 {published data only}
- Ngai FW, Chan SW, Ip WY. The effects of a childbirth psychoeducation program on learned resourcefulness, maternal role competence and perinatal depression: a quasi‐experiment. International Journal of Nursing Studies 2009;46(10):1298‐306. [DOI] [PubMed] [Google Scholar]
Noronha 2004 {published data only}
- Noronha JA. Effectiveness of teaching on episiotomy & perineal care among primipara women of selected hospitals in Karnataka. The Nursing Journal of India 2004;95(5):105‐6. [PubMed] [Google Scholar]
Phipps 2007 {published data only}
- Phipps H, Charlton S, Dietz HP. Can antenatal education influence how women push in labour? [abstract]. Journal of Paediatrics and Child Health 2007;43(Suppl 1):A67‐8. [DOI] [PubMed] [Google Scholar]
Phipps 2009 {published data only}
- Phipps H, Charlton S, Dietz HP. Can antenatal education influence how women push in labour?. Australian and New Zealand Journal of Obstetrics and Gynaecology 2009;49(3):274‐8. [DOI] [PubMed] [Google Scholar]
Powell 2007 {published data only}
- Powell Kennedy H, Farrell T, Paden R, Hill S, Jolivet R, Schindler Rising S. A randomized clinical trial of group prenatal care in the military [abstract]. Journal of Midwifery and Women's Health 2007;52(5):532. [Google Scholar]
Prieto 2011 {published data only}
- Prieto G, Torres MT, Frances L, Falguera G, Vila L, Manresa JM, et al. Nutritional status of iodine in pregnant women in Catalonia (Spain): Study on hygiene‐dietetic habits and iodine in urine. BMC Pregnancy and Childbirth 2011;11:17. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sandy 2009 {published data only}
- Sandy JM, Anisfeld E, Ramirez E. Effects of a prenatal intervention on breastfeeding initiation rates in a Latina immigrant sample. Journal of Human Lactation 2009;25(4):404‐11. [DOI] [PubMed] [Google Scholar]
Santelices 2011 {published data only}
- Santelices MP, Guzman GM, Aracena M, Farkas C, Armijo I, Perez‐Salas CP, et al. Promoting secure attachment: evaluation of the effectiveness of an early intervention pilot programme with mother‐infant dyads in Santiago, Chile. Child: Care, Health & Development 2011;37(2):203‐10. [DOI] [PubMed] [Google Scholar]
Sauve 2006 {published data only}
- Sauve N, Powrie RO, Larson L, Phipps M, Weitzen S, Fitzpatrick D, et al. The impact of an information pamphlet on knowledge and anxiety in patients with pre‐eclampsia [abstract]. Hypertension in Pregnancy 2006;25(Suppl 1):174. [Google Scholar]
Schulz 2006 {published data only}
- Schulz MS, Cowan CP, Cowan PA. Promoting healthy beginnings: a randomized controlled trial of a preventive intervention to preserve marital quality during the transition to parenthood. Journal of Consulting & Clinical Psychology 2006;74(1):20‐31. [DOI] [PubMed] [Google Scholar]
Sen 2006 {published data only}
- Sen DM. A randomised controlled trial of a midwife‐led twin antenatal programme ‐ the Newcastle Twin Study. [thesis]. Newcastle: University of Newcastle, 2006. [Google Scholar]
Svensson 2009 {published data only}
- Svensson J, Barclay L, Cooke M. Randomised‐controlled trial of two antenatal education programmes. Midwifery 2009;25(2):114‐25. [DOI] [PubMed] [Google Scholar]
Taghavi 2009 {published data only}
- Taghavi S, Hoseininasab D, Ahmadian heris S. The effect of antenatal education on pain intensity and labor. International Journal of Gynecology & Obstetrics 2009;107(Suppl 2):S493. [Google Scholar]
Thompson 1981 {published data only}
- Thompson JB. Nurse midwives and health promotion during pregnancy. Birth Defects: Original article series 1981;17(6):29‐57. [PubMed] [Google Scholar]
Tough 2007 {published data only}
- Tough S. A randomised controlled trial comparing group to individual prenatal care. Current Controlled Trials (www.controlled‐trials.com/) (accessed 30 October 2007) 2007.
