Abstract
Objective:
Interpersonal violence is a significant public health problem, with substance use a key risk factor. Intensive longitudinal methods (ILMs) provide data on daily patterns/relationships between substance use and violence, informing prevention. Prior daily research has not focused on these relationships among urban minority samples.
Methods:
Within an RCT comparing ILM assessment/schedule methods, 162-participants completed daily IVR (n = 81) or SMS (n = 81) assessments measuring 19 substance use and violence (partner/non-partner) behaviors daily for 90-days. GLMMs characterized between- and within-person predictors of daily violence.
Results:
Participants [48.7%-female; age = 24.4; 62.3%-African-American; 66.7%-public assistance] completed an average of 46.5 daily reports [SD = 26.7]. Across 90-days, alcohol was characterized by episodic weekend use (average = 10 days-of-use, 34.4% drinking-days involved binge-drinking), while marijuana use was continuous (average = 27 days-of-use; 1.7 times/day), with no weekend differences. Among 118-violent conflicts, 52.5% occurred on weekends; 57.6% were with non-partners/peers; 61.0% involved perpetration/57.6% victimization; and 52.5% involved severe violence. For violence conflicts, 27.1% were preceded by alcohol/22.9% preceded by drug use. Between-person predictors of daily violence included retaliatory attitudes (AOR = 3.2) and anxiety (AOR = 1.1). Within-person predictors included weekends (AOR = 1.6), binge drinking (AOR = 1.9), non-medical prescription opioid use (AOR = 3.5) and illicit drug use (AOR = 8.1).
Conclusion:
Among a high-risk urban minority sample, we found that higher baseline retaliatory attitudes and anxiety, as well as same-day binge drinking, non-medical prescription opioid use, and illicit drug use were associated with daily violence, likely reflecting both pharmacological and socio-contextual factors. Addressing substance use and retaliatory violence with tailored prevention efforts may aid in decreasing negative interpersonal violence outcomes.
Keywords: Intensive longitudinal data, Daily substance use/violence, Emergency medicine, Youth violence
1. Introduction
Homicide is the leading cause of death for African-American adolescents and emerging adults (A/EAs; age-14–24), and the third leading cause of death for A/EAs overall (WISQARS (Web-based injury Statistics Query and Reporting System), 2014). Substance use is an important risk factor for violence, particularly in low-resource, economically-challenged urban communities (Goldstick et al., 2015; Goldstick et al., 2016; Walton et al., 2009; White et al., 2009). As many as 55% of urban A/EAs receiving emergency department (ED) assault-injury treatment report recent substance misuse, with > 20% reporting substance use in the three-hours preceding an assault (Cunningham et al., 2015; Cunningham et al., 2014). Co-occurring substance use and violence has been linked with multiple outcomes, including substance use disorders, anxiety/depression, post-traumatic stress disorder (PTSD), incarceration, violent injury, and death (Cunningham et al., 2015; Cunningham et al., 2014; Cunningham et al., 2009; Gorman-Smith et al., 2004; Walton et al., 2007; Zatzick et al., 2013; Margolin et al., 2010; Boynton-Jarrett et al., 2008; Taylor et al., 2008; Carter et al., 2015; Stoddard et al., 2012; Pailler et al., 2007).
Several theories explain this relationship, including the pharmacological effects of alcohol/drug use (Chermack et al., 2010; Chermack & Giancola, 1997; Cunningham et al., 2006), shared risk/promotive factors (Jessor, 1987), and/or the association of violence with the illicit drug trade (Goldstein, 1985). Pharmacologically, alcohol increases aggression by impairing cognitive processing/impulse control, increasing risk for escalation of low-level conflict (Chermack et al., 2010; Chermack & Giancola, 1997). Acute impairment may increase victimization by impairing cognitive and physical functioning, decreasing risk perception in violent situations (Leonard & Quigley, 1999; Cattaneo et al., 2007). Findings for marijuana and violence are inconsistent. Although marijuana increases anxiety, arousal, confusion, and perceptual distortion in some individuals (Green et al., 2003; Hunault et al., 2014; Karila et al., 2014; Metrik et al., 2011), potentially escalating violent conflict (Ansell et al., 2015), studies generally do not find same-day associations for marijuana use and violence (Ansell et al., 2015; Testa et al., 2018). Instead, this association may reflect withdrawal and/or socio-contextual (e.g., buying/selling drugs) factors that increase violence risk (Goldstein, 1985). Drug use prior to conflict may also be an attempt to self-regulate aggressive impulses, while use following conflict may be an attempt to cope with negative affect resulting from violence (Mercado-Crespo & Mbah, 2013; Martens & Gilbert, 2008; Carter et al., 2017). Understanding these contextual/temporal relationships is key to developing effective prevention strategies.
While cross-sectional/longitudinal analyses have highlighted such relationships, studies are limited by use of aggregated measures (e.g., past 6-month use). Recently, researchers have utilized time-line follow-back (TLFB) methods to characterize daily relationships. Stoddard (Stoddard et al., 2015), examining non-partner violence, found that moderate victimization was more likely on days with alcohol and cocaine use, while severe victimization (e.g., knife/firearm) was more likely on alcohol use days. Moderate/severe aggression was more likely on either alcohol or sedative use days. Epstein-Ngo (Epstein-Ngo et al., 2014) found differential associations by violence type, finding that prescription sedative and opioids were more likely before partner conflicts, while alcohol and concurrent alcohol and marijuana use were more likely before non-partner conflicts. Carter (Carter et al., 2017) found that, in comparison to non-firearm conflicts, firearm conflicts more likely involved same-day marijuana use and that among those reporting firearm conflicts, alcohol, marijuana, and prescription drug use, but not illicit drug use, were higher on conflict (vs. non-conflict) days.
Such studies, while illustrative, are limited by retrospective recall. By contrast, intensive longitudinal methods (ILMs) allow for prospective data collection that assesses behaviors in close proximity to their occurrence, reducing memory-related recall biases and providing greater temporal resolution, ecologic validity, and causal inference (Bolger & Laurenceau, 2013). To date, daily ILM studies of substance use and violence (Testa et al., 2018; Shorey et al., 2017; Shorey et al., 2014; Shorey et al., 2014; Testa & Derrick, 2014; Moore et al., 2011; Stuart et al., 2013; Crane & Eckhardt, 2013; Rothman et al., 2018; Derrick & Testa, 2017; Shorey et al., 2018; Shorey et al., 2016; Shorey et al., 2016) have focused on alcohol or marijuana in relation to partner and/or sexual violence among collegiate youth or adult heterosexual couples. Few (Brown et al., 2018; Sheehan & Lau-Barraco, 2019; Parks et al., 2008; Mulvey et al., 2006; Neal & Fromme, 2007) have examined substance use and a broad range of interpersonal violence (i.e., non-partner/partner) behaviors. Among the few, four (Brown et al., 2018; Sheehan & Lau-Barraco, 2019; Parks et al., 2008; Neal & Fromme, 2007) were conducted in collegiate samples and one (Mulvey et al., 2006) among psychiatric patients. Rothman (Rothman et al., 2018), the only daily study conducted among a non-collegiate urban minority sample, found that while same-day alcohol use was associated with partner violence, it was not a proximal predictor, and same-day marijuana use was not associated with partner violence. Variability between samples likely reflects differences in drinking patterns, highlighting the importance examining multiple contexts/populations. No ILM studies have examined alcohol and/or marijuana in relation to both partner/non-partner violence among a predominantly minority urban sample. Further, no studies have examined other substances in relation to daily violence, which may be important given TLFB findings for illicit/prescription drugs (Stoddard et al., 2015; Epstein-Ngo et al., 2014), or adjusted for key violence risk factors (e.g., retaliation, community violence, mental health) (Cunningham et al., 2015; Carter et al., 2015; Cunningham et al., 2006).
The Flint Youth Injury (FYI-1) Study (Cunningham et al., 2015; Cunningham et al., 2014; Carter et al., 2015; Bohnert et al., 2015) is a two-year longitudinal study characterizing substance use and violence outcomes among a consecutively obtained ED sample of assault-injured youth (ages: 14–24) with past 6-month drug use, and a comparison group of non-assaulted drug-using youth. FYI-1 participants were recontacted to enroll in the FYI-2 study, a seperate randomized control trial (Buu et al., 2017) examining the best assessment (Interactive Voice Response [IVR] vs. Short Message System [SMS]) and schedule (daily-vs.-weekly) methods for collecting ILM data. In the present study, we analyze data from the FYI-2 study to: 1) characterize daily substance use and interpersonal violence behaviors among a minority urban sample; and, 2) examine between- and within-person predictors of daily violence. Results will provide data to support evidence-based violence interventions.
2. Methods
This analysis examines daily data collected via IVR/SMS during the 90-day FYI-2 study. Weekly and control condition data were not included. Procedures were approved by University of Michigan (UM) and Hurley Medical Center (HMC) institutional review boards (IRBs) and an NIH certificate of confidentiality (COC) was obtained. The study was conducted in Flint, Michigan. The FYI-1 sample was originally recruited in the Hurley Medical Center ED, the region’s only Level-1 trauma center. The sample reflects Flint’s socio-demographics (U.S. Census Bureau, 2010; Cunningham et al., 2009; Cunningham et al., 2009; Walton et al., 2010). Flint violence/crime rates are comparable to other urban settings (Federal Bureau of Investigation, 2014).
2.1. Procedures
FYI-2 recruitment (Buu et al., 2017) proceeded in two waves (Cohort-1: 3/2014–9/2014; Cohort-2: 1/2015–1/2016). Eligible participants (agreeing to recontact and not in prison/jail or deceased) were contacted. Following recontact/consent, participants completed a new baseline assessment, consisting of a 30-min self-administered computerized survey ($20-remuneration). Participants were randomized into five experimental groups (IVR daily, IVR weekly, SMS daily, SMS weekly, control). This analysis focuses on the 90-days of data collected in the daily IVR/SMS conditions. Participants were instructed to call (IVR)/text (SMS) the computer system to complete daily assessments. For those not completing assessments, the IVR/SMS system sent a reminder. RAs monitored compliance and contacted participants after missing two consecutive surveys to enhance participation. For cohort-1 (n = 87), remuneration was $1/survey with $10/month for completing > 75% of surveys. To increase compliance, a new payment structure was implemented for cohort-2 (n = 244); a flat $4/survey.
2.2. Measures
2.2.1. Daily measures
Measures were the same regardless of condition (~160-characters/question). The dependent variable was daily violence, defined as any physical altercation between a non-partner (e.g., peer, stranger) or partner (e.g., wife/husband, girlfriend/boyfriend). Daily violence, and the characteristics of conflicts, were measured using eight adapted TLFB Aggression Module (TLFB-AM) items (Chermack et al., 2010; Carter et al., 2017; Stoddard et al., 2015; Epstein-Ngo et al., 2014; Chermack et al., 2006; Chermack & Blow, 2002; Epstein-Ngo et al., 2013). Participants indicated if they were involved in a fight (altercation involving pushing, slapping, kicking, punching, beating up, threatening/using a gun/knife) the prior day (yes/no). For affirmative responses, they identified the combatant (i.e., non-partner/partner) and their own use of alcohol (yes/no) or drugs (yes/no) in the three-hours preceding conflict. Within this context “drugs” referred to either marijuana, illicit drug, or prescription drug use prior to the altercation. Of note, drug use prior to the violent encounter was not characterized by individual type of drug (i.e., illicit drug vs. marijuana use). Four items separately measured type/severity of aggression (i.e., they did to someone) and victimization (i.e., someone did to them) behaviors. Moderate (e.g., shove/grab) and severe (e.g., threaten/use a firearm/knife) behaviors mirrored the Conflict Tactics Scale (CTS-2) (Straus et al., 1996; Straus, 2007). For participants with no violence, alternate questions (e.g., physical activity) (Tucker et al., 2012; California Department of Public Health, 2010) were asked to prevent under-reporting for the purposes of saving time.
Daily substance use (regardless of occurance before or after the episode of violence) was also assessed using six TLFB-substance use module (Sobell et al., 1988; Sobell et al., 1979; Maisto et al., 1979) items from prior work (Carter et al., 2017; Stoddard et al., 2015; Epstein-Ngo et al., 2014; Epstein-Ngo et al., 2013). Participants were asked about prior-day alcohol quantity (i.e., number drinks) and marijuana frequency (i.e., number-of-times). They were also asked about use (yes/no) of illicit drugs (including cocaine, methamphetamine, inhalants, hallucinogens, or street opioids) or non-medical use (yes/no) of prescription drugs, including seperately asking about stimulants, sedatives, or opioids. Non-medical use was defined as using to get high, using more than prescribed, or using someone else’s medications.
2.2.2. Baseline measures
Socio-demographics were measured using Add-Health, SAOM, and DATOS items (Sieving et al., 2001; Handelsman et al., 2005; Add Health, 1997; Smith et al., 1996; Smith et al., 2006). Race/ethnicity (African-American-vs.-other) and relationship status (married/living with someone vs. other) were dichotomized.
The CTS-2 (Straus et al., 1996; Straus, 2007; Wolfe et al., 2001) physical-assault subscale measured past-6-month moderate/severe aggression/victimization behaviors for partners/non-partners. Response scales ranged from 0 (never) to 6 (≥20-times). Items were combined so that positive responses indicated any prior 6-month violence. Retaliatory attitudes were measured using the retaliation subscale of children’s perceptions of environmental violence (Hill & Noblin, 1991). Items were coded/summed such that higher scores indicated more willingness to retaliate (Copeland-Linder et al., 2007). Community violence exposure was assessed with five-items from the “Things Seen/Heard Survey.” (Richters & Saltzman, 1990; Richters & Martinez, 1990) For analysis, a summary score was created.
AUDIT-C (Saunders et al., 1993; Chung et al., 2000) and NIDA-ASSIST (Humeniuk et al., 2008; National Institute on Drug Abuse, 2009) seperately measured past 6-month substance use, including marijuana, illicit drugs, and non-medical prescription drug use. For analysis, alcohol and drug misuse were defined as AUDIT-C ≥ 4 or ASSIST≥4 on any subscale. Past week anxiety and depression symptoms were measured using the 12-item Brief Symptom Index (BSI). (Derogatis & Melisaratos, 1983; Derogatis & Spencer, 1982; Recklitis et al., 2006) Items were summed separately to create anxiety and depression scores. The 17-item civilian PTSD checklist assessed past-month PTSD symptoms. (Weathers et al., 1991) Mean score was used for analysis.
2.3. Analysis
Descriptive statistics were computed. Bivariate analyses were conducted for the dependent variable, daily violence during the 90-days, in relation to baseline factors. Next, we estimated a GLMM of between- and within-person predictors of daily violence using a Bernoulli sampling model and logit link via the GLIMMIX procedure (Snijders & Bosker, 1999; Raudenbush & Bryk, 2002) in SAS. (Institute S, 2011; Allison, 2012) Between-person predictors were included based on theory. (Cunningham et al., 2015; Carter et al., 2015; Cunningham et al., 2006) Due to multicollinearity, not all mental health variables could be included; anxiety was retained given it is a precursor symptom to other mental health conditions (e.g., PTSD).(Gorman-Smith & Tolan, 1998) Similarly, ED visit for violent injury at FYI-1 enrollment and any prior 6-month violence were highly correlated despite the visit occuring ~4 years prior; this was retained as a theoretical indicator of violence involvement severe enough to require medical treatment and to account for FYI-1 design. Baseline alcohol, marijuana, and prescription drug misuse were included to adjust for underlying substance use severity. Daily variables included same-day alcohol, marijuana, illicit drugs, and prescription opioid use. Presciption opioids were included over sedatives/stimulants given higher prevalence. Of note, we used maximum likelihood estimation for all GLMMs, allowing inclusion of participants with at least one daily observation. (Raudenbush & Bryk, 2002).
3. Results
Among 599 FYI-1 participants, 540 were eligible for FYI-2. EAs were ineligible if they were incarcerated (n = 52) or deceased (n = 7). Among eligible participants, 352 (65.2%) were recontacted/consented for FYI-2. The remainder did not consent for re-contact (n = 43), refused participation when they were contacted (n = 43), or were not reachable (n = 102). Baseline characteristics and group differences have been reported. (Buu et al., 2017) Other than sex/race/ethnicity (Female/Black EAs were more likely to enroll in FYI-2), there were no socio-demographic or group (assault-injury-vs.-comparison group) differences between FYI-2/FYI-1. This analysis focuses on the FYI-2 sub-sample (n = 162) completing daily IVR(n = 81)/SMS(n = 81) assessments, of which mean age was 24.4 (SD = 2.3), 62.3% (n = 101) were African-American, 48.7% (n = 79) were female, 66.7% (n = 108) were on public assistance, 39.5% reported living with a partner/being married, and 58.6% (n = 95) were in the FYI-1 assault-injury cohort. Of note, 59.9% (n = 97) reported their highest education was high-school/GED. We found no socio-demographic differences between daily IVR/SMS groups. Across the sample (n = 162), assessments were fully completed on 7541 of 14,580 (51.7%) days, averaging 46.5 daily assessments [SD = 26.7; range = 1–89] per participant. No compliance differences were noted by assessment method or socio-demographics; compliance was lower on weekends vs. weekdays (51.6%-vs-54.5%; p < 0.05) and increased from cohort 1-to-2 (34.1 days-vs.−51.2 days; p < 0.001).