Walkup 2009 {published data only}
- Walkup JT, Barlow A, Mullany BC, Pan W, Goklish N, Hasting R, et al. Randomized controlled trial of a paraprofessional‐delivered in‐home intervention for young reservation‐based American Indian mothers. Journal of the American Academy of Child & Adolescent Psychiatry 2009;48(6):591‐601. [DOI] [PMC free article] [PubMed] [Google Scholar]
Williams 1988 {published data only}
- Williams GE. An analysis of prenatal education classes: an early start to injury prevention. [thesis]. Kansas: University of Kansas, 1988. [Google Scholar]
Wockel 2007 {published data only}
- Wockel A, Schafer E, Beggel A, Abou‐Dakn M. Getting ready for birth: impending fatherhood. British Journal of Midwifery 2007;15(6):344‐8. [Google Scholar]
Wolf 2011 {published data only}
- Wolf M, Bailey S, You W, Grobman WA. Improving patient understanding of preeclampsia: a randomized controlled trial. American Journal of Obstetrics and Gynecology 2011;204(1 Suppl 1):S312. [DOI] [PubMed] [Google Scholar]
Wroe 2005 {published data only}
- Wroe AL, Turner N, Owens RG. Evaluation of a decision‐making aid for parents regarding childhood immunizations. Health Psychology 2005;24(6):539‐47. [DOI] [PubMed] [Google Scholar]
Yim 2005 {published data only}
- Yim IPW. The effect of a theory‐based intervention on promoting self‐efficacy for childbirth amongst pregnant women in Hong Kong. [thesis]. University of Hong Kong, 2005. [Google Scholar]
Additional references
Aldridge 2002
- Aldridge S, Halpern D, Fitzpatrick S. Social Capital, a discussion paper. London: Cabinet Office and Performance and Innovation Unit, 2002. [Google Scholar]
Balaskas 1992
- Balaskas J. Active birth: the new approach to giving birth naturally. Harvard Common Press, 1992. [Google Scholar]
Barclay 1996
- Barclay L, Donovan J, Genovese A. Men's experiences during their partner's first pregnancy: a grounded theory analysis. Australian Journal of Advanced Nursing 1996;13(3):12‐24. [PubMed] [Google Scholar]
Dick‐Read 1933
- Dick‐Read G. Natural childbirth. London: Heinemann, 1993. [Google Scholar]
Gagnon 1995
- Gagnon A, Waghorn K. Survey of women planning to attend childbirth education classes in Montreal. Personal communication 2000.
Lamaze 1958
- Lamaze F. Painless childbirth. Psychoprophylactic method. (translated by Celestin LR). London: Burke, 1958. [Google Scholar]
Lothian 2005
- Lothian J, DeVries, C. The Official Lamaze Guide: giving birth with confidence. Minnetonka: Meadowbrook Press, 2005. [Google Scholar]
Mongan 2005
- Mongan M. Hypnobirthing: the Mongan Method: a natural approach to a safe, easier, more comfortable birthing. 3rd Edition. Florida: Health Communications inc, 2005. [Google Scholar]
Nolan 1997a
- Nolan ML. Antenatal education ‐ where next?. Journal of Advanced Nursing 1997;25(6):1198‐204. [DOI] [PubMed] [Google Scholar]
Nolan 1997b
- Nolan ML, Hicks C. Aims, processes and problems of antenatal education as identified by three groups of childbirth teachers. Midwifery 1997;13(4):179‐88. [DOI] [PubMed] [Google Scholar]
RevMan 2003 [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan). Version 4.2 for Windows. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2003.
Smith 1999
- Smith NJ. Antenatal classes and the transition to fatherhood: a study of some fathers' views. MIDIRS Midwifery Digest 1996;9(3):327‐30. [Google Scholar]
Spiby 1999
- Spiby H, Henderson B, Slade P, Escott D, Fraser RB. Strategies for coping with labour: does antenatal education translate into practice?. Journal of Advanced Nursing 1999;29(2):388‐94. [DOI] [PubMed] [Google Scholar]
Sullivan 1993
- Sullivan PL. Felt learning needs of pregnant women. Canadian Nurse 1993;89(1):42‐5. [PubMed] [Google Scholar]