3.1. Substance use/violence at the individual/daily level
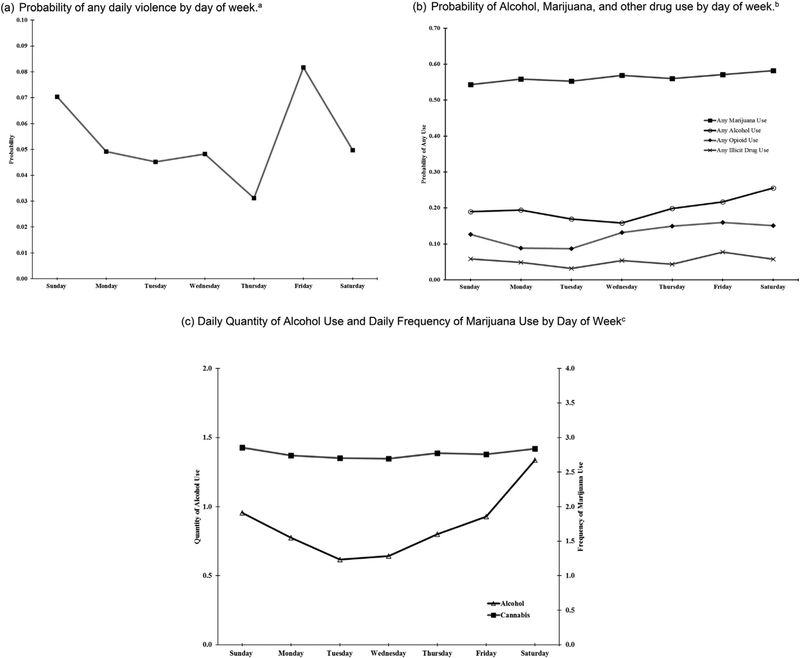
Across 90-days, substance use was high, with 77.8% (n = 126) of participants reporting alcohol, 74.7% (n = 121) marijuana, and 16.7% (n = 27) illicit drug use (Fig. 1). Past-90-day non-medical prescription opioid, stimulant, and sedative use were 25.3% (n = 41), 15.4% (n = 25), and 19.1% (n = 31), respectively. At the daily level, alcohol was reported on 16.5% of days, with 31.2% of drinking-days involved binge drinking and participants averaging of 10 drinking days. Marijuana use was reported on 42.3% of days, with participants averaging 27 days-of-use and using 2.8 times/day on a day of use. While no weekend/weekday differences were identified for marijuana (Fig. 1), alcohol use was highest on weekends (i.e., Friday/Saturday/Sunday). No trends were observed for daily, weekly, or monthly alcohol/drug use.
Fig. 1.
Patterns of Daily Violence, Alcohol, Marijuana, and other Drug Use by Day of Week. (a) Probability of any daily violence by day of week.a (b) Probability of Alcohol, Marijuana, and other drug use by day of week.b (c) Daily Quantity of Alcohol Use and Daily Frequency of Marijuana Use by Day of Weekc.
aData are based on participants who reported at least one incident of violence during the daily diary period. The “day of week” variable is coded so that each day corresponds to the day being reported on, e.g., results for Friday are based on reports completed on Saturday. bData are based on participants who reported at least one occasion of marijuana, alcohol, opioid, or illicit drug use during the daily diary period. Alcohol and Marijuana use are based on a binary coded version of a frequency question. The “day of week” variable is coded so that each day corresponds to the day being reported on, e.g., results for Friday are based on reports completed on Saturday. cAmong those who reported any alcohol use during the daily diary period, the average number of daily drinks was 4.4 (SD = 5.6). Among those who reported any marijuana use during the daily diary period, the average frequency of daily marijuana use was 2.8 (SD = 1.5). The “day of week” variable is coded so that each day corresponds to the day being reported on, e.g., results for Friday are based on reports completed on Saturday.
Across 90-days, 27.2% (n = 44) of participants reported violence, with 65.9% reporting one violent day. Of note, only 9.1% reported > 3 violence days. At the daily level, violent altercations were reported on 1.5% of days (118-conflict days), with 53% occurring on weekends (Fig. 1). Among conflicts, 57.6% occurred with non-partners (42.4% partners). Participants reported 61.0% (n = 72) involved aggression, 57.6% (n = 68) involved victimization, and 43.2% (n = 51) involved both aggression and victimization. Most (52.5%) incidents involved severe violence (e.g., knife/firearms). Among conflicts (n = 118), 45% were preceded by alcohol and/or drug (i.e., marijuana, illicit, or prescription) use, with 27.1% preceded by alcohol and 22.9% by drug use.
3.2. Daily violence correlates at the between-person level
Bivariate analyses (Table 1) comparing baseline characteristics of those reporting and not reporting violent conflicts during the 90-days found that those involved in conflict were less likely African-American and more likely to endorse retaliatory attitudes, community violence exposure, and higher anxiety/depression symptoms. They were also more likely to report marijuana misuse, non-medical prescription drug misuse, and alcohol misuse.
Table 1.
Bivariate comparison of violence involvement at the between-person level (n = 162).
| Any violent conflicts (n = 44, 27.2%) | No violent conflicts (n = 118, 72.8%) | Odds ratio (95% CI) | |
|---|---|---|---|
| Background characteristics | |||
| Age (mean, SD) | 24.0 (2.1) | 24.6 (2.4) | 0.9 (0.8, 1.1) |
| Sex (N, % Female) | 24 (54.5%) | 59 (50.0%) | 1.2 (0.6, 2.4) |
| African-American (n, %)* | 22 (50.0%) | 79 (66.9%) | 0.5 (0.2, 1.0) |
| Public assistance (n, %) | 32 (72.7%) | 76 (64.4%) | 1.5 (0.7, 3.2) |
| 1st wave enrollment | |||
| Violent Injury group (n, %) | 29 (65.9%) | 66 (55.9%) | 1.5 (0.7, 3.1) |
| Past 6-month violence behaviors | |||
| Retaliatory attitudes (mean, SD)* | 2.6 (0.5) | 2.3 (0.5) | 3.2 (1.5, 7.1) |
| Any Violence (n, %)* | 32 (72.7%) | 54 (45.8%) | 3.2 (1.5, 6.7) |
| Community violence (mean, SD)* | 1.4 (0.8) | 0.9 (0.7) | 2.1 (1.3, 3.4) |
| Past 6-month substance use | |||
| Marijuana Misuse (n, %)* | 34 (77.3%) | 65 (55.1%) | 2.8 (1.3, 6.1) |
| Illicit Drug Misuse (n, %) | 3 (6.8%) | 5 (4.2%) | 1.7 (0.4, 7.2) |
| Non-medical prescription stimulant use (n, %) | 4 (9.1%) | 3 (2.5%) | 3.8 (0.8, 17.9) |
| Non-medical prescription sedative use (n, %) | 1 (2.3%) | 4 (3.4%) | 0.7 (0.1, 6.1) |
| Non-medical prescription opioid use (n, %)* | 7 (15.9%) | 6 (5.1%) | 3.5 (1.1, 11.2) |
| Prescription drug misuse (n,%)* | 9 (20.5%) | 7 (5.9%) | 4.1 (1.4, 11.7) |
| AUDIT score (mean, SD)* | 5.4 (6.8) | 3.2 (3.7) | 1.1 (1.0, 1.2) |
| Alcohol misuse (n, %)* | 19 (43.2%) | 33 (28.0%) | 2.0 (1.0, 4.0) |
| Past 6-month mental health | |||
| Anxiety symptoms (mean, SD)* | 4.4 (4.9) | 1.8 (3.1) | 1.2 (1.1, 1.3) |
| Depression symptoms (mean, SD)* | 5.2 (5.5) | 2.5 (3.4) | 1.2 (1.1, 1.3) |
| PTSD symptoms (mean, SD) | 2.4 (1.1) | 1.9 (0.8) | 1.7 (1.0, 3.0) |
Significance levels:
< 0.05,
< 0.01,
< 0.001.
Prescription Drug Misuse – combines misuse of prescription stimulants, sedatives, or opioids.
3.3. Between- and within-person predictors of daily violence
Between- and within-person predictors of daily violence are presented (Table 2). At the individual-level, retaliatory attitudes and anxiety remained significant. In addition to weekends, significant same-day predictors included binge drinking, prescription drug use, and illicit drug use. In terms of effect size, it is notable that a one-unit increase in retaliatory attitudes was associated with a three-fold increase in the odds of daily violence, even after controlling for predictors. Daily illicit drug use emerged as the strongest predictor, with an 8-fold increase in violence. Of note, we tested separate models including cohort assignment (given different compliance rates) and survey day (adjusting for potential assessment-reactivity). Neither was significant or substantively influenced model results (available upon request).
Table 2.
Multi-level logistic regression model characterizing between- and within-person daily level predictors of daily violence incidents.
| AOR (95% CI) | |
|---|---|
| Between-person individual-level variables | |
| Age | 0.8 (0.7–1.0) |
| Sex (female vs. other) | 1.2 (0.6–2.7) |
| African-American | 0.5 (0.2–1.2) |
| Public Assistance | 1.9 (0.8–4.7) |
| Violent Injury Group | 1.7 (0.7–4.0) |
| Retaliatory attitudes* | 3.2 (1.3–7.5) |
| Community violence | 1.3 (0.8–2.3) |
| Alcohol misuse | 0.8 (0.4–1.9) |
| Prescription drug misuse | 1.1 (0.4–3.1) |
| Marijuana misuse | 1.9 (0.7–5.2) |
| Anxiety symptoms* | 1.1 (1.0–1.2) |
| Within-person daily-level variables Weekend day* | 1.6 (1.1–2.5) |
| Binge drinking (> 4 drinks)* | 1.9 (1.0–3.4) |
| Prescription opioid use*** | 3.5 (1.8–7.0) |
| Marijuana use (frequency of use) | 1.0 (0.9–1.2) |
| Illicit drug use (excluding MJ)*** | 8.1 (3.2–20.1) |
Significance levels:
< 0.05,
< 0.01,
< 0.001.
4. Discussion
This is the first ILM analysis to characterize daily relationships between a broad range of substances and interpersonal violence behaviors among a predominantly minority non-collegiate urban sample. We found that binge drinking was twice as likely on conflict days, but temporally preceded violence in only a quarter of conflicts, suggesting a bi-directional association between daily alcohol and violence. Within this sample, alcohol use was primarily episodic with frequent binge drinking, rather than chronic daily use. The episodic binge drinking pattern observed may suggest that alcohol consumption was driven primarily by social-oriented motives (e.g., attending weekend social events with friends where alcohol is available). (Kuntsche et al., 2005) Given that alcohol-involved social situations may enhance contact between those with prior conflict and amplify proactive aggression, retaliatory violence, and/or victimization, this pattern may explain conflicts occurring after or in the context of alcohol use. However, alcohol consumption following conflict may reflect use to cope with negative affect or calm down following altercations. Ecological momentary assessment studies are needed to collect such data, including motives, multiple times per day to further characterize this relationship. In the mean time, findings emphasize the need to include alcohol-specific content within violence interventions and tailor content to address underlying drinking motives/situations given variation in use before/after conflict.
Findings that illicit drugs (excluding marijuana) and prescription drugs are associated with same day violence are novel, given neither has been characterized in relation to daily violence using ILMs. It is important to note that while about one in four conflicts were preceded by any drug use (meaning three in four were not preceeded by other drug use), we were not able to disaggregate this by specific drug to determine temporal ordering of individual drug type before a violent encounter. Illicit drugs, despite lower base rates than other substances, had the strongest association with same-day conflict. This may reflect clustering of co-occurring problem behaviors (Jessor, 1987) among a small subset of violent participants with higher substance use, and/or the association of illicit drugs with violent contexts (e.g., buying/selling drugs). (Goldstein, 1985; Hoaken & Stewart, 2003) Alternatively, given that some illicit (e.g., methamphetamine, cocaine) drugs increase aggression, this may reflect acute pharmacological effects. (Boles & Miotto, 2003) Given that prescription opioids have been shown to decrease aggression, (Boles & Miotto, 2003) our finding that same-day prescription opioid use was three times more likely on conflict days may reflect attempts to self-regulate aggression before conflict, treat pain following assault-injuries, and/or cope with negative affect following conflict. (Mercado-Crespo & Mbah, 2013; Martens & Gilbert, 2008; Carter et al., 2017) Alternatively, this finding may reflect socio-contextual factors, such as opioid users finding themselves in violent situations because they are suffering from withdrawal and attempting to secure more drugs, or because they are committing illegal acts to acquire money for more drugs. (Boles & Miotto, 2003; Catalano et al., 2011; Murphy et al., 2014) To inform interventions, future studies should clarify these relationships with greater temporal resolution and identify motives underlying use on conflict days. Tailoring intervention content to address drug use motives/situational contexts may enhance efficacy, reducing violence outcomes.
We did not find an association between same-day marijuana use and daily violence. Although some prior TLFB studies (Carter et al., 2017; Epstein-Ngo et al., 2014) demonstrate an association between same-day marijuana use and non-partner conflict, and a prior adult EMA study found marijuana predicted impulsivity and interpersonal hostility, (Ansell et al., 2015) our results are consistent with the majority of prior studies demonstrating either no same-day relationship with partner violence (Shorey et al., 2014; Rothman et al., 2018; Buchholz et al., 2017) or that participants are less likely to perpetrate partner violence on use days. (Stuart et al., 2003) Our findings are also consistent with laboratory studies that show marijuana doesn’t routinely increase aggression. (Myerscough & Taylor, 1985) The apparent contradiction in results from prior studies may be explained by newer research suggesting that the relationship between marijuana use and aggression is dose-dependent and related to overall severity of use. (Reingle et al., 2012; Brook et al., 2014; Norström & Rossow, 2014) Recent research has identified that chronic heavier long-term use is associated with increased aggression due to altered neural functioning in the pre-frontal cortex. (Schoeler et al., 2016) Further, there is some evidence that occasional recreational users may experience stronger acute impulsivity effects than chronic users, also potentially explaining positive findings between marijuana and aggression at the daily level in some prior studies. (Theunissen et al., 2012) Third, prior research also indicates that among chronic users with a history of aggression, withdrawal from marijuana is associated with increased partner aggression. (Smith et al., 2013) Future daily research should investigate the possibility of such mechanisms explaining the variability in current research findings, as well as how such relationships may be affected by the increasing potency of marijuana used among community samples. (ElSohly et al., 2016) Despite the lack of an association in our study, it is important to note that the high levels of marijuana use, combined with anxiety as a violence predictor, may be indicative of marijuana use to self-treat anxiety, depression, or PTSD symptoms, all of which are elevated among violence-involved urban samples. (Cunningham et al., 2015; Bohnert et al., 2015) Thus, violence interventions should address higher severity marijuana use and provide mental health referrals for untreated conditions.
Higher retaliatory attitudes were associated with a three-fold higher odds of daily violence. This is consistent with research identifying retaliation as a key motivation for interpersonal violence. (Carter et al., 2015; Carter et al., 2017; Copeland-Linder et al., 2007) The code of the street theory explains this relationship, positing that youth/EAs living in urban settings have informal rules governing social interactions. (Copeland-Linder et al., 2007; Anderson, 1999) Within this context, youth/EAs perceive retaliatory violence as necessary to correct perceived injustices, restore peer respect, and deter future victimization. (Copeland-Linder et al., 2007; Anderson, 1999; Cota-McKinley et al., 2001) Such retaliation may be reactive (i.e., impulsive) or proactive (i.e., planned), emphasizing the need for tailored interventions addressing both subtypes. (Walton et al., 2010; Copeland-Linder et al., 2007) Motivational interventions combining behavioral therapy and cognitive skill building strategies have been efficacious decreasing violence among both universal and selective at-risk ED samples. (Walton et al., 2010; Carter et al., 2016) Within such interventions, skills-based strategies for reactive aggression include addressing emotion regulation, impulse control, and anger management, while proactive aggression strategies include conflict resolution skills or violence alternatives. (Walton et al., 2010; Carter et al., 2016)
Alcohol use and violence were higher on weekends, which was also predictive in the model. This is consistent with research finding that socially-oriented weekends are structurally different than work/school-oriented weekdays, (Finlay et al., 2012) and developmental theories emphasizing that leisure boredom and unstructured socializing increase problem behaviors. (Fergus & Zimmerman, 2005; Wegner & Flisher, 2009; Orcutt, 1984; Iso-Ahola & Crowley, 1991; Columbia Univ. NY, Ny. National Center on Addiction andSubstance Abuse. National Survey of American Attitudes on Substance Abuse Viii, 2003) EAs typically engage in either serious (e.g., community/religious), casual (e.g., “hanging out”), or project-based (e.g., volunteer) leisure activities. (Stebbins, 2007; Stebbins, 1997) Compared with goal-oriented activities promoting skill/knowledge development and supportive mentor relationships, casual activities are unstructured, focus on sensation-seeking or impulsive behaviors, and are often associated with delinquent peers. (Caldwell & Smith, 2006) EAs in disadvantaged urban neighborhoods may face increased barriers (e.g., lack of access/availability, neighborhood safety) to structured program participation, (Molnar et al., 2004) increasing unstructured leisure activities by default. Findings suggest that interventions increasing engagement in structured pro-social activities, especially on weekends, may be beneficial. This is consistent with resilience-based theories, emphasizing healthy development in spite of risk exposure by enhancing access to positive resources and building self-efficacy. (Fergus & Zimmerman, 2005)
While socio-demographics, including gender, were not predictive of violence, it is important to note that half of those reporting violence were female, highlighting the need to construct interventions for both sexes. Of note, 40% were married/living with a partner. This, combined with the finding that ~40% of conflicts (~60% among females) occurred with a partner, highlight the need to incorporate safety planning within interventions. We observed overlap among aggression and victimization behaviors for both partner and non-partner conflicts, with most involving severe behaviors (e.g., knife/gun) with elevated injury risk. Taken together, this emphasizes the need for violence interventions addressing multiple violence types, bi-directional behaviors, and higher severity behaviors (e.g., firearm carriage/use). Further, when considering the increased risk for partner homicide in homes with firearms, (Kellermann et al., 1993; Campbell et al., 2003) findings suggest interventions should include counseling to reduce firearm access during high-risk periods. (Zeoli et al., 2016; Vittes et al., 2013)
Several limitations require attention. First, data were from a high-risk drug-using sample originally recruited while seeking treatment in an urban Emergency Department, limiting generalizability to rural/suburban samples and general community samples. Yet our data may be generalizable to non-collegiate urban samples of high-risk youth and emerging adults with elevated rates of violence involvement not widely studied or characterized in prior literature; regardless replication is required. Second, while prospective ILMs is a strength, daily reports may nevertheless be biased by retrospective recall and/or social desirability. This is mitigated by the short recall period (Follingstad & Rogers, 2013) and privacy/confidentiality. Third, while causal attributions cannot be made unequivocally, assessments did indicate when alcohol preceded violence, providing data suggesting temporal ordering. Preceding drug use, however, was not able to be disaggregated by type, limiting temporal conclusions for illicit/prescription drugs. Future research should aid in clarifying the temporal ordering of individual drug type before subsequent violence encounters. Fourth, missing data for incomplete surveys has potential to bias results if day-specific behaviors are associated with survey completion. Given no gold standard for measuring daily marijuana quantity, our use estimates are limited, especially in the context of varying potency, multiple administration methods, and potential for participants to share marijuana. (Van der Pol et al., 2013) Sixth, we did not assess whether participants had spent time with their partner daily, limiting ability to assess partner violence within the context of daily exposure. While descriptively presented, the number of violence encounters were too small to analyze separately by type/behavior. In addition, rates were too low to assess behavioral reactivity. Yet, it should be noted that violence rates did not differ substantially between the first/second half (1.5%-vs-1.6%, NS) of the study and parallel analyses examining reactivity for daily alcohol/marijuana (Buu et al., 2019) found only short-term measurement reactivity for alcohol during the first week that remitted by the second and none for marijuana. Finally, while self-report data is a potential limitation, it has been shown to be reliable/valid when privacy/confidentially are assured as in our study. (Brener et al., 2003)
5. Conclusion
Limitations notwithstanding, results advance knowledge about substance use and interpersonal violence by focusing on a rarely studied population, examining temporally-organized daily data, and providing insights about contextual factors when substance use may precede violence. Results suggest factors that may both exacerbate and reduce violence, providing useful information to guide prevention. Findings also suggest that daily and ecological momentary assessment research expanding on this data to collect a broader range of contextual factors theorized to be associated with interpersonal violence, including conflict/use motives, firearm carriage, and underlying mood/affect would be a fruitful direction for future research. The closing of the digital divide in urban communities (Anderson & Rainie, 2015) combined with the advancement of m-health technologies, especially mobile applications and passive smarphone and wearable data collection, presents opportunities to leverage technology to collect this broader set of real-time data and will inform the next phase of critical violence interventions.
HIGHLIGHTS.
In a 90-day daily study, alcohol and marijuana were most frequently used substances.
Among 118 violence days, 58% were with non-partners and 61% involved aggression.
Among violent conflicts, 27% preceded by alcohol and 23% preceded by drugs.
Between-person predictors of daily violence were retaliatory attitudes and anxiety.
Same-day binge drinking and illicit/prescription drug use predicted daily violence.
Acknowledgements
The authors wish to acknowledge project staff, including Kaneesha Wallace, M.P.H., Sonia Kamat, M.S., and Wendi Mohl, BS, for their assistance in data and manuscript preparation. Finally, special thanks are owed to the patients and medical staff of the Hurley Medical Center (HMC) for their support of this project.
Role of the funding source
This work was funded by National Institutes of Health/National Institute on Drug Abuse R01DA035183 and R01DA024646. The work was also funded, in part, by Centers for Disease Control and Prevention 1R49CE002099 and National Institutes of Health/National Institute on Drug Abuse K23DA039341. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the funding agencies. Dr. Carter authored the first draft of this manuscript. No honoraria, grants or other form of payment were received for producing this manuscript.
Abbreviations:
- ED
Emergency Department
- HMC
Hurley Medical Center
- UM
University of Michigan
- IRB
Institutional Review Board
- CDC
Centers for Disease Control
Footnotes
Prior Presentations: Society for the Advancement of Violence and Injury Prevention (SAVIR) 2018; College of Problems on Drug Dependence (CPPD) 2018.
Declaration of Competing Interest
None of the authors has any financial interests or relationships relevant to the subject of this manuscript.
References
- Add Health (1997). The National Longitudinal Study of Adolescent to Adult Health. http://www.cpc.unc.edu/projects/addhealth, Accessed date: 5 June 2016.
- Allison PD (2012). Logistic regression using SAS: Theory and application. SAS Institute. [Google Scholar]
- Anderson E (1999). Code of the street: Decency, violence, and the moral life of the inner city. New York: W.W. Norton. [Google Scholar]
- Anderson M, & Rainie L (2015). Pew research center. Technology Device Ownership, 2015, 29. [Google Scholar]
- Ansell EB, Laws HB, Roche MJ, & Sinha R (2015). Effects of marijuana use on impulsivity and hostility in daily life. Drug and Alcohol Dependence, 148, 136–142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bohnert KM, Walton MA, Ranney M, et al. (2015). Understanding the service needs of assault-injured, drug-using youth presenting for care in an urban Emergency Department. Addictive Behaviors, 41, 97–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boles SM, & Miotto K (2003). Substance abuse and violence: A review of the literature. Aggression and Violent Behavior, 8(2), 155–174. [Google Scholar]
- Bolger N, & Laurenceau J-P (2013). Intensive longitudinal methods: An introduction to diary and experience sampling research. Guilford Press. [Google Scholar]
- Boynton-Jarrett R, Ryan LM, Berkman LF, & Wright RJ (2008). Cumulative violence exposure and self-rated health: Longitudinal study of adolescents in the United States. Pediatrics, 122(5), 961–970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brener ND, Billy JO, & Grady WR (2003). Assessment of factors affecting the validity of self-reported health-risk behavior among adolescents: Evidence from the scientific literature. The Journal of Adolescent Health, 33(6), 436–457. [DOI] [PubMed] [Google Scholar]
- Brook JS, Lee JY, Finch SJ, & Brook DW (2014). Developmental trajectories of marijuana use from adolescence to adulthood: Relationship with using weapons including guns. Aggressive Behavior, 40(3), 229–237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown WC, Wang W, & Testa M (2018). Alcohol and Marijuana use in undergraduate males: Between-and Within-Person associations with interpersonal conflict. Cannabis (Research Society on Marijuana), 1(2), 48–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buchholz KR, Bohnert KM, Sripada RK, Rauch SA, Epstein-Ngo QM, & Chermack ST (2017). Associations between PTSD and intimate partner and non-partner aggression among substance using veterans in specialty mental health. Addictive Behaviors, 64, 194–199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buu A, Massey L, Walton MA, Cranford J, Zimmerman MA, & Cunningham RM (2017). Assessment methods and schedules for collecting daily process data on substance use related health behaviors: A randomized control study. Drug & Alcohol Dependence, 178, 159–164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buu A, Yang S, Runze L, Zimmerman MA, Cunningham RM, & Walton MA (2019). Examining measurement reactivity in daily diary data on substance use: Results form a randomized experiment. Under Review. [DOI] [PMC free article] [PubMed]
- Caldwell LL, & Smith EA (2006). Leisure as a context for youth development and delinquency prevention. Australian & New Zealand Journal of Criminology, 39(3), 398–418. [Google Scholar]
- California Department of Public Health (2010). California Teens, Exercise, Eating, Nutrition (CalTEENS) Instrument. [Google Scholar]
- Campbell JC, Webster D, Koziol-McLain J, et al. (2003). Risk factors for femicide in abusive relationships: Results from a multisite case control study. American Jounal Public Health, 93(7), 1089–1097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carter PM, Walton MA, Goldstick J, et al. (2017). Violent Firearm-related conflicts among High-risk Youth: An Event-level and daily calendar analysis. Preventive Medicine, 102, 112–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carter PM, Walton MA, Roehler DR, et al. (2015). Firearm violence among high-risk emergency department youth after an assault injury. Pediatrics, 135(5), 805–815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carter PM, Walton MA, Zimmerman MA, Chermack ST, Roche JS, & Cunningham RM (2016). Efficacy of a universal brief intervention for violence among Urban Emergency Department Youth. Academic Emergency Medicine, 23(9), 1061–1070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Catalano RF, White HR, Fleming CB, & Haggerty KP (2011). Is nonmedical prescription opiate use a unique form of illicit drug use? Addictive Behaviors, 36(1–2), 79–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cattaneo LB, Bell ME, Goodman LA, & Dutton MA (2007). Intimate partner violence victims’ accuracy in assessing their risk of re-abuse. Journal of Family Violence, 22(6), 429–440. [Google Scholar]
- Chermack ST, & Blow FC (2002). Violence among individuals in substance abuse treatment: The role of alcohol and cocaine consumption. Drug and Alcohol Dependence, 66(1), 29–37. [DOI] [PubMed] [Google Scholar]
- Chermack ST, & Giancola PR (1997). The relation between alcohol and aggression: An integrated biopsychosocial conceptualization. Clinical Psychology Review, 17(6), 621–649. [DOI] [PubMed] [Google Scholar]
- Chermack ST, Grogan-Kaylor A, Perron BE, Murray RL, De Chavez P, & Walton MA (2010). Violence among men and women in substance use disorder treatment: A multi-level event-based analysis. Drug and Alcohol Dependence, 112(3), 194–200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chermack ST, Wyrobeck JM, Walton MA, & Blow FC (2006). Distal and proximal factors related to aggression severity among Patients in Substance Abuse Treatment: Family history, Alcohol use and expectancies. Addictive Behaviors, 31(5), 845–858. [DOI] [PubMed] [Google Scholar]
- Chung T, Colby SM, Barnett NP, Rohsenow DJ, Spirito A, & Monti PM (2000). Screening adolescents for problem drinking: performance of brief screens against DSM-IV alcohol diagnoses. Journal of Studies on Alcohol, 61(4), 579–587. [DOI] [PubMed] [Google Scholar]
- Columbia Univ. NY, Ny. National Center on Addiction andSubstance Abuse. National Survey of American Attitudes on Substance Abuse Viii (2003). Teens and Parents. National Center on Addiction and Substance Abuse at Columbia University. [Google Scholar]
- Copeland-Linder N, Jones VC, Haynie DL, Simons-Morton BG, Wright JL, & Cheng TL (2007). Factors associated with retaliatory attitudes among African American adolescents who have been assaulted. Journal of Pediatric Psychology, 32(7), 760–770. [DOI] [PubMed] [Google Scholar]
- Cota-McKinley AL, Woody WD, & Bell PA (2001). Vengeance: Effects of gender, age, and religious background. Aggressive Behavior, 27(5), 343–350. [Google Scholar]
- Crane C, & Eckhardt C (2013). Negative affect, alcohol consumption, and female-to-male intimate partner violence: A daily diary investigation. Partner Abuse, 4(3), 332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunningham R, Knox L, Fein J, et al. (2009). Before and after the trauma bay: The prevention of violent injury among youth. Annals of Emergency Medicine, 53(4), 490–500. [DOI] [PubMed] [Google Scholar]
- Cunningham R, Walton M, Trowbridge M, et al. (2006). Correlates of violent behavior among adolescents presenting to an urban emergency department. The Journal of Pediatrics, 149(6), 770–776. [DOI] [PubMed] [Google Scholar]
- Cunningham R, Walton MA, Weber JE, et al. (2009). One-year medical outcomes and emergency department recidivism after emergency department observation for cocaine-associated chest pain. Annals of Emergency Medicine, 53(3), 310–320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunningham RM, Carter PM, Ranney M, et al. (2015). Violent reinjury and mortality among youth seeking emergency department care for assault-related injury. JAMA Pediatrics, 169(1), 63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunningham RM, Ranney M, Newton M, Woodhull W, Zimmerman M, & Walton MA (2014). Characteristics of youth seeking emergency care for assault injuries. Pediatrics, 133(1), e96–e105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunningham RM, Walton MA, Goldstein A, et al. (2009). Three-month follow-up of brief computerized and therapist interventions for alcohol and violence among teens. Academic Emergency Medicine, 16(11), 1193–1207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derogatis LR, & Melisaratos N (1983). The Brief Symptom Inventory: An introductory report. Psychological Medicine, 13(3), 595–605. [PubMed] [Google Scholar]
- Derogatis LR, & Spencer PM (1982). The Brief Symptom Inventory (BSI): Administration, scoring, and procedures manual. Clinical Psychometric Research: Baltimore, MD. [Google Scholar]
- Derrick JL, & Testa M (2017). Temporal effects of perpetrating or receiving intimate partner aggression on alcohol consumption: A daily diary study of community couples. Journal of Studies on Alcohol and Drugs, 78(2), 213–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ElSohly MA, Mehmedic Z, Foster S, Gon C, Chandra S, & Church JC (2016). Changes in cannabis potency over the last 2 decades (1995–2014): Analysis of current data in the United States. Vol. 79(7), 613–619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epstein-Ngo QM, Cunningham RM, Whiteside LK, et al. (2013). A daily calendar analysis of substance use and dating violence among high risk urban youth. Drug and Alcohol Dependence, 130(1–3), 194–200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epstein-Ngo QM, Walton MA, Chermack ST, Blow FC, Zimmerman MA, & Cunningham RM (2014). Event-level analysis of antecedents for youth violence: Comparison of dating violence with non-dating violence. Addictive Behaviors, 39(1), 350–353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Federal Bureau of Investigation (2014). Annual uniform crime report. 2014 Crime in the United States. [Google Scholar]
- Fergus S, & Zimmerman MA (2005). Adolescent resilience: A framework for understanding healthy development in the face of risk. Annual Review of Public Health, 26, 399–419. [DOI] [PubMed] [Google Scholar]
- Finlay AK, Ram N, Maggs JL, & Caldwell LL (2012). Leisure activities, the social weekend, and alcohol use: Evidence from a daily study of first-year college students. Journal of Studies on Alcohol and Drugs, 73(2), 250–259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Follingstad DR, & Rogers MJ (2013). Validity concerns in the measurement of women’s and men’s report of intimate partner violence. Sex Roles, 69(3–4), 149–167. [Google Scholar]
- Goldstein PJ (1985). The drugs/violence Nexus: A Tripartite conceptual framework. Journal of Drug Issues, 15, 493–506. [Google Scholar]
- Goldstick JE, Lipton RI, Carter P, et al. (2015). The effect of neighborhood context on the relationship between substance misuse and weapons aggression in urban adolescents seeking ED care. Substance Use & Misuse, 50(5), 674–684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstick JE, Stoddard SA, Carter PM, Zimmerman MA, Walton MA, & Cunningham RM (2016). Characteristic substance misuse profiles among youth entering an urban emergency department: neighborhood correlates and behavioral comorbidities. The American Journal of Drug and Alcohol Abuse, 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gorman-Smith D, Henry DB, & Tolan PH (2004). Exposure to community violence and violence perpetration: The protective effects of family functioning. Journal of Clinical Child and Adolescent Psychology, 33(3), 439–449. [DOI] [PubMed] [Google Scholar]
- Gorman-Smith D, & Tolan PH (1998). The role of exposure to community violence and developmental problems in inner-city youth. Development and Psychopathplogy, 10, 101–116. [DOI] [PubMed] [Google Scholar]
- Green B, Kavanagh D, & Young R (2003). Being stoned: A review of self-reported cannabis effects. Drug and Alcohol Review, 22(4), 453–460. [DOI] [PubMed] [Google Scholar]
- Handelsman L, Stein JA, & Grella CE (2005). Contrasting predictors of readiness for substance abuse treatment in adults and adolescents: a latent variable analysis of DATOS and DATOS-A participants. Drug and Alcohol Dependence, 80(1), 63–81. [DOI] [PubMed] [Google Scholar]
- Hill H, & Noblin V (1991). Children’s perceptions of environmental violence. Washington, DC: Howard University. [Google Scholar]
- Hoaken PN, & Stewart SH (2003). Drugs of abuse and the elicitation of human aggressive behavior. Addictive Behaviors, 28(9), 1533–1554. [DOI] [PubMed] [Google Scholar]
- Humeniuk R, Ali R, Babor TF, et al. (2008). Validation of the Alcohol, smoking and substance involvement screening test (ASSIST). Addiction, 103(6), 1039–1047. [DOI] [PubMed] [Google Scholar]
- Hunault CC, Böcker KB, Stellato R, Kenemans JL, de Vries I, & Meulenbelt J (2014). Acute subjective effects after smoking joints containing up to 69 mg Δ9-tetrahydrocannabinol in recreational users: A randomized, crossover clinical trial. Psychopharmacology, 231(24), 4723–4733. [DOI] [PubMed] [Google Scholar]
- Institute S (2011). SAS/IML 9.3 user’s guide. Sas Institute. [Google Scholar]
- Iso-Ahola SE, & Crowley ED (1991). Adolescent substance abuse and leisure boredom. Journal of Leisure Research, 23(3), 260–271. [Google Scholar]
- Jessor R (1987). Problem-behavior theory, psychosocial development, and adolescent problem drinking. British Journal of Addiction, 82(4), 331–342. [DOI] [PubMed] [Google Scholar]
- Karila L, Roux P, Rolland B, et al. (2014). Acute and long-term effects of cannabis use: A review. Current Pharmaceutical Design, 20(25), 4112–4118. [DOI] [PubMed] [Google Scholar]
- Kellermann AL, Rivara FP, Rushforth NB, et al. (1993). Gun ownership as a risk factor for homicide in the home. The New England Journal of Medicine, 329(15), 1084–1091. [DOI] [PubMed] [Google Scholar]
- Kuntsche E, Knibbe R, Gmel G, & Engels R (2005). Why do young people drink? A review of drinking motives. Clinical Psychology Review, 25(7), 841–861. [DOI] [PubMed] [Google Scholar]
- Leonard KE, & Quigley BM (1999). Drinking and marital aggression in newlyweds: An event-based analysis of drinking and the occurrence of husband marital aggression. Journal of Studies on Alcohol, 60(4), 537–545. [DOI] [PubMed] [Google Scholar]
- Maisto SA, Sobell MB, Cooper AM, & Sobell LC (1979). Test-retest reliability of retrospective self-reports in three populations of alcohol abusers. Journal of Behavioral Assessment, 1(4), 315–326. [Google Scholar]
- Margolin G, Vickerman KA, Oliver PH, & Gordis EB (2010). Violence exposure in multiple interpersonal domains: Cumulative and differential effects. Journal of Adolescent Health, 47(2), 198–205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martens K, & Gilbert DG (2008). Marijuana and tobacco exposure predict affect-regulation expectancies in dual users. Addictive Behaviors, 33(11), 1484–1490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mercado-Crespo MC, & Mbah AK (2013). Race and ethnicity, substance use, and physical aggression among US high school students. Journal Interpers Violence, 28(7), 1367–1384. [DOI] [PubMed] [Google Scholar]
- Metrik J, Kahler CW, McGeary JE, Monti PM, & Rohsenow DJ (2011). Acute effects of marijuana smoking on negative and positive affect. Journal of Cognitive Psychotherapy, 25(1), 31–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molnar BE, Gortmaker SL, Bull FC, & Buka SL (2004). Unsafe to play? Neighborhood disorder and lack of safety predict reduced physical activity among urban children and adolescents. American Journal of Health Promotion, 18(5), 378–386. [DOI] [PubMed] [Google Scholar]
- Moore TM, Elkins SR, McNulty JK, Kivisto AJ, & Handsel VA (2011). Alcohol use and intimate partner violence perpetration among college students: Assessing the temporal association using electronic diary technology. Psychology of Violence, 1(4), 315. [Google Scholar]
- Mulvey EP, Odgers C, Skeem J, Gardner W, Schubert C, & Lidz C (2006). Substance use and community violence: A test of the relation at the daily level. Journal of Consulting and Clinical Psychology, 74(4), 743–754. [DOI] [PubMed] [Google Scholar]
- Murphy SM, McPherson S, & Robinson K (2014). Non-medical prescription opioid use and violent behaviour among adolescents. Journal of Child & Adolescent Mental Health, 26(1), 35–47. [DOI] [PubMed] [Google Scholar]
- Myerscough R, & Taylor SP (1985). The effects of marijuana on human physical aggression. Journal of Personality and Social Psychology, 49(6), 1541. [DOI] [PubMed] [Google Scholar]
- National Institute on Drug Abuse (2009). NIDA-Modified ASSIST—Prescreen V1.0. http://www.drugabuse.gov/nidamed/screening/nmassist.pdf, Accessed date: 5 June 2016.
- Neal DJ, & Fromme K (2007). Event-level covariation of alcohol intoxication and behavioral risks during the first year of college. Journal of Consulting and Clinical Psychology, 75(2), 294. [DOI] [PubMed] [Google Scholar]
- Norström T, & Rossow I (2014). Cannabis use and violence: Is there a link? Scandinavian Journal of Public Health, 42(4), 358–363. [DOI] [PubMed] [Google Scholar]
- Orcutt JD (1984). Contrasting effects of two kinds of boredom on alcohol use. Journal of Drug Issues, 14(1), 161–173. [Google Scholar]
- Pailler ME, Kassam-Adams N, Datner EM, & Fein JA (2007). Depression, acute stress and behavioral risk factors in violently injured adolescents. General Hospital Psychiatry, 29(4), 357–363. [DOI] [PubMed] [Google Scholar]
- Parks KA, Hsieh YP, Bradizza CM, & Romosz AM (2008). Factors influencing the temporal relationship between alcohol consumption and experiences with aggression among college women. Psychology of Addictive Behaviors, 22(2), 210–218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raudenbush SW, & Bryk AS (2002). Hierarchical linear models: Applications and data analysis methods. Thousand Oaks, CA: Sage Publications. [Google Scholar]
- Recklitis CJ, Parsons SK, Shih M-C, Mertens A, Robison LL, & Zeltzer L (2006). Factor structure of the brief symptom inventory–18 in adult survivors of childhood cancer: Results from the childhood cancer survivor study. Psychological Assessment, 18(1), 22. [DOI] [PubMed] [Google Scholar]
- Reingle JM, Staras SA, Jennings WG, Branchini J, & Maldonado-Molina MM (2012). The relationship between marijuana use and intimate partner violence in a nationally representative, longitudinal sample. Journal Interpers Violence, 27(8), 1562–1578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richters J, & Saltzman W (1990). Survey of exposure to community violence: Self report version. Rockville, MD: National Institute of Mental Health. [Google Scholar]
- Richters JE, & Martinez P (1990). Things I have seen and heard: A structured interview for assessing young children’s violence exposure. Rockville, MD: National Institute of Mental Health. [Google Scholar]
- Rothman EF, Stuart GL, Temple JR, & Heeren T (2018). Alcohol, marijuana, and dating abuse perpetration by young adults: Results of a daily call study. Violence Against Women, 24(10), 1187–1206. [DOI] [PubMed] [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, Delafuente JR, & Grant M (1993). Development of the Alcohol-Use Disorders Identification Test (Audit) - Who collaborative project on early detection of Persons with Harmful Alcohol-Consumption 2. Addiction, 88(6), 791–804. [DOI] [PubMed] [Google Scholar]
- Schoeler T, Theobald D, Pingault J-B, et al. (2016). Continuity of cannabis use and violent offending over the life course. Psychological Medicine, 46(8), 1663–1677. [DOI] [PubMed] [Google Scholar]
- Sheehan BE, & Lau-Barraco C (2019). A daily diary investigation of self-reported alcohol-related direct and indirect aggression. Aggressive Behavior, 1–9. [DOI] [PubMed] [Google Scholar]
- Shorey RC, Haynes E, Brem M, Florimbio AR, Grigorian H, & Stuart GL (2018). Marijuana use is associated with intimate partner violence perpetration among men arrested for domestic violence. Translational Issues in Psychological Science, 4(1), 108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shorey RC, McNulty JK, Moore TM, & Stuart GL (2016). Being the victim of violence during a date predicts next-day cannabis use among female college students. Addiction, 111(3), 492–498. [DOI] [PubMed] [Google Scholar]
- Shorey RC, McNulty JK, Moore TM, & Stuart GL (2017). Trait anger and partner-specific anger management moderate the temporal association between alcohol use and dating violence. Journal of Studies on Alcohol and Drugs, 78(2), 313–318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shorey RC, Moore TM, McNulty JK, & Stuart GL (2016). Do alcohol and marijuana increase the risk for female dating violence victimization? A prospective daily diary investigation. Psychology of Violence, 6(4), 509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shorey RC, Stuart GL, McNulty JK, & Moore TM (2014a). Acute alcohol use temporally increases the odds of male perpetrated dating violence: A 90-day diary analysis. Addictive Behaviors, 39(1), 365–368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shorey RC, Stuart GL, Moore TM, & McNulty JK (2014b). The temporal relationship between alcohol, marijuana, angry affect, and dating violence perpetration: A daily diary study with female college students. Psychology of Addictive Behaviors, 28(2), 516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sieving RE, Beuhring T, Resnick MD, et al. (2001). Development of adolescent self-report measures from the National Longitudinal study of Adolescent Health. The Journal of Adolescent Health, 28(1), 73–81. [DOI] [PubMed] [Google Scholar]
- Smith GR, Burnam MA, Mosley CL, Hollenberg JA, Mancino M, & Grimes W (2006). Reliability and validity of the substance abuse outcomes module. Psychiatric Services, 57(10), 1452–1460. [DOI] [PubMed] [Google Scholar]
- Smith GR, Ross RL, & Rost KM (1996). Psychiatric outcomes module: Substance Abuse Outcomes Module (SOAM) In Sederer LI, & Dickey B (Eds.). Outcomes assessment in clinical practice (pp. 85–88). Baltimore, MD: Williams & Wilkins. [Google Scholar]
- Smith PH, Homish GG, Leonard KE, & RLJD C (2013). Dependence a. Marijuana withdrawal and aggression among a representative sample of US marijuana users. Vol. 132(1–2), 63–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snijders T, & Bosker R (1999). Multilevel analysis: An introduction to basic and applied multilevel analysis. London: Sage. [Google Scholar]
- Sobell LC, Maisto SA, Sobell MB, & Cooper AM (1979). Reliability of alcohol abusers’ self-reports of drinking behavior. Behaviour Research and Therapy, 17(2), 157–160. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB, Leo GI, & Cancilla A (1988). Reliability of a timeline method: assessing normal drinkers’ reports of recent drinking and a comparative evaluation across several populations. British Journal of Addiction, 83(4), 393–402. [DOI] [PubMed] [Google Scholar]
- Stebbins RA (1997). Casual leisure: A conceptual statement. Leisure Studies, 16(1), 17–25. [Google Scholar]
- Stebbins RA (2007). Serious leisure: A perspective for our time. Vol. 95 Transaction Publishers. [Google Scholar]
- Stoddard SA, Epstein-Ngo Q, Walton MA, et al. (2015). Substance use and violence among Youth: A daily calendar analysis. Substance Use & Misuse, 50(3), 328–339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stoddard SA, Whiteside L, Zimmerman MA, Cunningham RM, Chermack ST, & Walton MA (2012). The relationship between cumulative risk and promotive factors and violent behavior among urban adolescents. American Journal of Community Psychology, 51(1–2), 57–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Straus MA (2007). Conflict tactics scales In Jackson NA (Ed.). Encyclopedia of domestic violence (pp. 824). New York: Routledge: Taylor & Francis Group. [Google Scholar]
- Straus MA, Hamby SL, Boney-McCoy S, & Sugarman DB (1996). The revised conflict tactics scales (CTS2) development and preliminary psychometric data. Journal of Family Issues, 17(3), 283–316. [Google Scholar]
- Stuart GL, Moore TM, Elkins SR, et al. (2013). The temporal association between substance use and intimate partner violence among women arrested for domestic violence. Journal of Consulting and Clinical Psychology, 81(4), 681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stuart GL, Moore TM, Kahler CW, & Ramsey SE (2003). Substance abuse and relationship violence among men court-referred to batterers’ intervention programs. Substance Abuse, 24(2), 107–122. [DOI] [PubMed] [Google Scholar]
- Taylor TJ, Freng A, Esbensen FA, & Peterson D (2008). Youth Gang membership and serious violent victimization: The importance of lifestyles and routine activities. Journal Interpers Violence, 23(10), 1441–1464. [DOI] [PubMed] [Google Scholar]
- Testa M, & Derrick JL (2014). A daily process examination of the temporal association between alcohol use and verbal and physical aggression in community couples. Psychology of Addictive Behaviors, 28(1), 127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Testa M, Derrick JL, Wang W, et al. (2018). Does marijuana contribute to intimate partner aggression? Temporal effects in a community sample of marijuana-using couples. Journal of Studies on Alcohol and Drugs, 79(3), 432–440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Theunissen EL, Kauert GF, Toennes SW, et al. (2012). Neurophysiological functioning of occasional and heavy cannabis users during THC intoxication. Psychopharmacology, 220(2), 341–350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tucker JA, Blum ER, Xie L, Roth DL, & Simpson CA (2012). Interactive voice response self-monitoring to assess risk behaviors in rural substance users living with HIV/AIDS. AIDS and Behavior, 16(2), 432–440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Census Bureau (2010). Quick facts. http://www.census.gov/quickfacts/table/PST045215/26290000,00, Accessed date: 4 June 2016.
- Van der Pol P, Liebregts N, Graaf R, Korf DJ, Brink W, & Laar M (2013). Validation of self-reported cannabis dose and potency: An ecological study. Addiction, 108(10), 1801–1808. [DOI] [PubMed] [Google Scholar]
- Vittes KA, Webster DW, Frattaroli S, Claire BE, & Wintemute GJ (2013). Removing guns from batterers: Findings from a pilot survey of domestic violence restraining order recipients in California. Violence Against Women, 19(5), 602–616. [DOI] [PubMed] [Google Scholar]
- Walton MA, Chermack ST, Shope JT, et al. (2010). Effects of a brief Intervention for reducing violence and Alcohol Misuse Among Adolescents. JAMA, 304(5), 527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walton MA, Cunningham RM, Chermack ST, Maio R, Blow FC, & Weber J (2007). Correlates of violence history among injured patients in an urban emergency department: Gender, substance use, and depression. Journal of Addictive Diseases, 26(3), 61–75. [DOI] [PubMed] [Google Scholar]
- Walton MA, Cunningham RM, Goldstein AL, et al. (2009). Rates and correlates of violent behaviors among adolescents treated in an urban emergency department. The Journal of Adolescent Health, 45(1), 77–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weathers FW, Huska JA, & Keane TM (1991). PCL-C for DSM-IV. Boston: National Center for PTSD-Behavioral Science Division. [Google Scholar]
- Wegner L, & Flisher AJ (2009). Leisure boredom and adolescent risk behaviour: A systematic literature review. Journal of Child and Adolescent Mental Health, 21(1), 1–28. [DOI] [PubMed] [Google Scholar]
- White H, Jackson K, & Loeber R (2009). Developmental sequences and comorbidity of substance use and violence In Krohn M, Lizotte A, & Hall G (Eds.). Handbook of deviance and crime (pp. 433–468). New York, NY: Springer Publications. [Google Scholar]
- WISQARS (Web-based injury Statistics Query and Reporting System) (2014). Centers for Disease Control and Prevention. Injury Prevention and Control. http://www.cdc.gov/injury/wisqars/index.html, Accessed date: 10 March 2017.
- Wolfe DA, Scott K, Reitzel-Jaffe D, Wekerle C, Grasley C, & Straatman AL (2001). Development and validation of the conflict in adolescent dating relationships inventory. Psychological Assessment, 13(2), 277–293. [PubMed] [Google Scholar]
- Zatzick D, Jurkovich G, Rivara FP, et al. (2013). A randomized stepped care intervention trial targeting Posttraumatic stress disorder for surgically hospitalized injury survivors. Annals of Surgery, 257(3), 390–399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeoli AM, Malinski R, & Turchan B (2016). Risks and targeted interventions: Firearms in intimate partner violence. Epidemiologic Reviews, 38(1), 125–139. [DOI] [PubMed] [Google Scholar]